E7 Oncogene HPV58 Variants Detected in Northeast Brazil: Genetic and Functional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Groups and DNA Isolation
2.2. HPV Detection and Genotyping
2.3. Phylogenetic Analysis
2.4. Analysis of Selective Pressure
2.5. Protein Structure Modeling
2.6. T-Cell and B-Cell Epitope Prediction
2.7. Plasmid Constructs
2.8. Transfection of the C33A Cells with Recombinant Expression Vectors
2.9. Evaluation of the E7 Gene Expression in Transfected C33A Cells
2.10. Statistical Analysis
3. Results
3.1. HPV Detection and Typing
3.2. HPV58 E7 Sequence Variations
3.3. Phylogenetic Analysis
3.4. Selective Pressure Analysis
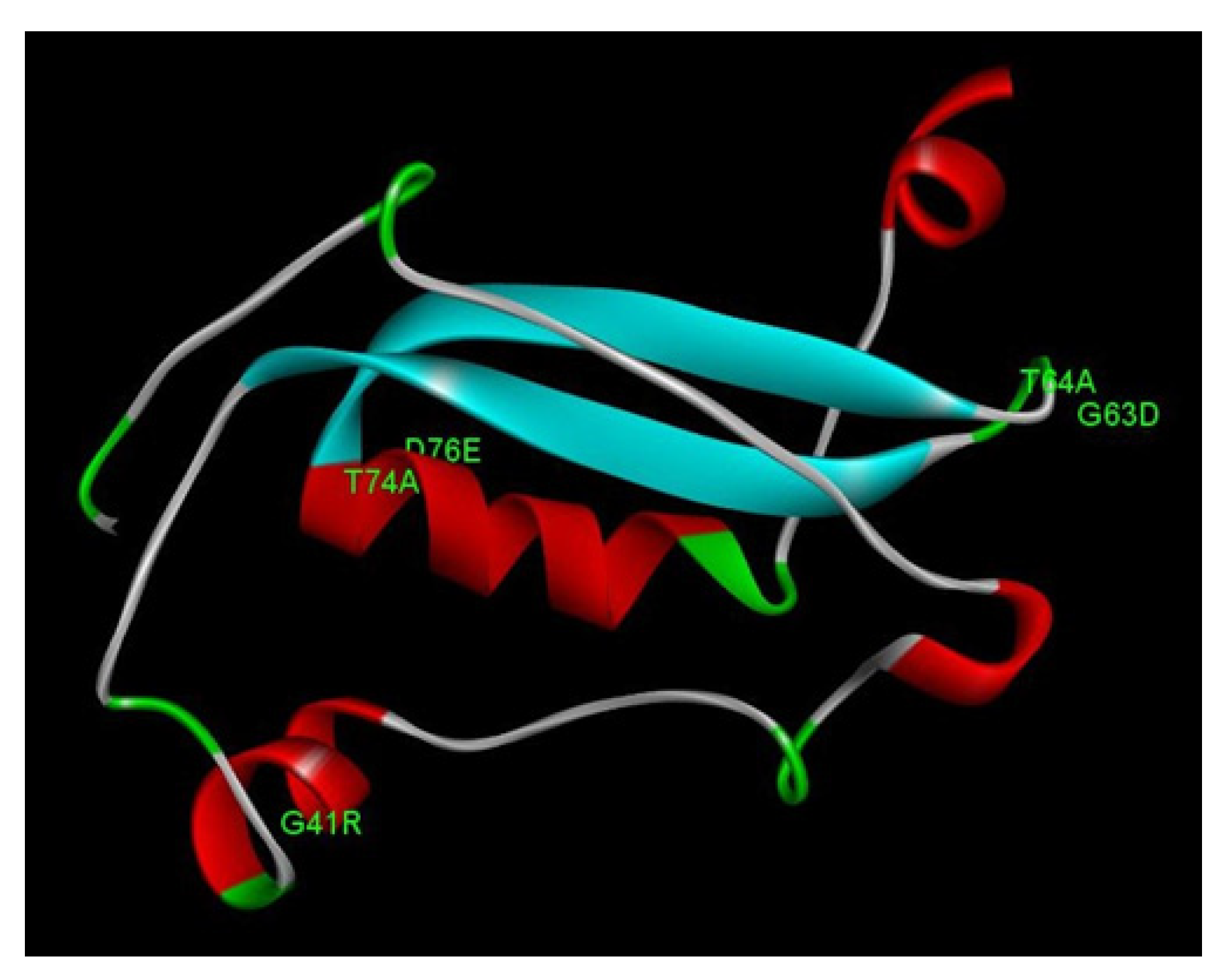
3.5. Structural Analysis of E7 Mutations
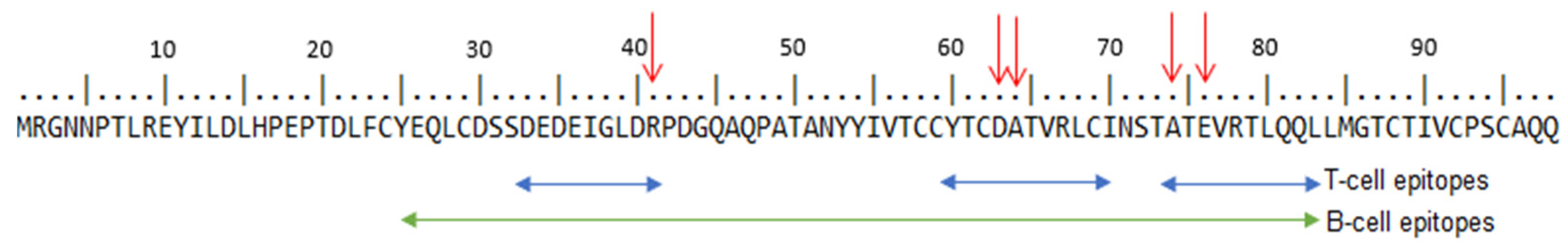
3.6. T-Cell and B-Cell Epitopes Prediction
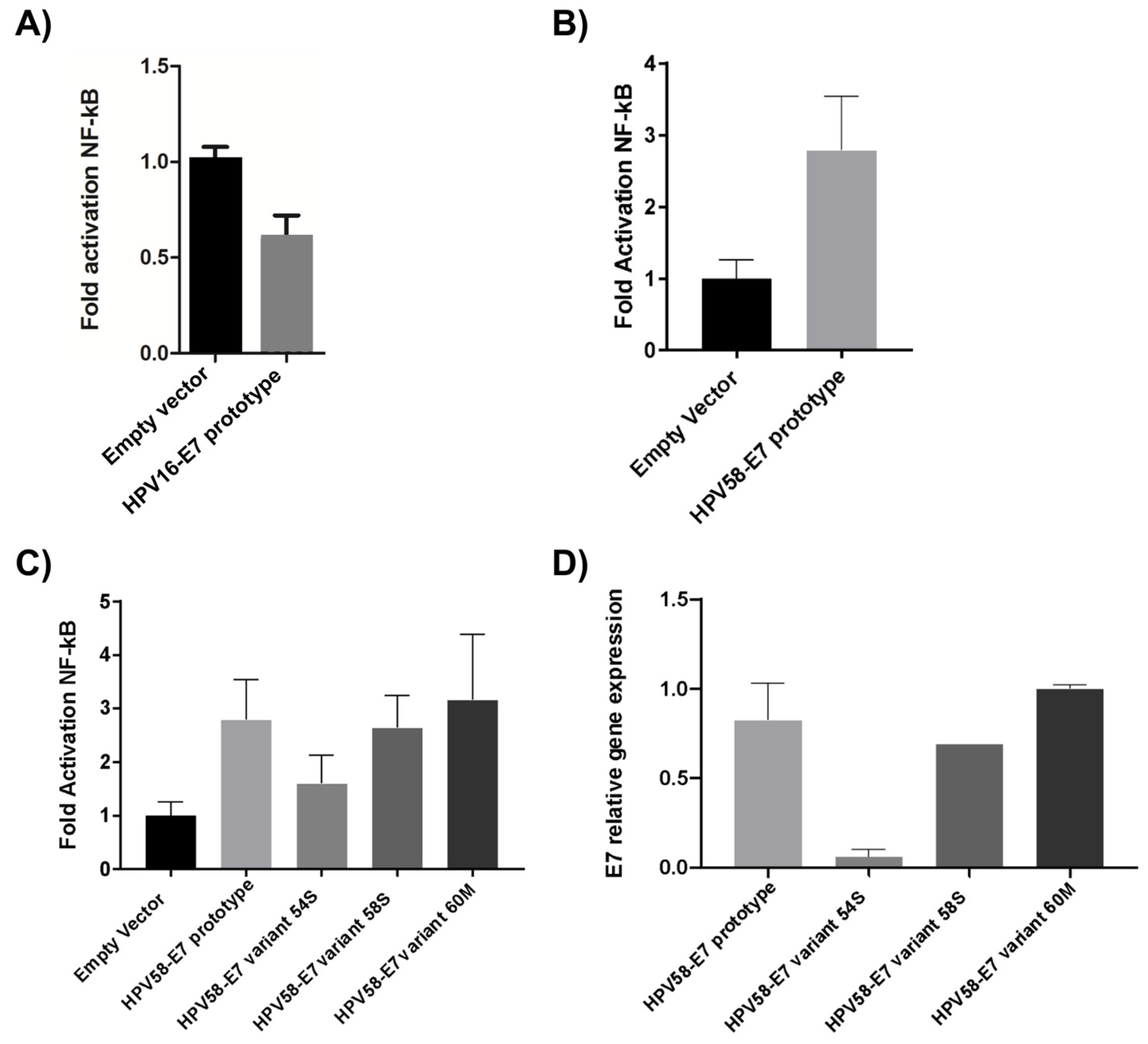
3.7. Effect of E7 Polymorphic Variants on the NF-kB Pathway
3.8. E7 Oncoprotein Gene Expression in C33A-Transfected Cells with HPV58 E7 Variants
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Zur, H.H. Papillomaviruses in the Causation of Human Cancers—A Brief Historical Account. Virology 2009, 384, 260–265. [Google Scholar] [CrossRef]
- Raiol, T.; Wyant, P.S.; De Amorim, R.M.S.; Cerqueira, D.M.; Milanezi, N.V.G.; Brígido, M.D.M.; Sichero, L.; Martins, C.R.F. Genetic Variability and Phylogeny of the High-Risk HPV-31, -33, -35, -52, and -58 in Central Brazil. J. Med. Virol. 2009, 81, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of Incidence and Mortality of Cervical Cancer in 2018: A Worldwide Analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Gurgel, A.P.A.D.; Chagas, B.S.; Do Amaral, C.M.; Nascimento, K.C.G.; Leal, L.R.S.; Silva Neto, J.D.C.; Cartaxo Muniz, M.T.; De Freitas, A.C. Prevalence of Human Papillomavirus Variants and Genetic Diversity in the L1 Gene and Long Control Region of HPV16, HPV31, and HPV58 Found in North-East Brazil. BioMed. Res. Int. 2015, 2015, 130828. [Google Scholar] [CrossRef]
- Fernandes, J.; Carvalho, M.; De Fernandes, T.; Araújo, J.; Azevedo, P.; Azevedo, J.; Meissner, R. Prevalence of Human Papillomavirus Type 58 in Women with or without Cervical Lesions in Northeast Brazil. Ann. Med. Health Sci. Res. 2013, 3, 504. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.K.S.; Zhang, C.; Park, J.-S.; Smith-McCune, K.K.; Palefsky, J.M.; Giovannelli, L.; Coutlée, F.; Hibbitts, S.; Konno, R.; Settheetham-Ishida, W.; et al. Geographical Distribution and Oncogenic Risk Association of Human Papillomavirus Type 58 E6 and E7 Sequence Variations. Int. J. Cancer 2013, 132, 2528–2536. [Google Scholar] [CrossRef]
- Chagas, B.S.; Batista, M.V.A.; Guimarães, V.; Balbino, V.Q.; Crovella, S.; Freitas, A.C. New Variants of E6 and E7 Oncogenes of Human Papillomavirus Type 31 Identified in Northeastern Brazil. Gynecol. Oncol. 2011, 123, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Boon, S.S.; Xia, C.; Lim, J.Y.; Chen, Z.; Law, P.T.Y.; Yeung, A.C.M.; Thomas, M.; Banks, L.; Chan, P.K.S. Human Papillomavirus 58 E7 T20I/G63S Variant Isolated from an East Asian Population Possesses High Oncogenicity. J. Virol. 2020, 94, e00090-20. [Google Scholar] [CrossRef] [PubMed]
- Xi, L.F.; Koutsky, L.A.; Hildesheim, A.; Galloway, D.A.; Wheeler, C.M.; Winer, R.L.; Ho, J.; Kiviat, N.B. Risk for High-Grade Cervical Intraepithelial Neoplasia Associated with Variants of Human Papillomavirus Types 16 and 18. Cancer Epidemiol. Biomark. Prev. 2007, 16, 4–10. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.A.; Peters, L.A.W.; Aziz, M.F.; Siregar, B.; Cornain, S.; Vrede, M.A.; Jordanova, E.S.; Fleuren, G.J. Human Papillomavirus Type 18 Variants: Histopathology and E6/E7 Polymorphisms in Three Countries. Int. J. Cancer 2005, 114, 422–425. [Google Scholar] [CrossRef] [PubMed]
- Law, P.T.; Boon, S.S.; Hu, C.; Lung, R.W.; Cheung, G.P.; Ho, W.C.; Chen, Z.; Massimi, P.; Thomas, M.; Pim, D.; et al. Oncogenic Comparison of Human Papillomavirus Type 58 E7 Variants. J. Cell. Mol. Med. 2019, 23, 1517–1527. [Google Scholar] [CrossRef] [PubMed]
- Ding, T.; Wang, X.; Ye, F.; Cheng, X.; Lu, W.; Xie, X. Distribution of Human Papillomavirus 16 E6/E7 Variants in Cervical Cancer and Intraepithelial Neoplasia in Chinese Women. Int. J. Gynecol. Cancer 2010, 20. [Google Scholar]
- He, J.; Yang, Y.; Chen, Z.; Liu, Y.; Bao, S.; Zhao, Y.; Ding, X. Identification of Variants and Therapeutic Epitopes in HPV-33/HPV-58 E6 and E7 in Southwest China. Virol. J. 2019, 16, 72. [Google Scholar] [CrossRef] [PubMed]
- Barros, M.R.; De Oliveira, T.H.A.; De Melo, C.M.L.; Venuti, A.; De Freitas, A.C. Viral Modulation of TLRs and Cytokines and the Related Immunotherapies for HPV-Associated Cancers. J. Immunol. Res. 2018, 2018, 2912671. [Google Scholar] [CrossRef]
- Barros, M.R.; De Melo, C.M.L.; Barros, M.L.C.M.G.; De Cássia Pereira De Lima, R.; De Freitas, A.C.; Venuti, A. Activities of Stromal and Immune Cells in HPV-Related Cancers. J. Exp. Clin. Cancer Res. 2018, 37, 137. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, A.C.; Gurgel, A.P.A.D.; Chagas, B.S.; Coimbra, E.C.; Do Amaral, C.M.M. Susceptibility to Cervical Cancer: An Overview. Gynecol. Oncol. 2012, 126, 304–311. [Google Scholar] [CrossRef]
- Ma, H.; Hu, Z.; Zhai, X.; Wang, S.; Wang, X.; Qin, J.; Jin, G.; Liu, J.; Wang, X.; Wei, Q.; et al. Polymorphisms in the MDM2 Promoter and Risk of Breast Cancer: A Case-Control Analysis in a Chinese Population. Cancer Lett. 2006, 240, 261–267. [Google Scholar] [CrossRef]
- Manos, M.M.; Ting, Y.; Wright, D.K.; Lewis, A.J.; Broker, T.R.; Wolinski, S.M. Use of Polymerase Chain Reaction Amplification for the Detection of Genital Human Papillomaviruses. Cancer Cells 1989, 7, 209–213. [Google Scholar]
- Staden, R. The Staden Sequence Analysis Package. Mol. Biotechnol. 1996, 5, 233–241. [Google Scholar] [CrossRef]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic Local Alignment Search Tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef]
- Tamura, K.; Stecher, G.; Kumar, S. MEGA11: Molecular Evolutionary Genetics Analysis Version 11. Mol. Biol. Evol. 2021, 38, 3022–3027. [Google Scholar] [CrossRef]
- Darriba, D.; Taboada, G.L.; Doallo, R.; Posada, D. JModelTest 2: More Models, New Heuristics and Parallel Computing. Nat. Methods 2012, 9, 772. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z. PAML 4: Phylogenetic Analysis by Maximum Likelihood. Mol. Biol. Evol. 2007, 24, 1586–1591. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z. Likelihood Ratio Tests for Detecting Positive Selection and Application to Primate Lysozyme Evolution. Mol. Biol. Evol. 1998, 15, 568–573. [Google Scholar] [CrossRef]
- Yang, Z.; Nielsen, R. Synonymous and Nonsynonymous Rate Variation in Nuclear Genes of Mammals. J. Mol. Evol. 1998, 46, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z. Complexity of the Simplest Phylogenetic Estimation Problem. Proc. R. Soc. Lond. B 2000, 267, 109–116. [Google Scholar] [CrossRef]
- Kim, D.E.; Chivian, D.; Baker, D. Protein Structure Prediction and Analysis Using the Robetta Server. Nucleic Acids Res. 2004, 32, W526–W531. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Nowotny, J.; Cao, R.; Cheng, J. 3Drefine: An Interactive Web Server for Efficient Protein Structure Refinement. Nucleic Acids Res. 2016, 44, W406–W409. [Google Scholar] [CrossRef]
- Laskowski, R.A.; MacArthur, M.W.; Moss, D.S.; Thornton, J.M. PROCHECK: A Program to Check the Stereochemical Quality of Protein Structures. J. Appl. Crystallogr. 1993, 26, 283–291. [Google Scholar] [CrossRef]
- Chen, V.B.; Arendall, W.B.; Headd, J.J.; Keedy, D.A.; Immormino, R.M.; Kapral, G.J.; Murray, L.W.; Richardson, J.S.; Richardson, D.C. MolProbity: All-Atom Structure Validation for Macromolecular Crystallography. Acta Crystallogr. D Biol. Crystallogr. 2010, 66, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Benkert, P.; Biasini, M.; Schwede, T. Toward the Estimation of the Absolute Quality of Individual Protein Structure Models. Bioinformatics 2011, 27, 343–350. [Google Scholar] [CrossRef]
- Zhang, Y. TM-Align: A Protein Structure Alignment Algorithm Based on the TM-Score. Nucleic Acids Res. 2005, 33, 2302–2309. [Google Scholar] [CrossRef] [PubMed]
- Lauck, F.; Smith, C.A.; Friedland, G.F.; Humphris, E.L.; Kortemme, T. RosettaBackrub—A Web Server for Flexible Backbone Protein Structure Modeling and Design. Nucleic Acids Res. 2010, 38, W569–W575. [Google Scholar] [CrossRef] [PubMed]
- Worth, C.L.; Preissner, R.; Blundell, T.L. SDM—A Server for Predicting Effects of Mutations on Protein Stability and Malfunction. Nucleic Acids Res. 2011, 39, W215–W222. [Google Scholar] [CrossRef]
- Singh, H.; Raghava, G.P.S. ProPred1: Prediction of Promiscuous MHC Class-I Bindingsites. Bioinformatics 2003, 19, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Raghava, G.P.S. ProPred: Prediction of HLA-DR Binding Sites. Bioinformatics 2001, 17, 1236–1237. [Google Scholar] [CrossRef]
- Saha, S.; Raghava, G.P.S. AlgPred: Prediction of Allergenic Proteins and Mapping of IgE Epitopes. Nucleic Acids Res. 2006, 34, W202–W209. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Roman, A.; Munger, K. The Papillomavirus E7 Proteins. Virology 2013, 445, 138–168. [Google Scholar] [CrossRef] [PubMed]
- Ramas, V.; Mirazo, S.; Bonilla, S.; Ruchansky, D.; Arbiza, J. Analysis of Human Papillomavirus 16 E6, E7 Genes and Long Control Region in Cervical Samples from Uruguayan Women. Gene 2018, 654, 103–109. [Google Scholar] [CrossRef]
- Yu, J.-H.; Shi, W.-W.; Zhou, M.-Y.; Liu, J.-M.; Han, Q.-Y.; Xu, H.-H. Genetic Variability and Oncogenic Risk Association of Human Papillomavirus Type 58 E6 and E7 Genes in Taizhou Area, China. Gene 2019, 686, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Molano, M.; Buitrago, O.; Moreno-Acosta, P.; Garland, S.; Morales, N.; Huertas, A.; Martinez, T.; Gamboa, O.; Tabrizi, S.; Cornall, A.; et al. Follow-up Study of HPV58 Variants in Women with Incident HPV58 Infection from a Colombian Cohort. Oncol. Lett. 2018, 16, 2511–2516. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Chen, J.; Xu, M.; Yang, H.; Wen, S.; Pan, Y.; Wang, X.; Ye, C.; Qiu, L.; Sun, Q. The Polymorphisms of LCR, E6, and E7 of HPV-58 Isolates in Yunnan, Southwest China. Virol. J. 2018, 15, 76. [Google Scholar] [CrossRef]
- Zhou, Z.; Yang, H.; Yang, L.; Yao, Y.; Dai, S.; Shi, L.; Li, C.; Yang, L.; Yan, Z.; Yao, Y. Human Papillomavirus Type 16 E6 and E7 Gene Variations Associated with Cervical Cancer in a Han Chinese Population. Infect. Genet. Evol. 2019, 73, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Conde-Ferraez, L.; Pacheco-Arjona, R.; Novelo Canul, C.; Gomez-Carballo, J.; Ramirez-Prado, J.H.; Ayora-Talavera, G.; González-Losa, M. del R. Genetic Variability in E6 and E7 Oncogenes from Human Papillomavirus Type 58 in Mexican Women. Intervirology 2017, 60, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Tenjimbayashi, Y.; Onuki, M.; Hirose, Y.; Mori, S.; Ishii, Y.; Takeuchi, T.; Tasaka, N.; Satoh, T.; Morisada, T.; Iwata, T.; et al. Whole-Genome Analysis of Human Papillomavirus Genotypes 52 and 58 Isolated from Japanese Women with Cervical Intraepithelial Neoplasia and Invasive Cervical Cancer. Infect. Agents Cancer 2017, 12, 44. [Google Scholar] [CrossRef]
- Berumen, J.; Ordonez, R.M.; Lazcano, E.; Salmeron, J.; Galvan, S.C.; Estrada, R.A.; Yunes, E.; Garcia-Carranca, A.; Gonzalez-Lira, G.; Madrigal-de La Campa, A. Asian-American Variants of Human Papillomavirus 16 and Risk for Cervical Cancer: A Case-Control Study. JNCI J. Natl. Cancer Inst. 2001, 93, 1325–1330. [Google Scholar] [CrossRef]
- Zuna, R.E.; Moore, W.E.; Shanesmith, R.P.; Dunn, S.T.; Wang, S.S.; Schiffman, M.; Blakey, G.L.; Teel, T. Association of HPV16 E6 Variants with Diagnostic Severity in Cervical Cytology Samples of 354 Women in a US Population. Int. J. Cancer 2009, 125, 2609–2613. [Google Scholar] [CrossRef]
- Cornet, I.; Gheit, T.; Iannacone, M.R.; Vignat, J.; Sylla, B.S.; Del Mistro, A.; Franceschi, S.; Tommasino, M.; Clifford, G.M. HPV16 Genetic Variation and the Development of Cervical Cancer Worldwide. Br. J. Cancer 2013, 108, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Burk, R.D.; Harari, A.; Chen, Z. Human Papillomavirus Genome Variants. Virology 2013, 445, 232–243. [Google Scholar] [CrossRef]
- Chan, P.K.S.; Luk, A.C.S.; Park, J.-S.; Smith-McCune, K.K.; Palefsky, J.M.; Konno, R.; Giovannelli, L.; Coutlée, F.; Hibbitts, S.; Chu, T.-Y.; et al. Identification of Human Papillomavirus Type 58 Lineages and the Distribution Worldwide. J. Infect. Dis. 2011, 203, 1565–1573. [Google Scholar] [CrossRef]
- Dearlove, B.; Lewitus, E.; Bai, H.; Li, Y.; Reeves, D.B.; Joyce, M.G.; Scott, P.T.; Amare, M.F.; Vasan, S.; Michael, N.L.; et al. A SARS-CoV-2 Vaccine Candidate Would Likely Match All Currently Circulating Variants. Proc. Natl. Acad. Sci. USA 2020, 117, 23652–23662. [Google Scholar] [CrossRef] [PubMed]
- Bao, E.L.; Cheng, A.N.; Sankaran, V.G. The Genetics of Human Hematopoiesis and Its Disruption in Disease. EMBO Mol. Med. 2019, 11, e10316. [Google Scholar] [CrossRef]
- Yang, Z.; Zhang, C.; Luo, P.; Ye, M.; Gong, Q.; Mei, B. Genetic Variability of E6 and E7 Genes of Human Papillomavirus Type 58 in Jingzhou, Hubei Province of Central China. Virol. J. 2022, 19, 71. [Google Scholar] [CrossRef]
- Hu, X.; Pang, T.; Guo, Z.; Pontén, J.; Nistér, M.; Bernard Afink, G. Oncogene Lineages of Human Papillomavirus Type 16 E6, E7 and E5 in Preinvasive and Invasive Cervical Squamous Cell Carcinoma: HPV16 Sequence Variations in Cervical Carcinoma. J. Pathol. 2001, 195, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, B.; Mandal, N.R.; Roy, S.; Sengupta, S. Characterization of Sequence Variations within HPV16 Isolates among Indian Women: Prediction of Causal Role of Rare Non-Synonymous Variations within Intact Isolates in Cervical Cancer Pathogenesis. Virology 2008, 377, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Makowsky, R.; Lhaki, P.; Wiener, H.W.; Bhatta, M.P.; Cullen, M.; Johnson, D.C.; Perry, R.T.; Lama, M.; Boland, J.F.; Yeager, M.; et al. Genomic Diversity and Phylogenetic Relationships of Human Papillomavirus 16 (HPV16) in Nepal. Infect. Genet. Evol. 2016, 46, 7–11. [Google Scholar] [CrossRef][Green Version]
- Silva, R.C.D.O.; Da Silva Júnior, A.H.P.; Gurgel, A.P.A.D.; Barros Junior, M.R.; Santos, D.L.; De Lima, R.D.C.P.; Batista, M.V.A.; Pena, L.J.; Chagas, B.S.; Freitas, A.C. Structural and Functional Impacts of E5 Genetic Variants of Human Papillomavirus Type 31. Virus Res. 2020, 290, 198143. [Google Scholar] [CrossRef]
- McLaughlin-Drubin, M.E.; Münger, K. Oncogenic Activities of Human Papillomaviruses. Virus Res. 2009, 143, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.A.; Azoitei, N.; Baumann, B.; Grünert, S.; Sommer, A.; Pehamberger, H.; Kraut, N.; Beug, H.; Wirth, T. NF-ΚB Is Essential for Epithelial-Mesenchymal Transition and Metastasis in a Model of Breast Cancer Progression. J. Clin. Investig. 2004, 114, 569–581. [Google Scholar] [CrossRef]
- Bodily, J.M.; Mehta, K.P.M.; Laimins, L.A. Human Papillomavirus E7 Enhances Hypoxia-Inducible Factor 1–Mediated Transcription by Inhibiting Binding of Histone Deacetylases. Cancer Res. 2011, 71, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Honegger, A.; Schilling, D.; Bastian, S.; Sponagel, J.; Kuryshev, V.; Sültmann, H.; Scheffner, M.; Hoppe-Seyler, K.; Hoppe-Seyler, F. Dependence of Intracellular and Exosomal MicroRNAs on Viral E6/E7 Oncogene Expression in HPV-Positive Tumor Cells. PLoS Pathog. 2015, 11, e1004712. [Google Scholar] [CrossRef]
- White, E.A.; Sowa, M.E.; Tan, M.J.A.; Jeudy, S.; Hayes, S.D.; Santha, S.; Münger, K.; Harper, J.W.; Howley, P.M. Systematic Identification of Interactions between Host Cell Proteins and E7 Oncoproteins from Diverse Human Papillomaviruses. Proc. Natl. Acad. Sci. USA 2012, 109, E260–E267. [Google Scholar] [CrossRef]
- Lou, H.; Boland, J.F.; Li, H.; Burk, R.; Yeager, M.; Anderson, S.K.; Wentzensen, N.; Schiffman, M.; Mirabello, L.; Dean, M. HPV16 E7 Nucleotide Variants Found in Cancer-Free Subjects Affect E7 Protein Expression and Transformation. Cancers 2022, 14, 4895. [Google Scholar] [CrossRef]
- Nunes, E.M.; Talpe-Nunes, V.; Sobrinho, J.S.; Ferreira, S.; Lino, V.D.S.; Termini, L.; Silva, G.Á.F.; Boccardo, E.; Villa, L.L.; Sichero, L. E6/E7 Functional Differences among Two Natural Human Papillomavirus 18 Variants in Human Keratinocytes. Viruses 2021, 13, 1114. [Google Scholar] [CrossRef] [PubMed]
- Vandermark, E.R.; Deluca, K.A.; Gardner, C.R.; Marker, D.F.; Schreiner, C.N.; Strickland, D.A.; Wilton, K.M.; Mondal, S.; Woodworth, C.D. Human Papillomavirus Type 16 E6 and E 7 Proteins Alter NF-KB in Cultured Cervical Epithelial Cells and Inhibition of NF-KB Promotes Cell Growth and Immortalization. Virology 2012, 425, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Spitkovsky, D.; Hehner, S.P.; Hofmann, T.G.; Möller, A.; Schmitz, M.L. The Human Papillomavirus Oncoprotein E7 Attenuates NF-ΚB Activation by Targeting the IκB Kinase Complex. J. Biol. Chem. 2002, 277, 25576–25582. [Google Scholar] [CrossRef] [PubMed]
- Byg, L.M.; Vidlund, J.; Vasiljevic, N.; Clausen, D.; Forslund, O.; Norrild, B. NF-ΚB Signalling Is Attenuated by the E7 Protein from Cutaneous Human Papillomaviruses. Virus Res. 2012, 169, 48–53. [Google Scholar] [CrossRef]
- Bicknell, A.A.; Ricci, E.P. When MRNA Translation Meets Decay. Biochem. Soc. Trans. 2017, 45, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Hanson, G.; Coller, J. Codon Optimality, Bias and Usage in Translation and MRNA Decay. Nat. Rev. Mol. Cell Biol. 2018, 19, 20–30. [Google Scholar] [CrossRef]
- Jia, L.; Mao, Y.; Ji, Q.; Dersh, D.; Yewdell, J.W.; Qian, S.-B. Decoding MRNA Translatability and Stability from the 5′ UTR. Nat. Struct. Mol. Biol. 2020, 27, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Tilborghs, S.; Corthouts, J.; Verhoeven, Y.; Arias, D.; Rolfo, C.; Trinh, X.B.; Van Dam, P.A. The Role of Nuclear Factor-Kappa B Signaling in Human Cervical Cancer. Crit. Rev. Oncol. Hematol. 2017, 120, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Schrank, T.P.; Prince, A.C.; Sathe, T.; Wang, X.; Liu, X.; Alzhanov, D.T.; Burtness, B.; Baldwin, A.S.; Yarbrough, W.G.; Issaeva, N. NF-ΚB over-Activation Portends Improved Outcomes in HPV-Associated Head and Neck Cancer. Oncotarget 2022, 13, 707–722. [Google Scholar] [CrossRef]
- Cai, H.; Yan, L.; Liu, N.; Xu, M.; Cai, H. IFI16 Promotes Cervical Cancer Progression by Upregulating PD-L1 in Immunomicroenvironment through STING-TBK1-NF-KB Pathway. Biomed. Pharmacother. 2020, 123, 109790. [Google Scholar] [CrossRef]

| E7 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nt | 694 | 744 | 756 | 761 | 763 | 793 | 798 | 801 | 840 | 852 |
| Reference | G | T | T | G | A | A | C | C | C | T |
| LSIL | ||||||||||
| HPV58-E7 58S | . | G | . | . | . | G | T | A | T | C |
| HPV58-E7 88S | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 60M | . | G | . | A | G | G | T | A | T | . |
| HPV58-E7 28M | A | G | . | A | . | . | . | . | . | . |
| HSIL | ||||||||||
| HPV58-E7 30S | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 31S | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 54S | A | G | C | A | . | . | . | . | . | . |
| HPV58-E7 59M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 1M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 45M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 79M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 92M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 28S | . | G | . | A | G | G | T | A | T | . |
| HPV58-E7 48S | A | G | . | A | . | . | . | . | . | . |
| Without lesion | ||||||||||
| HPV58-E7 29M | A | G | . | A | . | . | . | . | . | . |
| HPV58-E7 35P | A | G | . | A | . | . | . | . | . | . |
| Reference amino acid | G | G | T | T | D | |||||
| Amino acid position | 41 | 63 | 64 | 74 | 76 | |||||
| Amino acid changed | R | D | A | A | E | |||||
| Model 1 | Model 2 | LRT | Positively Selected Sites |
|---|---|---|---|
| M0 | M3 | 48.63069 | - |
| M1 | M2 | 31.954069 | 41G (0.979 *) 63G (1.000 **) 64T (0.826) 74T (0.976 *) 76D (0.997 **) |
| M1 | M3 | 31.954662 | 41G (0.997 **) 63G (1.000 **) 64T (0.893) 74T (0.997 **) 76D (1.000 **) |
| M7 | M8 | 32.308663 | 41G (0.987 *) 63G (1.000 **) 64T (0.857) 74T (0.985 *) 76D (0.999 **) |
| Protein | Mutation | Predicted ΔΔG | Outcome |
|---|---|---|---|
| E7 | G41R | −0.14 | Reduced stability |
| G63D | −2.48 | Reduced stability | |
| T64A | −0.12 | Reduced stability | |
| T74A | 1.26 | Increased stability | |
| D76E | 1.25 | Increased stability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chagas, B.S.; Tibúrcio Júnior, E.; Silva, R.C.d.O.; Santos, D.L.d.; Barros Junior, M.R.; Lima, R.d.C.P.d.; Invenção, M.d.C.V.; Santos, V.E.P.; França Neto, P.L.; Silva Júnior, A.H.; et al. E7 Oncogene HPV58 Variants Detected in Northeast Brazil: Genetic and Functional Analysis. Microorganisms 2023, 11, 1915. https://doi.org/10.3390/microorganisms11081915
Chagas BS, Tibúrcio Júnior E, Silva RCdO, Santos DLd, Barros Junior MR, Lima RdCPd, Invenção MdCV, Santos VEP, França Neto PL, Silva Júnior AH, et al. E7 Oncogene HPV58 Variants Detected in Northeast Brazil: Genetic and Functional Analysis. Microorganisms. 2023; 11(8):1915. https://doi.org/10.3390/microorganisms11081915
Chicago/Turabian StyleChagas, Bárbara Simas, Elias Tibúrcio Júnior, Ruany Cristyne de Oliveira Silva, Daffany Luana dos Santos, Marconi Rego Barros Junior, Rita de Cássia Pereira de Lima, Maria da Conceição Viana Invenção, Vanessa Emanuelle Pereira Santos, Pedro Luiz França Neto, Antônio Humberto Silva Júnior, and et al. 2023. "E7 Oncogene HPV58 Variants Detected in Northeast Brazil: Genetic and Functional Analysis" Microorganisms 11, no. 8: 1915. https://doi.org/10.3390/microorganisms11081915
APA StyleChagas, B. S., Tibúrcio Júnior, E., Silva, R. C. d. O., Santos, D. L. d., Barros Junior, M. R., Lima, R. d. C. P. d., Invenção, M. d. C. V., Santos, V. E. P., França Neto, P. L., Silva Júnior, A. H., Silva Neto, J. C., Batista, M. V. d. A., & Freitas, A. C. d. (2023). E7 Oncogene HPV58 Variants Detected in Northeast Brazil: Genetic and Functional Analysis. Microorganisms, 11(8), 1915. https://doi.org/10.3390/microorganisms11081915










