Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022
Abstract
1. Introduction
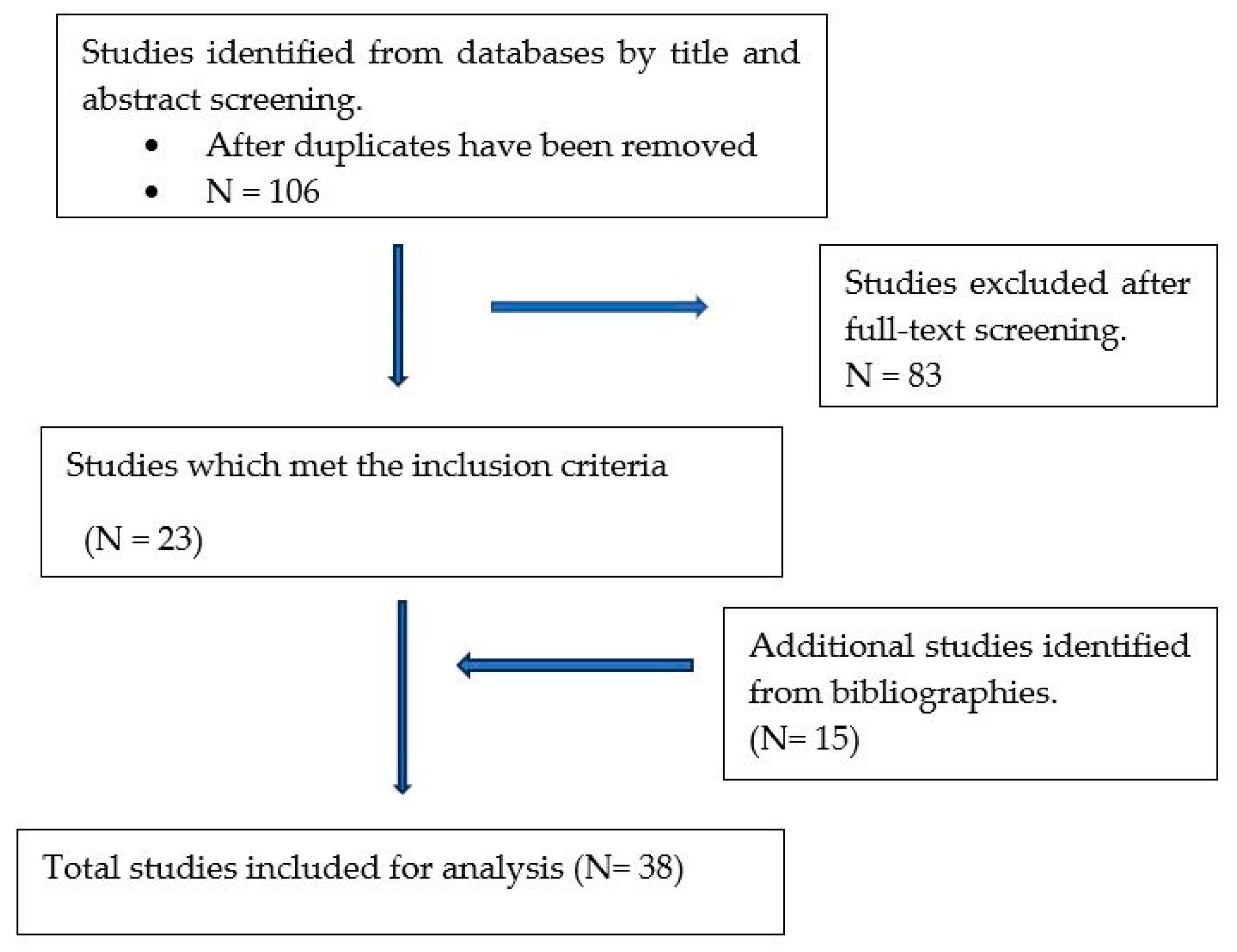
2. Methodology
2.1. Search Strategy and Selection Criteria
2.2. Data Categorisation
2.3. Data Analysis
3. Results
3.1. Causative Organism and Study Setting
| Country and Continent | Setting | Design | Age Group | Sample Size | Detection Methods (1E. coli and/or Pathotype, 2ESBL Genes) | Causative Organism | % blaCTX-M Reported | CTX-M Genes Detected | Other ESBLs Genes Detected | Study Period | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil, South America | ND | Case–control | 0–5 | 162 | 1PCR, 2PCR | EPEC, EAEC | 15 | CTX-M | TEM | [34] | |
| Egypt, North Africa | Hospital | Prospective | 0–5 | 113 | 1PCR, 2Sequencing | EAEC | 4.0 | CTX-M | TEM | 2016 | [35] |
| Egypt, North Africa | Hospital | Prospective | 0–5 | 320 | 1m-PCR, 1phylogrouping, 2PCR | EAEC, tEPEC, aEPEC | 37.5 | CTX-M-15 | TEM | 2018–2019 | [24] |
| Burkina Faso, West Africa | Health centre | Retrospective | 0–5 | ND | 1m-PCR, 2m-PCR | EPEC, EAEC | 7.1 | CTX-M | OXA | 2018–2019 | [23] |
| Libya, North Africa | Hospital | Prospective | 0–5 | 290 | 1m-PCR, 2m-PCR | EAEC, EIEC, EHEC | 60 | CTX-M-15 | CTX-8, CTX-M9 | 2012 | [36] |
| England, Europe | Primary healthcare | Retrospective | 0–16 | 660 | 1PCR, 1,2Sequencing | EAEC, ETEC, EPEC, EIEC | ND | CTX-M-15 | TEM1, CTXM1, CTX-M14, CTX-M27, SHV12 | 2015–2017 | [37] |
| India, Asia | Hospital | Prospective | 0–5 | 120 | 1m-PCR, 2Rt-PCR, 2Sequencing | EPEC, EAEC, ETEC, EHEC | 40 | CTX-M | TEM, SHV, OXA, NDM-1, IMP, VIM, ACT, DHA and CMY | ND | [38] |
| Korea, Asia | Hospital | Prospective longitudinal | Children and infants | ND | 1m-PCR, 2m-PCR | EPEC, ETEC, EHEC | 16 | CTX-M-15 | CTX-M14, CTX-M27, CTX-M55, CTX-M3, TEM1, PABLs, CMY2, DHA1 | 2007–2016 | [39] |
| Iran, Asia | Hospital | Descriptive cross-sectional study | 0–5 | 321 | 1m-PCR, 1serotyping, 2PCR | EPEC | 83.3 | CTX-M | TEM | 2016–2017 | [40] |
| Iran, Asia | Hospital | Prospective | 0–92 | 340 | 1PCR, 2PCR | STEC | 69 | CTX-M-9 | TEM | 2014 | [41] |
| Qatar, Asia | Hospital | Prospective | 0–10 | 175 | 1PCR, 2PCR | EPEC, EAEC | 88.2 | CTX-M-15 | CTX-M-3 | 2017–2018 | [42] |
| Iran, Asia | ND | Prospective | 0–10 | 1355 | 1PCR, 2PCR | EPEC | 10.9 | CTX-M | TEM, SHV, OXA | ND | [20] |
| China, Asia | Hospital | Prospective | 0–5 | 684 | 1PCR, 1Serotyping, 2PCR, 2Sequencing | EPEC, EAEC, ETEC, EIEC, STEC | 20 | CTX-M-15 | NDM1, KPC2, TEM1, CTX-M-55, CTX-M14, CTXM-65, CTX-M-137 | 2015–2016 | [3] |
| Iran, Asia | Hospital | Prospective | 0–15 | 395 | 1PCR, 1phylogrouping, 2PCR | ETEC, EPEC | ND | CTX-M | TEM | 2014–2015 | [43] |
| India, Asia | Paediatric institute | Prospective and retrospective | 0–10 | 900 | 1PCR, 1Serotyping, 2PCR | tEPEC, aEPEC | 11.5 | CTX-M-15 | (NDM-1), (VIM) | 2012–2013 | [30] |
| Indonesia, Asia | Hospital | Prospective | 0–3 | 133 | 1PCR, 2PCR, 2Sequencing | EAEC, EPEC | 84 | CTX-M-15 | TEM-1, SHV | 2012 | [44] |
| India, Asia | Hospital | Cross-sectional study | 0–5 | 120 | 1PCR,2PCR | tEPEC, aEPEC, ETEC, EIEC | ND | CTX-M | SHV, TEM | 2015–2016 | [31] |
| Pakistan, Asia | ND | Cross-sectional | 0–5 | 100 | 1PCR, 1Sequencing, 2PCR | EPEC | 93 | CTX-M | TEM | 2016–2017 | [45] |
| Japan, Asia | Clinics | Retrospective | ND | 167 | 1PCR, 1Phylogrouping, 2PCR, 2Sequencing | EAEC | 79 | CTX-M-15 | CTX-M14, CTX-M55 | 1992–2010 | [46] |
| India, Asia | Hospital | Prospective longitudinal | 0–14 | 8891 | 1m-PCR, 2PCR | ETEC, EAEC, EPEC | 30.2 | CTX-M3 | TEM, SHV, OXA1 | 2012–2019 | [47] |
| Iran, Asia | Hospital | Prospective | 0–10 | 303 | 1m-PCR, 2PCR | EAEC, EPEC, ETEC, EIEC, STEC | 25 | CTX-M-15 | TEM | 2018 | [48] |
| China, Asia | Hospital | Prospective | 0–5 | 1643 | 1PCR, 1Serotyping, 2PCR, 2Sequencing | EPEC | 60.3 | CTX-M-1 | CTX-M9, TEM, SHV | 2009 | [49] |
| Iran, Asia | Hospital | Descriptive cross-sectional study | 0–81 | 581 | 1PCR, 2PCR | EIEC | 77.8 | CTX-M-15 | CTX-M1, TEM1 | 2016–2017 | [50] |
| China, Asia | ND | Prospective | ND | 912 | 1PCR, 2PCR, 2Sequencing | ETEC, EPEC, EIEC, EAEC | ND | CTX-M-14 | CTX-M79, CTX-M28, TEM | 2013–2014 | [51] |
| Iran, Asia | Hospital | Prospective longitudinal | 0–10 | 342 | 1PCR, 1Serotyping, 2PCR | EPEC | 19 | CTX-M-15 | TEM, SHV | 2011–2013 | [4] |
| Iraq., Asia | ND | Prospective | 0–2 | 656 | 1Serotyping, 2PCR | EPEC | 77.3 | CTX-M | TEM, SHV, OXA, AmpC | 2009 | [52] |
| Iran, Asia | Referral centre | Prospective | 0–14 | 230 | 1PCR, 1Serotyping, 2PCR | EAEC, EPEC, EIEC, ETEC | 94.4 | CTX-M-15 | TEM, AmpC | 2015–2016 | [53] |
| Iran, Asia | Hospital | Prospective | 0–10 | 251 | 1PCR, 1Serotyping, 2PCR | EPEC | 70.6 | CTX-M-15 | TEM | 2015–2016 | [54] |
| Country and Continent | Setting | Design | Age Group | Sample Size | Detection Methods (1E. coli and/or Pathotype, 2ESBL Genes) | Causative Organism | % blaCTX-M Reported | CTX-M Genes Detected | Other ESBLs Genes Detected | Study Period | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| South Africa, Sub-Saharan Africa | Community | Prospective longitudinal | 0–1 | 65 | 1Cuture, 2PCR, 2Sequencing | *E. coli | 4.9 | CTX-M-14 | TEM-1, CTX-M-9 | ND | [12] |
| Nigeria, West Africa | Hospital | Prospective | 0–5 | 296 | 1Culture, 2PCR, 2Sequencing | *E. coli | 73.3 | CTX-M | TEM, SHV | ND | [55] |
| Libya, North Africa | Clinics | Prospective longitudinal | 3–12 | 243 | 1Culture, 1Phylogrouping, 2PCR, 2Sequencing | DEC: phylogroup B1, D, A and B2 | 13.4 | CTX-M-15 | CTX-M1, CTX-M3, TEM, SHV, OXA | 2001 and 2007 | [28] |
| France, Europe | Hospital | Prospective | 0–16 | 1118 | 1Culture, 2PCR, 2Sequencing | *E. coli | 4.3 | CTX-M-15 | TEM-24, TEM-19, SHV-5 | 2010–2011 | [56] |
| Italy, Europe | Community | Prospective | 0–6 | 482 | 1Culture, 1Phylogrouping, 2PCR, 2Sequencing | DEC: Phylogroup A, B1 and D | 43 | CTX-M | CTX-M1, CTX-M9, CTX-M8, CTX-M2 | 2011 | [33] |
| Poland, Europe | Hospital | Prospective | 0–5 | ND | 1Phylogrouping, 2PCR | DEC: Phylogroup A, B1, B2 and D | 76.6 | CTX-M | TEM, SHV | 2008–2009 | [7] |
| Iran, Asia | Hospital | Prospective | 0–80 | 216 | 1m-PCR, 1phylogrouping, 2PCR | DEC: phylogroup A, D, B1 and B2 | 25.9 | CTX-M-15 | OXA1 | 2013 | [32] |
| Iraq, Asia | Hospital | Prospective cross-sectional | 0–8 | 116 | 1PCR, 2PCR | DEC | 71.4 | CTX-M | TEM-1 | 2019 | [2] |
| Jordan, Asia | Hospital | Prospective | 0–1 | 288 | 1Culture and Biochemical test, 2PCR, 2Phylogrouping | *E. coli | 73.2 | CTX-M-15 | ND | 2012 | [57] |
| Malaysia, Asia | Hospital | Prospective | 0–5 | 110 | 1Culture, 2PCR | *E. coli | 9.1 | CTX-M-15 | TEM-1, CMY-2 | 2009–2010 | [58] |
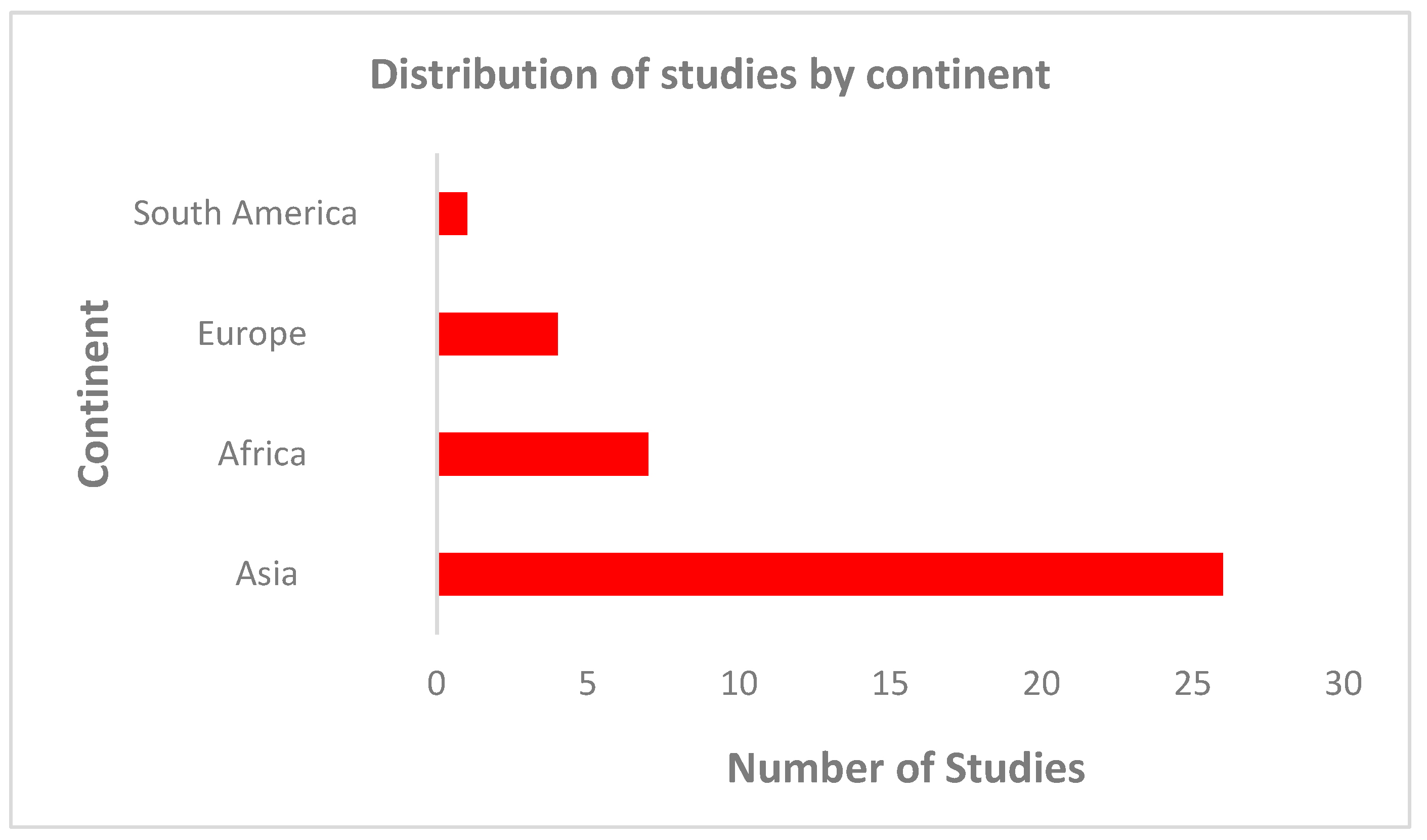
3.2. Distribution of Studies on CTX-M-Producing E. coli by Region
3.3. Age Distribution
3.4. Distribution of Studies by E. coli Pathotype
3.5. Prevalence of CTX-M and Other ESBLs
4. Discussion
5. Limitation
6. Closing Remarks
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Troeger, C.; Blacker, B.F.; Khalil, I.A.; Rao, P.C.; Cao, S.; Zimsen, S.R.; Albertson, S.B.; Stanaway, J.D.; Deshpande, A.; Abebe, Z.; et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: Asystematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef]
- Hamad, W.F. Genotypic and phenotypic study of E. coli isolated from children suffering from severe diarrhea with some antibiotic resistant gene. World J. Adv. Res. Rev. 2022, 15, 683–693. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhu, X.; Hou, H.; Lu, Y.; Yu, J.; Mao, L.; Mao, L.; Sun, Z. Characteristics of diarrheagenic Escherichia coli among children under 5 years of age with acute diarrhea: A hospital-based study. BMC Infect. Dis. 2018, 18, 63. [Google Scholar] [CrossRef] [PubMed]
- Memariani, M.; Peerayeh, S.N.; Salehi, T.Z.; Mostafavi, S.K.S. Occurrence of SHV, TEM and CTX-M β-Lactamase Genes among Enteropathogenic Escherichia coli Strains Isolated from Children with Diarrhea. Jundishapur J. Microbiol. 2015, 8, e15620. [Google Scholar] [CrossRef]
- Salleh, M.Z.; Zuraina, N.M.N.N.; Hajissa, K.; Ilias, M.I.; Deris, Z.Z. Prevalence of Multidrug-Resistant Diarrheagenic Escherichia coli in Asia: A Systematic Review and Meta-Analysis. Antibiotics 2022, 11, 1333. [Google Scholar] [CrossRef]
- Mosquito, S.; Pons, M.J.; Riveros, M.; Ruiz, J.; Ochoa, T.J. Diarrheagenic Escherichia coli Phylogroups Are Associated with Antibiotic Resistance and Duration of Diarrheal Episode. Sci. World J. 2015, 2015, 610403. [Google Scholar] [CrossRef] [PubMed]
- Franiczek, R.; Sobieszczańska, B.; Turniak, M.; Kasprzykowska, U.; Krzyżanowska, B.; Jermakow, K.; Mokracka-Latajka, G. ESBL-Producing Escherichia coli Isolated from Children with Acute Diarrhea—Antimicrobial Susceptibility, Adherence Patterns and Phylogenetic Background. Adv. Clin. Exp. Med. 2012, 21, 187–192. [Google Scholar] [PubMed]
- Alfinete, N.W.; Bolukaoto, J.Y.; Heine, L.; Potgieter, N.; Barnard, T.G. Virulence and phylogenetic analysis of enteric pathogenic Escherichia coli isolated from children with diarrhoea in South Africa. Int. J. Infect. Dis. 2022, 114, 226–232. [Google Scholar] [CrossRef]
- World Health Organization. WHO Report on Surveillance of Antibiotic Consumption: 2016–2018 Early Implementation; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Sidjabat, H.E.; Paterson, D.L. Multidrug-resistant Escherichia coli in Asia: Epidemiology and management. Expert Rev. Anti-Infect. Ther. 2015, 13, 575–591. [Google Scholar] [CrossRef]
- Kuenzli, E. Antibiotic resistance and international travel: Causes and consequences. Travel Med. Infect. Dis. 2016, 14, 595–598. [Google Scholar] [CrossRef]
- DeFrancesco, A.S.; Tanih, N.F.; Samie, A.; Guerrant, R.L.; Bessong, P.O. Antibiotic resistance patterns and beta-lactamase identification in Escherichia coli isolated from young children in rural Limpopo Province, South Africa: The MAL-ED cohort. S. Afr. Med. J. 2017, 107, 205. [Google Scholar] [CrossRef]
- Tzouvelekis, L.S.; Tzelepi, E.; Tassios, P.; Legakis, N. CTX-M-type β-lactamases: An emerging group of extended-spectrum enzymes. Int. J. Antimicrob. Agents 2000, 14, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Hisham, A. Molecular Characterization of CTX-M ESBLs among Pathogenic Enterobacteriaceae isolated from different regions in Sudan. Glob. Adv. Res. J. Microbiol. 2017, 7, 40–46. Available online: http://garj.org/garjm (accessed on 5 December 2023).
- Rossolini, G.M.; D’Andrea, M.; Mugnaioli, C. The spread of CTX-M-type extended-spectrum blactamases. Clin. Microbiol. Infect. 2008, 5, 21–24. [Google Scholar] [CrossRef]
- Seo, K.W.; Do, K.H.; Lee, W.K. Comparative Genetic Characterization of CTX-M-Producing Escherichia coli Isolated from Humans and Pigs with Diarrhea in Korea Using Next-Generation Sequencing. Microorganisms 2023, 11, 1922. [Google Scholar] [CrossRef] [PubMed]
- Osawa, K.; Shigemura, K.; Shimizu, R.; Kato, A.; Kusuki, M.; Jikimoto, T.; Nakamura, T.; Yoshida, H.; Arakawa, S.; Fujisawa, M.; et al. Molecular characteristics of extended-spectrum β-lactamase-producing Escherichia coli in a university teaching hospital. Microb. Drug Resist. 2015, 21, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Awosile, B.B.; Agbaje, M.; Adebowale, O.; Kehinde, O.; Omoshaba, E. Beta-lactamase resistance genes in Enterobacteriaceae from Nigeria. Afr. J. Lab. Med. 2022, 11, 1371. [Google Scholar] [CrossRef]
- Kim, J.S.; Kim, J.; Kim, S.-J.; Jeon, S.-E.; Oh, K.H.; Cho, S.-H.; Kang, Y.-H.; Han, S.Y.; Chung, G.T. Characterization of CTX-M-Type Extended-Spectrum Beta-Lactamase-Producing Diarrheagenic Escherichia coli Isolates in the Republic of Korea during 2008–2011. J. Microbiol. Biotechnol. 2014, 24, 421–426. [Google Scholar] [CrossRef]
- Karami, P.; Bazmamoun, H.; Sedighi, I.; Nejad, A.S.M.; Aslani, M.M.; Alikhani, M.Y. Antibacterial resistance patterns of extended spectrum β-lactamase-producing enteropathogenic Escherichia coli strains isolated from children. Arab. J. Gastroenterol. 2017, 18, 206–209. [Google Scholar] [CrossRef]
- Konaté, A.; Dembélé, R.; Kagambèga, A.; Soulama, I.; Kaboré, W.A.D.; Sampo, E.; Cissé, H.; Sanou, A.; Serme, S.; Zongo, S.; et al. Molecular characterization of diarrheagenic Escherichia coli in children less than 5 years of age with diarrhea in Ouagadougou, Burkina Faso. Eur. J. Microbiol. Immunol. 2017, 7, 220–228. [Google Scholar] [CrossRef]
- Swierczewski, B.E.; Odundo, E.A.; Koech, M.C.; Ndonye, J.N.; Kirera, R.K.; Odhiambo, C.P.; Cheruiyot, E.K.; Wu, M.T.; Lee, J.E.; Zhang, C.; et al. Surveillance for enteric pathogens in a case-control study of acute diarrhea in Western Kenya. Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 83–90. [Google Scholar] [CrossRef]
- Dembélé, R.; Konaté, A.; Traoré, O.; Kaboré, W.A.D.; Soulama, I.; Kagambèga, A.; Traoré, A.S.; Guessennd, N.K.; Aidara-Kane, A.; Gassama-Sow, A.; et al. Extended spectrum beta-lactamase and fluoroquinolone resistance genes among Escherichia coli and Salmonella isolates from children with diarrhea, Burkina Faso. BMC Pediatr. 2020, 20, 459. [Google Scholar] [CrossRef]
- Khairy, R.M.M.; Fathy, Z.A.; Mahrous, D.M.; Mohamed, E.S.; Abdelrahim, S.S. Prevalence, phylogeny, and antimicrobial resistance of Escherichia coli pathotypes isolated from children less than 5 years old with community acquired-diarrhea in Upper Egypt. BMC Infect. Dis. 2020, 20, 908. [Google Scholar] [CrossRef]
- Tellevik, M.G.; Blomberg, B.; Kommedal, Ø.; Maselle, S.Y.; Langeland, N.; Moyo, S.J. High Prevalence of Faecal Carriage of ESBL-Producing Enterobacteriaceae among Children in Dar es Salaam, Tanzania. PLoS ONE 2016, 11, e0168024. [Google Scholar] [CrossRef] [PubMed]
- Woerther, P.-L.; Angebault, C.; Jacquier, H.; Hugede, H.-C.; Janssens, A.-C.; Sayadi, S.; El Mniai, A.; Armand-Lefèvre, L.; Ruppé, E.; Barbier, F.; et al. Massive Increase, Spread, and Exchange of Extended Spectrum-Lactamase-Encoding Genes among Intestinal Enterobacteriaceae in Hospitalized Children with Severe Acute Malnutrition in Niger. Clin. Infect. Dis. 2011, 53, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Sewunet, T.; Asrat, D.; Woldeamanuel, Y.; Ny, S.; Westerlund, F.; Aseffa, A.; Giske, C.G. Polyclonal spread of blaCTX-M-15 through high-risk clones of Escherichia coli at a tertiary hospital in Ethiopia. J. Glob. Antimicrob. Resist. 2022, 29, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.F.; Ali, M.M.M.; Mohamed, Z.K.; Moussa, T.A.; Klena, J.D. Fecal carriage of extended-spectrum β-lactamases and AmpC-producing Escherichia coli in a Libyan community. Ann. Clin. Microbiol. Antimicrob. 2014, 13, 22. [Google Scholar] [CrossRef]
- Imtyaz, A.; Haleem, A.; Javaid, M. Analysing governmental response to the COVID-19 pandemic. J. Oral. Biol. Craniofac. Res. 2020, 10, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Malvi, S.; Appannanavar, S.; Mohan, B.; Kaur, H.; Gautam, N.; Bharti, B.; Kumar, Y.; Taneja, N. Comparative analysis of virulence determinants, antibiotic susceptibility patterns and serogrouping of atypical enteropathogenic Escherichia coli versus typical enteropathogenic E. coli in India. J. Med. Microbiol. 2015, 64, 1208–1215. [Google Scholar] [CrossRef][Green Version]
- Natarajan, M.; Kumar, D.; Mandal, J.; Biswal, N.; Stephen, S. A study of virulence and antimicrobial resistance pattern in diarrhoeagenic Escherichia coli isolated from diarrhoeal stool specimens from children and adults in a tertiary hospital, Puducherry, India. J. Health Popul. Nutr. 2018, 37, 17. [Google Scholar] [CrossRef]
- Alizade, H.; Fallah, F.; Ghanbarpour, R.; Aflatoonian, M.R.; Goudarzi, H.; Sharifi, H. Phylogenetic groups, extended-spectrum β-lactamases and metallo-β-lactamase in Escherichia coli isolated from fecal samples of patients with diarrhea in Iran. Gastro-enterol. Hepatol. Bed Bench 2015, 8, 207–214. [Google Scholar]
- Bartoloni, A.; Pallecchi, L.; Riccobono, E.; Mantella, A.; Magnelli, D.; Di Maggio, T.; Villagran, A.; Lara, Y.; Saavedra, C.; Strohmeyer, M.; et al. Relentless increase of resistance to fluoroquinolones and expanded-spectrum cephalosporins in Escherichia coli: 20 years of surveillance in resource-limited settings from Latin America. Clin. Microbiol. Infect. 2013, 19, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Ferro, T.A.F.; Moraes, F.C.; da Silva, A.M.; Porcy, C.; Soares, L.A.; Monteiro, C.A.; Lobão, N.T.M.; de Mello, F.A.A.; Mon-teiro-Neto, V.; Figueirêdo, P.d.M.S. Characterization of Virulence Factors in Enteroaggregative and Atypical Enteropathogenic Escherichia coli Strains Isolated from Children with Diarrhea. Adv. Infect. Dis. 2012, 2, 135–142. [Google Scholar] [CrossRef][Green Version]
- Abdelwahab, R.; Yasir, M.; Godfrey, R.E.; Christie, G.S.; Element, S.J.; Saville, F.; Hassan, E.A.; Ahmed, E.H.; Abu-Faddan, N.H.; Daef, E.A.; et al. Antimicrobial resistance and gene regulation in Enteroaggregative Escherichia coli from Egyptian children with diarrhoea: Similarities and differences. Virulence 2021, 12, 57–74. [Google Scholar] [CrossRef] [PubMed]
- Omran, E.A.; Mahafzan, A.M.; Shehabi, A.A. Antimicrobial resistance patterns of diarrheagenic and non-diarrheagenic Esch-erichia coli isolates from Libyan children. Int. Arab. J. Antimicrob. Agents 2014, 4, 1–8. [Google Scholar]
- Boxall, M.D.; Day, M.R.; Greig, D.R.; Jenkins, C. Antimicrobial resistance profiles of diarrhoeagenic Escherichia coli isolated from travellers returning to the UK, 2015–2017. J. Med. Microbiol. 2020, 69, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Singh, P.K.; Das, S.; Wani, S.; Jawed, A.; Dar, S.A. Transcriptome analysis of beta-lactamase genes in diarrheagenic Escherichia coli. Sci. Rep. 2019, 9, 3626. [Google Scholar] [CrossRef]
- Kim, K.G.; Jeong, J.; Kim, M.J.; Park, D.W.; Shin, J.H.; Park, H.J.; Chung, J.K.; Kee, H.Y. Prevalence and molecular epidemiology of ESBLs, plasmid-determined AmpC-type β-lactamases and carbapenemases among diarrhoeagenic Escherichia coli isolates from children in Gwangju, Korea: 2007–16. J. Antimicrob. Chemother. 2019, 74, 2181–2187. [Google Scholar] [CrossRef]
- Jomehzadeh, N.; Ahmadi, K.; Javaherizadeh, H.; Afzali, M. The first evaluation relationship of integron genes and the mul-tidrug-resistance in class A ESBLs genes in enteropathogenic Escherichia coli strains isolated from children with diarrhea in Southwestern Iran. Mol. Biol. Rep. 2021, 48, 307–313. [Google Scholar] [CrossRef]
- Jafari, E.; Oloomi, M.; Bouzari, S. Characterization of antimicrobial susceptibility, extended-spectrum β-lactamase genes and phylogenetic groups of Shigatoxin producing Escherichia coli isolated from patients with diarrhea in Iran. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 24. [Google Scholar] [CrossRef]
- Eltai, N.O.; Al Thani, A.A.; Al Hadidi, S.H.; Al Ansari, K.; Yassine, H.M. Antibiotic resistance and virulence patterns of pathogenic Escherichia coli strains associated with acute gastroenteritis among children in Qatar. BMC Microbiol. 2020, 20, 54. [Google Scholar] [CrossRef]
- Taghadosi, R.; Shakibaie, M.R.; Hosseini-Nave, H. Antibiotic resistance, ESBL genes, integrons, phylogenetic groups and MLVA profiles of Escherichia coli pathotypes isolated from patients with diarrhea and farm animals in south-east of Iran. Comp. Immunol. Microbiol. Infect. Dis. 2019, 63, 117–126. [Google Scholar] [CrossRef]
- Wasito, E.B.; Shigemura, K.; Osawa, K.; Fardah, A.; Kanaida, A.; Raharjo, D.; Kuntaman, K.; Hadi, U.; Harijono, S.; Sudarmo, S.M.; et al. Antibiotic Susceptibilities and Genetic Characteristics of Extended-Spectrum Beta-Lactamase-Producing Escherichia coli Isolates from Stools of Pediatric Diarrhea Patients in Surabaya, Indonesia. Jpn. J. Infect. Dis. 2017, 70, 378–382. [Google Scholar] [CrossRef]
- Nawaz, Z.; Zahoor, M.K.; Siddique, A.B.; Aslam, B.; Muzammil, S.; Yasmin, A.; Fayyaz, I.; Zahoor, M.A. Molecular identification of blaCTX-M and blaTEM genes among multi-drug resistant Enteropathogenic Escherichia coli isolated from children. Pak. J. Pharm. Sci. 2019, 32, 1215–1218. [Google Scholar] [PubMed]
- Imuta, N.; Ooka, T.; Seto, K.; Kawahara, R.; Koriyama, T.; Kojyo, T.; Iguchi, A.; Tokuda, K.; Kawamura, H.; Yoshiie, K.; et al. Phylogenetic Analysis of Enteroaggregative Escherichia coli (EAEC) Isolates from Japan Reveals Emergence of CTX-M-14-Producing EAEC O25:H4 Clones Related to Sequence Type 131. J. Clin. Microbiol. 2016, 54, 2128–2134. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, D.; Chowdhury, G.; Samanta, P.; Shaw, S.; Deb, A.K.; Bardhan, M.; Manna, A.; Miyoshi, S.-I.; Ramamurthy, T.; Dutta, S.; et al. Characterization of diarrhoeagenic Escherichia coli with special reference to antimicrobial resistance isolated from hospitalized diarrhoeal patients in Kolkata (2012–2019), India. J. Appl. Microbiol. 2022, 132, 4544–4554. [Google Scholar] [CrossRef]
- Shahbazi, G.; Rezaee, M.A.; Nikkhahi, F.; Ebrahimzadeh, S.; Hemmati, F.; Namarvar, B.B.; Gholizadeh, P. Characteristics of diarrheagenic Escherichia coli pathotypes among children under the age of 10 years with acute diarrhea. Gene Rep. 2021, 25, 101318. [Google Scholar] [CrossRef]
- Huang, Y.; Shan, X.-F.; Deng, H.; Huang, Y.-J.; Mu, X.-P.; Huang, A.-L.; Long, Q.-X. Epidemiology, Antimicrobial Resistance and β-lactamase Genotypic Features of Enteropathogenic Escherichia coli Isolated from Children with Diarrhea in Southern China. Jpn. J. Infect. Dis. 2015, 68, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Farajzadeh-Sheikh, A.; Savari, M.; Nave, H.H.; Ahmadi, K.A.; Afzali, M. Frequency and molecular epidemiology of class A ESBLs producing Enteroinvasive Escherichia coli (EIEC) isolates among patients with diarrhea. Gastroenterol. Hepatol. Bed Bench 2020, 13, 77–85. [Google Scholar]
- Bai, L.; Wang, L.; Yang, X.; Wang, J.; Gan, X.; Wang, W.; Xu, J.; Chen, Q.; Lan, R.; Fanning, S.; et al. Prevalence and Molecular Characteristics of Extended-Spectrum β-Lactamase Genes in Escherichia coli Isolated from Diarrheic Patients in China. Front. Microbiol. 2017, 8, 144. [Google Scholar] [CrossRef]
- Alsherees, H.A.A.; Alia, S.N.A. Preliminary Occurrence of Extended-Spectrum and AmpC Beta-Lactamases in Clinical Isolates of Enteropathogenic Escherichia coli in Najaf, Iraq. bioRxiv 2019, 512731. [Google Scholar] [CrossRef]
- Abbasi, E.; Mondanizadeh, M.; van Belkum, A.; Ghaznavi-Rad, E. Multi-Drug-Resistant Diarrheagenic Escherichia coli Patho-types in Pediatric Patients with Gastroenteritis from Central Iran. Infect. Drug Resist. 2020, 13, 1387–1396. [Google Scholar] [CrossRef]
- Sirous, M.; Hashemzadeh, M.; Keshtvarz, M.; Amin, M.; Shams, N.; Dastoorpoor, M.; Shahin, M.; Koraei, D. Molecular Characterization and Antimicrobial Resistance of Enteropathogenic Escherichia coli in Children from Ahvaz, Iran. Jundishapur J. Microbiol. 2020, 13, e100877. [Google Scholar] [CrossRef]
- Saka, H.K.; García-Soto, S.; Dabo, N.T.; Lopez-Chavarrias, V.; Muhammad, B.; Ugarte-Ruiz, M.; Alvarez, J. Molecular detection of extended spectrum β-lactamase genes in Escherichia coli clinical isolates from diarrhoeic children in Kano, Nigeria. PLoS ONE 2020, 15, e0243130. [Google Scholar] [CrossRef] [PubMed]
- Boutet-Dubois, A.; Pantel, A.; Prère, M.-F.; Bellon, O.; Brieu-Roche, N.; Lecaillon, E.; Coustumier, A.; Davin-Regli, A.; Villeneuve, L.; Bouziges, N.; et al. Faecal carriage of oxyiminocephalosporin-resistant Enterobacteriaceae among paediatric units in different hospitals in the south of France. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Salah, M.A.A.; Badran, E.F.; Shehabi, A.A. High incidence of multidrug resistant Escherichia coli producing CTX-M-type ESBLs colonizing the intestine of Jordanian infants. Int. Arab. J. Antimicrob. Agents 2013, 3, 1–8. [Google Scholar]
- Ho, W.S.; Balan, G.; Puthucheary, S.; Kong, B.H.; Lim, K.T.; Tan, L.K.; Koh, X.P.; Yeo, C.C.; Thong, K.L.; Yap, K.-P.; et al. Prevalence and characterization of multidrug-resistant and extended-spectrum beta-lactamase-producing Escherichia coli from pediatric wards of a Malaysian hospital. Microb. Drug Resist. 2012, 18, 408–416. [Google Scholar] [CrossRef]
- O’connor, C.; Philip, R.K.; Kelleher, J.; Powell, J.; O’gorman, A.; Slevin, B.; Woodford, N.; Turton, J.F.; McGrath, E.; Finnegan, C.; et al. The first occurrence of a CTX-M ESBL-producing Escherichia coli outbreak mediated by mother to neonate transmission in an Irish neonatal intensive care unit. BMC Infect. Dis. 2017, 17, 16. [Google Scholar] [CrossRef]
- Kang, C.I.; Song, J.H. Antimicrobial resistance in Asia: Current epidemiology and clinical implications. Infect. Chemother. 2013, 45, 22–31. [Google Scholar] [CrossRef]
- Adedokun, S.T.; Yaya, S. Childhood morbidity and its determinants: Evidence from 31 countries in sub-Saharan Africa. BMJ Global Health 2020, 5, e003109. [Google Scholar] [CrossRef]
- Oppong, T.B.; Yang, H.; Amponsem-Boateng, C.; Kyere, E.D.; Abdulai, T.; Duan, G.; Opolot, G. Enteric pathogens associated with gastroenteritis among children under 5 years in sub-Saharan Africa: A systematic review and meta-analysis. Epidemiol. Infect. 2020, 148, e64. [Google Scholar] [CrossRef]
- Peirano, G.; Pitout, J.D. Molecular epidemiology of Escherichia coli producing CTX-M beta-lactamases: The worldwide emergence of clone ST131 O25:H4. Int. J. Antimicrob. Agents 2010, 35, 316–321. [Google Scholar] [CrossRef]
- Karanika, S.; Karantanos, T.; Arvanitis, M.; Grigoras, C.; Mylonakis, E. Fecal Colonization with Extended-spectrum Be-ta-lactamase-Producing Enterobacteriaceae and Risk Factors among Healthy Individuals: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2016, 63, 310–318. [Google Scholar] [CrossRef]
| No. of EPEC Isolates | Prevalence of CTX-M Producers (%) | Prevalence of blaCTXM-15 | Reference |
|---|---|---|---|
| 87 | 13 (15) | ND | [45] |
| 59 | 7 (12) | 7 | [30] |
| 58 | 31 (56) | ND | [49] |
| 192 | 21 (11) | ND | [20] |
| 22 | 17 (77) | ND | [52] |
| 14 | 10 (71) | ND | [40] |
| 42 | 8 (19) | 8 | [4] |
| 17 | 12 (71) | ND | [54] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karambwe, S.; Traoré, A.N.; Potgieter, N. Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022. Microorganisms 2024, 12, 171. https://doi.org/10.3390/microorganisms12010171
Karambwe S, Traoré AN, Potgieter N. Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022. Microorganisms. 2024; 12(1):171. https://doi.org/10.3390/microorganisms12010171
Chicago/Turabian StyleKarambwe, Simbarashe, Afsatou Ndama Traoré, and Natasha Potgieter. 2024. "Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022" Microorganisms 12, no. 1: 171. https://doi.org/10.3390/microorganisms12010171
APA StyleKarambwe, S., Traoré, A. N., & Potgieter, N. (2024). Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022. Microorganisms, 12(1), 171. https://doi.org/10.3390/microorganisms12010171





