The Impact of Earthquakes on Public Health: A Narrative Review of Infectious Diseases in the Post-Disaster Period Aiming to Disaster Risk Reduction
Abstract
1. Introduction
2. Search Strategy
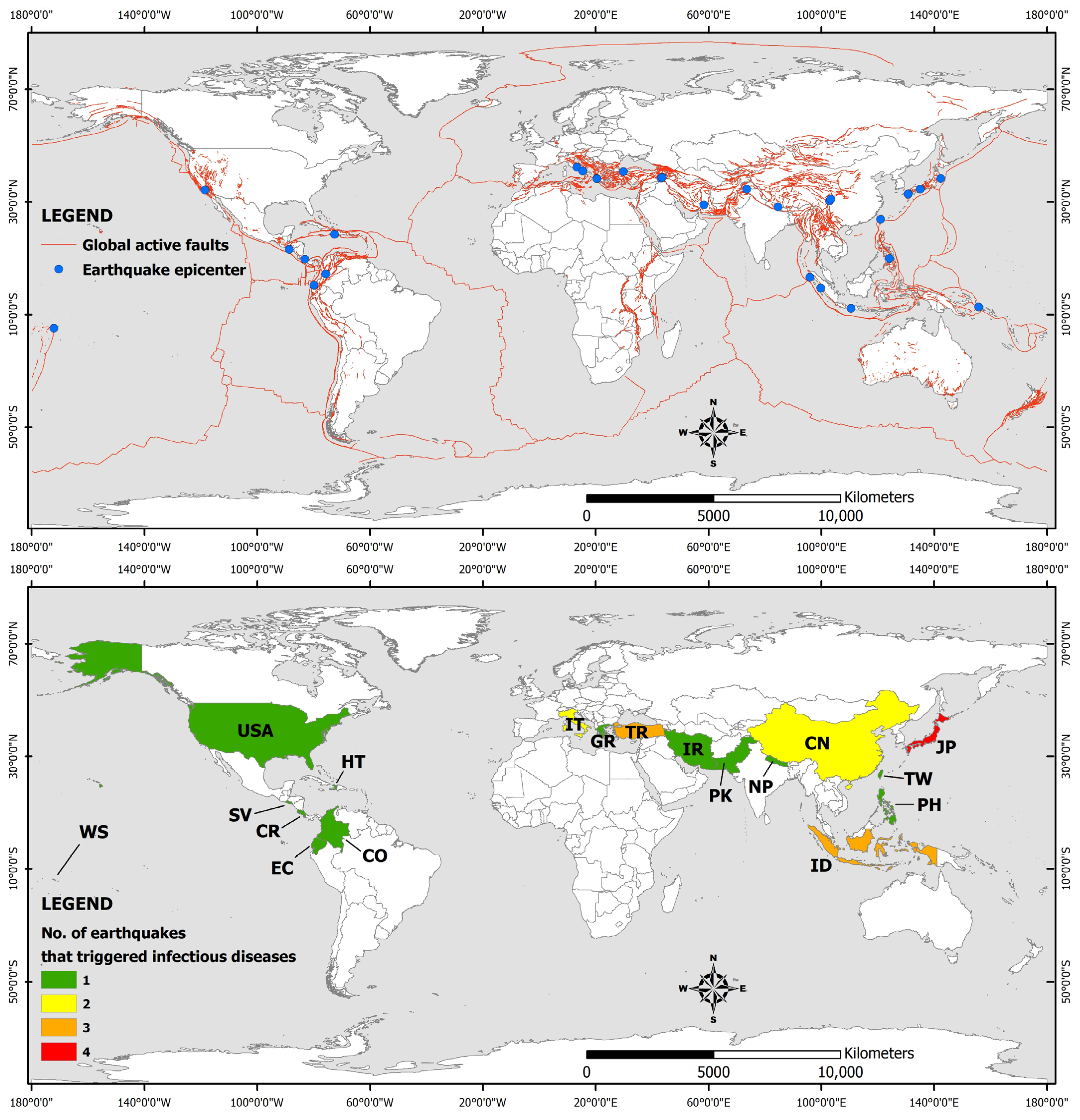
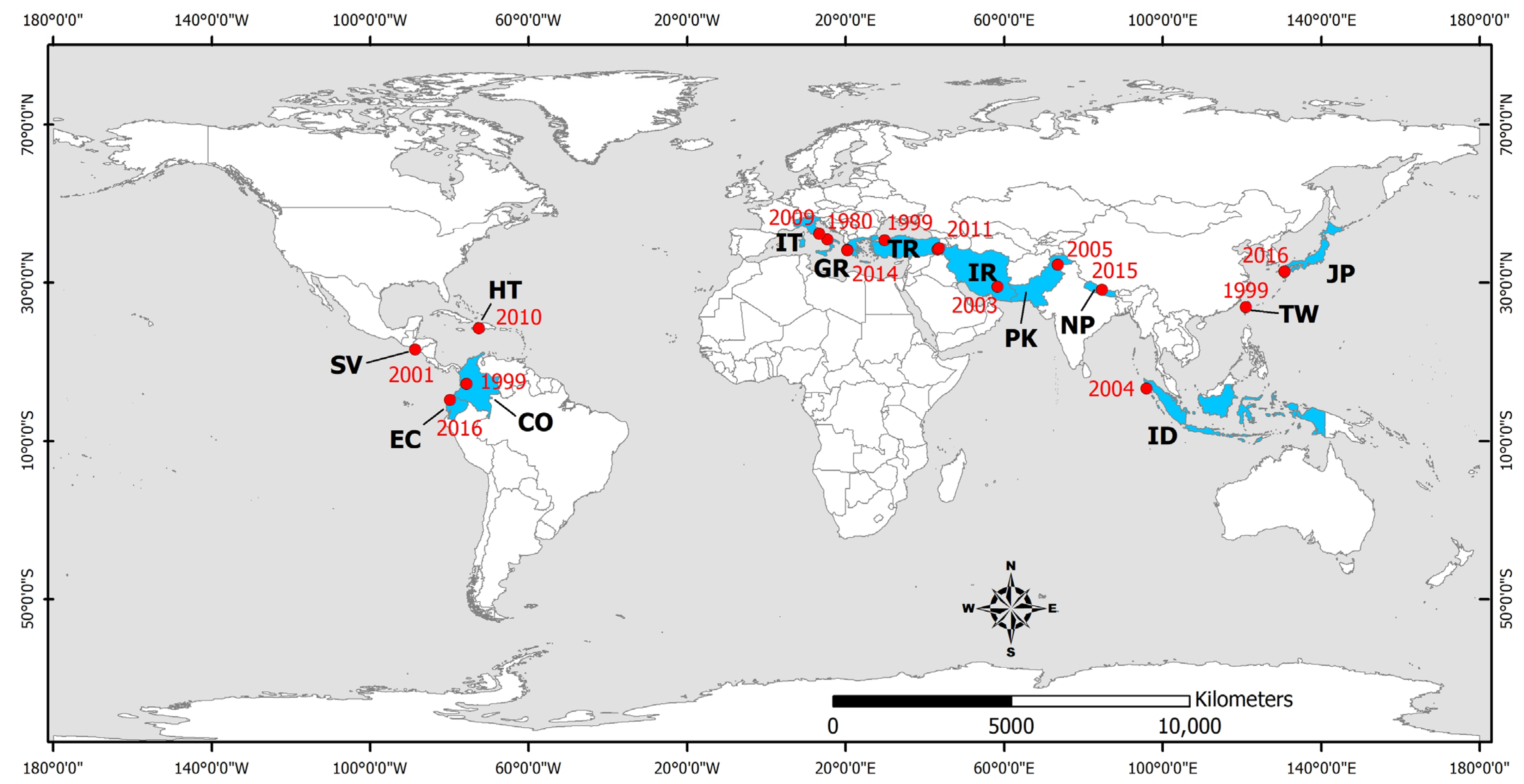
3. Spatial Distribution and Parameters of Earthquakes Associated with Infectious Diseases during Post-Disaster Period
| No | Earthquake Occurrence (Date/Month/Year) | Epicentral Area | Affected Areas | Mw | I | HL | IP | TA |
|---|---|---|---|---|---|---|---|---|
| 1 | 23/11/1980 | Irpinia, (Italy) | Campania, Naples, Salerno | 6.9 | X | 4689 | 7700 | 407,700 |
| 2 | 22/04/1991 | Limon, (Costa Rica) | Costa Rica, Panama | 7.7 | X | 47 | 199 | 10,419 |
| 3 | 17/01/1994 | Northridge (California United States) | Greater Los Angeles area, Southern California | 6.7 | IX | 60 | 7000 | 27,000 |
| 4 | 17/01/1995 | Kobe (Japan) | Japan | 6.9 | XI | 5297 | 34,492 | 541,636 |
| 5 | 25/01/1999 | Armenia (Colombia) | Armenia, Pereira | 6.2 | X | 1186 | 8563 | 1,205,933 |
| 6 | 17/08/1999 | Izmit (Turkey) | Marmara area, Adapazari, Gölcük, Izmit and Yalova | 7.6 | X | 17,127 | 43,953 | 1,358,953 |
| 7 | 21/09/1999 | Chi-Chi (Taiwan) | central Taiwan Nantou County Taichung County | 7.7 | X | 2264 | 8664 | 108,664 |
| 8 | 13/01/2001 | El Salvador | El Salvador, Guatemala, Honduras | 7.7 | VIII | 844 | 4723 | 1,334,529 |
| 9 | 26/12/2003 | Bam (Iran) | Kerman Province | 6.6 | IX | 26,796 | 22,628 | 267,628 |
| 10 | 26/12/2004 | Indonesia | Indian Ocean coastal countries | 9.2 | IX | 165,708 | - | 523,898 |
| 11 | 08/10/2005 | Kashmir (Pakistan) | Pakistan, India | 7.6 | XI | 86,000–87,351 | 69,000–75,266 | 2,800,000 |
| 12 | 27/05/2006 | Yogyakarta (Indonesia) | Yogyakarta, Java, Indonesia | 6.4 | IX | 5749–5778 | 38,568–137,883 | 600,000–699,295 |
| 13 | 02/04/2007 | Solomon Islands | Solomon Islands, Papua, New Guinea | 8.1 | VIII | 52 | 9 | 2384 |
| 14 | 12/05/2008 | Sichuan (China) | Sichuan Province | 7.9 | ΧΙ | 87,476 | 366,596 | 45,976,596 |
| 15 | 06/04/2009 | L’Aquila (Italy) | Abruzzo | 6.3 | Χ | 295 | 1000 | 56,000 |
| 16 | 30/09/2009 | Sumatra (Indonesia) | Sumatra | 6.3 | VII | 1195 | 1798 | 2,501,798 |
| 17 | 12/01/2010 | Haiti | Haiti | 7.0 | X | 222,570 | 300,000 | 3,700,000 |
| 18 | 23/10/2011 | Van (Turkey) | Eastern Turkey | 7.1 | VIII | 604 | 4152 | 32,938 |
| 19 | 09/11/2011 | Van (Turkey) | Eastern Turkey | 5.6 | VII | 40 | 30 | 105 |
| 20 | 11/03/2011 | Tōhoku (Japan) | Eastern Japan | 9.1 | IX | 19,759 | 6242 | 2553 |
| 21 | 20/04/2013 | Lushan (China) | Sichuan, Chongqing, Shaanxi | 7.0 | VIII | 198 | 14,785 | 2,198,785 |
| 22 | 15/10/2013 | Bohol (Philippines) | Philippines | 7.2 | IX | 230 | 976 | 3,222,224 |
| 23 | 26/01/2014 | Cephalonia Island (Greece) | Western Cephalonia | 6.1 | VII | 0 | 0 | - |
| 24 | 03/02/2014 | Cephalonia Island (Greece) | Western Cephalonia | 5.9 | VIII | 0 | 10 | - |
| 25 | 25/04/2015 | Gorkha (Nepal) | Kathmandu Valley, Everest | 7.8 | Χ | 8831 | 17,932 | 5,639,722 |
| 26 | 16/04/2016 | Ecuador | Ecuador, Colombia, Peru | 7.8 | VIII | 672 | 6274 | 389,364 |
| 27 | 14/04/2016 | Kumamoto (Japan) | Kumamoto Province, Kyushu, Japan | 6.2 | - | 9 | 800 | 120,800 |
| 28 | 16/04/2016 | Kumamoto (Japan) | Kumamoto Province, Kyushu, Japan | 7.0 | IX | 49 | 1684 | 298,432 |
4. Earthquake-Triggered Respiratory Infectious Diseases
4.1. Viral-Associated Diseases
4.2. Fungal-Associated Diseases
Coccidioidomycosis
4.3. Mycobacterial-Associated Diseases
Tuberculosis
5. Earthquake-Triggered Gastrointestinal Diseases (Water- and Food-Borne Diseases)
5.1. Bacterial-Associated Diseases
5.1.1. Shigella
5.1.2. Salmonella Enterica
5.1.3. Tularemia
5.1.4. Cholera
5.1.5. Helicobacter Pylori
5.2. Protozoa-Associated Diseases
Giardiasis
5.3. Virus-Associated Diseases
5.3.1. Rotavirus
5.3.2. Hepatitis A and E
6. Earthquake-Triggered Vector-Borne Diseases
6.1. Bacterial-Associated Diseases
Scrub Typhus
6.2. Protozoan-Associated Diseases
6.2.1. Malaria
6.2.2. Leishmaniasis
6.3. Viral-Associated Diseases
Zika Virus
7. Wound and Skin Infections
7.1. Tetanus
7.2. Gas Gangrene (Myonecrosis)
7.3. Other Skin Infections
8. Risk Factors and Preventive Measures
8.1. Risk Factors for Infectious Diseases Occurence
- Heavy structural damage to critical healthcare infrastructure, including facilities and buildings, remained unfixed during the emergency response and the subsequent recovery, causing delayed management and treatment of severe infectious diseases cases.
- Lack of awareness and provision of early or real-time warning for the upcoming and the ongoing events, resulting in little time for preparedness or evacuation.
- Severely injured earthquake and tsunami survivors highly exposed to high pathogen densities in soil and water.
- Immense changes in climate and aggravating weather conditions in the emergency response phase including dramatic temperature changes.
- Prolonged physical exposure to and inhalation of:
- ○
- airborne particulate matter due to large dust clouds formed by earthquake-triggered landslides.
- ○
- airborne particulate matter due to contaminated ejecta dust formed by earthquake-triggered liquefaction phenomena with a destructive impact on water and sewage systems.
- Prolonged physical exposure to and aspiration of contaminated water due to tsunami generation and impact on the coastal residential zones.
- Emergency shelters and evacuation camps with:
- ○
- High population density and overcrowding.
- ○
- Poor living conditions comprising small places for individuals and families and insufficient equipment for the homeless and evacuees (blankets, bed clothes, sleeping bags, etc.).
- ○
- Lack of clean running water due to damage and contamination of the water supply systems and water sources, respectively.
- ○
- Unsanitary conditions (poor hand hygiene) due to a shortage of personal hygiene items.
- ○
- Malnutrition due to insufficient food provision and shortage of long-lasting food supplies.
- ○
- Insufficient equipment comprising essentials and poor heating, ventilation and air conditioning systems among others.
- ○
- Rodent/vector infestation.
- Increased exposure to vectors and rodents due to earthquake-triggered ecological changes, leading to extensive formation of potential breeding and feeding sites of vectors and rodents.
- The weak immune system of vulnerable groups of the affected population comprising the elderly, the chronically ill individuals, and young children.
- The dependency of young children, people with disabilities, and elders of the affected communities seeking assistance with daily activities.
- Poor socio-economic conditions, including large percentage of low education level, a large part of the population living below the national poverty line leading to insufficient personal hygiene and denial of risk, disinterest, and ignorance of risk, as well as poorly constructed buildings and infrastructures.
- Poor health education and training on infectious disease prevention and control.
- Lack of emergency preparedness and training of residents and medical staff for infectious disease prevention.
- Insufficient or low vaccination coverage due to limited vaccination campaigns and short supplies.
- Close contact with cases and activities and interaction in areas where clusters of infectious disease cases have been observed.
8.2. Prevention Strategies and Actions for Mitigating the Risk of Earthquake-Triggered Infectious Diseases
8.2.1. Establishment of a Proper Disease Surveillance System
8.2.2. Prevention of Infectious Diseases in Emergency Shelters
8.2.3. Prevention of Infectious Diseases among First Responders and Affected Population
- Ensuring the safety of drinking water and sewerage systems not only in either temporary or permanent relief camps but also in areas characterized by high risk
- Compliance with the existing safety and hygiene measures
- Where existing measures are not sufficient, educational activities for hygiene and sanitation awareness raising should be conducted, aiming for the integration of safe water and hand hygiene best practices into households, communities, and countries
- Large-scale preventive vaccination and medicine programs for several infectious diseases should be implemented, along with the establishment of a proper disease surveillance program and a long–term empowering and strengthening of the public-sector health system.
8.2.4. Measures for Mitigating the Risk of Respiratory Infectious Diseases
8.2.5. Measures for Mitigating the Risk of Waterborne Diseases
8.2.6. Measures for Mitigating the Risk of Vector- and Rodent-Borne Diseases
8.2.7. Education, Training, and Awareness-Raising Actions
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centre for Research on the Epidemiology of Disasters—United Nations Office for Disaster Risk Reduction. Human Cost of Disasters: An Overview of the Last 20 Years (2000–2019); CRED-UNDRR: Brussels, Belgium, 2020; 30p. [Google Scholar]
- Guha-Sapir, D. Rapid assessment of health needs in mass emergencies: Review of current concepts and methods. World Health Stat. Q. 1991, 44, 171–179. [Google Scholar]
- Alexander, D.E. Death and Injury in Earthquakes. Disasters 1985, 9, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, L.E.; Reutershan, T.P. Catastrophic disasters and the design of disaster medical care systems. Ann. Emerg. Med. 1987, 16, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.P.; Noji, E.X.; Krimgold, F.; Smith, G.S. Considerations in the Epidemiology of Earthquake Injuries. Earthq. Spectra 1990, 6, 507–528. [Google Scholar] [CrossRef]
- Alexander, D. The Health Effects of Earthquakes in the Mid-1990s. Disasters 1996, 20, 231–247. [Google Scholar] [CrossRef] [PubMed]
- Peek-Asa, C.; Ramirez, M.; Seligson, H.; Shoaf, K. Seismic, structural, and individual factors associated with earthquake related injury. Int. Prev. 2003, 9, 62–66. [Google Scholar] [CrossRef]
- Gutiérrez, E.; Taucer, F.; De Groeve, T.; Al-Khudhairy, D.H.A.; Zaldivar, J.M. Analysis of Worldwide Earthquake Mortality using Multivariate Demographic and Seismic Data. Am. J. Epidemiol. 2005, 161, 1151–1158. [Google Scholar] [CrossRef]
- Ramirez, M.; Peek-Asa, C. Epidemiology of traumatic injuries from earthquakes. Epidemiol. Rev. 2005, 27, 47–55. [Google Scholar] [CrossRef]
- Jiang, J.; Li, Y.; Huang, X.; Li, B.; Su, L.; Zhong, D.; Shi, C.; Li, M.; Shan, J.; Chen, Y. Lessons learnt from the Wenchuan earthquake: Performance evaluation of treatment of critical injuries in hardest-hit areas. J. Evid. Based Med. 2012, 5, 114–123. [Google Scholar] [CrossRef]
- Bar-On, E.; Lebel, E.; Blumberg, N.; Sagi, R.; Kreiss, Y. Pediatric Orthopedic Injuries Following an Earthquake: Experience in an Acute-Phase Field Hospital. J. Trauma Nurs. 2015, 22, 223–228. [Google Scholar] [CrossRef]
- Clements, B.W.; Casani, J.A.P. Disasters and Public Health: Planning and Response, 2nd ed.; Butterworth-Heinemann: Oxford, UK, 2016; 538p, ISBN 978-0-12-801980-1. [Google Scholar]
- Michetti, A.M.; Esposito, E.; Guerrieri, L.; Porfido, S.; Serva, L.; Tatevossian, R.; Vittori, E.; Audemard, F.; Azuma, T.; Clague, J.; et al. Environmental Seismic Intensity Scale 2007—ESI. Mem. Descr. Carta Geol. Ital. 2007, 74, 7–54. [Google Scholar]
- Audemard, F.; Azuma, T.; Baiocco, F.; Baize, S.; Blumetti, A.M.; Brustia, E.; Clague, J.; Comerci, V.; Esposito, E.; Guerrieri, L.; et al. Earthquake Environmental Effect for Seismic Hazard Assessment: The ESI Intensity Scale and the EEE Catalogue. Mem. Carta Geol. D’ Ital. 2015, 97, 5–8. [Google Scholar]
- Kunii, O.; Akagi, M.; Kita, E. The medical and public health response to the great Hanshin-Awaji earthquake in Japan: A case study in disaster planning. Med. Glob. Surviv. 1995, 2, 214–226. [Google Scholar]
- Tatemachi, K. Acute diseases during and after the Great Han-shin- Awaji earthquake. In Proceedings of the a WHO Symposium: Earthquakes and People’s Health—Vulnerability Reduction, Preparedness and Rehabilitation, Kobe, Japan, 27–30 January 1997; pp. 48–52. [Google Scholar]
- Naghii, M.R. Public health impact and medical consequences of earthquakes. Public health impact and medical consequences of earthquakes. SciELO Public Health 2005, 18, 216–221. [Google Scholar] [CrossRef]
- Partridge, R.A.; Proano, L.; Marcozzi, D.; Garza, A.G.; Nemeth, I.; Brinsfield, K.; Weinstein, E.S. Oxford American Handbook of Disaster Medicine. Oxford University Press: Oxford, UK, 2012; 1048p. [Google Scholar]
- Lomnitz, C. Major earthquakes and tsunamis in Chile during the period 1535 to 1955. Geol. Rundsch. 1970, 59, 938–960. [Google Scholar] [CrossRef]
- De Bruycker, M.; Greco, D.; Lechat, M.F. The 1980 Earthquake in Southern Italy: Mortality and Morbidity. Int. J. Epidemiol. 1985, 14, 113–117. [Google Scholar] [CrossRef]
- Armenian, H.K.; Noji, E.K.; Oganessian, A.P. Case Control Study of Injuries Due to the Earthquake in Soviet Armenia. Bull. World Health Organ. 1992, 70, 251–257. [Google Scholar]
- Eberhart-Phillips, J.E.; Saunders, T.M.; Robinson, A.L.; Hatch, D.L.; Gibson Parrish, R. Profile of Mortality from the 1989 Loma Prieta Earthquake using Coroner and Medical Examiner Reports. Disasters 1994, 18, 160–170. [Google Scholar] [CrossRef]
- Pretto, E.A.; Angus, D.C.; Abrams, J.I.; Shen, B.; Bissell, R.; Castro, V.M.; Sawyers, R.; Watoh, Y.; Ceciliano, N.; Ricci, E.; et al. An analysis of prehospital mortality in an earthquake: Disaster reanimatology study group. Prehosp. Disaster Med. 1994, 9, 107–117. [Google Scholar] [CrossRef]
- Parasuraman, S. The Impact of the 1993 Latur-Osmanabad (Maharashtra) Earthquake on Lives, Livelihoods and Property. Disasters 1995, 19, 156–169. [Google Scholar] [CrossRef]
- Tanida, N. What happened to elderly people in the great Hanshin earthquake? BMJ 1996, 313, 1133. [Google Scholar] [CrossRef]
- Angus, D.C.; Pretto, E.A.; Abrams, J.I.; Ceciliano, N.; Watoh, Y.; Kirimli, B.; Certug, A.; Comfort, L.K.; Disaster Reanimatology Study Group. Epidemiologic assessment of mortality, building collapse pattern, and medical response after the 1992 earthquake in Turkey. Prehosp. Disaster Med. 1997, 12, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Kuwagata, Y.; Oda, J.; Tanaka, H.; Iwai, A.; Matsuoka, T.; Takaoka, M.; Kishi, M.; Morimoto, F.; Ishikawa, K.; Mizushima, Y.; et al. Analysis of 2,702 Traumatized Patients in the 1995 Hanshin-Awaji Earthquake. J. Trauma 1997, 43, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Oda, J.; Iwai, A.; Kuwagata, Y.; Matsuoka, T.; Takaoka, M.; Kishi, M.; Morimoto, F.; Ishikawa, K.; Mizushima, Y.; et al. Morbidity and mortality of hospitalized patients after the 1995 Hanshin Awaji earthquake. Am. J. Emerg. Med. 1999, 17, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Peek-Asa, C.; Ramirez, M.R.; Shoaf, K.; Seligson, H.; Kraus, J.F. GIS mapping of earthquake-related deaths and hospital admissions from the 1994 Northridge, California, Earthquake. Ann. Epidemiol. 2000, 10, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Liang, N.J.; Shih, Y.T.; Shih, F.Y.; Wu, H.M.; Wang, H.J.; Shi, S.F.; Liu, M.Y.; Wang, B.B. Disaster epidemiology and medical response in the Chi-Chi earthquake in Taiwan. Ann. Emerg. Med. 2001, 38, 549–555. [Google Scholar] [CrossRef]
- Chan, C.C.; Lin, Y.P.; Chen, H.H.; Chang, T.Y.; Cheng, T.J.; Chen, L.S. A population-based study on the immediate and prolonged effects of the 1999 Taiwan earthquake on mortality. Ann. Epidemiol. 2003, 13, 502–508. [Google Scholar] [CrossRef]
- Musson, R.M.W. Fatalities in British earthquakes. Astron. Geophys. 2003, 44, 14–16. [Google Scholar] [CrossRef]
- Aoki, N.; Nishimura, A.; Pretto, E.A.; Sugimoto, K.; Beck, J.R.; Fukui, T. Survival and Cost Analysis of Fatalities of the Kobe Earthquake in Japan. Prehosp. Emerg. Care 2004, 8, 217–222. [Google Scholar] [CrossRef]
- Bissell, R.A.; Pinet, L.; Nelson, M.; Levy, M. Evidence of the effectiveness of health sector preparedness in disaster response, the example of four earthquakes. Fam. Community Health 2004, 27, 193–203. [Google Scholar] [CrossRef]
- Fu, Z.X.; Liu, G.P.; Shao, H.C.; Ding, X. Overview on shallow strong earthquake activity and earthquake live losses of Chinese mainland in the centenary from 1901 to 2001. Acta Seismol. Sin. 2005, 18, 392401. [Google Scholar]
- Abolghasemi, H.; Radfar, M.H.; Khatami, M.; Saghafi Nia, M.; Amid, A.; Briggs, S.M. International medical response to a natural disaster: Lessons learned from the Bam earthquake experience. Prehosp. Disaster Med. 2006, 21, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Hatamizadeh, P.; Najafi, I.; Vanholder, R.; Rashid-Farokhi, F.; Sanadgol, H.; Seyrafian, S.; Mooraki, A.; Atabak, S.; Samimagham, H.; Pourfarziani, V.; et al. Epidemiologic aspects of the Bam earthquake in Iran: The nephrologic perspective. Am. J. Kidney Dis. 2006, 47, 428–438. [Google Scholar] [CrossRef] [PubMed]
- So, E.; Spence, R. Estimating shaking-induced casualties and building damage for global earthquake events: A proposed modelling approach. Bull. Earthq. Eng. 2013, 11, 347–363. [Google Scholar] [CrossRef]
- Bilham, R. Lessons from the Haiti earthquake. Nature 2010, 463, 878–879. [Google Scholar] [CrossRef]
- Doocy, S.; Jacquet, G.; Cherewick, M.; Kirsch, T.D. The injury burden of the 2010 Haiti earthquake: A stratified cluster survey. Inj. Int. J. Care Inj. 2013, 44, 842–847. [Google Scholar] [CrossRef]
- Alexander, D.; Magni, M. Mortality in the L’Aquila (Central Italy) Earthquake of 6 April 2009: A Study in Victimisation. PLoS Curr. Disasters 2013, 5, e50585b8e6efd1. [Google Scholar] [CrossRef]
- Kongsaengdao, S.; Bunnag, S.; Siriwiwattnakul, N. Treatment of survivors after the tsunami. N. Engl. J. Med. 2005, 352, 2654–2655. [Google Scholar] [CrossRef]
- Lim, P.L. Wound Infections in Tsunami Survivors: A Commentary. Ann. Acad. Med. Singap. 2005, 34, 582–585. [Google Scholar]
- Keim, M.E. Cyclones, Tsunamis, and Human Health: The Key Role of Preparedness. Oceanography 2006, 19, 40–49. [Google Scholar] [CrossRef]
- Keim, M.E. Health-related impacts of Tsunami disasters. In WIT Transactions on State of the Art in Science and Engineering; WIT Press: Paris, France, 2013; Volume 6, pp. 139–153. [Google Scholar] [CrossRef]
- Scawthorn, C. Fire Losses from Earthquakes: State of the Art. Dev. Geotech. Eng. 1987, 45, 237–261. [Google Scholar] [CrossRef]
- Scawthorn, C.; Eidinger, J.M.; Schiff, A.J. Fire Following Earthquake; Technical Council on Lifeline Earthquake Engineering (TCLEE) Monograph 26; American Society of Civil Engineers: Reston, VA, USA; National Fire Protection Association (NFPA): Quincy, MA, USA, 2005; 332p. [Google Scholar]
- Zhang, B.H.; Chen, H.D. Investigation on earthquake-induced fire disasters. J. Nat. Disasters 1994, 3, 39–48. [Google Scholar] [CrossRef]
- Marano, K.D.; Wald, D.J.; Allen, T.I. Global earthquake casualties due to secondary effects: A quantitative analysis for improving rapid loss analyses. Nat. Hazards 2010, 52, 319–328. [Google Scholar] [CrossRef]
- Petley, D. Global patterns of loss of life from landslides. Geology 2012, 40, 927–930. [Google Scholar] [CrossRef]
- Kennedy, I.T.R.; Petley, D.N.; Williams, R.; Murray, V. A Systematic Review of the Health Impacts of Mass Earth Movements (Landslides). PLoS Curr. 2015, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Bird, J.F.; Bommer, J.J. Earthquake losses due to ground failure. Eng. Geol. 2014, 75, 147–179. [Google Scholar] [CrossRef]
- Sanchez-Carrillo, C.I. Morbidity following Mexico City’s 1985 earthquakes: Clinical and epidemiologic findings from hospitals and emergency units. Public Health Rep. 1989, 104, 482–488. [Google Scholar]
- Peek-Asa, C.; Kraus, J.F.; Bourque, L.B.; Vimalachandra, D.; Yu, J.; Abrams, J. Fatal and hospitalized injuries resulting from the 1994 Northridge earthquake. Int. J. Epidemiol. 1998, 27, 459–465. [Google Scholar] [CrossRef]
- Fan, Z.; Li, A.; Lian, B.; Zhou, W.; Wei, H.; Chen, C.; Xu, P. Injury types of victims in the 12th May 2008 Wenchuan earthquake: Analysis of 1,038 patients in Jiangyou City. Eur. J. Trauma Emerg. Surg. 2011, 37, 3–7. [Google Scholar] [CrossRef]
- Salcioglu, E.; Basoglu, M.; Livanou, M. Post-traumatic stress disorder and comorbid depression among survivors of the 1999 earthquake in Turkey. Disasters 2007, 31, 115–129. [Google Scholar] [CrossRef]
- Carr, V.J.; Lewin, T.J.; Webster, R.A.; Hazell, P.L.; Kenardy, J.A.; Carter, G.L. Psychosocial sequelae of the 1989 Newcastle earthquake: I. Community disaster experiences and psychological morbidity 6 months post-disaster. Psychol. Med. 1995, 25, 539–555. [Google Scholar] [CrossRef] [PubMed]
- Goenjian, A.K.; Najarian, L.M.; Pynoos, R.S.; Steinberg, A.M.; Petrosian, P.; Setrakyan, S.; Fairbanks, L.A. Posttraumatic stress reactions after single and double trauma. Acta Psychiatr. Scand. 1994, 90, 214–221. [Google Scholar] [CrossRef] [PubMed]
- McMillen, C.; North, C.S.; Smith, E.M. What parts of PTSD are normal: Intrusion, avoidance, or arousal? Data from the Northridge, California, earthquake. J. Trauma Stress 2000, 13, 57–75. [Google Scholar] [CrossRef] [PubMed]
- Sharan, P.; Chaudhary, G.; Kavathekar, S.A.; Saxena, S. Preliminary report of psychiatric disorders in survivors of a severe earthquake. Am. J. Psychiatry 1996, 153, 556–558. [Google Scholar] [PubMed]
- Başoğlu, M.; Salcioglu, E.; Livanou, M. Traumatic Stress Responses in Earthquake Survivors in Turkey. J. Trauma. Stress 2002, 15, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ho, S.M. Risk factors of posttraumatic stress disorder among survivors after the 512 Wenchuan earthquake in China. PLoS ONE 2011, 6, e22371. [Google Scholar] [CrossRef]
- Zhang, Z.; Ran, M.-S.; Li, Y.-H.; Ou, G.-J.; Gong, R.-R.; Li, R.-H.; Fan, M.; Jiang, Z.; Fang, D.-Z. Prevalence of post-traumatic stress disorder among adolescents after the Wenchuan earthquake in China. Psychol. Med. 2012, 42, 1687–1693. [Google Scholar] [CrossRef]
- Kouadio, I.K.; Aljunid, S.; Kamigaki, T.; Hammad, K.; Oshitani, H. Infectious diseases following natural disasters: Prevention and control measures. Expert Rev. Anti-Infect. Ther. 2012, 10, 95–104. [Google Scholar] [CrossRef]
- World Health Organization. Communicable Diseases Following Natural Disasters–Risk Assessment and Priority Interventions. In Pro-Gramme on Disease Control in Humanitarian Emergencies Communicable Diseases Cluster; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Centre for Research on the Epidemiology of Disasters (CRED). EM-DAT—The International Disaster Database. Available online: https://public.emdat.be/ (accessed on 15 July 2022).
- Styron, R.; Pagani, M. The GEM Global Active Faults Database. Earthq. Spectra 2020, 36, 160–180. [Google Scholar] [CrossRef]
- Schneider, E.; Hajjeh, R.A.; Spiegel, R.A.; Jibson, R.W.; Harp, E.L.; Marshall, G.A.; Gunn, R.A.; McNeil, M.M.; Pinner, R.W.; Baron, R.C.; et al. A coccidioidomycosis outbreak following the Northridge, Calif, earthquake. J. Am. Med. Assoc. JAMA 1997, 277, 904–908. [Google Scholar] [CrossRef]
- Jibson, R.W. A Public Health Issue Related To Collateral Seismic Hazards: The Valley Fever Outbreak Triggered By The 1994 Northridge, California Earthquake. Surv. Geophys. 2002, 23, 511–528. [Google Scholar] [CrossRef]
- Woersching, J.C.; Snyder, A.E. Earthquakes in El Salvador: A descriptive study of health concerns in a rural community and the clinical implications, part I. Disaster Manag. Response 2003, 1, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Woersching, J.C.; Snyder, A.E. Earthquakes in El Salvador: A descriptive study of health concerns in a rural community and the clinical implications—Part II. Disaster Manag. Response 2004, 2, 10–13. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Launching a National Surveillance System after an earthquake—Haiti, 2010. MMWR Morb. Mortal Wkly. Rep. 2010, 59, 933–938. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Malaria acquired in Haiti—2010. MMWR Morb. Mortal Wkly. Rep. 2010, 59, 217–219. [Google Scholar]
- Neuberger, A.; Tenenboim, S.; Golos, M.; Pex, R.; Krakowsky, Y.; Urman, M.; Vernet, S.; Schwartz, E. Infectious diseases seen in a primary care clinic in Leogane, Haiti. Am. J. Trop. Med. Hyg. 2012, 86, 11–15. [Google Scholar] [CrossRef]
- Koenig, S.P.; Rouzier, V.; Vilbrun, S.C.; Morose, W.; Collins, S.E.; Joseph, P.; Decome, D.; Ocheretina, O.; Galbaud, S.; Hashiguchi, L.; et al. Tuberculosis in the aftermath of the 2010 earthquake in Haiti. Bull. World Health Organ. 2015, 93, 498–502. [Google Scholar] [CrossRef]
- Masur, J.; Koenig, S.P.; Julma, P.; Ocheretina, O.; Durán-Mendicuti, M.A.; Fitzgerald, D.W.; Pape, J.W. Active Tuberculosis Case Finding in Haiti. Am. J. Trop. Med. Hyg. 2017, 97, 433–435. [Google Scholar] [CrossRef]
- Dube, A.; Moffatt, M.; Davison, C.; Bartels, S. Health Outcomes for Children in Haiti since the 2010 Earthquake: A Systematic Review. Prehosp. Disaster Med. 2018, 33, 77–88. [Google Scholar] [CrossRef]
- Petrazzi., L.; Striuli, R.; Polidoro, L.; Petrarca, M.; Scipioni, R.; Struglia, M.; Giorgini, P.; Necozione, S.; Festuccia, V.; Ferri, C. Causes of hospitalisation before and after the 2009 L’Aquila earthquake. Intern. Med. J. 2013, 43, 1031–1034. [Google Scholar] [CrossRef]
- Silvestros, C.; Mellou, K.; Williams, C.; Triantafyllou, E.; Rigakos, G.; Papoutsidou, E.; Tsekou, K.; Likiardopoulos, S.; Pantelios, G.; Kouris, G.; et al. A rapid post-disaster surveillance model enabling outbreak detection and healthcare response following earthquakes on Kefalonia island, Greece, February–May 2014. Rural Remote Health 2017, 17, 3744. [Google Scholar] [CrossRef]
- Takakura, R.; Himeno, S.; Kanayama, Y.; Sonoda, T.; Kiriyama, K.; Furubayashi, T.; Yabu, M.; Yoshida, S.; Nagasawa, Y.; Inoue, S.; et al. Follow-up after the Hanshin-Awaji earthquake: Diverse influences on pneumonia, bronchial asthma, peptic ulcer and diabetes mellitus. Intern Med. 1997, 36, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Chen, W.J.; Malilay, J.; Twu, S.J. The public health response to the Chi-Chi earthquake in Taiwan, 1999. Public Health Rep. 2003, 118, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.W.; Liu, C.S.; Li, C.I.; Tan, C.K.; Ng, K.C.; Lai, M.M.; Lin, C.C. Post-earthquake illness and disease after the Chi-Chi earthquake. Eur. J. Intern. Med. 2000, 11, 353–354. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.E.; Farshad, A.A.; Asadi-Lari, M. The devastation of Bam: An overview of health issues 1 month after the earth-quake. Public Health 2004, 118, 403–408. [Google Scholar] [CrossRef]
- Jafari, N.J.; Radfar, M.H.; Ghofrani, H. Incidence of Infectious Diseases One Month after the Bam Earthquake (2004). J. Med. Sci. 2007, 7, 597–602. [Google Scholar] [CrossRef]
- Mavrouli, M.; Mavroulis, S.; Lekkas, E.; Tsakris, A. Respiratory Infections Following Earthquake-Induced Tsunamis: Transmission Risk Factors and Lessons Learned for Disaster Risk Management. Int. J. Environ. Res. Public Health 2021, 18, 4952. [Google Scholar] [CrossRef]
- Laverick, S.; Kazmi, S.; Ahktar, S.; Raja, J.; Perera, S.; Bokhari, A.; Meraj, S.; Ayub, K.; da Silva, A.; Pye, M.; et al. Asian earthquake: Report from the first volunteer British hospital team in Pakistan. Emerg. Med. J. 2007, 24, 543–546. [Google Scholar] [CrossRef]
- Shah, N.; Abro, M.A.; Abro, M.A.; Khan, A.; Anwar, F.; Akhtar, H. Disease pattern in earthquake affected areas of Pakistan: Data from Kaghan valley. J. Ayub. Med. Coll. Abbottabad (JAMC) 2010, 22, 81–86. [Google Scholar]
- Tan, C.M.; Lee, V.J.; Chang, G.H.; Ang, H.X.; Seet, B. Medical response to the 2009 Sumatra earthquake: Health needs in the post-disaster period. Singap. Med. J. 2012, 53, 99–103. [Google Scholar]
- Aoyagi, T.; Yamada, M.; Kunishima, H.; Tokuda, K.; Yano, H.; Ishibashi, N.; Hatta, M.; Endo, S.; Arai, K.; Inomata, S.; et al. Characteristics of infectious diseases in hospitalized patients during the early phase after the 2011 great East Japan earthquake: Pneumonia as a significant reason for hospital care. Chest 2013, 143, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Fan, H.; Lv, Q.; Liu, Z.; Zhang, Y.; Hou, S. Analyses of the Disease Spectrum of Children after the Lushan Earthquake. Pediatr. Emerg. Care 2015, 31, 496–498. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.; Zong, Z.; Wang, X.; Zhou, G.; Feng, P.; Chen, M.; Wang, B.; Yang, C.; Yin, W.; Jin, X.; et al. Severe infections as the leading complication after the Lushan earthquake. Intensive Care Med. 2015, 41, 560–561. [Google Scholar] [CrossRef]
- Salazar, M.A.; Pesigan, A.; Law, R.; Winkler, V. Post-disaster health impact of natural hazards in the Philippines in 2013. Glob. Health Action 2016, 9, 31320. [Google Scholar] [CrossRef]
- Murray, K.O.; Castillo-Carandang, N.T.; Mandalakas, A.M.; Cruz, A.T.; Leining, L.M.; Gatchalian, S.R.; PEER Health Bohol Pediatric Study Team. Prevalence of Tuberculosis in Children after Natural Disasters, Bohol, Philippines. Emerg. Infect. Dis. 2019, 25, 1884–1892. [Google Scholar] [CrossRef] [PubMed]
- Lachish, T.; Bar, A.; Alalouf, H.; Merin, O.; Schwartz, E. Morbidity among the Israeli Defense Force response team during Nepal, post-earthquake mission, 2015. J. Travel. Med. 2017, 24, taw083. [Google Scholar] [CrossRef]
- Malla, T.; Malla, K.K.; Singh, S.K.; Shrestha, S. Analysis of Post Earthquake Disease Pattern in a Camp at Gyampesal Gorkha. Kathmandu Univ. Med. J. 2016, 14, 249–253. [Google Scholar]
- Wang, J.; Ding, H.; Lv, Q.; Chen, J.H.; Sun, Y.F.; Fan, H.J.; Liu, Q.L. 2015 Nepal Earthquake: Analysis of Child Rescue and Treatment by a Field Hospital. Disaster Med. Public Health Prep. 2016, 10, 716–719. [Google Scholar] [CrossRef]
- Bhandari, D.; Pandey, P. Health Problems while Working as a Volunteer or Humanitarian Aid Worker in Post-Earthquake Nepal. JNMA J. Nepal Med. Assoc. 2018, 56, 691–695. [Google Scholar] [CrossRef]
- Giri, B.R.; Chapagain, R.H.; Sharma, S.; Shrestha, S.; Ghimire, S.; Shankar, P.R. Effect of the 2015 earthquake on pediatric inpatient pattern at a tertiary care hospital in Nepal. BMC Pediatr. 2018, 18, 28. [Google Scholar] [CrossRef]
- Shrestha, D.; Shrestha, M.K.; Raya, G.B.; Bhattachan, A.; Hayashi, K.; Ariyoshi, K.; Parry, C.M.; Dhoubhadel, B.G. A 14-year-old girl presenting with tuberculous intestinal perforation while in a temporary shelter after the 2015 earthquake in Nepal. Paediatr. Int. Child Health 2018, 38, 69–72. [Google Scholar] [CrossRef]
- Yorifuji, T.; Sato, T.; Yoneda, T.; Kishida, Y.; Yamamoto, S.; Sakai, T.; Sashiyama, H.; Takahashi, S.; Orui, H.; Kato, D.; et al. Disease and injury trends among evacuees in a shelter located at the epicenter of the 2016 Kumamoto earthquakes, Japan. Arch. Environ. Occup. Health 2018, 73, 284–291. [Google Scholar] [CrossRef]
- Yang, X.; Liu, Q.; Zhang, R. Epidemiology of pulmonary tuberculosis in Wenchuan earthquake stricken area: Population-based study. J. Evid. Based Med. 2013, 6, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Greco, D.; Faustini, A.; Forastiere, F.; Galanti, M.R.; Magliola, M.E.; Moro, M.L.; Piergentili, P.; Rosmini, F.; Stazi, M.A.; Luzi, S.; et al. Epidemiological surveillance of diseases following the earthquake of 23rd November 1980 in Southern Italy. Disasters 1981, 5, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Gdalevich, M.; Ashkenazi, I. Infection control in earthquake rescue team. Lancet 1999, 354, P1564. [Google Scholar] [CrossRef]
- Vahaboglu, H.; Gundes, S.; Karadenizli, A.; Mutlu, B.; Cetin, S.; Kolayli, F.; Coskunkan, F.; Dündar, V. Transient increase in diarrheal diseases after the devastating earthquake in Kocaeli, Turkey: Results of an infectious disease surveillance study. Clin. Infect. Dis. 2000, 31, 1386–1389. [Google Scholar] [CrossRef]
- Oztürk, C.E.; Sahin, I.; Yavuz, T.; Oztürk, A.; Akgünoğlu, M.; Kaya, D. Intestinal parasitic infection in children in post-disaster situations years after earthquake. Pediatr. Int. 2004, 46, 656–662. [Google Scholar] [CrossRef]
- Sencan, I.; Sahin, I.; Kaya, D.; Oksuz, S.; Yildirim, M. Assessment of HAV and HEV seroprevalence in children living in post-earthquake camps from Düzce, Turkey. Eur. J. Epidemiol. 2004, 19, 461–465. [Google Scholar] [CrossRef]
- Karadenizli, A.; Gurcan, S.; Kolayli, F.; Vahaboglu, H. Outbreak of tularaemia in Golcuk, Turkey in 2005: Report of 5 cases and an overview of the literature from Turkey. Scand. J. Infect. Dis. 2005, 37, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.D.; Ozturk, C.E.; Yavuz, T.; Ozaydin, C.; Bahcebasi, T. Changing patterns of hepatitis A and E sero-prevalences in children after the 1999 earthquakes in Duzce, Turkey. J. Paediatr. Child Health 2008, 44, 205–207. [Google Scholar] [CrossRef]
- Lora-Suarez, F.; Marin-Vasquez, C.; Loango, N.; Gallego, M.; Torres, E.; Gonzalez, M.M.; Castaño-Osorio, J.C.; Gómez-Marín, J.E. Giardiasis in children living in post-earthquake camps from Armenia (Colombia). BMC Public Health 2002, 2, 5. [Google Scholar] [CrossRef]
- Brennan, R.J.; Rimba, K. Rapid health assessment in Aceh Jaya District, Indonesia, following the December 26 tsunami. Emerg. Med. Australas 2005, 17, 341–350. [Google Scholar] [CrossRef]
- Karmakar, S.; Rathore, A.S.; Kadri, S.M.; Dutt, S.; Khare, S.; Lal, S. Post-earthquake outbreak of rotavirus gastroenteritis in Kashmir (India): An epidemiological analysis. Public Health 2008, 122, 981–989. [Google Scholar] [CrossRef]
- Nigro, G.; Bottone, G.; Maiorani, D.; Trombatore, F.; Falasca, S.; Bruno, G. Pediatric Epidemic of Salmonella enterica Serovar Typhimurium in the Area of L’Aquila, Italy, Four Years after a Catastrophic Earthquake. Int. J. Environ. Res. Public Health 2016, 13, 475. [Google Scholar] [CrossRef]
- Tappero, J.W.; Tauxe, R.V. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg. Infect. Dis. 2011, 17, 2087–2093. [Google Scholar] [CrossRef] [PubMed]
- Suvak, B.; Dulger, A.C.; Suvak, O.; Aytemiz, E.; Kemik, O. The prevalence of helicobacter pylori among dyspeptic patients in an earthquake-stricken area. Clinics 2015, 70, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P. Letter from Nepal, August 12, 2015—Cholera in post-earthquake Kathmandu. Travel Med. Infect. Dis. 2015, 13, 425. [Google Scholar] [CrossRef] [PubMed]
- Sekine, K.; Roskosky, M. Lessons Learned from Enhancing Sentinel Surveillance for Cholera in Post-Earthquake Nepal in 2016. Am. J. Trop. Med. Hyg. 2019, 100, 494–496. [Google Scholar] [CrossRef]
- Ranjbar, R.; Hosseini, M.J.; Kaffashian, A.R.; Farshad, S. An outbreak of shigellosis due to Shigella flexneri serotype 3a in a prison in Iran. Arch. Iran. Med. 2010, 13, 413–416. [Google Scholar]
- Genobile, D.; Gaston, J.; Tallis, G.F.; Gregory, J.E.; Griffith, J.M.; Valcanis, M.; Lightfoot, D.; Marshall, J.A. An outbreak of shigellosis in a child care centre. Commun. Dis. Intell. Q. Rep. 2004, 28, 225–229. [Google Scholar]
- Hunter, P.R.; Hutchings, P.G. Outbreak of Shigella sonnei dysentery on a long stay psychogeriatric ward. J. Hosp. Infect. 1987, 10, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Liu, M.C.; Ko, C.F.; Lu, C.H.; Tseng, Y.H. Molecular epidemiology of Shigella flexneri in a long-stay psychiatric nursing center during 2001 to 2003. J. Clin. Microbiol. 2005, 43, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Lederer, I.; Taus, K.; Allerberger, F.; Fenkart, S.; Spina, A.; Springer, B.; Schmid, D. Shigellosis in refugees, Austria, July to November 2015. Eurosurveillance 2015, 20, 30081. [Google Scholar] [CrossRef]
- Mellou, K.; Mandilara, G.; Chrysostomou, A.; Tryfinopoulou, K.; Sideroglou, T.; Karadimas, K.; Agiassoti, V.T.; Lamprou, D.; Zampeta, E.; Antoniou, G.; et al. Public health and clinical implications of multidrug-resistant shigellosis cases in a reception centre for refugees/migrants, Greece, October-December 2019. Eur. J. Public Health 2021, 31, 588–590. [Google Scholar] [CrossRef] [PubMed]
- Yeni, D.K.; Büyük, F.; Ashraf, A.; Shah, M.S.U.D. Tularemia: A re-emerging tick-borne infectious disease. Folia Microbiol. 2021, 66, 1–14. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Factsheet on Tularaemia. Available online: https://www.ecdc.europa.eu/en/tularaemia/facts (accessed on 20 August 2022).
- World Health Organization. Cholera. Available online: https://www.who.int/news-room/fact-sheets/detail/cholera (accessed on 20 August 2022).
- Lantagne, D.; Balakrish Nair, G.; Lanata, C.F.; Cravioto, A. The cholera outbreak in Haiti: Where and how did it begin? Curr. Top. Microbiol. Immunol. 2014, 379, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Halliez, M.C.; Buret, A.G. Extra-intestinal and long term consequences of Giardia duodenalis infections. World J. Gastroenterol. 2013, 19, 8974–8985. [Google Scholar] [CrossRef]
- Troeger, C.; Khalil, I.A.; Rao, P.C.; Cao, S.; Blacker, B.F.; Ahmed, T.; Armah, G.; Bines, J.E.; Brewer, T.G.; Colombara, D.V.; et al. Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea Among Children Younger Than 5 Years. JAMA Pediatr. 2018, 172, 958–965. [Google Scholar] [CrossRef]
- Hofmeister, M.G.; Foster, M.A.; Teshale, E.H. Epidemiology and Transmission of Hepatitis A Virus and Hepatitis E Virus Infections in the United States. Cold Spring Harb. Perspect. Med. 2019, 9, a033431. [Google Scholar] [CrossRef]
- Church, D.L. Major factors affecting the emergence and re-emergence of infectious diseases. Clin. Lab. Med. 2004, 24, 559–586. [Google Scholar] [CrossRef]
- Reyes, R.; Ahn, R.; Thurber, K.; Burke, T.F. Urbanization and Infectious Diseases: General Principles, Historical Perspectives, and Contemporary Challenges. In Challenges in Infectious Diseases. Emerging Infectious Diseases of the 21st Century; Fong, I., Ed.; Springer: New York, NY, USA, 2013; pp. 123–146. [Google Scholar] [CrossRef]
- Sáenz, R.; Bissell, R.A.; Paniagua, F. Post-disaster malaria in Costa Rica. Prehosp. Disaster Med. 1995, 10, 154–160. [Google Scholar] [CrossRef]
- Fakoorziba, M.R.; Baseri, A.; Eghbal, F.; Rezaee, S.; Azizi, K.; Moemenbellah-Fard, M.D. Post-earthquake outbreak of cutaneous leishmaniasis in a rural region of southern Iran. Ann. Trop. Med. Parasitol. 2011, 105, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, I.; Nakhaei, N.; Aflatoonian, M.; Parizi, M.H.; Fekri, A.; Safizadeh, H.; Shirzadi, M.; Gooya, M.; Khamesipour, A.; Nadim, A. Cutaneous leishmaniasis in Bam: A comparative evaluation of pre- and post-earthquake years (1999–2008). Iran J. Public Health 2011, 40, 49–56. [Google Scholar] [PubMed]
- Sharifi, I.; Poursmaelian, S.; Aflatoonian, M.R.; Ardakani, R.F.; Mirzaei, M.; Fekri, A.R.; Khamesipour, A.; Parizi, M.H.; Harandi, M.F. Emergence of a new focus of anthroponotic cutaneous leishmaniasis due to Leishmania tropica in rural communities of Bam district after the earthquake, Iran. Trop. Med. Int. Health 2011, 16, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Aflatoonian, M.R.; Sharifi, I.; Poursmaelian, S.; Hakimi-Parizi, M.; Ziaali, N. The emergence of anthroponotic cutaneous leishmaniasis following the earthquake in southern villages of Bam district, southeastern Iran, 2010. J. Arthropod. Borne Dis. 2013, 10, 8–14. [Google Scholar]
- Sharifi, I.; Aflatoonian, M.R.; Fekri, A.R.; Hakimi Parizi, M.; Aghaei Afshar, A.; Khosravi, A.; Sharifi, F.; Aflatoonian, B.; Khamesipour, A.; Dowlati, Y.; et al. A comprehensive review of cutaneous leishmaniasis in Kerman province, southeastern Iran-narrative review article. Iran. J. Public Health 2015, 44, 299–307. [Google Scholar]
- Aflatoonian, M.R.; Sharifi, I.; Aflatoonian, B.; Shirzadi, M.R.; Gouya, M.M.; Kermanizadeh, A. A Review of Impact of Bam Earthquake on Cutaneous Leishmaniasis and Status: Epidemic of Old Foci, Emergence of New Foci and Changes in Features of the Disease. J. Arthropod. Borne Dis. 2016, 10, 271–280. [Google Scholar]
- Zhang, S.; Lu, Z.; Liu, H.; Xiao, X.; Zhao, Z.; Bao, G.; Han, J.; Jing, T.; Chen, G. Incidence of Japanese encephalitis, visceral leishmaniasis and malaria before and after the Wenchuan earthquake, in China. Acta Trop. 2013, 128, 85–89. [Google Scholar] [CrossRef]
- Basnyat, B. Typhoid versus typhus fever in post-earthquake Nepal. Lancet Glob. Health 2016, 4, e516–e517. [Google Scholar] [CrossRef]
- Dhimal, M.; Dumre, S.P.; Sharma, G.N.; Khanal, P.; Ranabhat, K.; Shah, L.P.; Lal, B.K.; Jha, R.; Upadhyaya, B.P.; Acharya, B.; et al. An outbreak investigation of scrub typhus in Nepal: Confirmation of local transmission. BMC Infect. Dis. 2021, 21, 193. [Google Scholar] [CrossRef]
- Sorensen, C.J.; Borbor-Cordova, M.J.; Calvello-Hynes, E.; Diaz, A.; Lemery, J.; Stewart-Ibarra, A.M. Climate Variability, Vulnerability, and Natural Disasters: A Case Study of Zika Virus in Manabi, Ecuador Following the 2016 Earthquake. Geohealth 2017, 1, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Reina Ortiz, M.; Le, N.K.; Sharma, V.; Hoare, I.; Quizhpe, E.; Teran, E.; Naik, E.; Salihu, H.M.; Izurieta, R. Post-earthquake Zika virus surge: Disaster and public health threat amid climatic conduciveness. Sci. Rep. 2017, 7, 15408. [Google Scholar] [CrossRef] [PubMed]
- Vasquez, D.; Palacio, A.; Nuñez, J.; Briones, W.; Beier, J.C.; Pareja, D.C.; Tamariz, L. Impact of the 2016 Ecuador Earthquake on Zika Virus Cases. Am. J. Public Health. 2017, 107, 1137–1142. Available online: https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2017.303769 (accessed on 30 November 2022). [CrossRef] [PubMed]
- Pacheco Barzallo, D.; Pacheco Barzallo, A.; Narvaez, E. The 2016 Earthquake in Ecuador: Zika Outbreak after a Natural Disaster. Health Secur. 2018, 16, 127–134. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Scrub Typhus. Available online: https://www.cdc.gov/typhus/scrub/index.html (accessed on 20 August 2022).
- Desjeux, P. Leishmaniasis: Current situation and new perspectives. Comp. Immunol. Microbiol. Infect. Dis. 2004, 27, 305–318. [Google Scholar] [CrossRef]
- Esfandiarpour, I.; Dabiri, S.H. Treatment of cutaneous leishmaniasis recidivans with a combination of allopurinol and meglumine antimoniate: A clinical and histologic study. Int. J. Dermatol. 2007, 46, 848–852. [Google Scholar] [CrossRef]
- Reithinger, R.; Dujardin, J.C.; Louzir, H.; Pirmez, C.; Alexander, B.; Brooker, S. Cutaneous leishmaniasis. Lancet Infect. Dis. 2007, 7, 581–596. [Google Scholar] [CrossRef]
- Petersen, L.R.; Jamieson, D.J.; Honein, M.A. Zika Virus. N. Engl. J. Med. 2016, 375, 294–295. [Google Scholar] [CrossRef]
- Bayramgürler, D.; Bilen, N.; Namli, S.; Altinaş, L.; Apaydin, R. The effects of 17 August Marmara earthquake on patient admittances to our dermatology department. J. Eur. Acad. Dermatol. Venereol. 2002, 16, 249–252. [Google Scholar] [CrossRef]
- Keven, K.; Ates, K.; Sever, M.S.; Yenicesu, M.; Canbakan, B.; Arinsoy, T.; Ozdemir, N.; Duranay, M.; Altun, B.; Erek, E. Infectious complications after mass disasters: The Marmara earthquake experience. Scand. J. Infect. Dis. 2003, 35, 110–113. [Google Scholar] [CrossRef]
- Oncül, O.; Keskin, O.; Acar, H.V.; Küçükardali, Y.; Evrenkaya, R.; Atasoyu, E.M.; Top, C.; Nalbant, S.; Ozkan, S.; Emekdaş, G.; et al. Hospital-acquired infections following the 1999 Marmara earthquake. J. Hosp. Infect. 2002, 51, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.C.; Lee, T.S.; Lin, Y.M.; Shu, K.H. Clinical features and outcome of crush syndrome caused by the Chi-Chi earthquake. J. Formos Med. Assoc. 2002, 101, 249–256. [Google Scholar] [PubMed]
- Kiani, Q.H.; Amir, M.; Ghazanfar, M.A.; Iqbal, M. Microbiology of wound infections among hospitalised patients following the 2005 Pakistan earthquake. J. Hosp. Infect. 2009, 73, 71–78. [Google Scholar] [CrossRef]
- Hiransuthikul, N.; Tantisiriwat, W.; Lertutsahakul, K.; Vibhagool, A.; Boonma, P. Skin and soft-tissue infections among tsunami survivors in southern Thailand. Clin. Infect. Dis. 2005, 41, e93–e96. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Choi, C.P.; Eun, H.C.; Kwon, O.S. Skin problems after a tsunami. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 860–863. [Google Scholar] [CrossRef] [PubMed]
- Chambers, A.J.; Campion, M.J.; Courtenay, B.G.; Crozier, J.A.; New, C.H. Operation Sumatra Assist: Surgery for survivors of the tsunami disaster in Indonesia. ANZ J. Surg. 2006, 76, 39–42. [Google Scholar] [CrossRef]
- Fan, S.W. Clinical cases seen in tsunami hit Banda Aceh: From a primary health care perspective. Ann. Acad. Med. Singap. 2006, 35, 54–59. [Google Scholar]
- Aceh Epidemiology Group. Outbreak of tetanus cases following the tsunami in Aceh Province, Indonesia. Glob. Public Health 2006, 1, 173–177. [Google Scholar] [CrossRef]
- Jeremijenko, A.; McLaws, M.L.; Kosasih, H. A tsunami related tetanus epidemic in Aceh, Indonesia. Asia Pac. J. Public Health 2007, 19, 40–44. [Google Scholar] [CrossRef]
- Pascapurnama, D.N.; Murakami, A.; Chagan-Yasutan, H.; Hattori, T.; Sasaki, H.; Egawa, S. Prevention of Tetanus Outbreak Following Natural Disaster in Indonesia: Lessons Learned from Previous Disasters. Tohoku J. Exp. Med. 2016, 238, 219–227. [Google Scholar] [CrossRef]
- Sutiono, A.B.; Qiantori, A.; Suwa, H.; Ohta, T. Characteristic tetanus infection in disaster-affected areas: Case study of the Yogyakarta earthquakes in Indonesia. BMC Res. Notes 2009, 2, 34. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Wang, H.Y.; Zhong, H.J.; Zhou, L.; Jiang, D.M.; Du, D.Y.; Hu, P.; Jiang, J.X. The epidemiological analyses of trauma patients in Chongqing teaching hospitals following the Wenchuan earthquake. Injury 2009, 40, 488–492. [Google Scholar] [CrossRef]
- Kang, M.; Xie, Y.; Mintao, C.; Chen, Z.; Chen, H.; Fan, H.; Chen, W.; Guo, X. Antimicrobial susceptibility of clinical isolates from earthquake victims in Wenchuan. Clin. Microbiol. Infect. 2009, 15, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Tao, C.; Kang, M.; Chen, Z.; Xie, Y.; Fan, H.; Qin, L.; Ma, Y. Microbiologic study of the pathogens isolated from wound culture among Wenchuan earthquake survivors. Diagn Microbiol. Infect. Dis. 2009, 63, 268–270. [Google Scholar] [CrossRef] [PubMed]
- Ran, Y.-C.; Ao, X.-X.; Liu, L.; Fu, Y.-L.; Tuo, H.; Xu, F. Microbiological study of pathogenic bacteria isolated from paediatric wound infections following the 2008 Wenchuan earthquake. Scand. J. Infect. Dis. 2010, 42, 347–350. [Google Scholar] [CrossRef]
- Wang, T.; Li, D.; Xie, Y.; Kang, M.; Chen, Z.; Chen, H.; Fan, H.; Wang, L.; Tao, C. The microbiological characteristics of patients with crush syndrome after the Wenchuan earthquake. Scand. J. Infect. Dis. 2010, 42, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hao, P.; Lu, B.; Yu, H.; Huang, W.; Hou, H.; Dai, K. Causes of infection after earthquake, China, 2008. Emerg. Infect. Dis. 2010, 16, 974–975. [Google Scholar] [CrossRef]
- Chen, X.; Zhong, H.; Fu, P.; Hu, Z.; Qin, W.; Tao, Y. Infections in crush syndrome: A retrospective observational study after the Wenchuan earthquake. Emerg. Med. J. 2011, 28, 14–17. [Google Scholar] [CrossRef]
- Chen, E.; Deng, L.; Liu, Z.; Zhu, X.; Chen, X.; Tang, H. Management of gas gangrene in Wenchuan earthquake victims. J. Huazhong Univ. Sci. Technol. Med. Sci. 2011, 31, 83–87. [Google Scholar] [CrossRef]
- Liu, J.; Ma, L.; You, C. Analysis of scalp wound infections among craniocerebral trauma patients following the 2008 wenchuan earthquake. Turk. Neurosurg. 2012, 22, 27–31. [Google Scholar] [CrossRef]
- Zhang, B.; Liu, Z.; Lin, Z.; Zhang, X.; Fu, W. Microbiologic characteristics of pathogenic bacteriafrom hospitalized trauma patients who survivedWenchuan earthquake. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 2529–2535. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zeng, J.W.; Wang, G.L.; Tu, C.Q.; Huang, F.G.; Pei, F.X. Infectious complications in patients with crush syndrome following the Wenchuan earthquake. Chin. J. Traumatol. 2013, 16, 10–15. [Google Scholar] [PubMed]
- Miskin, I.N.; Nir-Paz, R.; Block, C.; Merin, O.; Burshtein, S.; Pirogovsky, S.; Halperin, T.; Schwartz, D.; Schwaber, M.J. Antimicrobial therapy for wound infections after catastrophic earthquakes. N. Engl. J. Med. 2010, 363, 2571–2573. [Google Scholar] [CrossRef] [PubMed]
- Firth, P.G.; Solomon, J.B.; Roberts, L.L.; Gleeson, T.D. Airway management of tetanus after the Haitian earthquake: New aspects of old observations. Anesth. Analg. 2011, 113, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Bekçibaşı, M.; Hoşoğlu, S.; Deveci, Ö.; Dayan, S. Therapy for wound infections after earthquakes requires inclusion of drugs targeting Gram-negative bacteria. Infect. Dis. 2017, 49, 862–864. [Google Scholar] [CrossRef]
- Lachish, T.; Halperin, T.; Snitser, O.; Kashat, L.; Merin, O.; Bader, T.; Rokney, A.; Schwartz, E.; Assous, M.V. The spectrum of bacteria and mechanisms of resistance identified from the casualties treated in the Israeli field hospital after the earthquake in Nepal, 2015: A retrospective analysis. Travel. Med. Infect. Dis. 2020, 37, 101707. [Google Scholar] [CrossRef]
- World Health Organization. Tetanus. Available online: https://www.who.int/news-room/fact-sheets/detail/tetanus (accessed on 20 August 2022).
- Afshar, M.; Raju, M.; Ansell, D.; Bleck, T.P. Narrative review: Tetanus-a health threat after natural disasters in developing countries. Ann. Intern. Med. 2011, 154, 329–335. [Google Scholar] [CrossRef]
- Sugunan, A.P.; Murhekar, M.V.; Naik, T.N.; Sehgal, S.C. Outbreak of rotaviral diarrhoea in a relief camp for tsunami victims at Car Nicobar Island, India. J. Public Health 2007, 29, 449–450. [Google Scholar] [CrossRef]
- Suzuki, M.; Uwano, C.; Ohrui, T.; Ebihara, T.; Yamasaki, M.; Asamura, T.; Tomita, N.; Kosaka, Y.; Furukawa, K.; Arai, H. Shelter-Acquired pneumonia after a catastrophic earthquake in Japan. J. Am. Geriatr. Soc. 2011, 59, 1968–1970. [Google Scholar] [CrossRef]
- Takahashi, H.; Fujimura, S.; Ubukata, S.; Sato, E.; Shoji, M.; Utagawa, M.; Kikuchi, T.; Watanabe, A. Pneumonia after earthquake, Japan, 2011. Emerg. Infect. Dis. 2012, 18, 1909–1911. [Google Scholar] [CrossRef]
- Daito, H.; Suzuki, M.; Shiihara, J.; Kilgore, P.E.; Ohtomo, H.; Morimoto, K.; Ishida, M.; Kamigaki, T.; Oshitani, H.; Hashizume, M.; et al. Impact of the Tohoku earthquake and tsunami on pneumonia hospitalisations and mortality among adults in northern Miyagi, Japan: A multicentre observational study. Thorax 2013, 68, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.C.; Malamud, B.D. Reviewing and visualizing the interactions of natural hazards. Rev. Geophys. 2014, 52, 680–722. [Google Scholar] [CrossRef]
- Gill, J.C.; Malamud, B.D. Hazard interactions and interaction networks (cascades) within multi-hazard methodologies. Earth Syst. Dyn. 2016, 7, 659–679. [Google Scholar] [CrossRef]
- Mavroulis, S.; Mavrouli, M.; Lekkas, E. Geological and hydrometeorological hazards and related disasters amid COVID-19 pandemic in Greece: Post-disaster trends and factors affecting the COVID-19 evolution in affected areas. Saf. Sci. 2021, 138, 105236. [Google Scholar] [CrossRef] [PubMed]
- Mavroulis, S.; Mavrouli, M.; Kourou, A.; Thoma, T.; Lekkas, E. Multi-Hazard Emergency Response for Geological Hazards Amid the Evolving COVID-19 Pandemic: Good Practices and Lessons Learned from Earthquake Disaster Management in Greece. Sustainability 2022, 14, 8486. [Google Scholar] [CrossRef]
- Mavroulis, S.; Mavrouli, M.; Carydis, P.; Agorastos, K.; Lekkas, E. The March 2021 Thessaly earthquakes and their impact through the prism of a multi-hazard approach in disaster management. Bull. Geol. Soc. Greece 2021, 58, 1–36. [Google Scholar] [CrossRef]
- Mavroulis, S.; Ilgac, M.; Tunçağ, M.; Lekkas, E.; Püskülcü, S.; Kourou, A.; Sextos, A.; Mavrouli, M.; Can, G.; Thoma, T.; et al. Emergency response, intervention, and societal recovery in Greece and Turkey after the 30th October 2020, MW = 7.0, Samos (Aegean Sea) earthquake. Bull. Earthq. Eng. 2022, 20, 7933–7955. [Google Scholar] [CrossRef]
- Chin, C.-S.; Sorenson, J.; Harris, J.B.; Robins, W.P.; Charles, R.C.; Jean-Charles, R.R.; Bullard, J.; Webster, D.R.; Kasarskis, A.; Peluso, P.; et al. The Origin of the Haitian Cholera Outbreak Strain. N. Engl. J. Med. 2011, 364, 33–42. [Google Scholar] [CrossRef]
- Piarroux, R.; Barrais, R.; Faucher, B.; Haus, R.; Piarroux, M.; Gaudart, J.; Magloire, R.; Raoult, D. Understanding the Cholera Epidemic, Haiti. Emerg. Infect. Dis. 2011, 17, 1161–1168. [Google Scholar] [CrossRef]
- Brown, C.; Ripp, J.; Kazura, J. Perspectives on Haiti Two Years after the Earthquake. Am. J. Trop. Med. Hyg. 2012, 86, 5–6. [Google Scholar] [CrossRef]
- Rempel, A. Examining Communicable Disease in the Context of Natural Disasters: Learning from the Haitian Earthquake to Establish Surveillance among Displaced Populations. Available online: https://med.stanford.edu/content/dam/sm/schoolhealtheval/documents/AnnieRempel_HumBio122PolicyBriefJun2015.pdf (accessed on 20 August 2022).
- Walton, D.A.; Ivers, L.C. Responding to Cholera in Post-Earthquake Haiti. N. Engl. J. Med. 2016, 364, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, J.; Luquero, F.; Francois, G.; Rousseau, C.; Caleo, G.; Ciglenecki, I.; Delacre, C.; Siddiqui, M.R.; Terzian, M.; Verhenne, L.; et al. Public Health Surveillance after the 2010 Haiti Earthquake: The Experience of Médecins Sans Frontières. PLoS Curr. Disasters 2013, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.C.; Velasco-Hernandez, J.; Min, K.D.; Leonel, D.G.; Baca-Carrasco, D.; Gompper, M.E.; Hartskeerl, R.; Munoz-Zanzi, C. The Use of Chemoprophylaxis after Floods to Reduce the Occurrence and Impact of Leptospirosis Outbreaks. Int. J. Environ. Res. Public Health. 2017, 14, 594. [Google Scholar] [CrossRef] [PubMed]
- Pearson, A.L.; Kingham, S.; Mitchell, P.; Apparicio, P. Exploring hotspots of pneumococcal pneumonia and potential impacts of ejecta dust exposure following the Christchurch earthquakes. Spat. Spatio-Temporal Epidemiol. 2013, 7, 1–9. [Google Scholar] [CrossRef]
- Kawano, T.; Tsugawa, Y.; Nishiyama, K.; Morita, H.; Yamamura, O.; Hasegawa, K. Shelter crowding and increased incidence of acute respiratory infection in evacuees following the Great Eastern Japan Earthquake and tsunami. Epidemiol. Infect. 2016, 144, 787–795. [Google Scholar] [CrossRef]
- United Nations High Commissioner for Refugees (UNHCR). Handbook for Emergencies, 3rd ed.; UNHCR: Geneva, Switzerland, 2007; 595p. [Google Scholar]
- Alexander, D. Disease Epidemiology and Earthquake Disaster: The Example of Southern Italy after the 23 November 1980 Earthquake. Sot. Sci. Med. 1982, 16, 1959–1969. [Google Scholar] [CrossRef]
- Brunton, C.; Humphrey, A.; Pink, R. The public health response to microbiological hazards after the Canterbury earthquakes. Pathology 2012, 44, S45. [Google Scholar] [CrossRef]



| Earthquake Occurrence (DD/MM/YYYY) | Earthquake Affected Area | Infectious Diseases (Causative Factors–Cases, Outbreaks, Epidemics) | References |
|---|---|---|---|
| 17/01/1994 | Northridge California, United States | Outbreak of coccidioidomycosis (Coccidiodes immitis), 203 cases (including 3 deaths) | [68] |
| Outbreak of coccidioidomycosis (C. immitis) | [69] | ||
| 17/01/1995 | Kobe, Japan | Increase in the number of patients with respiratory diseases by 4.5 times | [80] |
| 21/09/1999 | Chi-Chi, Taiwan | Acute respiratory infections | [81] |
| Upper respiratory tract infection | [82] | ||
| 13/01/2001 | El Salvador | Upper respiratory infections (30%) | [70] |
| Respiratory infections | [71] | ||
| 26/12/2003 | Bam, Iran | Respiratory infections (6.86% of the total population within 1 month) | [84] |
| Respiratory tract infections | [83] | ||
| 08/10/2005 | Kashmir, Pakistan | Viral upper respiratory tract infection (23%) | [87] |
| 12/05/2008 | Sichuan, China | Increase of tuberculosis cases in hospitals of the affected area | [101] |
| 30/09/2009 | Sumatra, Indonesia | Respiratory infections | [88] |
| 12/01/2010 | Haiti | Acute respiratory infection (16.3%) | [72] |
| Increase in tuberculosis in the affected population: 3-fold in a camp for internally displaced persons (693/100,000) and 5-fold in an urban slum (1165/100,000) | [75] | ||
| Tuberculosis | [76] | ||
| 11/03/2011 | Tōhoku, Japan | 43% of cases-community pneumonia (Streptococcus pneumoniae, Moraxella catarrhalis and Haemophilus influenzae) | [89] |
| 20/04/2013 | Lushan, China | Respiratory tract infections | [90] |
| Respiratory infection (45.7%) | [91] | ||
| 15/10/2013 | Bohol, Philippines | Acute respiratory infections | [92] |
| 476/3555 children: positive to tuberculin skin reaction–TST, 16 with active tuberculosis | [93] | ||
| 26/01/2014 03/02/2014 | Cephalonia, Greece | Increase of respiratory infection cases | [79] |
| 25/04/2015 | Gorkha, Nepal | Pneumonia and post-streptococcal glomerulonephritis: high incidence among children from affected areas | [98] |
| Upper respiratory tract infections | [95] | ||
| Infections of the respiratory tract (42.3%) | [96] | ||
| 1 case of tuberculous peritonitis (1 girl 14 years old with fever, abdominal pain and vomiting) | [99] | ||
| 14/04/2016, 16/04/2016 | Kumamoto, Japan | Upper respiratory infections | [100] |
| Earthquake Occurrence (DD/MM/YYYY) | Earthquake Affected Area | Infectious Diseases (Causative Factors–Cases, Outbreaks, Epidemics) | References |
|---|---|---|---|
| 23/11/1980 | Irpinia, Italy | 1 outbreak of gastroenteritis (39 cases, firefighters) 1 outbreak of viral hepatitis (6 cases, city of Potenza) | [102] |
| 17/08/1999 | Izmit, Turkey | Giardia lamblia and Enterobius vermicularis infections in children still living and studying in temporary settlements and schools even years after the earthquakes | [105] |
| Hepatitis A and E | [108] | ||
| Hepatitis A and E | [106] | ||
| Tularemia outbreak (Francisella tularensis, 5 cases) | [107] | ||
| A mild gastroenteritis outbreak among SAR personnel (two to three loose or watery stools accompanied by abdominal pain) | [103] | ||
| Current increase in diarrheal infections (Shigella) | [104] | ||
| 21/09/1999 | Chi-Chi, Taiwan | Acute gastroenteritis (15 shigellosis cases) | [81] |
| Acute gastroenteritis | [82] | ||
| 25/01/1999 | Armenia, Colombia | Giardiasis (Giardia lamblia) | [109] |
| 13/01/2001 | El Salvador | Gastrointestinal infections | [71] |
| 26/12/2003 | Bam, Iran | Gastrointestinal infections (0.81% of the total population within 1 month) | [84] |
| Diarrheal diseases | [83] | ||
| 26/12/2004 | Indonesia | Tsunami survivors: waterborne infections (85% of children under 5 years old: diarrhea, 100% of the population had no access to clean drinking water and sanitation systems). | [110] |
| 08/10/2005 | Kashmir, Pakistan | Rotavirus outbreak | [111] |
| Acute digestive disease (14.3%) | [87] | ||
| 06/04/2009 | L’Aquila, Italy | Salmonella enterica epidemic in children | [112] |
| 12/01/2010 | Haiti | Cholera and cholera-like disease | [77] |
| Cholera outbreak | [113] | ||
| 23/10/2011 09/11/2011 | Van, Turkey | Significantly higher prevalence of Helicobacter pylori in dyspeptic patients-disaster survivors compared to dyspeptic patients in the pre-disaster period | [114] |
| 26/01/2014 03/02/2014 | Cephalonia, Greece | Gastroenteritis outbreak (22 gastroenteritis cases among soldiers) | [79] |
| 25/04/2015 | Gorkha, Nepal | Gastrointestinal infections | [94,97] |
| Acute gastroenteritis: high incidence among children from affected areas | [98] | ||
| Cholera (Vibrio cholerae serogroup 01 Ogawa serotype) | [115] | ||
| Acute watery diarrhea (Vibrio cholerae): 169 cases, of which 150 were in the Kathmandu Valley | [116] | ||
| 14/04/2016, 16/04/2016 | Kumamoto, Japan | Gastrointestinal infections | [100] |
| Εarthquake Occurrence (DD/MM/YYYY) | Earthquake Affected Area | Infectious Diseases (Causative Factors–Cases, Outbreaks, Epidemics) | References |
|---|---|---|---|
| 22/04/1991 | Limon, Costa Rica | Malaria (Plasmodium falciparum) | [132] |
| 26/12/2003 | Bam, Iran | Cutaneous leishmaniasis (20,999 cases (1993–2012): 6731 before and 14,268 after the earthquake | [138] |
| Anthroponic cutaneous leishmaniasis: increase in annual incidence from 58.6 cases/100,000 in the 12 months before the earthquakes to 864 cases/100,000 in the following 12 months | [133] | ||
| Cutaneous leishmaniasis | [134,135,136,137] | ||
| 12/05/2008 | Sichuan, China | Visceral leishmaniasis | [139] |
| 12/01/2010 | Haiti | Suspected malaria (10.3%) | [72] |
| 11 laboratory-confirmed cases of P. falciparum malaria (7 US residents-emergency responders, 2 Haitians, 1 US traveler) | [73] | ||
| Malaria | [77] | ||
| P. falciparum malaria (76/255 patients) | [74] | ||
| 25/04/2015 | Gorkha, Nepal | Outbreak of scrub typhus (Orientia tsutsugamushi) | [140,141] |
| 16/04/2016 | Ecuador | Zika virus outbreak | [142,144,145] |
| Zika virus outbreak (89 cases in the pre-earthquake period-2103 in the post-earthquake period) | [143] |
| Εarthquake Occurrence (DD/MM/YYYY) | Earthquake-Affected Area | Infectious Diseases (Causative Factors/Cases, Outbreaks, Epidemics) | References |
|---|---|---|---|
| 17/08/1999 | Izmit, Turkey | Infections/infestations, cutaneous superficial fungal infections (Tinea pedis), cases of viral skin diseases, insect bites | [151] |
| Ιnfectious complications (wound infections): gram-negative bacteria (mainly Acinetobacter spp.), Staphylococcus spp. | [152] | ||
| Wound infections: Gram-negative bacteria (Acinetobacter baumanii, P. aeruginosa, Escherichia coli, Klebsiella pneumoniae, Stenotrophomonas maltophilia) and Staphylococcus spp. (630 injured) | [153] | ||
| 21/09/1999 | Chi-Chi, Taiwan | Wound infections—Crush syndrome | [154] |
| 26/12/2004 | Indonesia | Wound infections: tetanus (106 cases), Clostridium tetani | [162] |
| Ιnfections—infestations, traumatic skin lesions, and contact dermatitis | [157] | ||
| Wound infections (Aeromonas spp., E. coli, K. pneumoniae, P. aeruginosa, and Proteus spp.) | [156] | ||
| Skin and soft tissue infections | [158] | ||
| Ιnfected superficial wounds on the limbs and face (recurrence: necrosis of underlying tissues, need for repeated cleaning, and dressing of wounds) | [159] | ||
| Tetanus outbreak | [160,161] | ||
| 08/10/2005 | Kashmir, Pakistan | Gas gangrene of the limbs and tetanus requiring respiratory support (51 patients with tetanus, of whom 22 died) | [86] |
| Wound infections: P. aeruginosa, Enterobacter spp. and Acinetobacter spp. (multi-resistant strains) | [155] | ||
| 27/05/2006 | Yogyakarta, Indonesia | Wound infections: tetanus (71 cases) | [162] |
| Wound infections: tetanus (26 cases) | [163] | ||
| 12/05/2008 | Sichuan, China | Wound infections (E. coli, S. aureus, S. haemolyticus, A. baumanii, A. cloacae, P. aeruginosa, C-type chain coccus, and Bacillus aerogenes capsulatus), gas gangrene (Clostridium perfringens) | [164] |
| 67 probable cases (2.41%) of gas gangrene of which 5 were confirmed by culture (C. perfringens) | [171] | ||
| Crush syndrome–wound infections: A. baumanii, P. aeruginosa, E. cloacae, and E.coli | [170] | ||
| Wound infections: Gram-negative bacilli, Gram-positive bacteria, Candida spp., Gram-negative cocci, Clostridium sordelli | [165] | ||
| Skull wound infections: Gram-positive bacteria (S. aureus, S. epidermidis), Gram-negative bacteria (E. cloacae, K. pneumoniae, Serratia rubidaea) | [172] | ||
| Wound infections in 50 children: Gram-positive bacteria (16%), Gram-negative bacteria (82%) (A. baumannii, E. cloacae, P. aeruginosa), 1 month after the earthquake | [167] | ||
| Wound infections (24.4% Gram-positive bacteria: Staphylococcus aureus, −73.2% Gram-negative bacteria: Escherichia coli, Acinetobacter baumannii, Enterobacter cloacae, and P. aeruginosa) | [166] | ||
| Crush syndrome—wound infections: A. baumannii, E. coli, S. aureus, gas gangrene | [169] | ||
| Wound infections: Gram-negative bacteria | [168] | ||
| Wound infections: A. baumannii, Burkholderia cepacia, S. aureus, and Enterococcus spp. | [173] | ||
| Crush syndrome | [174] | ||
| 12/01/2010 | Haiti | Wound/skin infections | [77] |
| Wound infections (polymicrobial, 89% Gram-negative bacteria, antimicrobial resistant) | [175] | ||
| Wound infections: tetanus (2 cases) | [176] | ||
| 23/10/2011 09/11/2011 | Van, Turkey | Wound infections: Gram-negative aerobic bacteria and A. baumannii, P. aeruginosa, E. coli, and E. faecium | [177] |
| 20/04/2013 | Lushan, China | Intracranial infection (initial stage of hospitalization: S. aureus and E. coli—prolonged stay in ICU: A. baumannii and K. pneumoniae | [91] |
| 25/04/2015 | Gorkha, Nepal | 56 human losses: 68% Gram-negative bacilli (55%, Enterobacteriaceae) | [178] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mavrouli, M.; Mavroulis, S.; Lekkas, E.; Tsakris, A. The Impact of Earthquakes on Public Health: A Narrative Review of Infectious Diseases in the Post-Disaster Period Aiming to Disaster Risk Reduction. Microorganisms 2023, 11, 419. https://doi.org/10.3390/microorganisms11020419
Mavrouli M, Mavroulis S, Lekkas E, Tsakris A. The Impact of Earthquakes on Public Health: A Narrative Review of Infectious Diseases in the Post-Disaster Period Aiming to Disaster Risk Reduction. Microorganisms. 2023; 11(2):419. https://doi.org/10.3390/microorganisms11020419
Chicago/Turabian StyleMavrouli, Maria, Spyridon Mavroulis, Efthymios Lekkas, and Athanassios Tsakris. 2023. "The Impact of Earthquakes on Public Health: A Narrative Review of Infectious Diseases in the Post-Disaster Period Aiming to Disaster Risk Reduction" Microorganisms 11, no. 2: 419. https://doi.org/10.3390/microorganisms11020419
APA StyleMavrouli, M., Mavroulis, S., Lekkas, E., & Tsakris, A. (2023). The Impact of Earthquakes on Public Health: A Narrative Review of Infectious Diseases in the Post-Disaster Period Aiming to Disaster Risk Reduction. Microorganisms, 11(2), 419. https://doi.org/10.3390/microorganisms11020419







