Biofilm Composition Changes During Orthodontic Clear Aligners Compared to Multibracket Appliances: A Systematic Review
Abstract
1. Introduction
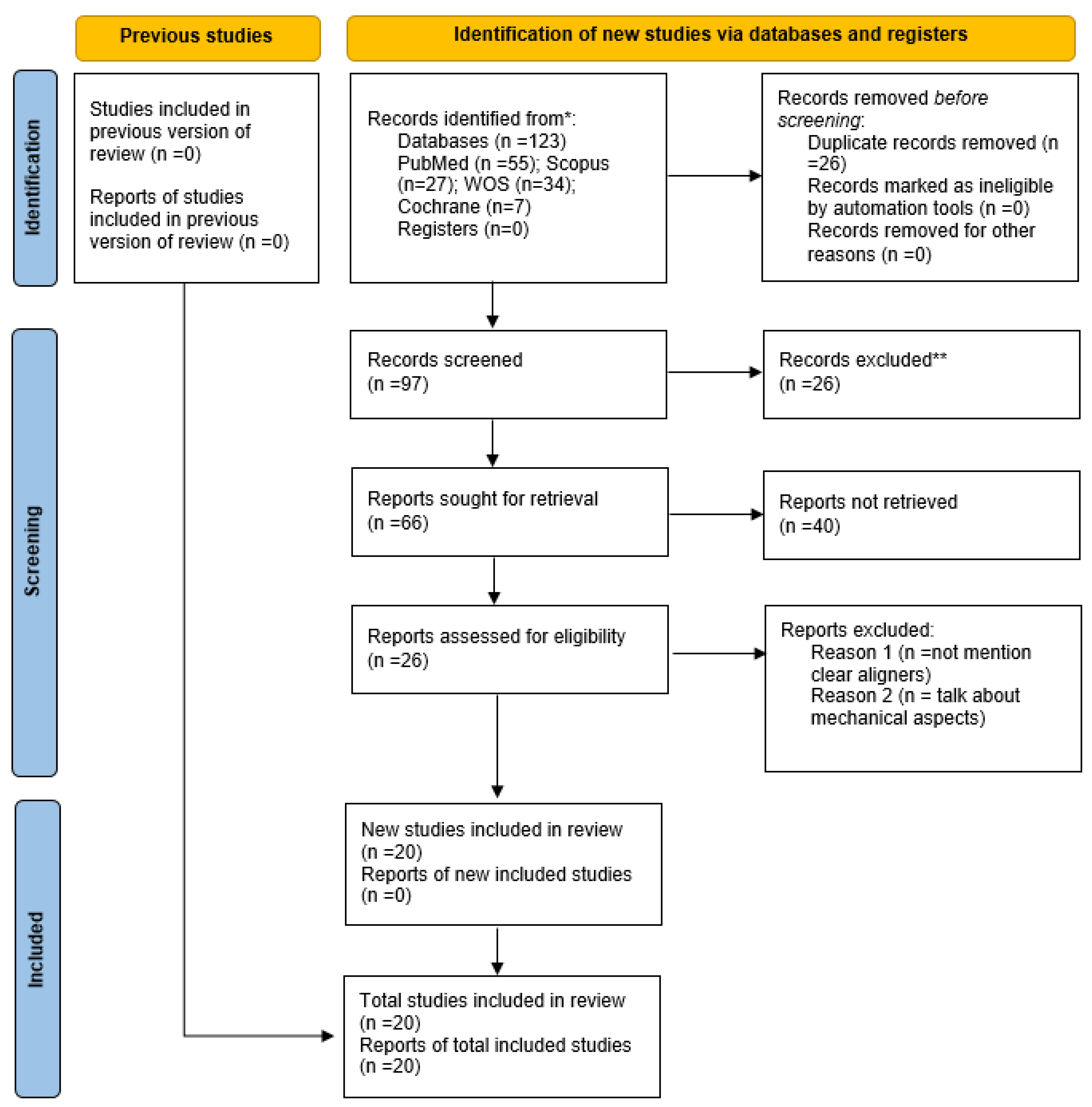
2. Methodology
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. PICO Question
- Population (P): patients using clear aligners as orthodontic treatment.
- Intervention (I): microbiological analysis of the oral biofilm obtained from subgingival or supragingival saliva. The most common methodology used to assess biofilm in the included studies was polymerase chain reaction (PCR) and 16-gene rRNA sequencing in private micro-biology laboratories.
- Comparison (C): group with brackets (self-ligating, lingual, and conventional buccal brackets).
- Outcomes: differences between fixed brackets and clear aligners in the oral microbiota that could affect periodontal status.
2.4. Risk of Biases
2.5. Data Extraction
3. Results
3.1. Analysis of Results
3.2. Subgingival Versus Supragingival Biofilm
3.3. Biofilm Changes in Saliva
3.4. Composition of the Microbiota Before and During Clear Aligner Treatment
3.5. Composition of the Microbiota with Aligners Versus Multibrackets Appliances
3.6. Periodontal Health
3.7. Analysis of Biases
4. Discussion
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kesling, H.D. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am. J. Orthod. Oral. Surg. 1946, 32, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mir, C. Clear Aligner Therapy Might Provide a Better Oral Health Environment for Orthodontic Treatment Among Patients at Increased Periodontal Risk. J. Evid. Based Dent. Pract. 2019, 19, 198–199. [Google Scholar] [CrossRef]
- Pardo, A.; Signoriello, A.; Zangani, A.; Messina, E.; Gheza, S.; Faccioni, P.; Albanese, M.; Lombardo, G. Home Biofilm Management in Orthodontic Aligners: A Systematic Review. Dent. J. 2024, 12, 335. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- España-Pamplona, P.; Bernés-Martínez, L.; Andrés-Castelló, C.; Bolás-Colveé, B.; Adobes-Martín, M.; Garcovich, D. Changes in the Oral Microbiota with the Use of Aligners vs. Braces: A Systematic Review. J. Clin. Med. 2024, 13, 7435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dipalma, G.; Inchingolo, A.D.; Fiore, A.; Balestriere, L.; Nardelli, P.; Casamassima, L.; Di Venere, D.; Palermo, A.; Inchingolo, F.; Inchingolo, A.M. The Differential Impact of Clear Aligners and Fixed Orthodontic Appliances on Periodontal Health: A Systematic Review. Children 2025, 12, 138. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, J.; Zhang, A.-M.; Zhang, Z.-M.; Jia, J.-L.; Sui, X.-X.; Yu, L.; Liu, H.-T. Efficacy of combined orthodontic-periodontic treatment for patients with periodontitis and its effect on inflammatory cytokines: A comparative study. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 494–500. [Google Scholar] [CrossRef]
- Wu, Y.; Cao, L.; Cong, J. The periodontal status of removable appliances vs fixed appliances. A comparative meta-analysis. Medicine 2020, 99, 50. [Google Scholar] [CrossRef]
- Jiang, Y.; Song, B.; Brandt, B.W.; Cheng, L.; Zhou, X.; Exterkate, R.A.M.; Crielaard, W.; Deng, D.M. Comparison of Red-Complex Bacteria Between Saliva and Subgingival Plaque of Periodontitis Patients: A Systematic Review and Meta-Analysis. Front. Cell Infect. Microbiol. 2021, 11, 727732. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, Y.J.; Park, J.; Shin, M.G.; Jung, B.K.; Shin, H.; Cho, S.; Cho, H.I.; Nah, E.H. Distribution and Characteristics of Oral Pathogens According to Blood Glucose Levels in South Korean Health Examinees. Int. J. Mol. Sci. 2025, 26, 2638. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhuang, J.; Ren, Y.; Chen, M.; Yue, M.; Yuan, C.; Duan, R. Efficacy of localized sustained-release drugs in periodontitis and comorbid diabetes: A systematic review and meta-analysis. iScience 2025, 28, 112182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raghav, P.; Khera, A.K.; Bisht, S. Comparative evaluation of antimicrobial properties of silver nanoparticles and chlorhexidine mouthwashes on the colonization of microflora and oral health during orthodontic treatment: A double-blind randomized controlled trial. Dental Press. J. Orthod. 2025, 30, e2524112. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sabuncuoğlu, F.A.; Akgün, Ö.M.; Yıldırım, C.; Azizov, R.; Özgürtaş, T.; Demir, P.; Kaplan, C.; Altun, C. Evaluation of the Effect of Antibacterial Toothpastes Containing Chlorhexidine and Amine Fluoride on Oral Flora in Patients Undergoing Orthodontic Treatment-A Randomised Controlled Trial. Int. J. Dent. Hyg. 2025, 23, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Kredig, C.; Peuckert, E.; Schmidtmann, I.; Drechsler, T.; Erbe, C. Oral health in adolescents: Periodontal inflammatory biomarkers during orthodontic clear aligner therapy. Clin. Oral. Investig. 2025, 29, 168. [Google Scholar] [CrossRef]
- Pasaoglu Bozkurt, A.; Demirci, M.; Erdogan, P.; Kayalar, E. Comparison of microbial adhesion and biofilm formation on different orthodontic aligners. Am. J. Orthod. Dentofacial Orthop. 2025, 167, 47–62. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Zhou, K.; Li, S.; Yue, Z.; Zhang, Q.; Li, Y.; Mi, X. Different Effects of Fixed Appliances and Clear Aligners on the Microbiome and Metabolome of Dental Plaque. Orthod. Craniofac. Res. 2024. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, C.; He, S.; Wang, Q.; Gao, H. The microbiome alterations of supragingival plaque among adolescents using clear aligners: A metagenomic sequencing analysis. Prog. Orthod. 2024, 25, 48. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moradinezhad, M.; Abbasi Montazeri, E.; Hashemi Ashtiani, A.; Pourlotfi, R.; Rakhshan, V. Biofilm formation of Streptococcus mutans, Streptococcus sanguinis, Staphylococcus epidermidis, Staphylococcus aureus, Lactobacillus casei, and Candida albicans on 5 thermoform and 3D printed orthodontic clear aligner and retainer materials at 3 time points: An in vitro study. BMC Oral. Health 2024, 24, 1107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cenzato, N.; Occhipinti, C.; D’amici, E.; Savadori, P.; Baldini, B.; Maspero, C. Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments. Dent. J. 2024, 12, 168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zheng, J.; Wang, X.; Zhang, T.; Jiang, J.; Wu, J. Comparative characterization of supragingival plaque microbiomes in malocclusion adult female patients undergoing orthodontic treatment with removable aligners or fixed appliances: A descriptive cross-sectional study. Front. Cell Infect. Microbiol. 2024, 14, 1350181. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, M.; Chen, J.; Wang, Z.; Wang, Y.; Zhang, Y.; Feng, Q.; Wei, F. Salivary microbiomes vary among orthodontic appliances and associate with clinical periodontal parameters. Orthod. Craniofac Res. 2024, 27, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Chen, J.; Bai, D.; Wang, P.; Shu, R. Effects of clear aligners and traditional removable appliances on oral microbiome in mixed dentition: A comparative study. BMC Oral Health 2024, 24, 1276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rouzi, M.; Jiang, Q.; Zhang, H.; Li, X.; Long, H.; Lai, W. Characteristics of oral microbiota and oral health in the patients treated with clear aligners: A prospective study. Clin. Oral. Investig. 2023, 27, 6725–6734. [Google Scholar] [CrossRef]
- Song, Z.; Fang, S.; Guo, T.; Wen, Y.; Liu, Q.; Jin, Z. Microbiome and metabolome associated with white spot lesions in patients treated with clear aligners. Front. Cell Infect. Microbiol. 2023, 13, 1119616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shokeen, B.; Viloria, E.; Duong, E.; Rizvi, M.; Murillo, G.; Mullen, J.; Shi, B.; Dinis, M.; Li, H.; Tran, N.C.; et al. The impact of fixed orthodontic appliances and clear aligners on the oral microbiome and the association with clinical parameters: A longitudinal comparative study. Am. J. Orthod. Dentofac. Orthop. 2022, 161, e475–e485. [Google Scholar] [CrossRef] [PubMed]
- Cenzato, N.; Marcolongo, L.; Sanchez, S.; Maspero, C.M. Qualitative Microbiological Evaluation of Dental Plaque in Patients with Fixed Appliances and Clear Aligners. J. Biol. Regul. Homeost. Agents 2022, 36, 647–653. [Google Scholar] [CrossRef]
- Lombardo, L.; Palone, M.; Scapoli, L.; Siciliani, G.; Carinci, F. Short-term variation in the subgingival microbiota in two groups of patients treated with clear aligners and vestibular fixed appliances: A longitudinal study. Orthod. Craniofac. Res. 2021, 24, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Nota, A.; Albani, F.; Marchetti, E.; Gatto, R.; Marzo, G.; Quinzi, V.; Tecco, S. Salivary levels of Streptococcus mutans and Lactobacilli and other salivary indices in patients wearing clear aligners versus fixed orthodontic appliances: An observational study. PLoS ONE 2020, 24, 15. [Google Scholar]
- Yan, D.; Liu, Y.; Che, X.; Mi, S.; Jiao, Y.; Guo, L.; Li, S. Changes in the Microbiome of the Inner Surface of Clear Aligners After Different Usage Periods. Curr. Microbiol. 2021, 78, 566–575. [Google Scholar]
- Gujar, A.N.; Al-Hazmi, A.; Raj, A.T.; Patil, S. Microbial profile in different orthodontic appliances by check-erboard DNA-DNA hybridization: An in-vivo study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 49–58. [Google Scholar] [CrossRef]
- Zhao, R.; Huang, R.; Long, H.; Li, Y.; Gao, M.; Lai, W. The dynamics of the oral microbiome and oral health among patients receiving clear aligner orthodontic treatment. Oral Dis. 2020, 26, 473–483. [Google Scholar] [CrossRef]
- Sifakakis, I.; Papaioannou, W.; Papadimitriou, A.; Kloukos, D.; Papageorgiou, S.N.; Eliades, T. Salivary levels of cariogenic bacterial species during orthodontic treatment with thermoplastic aligners or fixed applianc-es: A prospective cohort study. Prog. Orthod. 2018, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Ma, J.B.; Wang, B.; Zhang, X.; Yin, Y.L.; Bai, H. Alterations of the oral microbiome in patients treated with the Invisalign system or with fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2020, 156, 633–640. [Google Scholar] [CrossRef]
- Nagu, P.; Parashar, A.; Behl, T.; Mehta, V. Gut Microbiota Composition and Epigenetic Molecular Changes Connected to the Pathogenesis of Alzheimer’s Disease. J. Mol. Neurosci. 2021, 71, 1436–1455. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Gibiino, G.; Lopetuso, L.R.; Scaldaferri, F.; Rizzatti, G.; Binda, C.; Gasbarrini, A. Exploring Bacteroidetes: Metabolic key points and immunological tricks of our gut commensals. Dig. Liver Dis. 2018, 50, 635–639. [Google Scholar] [CrossRef]
- Ramos, R.T.; Sodré, C.S.; de Sousa Rodrigues, P.M.G.R.; da Silva, A.M.P.; Fuly, M.S.; Dos Santos, H.F.; Gonçalves, L.S.; de Carvalho Ferreira, D.; Ribeiro, M.G. High-throughput nucleotide sequencing for bacteriome studies in oral squamous cell carcinoma: A systematic review. Oral. Maxillofac. Surg. 2020, 24, 387–401. [Google Scholar] [CrossRef] [PubMed]
- Vander Wyst, K.B.; Ortega-Santos, C.P.; Toffoli, S.N.; Lahti, C.E.; Whisner, C.M. Diet, adiposity, and the gut microbiota from infancy to adolescence: A systematic review. Obes. Rev. 2021, 22, e13175. [Google Scholar] [CrossRef]
- Chapple, I.L.; Bouchard, P.; Cagetti, M.G.; Campus, G.; Carra, M.C.; Cocco, F.; Nibali, L.; Hujoel, P.; Laine, M.L.; Lingstrom, P.; et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: Consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S39–S51. [Google Scholar] [CrossRef]
- Alaminos-Torres, A.; Sánchez, M. Identificación del Perfil Socio-Ecológico Ligado a la Nutrición y Salud del Barrio de san Cristóbal de los Ángeles; EPINUT: Tours, France, 2019. [Google Scholar]
- Skoczek-Rubińska, A.; Bajerska, J.; Menclewicz, K. Effects of fruit and vegetables intake in periodontal diseases: A systematic review. Dent. Med. Probl. 2018, 55, 431–439. [Google Scholar] [CrossRef]
- Di Spirito, F.; D’Ambrosio, F.; Cannatà, D.; D’Antò, V.; Giordano, F.; Martina, S. Impact of Clear Aligners versus Fixed Appliances on Periodontal Status of Patients Undergoing Orthodontic Treatment: ASystematic Review of Systematic Reviews. Healthcare 2023, 11, 1340. [Google Scholar] [CrossRef]
- Lucchese, A.; Bondemark, L.; Marcolina, M.; Manuelli, M. Changes in oral microbiota due to orthodontic appliances: A systematic review. J. Oral. Microbiol. 2018, 10, 1476645. [Google Scholar] [CrossRef] [PubMed]
- Contaldo, M.; Lucchese, A.; Lajolo, C.; Rupe, C.; Di Stasio, D.; Romano, A.; Petruzzi, M.; Serpico, R. The Oral Microbiota Changes in Orthodontic Patients and Effects on Oral Health: An Overview. J. Clin. Med. 2021, 10, 780. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Li, J.; Mei, L.; Du, J.; Levrini, L.; Abbate, G.M.; Li, H. Periodontal health during orthodontic treat-ment with clear aligners and fixed appliances: A meta-analysis. J. Am. Dent. Assoc. 2018, 149, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Xavier, G.M.; Cobourne, M.T.; Eliades, T. Effect of orthodontic treatment on the subgin-gival microbiota: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2018, 21, 175–185. [Google Scholar] [CrossRef]
- Perkowski, K.; Baltaza, W.; Conn, D.B.; Marczyńska-Stolarek, M.; Chomicz, L. Examination of oral biofilm microbiota in patients using fixed orthodontic appliances in order to prevent risk factors for health com-plications. Ann. Agric. Environ. Med. 2019, 26, 231–235. [Google Scholar] [CrossRef]
| Author/Year | Funds | Study Type | Sample (n) | Aligners Sample (n Aligners) | Multibrackets Sample (n Multibrackets) | Follow-Up | Analysis |
|---|---|---|---|---|---|---|---|
| Kredig et al., 2025 [13] | Invisalign® Research Award | Prospective study | 50 | 50 | 0 | 1 year | Quantitative analysis |
| Pasaougly et al., 2025 [14] | Not specified | Compative study | 6 | 6 | 0 | 240 days | Quantitative analysis (SM and LA abundance) |
| Gong et al., 2024 [15] | Shanghai Municipal HealthCommission and the National NaturalScience Foundation of China | n-RCT | 20 | 10 | 10 | 6 months | Quantitative and qualitative analysis |
| Wang et al., 2024 [16] | Guangdong Medical Research Fund | n-RCT | 15 | 15 | 0 | 3 months | Qualitative analysis |
| Moradinezhad et al., 2024 [17] | No funding | In vitro | 345 | 270 | 0 | 3 days | Qualitative analysis of selected bacteria |
| Cenzato et al., 2024 [18] | Partial funding Italian Ministry of Health Current research IRCCS | n-RCT | 60 | 20 | 20 | 1 year | Qualitative and semi-quantitative analysis |
| Zheng et al., 2024 [19] | Beijing Natural Science Foundation, University School and Hospital of Stomatology, Peking University School and Hospital of Stomatology First Clinical Division | n-RCT | 48 | 18 | 17 | nAv | Quantitative and qualitative analysis |
| Wang et al., 2024 [20] | National Natural Science Foundationof China and Construction EngineeringSpecial Fund ‘Taishan Scholars’ | n-RCT | 21 | 10 | 11 | 6 months | Qualitative and quantitative analysis (relative abundances) |
| Cheng et al., 2024 [21] | China Oral Health Foundation, National Natural Science Foundation of China, Nature Science Foundation of Sichuan and Align Technology | n-RCT | 25 | 25 | 0 | 6 months | Qualitative analysis |
| Rouzi et al., 2023 [22] | National Nature Science Foundation of China | n-RCT | 15 | 15 | 0 | 3 months | Qualitative and quantitative analysis (abundance of SM) |
| Song et al., 2023 [23] | National Clinical Research Center for Oral Diseases Key Research and Development Program of Shaanxi Province | n-RCT | 55 | 55 | 0 | nAv | Quantitative analysis (relative abundance of selected bacteria) |
| Shokeen et al., 2022 [24] | University of Buffalo and The Forsyth Institute | n-RCT | 12 | 6 | 6 | 12 months | Qualitative analysis, plaque and gingival index. |
| Cenzato et. al., 2022 [25] | No funding. | n-RCT | 16 | 8 | 8 | nAv | Quantitative analysis of selected groups of bacteria. |
| Lombardo et. al., 2021 [26] | No funding. | n-RCT | 27 | 14 | 13 | 6 months | Qualitative analysis |
| Mummolo et al., 2020 [27] | No funding | CC | 80 | 40 | 40 | 6 months | Quantitative analysis (SM and LB abundance) |
| Yan et al., 2020 [28] | National Science Foundation of China. | CH | 8 | 8 | 0 | 24 h | Quantitative (relative abundance) and qualitative analysis (alpha and beta diversity, Shannon Index, Simpson Index) |
| Gujar et al., 2020 [29] | Not specified. | CC | 60 | 20 | 40 | 1 month | Quantitative analysis (Relative abundance) |
| Zhao et al., 2019 [30] | Align Technology. Invisalign® | CH | 25 | 25 | 0 | 6 months | Quantitative (abundance coverage estimator) and qualitative analysis (alpha and beta diversity, Chaol index, Shannon Index, Simpson Index) |
| Sifakakis et al., 2018 [31] | No funding | CH | 30 | 15 | 15 | 1 month | Qualitative analysis (descriptive PCR) |
| Wa et al., 2018 [32] | No specified | CC | 26 | 5 | 5 | 6 months | Qualitative (OUT) and quantitarive analysis (Shannon Index) |
| Author | Population | Intervention | Comparison | Outcomes |
|---|---|---|---|---|
| Pasaougly et al. [14] | In vitro biofilm | Bacterial suspension and optical density of LA and SM on different aligners. | Before treatment; 24 h, 48 h, 72 h, 96 h, 120 h, 168 h, and 240 h after the initiation of treatment; and 1 year post-treatment. | SM and LA formed more biofilm at 120 and 168 h when using Graphy than when using Invisalign (p < 0.05). |
| Moradinezhaz et al. [17] | In vitro specimens | Biofilm analysis using ELISA of microorganisms cultured discs. | Before treatment, and after 24, 72, and 120 h. Comparing plastic materials (polyethylene terephthalate glycol, MMA-free polymer, poly-ethylene, and polyester based on terephthalic acid). | No differences in terms of bacteria growth between plastic materials, but the Candida albicans biofilm was more variable in pattern. |
| Author | Population | Intervention | Comparison | Outcomes |
|---|---|---|---|---|
| Kreding et al. [13] | Fifty adolescent patients (13.3 ± 1.8 years). | Gingival sulcus fluid collected with paper strips. DNA analysis of 11 periodontopathogenic bacteria. | Before treatment. 1 week, 4 weeks, 6 months, 1 year, and 30 months after the start of treatment. One year post-treatment. | Signifcant changes occurred in the orange and green complexes, particularly Capnocytophaga spp. (p = 0.0042) and Fusobacterium spp. (p = 0.0365). |
| Cenzato et al. [18] | Sixty patients (12–65 years old). | Bacterial morphotype analysis of subgingival analysis. | Control group vs. clear aligners vs. fixed bracket appliances. | Clear aligners showed better periodontal bacteria status than conventional brackets. |
| Rouzi et al. [22] | Fifteen patients (19–35 years old) | Subgingival sulculus and plaque from the inner surface of the aligner analyzed via 16S rRNA gene sequencing. | Before treatment, and after 1 and 3 months. | The relative abundance of SM increased significantly during aligner treatment, but the alpha and beta diversity were similar. |
| Lombardo et al. [26] | Twenty-seven patients (13–22 years old) | Subgingival fluid PCR | Fixed appliances vs. clear aligners. Before treatment, 3 and 6 months of treatment. | Total bacterial load did not vary in the clear aligner group, but it did in the bracket group. |
| Author | Population | Intervention | Comparison | Outcomes |
|---|---|---|---|---|
| Gong et al. [15] | Patients between 11 and 34 years old. | Supragingival plaques analyzed by 16S rRNA gene sequiencing and chromatography. | Fixed multibracket appliances vs. clear aligners. Before treatment, after 1–3 months and after 6 months of treatment. | No significant changes were observed in alpha and beta diversity but the relative abundace of Veillonella, Mogibacterium and Actinomyces experienced the most significant changes. |
| Wang et al. [16] | Fifteen adolescents (12–15 yearsold). | Supragingival plaque DNA extraction and metagenomic sequencing. | Before tratment and 3 months of treatment. | Higher relative abundance of Capnocytophaga, Neisseria, and Arachnia after 3 months of treatment. Also the virulence factor associated with type IV pili was higher than before treatment. |
| Zheng et al. [19] | Forty eight female patients (18–38 years old) | 16S rRNA gene sequencing of selected bacteria. | Control vs. bracket vs. aligner. After eating and after brushing teeth. | Actinobacteriota was significantly more prevalent in the control group, Lautropia in the aligner group and Prevotellacae in the brackets group. |
| Wang et al. [20] | Twenty-one patients (11–30 years old) | 16S rDNA gene PCR. | Bracket vs. clear aligner group. Before treatment, three months and six months of treatment. | Beta diversity showed different biofilm in the aligners and bracket group. Periodontopathogens might be more present in the bracket group. |
| Cheng et al. [21] | Twenty five children | Supragingival 16S rDNA gene sequencing | Bedore treatment and after 6 months. | No statistical differences were found between groups and time points (p > 0.05) |
| Shokeen et al. [24] | Twelve patients (8–56 years old) | Supragingival plaque analysis with 16S rRNA gene sequencing. | Fixed bracket vs. clear aligners. After 1, 3, 6 and 12 months of treatment. | Only beta but not alpha communities were diferent between aligner and bracket treatment. Aligner showed better microbial outcomes. |
| Cenzato et al. [25] | Sixteen patients (7–35 years old) | Supragingival plaque sample from lower right first molars gene gram staining procedures. | Fixed appliances vs. clear aligners. | The bracket group showed 25% less gram+ cocci, 50% more Gram− cocci, 40% more gram+ bacilli and 12% more gram− bacilli than aligners group. |
| Yan et al. [28] | Eight female patients (18–25 years) | Inner aligner surface plaque analysis with 16rRNA gene sequencing | Before treatment, after 4, 8, 12 and 24 h. | The beta diversity did not suffer significant increases after 24 months of treatment with aligners. The relative abundances of Firmicutes and Bacteroidales increased while Actinomyces and Rothia decreased. |
| Gujar et al. [29] | Sixty patients | Plaque of the appliance surface with DNA-DNA hybridization. | Clear aligner vs. labial bracket vs. lingual bracket after 30 days of use | Treponema denticola statistically increased in all the appliances. |
| Zhao et al. [30] | Twenty five adult patients | 16S rRNA gene sequiencing | Before and after 6 months of clear aligner treatment (Invisalign). | The biofilm did not change in patients with good oral hygiene and aligners. |
| Authors | Population | Intervention | Comparison | Outcomes |
|---|---|---|---|---|
| Song et al. [23] | Fifty five patients (11–18 years old) | Saliva 16S rRNA gene sequencing and chromatography mass spectrometry. | Control group vs clear aligners after 3 months. | Lachnoanaerobaculum, Rothia, Subdoligranulum and some aminoacids were increased during aligner treatment. |
| Mummolo et al. [27] | Eighty patients (19–24 years old) | Salivary levels of SM and Lactobacillus. | Before treatment, after 3 and 6 months of treatment. | Lower colonizations of SM and Lactobacillus was observed with aligners compared to bracket appliances. |
| Sifikakis et al. [31] | Thirty adolescent patients | Salivary bacterial analysis with PCR | Self-ligating bracket with nickel-titanium archwire vs aligner of polyethylenterephthalat-glycol copolyester. Before, after 2 weeks and 1 month. | Even participants in the aligner group have better hygiene than in the bracket group, no higher loads of SM were observed. |
| Wang et al. [32] | Twenty six patients (20–25 years) | Saliva 16S rRNA analysis | Control vs fixed appliances vs clear aligner (Invisalign) | Firmicutes and Neisseria showed significant differences. Aligners treatment showed disbyiosis being dependent of patient hygiene. |
| JADAD CRITERIA | ||||||
|---|---|---|---|---|---|---|
| Author/Year | Is the Study Described as Randomized? | Is the Study Described as Double-Blinded? | Was There a Description of Withdrawals and Dropouts? | Was the Method of Randomization Adequate? | Was the Method of Blinding Appropriate? | Score |
| Kredig et al., 2025 [13] | 0 | NA | NA | 0 | NA | NA |
| Pasaougly et al., 2025 [14] | 0 | NA | NA | 0 | NA | NA |
| Gong et al., 2024 [15] | 0 | 1 | 1 | 0 | 0 | 2 |
| Wang et al., 2024 [16] | 0 | 1 | 1 | 0 | 0 | 2 |
| Moradinezhard et al., 2024 [17] | 0 | NA | 1 | NA | NA | 1 |
| Cenzato et al., 2024 [18] | 0 | 1 | 1 | 0 | 0 | 2 |
| Zheng et al., 2024 [19] | 0 | 1 | 0 | NA | 0 | 1 |
| Wang et al., 2024 [20] | 0 | 1 | 1 | 0 | 0 | 2 |
| Cheng et al., 2024 [21] | 0 | 1 | 1 | 0 | 0 | 2 |
| Rouzi et al., 2023 [22] | 0 | 1 | 1 | 0 | 0 | 2 |
| Soung et al., [23] | 0 | 1 | 1 | 0 | 0 | 2 |
| Shokeem et al., 2022 [24] | 0 | 1 | 1 | 0 | 0 | 2 |
| Cenzato et al., 2022 [25] | 0 | 0 | 1 | 0 | 0 | 1 |
| Lombardo et al., 2021 [26] | 0 | 0 | 1 | 0 | 0 | 1 |
| Mummolo et al., 2020 [27] | 0 | NA | 0 | NA | NA | NA |
| Yan et al., 2020 [28] | 0 | NA | NA | 0 | NA | NA |
| Gujar et al., 2020 [29] | 0 | NA | NA | 0 | NA | NA |
| Zhao et al., 2019 [30] | 0 | NA | NA | 0 | NA | NA |
| Sifakakis et al., 2018 [31] | 0 | NA | NA | 0 | NA | NA |
| Wang et al., 2018 [32] | 0 | NA | NA | 0 | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belanche Monterde, A.; Flores-Fraile, J.; Pérez Pevida, E.; Zubizarreta-Macho, Á. Biofilm Composition Changes During Orthodontic Clear Aligners Compared to Multibracket Appliances: A Systematic Review. Microorganisms 2025, 13, 1039. https://doi.org/10.3390/microorganisms13051039
Belanche Monterde A, Flores-Fraile J, Pérez Pevida E, Zubizarreta-Macho Á. Biofilm Composition Changes During Orthodontic Clear Aligners Compared to Multibracket Appliances: A Systematic Review. Microorganisms. 2025; 13(5):1039. https://doi.org/10.3390/microorganisms13051039
Chicago/Turabian StyleBelanche Monterde, Alba, Javier Flores-Fraile, Esteban Pérez Pevida, and Álvaro Zubizarreta-Macho. 2025. "Biofilm Composition Changes During Orthodontic Clear Aligners Compared to Multibracket Appliances: A Systematic Review" Microorganisms 13, no. 5: 1039. https://doi.org/10.3390/microorganisms13051039
APA StyleBelanche Monterde, A., Flores-Fraile, J., Pérez Pevida, E., & Zubizarreta-Macho, Á. (2025). Biofilm Composition Changes During Orthodontic Clear Aligners Compared to Multibracket Appliances: A Systematic Review. Microorganisms, 13(5), 1039. https://doi.org/10.3390/microorganisms13051039








