Epidemiological Evidence for Upper Respiratory Infections as a Potential Risk Factor for Meniere’s Disease: A Korean National Health Sample Cohort Study
Abstract
1. Introduction
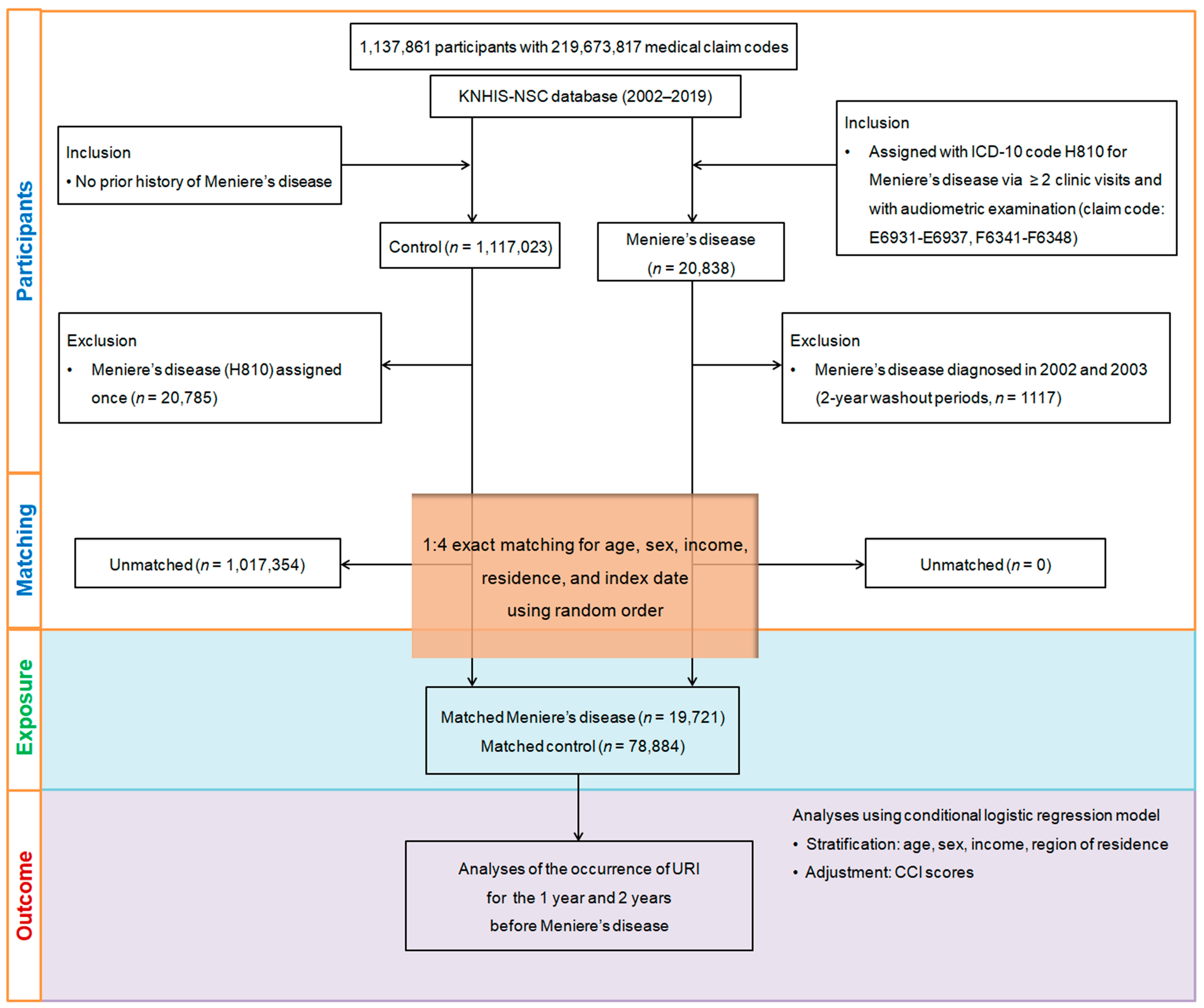
2. Materials and Methods
2.1. Data Source and Participant Selection
2.2. Exposure (Upper Respiratory Infection) and Outcome (Meniere’s Disease)
2.3. Covariates
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopez-Escamez, J.A.; Perez-Carpena, P. Update on the pathophysiology, diagnosis and management of Meniere’s disease. Curr. Opin. Otolaryngol. Head Neck Surg. 2024, 35, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Tyrrell, J.S.; Whinney, D.J.D.; Ukoumunne, O.C.; Fleming, L.E.; Osborne, N.J. Prevalence, Associated Factors, and Comorbid Conditions for Ménière’s Disease. Ear Hear. 2014, 35, e162–e169. [Google Scholar] [CrossRef] [PubMed]
- Pyykko, I.; Nakashima, T.; Yoshida, T.; Zou, J.; Naganawa, S. Meniere’s disease: A reappraisal supported by a variable latency of symptoms and the MRI visualisation of endolymphatic hydrops. BMJ Open 2013, 3, e001555. [Google Scholar] [CrossRef]
- Wladislavosky-Waserman, P.; Facer, G.W.; Mokri, B.; Kurland, L.T. Meniere’s disease: A 30-year epidemiologic and clinical study in Rochester, Mn, 1951–1980. Laryngoscope 1984, 94, 1098–1102. [Google Scholar] [CrossRef]
- da Costa, S.S.; de Sousa, L.C.; Piza, M.R. Meniere’s disease: Overview, epidemiology, and natural history. Otolaryngol. Clin. N. Am. 2002, 35, 455–495. [Google Scholar] [CrossRef] [PubMed]
- Espinosa-Sanchez, J.M.; Lopez-Escamez, J.A. Chapter 19—Menière’s disease. In Handbook of Clinical Neurology; Furman, J.M., Lempert, T., Eds.; Elsevier: Amsterdam, The Netherlands, 2016; Volume 137, pp. 257–277. [Google Scholar]
- Shojaku, H.; Watanabe, Y.; Yagi, T.; Takahashi, M.; Takeda, T.; Ikezono, T.; Ito, J.; Kubo, T.; Suzuki, M.; Takumida, M.; et al. Changes in the characteristics of definite Meniere’s disease over time in Japan: A long-term survey by the Peripheral Vestibular Disorder Research Committee of Japan, formerly the Meniere’s Disease Research Committee of Japan. Acta Otolaryngol. 2009, 129, 155–160. [Google Scholar] [CrossRef]
- Kim, M.H.; Cheon, C. Epidemiology and Seasonal Variation of Meniere’s Disease: Data from a Population-Based Study. Audiol. Neurootol. 2020, 25, 224–230. [Google Scholar] [CrossRef]
- Frejo, L.; Lopez-Escamez, J.A. Cytokines and Inflammation in Meniere Disease. Clin. Exp. Otorhinolaryngol. 2022, 15, 49–59. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lee, C.H.; Yoo, D.M.; Kwon, M.J.; Kim, J.H.; Kim, J.H.; Park, B.; Lee, H.J.; Choi, H.G. Association Between Meniere Disease and Migraine. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 457–464. [Google Scholar] [CrossRef]
- Uranaka, T.; Kashio, A.; Ueha, R.; Sato, T.; Bing, H.; Ying, G.; Kinoshita, M.; Kondo, K.; Yamasoba, T. Expression of ACE2, TMPRSS2, and Furin in Mouse Ear Tissue, and the Implications for SARS-CoV-2 Infection. Laryngoscope 2021, 131, E2013–E2017. [Google Scholar] [CrossRef]
- Saarentaus, E.C.; Karjalainen, J.; Ramo, J.T.; Kiiskinen, T.; Havulinna, A.S.; Mehtonen, J.; Hautakangas, H.; Ruotsalainen, S.; Tamlander, M.; Mars, N.; et al. Inflammatory and infectious upper respiratory diseases associate with 41 genomic loci and type 2 inflammation. Nat. Commun. 2023, 14, 83. [Google Scholar] [CrossRef]
- Heikkinen, T.; Ruuskanen, O. Upper Respiratory Tract Infection. In Encyclopedia of Respiratory Medicine; Academic Press: Cambridge, MA, USA, 2006; pp. 385–388. [Google Scholar] [CrossRef]
- Leong, S.; Teh, B.M.; Kim, A.H. Characterization of otologic symptoms appearing after COVID-19 vaccination. Am. J. Otolaryngol. 2023, 44, 103725. [Google Scholar] [CrossRef] [PubMed]
- Lovato, A.; Frosolini, A.; Marioni, G.; de Filippis, C. Higher incidence of Ménière’s disease during COVID-19 pandemic: A preliminary report. Acta Oto-Laryngol. 2021, 141, 921–924. [Google Scholar] [CrossRef]
- Yazawa, Y.; Suzuki, M.; Hanamitsu, M.; Kimura, H.; Tooyama, I. Detection of viral DNA in the endolymphatic sac in Meniere’s disease by in situ hybridization. ORL J. Otorhinolaryngol. Relat. Spec. 2003, 65, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Dean, N.J.; Pastras, C.; Brown, D.; Camp, A. Are viral-infections associated with Meniere’s Disease? A systematic review and meta-analysis of molecular-markers of viral-infection in case-controlled observational studies of MD. PLoS ONE 2019, 14, e0225650. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.-H.; Shin, S.A.; Kim, K. Cohort profile: The national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef] [PubMed]
- Kyoung, D.-S.; Kim, H.-S. Understanding and utilizing claim data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) database for research. J. Lipid Atheroscler. 2022, 11, 103. [Google Scholar]
- Kang, H.S.; Kim, J.H.; Kim, J.H.; Bang, W.J.; Choi, H.G.; Kim, N.Y.; Park, H.Y.; Kwon, M.J. Unlocking the Protective Potential of Upper Respiratory Infection Treatment Histories against Alzheimer’s Disease: A Korean Adult Population Study. J. Clin. Med. 2024, 13, 260. [Google Scholar] [CrossRef]
- Kwon, M.J.; Byun, S.H.; Kim, J.H.; Kim, J.H.; Kim, S.H.; Kim, N.Y.; Park, H.R.; Choi, H.G. Longitudinal follow-up study of the association between statin use and chronic periodontitis using national health screening cohort of Korean population. Sci. Rep. 2022, 12, 5504. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef]
- Lin, C.Y.; Kuo, P.H.; Wu, S.Y. Association of Acute Upper Respiratory Tract Infections with Sudden Sensorineural Hearing Loss: A Case-Crossover, Nationwide, Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 10745. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Ota, I.; Yamanaka, T.; Kitahara, T. The Impact of the COVID-19 Pandemic on Follow-Ups for Vertigo/Dizziness Outpatients. Ear Nose Throat J. 2021, 100, 163S–168S. [Google Scholar] [CrossRef]
- Branche, A.R.; Falsey, A.R. Parainfluenza Virus Infection. Semin. Respir. Crit. Care Med. 2016, 37, 538–554. [Google Scholar] [CrossRef]
- Talbot, H.K.; Falsey, A.R. The diagnosis of viral respiratory disease in older adults. Clin. Infect. Dis. 2010, 50, 747–751. [Google Scholar] [CrossRef]
- Wen, Y.C.; Hsiao, F.Y.; Chan, K.A.; Lin, Z.F.; Shen, L.J.; Fang, C.C. Acute Respiratory Infection and Use of Nonsteroidal Anti-Inflammatory Drugs on Risk of Acute Myocardial Infarction: A Nationwide Case-Crossover Study. J. Infect. Dis. 2017, 215, 503–509. [Google Scholar] [CrossRef]
- Shulman, A.; Goldstein, B. Brain and inner-ear fluid homeostasis, cochleovestibular-type tinnitus, and secondary endolymphatic hydrops. Int. Tinnitus J. 2006, 12, 75–81. [Google Scholar]
- Delgado, L.P.; Rodrigo, J.F.; Pena, P.A. Intratympanic gentamicin in Meniere’s disease: Our experience. J. Laryngol. Otol. 2011, 125, 363–369. [Google Scholar] [CrossRef]
- Lee, J.M.; Kim, M.J.; Jung, J.; Kim, H.J.; Seo, Y.J.; Kim, S.H. Genetic aspects and clinical characteristics of familial Meniere’s disease in a South Korean population. Laryngoscope 2015, 125, 2175–2180. [Google Scholar] [CrossRef]
- Postema, R.J.; Kingma, C.M.; Wit, H.P.; Albers, F.W.; Van Der Laan, B.F. Intratympanic gentamicin therapy for control of vertigo in unilateral Menire’s disease: A prospective, double-blind, randomized, placebo-controlled trial. Acta Otolaryngol. 2008, 128, 876–880. [Google Scholar] [CrossRef]
- Frejo, L.; Requena, T.; Okawa, S.; Gallego-Martinez, A.; Martinez-Bueno, M.; Aran, I.; Batuecas-Caletrio, A.; Benitez-Rosario, J.; Espinosa-Sanchez, J.M.; Fraile-Rodrigo, J.J.; et al. Regulation of Fn14 Receptor and NF-kappaB Underlies Inflammation in Meniere’s Disease. Front. Immunol. 2017, 8, 1739. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kwon, S.; Choi, E.-K.; Choi, Y.-j.; Lee, E.; Choe, W.; Lee, S.-R.; Cha, M.-J.; Lim, W.-H.; Oh, S. Validation of diagnostic codes of major clinical outcomes in a National Health Insurance database. Int. J. Arrhythmia 2019, 20, 5. [Google Scholar] [CrossRef]
- Simo, H.; Yang, S.; Qu, W.; Preis, M.; Nazzal, M.; Baugh, R. Meniere’s disease: Importance of socioeconomic and environmental factors. Am. J. Otolaryngol. 2015, 36, 393–398. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Meniere’s Disease | Control | Standardized Difference |
|---|---|---|---|
| Age (y), n (%) | 0.00 | ||
| 0–4 | 3 (0.02) | 12 (0.02) | |
| 5–9 | 31 (0.16) | 124 (0.16) | |
| 10–14 | 135 (0.68) | 540 (0.68) | |
| 15–19 | 387 (1.96) | 1548 (1.96) | |
| 20–24 | 471 (2.39) | 1884 (2.39) | |
| 25–29 | 596 (3.02) | 2384 (3.02) | |
| 30–34 | 838 (4.25) | 3352 (4.25) | |
| 35–39 | 1178 (5.97) | 4712 (5.97) | |
| 40–44 | 1415 (7.18) | 5660 (7.18) | |
| 45–49 | 1718 (8.71) | 6872 (8.71) | |
| 50–54 | 1947 (9.87) | 7788 (9.87) | |
| 55–59 | 2113 (10.71) | 8452 (10.71) | |
| 60–64 | 1979 (10.03) | 7916 (10.03) | |
| 65–69 | 2046 (10.37) | 8184 (10.37) | |
| 70–74 | 1965 (9.96) | 7860 (9.96) | |
| 75–79 | 1572 (7.97) | 6288 (7.97) | |
| 80–84 | 901 (4.57) | 3604 (4.57) | |
| 85+ | 426 (2.16) | 1704 (2.16) | |
| Sex, n (%) | 0.00 | ||
| Male | 5998 (30.41) | 23,992 (30.41) | |
| Female | 13,723 (69.59) | 54,892 (69.59) | |
| Income, n (%) | 0.00 | ||
| 1 (lowest) | 4062 (20.60) | 16,248 (20.60) | |
| 2 | 2674 (13.56) | 10,696 (13.56) | |
| 3 | 3109 (15.76) | 12,436 (15.76) | |
| 4 | 4257 (21.59) | 17,028 (21.59) | |
| 5 (highest) | 5619 (28.49) | 22,476 (28.49) | |
| Region of residence, n (%) | 0.00 | ||
| Urban | 8414 (42.67) | 33,656 (42.67) | |
| Rural | 11,307 (57.33) | 45,228 (57.33) | |
| CCI score (mean, SD) | 0.76 (1.40) | 0.71 (1.45) | 0.03 |
| The number of upper respiratory infections (mean, SD) | |||
| within 1 year | 2.09 (3.62) | 1.34 (3.02) | 0.23 |
| within 2 year | 4.10 (6.35) | 2.69 (5.13) | 0.24 |
| Characteristics | Odd Ratios for Meniere’s Disease (95% Confidence Interval) | ||||
|---|---|---|---|---|---|
| Crude † | p | Adjusted ‡ | p | ||
| From the index date to before the 1-year period | |||||
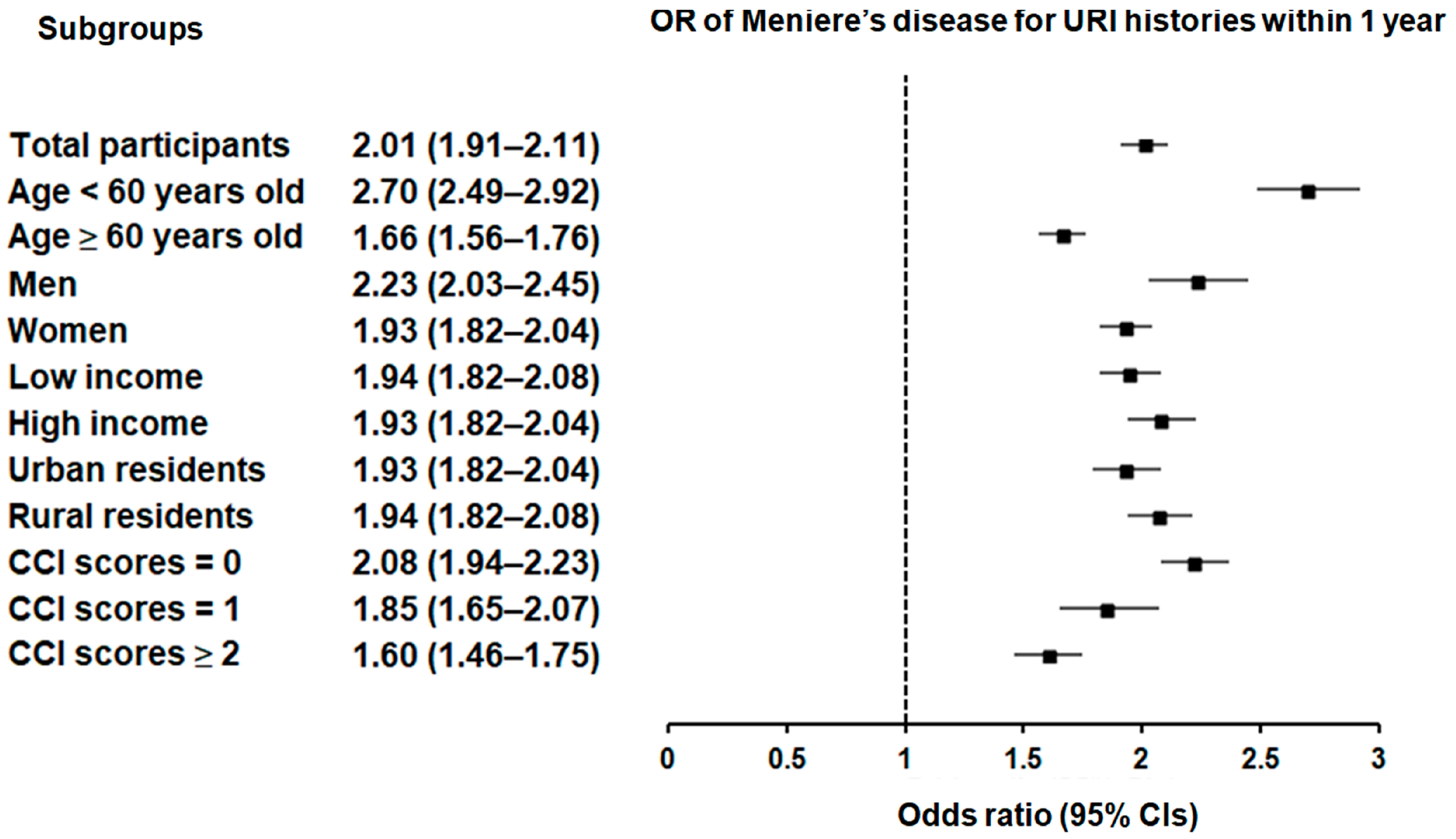
| Total participants (n = 98,605) | 2.01 (1.92–2.11) | <0.001 * | 2.01 (1.91–2.11) | <0.001 * | |
| Age < 60 years old (n = 54,160) | 2.72 (2.51–2.94) | <0.001 * | 2.70 (2.49–2.92) | <0.001 * | |
| Age ≥ 60 years old (n = 44,445) | 1.66 (1.56–1.76) | <0.001 * | 1.66 (1.56–1.76) | <0.001 * | |
| Male (n = 29,990) | 2.24 (2.04–2.45) | <0.001 * | 2.23 (2.03–2.45) | <0.001 * | |
| Female (n = 68,615) | 1.93 (1.82–2.05) | <0.001 * | 1.93 (1.82–2.04) | <0.001 * | |
| Low income group (n = 49,225) | 1.95 (1.82–2.09) | <0.001 * | 1.94 (1.82–2.08) | <0.001 * | |
| High income group (n = 49,380) | 2.08 (1.94–2.23) | <0.001 * | 2.08 (1.94–2.23) | <0.001 * | |
| Urban residents (n = 42,070) | 1.93 (1.79–2.08) | <0.001 * | 1.93 (1.79–2.08) | <0.001 * | |
| Rural residents (n = 56,535) | 2.08 (1.95–2.21) | <0.001 * | 2.07 (1.94–2.21) | <0.001 * | |
| CCI scores = 0 (n = 67,493) | 2.21 (2.07–2.36) | <0.001 * | 2.22 (2.08–2.37) | <0.001 * | |
| CCI scores = 1 (n = 14,086) | 1.85 (1.65–2.07) | <0.001 * | 1.85 (1.65–2.07) | <0.001 * | |
| CCI scores ≥ 2 (n = 17,026) | 1.59 (1.45–1.74) | <0.001 * | 1.60 (1.46–1.75) | <0.001 * | |
| From the index date to before the 2-year period | |||||
| Total participants (n = 98,605) | 1.54 (1.50–1.59) | <0.001 * | 1.54 (1.50–1.59) | <0.001 * | |
| Age < 60 years old (n = 54,160) | 1.87 (1.79–1.96) | <0.001 * | 1.86 (1.78–1.95) | <0.001 * | |
| Age ≥ 60 years old (n = 44,445) | 1.37 (1.32–1.42) | <0.001 * | 1.37 (1.32–1.42) | <0.001 * | |
| Male (n = 29,990) | 1.62 (1.54–1.71) | <0.001 * | 1.62 (1.53–1.71) | <0.001 * | |
| Female (n = 68,615) | 1.51 (1.46–1.57) | <0.001 * | 1.51 (1.46–1.56) | <0.001 * | |
| Low income group (n = 49,225) | 1.54 (1.48–1.60) | <0.001 * | 1.54 (1.48–1.60) | <0.001 * | |
| High income group (n = 49,380) | 1.55 (1.49–1.61) | <0.001 * | 1.55 (1.49–1.61) | <0.001 * | |
| Urban residents (n = 42,070) | 1.51 (1.45–1.58) | <0.001 * | 1.51 (1.45–1.58) | <0.001 * | |
| Rural residents (n = 56,535) | 1.57 (1.51–1.63) | <0.001 * | 1.57 (1.51–1.63) | <0.001 * | |
| CCI scores = 0 (n = 67,493) | 1.64 (1.58–1.70) | <0.001 * | 1.65 (1.58–1.71) | <0.001 * | |
| CCI scores = 1 (n = 14,086) | 1.46 (1.37–1.55) | <0.001 * | 1.46 (1.37–1.55) | <0.001 * | |
| CCI scores ≥ 2 (n = 17,026) | 1.32 (1.25–1.39) | <0.001 * | 1.32 (1.25–1.40) | <0.001 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, M.J.; Kang, H.S.; Kim, J.-H.; Kim, J.H.; Bang, W.J.; Yoo, D.M.; Lee, N.-E.; Han, K.M.; Kim, N.Y.; Choi, H.G.; et al. Epidemiological Evidence for Upper Respiratory Infections as a Potential Risk Factor for Meniere’s Disease: A Korean National Health Sample Cohort Study. Microorganisms 2024, 12, 2047. https://doi.org/10.3390/microorganisms12102047
Kwon MJ, Kang HS, Kim J-H, Kim JH, Bang WJ, Yoo DM, Lee N-E, Han KM, Kim NY, Choi HG, et al. Epidemiological Evidence for Upper Respiratory Infections as a Potential Risk Factor for Meniere’s Disease: A Korean National Health Sample Cohort Study. Microorganisms. 2024; 12(10):2047. https://doi.org/10.3390/microorganisms12102047
Chicago/Turabian StyleKwon, Mi Jung, Ho Suk Kang, Joo-Hee Kim, Ji Hee Kim, Woo Jin Bang, Dae Myoung Yoo, Na-Eun Lee, Kyeong Min Han, Nan Young Kim, Hyo Geun Choi, and et al. 2024. "Epidemiological Evidence for Upper Respiratory Infections as a Potential Risk Factor for Meniere’s Disease: A Korean National Health Sample Cohort Study" Microorganisms 12, no. 10: 2047. https://doi.org/10.3390/microorganisms12102047
APA StyleKwon, M. J., Kang, H. S., Kim, J.-H., Kim, J. H., Bang, W. J., Yoo, D. M., Lee, N.-E., Han, K. M., Kim, N. Y., Choi, H. G., Kim, M.-J., & Kim, E. S. (2024). Epidemiological Evidence for Upper Respiratory Infections as a Potential Risk Factor for Meniere’s Disease: A Korean National Health Sample Cohort Study. Microorganisms, 12(10), 2047. https://doi.org/10.3390/microorganisms12102047






