Identification and Genetic Characterization of a Strain of African Horse Sickness Virus Serotype 1 and Its Safety Evaluation in a Mouse Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Virus Strain and Cell Culture
2.2. Virus Resuscitation
2.3. AHSV/M Adaptation to Cell Culture
2.4. Virus Titration
2.5. Plaque Purification
2.6. Determination of Virus Growth Curve
2.7. RT-PCR (Reverse Transcription Polymerase Chain Reaction)
2.8. Virus Neutralization Test
2.9. IFA (Immunofluorescence Assay)
2.10. Whole-Genome Sequencing and Analysis
2.11. Safety Evaluation of AHSV/C in a Mouse Model
3. Results and Discussion
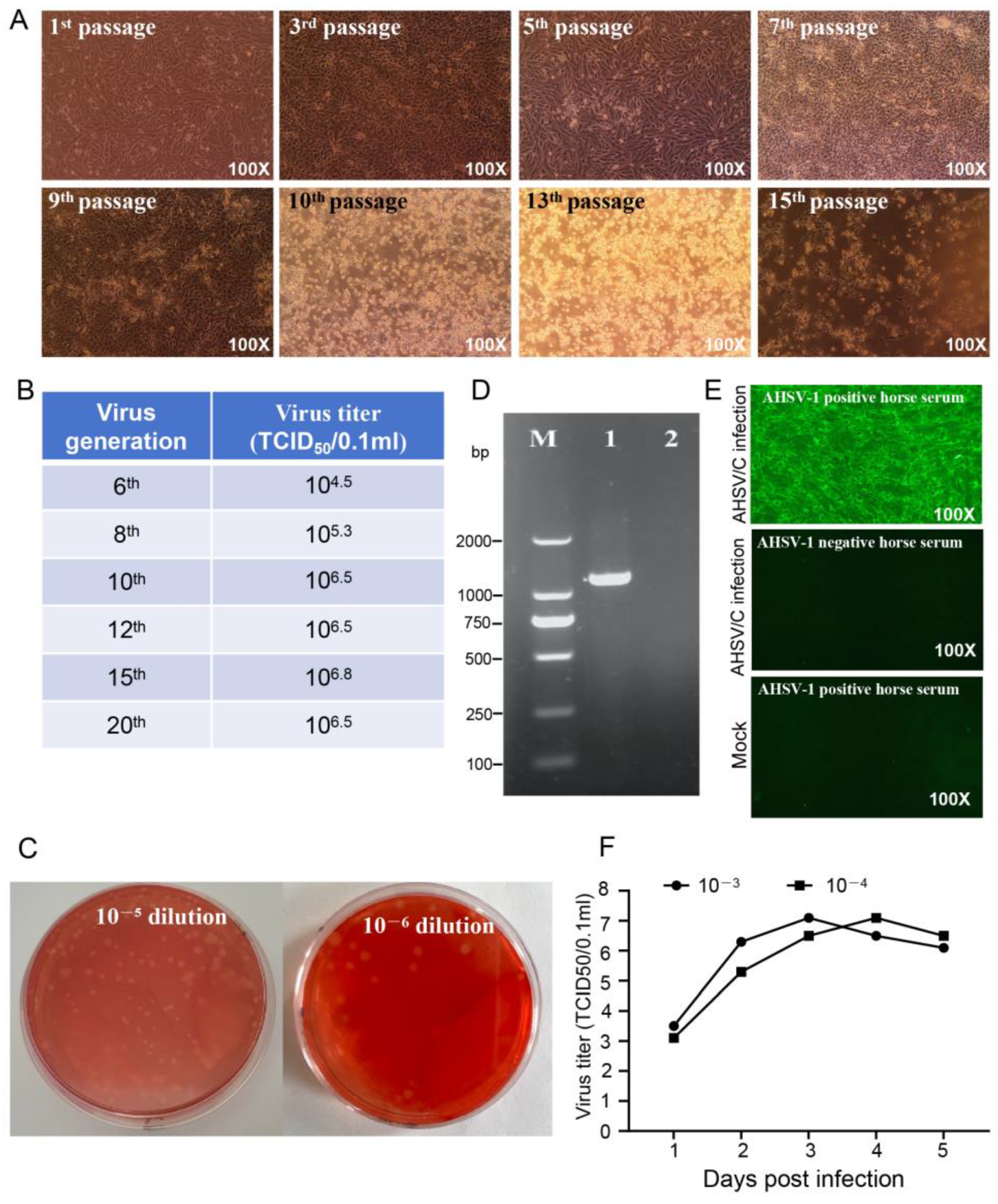
3.1. Characterization of AHSV/C Strain
3.2. Genomic Characterization and Phylogenetic Analysis of AHSV/C
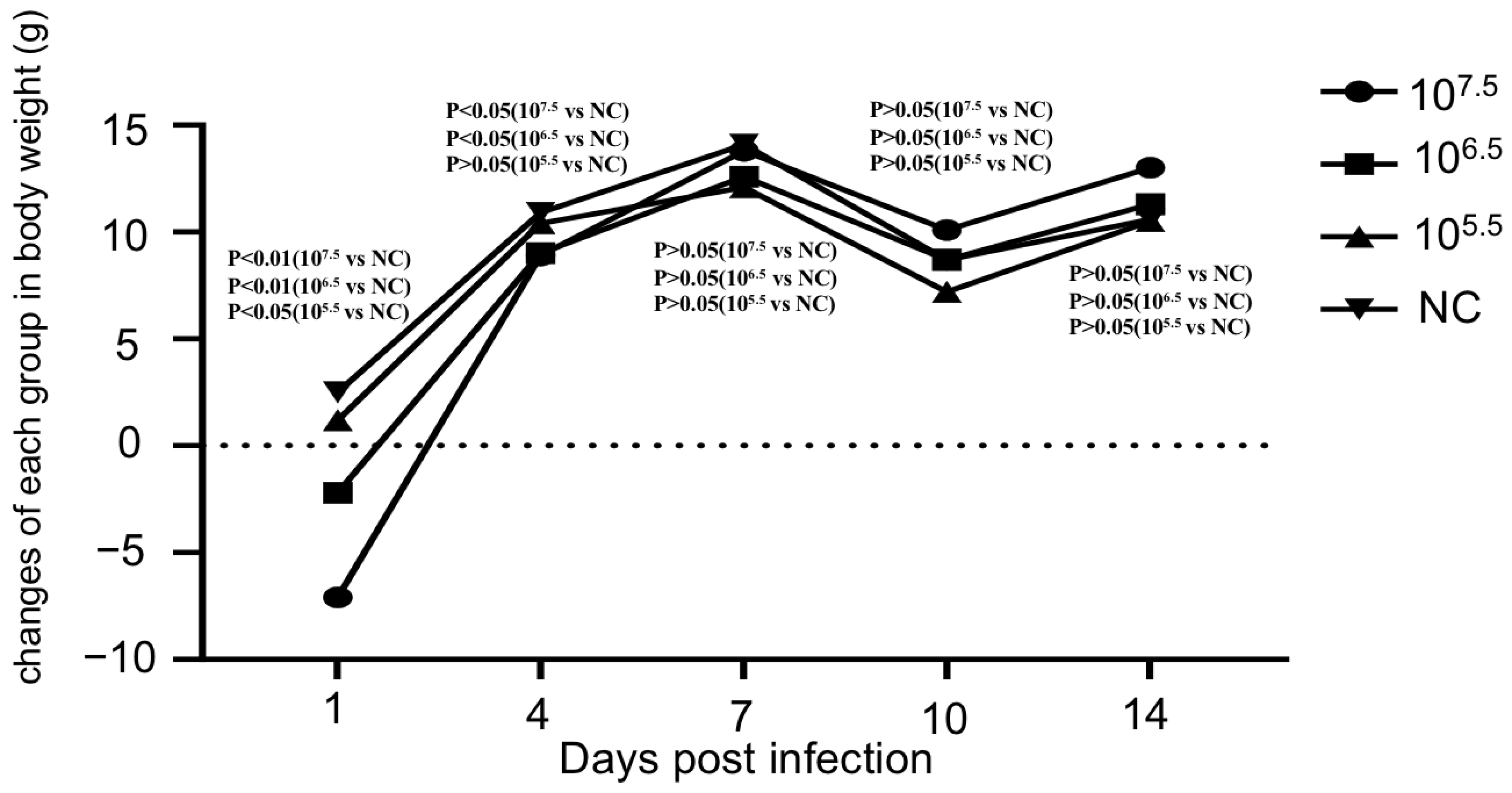
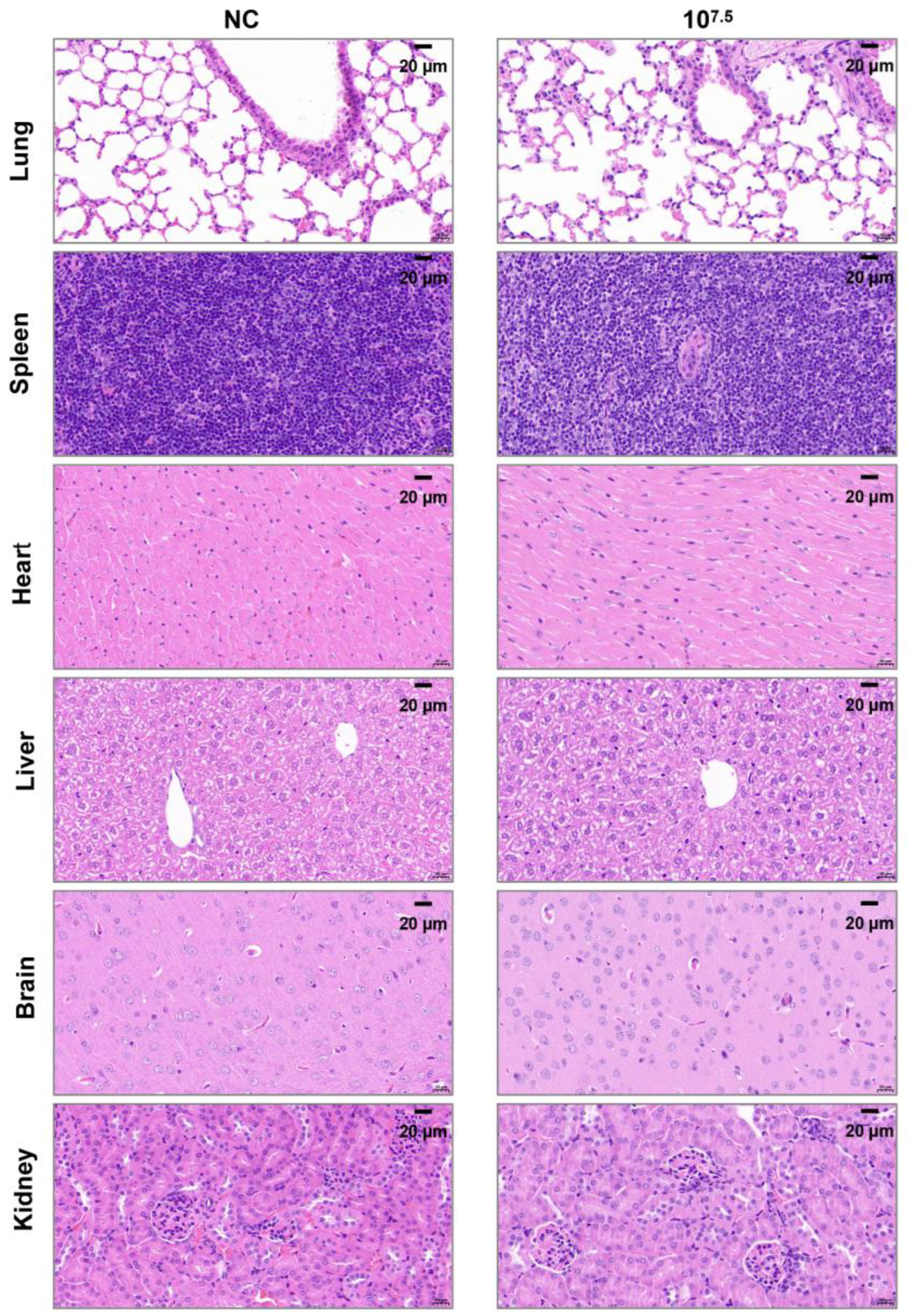
3.3. Safety Evaluation of AHSV/C in a Mouse Model
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHSV | African horse sickness virus |
| AHS | African horse sickness |
| RT-PCR | Reverse transcription polymerase chain reaction |
| LD50 | Lethal dose, 50% |
| TCID50 | 50% tissue culture infectious dose |
| PBS | Phosphate-buffered saline |
References
- Department of Veterinary Services Malaysia. African Horse Sickness in Malaysia. 2020. Available online: https://rr-asia.woah.org/app/uploads/2020/11/malaysia_ahs-situation_10nov2020.pdf (accessed on 25 September 2025).
- Bunpapong, N.; Charoenkul, K.; Nasamran, C.; Chamsai, E.; Udom, K.; Boonyapisitsopa, S.; Tantilertcharoen, R.; Kesdangsakonwut, S.; Techakriengkrai, N.; Suradhat, S.; et al. African Horse Sickness Virus Serotype 1 on Horse Farm, Thailand, 2020. Emerg. Infect. Dis. 2021, 27, 2208–2211. [Google Scholar] [CrossRef]
- Dennis, S.J.; Meyers, A.E.; Hitzeroth, I.I.; Rybicki, E.P. African Horse Sickness: A Review of Current Understanding and Vaccine Development. Viruses 2019, 11, 844. [Google Scholar] [CrossRef]
- WOAH. Terrestrial Animal Health Code, Chapter 12.1—Infection with African Horse Sickness Virus; 2024 ed.; WOAH: Paris, France, 2024. [Google Scholar]
- Van Rensberg, I.B.; De Clerk, J.; Groenewald, H.B.; Botha, W.S. An outbreak of African horsesickness in dogs. J. S. Afr. Vet. Assoc. 1981, 52, 323–325. [Google Scholar]
- Kandeel, M.; Al-Mubarak, A.I.A. Camel viral diseases: Current diagnostic, therapeutic, and preventive strategies. Front. Vet. Sci. 2022, 9, 915475. [Google Scholar] [CrossRef] [PubMed]
- Hanekom, J.; Lubisi, B.A.; Leisewitz, A.; Guthrie, A.; Fosgate, G.T. The seroprevalence of African horse sickness virus, and risk factors to exposure, in domestic dogs in Tshwane, South Africa. Prev. Vet. Med. 2023, 213, 105868. [Google Scholar] [CrossRef]
- Alexander, K.A.; Kat, P.W.; House, J.; House, C.; O’Brien, S.J.; Laurenson, M.K.; McNutt, J.W.; Osburn, B.I. African horse sickness and African carnivores. Vet. Microbiol. 1995, 47, 133–140. [Google Scholar] [CrossRef] [PubMed]
- WOAH. Terrestrial Manual-Section 3.6. Equidae-Chapter 3.6.1-African Horse Sickness (Infection with African Horse Sickness Virus); WOAH: Paris, France, 2019. [Google Scholar]
- Erasmus, B.J. Cultivation of Horsesickness Virus in Tissue Culture. Nature 1963, 200, 716. [Google Scholar] [CrossRef] [PubMed]
- MacLachlan, N.J.; Dubovi, E.J. (Eds.) Reoviridae. In Fenner’s Veterinary Virology, 5th ed.; Academic Press: Boston, MA, USA, 2017; pp. 299–317. [Google Scholar]
- O’Hara, R.S.; Meyer, A.J.; Burroughs, J.N.; Pullen, L.; Martin, L.A.; Mertens, P.P. Development of a mouse model system, coding assignments and identification of the genome segments controlling virulence of African horse sickness virus serotypes 3 and 8. Arch. Virol. Suppl. 1998, 14, 259–279. [Google Scholar]
- Ozawa, Y. Studies on the replication of African horse-sickness virus in two different cell line cultures. Archiv für die gesamte Virusforsch. 1967, 21, 155–169. [Google Scholar] [CrossRef]
- Wilson, A.; Mellor, P.S.; Szmaragd, C.; Mertens, P.P. Adaptive strategies of African horse sickness virus to facilitate vector transmission. Vet. Res. 2009, 40, 16. [Google Scholar] [CrossRef]
- Zwart, L.; Potgieter, C.A.; Clift, S.J.; van Staden, V. Characterising Non-Structural Protein NS4 of African Horse Sickness Virus. PLoS ONE 2015, 10, e0124281. [Google Scholar] [CrossRef] [PubMed]
- Boughan, S.; Potgieter, A.C.; van Staden, V. African horse sickness virus NS4 is a nucleocytoplasmic protein that localizes to PML nuclear bodies. J. Gen. Virol. 2020, 101, 366–384. [Google Scholar] [PubMed]
- Bekker, S.; Potgieter, C.A.; van Staden, V.; Theron, J. Investigating the Role of African Horse Sickness Virus VP7 Protein Crystalline Particles on Virus Replication and Release. Viruses 2022, 14, 2193. [Google Scholar] [CrossRef] [PubMed]
- Maree, S.; Durbach, S.; Maree, F.F.; Vreede, F.; Huismans, H. Expression of the major core structural proteins VP3 and VP7 of African horse sickness virus, and production of core-like particles. Arch. Virol. Suppl. 1998, 14, 203–209. [Google Scholar]
- van Staden, V.; Smit, C.C.; Stoltz, M.A.; Maree, F.F.; Huismans, H. Characterization of two African horse sickness virus nonstructural proteins, NS1 and NS3. Arch. Virol. Suppl. 1998, 14, 251–258. [Google Scholar]
- Stassen, L.; Huismans, H.; Theron, J. Silencing of African horse sickness virus VP7 protein expression in cultured cells by RNA interference. Virus Genes 2007, 35, 777–783. [Google Scholar] [CrossRef]
- de la Poza, F.; Calvo-Pinilla, E.; Lopez-Gil, E.; Marin-Lopez, A.; Mateos, F.; Castillo-Olivares, J.; Lorenzo, G.; Ortego, J. Ns1 is a key protein in the vaccine composition to protect Ifnar(-/-) mice against infection with multiple serotypes of African horse sickness virus. PLoS ONE 2013, 8, e70197. [Google Scholar] [CrossRef]
- Bekker, S.; Huismans, H.; van Staden, V. Factors that affect the intracellular localization and trafficking of African horse sickness virus core protein, VP7. Virology 2014, 456–457, 279–291. [Google Scholar] [CrossRef]
- van de Water, S.G.; van Gennip, R.G.; Potgieter, C.A.; Wright, I.M.; van Rijn, P.A. VP2 Exchange and NS3/NS3a Deletion in African Horse Sickness Virus (AHSV) in Development of Disabled Infectious Single Animal Vaccine Candidates for AHSV. J. Virol. 2015, 89, 8764–8772. [Google Scholar] [CrossRef]
- van Gennip, R.G.P.; van de Water, S.G.P.; Potgieter, C.A.; van Rijn, P.A. Structural Protein VP2 of African Horse Sickness Virus Is Not Essential for Virus Replication In Vitro. J. Virol. 2017, 91, 4. [Google Scholar] [CrossRef]
- Fearon, S.H.; Dennis, S.J.; Hitzeroth, I.I.; Rybicki, E.P.; Meyers, A.E. Humoral and cell-mediated immune responses to plant-produced African horse sickness virus VP7 quasi-crystals. Virus Res. 2021, 294, 198284. [Google Scholar] [CrossRef]
- Wall, G.V.; Wright, I.M.; Barnardo, C.; Erasmus, B.J.; van Staden, V.; Potgieter, A.C. African horse sickness virus NS4 protein is an important virulence factor and interferes with JAK-STAT signaling during viral infection. Virus Res. 2021, 298, 198407. [Google Scholar] [CrossRef]
- De Waal, P.J.; Huismans, H. Characterization of the nucleic acid binding activity of inner core protein VP6 of African horse sickness virus. Arch. Virol. 2005, 150, 2037–2050. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Na, L.; Guo, K.; Wang, J.; Hu, Z.; Du, C.; Wang, X.; Wang, X. Development and evaluation of a RT-RAA-combined CRISPR/Cas12a assay for the detection of African horse sickness virus. J. Integr. Agric. 2024, 23, 4267–4271. [Google Scholar] [CrossRef]
- Kanai, Y.; van Rijn, P.A.; Maris-Veldhuis, M.; Kaname, Y.; Athmaram, T.N.; Roy, P. Immunogenicity of recombinant VP2 pro-teins of all nine serotypes of African horse sickness virus. Vaccine 2014, 32, 4932–4937. [Google Scholar] [CrossRef]
- Martinez-Torrecuadrada, J.L.; Langeveld, J.P.M.; Meloen, R.H.; Casal, J.I. Definition of neutralizing sites on African horse sickness virus serotype 4 VP2 at the level of peptides. J. Gen. Virol. 2001, 82 Pt 10, 2415–2424. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Torrecuadrada, J.L.; Casal, J.I. Identification of a linear neutralization domain in the protein VP2 of African horse sickness virus. Virology 1995, 210, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.; Mertens, P.P.; Casal, I. African horse sickness virus structure. Comp. Immunol. Microbiol. Infect. Dis. 1994, 17, 243–273. [Google Scholar] [CrossRef]
- Girmanesh Tkubet, A.F. Yitayew Demessie, Genet Bezie and Atsede Gebre Yohannes, A Review on African Horse Sickness. World J. Agric. Sci. 2016, 12, 12. [Google Scholar]
- Skowronek, A.J.; LaFranco, L.; Stone-Marschat, M.A.; Burrage, T.G.; Rebar, A.H.; Laegreid, W.W. Clinical pathology and hemostatic abnormalities in experimental African horsesickness. Vet. Pathol. 1995, 32, 112–121. [Google Scholar] [CrossRef]
- Sailleau, C.; Moulay, S.; Cruciere, C.; Laegreid, W.W.; Zientara, S. Detection of African horse sickness virus in the blood of experimentally infected horses: Comparison of virus isolation and a PCR assay. Res. Vet. Sci. 1997, 62, 229–232. [Google Scholar] [CrossRef] [PubMed]
- de la Grandière, M.A.; Dal Pozzo, F.; Tignon, M.; Zonta, W.; Thiry, D.; Mauroy, A.; Mathijs, É.; Caij, A.B.; Saegerman, C.; Thiry, É. Study of the virulence of serotypes 4 and 9 of African horse sickness virus in IFNAR−/−, Balb/C and 129 Sv/Ev mice. Vet. Microbiol. 2014, 174, 322–332. [Google Scholar] [CrossRef]
- Srinivas, J. Plaque Purification of Bluetongue Virus -12 (BTV-12). Int. J. Pure Appl. Biosci. 2018, 6, 128–135. [Google Scholar] [CrossRef]
- Bisht, D.; Saxena, S.; Kharayat, N.S.; Gautam, S. Protocols for Immunofluorescence Techniques. In Protocols for the Diagnosis of Pig Viral Diseases; Deb, R., Yadav, A.K., Rajkhowa, S., Malik, Y.S., Eds.; Springer: New York, NY, USA, 2022; pp. 215–229. [Google Scholar]
- Guthrie, A.J.; Coetzee, P.; Martin, D.P.; Lourens, C.W.; Venter, E.H.; Weyer, C.T.; Joone, C.; le Grange, M.; Harper, C.K.; Howell, P.G.; et al. Complete Genome Sequences of Four African Horse Sickness Virus Strains from a Commercial Tetravalent Live Attenuated Vaccine. Genome Announc. 2015, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.P.; Varsani, A.; Roumagnac, P.; Botha, G.; Maslamoney, S.; Schwab, T.; Kelz, Z.; Kumar, V.; Murrell, B. RDP5: A computer program for analyzing recombination in, and removing signals of recombination from, nucleotide sequence datasets. Virus Evol. 2021, 7, veaa087. [Google Scholar] [CrossRef] [PubMed]
- Potgieter, A.C.; Wright, I.M.; van Dijk, A.A. Consensus Sequence of 27 African Horse Sickness Virus Genomes from Viruses Collected over a 76-Year Period (1933 to 2009). Genome Announc. 2015, 3, 5. [Google Scholar] [CrossRef]
- King, S.; Rajko-Nenow, P.; Ashby, M.; Frost, L.; Carpenter, S.; Batten, C. Outbreak of African horse sickness in Thailand, 2020. Transbound. Emerg. Dis. 2020, 67, 1764–1767. [Google Scholar] [CrossRef]
- Burrage, T.G.; Trevejo, R.; Stone-Marschat, M.; Laegreid, W.W. Neutralizing epitopes of African horsesickness virus serotype 4 are located on VP2. Virology 1993, 196, 799–803. [Google Scholar] [CrossRef]
- Guthrie, A.J.; Quan, M.; Lourens, C.W.; Audonnet, J.C.; Minke, J.M.; Yao, J.; He, L.; Nordgren, R.; Gardner, I.A.; Maclachlan, N.J. Protective immunization of horses with a recombinant canarypox virus vectored vaccine co-expressing genes encoding the outer capsid proteins of African horse sickness virus. Vaccine 2009, 27, 4434–4438. [Google Scholar] [CrossRef]
- Gao, S.; Zeng, Z.; Wang, H.; Chen, F.; Huang, L.; Wang, X. Predicting the possibility of African horse sickness (AHS) introduction into China using spatial risk analysis and habitat connectivity of Culicoides. Sci. Rep. 2022, 12, 3910. [Google Scholar] [CrossRef]
- Kutumbetov, L.; Ragatova, A.; Azanbekova, M.; Myrzakhmetova, B.; Aldayarov, N.; Zhugunissov, K.; Abduraimov, Y.; Nissanova, R.; Sarzhigitova, A.; Kemalova, N.; et al. Investigation of the Pathogenesis of Lumpy Skin Disease Virus in Indigenous Cattle in Kazakhstan. Pathogens 2025, 14, 577. [Google Scholar] [CrossRef] [PubMed]


| Genome Segment | mRNA Length | CDS Length | GenBank Accession No. | Percent Identity with AHSV-1 Isolate 1180 f (%) | Percent Identity with Thailand 2020 Strain (TAI2020/01) g (%) |
|---|---|---|---|---|---|
| Segments encoding VP1 | 3965 | 3918 (14–3931) | PX069092 | 99.47 | 88.9 |
| Segments encoding VP2 | 3218 | 3171 (13–3183) | PX069094 | 98.97 | 95.28 |
| Segments encoding VP3 | 2792 | 2718 (27–2744) | PX069096 | 99.32 | 95.27 |
| Segments encoding VP4 | 1978 | 1929 (12–1940) | PX069098 | 91.00 | 89.07 |
| Segments encoding VP5 | 1564 | 1518 (20–1537) | PX0690100 | 84.65 | 95.46 |
| Segments encoding VP6 | 1169 | 1110 (18–1127) a 240 (196–435) b 288 (148–435) c | PX0690102 | 97.95 | 95.38 |
| Segments encoding VP7 | 1167 | 1050 (18–1067) | PX0690104 | 99.57 | 96.39 |
| Segments encoding NS1 | 1748 | 1647 (36–1682) | PX0690106 | 99.37 | 96.85 |
| Segments encoding NS2 | 1166 | 1098 (23–1120) | PX0690108 | 99.31 | 95.18 |
| Segments encoding NS3 | 763 | 657 (19–675) d 627 (49–675) e | PX0690110 | 97.27 | 95.54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Wang, X.-F.; Guo, S.-F.; Wang, L.; Fu, B.-F.; Wang, J.-W.; Song, Y.-F.; Yang, X.-Y.; Hao, S.-Y.; Zhang, Q.-Y.; et al. Identification and Genetic Characterization of a Strain of African Horse Sickness Virus Serotype 1 and Its Safety Evaluation in a Mouse Model. Microorganisms 2025, 13, 2314. https://doi.org/10.3390/microorganisms13102314
Zhang M, Wang X-F, Guo S-F, Wang L, Fu B-F, Wang J-W, Song Y-F, Yang X-Y, Hao S-Y, Zhang Q-Y, et al. Identification and Genetic Characterization of a Strain of African Horse Sickness Virus Serotype 1 and Its Safety Evaluation in a Mouse Model. Microorganisms. 2025; 13(10):2314. https://doi.org/10.3390/microorganisms13102314
Chicago/Turabian StyleZhang, Min, Xue-Feng Wang, Si-Fan Guo, Lei Wang, Bo-Fan Fu, Jing-Wen Wang, Ya-Fen Song, Xiao-Yue Yang, Si-Yuan Hao, Qian-Yi Zhang, and et al. 2025. "Identification and Genetic Characterization of a Strain of African Horse Sickness Virus Serotype 1 and Its Safety Evaluation in a Mouse Model" Microorganisms 13, no. 10: 2314. https://doi.org/10.3390/microorganisms13102314
APA StyleZhang, M., Wang, X.-F., Guo, S.-F., Wang, L., Fu, B.-F., Wang, J.-W., Song, Y.-F., Yang, X.-Y., Hao, S.-Y., Zhang, Q.-Y., Zhang, B., & Yang, C.-H. (2025). Identification and Genetic Characterization of a Strain of African Horse Sickness Virus Serotype 1 and Its Safety Evaluation in a Mouse Model. Microorganisms, 13(10), 2314. https://doi.org/10.3390/microorganisms13102314






