Evaluation of the Effectiveness and Use of Anti-Methicillin-Resistant Staphylococcus aureus Agents for Aspiration Pneumonia in Older Patients Using a Nationwide Japanese Administrative Database
Abstract
1. Introduction
2. Materials and Methods
2.1. Database
2.2. Patient Consent Statement
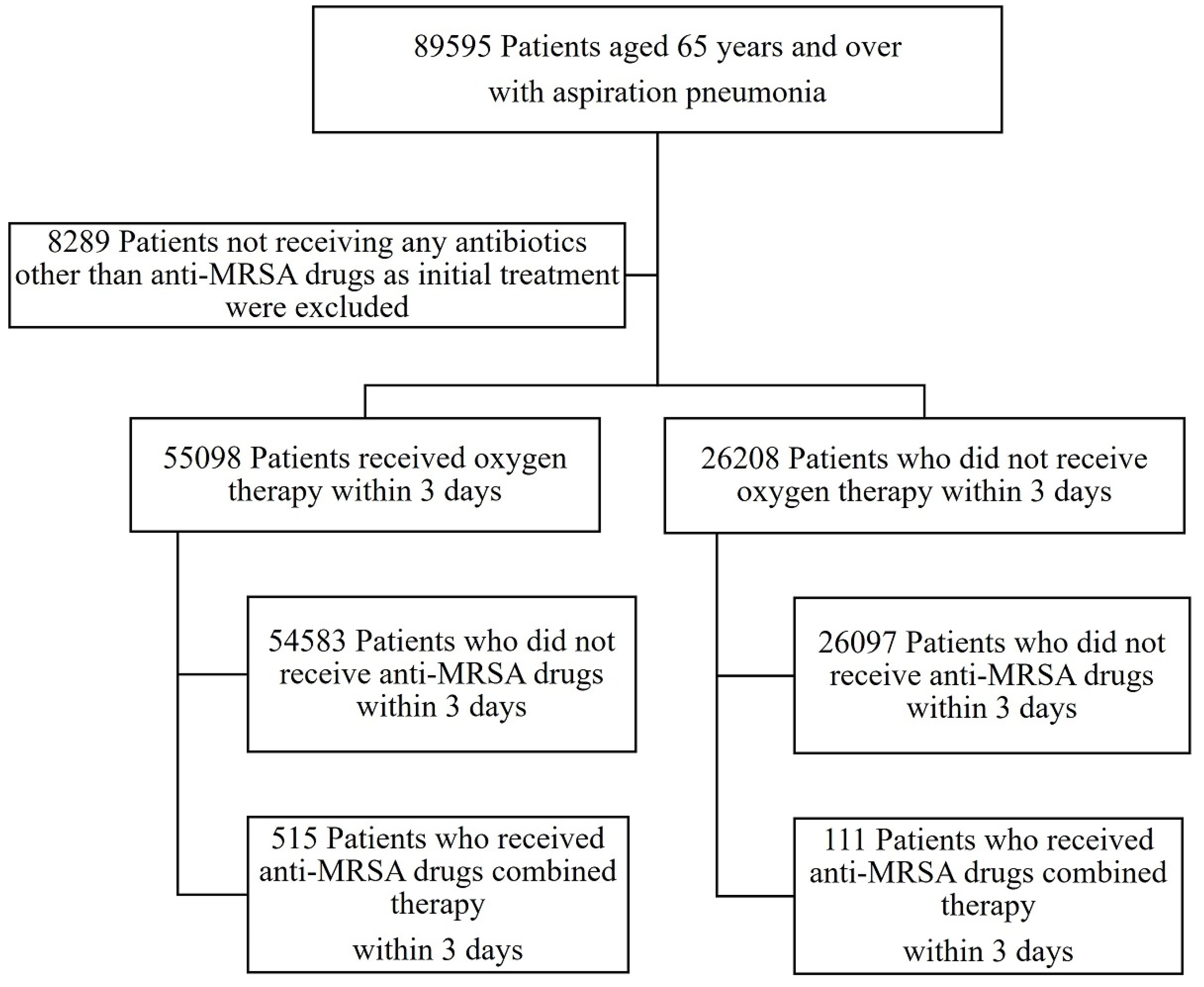
2.3. Patient Selection
2.4. Variables
2.5. Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Yokoyama, T. National Health Promotion Measures in Japan. Health Japan 21 (the second term). J. Natl. Inst. Public Health 2020, 69, 14–24. [Google Scholar]
- Leading Causes of Death, UK: 2001 to 2008. Office for National Statistics. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/articles/leadingcausesofdeathuk/2001to2018 (accessed on 10 January 2023).
- Teramoto, S.; Fukuchi, Y.; Sasaki, H.; Sato, K.; Sekizawa, K.; Matsuse, T.; Japanese Study Group on Aspiration Pulmonary Disease. High Incidence of Aspiration Pneumonia in Community- and Hospital-Acquired Pneumonia in Hospitalized Patients: A Multicenter, Prospective Study in Japan. J. Am. Geriatr. Soc. 2008, 56, 577–579. [Google Scholar] [PubMed]
- Gupte, T.; Knack, A.; Cramer, J.D. Mortality from Aspiration Pneumonia: Incidence, Trends, and Risk Factors. Dysphagia 2022, 37, 1493–1500. [Google Scholar] [CrossRef]
- JoJones, B.E.; Ying, J.; Stevens, V.; Haroldsen, C.; He, T.; Nevers, M.; Christensen, M.A.; Nelson, R.E.; Stoddard, G.J.; Saue, B.C.; et al. Empirical Anti-MRSA vs Standard Antibiotic Therapy and Risk of 30-Day Mortality in Patients Hospitalized for Pneumonia. JAMA Intern. Med. 2020, 180, 552–560. [Google Scholar] [CrossRef] [PubMed]
- The Japanese Respiratory Society. The JRS Guidelines for the Management of Pneumonia in Adults 2017. Jpn. Respir. Soc. 2017, 1, 9–48. (In Japanese) [Google Scholar]
- MMetlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-Acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- Kawanami, T.; Yatera, K.; Yamasaki, K.; Noguchi, S.; Fukuda, K.; Akata, K.; Naito, K.; Kido, T.; Ishimoto, H.; Taniguchi, H.; et al. Clinical Impact of Methicillin-Resistant Staphylococcus Aureus on Bacterial Pneumonia: Cultivation and 16S Ribosomal RNA Gene Analysis of Bronchoalveolar Lavage Fluid. BMC Infect. Dis. 2016, 16, 155. [Google Scholar] [CrossRef]
- Leroy, O.; Jaffreé, S.; d’Escrivan, T.; Devos, P.; Georges, H.; Alfandari, S.; Beaucaire, G. Hospital-Acquired Pneumonia: Risk Factors for Antimicrobial-Resistant Causative Pathogens in Critically Ill Patients. Chest 2003, 123, 2034–2042. [Google Scholar] [CrossRef]
- Khadka, S.; Khan, S.; King, A.; Goldberg, L.R.; Crocombe, L.; Bettiol, S. Poor Oral Hygiene, Oral Microorganisms and Aspiration Pneumonia Risk in Older People in Residential Aged Care: A Systematic Review. Age Ageing 2021, 50, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Iwagami, M.; Yasunaga, H.; Doi, K.; Horiguchi, H.; Fushimi, K.; Matsubara, T.; Yahagi, N.; Noiri, E. Postoperative Polymyxin B Hemoperfusion and Mortality in Patients with Abdominal Septic Shock: A Propensity-Matched Analysis. Crit. Care Med. 2014, 42, 1187–1193. [Google Scholar] [CrossRef]
- Hayashida, K.; Murakami, G.; Matsuda, S.; Fushimi, K. History and Profile of Diagnosis Procedure Combination (DPC): Development of a Real Data Collection System for Acute Inpatient Care in Japan. J. Epidemiol. 2021, 31, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kido, T.; Muramatsu, K.; Yatera, K.; Asakawa, T.; Otsubo, H.; Kubo, T.; Fujino, Y.; Matsuda, S.; Mayumi, T.; Mukae, H. Efficacy of Early Sivelestat Administration on Acute Lung Injury and Acute Respiratory Distress Syndrome. Respirology 2017, 22, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Horita, N.; Hashimoto, S.; Miyazawa, N.; Fujita, H.; Kojima, R.; Inoue, M.; Ueda, A.; Ishigatsubo, Y.; Kaneko, T. Impact of Corticosteroids on Mortality in Patients with Acute Respiratory Distress Syndrome: A Systematic Review and Meta-analysis. Intern. Med. 2015, 54, 1473–1479. [Google Scholar] [CrossRef] [PubMed]
- Van Hal, S.J.; Paterson, D.L.; Lodise, T.P. Systematic Review and Meta-analysis of Vancomycin-Induced Nephrotoxicity Associated with Dosing Schedules That Maintain Troughs between 15 and 20 Milligrams per Liter. Antimicrob. Agents Chemother. 2013, 57, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Niederman, M.S.; Kollef, M.H.; Shorr, A.F.; Kunkel, M.J.; Baruch, A.; McGee, W.T.; Reisman, A.; Chastre, J. Linezolid in Methicillin-Resistant Staphylococcus Aureus Nosocomial Pneumonia: A Randomized, Controlled Study. Clin. Infect. Dis. 2012, 54, 621–629. [Google Scholar] [CrossRef]
- Liu, X.; Aoki, M.; Osa, S.; Ito, C.; Saiki, R.; Nagai, T.; Enoki, Y.; Taguchi, K.; Matsumoto, K. Safety of linezolid in patients with decreased renal function and trough monitoring: A systematic review and meta-analysis. BMC Pharmacol. Toxicol. 2022, 23, 89. [Google Scholar] [CrossRef]
- Matsumoto, K.; Takeda, Y.; Takeshita, A.; Fukunaga, N.; Shigemi, A.; Yaji, K.; Shimodozono, Y.; Yamada, K.; Ikawa, K.; Morikawa, N. Renal function as a predictor of linezolid-induced thrombocytopenia. Int. J. Antimicrob. Agents 2009, 33, 98–99. [Google Scholar] [CrossRef]
- Webb, B.J.; Sorensen, J.; Jephson, A.; Mecham, I.; Dean, N.C. Broad-Spectrum Antibiotic Use and Poor Outcomes in Community-Onset Pneumonia: A Cohort Study. Eur. Respir. J. 2019, 54, 1900057. [Google Scholar] [CrossRef]
- Komiya, K.; Ishii, H.; Kadota, J. Healthcare-Associated Pneumonia and Aspiration Pneumonia. Aging Dis. 2015, 6, 27–37. [Google Scholar] [CrossRef]
- David, M.Z.; Daum, R.S. Community-associated methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 2010, 23, 616–687. [Google Scholar] [CrossRef]
- King, M.D.; Humphrey, B.J.; Wang, Y.F.; Kourbatova, E.V.; Ray, S.M.; Blumberg, H.M. Emergence of Community-Acquired Methicillin-Resistant Staphylococcus aureus USA 300 Clone as the Predominant Cause of Skin and Soft-Tissue Infections. Ann. Intern. Med. 2006, 144, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Funaki, T.; Yasuhara, T.; Kugawa, S.; Yamazaki, Y.; Sugano, E.; Nagakura, Y.; Yoshida, K.; Fukuchi, K. SCCmec Typing of PVL-Positive Community-Acquired Staphylococcus aureus (CA-MRSA) at a Japanese Hospital. Heliyon 2019, 5, e01415. [Google Scholar] [CrossRef] [PubMed]
- Yasunaga, H.; Hashimoto, H.; Horiguchi, H.; Miyata, H.; Matsuda, S. Variation in Cancer Surgical Outcomes Associated with Physician and Nurse Staffing: A Retrospective Observational Study Using the Japanese Diagnosis Procedure Combination Database. BMC Health Serv. Res. 2012, 12, 129. [Google Scholar]
- Chikuda, H.; Yasunaga, H.; Takeshita, K.; Horiguchi, H.; Kawaguchi, H.; Ohe, K.; Fushimi, K.; Tanaka, S. Mortality and Morbidity after High-Dose Methylprednisolone Treatment in Patients with Acute Cervical Spinal Cord Injury: A Propensity-Matched Analysis Using a Nationwide Administrative Database. Emerg. Med. J. 2014, 31, 201–206. [Google Scholar]
- Hamada, T.; Yasunaga, H.; Nakai, Y.; Isayama, H.; Horiguchi, H.; Matsuda, S.; Fushimi, K.; Koike, K. Continuous Regional Arterial Infusion for Acute Pancreatitis: A Propensity Score Analysis Using a Nationwide Administrative Database. Crit. Care 2013, 17, R214. [Google Scholar]
- Webb, B.J.; Dascomb, K.; Stenehjem, E.; Dean, N. Predicting risk of drug-resistant organisms in pneumonia: Moving beyond the HCAP model. Respir. Med. 2015, 109, 1–10. [Google Scholar]
- Aliberti, S.; Reyes, L.F.; Faverio, P.; Sotgiu, G.; Dore, S.; Rodriguez, A.H.; Soni, N.J.; Restrepo, M.I.; on behalf of the GLIMP investigators and Eva Van Braeckel (UGent). Global initiative for meticillinmethicillin-resistant Staphylococcus aureus pneumonia (GLIMP): An international, observational cohort study. Lancet Infect. Dis. 2016, 16, 1364–1376. [Google Scholar] [CrossRef]
| (a) | |||
| Outcomes | Anti-MRSA Agents Group | Non-Anti-MRSA Agents | p-Value |
| In-hospital mortality (%) | 31.38 | 19.96 | <0.001 |
| 30-day mortality (%) | 22.52 | 14.11 | <0.001 |
| 90-day mortality (%) | 29.97 | 19.03 | <0.001 |
| Hospital stay, mean days (SE) | 29.66 (1.80) | 27.74 (0.289) | 0.289 |
| Oxygen administration, mean days (SE) | 11.41 (0.81) | 9.69 (0.06) | 0.035 |
| ICU admission, mean days (SE) | 0.06 (0.01) | 0.07 (0.003) | 0.13 |
| (b) | |||
| Outcomes | Anti-MRSA Agents Group | Non-Anti-MRSA Agents | p-Value |
| In hospital mortality (%) | 14.70 | 9.07 | 0.315 |
| 30-day mortality (%) | 12.62 | 4.3 | 0.129 |
| 90-day mortality (%) | 14.70 | 8.10 | 0.238 |
| Hospital stay, mean days (SE) | 27.60 (2.08) | 26.19 (0.498) | 0.498 |
| ICU admission, mean days (SE) | 0.79 (0.004) | 1.89 (0.002) | 0.420 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koga, S.; Takazono, T.; Kido, T.; Muramatsu, K.; Tokutsu, K.; Tokito, T.; Okuno, D.; Ito, Y.; Yura, H.; Takeda, K.; et al. Evaluation of the Effectiveness and Use of Anti-Methicillin-Resistant Staphylococcus aureus Agents for Aspiration Pneumonia in Older Patients Using a Nationwide Japanese Administrative Database. Microorganisms 2023, 11, 1905. https://doi.org/10.3390/microorganisms11081905
Koga S, Takazono T, Kido T, Muramatsu K, Tokutsu K, Tokito T, Okuno D, Ito Y, Yura H, Takeda K, et al. Evaluation of the Effectiveness and Use of Anti-Methicillin-Resistant Staphylococcus aureus Agents for Aspiration Pneumonia in Older Patients Using a Nationwide Japanese Administrative Database. Microorganisms. 2023; 11(8):1905. https://doi.org/10.3390/microorganisms11081905
Chicago/Turabian StyleKoga, Satoru, Takahiro Takazono, Takashi Kido, Keiji Muramatsu, Kei Tokutsu, Takatomo Tokito, Daisuke Okuno, Yuya Ito, Hirokazu Yura, Kazuaki Takeda, and et al. 2023. "Evaluation of the Effectiveness and Use of Anti-Methicillin-Resistant Staphylococcus aureus Agents for Aspiration Pneumonia in Older Patients Using a Nationwide Japanese Administrative Database" Microorganisms 11, no. 8: 1905. https://doi.org/10.3390/microorganisms11081905
APA StyleKoga, S., Takazono, T., Kido, T., Muramatsu, K., Tokutsu, K., Tokito, T., Okuno, D., Ito, Y., Yura, H., Takeda, K., Iwanaga, N., Ishimoto, H., Sakamoto, N., Yatera, K., Izumikawa, K., Yanagihara, K., Fujino, Y., Fushimi, K., Matsuda, S., & Mukae, H. (2023). Evaluation of the Effectiveness and Use of Anti-Methicillin-Resistant Staphylococcus aureus Agents for Aspiration Pneumonia in Older Patients Using a Nationwide Japanese Administrative Database. Microorganisms, 11(8), 1905. https://doi.org/10.3390/microorganisms11081905






