Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp.
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Isolates
2.2. Cefiderocol Susceptibility Testing
2.2.1. Broth Microdilution Reference Method (BMD)
2.2.2. Other Susceptibility Testing Methods
2.3. Data Analysis
3. Results
3.1. Broth Microdilution
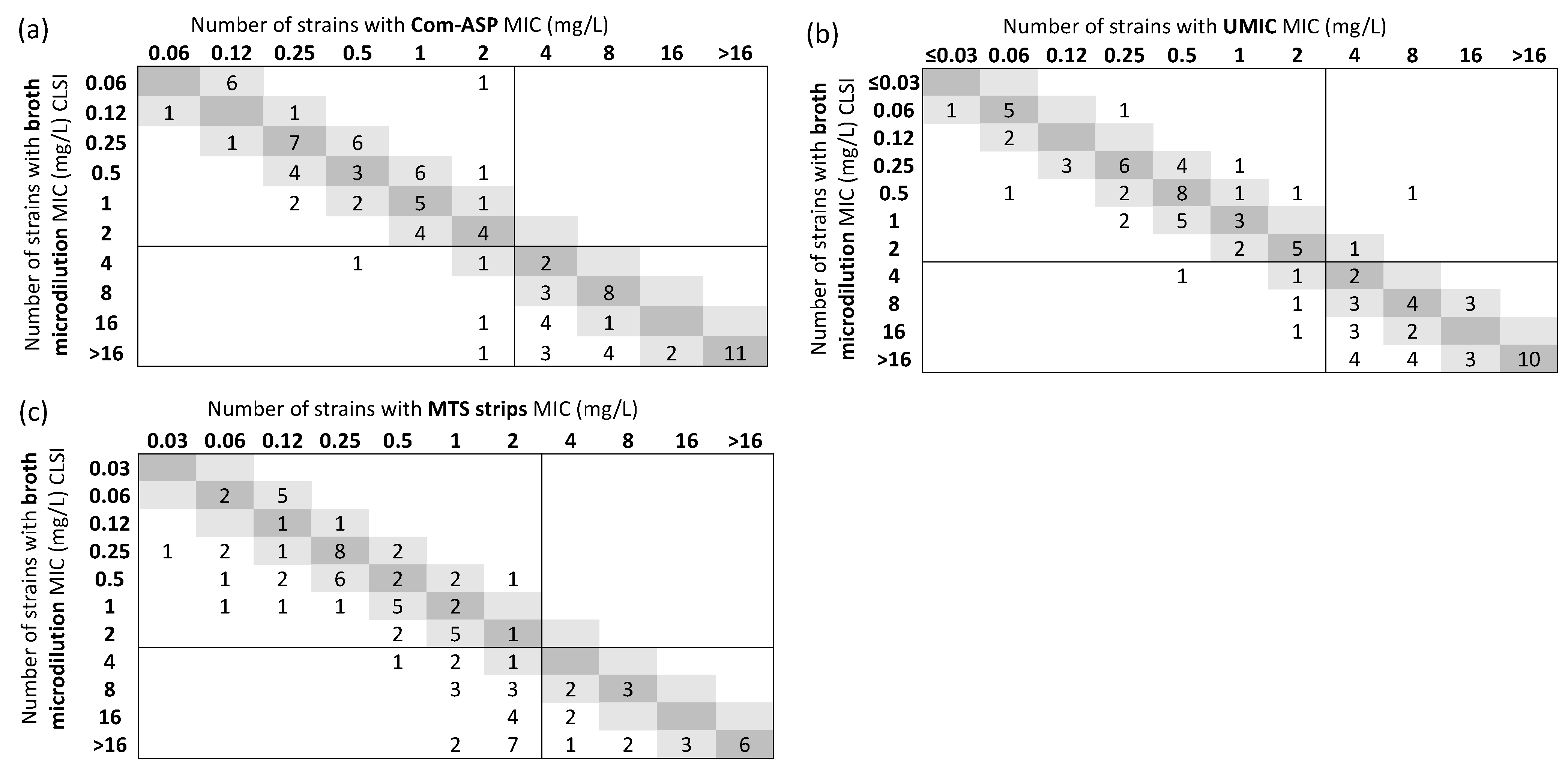
3.2. Gradient Strips
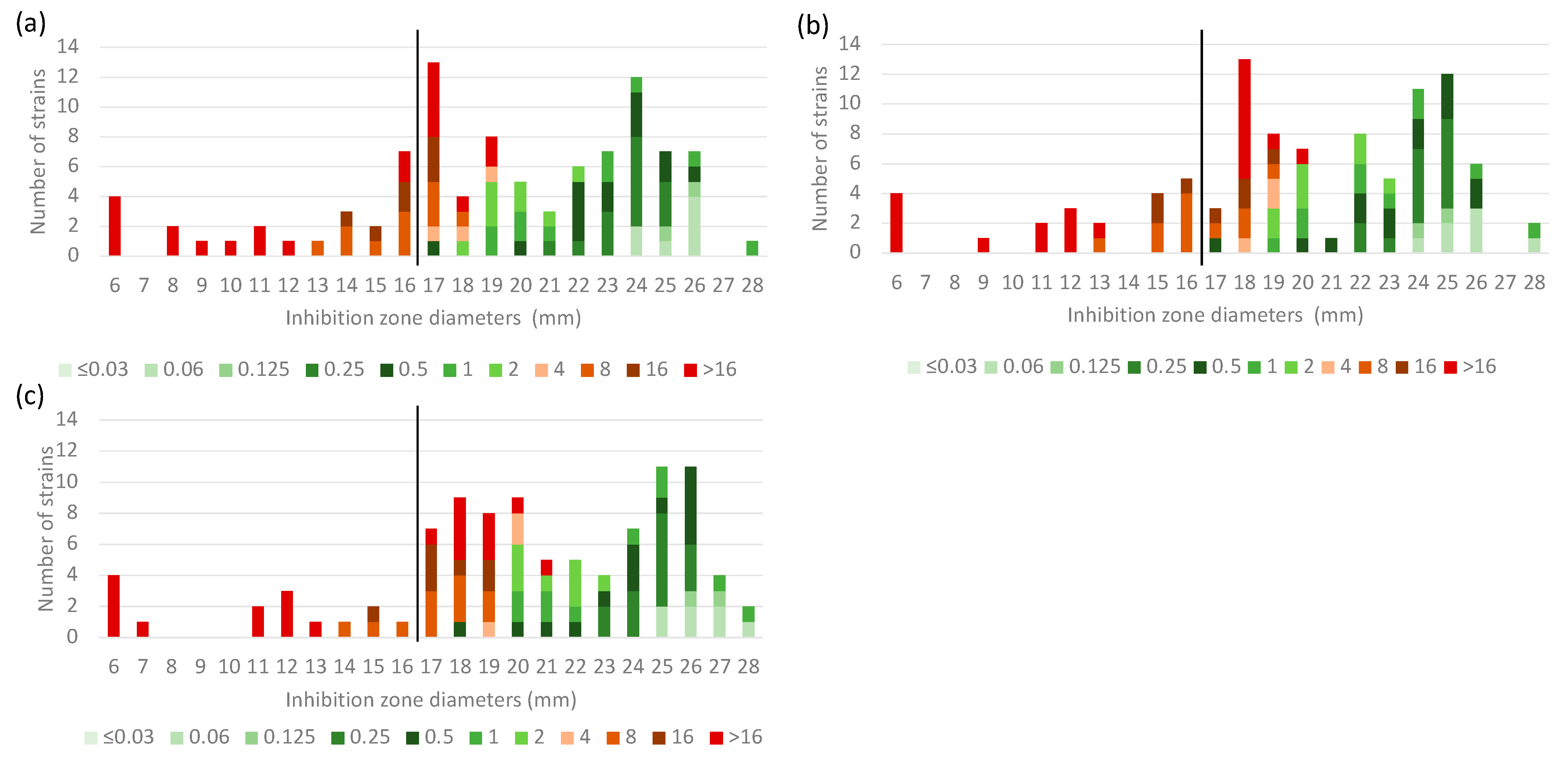
3.3. Disc Diffusion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Jiang, Y.; Ding, Y.; Wei, Y.; Jian, C.; Liu, J.; Zeng, Z. Carbapenem-resistant Acinetobacter baumannii: A challenge in the intensive care unit. Front. Microbiol. 2022, 13, 1045206. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and pathophysiological overview of Acinetobacter infections: A century of challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Candel, F.J.; Santerre Henriksen, A.; Longshaw, C.; Yamano, Y.; Oliver, A. In vitro activity of the novel siderophore cephalosporin, cefiderocol, in Gram-negative pathogens in Europe by site of infection. Clin. Microbiol. Infect. 2022, 28, 447.e1–447.e6. [Google Scholar] [CrossRef] [PubMed]
- Karlowsky, J.A.; Hackel, M.A.; Tsuji, M.; Yamano, Y.; Echols, R.; Sahm, D.F. In vitro activity of cefiderocol, a siderophore cephalosporin, against Gram-negative bacilli isolated by clinical laboratories in North America and Europe in 2015–2016: SIDERO-WT-2015. Int. J. Antimicrob. Agents 2019, 53, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Zhanel, G.G.; Golden, A.R.; Zelenitsky, S.; Wiebe, K.; Lawrence, C.K.; Adam, H.J.; Idowu, T.; Domalaon, R.; Schweizer, F.; Zhanel, M.A.; et al. Cefiderocol: A siderophore cephalosporin with activity against carbapenem-resistant and multidrug-resistant Gram-negative bacilli. Drugs 2019, 79, 271–289. [Google Scholar] [CrossRef] [PubMed]
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America guidance on the treatment of AmpC β-lactamase-producing Enterobacterales, carbapenem-resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia infections. Clin. Infect. Dis. 2022, 74, 2089–2114. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Carrara, E.; Retamar, P.; Tängdén, T.; Bitterman, R.; Bonomo, R.A.; de Waele, J.; Daikos, G.L.; Akova, M.; Harbarth, S.; et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused bymultidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin. Microbiol. Infect. 2022, 28, 521–547. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing. Cefiderocol MIC Testing—Guidance Document. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Guidance_documents/Cefiderocol_MIC_testing_EUCAST_guidance_document_201217.pdf (accessed on 2 July 2023).
- Devoos, L.; Biguenet, A.; Rousselot, J.; Bour, M.; Plésiat, P.; Fournier, D.; Jeannot, K. Performance of discs, sensititre EUMDROXF microplates and MTS gradient strips for the determination of the susceptibility of multidrug-resistant Pseudomonas aeruginosa to cefiderocol. Clin. Microbiol. Infect. 2023, 29, 652.e1–652.e8. [Google Scholar] [CrossRef] [PubMed]
- Bonnin, R.A.; Emeraud, C.; Jousset, A.B.; Naas, T.; Dortet, L. Comparison of disk diffusion, MIC test strip and broth microdilution methods for cefiderocol susceptibility testing on carbapenem-resistant Enterobacterales. Clin. Microbiol. Infect. 2022, 28, 1156.e1–1156.e5. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing. EUCAST Warnings. Available online: https://www.eucast.org/ast-of-bacteria/warnings (accessed on 12 June 2023).
- Simner, P.J.; Patel, R. Cefiderocol antimicrobial susceptibility testing considerations: The Achilles’ Heel of the Trojan Horse? J. Clin. Microbiol. 2020, 59, e00951-20. [Google Scholar] [CrossRef] [PubMed]
- Simner, P.J.; Palavecino, E.L.; Satlin, M.J.; Mathers, A.J.; Weinstein, M.P.; Lewis, J.S.; Humphries, R. Potential of inaccurate cefiderocol susceptibility results: A CLSI AST subcommittee advisory. J. Clin. Microbiol. 2023, 61, e0160022. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 13.0. 2023. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf (accessed on 12 May 2023).
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing M100 S, 33rd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2023. [Google Scholar]
- Matuschek, E.; Longshaw, C.; Takemura, M.; Yamano, Y.; Kahlmeter, G. Cefiderocol: EUCAST criteria for disc diffusion and broth microdilution for antimicrobial susceptibility testing. J. Antimicrob. Chemother. 2022, 77, 1662–1669. [Google Scholar] [CrossRef] [PubMed]
- Dortet, L.; Niccolai, C.; Pfennigwerth, N.; Frisch, S.; Gonzalez, C.; Antonelli, A.; Giani, T.; Hoenings, R.; Gatermann, S.; Rossolini, G.M.; et al. Performance evaluation of the UMIC® Cefiderocol to determine MIC in Gram-negative bacteria. J. Antimicrob. Chemother. 2023, 20, dkad149, epub ahead of print. [Google Scholar] [CrossRef]
- Poirel, L.; Sadek, M.; Nordmann, P. Contribution of PER-type and NDM-type β-Lactamases to cefiderocol resistance in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2021, 65, e0087721. [Google Scholar] [CrossRef]
- Kaye, K.S.; Naas, T.; Pogue, J.M.; Rossolini, G.M. Cefiderocol, a siderophore cephalosporin, as a treatment option for infections caused by carbapenem-resistant Enterobacterales. Infect. Dis. Ther. 2023, 12, 777–806. [Google Scholar] [CrossRef] [PubMed]
| Performances (%, [n]) | ||||||
| CA | EA | Bias high | Bias low | Difference of bias | ||
| Cefiderocol MIC determination | ||||||
| ComASP | 95.9 (93) | 81.4 (79) | +28.9% (22/76) | −36.1% (35/97) | −7.2% | |
| UMIC | 93.8 (91) | 78.4 (76) | +17.1% (13/76) | −42.3% (41/97) | −25.2% | |
| MTS strips | 76.3 (74) | 59.8 (58) | +14.5% (11/76) | −62.9% (61/97) | −48.4% | |
| Disc diffusion (cefiderocol, 30 μg) | ||||||
| MAST | 81.4 (79) | - | - | - | - | |
| Liofilchem | 78.4 (76) | - | - | - | - | |
| Oxoid | 72.2 (70) | - | - | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeannot, K.; Gaillot, S.; Triponney, P.; Portets, S.; Pourchet, V.; Fournier, D.; Potron, A. Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp. Microorganisms 2023, 11, 1971. https://doi.org/10.3390/microorganisms11081971
Jeannot K, Gaillot S, Triponney P, Portets S, Pourchet V, Fournier D, Potron A. Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp. Microorganisms. 2023; 11(8):1971. https://doi.org/10.3390/microorganisms11081971
Chicago/Turabian StyleJeannot, Katy, Susie Gaillot, Pauline Triponney, Sylvain Portets, Valentin Pourchet, Damien Fournier, and Anaïs Potron. 2023. "Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp." Microorganisms 11, no. 8: 1971. https://doi.org/10.3390/microorganisms11081971
APA StyleJeannot, K., Gaillot, S., Triponney, P., Portets, S., Pourchet, V., Fournier, D., & Potron, A. (2023). Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp. Microorganisms, 11(8), 1971. https://doi.org/10.3390/microorganisms11081971






