Distribution and Drug Resistance of Bacterial Infection in Hospitalized Patients at the Respiratory Department before and after the COVID-19 Pandemic in Guangzhou, China
Abstract
:1. Introduction
2. Results
2.1. Demographic and Clinical Characteristics of Inpatients
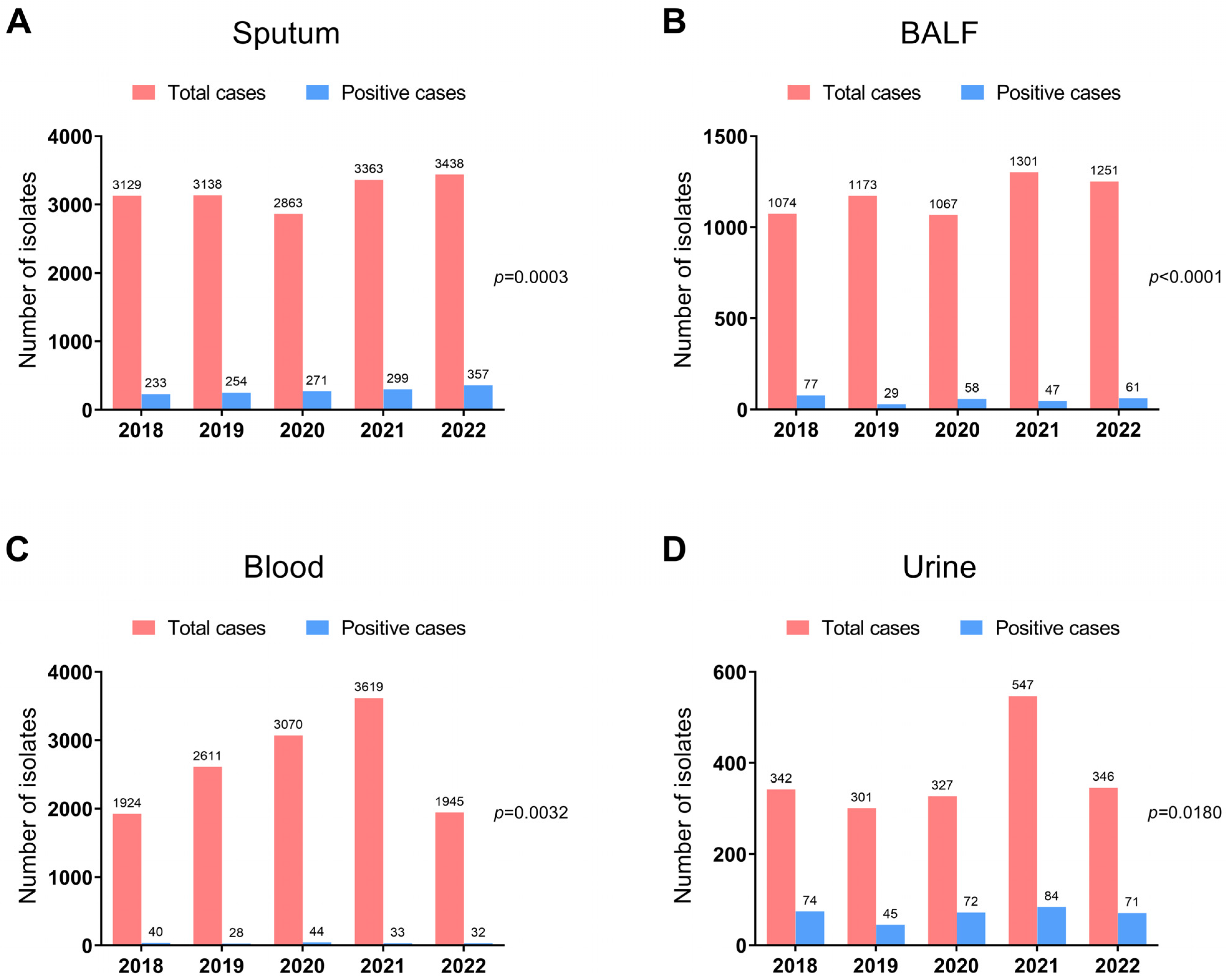
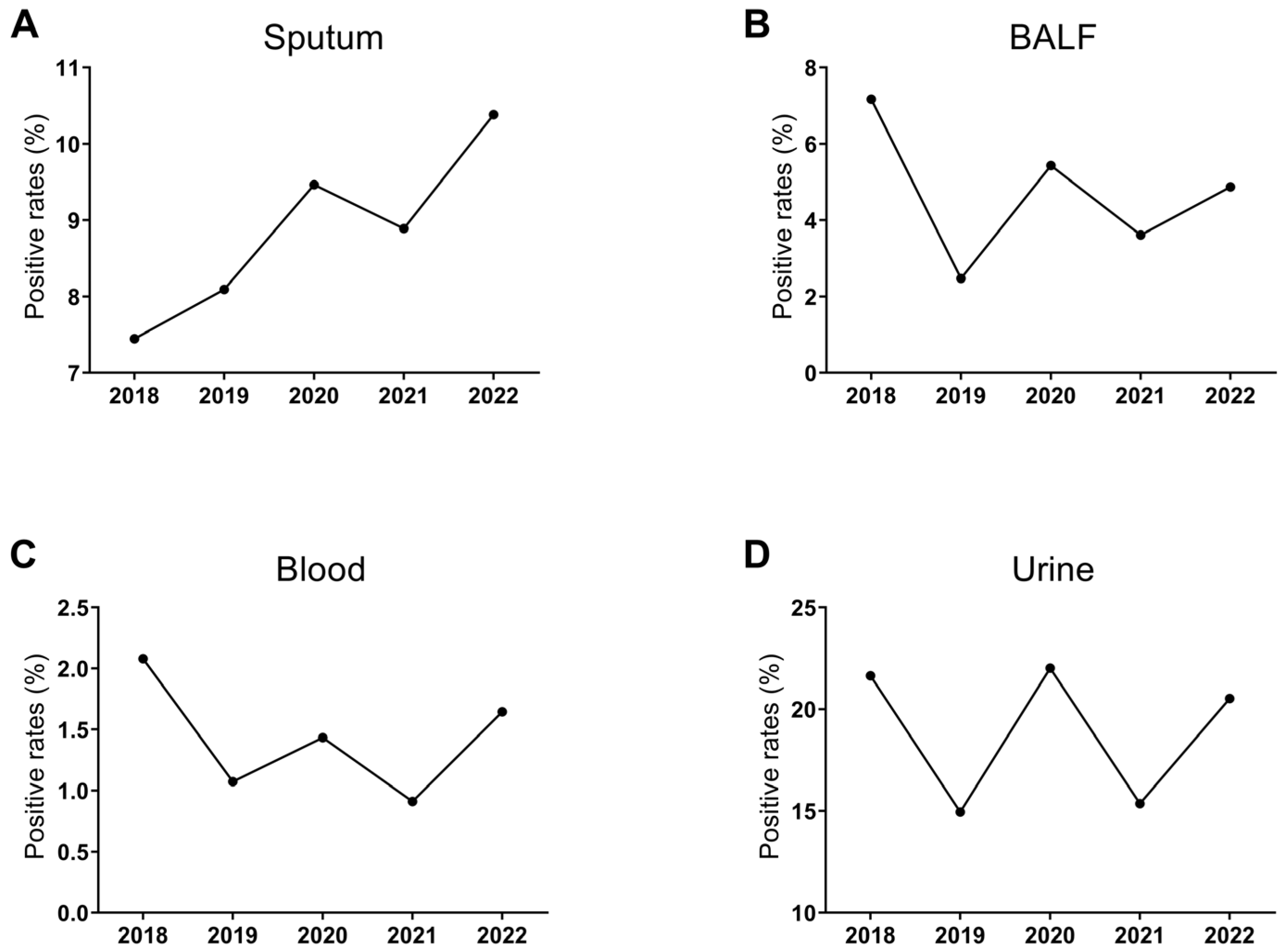
2.2. Bacterial Detection from 2018 to 2022
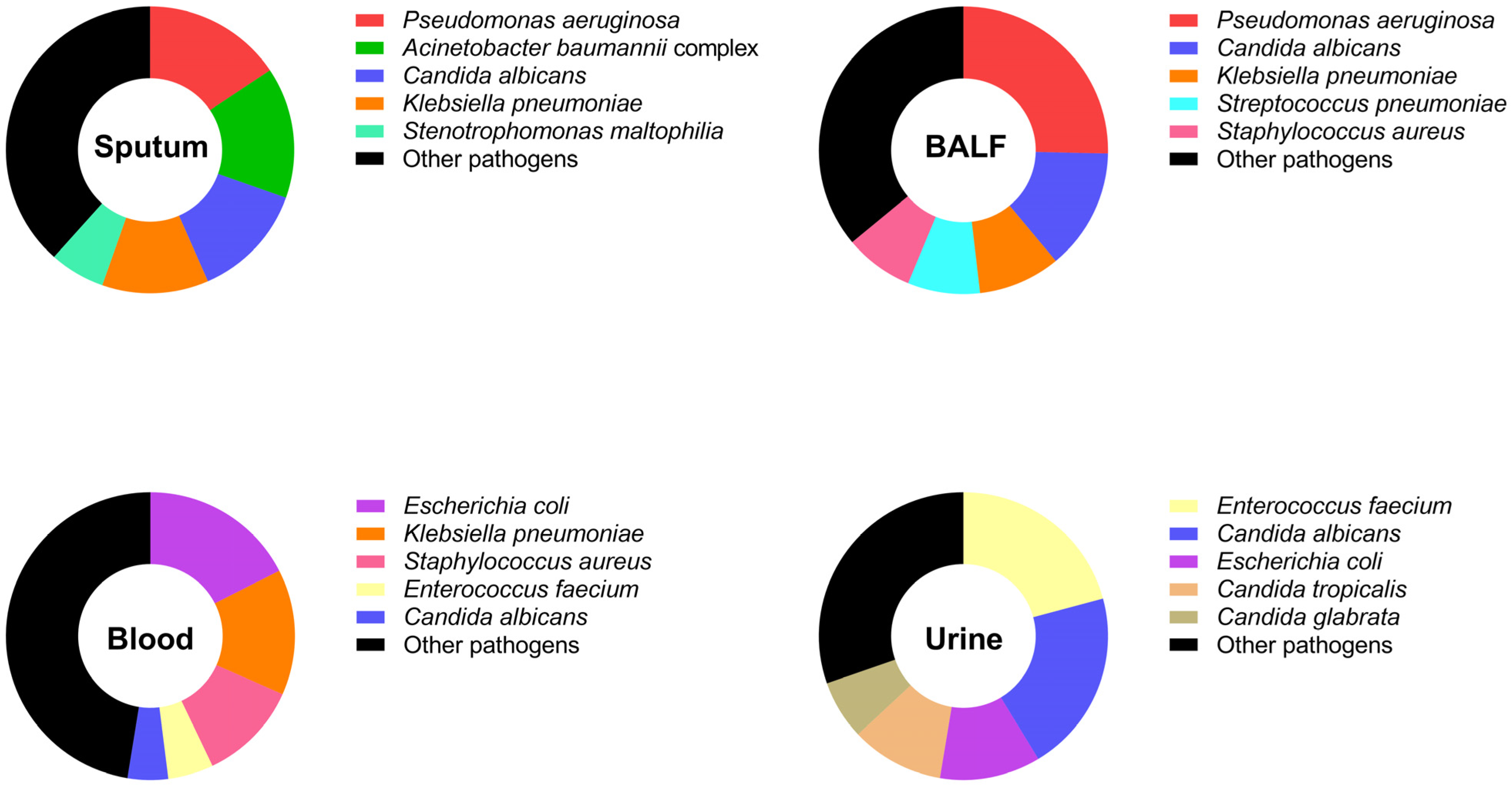
2.3. Identified Bacteria from Tested Specimens
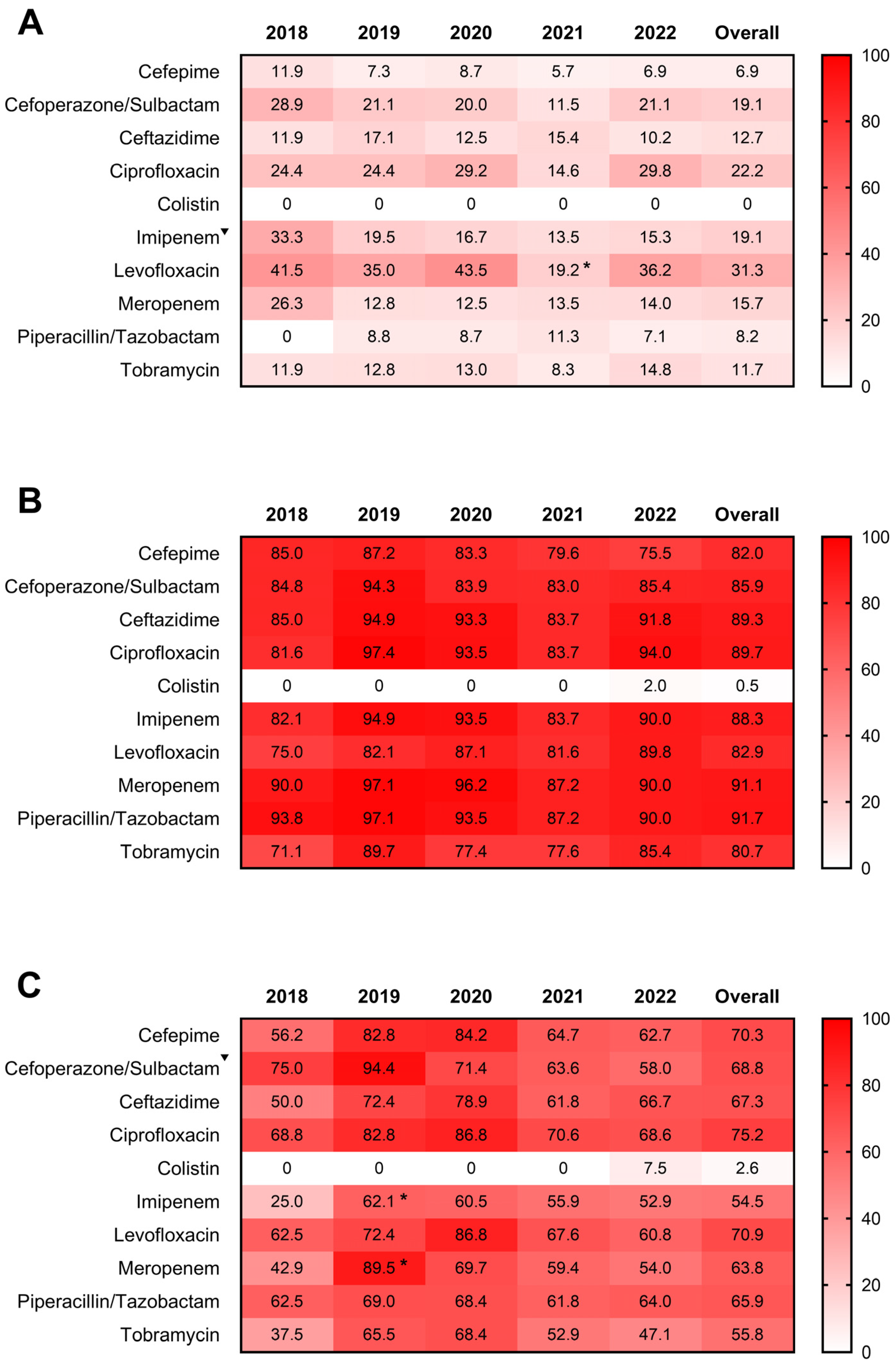
2.4. Antimicrobial Resistance Profiles of Detected Bacterial Isolates
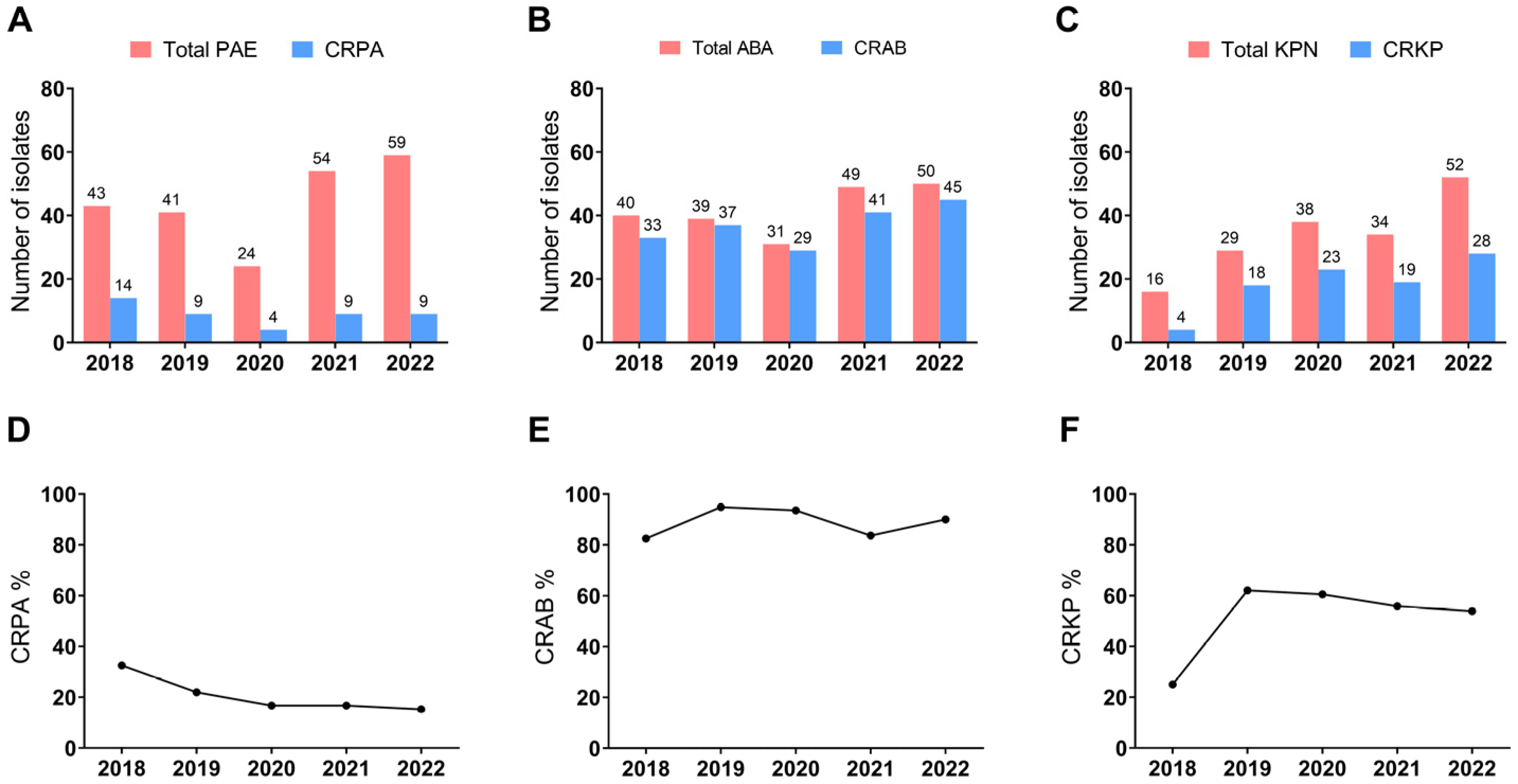
2.5. Prevalence of Carbapenem-Resistant Bacteria Infection
3. Discussion
4. Materials and Methods
4.1. Collection of Specimens for Bacterial Investigation
4.2. Antibiotic Susceptibility Testing
4.3. Analysis of Demographic and Clinical Data
4.4. Statistical Analysis
4.5. Ethics Statement
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2023. Available online: https://covid19.who.int/ (accessed on 17 August 2023).
- Lim, R.H.; Chow, A.; Ho, H.J. Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J. Infect. 2020, 81, e19–e21. [Google Scholar] [CrossRef]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef]
- Lai, C.C.; Chen, S.Y.; Ko, W.C.; Hsueh, P.R. Increased antimicrobial resistance during the COVID-19 pandemic. Int. J. Antimicrob. Agents 2021, 57, 106324. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Teich, V.D.; Klajner, S.; Almeida, F.A.S.; Dantas, A.C.B.; Laselva, C.R.; Torritesi, M.G.; Canero, T.R.; Berwanger, O.; Rizzo, L.V.; Reis, E.P.; et al. Epidemiologic and clinical features of patients with COVID-19 in Brazil. Einstein (Sao Paulo, Brazil) 2020, 18, eAO6022. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Moore, L.S.P.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A. Bacterial and Fungal Coinfection in Individuals With Coronavirus: A Rapid Review To Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Simeonova, M.; Leung, V.; Lo, J.; Kan, T.; Raybardhan, S.; Sapin, M.E.; Mponponsuo, K.; Farrell, A.; et al. Antimicrobial resistance in patients with COVID-19: A systematic review and meta-analysis. Lancet Microbe 2023, 4, e179–e191. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Baker, M.A.; Sands, K.E.; Huang, S.S.; Kleinman, K.; Septimus, E.J.; Varma, N.; Blanchard, J.; Poland, R.E.; Coady, M.H.; Yokoe, D.S.; et al. The Impact of Coronavirus Disease 2019 (COVID-19) on Healthcare-Associated Infections. Clin. Infect. Dis. 2022, 74, 1748–1754. [Google Scholar] [CrossRef]
- Amarsy, R.; Trystram, D.; Cambau, E.; Monteil, C.; Fournier, S.; Oliary, J.; Junot, H.; Sabatier, P.; Porcher, R.; Robert, J.; et al. Surging bloodstream infections and antimicrobial resistance during the first wave of COVID-19: A study in a large multihospital institution in the Paris region. Int. J. Infect. Dis. 2022, 114, 90–96. [Google Scholar] [CrossRef]
- Lemenand, O.; Coeffic, T.; Thibaut, S.; Colomb Cotinat, M.; Caillon, J.; Birgand, G.; Clinical Laboratories of PRIMO Network. Nantes, France. Decreasing proportion of extended-spectrum beta-lactamase among E. coli infections during the COVID-19 pandemic in France. J. Infect. 2021, 83, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Duverger, C.; Monteil, C.; Souyri, V.; Fournier, S. AP-HP Infection Prevention and Control Teams. Decrease of carbapenemase-producing Enterobacteriaceae incidence during the first year of the COVID-19 pandemic. J. Infect. 2022, 85, 90–122. [Google Scholar] [CrossRef]
- Denissen, J.; Reyneke, B.; Waso-Reyneke, M.; Havenga, B.; Barnard, T.; Khan, S.; Khan, W. Prevalence of ESKAPE pathogens in the environment: Antibiotic resistance status, community-acquired infection and risk to human health. Int. J. Hyg. Environ. Health 2022, 244, 114006. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 LRI Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2017, 17, 1133–1161. [Google Scholar] [CrossRef]
- Nordmann, P.; Poirel, L. Epidemiology and Diagnostics of Carbapenem Resistance in Gram-negative Bacteria. Clin. Infect. Dis. 2019, 69 (Suppl. S7), S521–S528. [Google Scholar] [CrossRef] [PubMed]
- Budden, K.F.; Shukla, S.D.; Rehman, S.F.; Bowerman, K.L.; Keely, S.; Hugenholtz, P.; Armstrong-James, D.P.H.; Adcock, I.M.; Chotirmall, S.H.; Chung, K.F.; et al. Functional effects of the microbiota in chronic respiratory disease. Lancet Respir. Med. 2019, 7, 907–920. [Google Scholar] [CrossRef]
- Kollef, M.H.; Torres, A.; Shorr, A.F.; Martin-Loeches, I.; Micek, S.T. Nosocomial Infection. Crit. Care Med. 2021, 49, 169–187. [Google Scholar] [CrossRef]
- Network CAS. China Antimicrobial Surveillance Network. 2022. Available online: http://www.chinets.com/Data/AntibioticDrugFast (accessed on 21 August 2023).
- Daoud, Z.; Salem Sokhn, E.; Masri, K.; Matar, G.M.; Doron, S. Escherichia coli Isolated from Urinary Tract Infections of Lebanese Patients between 2005 and 2012: Epidemiology and Profiles of Resistance. Front. Med. 2015, 2, 26. [Google Scholar]
- Delcaru, C.; Podgoreanu, P.; Alexandru, I.; Popescu, N.; Măruţescu, L.; Bleotu, C.; Mogoşanu, G.D.; Chifiriuc, M.C.; Gluck, M.; Lazăr, V. Antibiotic Resistance and Virulence Phenotypes of Recent Bacterial Strains Isolated from Urinary Tract Infections in Elderly Patients with Prostatic Disease. Pathogens 2017, 6, 22. [Google Scholar] [CrossRef]
- Routh, J.C.; Alt, A.L.; Ashley, R.A.; Kramer, S.A.; Boyce, T.G. Increasing prevalence and associated risk factors for methicillin resistant Staphylococcus aureus bacteriuria. J. Urol. 2009, 181, 1694–1698. [Google Scholar] [CrossRef]
- Das, R.; Perrelli, E.; Towle, V.; van Ness, P.H.; Juthani-Mehta, M. Antimicrobial susceptibility of bacteria isolated from urine samples obtained from nursing home residents. Infect. Control Hosp. Epidemiol. 2009, 30, 1116–1119. [Google Scholar] [CrossRef]
- Bazaid, A.S.; Barnawi, H.; Qanash, H.; Alsaif, G.; Aldarhami, A.; Gattan, H.; Alharbi, B.; Alrashidi, A.; Al-Soud, W.A.; Moussa, S.; et al. Bacterial Coinfection and Antibiotic Resistance Profiles among Hospitalised COVID-19 Patients. Microorganisms 2022, 10, 495. [Google Scholar] [CrossRef]
- Yang, S.; Hua, M.; Liu, X.; Du, C.; Pu, L.; Xiang, P.; Wang, L.; Liu, J. Bacterial and fungal co-infections among COVID-19 patients in intensive care unit. Microbes. Infect. 2021, 23, 104806. [Google Scholar] [CrossRef]
- Wei, X.L.; Zeng, Q.L.; Xie, M.; Bao, Y. Pathogen Distribution, Drug Resistance Risk Factors, and Construction of Risk Prediction Model for Drug-Resistant Bacterial Infection in Hospitalized Patients at the Respiratory Department During the COVID-19 Pandemic. Infect. Drug Resist. 2023, 16, 1107–1121. [Google Scholar] [CrossRef]
- Lyu, J.; Chen, H.; Bao, J.; Liu, S.; Chen, Y.; Cui, X.; Guo, C.; Gu, B.; Li, L. Clinical Distribution and Drug Resistance of Pseudomonas aeruginosa in Guangzhou, China from 2017 to 2021. J. Clin. Med. 2023, 12, 1189. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, N.; Duran, N.; Ay, E.; Cimen, F.; Tek, E. Genotyping, drug resistance and virulence factors of Candida species isolated from patients using long-term inhaled steroids. Int. J. Clin. Pract. 2021, 75, e14820. [Google Scholar] [CrossRef]
- Zhou, J.; Zhao, P.; Nie, M.; Gao, K.; Yang, J.; Sun, J. Changes of Haemophilus influenzae infection in children before and after the COVID-19 pandemic, Henan, China. J. Infect. 2023, 86, 66–117. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Ye, T.; Zhong, H.; Luo, Y.; Xu, J.; Zhang, Q.; Luo, X.; Wang, Q.; Zhang, L.; Song, P.; et al. Distribution and Drug Resistance of Bacterial Pathogens Associated with Lower Respiratory Tract Infection in Children and the Effect of COVID-19 on the Distribution of Pathogens. Can. J. Infect. Dis. Med. Microbiol. 2022, 2022, 1181283. [Google Scholar] [CrossRef]
- McTaggart, L.R.; Cronin, K.; Seo, C.Y.; Wilson, S.; Patel, S.N.; Kus, J.V. Increased Incidence of Invasive Haemophilus influenzae Disease Driven by Non-Type B Isolates in Ontario, Canada, 2014 to 2018. Microbiol. Spectr. 2021, 9, e0080321. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yu, Z.; Li, M.; Sun, H. Changes of Acinetobacter baumannii infections in children before and after the COVID-19 pandemic in Zhengzhou, China. J. Infect. 2023, 86, 154–225. [Google Scholar] [CrossRef]
- Li, Y.; Guo, Y.; Duan, Y. Changes in Streptococcus pneumoniae infection in children before and after the COVID-19 pandemic in Zhengzhou, China. J. Infect. 2022, 85, e80–e81. [Google Scholar] [CrossRef]
- Hu, F.; Guo, Y.; Zhu, D.; Wang, F.; Jiang, X.; Xu, C.; Zhang, X.; Zhang, Z.; Ji, P.; Xie, Y.; et al. CHINET surveillance of antimicrobial resistance among the bacterial isolates in 2021. Chin. J. Infect. Chemother. 2022, 22, 521–530. (In Chinese) [Google Scholar]
- Polemis, M.; Mandilara, G.; Pappa, O.; Argyropoulou, A.; Perivolioti, E.; Koudoumnakis, N.; Pournaras, S.; Vasilakopoulou, A.; Vourli, S.; Katsifa, H.; et al. COVID-19 and Antimicrobial Resistance: Data from the Greek Electronic System for the Surveillance of Antimicrobial Resistance-WHONET-Greece (January 2018–March 2021). Life 2021, 11, 996. [Google Scholar] [CrossRef] [PubMed]
- Said, K.B.; Alsolami, A.; Khalifa, A.M.; Khalil, N.A.; Moursi, S.; Osman, A.; Fahad, D.; Rakha, E.; Rashidi, M.; Moussa, S.; et al. A Multi-Point Surveillance for Antimicrobial Resistance Profiles among Clinical Isolates of Gram-Negative Bacteria Recovered from Major Ha’il Hospitals, Saudi Arabia. Microorganisms 2021, 9, 2024. [Google Scholar] [CrossRef] [PubMed]
- Karataş, M.; Yaşar-Duman, M.; Tünger, A.; Çilli, F.; Aydemir, Ş.; Özenci, V. Secondary bacterial infections and antimicrobial resistance in COVID-19: Comparative evaluation of pre-pandemic and pandemic-era, a retrospective single center study. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 51. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Nation, R.L.; Turnidge, J.D.; Milne, R.W.; Coulthard, K.; Rayner, C.R.; Paterson, D.L. Colistin: The re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect. Dis. 2006, 6, 589–601. [Google Scholar] [CrossRef]
- World Health Organization. Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- O’Toole, R.F. The interface between COVID-19 and bacterial healthcare-associated infections. Clin. Microbiol. Infect. 2021, 27, 1772–1776. [Google Scholar] [CrossRef]
- Su, Z.; Huang, B.; Mu, Q.; Wen, D. Evaluating the Potential Antibiotic Resistance Status in Environment Based on the Trait of Microbial Community. Front. Microbiol. 2020, 11, 575707. [Google Scholar] [CrossRef]
- Shang, H.; Wang, Y.; Shen, Z. National Guidelines for Clinical Laboratory Practice; People’s Medical Publishing House: Beijing, China, 2014; pp. 717–720. (In Chinese) [Google Scholar]
- M100; Performance Standards for Antimicrobial Susceptibility Testing. 32st ed, Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2022.
| 2018 | 2019 | 2020 | 2021 | 2022 | Total | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 2201 | 2228 | 1776 | 2189 | 2097 | 10,491 |
| Female | 1244 | 1298 | 934 | 1074 | 1032 | 5582 |
| Age | ||||||
| <15 | 7 | 15 | 4 | 3 | 3 | 32 |
| 15–24 | 116 | 101 | 75 | 70 | 50 | 412 |
| 25–34 | 127 | 162 | 81 | 92 | 92 | 554 |
| 35–44 | 168 | 180 | 118 | 128 | 113 | 707 |
| 45–54 | 319 | 315 | 294 | 351 | 332 | 1611 |
| 55–64 | 743 | 769 | 572 | 704 | 603 | 3391 |
| >64 | 1965 | 1984 | 1566 | 1915 | 1936 | 9366 |
| Co-morbidities | ||||||
| Hypertension | 1466 | 1590 | 1137 | 1316 | 1306 | 6815 |
| Diabetes | 698 | 639 | 546 | 579 | 582 | 3044 |
| COPD | 776 | 811 | 551 | 764 | 693 | 3595 |
| Asthma | 150 | 172 | 115 | 94 | 152 | 683 |
| Pathogen | 2018 (n = 233) | 2019 (n = 254) | 2020 (n = 271) | 2021 (n = 299) | 2022 (n = 357) |
|---|---|---|---|---|---|
| Pseudomonas aeruginosa | 43 (18.45%) | 41 (16.14%) | 24 (8.86%) * | 54 (18.06%) | 59 (16.53%) |
| Acinetobacter baumannii complex | 40 (17.17%) | 39 (15.35%) | 31 (11.44%) | 49 (16.39%) | 50 (14.01%) |
| Candida albicans | 41 (17.60%) | 25 (9.84%) * | 29 (10.70%) | 38 (12.71%) | 51 (14.29%) |
| Klebsiella pneumoniae | 16 (6.87%) | 29 (11.42%) | 38 (14.02%) * | 34 (11.37%) | 52 (14.57%) |
| Stenotrophomonas maltophilia | 9 (3.86%) | 9 (3.54%) | 21 (7.75%) * | 28 (9.36%) | 21 (5.88%) |
| Haemophilus influenzae | 23 (9.87%) | 35 (13.78%) | 11 (4.06%) *** | 8 (2.68%) | 8 (2.24%) |
| Streptococcus pneumoniae | 20 (8.58%) | 11 (4.33%) | 11 (4.06%) * | 17 (5.69%) | 14 (3.92%) |
| Staphylococcus aureus | 8 (3.43%) | 7 (2.76%) | 4 (1.48%) | 11 (3.68%) | 32 (8.96%) |
| Burkholderia cepacia complex | 13 (5.58%) | 6 (2.36%) | 22 (8.12%) | 5 (1.67%) | 6 (1.68%) |
| Moraxella catarrhalis | 8 (3.43%) | 12 (4.72%) | 4 (1.48%) | 11 (3.68%) | 7 (1.96%) |
| Escherichia coli | 4 (1.72%) | 8 (3.15%) | 5 (1.84%) | 6 (2.01%) | 9 (2.52%) |
| Other pathogens | 8 (3.43%) | 32 (12.60%) | 71 (26.20%) | 38 (12.71%) | 48 (13.45%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hao, L.; Yang, X.; Chen, H.; Wei, S.; Xu, B.; Zhao, Z. Distribution and Drug Resistance of Bacterial Infection in Hospitalized Patients at the Respiratory Department before and after the COVID-19 Pandemic in Guangzhou, China. Microorganisms 2023, 11, 2542. https://doi.org/10.3390/microorganisms11102542
Hao L, Yang X, Chen H, Wei S, Xu B, Zhao Z. Distribution and Drug Resistance of Bacterial Infection in Hospitalized Patients at the Respiratory Department before and after the COVID-19 Pandemic in Guangzhou, China. Microorganisms. 2023; 11(10):2542. https://doi.org/10.3390/microorganisms11102542
Chicago/Turabian StyleHao, Ling, Xiao Yang, Huiling Chen, Shuquan Wei, Banglao Xu, and Ziwen Zhao. 2023. "Distribution and Drug Resistance of Bacterial Infection in Hospitalized Patients at the Respiratory Department before and after the COVID-19 Pandemic in Guangzhou, China" Microorganisms 11, no. 10: 2542. https://doi.org/10.3390/microorganisms11102542
APA StyleHao, L., Yang, X., Chen, H., Wei, S., Xu, B., & Zhao, Z. (2023). Distribution and Drug Resistance of Bacterial Infection in Hospitalized Patients at the Respiratory Department before and after the COVID-19 Pandemic in Guangzhou, China. Microorganisms, 11(10), 2542. https://doi.org/10.3390/microorganisms11102542






