Bacteria That Made History: Detection of Enterobacteriaceae and Carbapenemases in the Waters of Southern Brazil’s Largest Flood
Abstract
1. Introduction
2. Materials and Methods
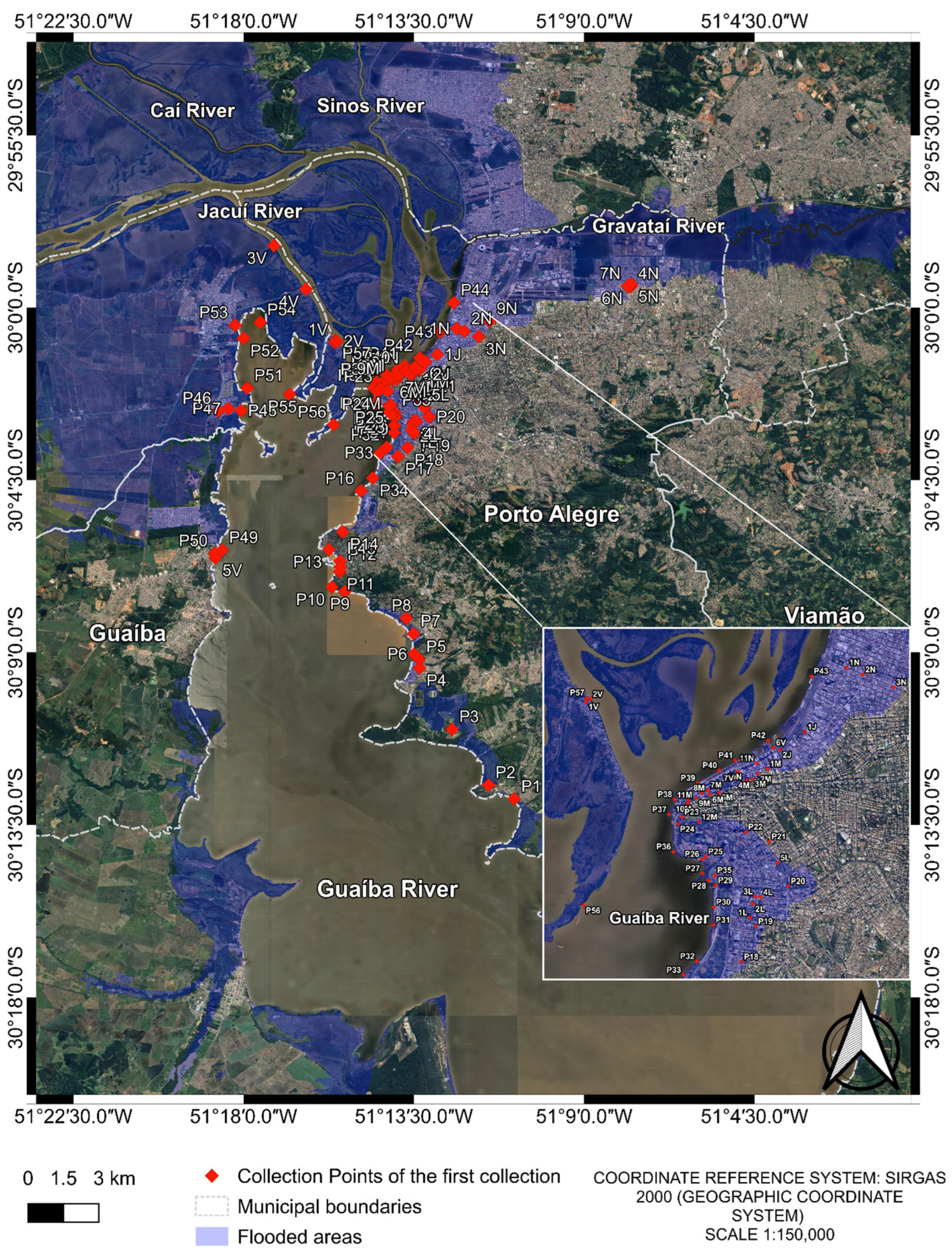
2.1. Water Sample Collection

2.2. Sample Transport
2.3. DNA Extraction from Water Samples
2.4. Detection of Enterobacteriaceae and Carbapenemases Genes by qPCR
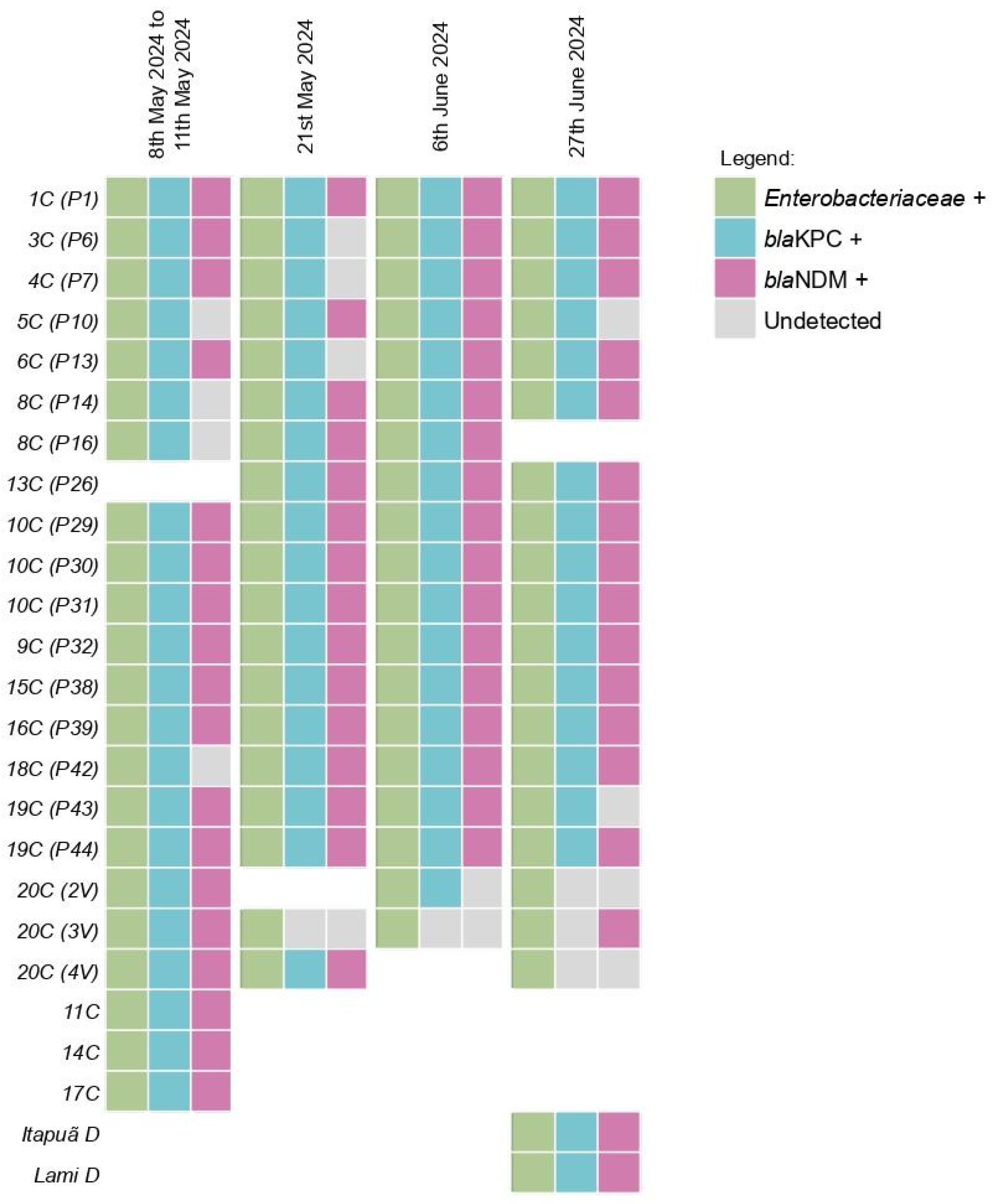
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | Antimicrobial resistantance |
| DNA | Deoxyribonucleic acid |
| qPCR | Quantitative polymerase chain reaction |
| PCR | Polymerase chain reaction |
| ARG | Antimicrobial resistance gene |
| WHO | World Health Organization |
| AIDS | Acquired Immune Deficiency Syndrome |
| HIV | Human Immunodeficiency Virus |
| KPC | Klebsiella pneumoniae carbapenemase |
| NDM | New Delhi metallo-β-lactamase |
| CRE | Carbapenem-resistant Enterobacterales |
| WOAH | World Organisation for Animal Health |
| MGE | Mobile genetic element |
| WBE | Wastewater-based epidemiology |
| NLE | No longer existed |
| NEY | Not exist yet |
Appendix A
| Point | Date 1 5.09 m [38] | Date 2 4.06 m [39] | Date 3 3.21 m [40] | Date 4 3.32 m [41] |
|---|---|---|---|---|
| P1 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P2 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P3 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P4 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P5 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P6 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P7 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P8 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P9 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P10 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P11 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P12 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P13 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P14 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P16 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P17 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P18 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P19 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P20 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P21 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P22 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P23 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P24 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P25 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P26 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P27 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P28 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P29 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P30 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P31 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P32 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P33 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P34 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P35 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P36 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P37 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P38 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P39 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P40 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P41 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| P42 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P43 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P44 | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| P45 | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 1J | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 2J | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 1L | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 2L | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 3L | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 4L | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 5L | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 1M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 2M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 3M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 4M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 5M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 6M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 8M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 9M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 10M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 11M | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 1N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 2N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 3N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 9N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 10N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 11N | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 1V | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 2V | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| 3V | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| 4V | 8 May 2024 to 11 May 2024 | 21 May 2024 | 6 June 2024 | 27 June 2024 |
| 6V | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| 7V | 8 May 2024 to 11 May 2024 | NLE | NLE | NLE |
| Itapuã D | NEY | NEY | NEY | 27 June 2024 |
| Lami D | NEY | NEY | NEY | 27 June 2024 |
References
- Suk, J.E.; Vaughan, E.C.; Cook, R.G.; Semenza, J.C. Natural disasters and infectious disease in Europe: A literature review to identify cascading risk pathways. Eur. J. Public Health 2020, 30, 928–935. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Civil Defense Newsletter of Rio Grande do Sul. Available online: https://www.defesacivil.rs.gov.br/defesa-civil-atualiza-balanco-das-enchentes-no-rs-10-7-66b67813ba21f-66c4eed627af9 (accessed on 10 June 2025).
- Salazar, C.; Giménez, M.; Riera, N.; Parada, A.; Puig, J.; Galiana, A.; Grill, F.; Vieytes, M.; Mason, C.E.; Antelo, V.; et al. Human microbiota drives hospital-associated antimicrobial resistance dissemination in the urban environment and mirrors patient case rates. Microbiome 2022, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- WHO. Ten Threats to Global Health in 2019. World Health Organization (WHO). 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 8 May 2025).
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655, Erratum in Lancet 2022, 400, 1102. [Google Scholar] [CrossRef] [PubMed]
- World Bank Group. Addressing the Grand Pandemic of Antimicrobial Resistance. Available online: https://documents1.worldbank.org/curated/en/099033025183522832/pdf/P174464-c83979e9-4760-49e8-8033-eabf8d0a64ea.pdf (accessed on 8 May 2025).
- WHO. Bacterial Priority Pathogens List, 2024: Bacterial Pathogens of Public Health Importance to Guide Research, Development and Strategies to Prevent and Control Antimicrobial Resistance; World Health Organization: Geneva, Swizterland, 2024. [Google Scholar]
- Bonomo, R.A.; Burd, E.M.; Conly, J.; Limbago, B.M.; Poirel, L.; Segre, J.A.; Westblade, L.F. Carbapenemase-Producing Organisms: A Global Scourge. Clin. Infect. Dis. 2018, 66, 1290–1297. [Google Scholar] [CrossRef]
- Antochevisa, L.C.; Wilhelma, C.M.; Arnsa, B.; Sganzerla, D.; Sudbrackg, L.O.; Nogueirag, T.C.R.L.; Guzmanh, R.D.; Martinsi, A.S.; Cappai, D.S.; de Souza, Â.C.; et al. World Health Organization priority antimicrobial resistance in Enterobacterales, Acinetobacter baumannii, Pseudomonas aeruginosa, Staphylococcus aureus and Enterococcus faecium healthcare-associated bloodstream infections in Brazil (ASCENSION): A prospective, multicentre, observational study. Lancet Reg. Health Am. 2025, 43, 101004. [Google Scholar] [CrossRef]
- National Guide for Sample Collection and Preservation. Available online: https://cetesb.sp.gov.br/wp-content/uploads/2021/10/Guia-nacional-de-coleta-e-preservacao-de-amostras-2012.pdf (accessed on 8 May 2025).
- WHO—World Health Organization. Integrated Surveillance of Antimicrobial Resistance in Foodborne Bacteria: Application of a One Health Approach; World Health Organization: Geneva, Swizterland, 2017. [Google Scholar]
- WOAH—World Organisation for Animal Health. Terrestrial Code, 28th ed.; World Organisation for Animal Health: Paris, France, 2019. [Google Scholar]
- Leimbach, A.; Hacker, J.; Dobrindt, U.E. coli as an all-rounder: The thin line between commensalism and pathogenicity. Curr. Top. Microbiol. Immunol. 2013, 358, 3–32. [Google Scholar] [CrossRef]
- Braz, V.S.; Melchior, K.; Moreira, C.G. Escherichia coli as a Multifaceted Pathogenic and Versatile Bacterium. In Frontiers in Cellular and Infection Microbiology; Frontiers Media SA: Lausanne, Switzerland, 2020; Volume 10. [Google Scholar] [CrossRef]
- Martins, A.F.; Rabinowitz, P. The impact of antimicrobial resistance in the environment on public health. Future Microbiol. 2020, 15, 699–702. [Google Scholar] [CrossRef]
- Ramalho, R.; Mezzomo, L.C.; Machado, W.; da Silva Morais Hein, C.; Müller, C.Z.; da Silva, T.; Jank, L.; Lamas, A.E.; da Costa Ballestrin, R.A.; Wink, P.L.; et al. The occurrence of antimicrobial residues and antimicrobial resistance genes in urban drinking water and sewage in Southern Brazil. Braz. J. Microbiol. 2022, 53, 1483–1489. [Google Scholar] [CrossRef]
- Urase, T.; Goto, S.; Sato, M. Monitoring Carbapenem-Resistant Enterobacterales in the Environment to Assess the Spread in the Community. Antibiotics 2022, 11, 917. [Google Scholar] [CrossRef]
- Tsvetanova, Z.; Boshnakov, R. Resistência antimicrobiana do microbioma de águas residuais em uma estação de tratamento de águas residuais urbanas. Water 2025, 17, 39. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, X.; Luo, L.; Hu, N.; Duan, J.; Tang, Z.; Zhong, R.; Li, Y. Prevalência e Caracterização de Bactérias Produtoras de β-Lactamases e Carbapenemase de Espectro Estendido em Esgoto Hospitalar, Efluentes Tratados e Rios Recebedores. Int. J. Environ. Res. Public Health 2020, 17, 1183. [Google Scholar] [CrossRef]
- Rizzo, L.; Manaia, C.; Merlin, C.; Schwartz, T.; Dagot, C.; Ploy, M.C.; Michael, I.; Fatta-Kassinos, D. Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: A review. Sci. Total Environ. 2013, 447, 345–360. [Google Scholar] [CrossRef]
- Knight, M.E.; Webster, G.; Perry, W.B.; Baldwin, A.; Rushton, L.; Pass, D.A.; Cross, G.; Durance, I.; Muziasari, W.; Kille, P.; et al. National-scale antimicrobial resistance surveillance in wastewater: A comparative analysis of HT qPCR and metagenomic approaches. Water Res. 2024, 262, 121989. [Google Scholar] [CrossRef] [PubMed]
- Arsand, J.B.; Hoff, R.B.; Jank, L.; Bussamara, R.; Dallegrave, A.; Bento, F.M.; Kmetzsch, L.; Falção, D.A.; Peralba, M.D.C.R.; Gomes, A.d.A.; et al. Presence of antibiotic resistance genes and its association with antibiotic occurrence in Dilúvio River in southern Brazil. Sci. Total. Environ. 2020, 738, 139781. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, D.V.; Nunes, L.S.; Barth, A.L.; Van Der Sand, S.T. Genetic Background of β-Lactamases in Enterobacteriaceae Isolates from Environmental Samples. Microb. Ecol. 2017, 74, 599–607. [Google Scholar] [CrossRef]
- Peterson, E.; Kaur, P. Antibiotic Resistance Mechanisms in Bacteria: Relationships Between Resistance Determinants of Antibiotic Producers, Environmental Bacteria, and Clinical Pathogens. Front. Microbiol. 2018, 9, 2928. [Google Scholar] [CrossRef]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.A.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef]
- Choi, P.M.; Tscharke, B.J.; Donner, E.; O’BRien, J.W.; Grant, S.C.; Kaserzon, S.L.; Mackie, R.; O’MAlley, E.; Crosbie, N.D.; Thomas, K.V.; et al. Wastewater-based epidemiology biomarkers: Past, present and future. TrAC Trends Anal. Chem. 2018, 105, 453–469. [Google Scholar] [CrossRef]
- Ahmed, W.; Angel, N.; Edson, J.; Bibby, K.; Bivins, A.; O’Brien, J.W.; Choi, P.M.; Kitajima, M.; Simpson, S.L.; Li, J.; et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020, 728, 138764. [Google Scholar] [CrossRef]
- Hendriksen, R.S.; Munk, P.; Njage, P.; Van Bunnik, B.; McNally, L.; Lukjancenko, O.; Röder, T.; Nieuwenhuijse, D.; Pedersen, S.K.; Kjeldgaard, J.; et al. Global monitoring of antimicrobial resistance based on metagenomics analyses of urban sewage. Nat. Commun. 2019, 10, 1124. [Google Scholar] [CrossRef]
- Su, J.-Q.; An, X.-L.; Li, B.; Chen, Q.-L.; Gillings, M.R.; Chen, H.; Zhang, T.; Zhu, Y.-G. Metagenomics of urban sewage identifies an extensively shared antibiotic resistome in China. Microbiome 2017, 5, 84. [Google Scholar] [CrossRef]
- Aarestrup, F.M.; Woolhouse, M.E.J. Using sewage for surveillance of antimicrobial resistance. Science 2020, 367, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Majeed, H.J.; Riquelme, M.V.; Davis, B.C.; Gupta, S.; Angeles, L.; Aga, D.S.; Garner, E.; Pruden, A.; Vikesland, P.J. Evaluation of Metagenomic-Enabled Antibiotic Resistance Surveillance at a Conventional Wastewater Treatment Plant. Front. Microbiol. 2021, 12, 657954. [Google Scholar] [CrossRef] [PubMed]
- Pazda, M.; Kumirska, J.; Stepnowski, P.; Mulkiewicz, E. Antibiotic resistance genes identified in wastewater treatment plant systems—A review. Sci. Total. Environ. 2019, 697, 134023. [Google Scholar] [CrossRef] [PubMed]
- Charles, F.R.; Lim, J.X.; Chen, H.; Goh, S.G.; He, Y.; Gin, K.Y.-H. Prevalence and characterization of antibiotic resistant bacteria in raw community sewage from diverse urban communities. Sci. Total. Environ. 2022, 825, 153926. [Google Scholar] [CrossRef]
- Liguori, K.; Keenum, I.; Davis, B.C.; Calarco, J.; Milligan, E.; Harwood, V.J.; Pruden, A. Antimicrobial Resistance Monitoring of Water Environments: A Framework for Standardized Methods and Quality Control. Environ. Sci. Technol. 2022, 56, 9149–9160. [Google Scholar] [CrossRef]
- Jeleff, M.; Lehner, L.; Giles-Vernick, T.; Dückers, M.L.; Napier, A.D.; Jirovsky-Platter, E.; Kutalek, R. Vulnerability and One Health assessment approaches for infectious threats from a social science perspective: A systematic scoping review. Lancet Planet. Health 2022, 6, e682–e693. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Tang, X.; Liu, J.; Visbeck, M.; Guo, H.; Murray, V.; Mcgillycuddy, C.; Ke, B.; Kalonji, G.; Zhai, P.; et al. From concept to action: A united, holistic and One Health approach to respond to the climate change crisis. Infect. Dis. Poverty 2022, 11, 17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gongal, G.; Ofrin, R.H. Animal welfare, One Health and emergency preparedness and response in the Asia-Pacific region. WHO South-East Asia J. Public Health 2020, 9, 50–51. [Google Scholar] [CrossRef] [PubMed]
- Guaíba Water Level: Updated Forecasts. Available online: https://www.ufrgs.br/iph/previsoes-atualizadas-de-niveis-dagua-no-guaiba-quarta-feira-08-05-24-12h/ (accessed on 8 May 2025).
- Guaíba Water Level: Updated Forecasts. Available online: https://www.ufrgs.br/iph/previsoes-atualizadas-de-niveis-dagua-no-guaiba-terca-feira-21-05-24-12h/ (accessed on 8 May 2025).
- Guaíba Water Level: Updated Forecasts. Available online: https://www.ufrgs.br/iph/previsoes-atualizadas-de-niveis-dagua-no-guaiba-quinta-feira-06-06-24-12h/ (accessed on 8 May 2025).
- Guaíba Water Level: Updated Forecasts. Available online: https://www.ufrgs.br/iph/previsoes-atualizadas-de-niveis-dagua-no-guaiba-sexta-feira-28-06-24-12h/ (accessed on 8 May 2025).
| Pool Identification | Collection Point |
|---|---|
| 1C | P1, P2 e P3 |
| 3C | P4, P5 e P6 |
| 4C | P7 e P8 |
| 5C | P9, P10 e P11 |
| 6C | P12, P45 e P13 |
| 8C | P14, P16 e P34 |
| 9C | P17, 18, P32 e 33 |
| 10C | P29, P30 e P31 |
| 11C | P19, 1L, 2L, 3L e 4L |
| 13C | P28, P27, P35, P25 e P26 |
| 14C | P20, 5L, P21 e P22 |
| 15C | P36, P24, P37, P23 e P38 |
| 16C | 10M, 11M, 9M, 8M, 6M, 5M, 7V, P39 e P40 |
| 17C | P41, 10N, 4M, 3M, 2M, 11N e 1M |
| 18C | P42, 6V, 2J e 1J |
| 19C | P43, 1N, 2N, 3N, 9N e P44 |
| 20C | 3V, 4V, 2V e 1V |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardoso, J.V.B.; Pereira, D.C.; Matos, W.L.; de Oliveira, G.S.; de Carvalho, V.R.; Albornoz, L.L.; Barth, A.L.; da Silva, S.W.; Martins, A.F. Bacteria That Made History: Detection of Enterobacteriaceae and Carbapenemases in the Waters of Southern Brazil’s Largest Flood. Microorganisms 2025, 13, 2365. https://doi.org/10.3390/microorganisms13102365
Cardoso JVB, Pereira DC, Matos WL, de Oliveira GS, de Carvalho VR, Albornoz LL, Barth AL, da Silva SW, Martins AF. Bacteria That Made History: Detection of Enterobacteriaceae and Carbapenemases in the Waters of Southern Brazil’s Largest Flood. Microorganisms. 2025; 13(10):2365. https://doi.org/10.3390/microorganisms13102365
Chicago/Turabian StyleCardoso, João Vitor Barboza, Dariane Castro Pereira, William Latosinski Matos, Gabriela Simões de Oliveira, Victória Rodrigues de Carvalho, Louidi Lauer Albornoz, Afonso Luis Barth, Salatiel Wohlmuth da Silva, and Andreza Francisco Martins. 2025. "Bacteria That Made History: Detection of Enterobacteriaceae and Carbapenemases in the Waters of Southern Brazil’s Largest Flood" Microorganisms 13, no. 10: 2365. https://doi.org/10.3390/microorganisms13102365
APA StyleCardoso, J. V. B., Pereira, D. C., Matos, W. L., de Oliveira, G. S., de Carvalho, V. R., Albornoz, L. L., Barth, A. L., da Silva, S. W., & Martins, A. F. (2025). Bacteria That Made History: Detection of Enterobacteriaceae and Carbapenemases in the Waters of Southern Brazil’s Largest Flood. Microorganisms, 13(10), 2365. https://doi.org/10.3390/microorganisms13102365






