SARS-CoV-2 Induced Herpes Virus Reactivations and Related Implications in Oncohematology: When Lymphocytopenia Sets in and Immunosurveillance Drops Out
Conflicts of Interest
References
- Roncati, L.; Palmieri, B. What about the original antigenic sin of the humans versus SARS-CoV-2? Med. Hypotheses 2020, 142, 109824. [Google Scholar] [CrossRef]
- Roncati, L.; Corsi, L. Nucleoside-modified messenger RNA COVID-19 vaccine platform. J. Med. Virol. 2021, 93, 4054–4057. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 26 July 2023).
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef] [PubMed]
- Roncati, L.; Gallo, G.; Manenti, A.; Palmieri, B. Renin-angiotensin system: The unexpected flaw inside the human immune system revealed by SARS-CoV-2. Med. Hypotheses 2020, 140, 109686. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef] [PubMed]
- Roncati, L.; Lusenti, B. The «moonlighting protein» able to explain the Th1 immune lockdown in severe COVID-19. Med. Hypotheses 2020, 143, 110087. [Google Scholar] [CrossRef] [PubMed]
- Sehrawat, S.; Kumar, D.; Rouse, B.T. Herpesviruses: Harmonious pathogens but relevant cofactors in other diseases? Front. Cell. Infect. Microbiol. 2018, 8, 177. [Google Scholar] [CrossRef]
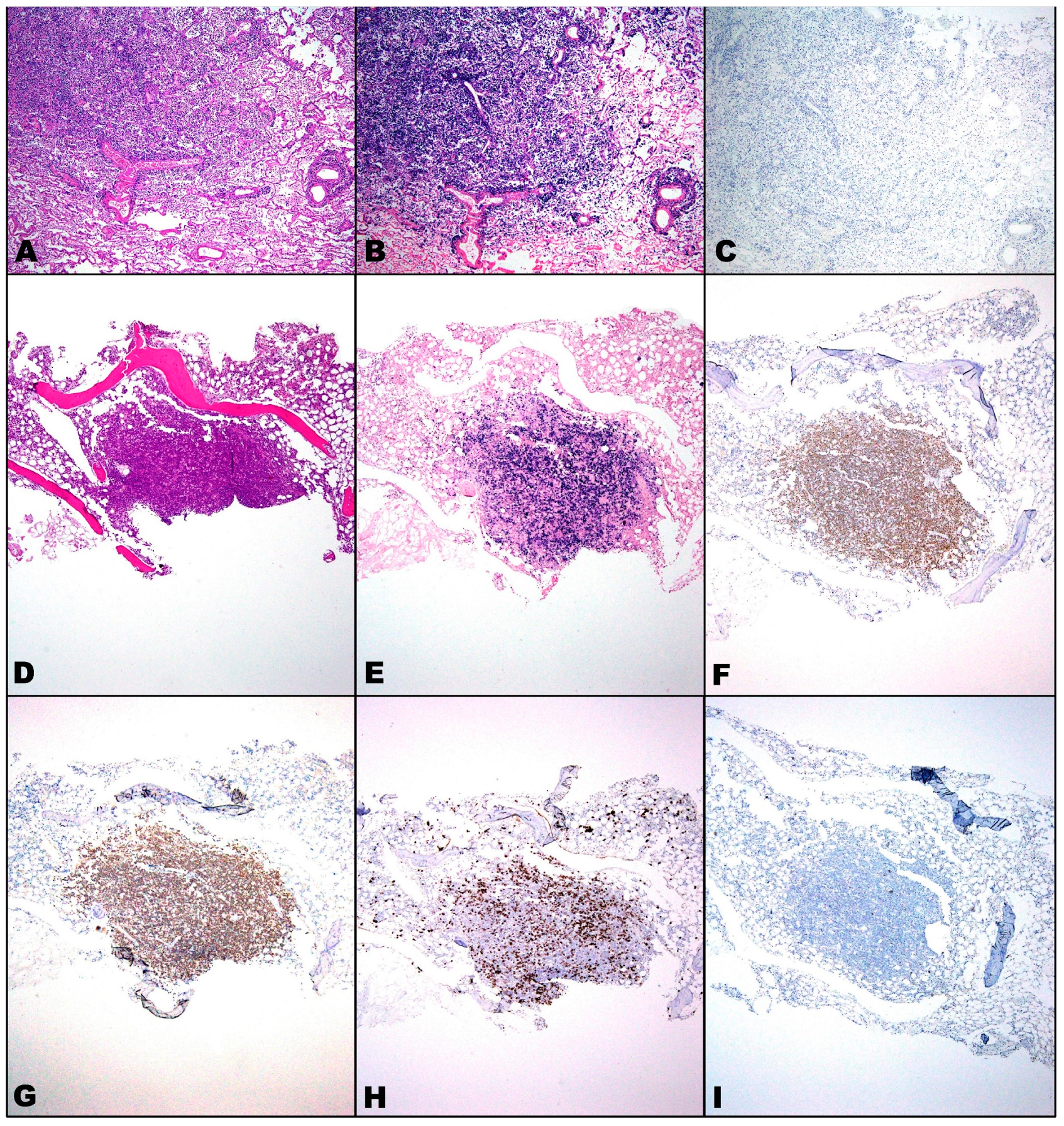
- Roncati, L.; Manenti, A.; Fabbiani, L.; Malagoli, C.; Nasillo, V.; Lusenti, B.; Lupi, M.; Zanelli, G.; Salviato, T.; Costantini, M.; et al. HSV1 viremia with fulminant hepatitis as opportunistic sequela in severe COVID-19. Ann. Hematol. 2022, 101, 229–231. [Google Scholar] [CrossRef]
- Franceschini, E.; Cozzi-Lepri, A.; Santoro, A.; Bacca, E.; Lancellotti, G.; Menozzi, M.; Gennari, W.; Meschiari, M.; Bedini, A.; Orlando, G.; et al. Herpes simplex virus re-activation in patients with SARS-CoV-2 pneumonia: A prospective, observational study. Microorganisms 2021, 9, 1896. [Google Scholar] [CrossRef]
- Shafiee, A.; Teymouri Athar, M.M.; Amini, M.J.; Hajishah, H.; Siahvoshi, S.; Jalali, M.; Jahanbakhshi, B.; Mozhgani, S.H. Reactivation of herpesviruses during COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2023, 33, e2437. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Di Bella, S.; Dettori, S.; Brucci, G.; Zerbato, V.; Pol, R.; Segat, L.; D’Agaro, P.; Roman-Pognuz, E.; Friso, F.; et al. Reactivation of herpes simplex virus type 1 (HSV-1) detected on bronchoalveolar lavage fluid (BALF) samples in critically ill COVID-19 patients undergoing invasive mechanical ventilation: Preliminary results from two Italian centers. Microorganisms 2022, 10, 362. [Google Scholar] [CrossRef]
- Bhavsar, A.; Lonnet, G.; Wang, C.; Chatzikonstantinidou, K.; Parikh, R.; Brabant, Y.; Servotte, N.; Shi, M.; Widenmaier, R.; Aris, E. Increased risk of herpes zoster in adults ≥50 years old diagnosed with COVID-19 in the United States. Open Forum Infect. Dis. 2022, 9, ofac118. [Google Scholar] [CrossRef] [PubMed]
- Fuest, K.E.; Erber, J.; Berg-Johnson, W.; Heim, M.; Hoffmann, D.; Kapfer, B.; Kriescher, S.; Ulm, B.; Schmid, R.M.; Rasch, S.; et al. Risk factors for herpes simplex virus (HSV) and cytomegalovirus (CMV) infections in critically ill COVID-19 patients. Multidiscip. Respir. Med. 2022, 17, 815. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Pedrero Sánchez-Belmonte, M.J.; Sánchez-Casado, M.; Moran Gallego, F.J.; Piza Pinilla, R.; Gomez Hernando, C.; Paredes Borrachero, I. Herpes simplex virus type 1 (HSV-1) over-infection in patients with acute respiratory distress syndrome secondary to COVID-19 pneumonia: Impact on mortality. Med. Clin. 2023, 160, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Giacobbe, D.R.; Di Bella, S.; Lovecchio, A.; Ball, L.; De Maria, A.; Vena, A.; Bruzzone, B.; Icardi, G.; Pelosi, P.; Luzzati, R.; et al. Herpes simplex virus 1 (HSV-1) reactivation in critically ill COVID-19 patients: A brief narrative review. Infect. Dis. Ther. 2022, 11, 1779–1791. [Google Scholar] [CrossRef] [PubMed]
- Marques, N.P.; Maia, C.M.F.; Marques, N.C.T.; de Lucena, E.H.G.; Martelli, D.R.B.; Oliveira, E.A.; Martelli-Júnior, H. Continuous increase of herpes zoster cases in Brazil during the COVID-19 pandemic. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 133, 612–614. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, V.C.S.; Alves-Leon, S.V.; Sarmento, D.J.S.; Coelho, W.L.D.C.N.P.; Moreira, O.D.C.; Salvio, A.L.; Ramos, C.H.F.; Ramos Filho, C.H.F.; Marques, C.A.B.; da Costa Gonçalves, J.P.; et al. Herpesvirus and neurological manifestations in patients with severe coronavirus disease. Virol. J. 2022, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Czech, T.; Nishimura, Y. Characteristics of herpes zoster infection in patients with COVID-19: A systematic scoping review. Int. J. Dermatol. 2022, 61, 1087–1092. [Google Scholar] [CrossRef]
- Ramírez-Colombres, M.; Maenza, C.E.; Rocchetti, N.S.; Gattino, S.P.; Diodati, S.; Luchitta, C.A.; Ré, M.D.; Settecase, C.J.; Bagilet, D.H. COVID-19 and herpesvirus encephalitis. Rev. Neurol. 2022, 74, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Majtanova, N.; Kriskova, P.; Keri, P.; Fellner, Z.; Majtan, J.; Kolar, P. Herpes simplex keratitis in patients with SARS-CoV-2 infection: A series of five cases. Medicina 2021, 57, 412. [Google Scholar] [CrossRef]
- Meyer, A.; Buetti, N.; Houhou-Fidouh, N.; Patrier, J.; Abdel-Nabey, M.; Jaquet, P.; Presente, S.; Girard, T.; Sayagh, F.; Ruckly, S.; et al. HSV-1 reactivation is associated with an increased risk of mortality and pneumonia in critically ill COVID-19 patients. Crit. Care 2021, 25, 417. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Reviejo, R.; Tejada, S.; Adebanjo, G.A.R.; Chello, C.; Machado, M.C.; Parisella, F.R.; Campins, M.; Tammaro, A.; Rello, J. Varicella zoster virus reactivation following severe acute respiratory syndrome coronavirus 2 vaccination or infection: New insights. Eur. J. Intern. Med. 2022, 104, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Maple, P.A.C. COVID-19, SARS-CoV-2 vaccination, and human herpesviruses infections. Vaccines 2023, 11, 232. [Google Scholar] [CrossRef] [PubMed]
- Hertel, M.; Heiland, M.; Nahles, S.; von Laffert, M.; Mura, C.; Bourne, P.E.; Preissner, R.; Preissner, S. Real-world evidence from over one million COVID-19 vaccinations is consistent with reactivation of the varicella zoster virus. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Wan, E.Y.F.; Chui, C.S.L.; Wang, Y.; Ng, V.W.S.; Yan, V.K.C.; Lai, F.T.T.; Li, X.; Wong, C.K.H.; Chan, E.W.Y.; Wong, C.S.M.; et al. Herpes zoster related hospitalization after inactivated (CoronaVac) and mRNA (BNT162b2) SARS-CoV-2 vaccination: A self-controlled case series and nested case-control study. Lancet Reg. Health West. Pac. 2022, 21, 100393. [Google Scholar] [CrossRef] [PubMed]
- Gringeri, M.; Battini, V.; Cammarata, G.; Mosini, G.; Guarnieri, G.; Leoni, C.; Pozzi, M.; Radice, S.; Clementi, E.; Carnovale, C. Herpes zoster and simplex reactivation following COVID-19 vaccination: New insights from a vaccine adverse event reporting system (VAERS) database analysis. Expert Rev. Vaccines 2022, 21, 675–684. [Google Scholar] [CrossRef]
- Chu, C.W.; Jiesisibieke, Z.L.; Yang, Y.P.; Wu, P.C.; Lin, H.L.; Tung, T.H. Association of COVID-19 vaccination with herpes zoster: A systematic review and meta-analysis. Expert Rev. Vaccines 2022, 21, 601–608. [Google Scholar] [CrossRef]
- Naoum, C.; Hartmann, M. Herpes zoster reactivation after COVID-19 vaccination—A retrospective case series of 22 patients. Int. J. Dermatol. 2022, 61, 628–629. [Google Scholar] [CrossRef]
- Chen, J.; Li, F.; Tian, J.; Xie, X.; Tang, Q.; Chen, Y.; Ge, Y. Varicella zoster virus reactivation following COVID-19 vaccination in patients with autoimmune inflammatory rheumatic diseases: A cross-sectional Chinese study of 318 cases. J. Med. Virol. 2023, 95, e28307. [Google Scholar] [CrossRef]
- Akpandak, I.; Miller, D.C.; Sun, Y.; Arnold, B.F.; Kelly, J.D.; Acharya, N.R. Assessment of herpes zoster risk among recipients of COVID-19 vaccine. JAMA Netw. Open 2022, 5, e2242240. [Google Scholar] [CrossRef]
- Singh, R.B.; Parmar, U.P.S.; Ichhpujani, P.; Jeng, B.H.; Jhanji, V. Herpetic eye disease after SARS-CoV-2 vaccination: A CDC-VAERS database analysis. Cornea 2023, 42, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Kuziez, L.; Eleiwa, T.K.; Chauhan, M.Z.; Sallam, A.B.; Elhusseiny, A.M.; Saeed, H.N. Corneal adverse events associated with SARS-CoV-2/COVID-19 vaccination: A systematic review. Vaccines 2023, 11, 166. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Y.; Chiang, C.C.; Li, Y.L.; Lai, H.Y.; Hsieh, Y.C.; Wu, Y.H.; Tsai, Y.Y. Corneal complications after COVID-19 vaccination: A systemic review. J. Clin. Med. 2022, 11, 6828. [Google Scholar] [CrossRef]
- Ichhpujani, P.; Parmar, U.P.S.; Duggal, S.; Kumar, S. COVID-19 vaccine-associated ocular adverse effects: An overview. Vaccines 2022, 10, 1879. [Google Scholar] [CrossRef] [PubMed]
- Pillar, S.; Weinberg, T.; Amer, R. Posterior ocular manifestations following BNT162b2 mRNA COVID-19 vaccine: A case series. Int. Ophthalmol. 2022, 43, 1677–1686. [Google Scholar] [CrossRef]
- Alpalhão, M.; Filipe, P. Herpes zoster following SARS-CoV-2 vaccination—A series of four cases. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 750–752. [Google Scholar] [CrossRef]
- Rodríguez-Jiménez, P.; Chicharro, P.; Cabrera, L.M.; Seguí, M.; Morales-Caballero, Á.; Llamas-Velasco, M.; Sánchez-Pérez, J. Varicella zoster virus reactivation after SARS-CoV-2 BNT162b2 mRNA vaccination: Report of 5 cases. JAAD Case Rep. 2021, 12, 58–59. [Google Scholar] [CrossRef] [PubMed]
- Furer, V.; Zisman, D.; Kibari, A.; Rimar, D.; Paran, Y.; Elkayam, O. Herpes zoster following BNT162b2 mRNA COVID-19 vaccination in patients with autoimmune inflammatory rheumatic diseases: A case series. Rheumatology 2021, 60, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Papasavvas, I.; de Courten, C.; Herbort, C.P., Jr. Varicella-zoster virus reactivation causing herpes zoster ophthalmicus (HZO) after SARS-CoV-2 vaccination—Report of three cases. J. Ophthalmic Inflamm. Infect. 2021, 11, 28. [Google Scholar] [CrossRef]
- Fathy, R.A.; McMahon, D.E.; Lee, C.; Chamberlin, G.C.; Rosenbach, M.; Lipoff, J.B.; Tyagi, A.; Desai, S.R.; French, L.E.; Lim, H.W.; et al. Varicella zoster and herpes simplex virus reactivation post-COVID-19 vaccination: A review of 40 cases in an International Dermatology Registry. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 6–9. [Google Scholar] [CrossRef]
- Ibuchi, Y.; Tamayose, F.; Katayama, H.; Saeki, H.; Osada, S.I. Varicella zoster virus reactivation after coronavirus disease 2019 vaccination in Japanese patients: A series of 14 cases. J. Dermatol. 2022, 49, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Koumaki, D.; Krueger-Krasagakis, S.E.; Papadakis, M.; Katoulis, A.; Koumaki, V.; Evangelou, G.; Stefanidou, M.; Mylonakis, D.; Zografaki, K.; Krasagakis, K. Herpes zoster viral infection after AZD1222 and BNT162b2 coronavirus disease 2019 mRNA vaccines: A case series. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 85–86. [Google Scholar] [CrossRef] [PubMed]
- Katsikas Triantafyllidis, K.; Giannos, P.; Mian, I.T.; Kyrtsonis, G.; Kechagias, K.S. Varicella zoster virus reactivation following COVID-19 vaccination: A systematic review of case reports. Vaccines 2021, 9, 1013. [Google Scholar] [CrossRef] [PubMed]
- Kluger, N.; Klimenko, T.; Bosonnet, S. Herpes simplex, herpes zoster and periorbital erythema flares after SARS-CoV-2 vaccination: 4 cases. Ann. Dermatol. Venereol. 2022, 149, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Fukuoka, H.; Fukuoka, N.; Kibe, T.; Tubbs, R.S.; Iwanaga, J. Oral herpes zoster infection following COVID-19 vaccination: A report of five cases. Cureus 2021, 13, e19433. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.J.; Lu, C.H.; Hsieh, S.C. Herpes zoster reactivation after mRNA-1273 vaccination in patients with rheumatic diseases. Ann. Rheum. Dis. 2022, 81, 595–597. [Google Scholar] [CrossRef] [PubMed]
- Tejada Cifuentes, F.; Lloret Callejo, Á.; Tirado Peláez, M.J. COVID-19 vaccines and herpes infection. Med. Clin. 2021, 157, 355–356. [Google Scholar] [CrossRef]
- Chen, I.L.; Chiu, H.Y. Association of herpes zoster with COVID-19 vaccination: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2023, 21, 601–608. [Google Scholar] [CrossRef]
- Twagirimana, S.; Doucet, S.; Meunier, C.; Maietta, A. Expanding the spectrum of Epstein-Barr virus and human herpesvirus-8 co-infection associated large B-cell lymphomas with plasmablastic differentiation in HIV-positive patients: Report of two unusual cases and review of the literature. Hum. Pathol. Rep. 2022, 29, 300657. [Google Scholar] [CrossRef]
- Roncati, L.; Lusenti, B.; Nasillo, V.; Manenti, A. Fatal SARS-CoV-2 coinfection in course of EBV-associated lymphoproliferative disease. Ann. Hematol. 2020, 99, 1945–1946. [Google Scholar] [CrossRef]
- Paolucci, S.; Cassaniti, I.; Novazzi, F.; Fiorina, L.; Piralla, A.; Comolli, G.; Bruno, R.; Maserati, R.; Gulminetti, R.; Novati, S.; et al. EBV DNA increase in COVID-19 patients with impaired lymphocyte subpopulation count. Int. J. Infect. Dis. 2021, 104, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, A.; Aghajanian, S.; Athar, M.M.T.; Gargari, O.K. Epstein-Barr virus and COVID-19. J. Med. Virol. 2022, 94, 4040–4042. [Google Scholar] [CrossRef] [PubMed]
- Im, J.H.; Nahm, C.H.; Je, Y.S.; Lee, J.S.; Baek, J.H.; Kwon, H.Y.; Chung, M.H.; Jang, J.H.; Kim, J.S.; Lim, J.H.; et al. The effect of Epstein-Barr virus viremia on the progression to severe COVID-19. Medicine 2022, 101, e29027. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Cao, S.; Dong, H.; Lv, H.; Teng, X.; Zhang, J.; Wang, T.; Zhang, X.; Qin, Y.; Chai, Y.; et al. Clinical characteristics and outcomes of critically ill patients with acute COVID-19 with Epstein-Barr virus reactivation. BMC Infect. Dis. 2021, 21, 955. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, S.; Ying, L.Y. Epstein-Barr virus reactivation during COVID-19 hospitalization significantly increased mortality/death in SARS-CoV-2(+)/EBV(+) than SARS-CoV-2(+)/EBV(-) patients: A comparative meta-analysis. Int. J. Clin. Pract. 2023, 2023, 1068000. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Song, J.; Liu, H.; Zheng, H.; Chen, C. Positive Epstein-Barr virus detection in coronavirus disease 2019 (COVID-19) patients. Sci. Rep. 2021, 11, 10902. [Google Scholar] [CrossRef] [PubMed]
- Brooks, B.; Tancredi, C.; Song, Y.; Mogus, A.T.; Huang, M.W.; Zhu, H.; Phan, T.L.; Zhu, H.; Kadl, A.; Woodfolk, J.; et al. Epstein-Barr virus and human herpesvirus 6 reactivation in acute COVID-19 patients. Viruses 2022, 14, 1872. [Google Scholar] [CrossRef]
- Nadeem, A.; Suresh, K.; Awais, H.; Waseem, S. Epstein-Barr virus coinfection in COVID-19. J. Investig. Med. High Impact Case Rep. 2021, 9, 23247096211040626. [Google Scholar] [CrossRef]
- García-Martínez, F.J.; Moreno-Artero, E.; Jahnke, S. SARS-CoV-2 and EBV coinfection. Med. Clin. 2020, 155, 319–320. [Google Scholar] [CrossRef]
- Meng, M.; Zhang, S.; Dong, X.; Sun, W.; Deng, Y.; Li, W.; Li, R.; Annane, D.; Wu, Z.; Chen, D. COVID-19 associated EBV reactivation and effects of ganciclovir treatment. Immun. Inflamm. Dis. 2022, 10, e597. [Google Scholar] [CrossRef]
- Villafuerte, D.B.; Lavrynenko, O.; Qazi, R.; Passeri, M.F.; Sanchez, F.L. Chronic active Epstein-Barr exacerbated by COVID-19 co-infection. Int. J. Infect. Dis. 2022, 122, 976–978. [Google Scholar] [CrossRef] [PubMed]
- Dias, E.; Marques, M.; Lopes, S.; Gullo, I.; Bastos, J.; Macedo, G. Acute gastrointestinal graft-versus-host disease with cytomegalovirus and Epstein-Barr virus superinfection in a patient with COVID-19. Rev. Esp. Enferm. Dig. 2023, 115, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.; Karimi, S.; Follows, G.; Torpey, N.; Suchanek, O. Use of rituximab in SARS-CoV-2-positive renal transplant recipient with EBV reactivation and probable haemophagocytic lymphohistiocytosis. CEN Case Rep. 2023, 12, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Gardini, G.; Odolini, S.; Moioli, G.; Papalia, D.A.; Ferrari, V.; Matteelli, A.; Caligaris, S. Disseminated Kaposi sarcoma following COVID-19 in a 61-year-old Albanian immunocompetent man: A case report and review of the literature. Eur. J. Med. Res. 2021, 26, 152. [Google Scholar] [CrossRef] [PubMed]
- Magri, F.; Giordano, S.; Latini, A.; Muscianese, M. New-onset cutaneous Kaposi’s sarcoma following SARS-CoV-2 infection. J. Cosmet. Dermatol. 2021, 20, 3747–3750. [Google Scholar] [CrossRef] [PubMed]
- Yanes, R.R.; Malijan, G.M.B.; Escora-Garcia, L.K.; Ricafrente, S.A.M.; Salazar, M.J.; Suzuki, S.; Smith, C.; Ariyoshi, K.; Solante, R.M.; Edrada, E.M.; et al. Detection of SARS-CoV-2 and HHV-8 from a large pericardial effusion in an HIV-positive patient with COVID-19 and clinically diagnosed Kaposi sarcoma: A case report. Trop. Med. Health 2022, 50, 72. [Google Scholar] [CrossRef]
- Tang, W.R.; Hsu, C.W.; Lee, C.C.; Huang, W.L.; Lin, C.Y.; Hsu, Y.T.; Chang, C.; Tsai, M.T.; Hu, Y.N.; Hsu, C.H.; et al. A case report of posttransplant lymphoproliferative disorder after AstraZeneca Coronavirus Disease 2019 vaccine in a heart transplant recipient. Transplant. Proc. 2022, 54, 1575–1578. [Google Scholar] [CrossRef]
- Musialik, J.; Kolonko, A.; Więcek, A. Increased EBV DNAemia after anti-SARS-CoV-2 vaccination in solid organ transplants. Vaccines 2022, 10, 992. [Google Scholar] [CrossRef]
- Goldman, S.; Bron, D.; Tousseyn, T.; Vierasu, I.; Dewispelaere, L.; Heimann, P.; Cogan, E.; Goldman, M. Rapid progression of angioimmunoblastic T cell lymphoma following BNT162b2 mRNA vaccine booster shot: A case report. Front. Med. 2021, 8, 798095. [Google Scholar] [CrossRef]
- Herzum, A.; Trave, I.; D’Agostino, F.; Burlando, M.; Cozzani, E.; Parodi, A. Epstein-Barr virus reactivation after COVID-19 vaccination in a young immunocompetent man: A case report. Clin. Exp. Vaccine Res. 2022, 11, 222–225. [Google Scholar] [CrossRef]
- Vavoulidis, E.; Margioula-Siarkou, C.; Petousis, S.; Dinas, K. SARS-CoV-2 infection and impact on female genital tract: An untested hypothesis. Med. Hypotheses 2020, 144, 110162. [Google Scholar] [CrossRef] [PubMed]
- Hinten, F.; Hilbrands, L.B.; Meeuwis, K.A.P.; IntHout, J.; Quint, W.G.V.; Hoitsma, A.J.; Massuger, L.F.A.G.; Melchers, W.J.G.; de Hullu, J.A. Reactivation of latent HPV infections after renal transplantation. Am. J. Transplant. 2017, 17, 1563–1573. [Google Scholar] [CrossRef] [PubMed]
- Strickler, H.D.; Burk, R.D.; Fazzari, M.; Anastos, K.; Minkoff, H.; Massad, L.S.; Hall, C.; Bacon, M.; Levine, A.M.; Watts, D.H.; et al. Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus-positive women. J. Natl. Cancer Inst. 2005, 97, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Sri, T.; Merideth, M.A.; Pulanic, T.K.; Childs, R.; Stratton, P. Human papillomavirus reactivation following treatment of genital graft-versus-host disease. Transpl. Infect. Dis. 2013, 15, E148–E151. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.; Jonigk, D.; Luft, A.; Dübbel, L.; Werlein, C.; Malik, E.; Schild-Suhren, M. COVID-19 can lead to rapid progression of cervical intraepithelial neoplasia by dysregulating the immune system: A hypothesis. J. Reprod. Immunol. 2022, 154, 103763. [Google Scholar] [CrossRef]
| Name, Acronym & Synonym | Diseases | Latency | Transmission |
|---|---|---|---|
| HHV1 alias HSV1 (Herpes Simplex Virus 1) | Oral herpes | Neurons | Close contact |
| Genital herpes | (sensory) | (oral and sexual) | |
| Herpes keratitis | (ganglia) | ||
| HHV2 alias HSV2 (Herpes Simplex Virus 2) | Oral herpes | Neurons | Close contact |
| Genital herpes | (sensory) | (oral and sexual) | |
| Herpes keratitis | (ganglia) | ||
| Mollaret’s meningitis | |||
| HHV3 alias VZV (Varicella Zoster Virus) | Chickenpox | Neurons | Respiratory and |
| Shingles | (sensory) | close contact | |
| (ganglia) | (oral and sexual) | ||
| HHV4 alias EBV (Epstein–Barr Virus) | Infectious mononucleosis (IM) | B cells | Close contact, |
| Lymphoproliferative disorders | transfusions, | ||
| Inflammatory pseudotumor | tissue transplant | ||
| Nasopharyngeal carcinoma | and congenital | ||
| HHV5 alias CMV (Cytomegalovirus) | IM-like syndrome | Monocytes | Saliva, urine, |
| Retinitis | blood and milk | ||
| HHV6 (A & B) (Human Betaherpesvirus 6A & 6B) | Sixth disease (roseola infantum | T cells | Respiratory and |
| or exanthem subitum) | close contact | ||
| HHV7 (Human Betaherpesvirus 7) | IM-like syndrome | T cells | Respiratory and |
| Hepatitis | close contact | ||
| HHV8 alias KSHV (Kaposi’s Sarcoma Associated Herpesvirus) | Kaposi’s sarcoma | B cells | Close contact |
| Primary effusion lymphoma | (sexual) and | ||
| Multicentric Castleman’s disease | saliva (?) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roncati, L.; Sweidan, E.; Tchawa, C.; Gianotti, G.; Di Massa, G.; Siciliano, F.; Paolini, A. SARS-CoV-2 Induced Herpes Virus Reactivations and Related Implications in Oncohematology: When Lymphocytopenia Sets in and Immunosurveillance Drops Out. Microorganisms 2023, 11, 2223. https://doi.org/10.3390/microorganisms11092223
Roncati L, Sweidan E, Tchawa C, Gianotti G, Di Massa G, Siciliano F, Paolini A. SARS-CoV-2 Induced Herpes Virus Reactivations and Related Implications in Oncohematology: When Lymphocytopenia Sets in and Immunosurveillance Drops Out. Microorganisms. 2023; 11(9):2223. https://doi.org/10.3390/microorganisms11092223
Chicago/Turabian StyleRoncati, Luca, Elizabeth Sweidan, Cyrielle Tchawa, Greta Gianotti, Gianluca Di Massa, Flavia Siciliano, and Ambra Paolini. 2023. "SARS-CoV-2 Induced Herpes Virus Reactivations and Related Implications in Oncohematology: When Lymphocytopenia Sets in and Immunosurveillance Drops Out" Microorganisms 11, no. 9: 2223. https://doi.org/10.3390/microorganisms11092223
APA StyleRoncati, L., Sweidan, E., Tchawa, C., Gianotti, G., Di Massa, G., Siciliano, F., & Paolini, A. (2023). SARS-CoV-2 Induced Herpes Virus Reactivations and Related Implications in Oncohematology: When Lymphocytopenia Sets in and Immunosurveillance Drops Out. Microorganisms, 11(9), 2223. https://doi.org/10.3390/microorganisms11092223







