Identification and Characterisation of Nontuberculous Mycobacteria in African Buffaloes (Syncerus caffer), South Africa
Abstract
1. Introduction
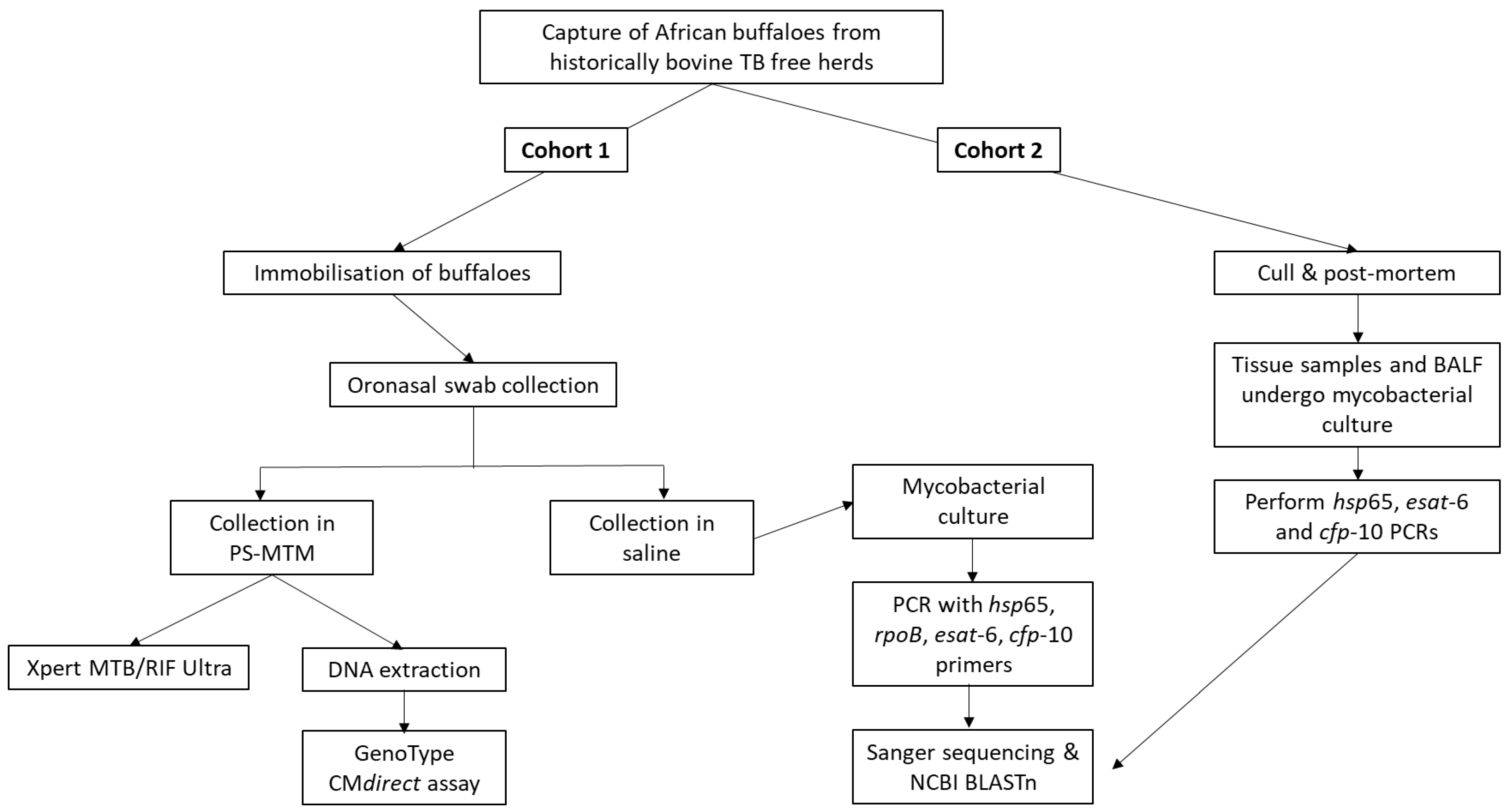
2. Materials and Methods
2.1. Animals and Sample Collection
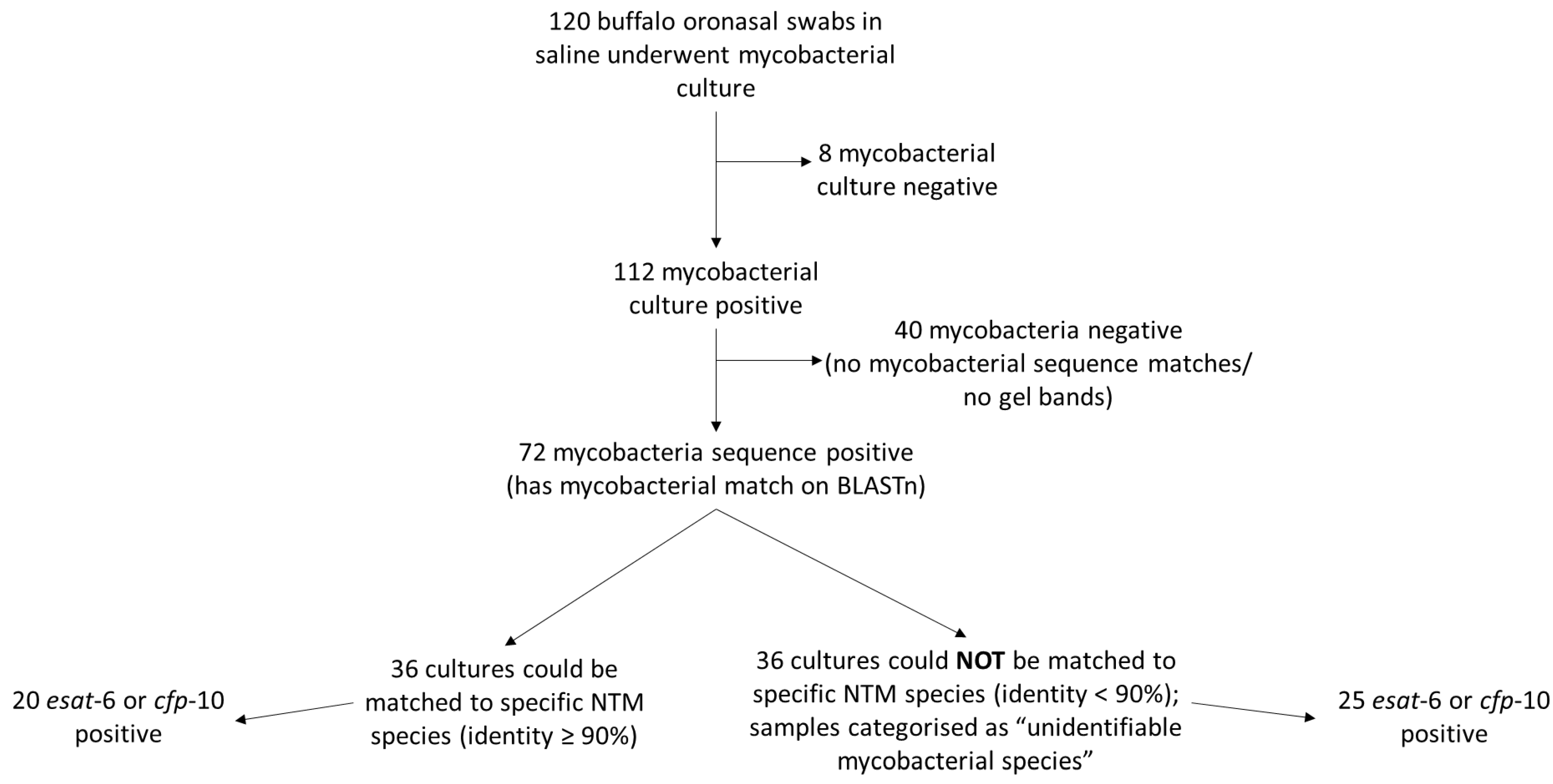
2.2. Characterisation of NTMs from Mycobacterial Cultures
2.3. Characterisation of NTMs Directly from Oronasal Swabs
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scherrer, S.; Landolt, P.; Friedel, U.; Stephan, R. Distribution and Expression of Esat-6 and Cfp-10 in Non-Tuberculous Mycobacteria Isolated from Lymph Nodes of Slaughtered Cattle in Switzerland. J. Vet. Diagn. Investig. 2019, 31, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Zulu, M.; Monde, N.; Nkhoma, P.; Malama, S.; Munyeme, M. Nontuberculous Mycobacteria in Humans, Animals, and Water in Zambia: A Systematic Review. Front. Trop. Dis. 2021, 2, 679501. [Google Scholar] [CrossRef]
- Fedrizzi, T.; Meehan, C.J.; Grottola, A.; Giacobazzi, E.; Fregni Serpini, G.; Tagliazucchi, S.; Fabio, A.; Bettua, C.; Bertorelli, R.; De Sanctis, V.; et al. Genomic Characterization of Nontuberculous Mycobacteria. Sci. Rep. 2017, 7, 45258. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.; Reischl, U.; Streubel, A.; Naumann, L.; Kroppenstedt, R.M.; Habicht, M.; Fischer, M.; Mauch, H. Novel Diagnostic Algorithm for Identification of Mycobacteria Using Genus-Specific Amplification of the 16S-23S rRNA Gene Spacer and Restriction Endonucleases. J. Clin. Microbiol. 2000, 38, 1094. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Huang, L.; Cai, M.; Wang, W.; Shi, X.; Chen, W. Characterization of Non-Tuberculous Mycobacterial Pulmonary Disease in Nanjing District of China. BMC Infect. Dis. 2019, 19, 764. [Google Scholar] [CrossRef]
- Vordermeier, H.M.; Brown, J.; Cockle, P.J.; Franken, W.P.J.; Arend, S.M.; Ottenhoff, T.H.M.; Jahans, K.; Hewinson, R.G. Assessment of Cross-Reactivity between Mycobacterium bovis and M. kansasii ESAT-6 and CFP-10 at the T-Cell Epitope Level. Clin. Vaccine Immunol. 2007, 14, 1203–1209. [Google Scholar] [CrossRef]
- Rónai, Z.; Eszterbauer, E.; Csivincsik, A.; Guti, C.F.; Dencső, L.; Jánosi, S. Dán Detection of Wide Genetic Diversity and Several Novel Strains among Non-Avium Nontuberculous Mycobacteria Isolated from Farmed and Wild Animals in Hungary. J. Appl. Microbiol. 2016, 121, 41–54. [Google Scholar] [CrossRef]
- Coad, M.; Doyle, M.; Steinbach, S.; Gormley, E.; Vordermeier, M.; Jones, G. Simultaneous Measurement of Antigen-Induced CXCL10 and IFN-γ Enhances Test Sensitivity for Bovine TB Detection in Cattle. Vet. Microbiol. 2019, 230, 1–6. [Google Scholar] [CrossRef]
- de la Rua-Domenech, R.; Goodchild, A.T.; Vordermeier, H.M.; Hewinson, R.G.; Christiansen, K.H.; Clifton-Hadley, R.S. Ante Mortem Diagnosis of Tuberculosis in Cattle: A Review of the Tuberculin Tests, γ-Interferon Assay and Other Ancillary Diagnostic Techniques. Res. Vet. Sci. 2006, 81, 190–210. [Google Scholar] [CrossRef]
- De Vos, V.; Bengis, R.G.; Kriek, N.P.J.; Michel, A.; Keet, D.F.; Raath, J.P.; Huchzermeyer, H.F.K.A. The Epidemiology of Tuberculosis in Free-Ranging African Buffalo (Syncerus Caffer) in the Kruger National Park, South Africa. Onderstepoort J. Vet. Res. 2001, 68, 119–130. [Google Scholar]
- Michel, A.; Bengis, R.; Keet, D.; Hofmeyr, M.; de Klerk, L.; Cross, P.; Jolles, A.; Cooper, D.; Whyte, I.; Buss, P.; et al. Wildlife Tuberculosis in South African Conservation Areas: Implications and Challenges. Vet. Microbiol. 2006, 112, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Arnot, L.F.; Michel, A. Challenges for Controlling Bovine Tuberculosis in South Africa. Onderstepoort J. Vet. Res. 2020, 87, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Parsons, S.D.C.; Cooper, D.; McCall, A.J.; McCall, W.A.; Streicher, E.M.; le Maitre, N.C.; Müller, A.; Gey van Pittius, N.C.; Warren, R.M.; van Helden, P.D. Modification of the QuantiFERON-TB Gold (In-Tube) Assay for the Diagnosis of Mycobacterium bovis Infection in African Buffaloes (Syncerus caffer). Vet. Immunol. Immunopathol. 2011, 142, 113–118. [Google Scholar] [CrossRef]
- Clarke, C.; Cooper, D.V.; Miller, M.A.; Goosen, W.J. Detection of Mycobacterium Tuberculosis Complex DNA in Oronasal Swabs from Infected African Buffaloes (Syncerus caffer). Sci. Rep. 2022, 12, 1834. [Google Scholar] [CrossRef] [PubMed]
- Goosen, W.J.; Miller, M.A.; Chegou, N.N.; Cooper, D.; Warren, R.M.; van Helden, P.D.; Parsons, S.D.C. Agreement between Assays of Cell-Mediated Immunity Utilizing Mycobacterium bovis-Specific Antigens for the Diagnosis of Tuberculosis in African Buffaloes (Syncerus caffer). Vet. Immunol. Immunopathol. 2014, 160, 133–138. [Google Scholar] [CrossRef]
- Adékambi, T.; Colson, P.; Drancourt, M. RpoB-Based Identification of Nonpigmented and Late-Pigmenting Rapidly Growing Mycobacteria. J. Clin. Microbiol. 2003, 41, 5699–5708. [Google Scholar] [CrossRef]
- Telenti, A.; Marchesi, F.; Balz, M.; Bally, F.; Bottger, E.C.; Bodmer, T. Rapid Identification of Mycobacteria to the Species Level by Polymerase Chain Reaction and Restriction Enzyme Analysis. J. Clin. Microbiol. 1993, 31, 175. [Google Scholar] [CrossRef]
- Van Ingen, J.; De Zwaan, R.; Dekhuijzen, R.; Boeree, M.; Van Soolingen, D. Region of Difference 1 in Nontuberculous Mycobacterium Species Adds a Phylogenetic and Taxonomical Character. J. Bacteriol. 2009, 191, 5865–5867. [Google Scholar] [CrossRef]
- Arend, S.M.; De Haas, P.; Leyten, E.; Rosenkrands, I.; Rigouts, L.; Andersen, P.; Mijs, W.; Van Dissel, J.T.; Van Soolingen, D. ESAT-6 and CFP-10 in Clinical versus Environmental Isolates of Mycobacterium kansasii. J. Infect. Dis. 2005, 191, 1301–1310. [Google Scholar] [CrossRef][Green Version]
- Warren, R.M.; Gey Van Pittius, N.C.; Barnard, M.; Hesseling, A.; Engelke, E.; De Kock, M.; Gutierrez, M.C.; Chege, G.K.; Victor, T.C.; Hoal, E.G.; et al. Differentiation of Mycobacterium tuberculosis Complex by PCR Amplification of Genomic Regions of Difference. Int. J. Tuberc. Lung Dis. 2006, 10, 818–822. [Google Scholar]
- Clarke, C.; Smith, K.; Goldswain, S.J.; Helm, C.; Cooper, D.V.; Kerr, T.J.; Kleynhans, L.; van Helden, P.D.; Warren, R.M.; Miller, M.A.; et al. Novel Molecular Transport Medium Used in Combination with Xpert MTB/RIF Ultra Provides Rapid Detection of Mycobacterium bovis in African Buffaloes. Sci. Rep. 2021, 11, 7061. [Google Scholar] [CrossRef] [PubMed]
- Goosen, W.J.; Kerr, T.J.; Kleynhans, L.; Warren, R.M.; Van Helden, P.D.; Persing, D.H.; Parsons, S.D.C.; Buss, P.; Miller, M.A. The Xpert MTB/RIF Ultra Assay Detects Mycobacterium tuberculosis Complex DNA in White Rhinoceros (Ceratotherium simum) and African Elephants (Loxodonta africana). Sci. Rep. 2020, 10, 14482. [Google Scholar] [CrossRef] [PubMed]
- Gcebe, N.; Hlokwe, T.M. Non-Tuberculous Mycobacteria in South African Wildlife: Neglected Pathogens and Potential Impediments for Bovine Tuberculosis Diagnosis. Front. Cell. Infect. Microbiol. 2017, 7, 15. [Google Scholar] [CrossRef]
- Adékambi, T.; Drancourt, M. Dissection of Phylogenetic Relationships among 19 Rapidly Growing Mycobacterium Species by 16S rRNA, hsp65, sodA, recA and rpoB Gene Sequencing. Int. J. Syst. Evol. Microbiol. 2004, 54, 2095–2105. [Google Scholar] [CrossRef] [PubMed]
- Devulder, G.; de Montclos, M.P.; Flandrois, J.P. A Multigene Approach to Phylogenetic Analysis Using the Genus Mycobacterium as a Model. Int. J. Syst. Evol. Microbiol. 2005, 55, 293–302. [Google Scholar] [CrossRef] [PubMed]
- De Zwaan, R.; Van Ingen, J.; Van Soolingen, D. Utility of RpoB Gene Sequencing for Identification of Nontuberculous Mycobacteria in the Netherlands. J. Clin. Microbiol. 2014, 52, 2544–2551. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Lee, S.H.; Lyu, M.A.; Kim, S.J.; Bai, G.H.; Kim, S.J.; Chae, G.T.; Kim, E.C.; Cha, C.Y.; Kook, Y.H. Identification of Mycobacterial Species by Comparative Sequence Analysis of the RNA Polymerase Gene (rpoB). J. Clin. Microbiol. 1999, 37, 1714. [Google Scholar] [CrossRef]
- Manjeese, W.; Muzividzi, B.; Mbanga, J.; Mufandaedza, J.; Chin’ombe, N.; Osunsanmi, F.O.; Vagholkar, K. RpoB Gene-Based Characterization of Non-Tuberculous Mycobacteria in Zimbabwe. J. Adv. Microbiol. 2017, 6, 1–7. [Google Scholar] [CrossRef]
- Kim, H.; Kim, S.H.; Shim, T.S.; Kim, M.N.; Bai, G.H.; Park, Y.G.; Lee, S.H.; Chae, G.T.; Cha, C.Y.; Kook, Y.H.; et al. Differentiation of Mycobacterium Species by Analysis of the Heat-Shock Protein 65 Gene (hsp65). Int. J. Syst. Evol. Microbiol. 2005, 55, 1649–1656. [Google Scholar] [CrossRef]
- Brunello, F.; Ligozzi, M.; Cristelli, E.; Bonora, S.; Tortoli, E.; Fontana, R. Identification of 54 Mycobacterial Species by PCR-Restriction Fragment Length Polymorphism Analysis of the hsp65 Gene. J. Clin. Microbiol. 2001, 39, 2799. [Google Scholar] [CrossRef]
- Wood, R.C.; Luabeya, A.K.; Weigel, K.M.; Wilbur, A.K.; Jones-Engel, L.; Hatherill, M.; Cangelosi, G.A. Detection of Mycobacterium tuberculosis DNA on the Oral Mucosa of Tuberculosis Patients. Sci. Rep. 2015, 5, 8668. [Google Scholar] [CrossRef] [PubMed]
- Mesman, A.W.; Calderon, R.; Soto, M.; Coit, J.; Aliaga, J.; Mendoza, M.; Franke, M.F. Mycobacterium tuberculosis Detection from Oral Swabs with Xpert MTB/RIF ULTRA: A Pilot Study. BMC Res. Notes 2019, 12, 349. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.C.; Andama, A.; Hermansky, G.; Burkot, S.; Asege, L.; Job, M.; Katumba, D.; Nakaye, M.; Mwebe, S.Z.; Mulondo, J.; et al. Characterization of Oral Swab Samples for Diagnosis of Pulmonary Tuberculosis. PLoS ONE 2021, 16, e0251422. [Google Scholar] [CrossRef]
- Tingan, T.K.; Mensah, G.I.; Agyekum, E.B.; Amanor, I.B.; Addo, S.O.; Ayamdoo, Y.I.; Duah, M.S.; Mosi, L.; Addo, K.K. Non-Tuberculous Mycobacteria, Not Mycobacterium bovis, Are a Significant Cause of TB-like Lesions Observed in Slaughtered Cattle in Ghana. IJID Reg. 2022, 3, 8. [Google Scholar] [CrossRef] [PubMed]
- Katale, B.Z.; Mbugi, E.V.; Karimuribo, E.D.; Keyyu, J.D.; Kendall, S.; Kibiki, G.S.; Godfrey-Faussett, P.; Michel, A.L.; Kazwala, R.R.; van Helden, P.; et al. Prevalence and Risk Factors for Infection of Bovine tuberculosis in Indigenous Cattle in the Serengeti Ecosystem, Tanzania. BMC Vet. Res. 2013, 9, 1267. [Google Scholar] [CrossRef]
- Deurenberg, R.H.; Bathoorn, E.; Chlebowicz, M.A.; Couto, N.; Ferdous, M.; García-Cobos, S.; Kooistra-Smid, A.M.D.; Raangs, E.C.; Rosema, S.; Veloo, A.C.M.; et al. Application of next Generation Sequencing in Clinical Microbiology and Infection Prevention. J. Biotechnol. 2017, 243, 16–24. [Google Scholar] [CrossRef]
- Vierhout, B.P.; Ott, A.; Kruithof, I.; Wisselink, G.; van Zanten, E.; Kooistra-Smid, A.M.D.; Zeebregts, C.J.; Pol, R.A. Inguinal Microbiome in Patients Undergoing an Endovascular Aneurysm Repair: Application of next-Generation Sequencing of the 16S-23S RRNA Regions. Med. Hypotheses 2019, 132, 109358. [Google Scholar] [CrossRef]
- Varela-Castro, L.; Barral, M.; Arnal, M.C.; Fernández de Luco, D.; Gortázar, C.; Garrido, J.M.; Sevilla, I.A. Beyond Tuberculosis: Diversity and Implications of Non-Tuberculous Mycobacteria at the Wildlife-Livestock Interface. Transbound. Emerg. Dis. 2022. [Google Scholar] [CrossRef]
- Botha, L.; Gey van Pittius, N.C.; van Helden, P.D. Mycobacteria and Disease in Southern Africa. Transbound. Emerg. Dis. 2013, 60 (Suppl. 1), 147–156. [Google Scholar] [CrossRef]
- Biet, F.; Boschiroli, M.L.; Thorel, M.F.; Guilloteau, L.A. Zoonotic Aspects of Mycobacterium bovis and Mycobacterium avium-Intracellulare Complex (MAC). Vet. Res. 2005, 36, 411–436. [Google Scholar] [CrossRef]
- Gcebe, N.; Rutten, V.; Gey van Pittius, N.C.; Michel, A. Prevalence and Distribution of Non-Tuberculous Mycobacteria (NTM) in Cattle, African Buffaloes (Syncerus caffer) and Their Environments in South Africa. Transbound. Emerg. Dis. 2013, 60 (Suppl. 1), 74–84. [Google Scholar] [CrossRef] [PubMed]
- Katale, B.Z.; Mbugi, E.V.; Botha, L.; Keyyu, J.D.; Kendall, S.; Dockrell, H.M.; Michel, A.L.; Kazwala, R.R.; Rweyemamu, M.M.; van Helden, P.; et al. Species Diversity of Non-Tuberculous Mycobacteria Isolated from Humans, Livestock and Wildlife in the Serengeti Ecosystem, Tanzania. BMC Infect. Dis. 2014, 14, 616. [Google Scholar] [CrossRef] [PubMed]
- Gcebe, N.; Michel, A.; van Pittius, N.C.G.; Rutten, V. Comparative Genomics and Proteomic Analysis of Four Non-Tuberculous Mycobacterium Species and Mycobacterium tuberculosis Complex: Occurrence of Shared Immunogenic Proteins. Front. Microbiol. 2016, 7, 795. [Google Scholar] [CrossRef] [PubMed]
- Michel, A.L. Mycobacterium Fortuitum Infection Interference with Mycobacterium bovis Diagnostics: Natural Infection Cases and a Pilot Experimental Infection. J. Vet. Diagn. Investig. 2008, 20, 501–503. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.; Terrell, S.; Lyashchenko, K.; Greenwald, R.; Harris, B.; Thomsen, B.V.; Fontenot, D.; Stetter, M.; Neiffer, D.; Fleming, G. Mycobacterium kansasii Infection in a Bontebok (Damaliscus pygaragus dorcas) Herd: Diagnostic Challenges in Differentiating from the Mycobacterium Tuberculosis Complex. J. Zoo Wildl. Med. 2011, 42, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Lacasse, C.; Terio, K.; Kinsel, M.J.; Farina, L.L.; Travis, D.A.; Greenwald, R.; Lyashchenko, K.P.; Miller, M.; Gamble, K.C. Two Cases of Atypical Mycobacteriosis Caused by Mycobacterium szulgai Associated with Mortality in Captive African Elephants (Loxodonta africana). J. Zoo Wildl. Med. 2007, 38, 101–107. [Google Scholar] [CrossRef]
- Hernández-Jarguín, A.M.; Martínez-Burnes, J.; Molina-Salinas, G.M.; de la Cruz-Hernández, N.I.; Palomares-Rangel, J.L.; Mayagoitia, A.L.; Barrios-García, H.B. Isolation and Histopathological Changes Associated with Non-Tuberculous Mycobacteria in Lymph Nodes Condemned at a Bovine Slaughterhouse. Vet. Sci. 2020, 7, 172. [Google Scholar] [CrossRef]
- Gey van Pittius, N.C.; Warren, R.M.; Van Heiden, P.D.; Geluk, A.; Ottenhoff, T.H.M.; Arend, S.M.; Andersen, P.; Doherty, T.M. ESAT-6 and CFP-10: What Is the Diagnosis? Infect. Immun. 2002, 70, 6509. [Google Scholar] [CrossRef]
- Tortoli, E.; Pecorari, M.; Fabio, G.; Messinò, M.; Fabio, A. Commercial DNA Probes for Mycobacteria Incorrectly Identify a Number of Less Frequently Encountered Species. J. Clin. Microbiol. 2010, 48, 307–310. [Google Scholar] [CrossRef]
- Kuria, J.K.N.; Akwalu, S.K.; Muema, L.M. The Etiology and Public Health Significance of Mycobacteriosis of Cattle in Kenya. Int. J. Mycobacteriol. 2018, 7, 251–256. [Google Scholar] [CrossRef]
- Mekkaoui, L.; Hallin, M.; Mouchet, F.; Payen, M.C.; Maillart, E.; Clevenbergh, P.; Georgala, A.; Van den Wijngaert, S. Performance of Xpert MTB/RIF Ultra for Diagnosis of Pulmonary and Extra-Pulmonary Tuberculosis, One Year of Use in a Multi-Centric Hospital Laboratory in Brussels, Belgium. PLoS ONE 2021, 16, e0249734. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.K.; Jorwal, P.; Soneja, M.; Sharma, R.; Wig, N. Acta Scientific Medical Sciences. In Trace Result in Xpert MTB/RIF Ultra: A Diagnostic Dilemma and Interpretation? Acta Scientific Publications OPC Private Limited: Hyderabad, India, 2017; ISSN 2582-0931. [Google Scholar]
- Perez-Risco, D.; Rodriguez-Temporal, D.; Valledor-Sanchez, I.; Alcaide, F. Evaluation of the Xpert MTB/RIF Ultra Assay for Direct Detection of Mycobacterium tuberculosis Complex in Smear-Negative Extrapulmonary Samples. J. Clin. Microbiol. 2018, 56, e00659-18. [Google Scholar] [CrossRef] [PubMed]
- Piersimoni, C.; Gherardi, G.; Gracciotti, N.; Pocognoli, A. Comparative Evaluation of Xpert MTB/RIF and the New Xpert MTB/RIF Ultra with Respiratory and Extra-Pulmonary Specimens for Tuberculosis Case Detection in a Low Incidence Setting. J. Clin. Tuberc. Other Mycobact. Dis. 2019, 15, 100094. [Google Scholar] [CrossRef] [PubMed]


| Primer Name | Forward Primer Sequence (5′–3′) | Reverse Primer Sequence (5′–3′) | Annealing Temperature | Product Size |
|---|---|---|---|---|
| rpoB | GGCAAGGTCACCCCGAAGGG | AGCGGCTGCTGGGTGATCATC | 64 °C | ±764 bp |
| hsp65 | ACCAACGATGGTGTGTCCAT | CTTGTCGAACCGCATACCCT | 60 °C | ±439 bp |
| esat-6 | CATGACAGAGCAGCAGTG | GCCCTATGCGAACATCCC | 60 °C | ±292 bp |
| cfp-10 | GTAGCCCGGGATGGCAGAGATGAAGACCGATGCC | TCAGAAGCCCATTTGCGAGGACAGC | 60 °C | ±300 bp |
| bp; base pairs | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clarke, C.; Kerr, T.J.; Warren, R.M.; Kleynhans, L.; Miller, M.A.; Goosen, W.J. Identification and Characterisation of Nontuberculous Mycobacteria in African Buffaloes (Syncerus caffer), South Africa. Microorganisms 2022, 10, 1861. https://doi.org/10.3390/microorganisms10091861
Clarke C, Kerr TJ, Warren RM, Kleynhans L, Miller MA, Goosen WJ. Identification and Characterisation of Nontuberculous Mycobacteria in African Buffaloes (Syncerus caffer), South Africa. Microorganisms. 2022; 10(9):1861. https://doi.org/10.3390/microorganisms10091861
Chicago/Turabian StyleClarke, Charlene, Tanya J. Kerr, Robin M. Warren, Léanie Kleynhans, Michele A. Miller, and Wynand J. Goosen. 2022. "Identification and Characterisation of Nontuberculous Mycobacteria in African Buffaloes (Syncerus caffer), South Africa" Microorganisms 10, no. 9: 1861. https://doi.org/10.3390/microorganisms10091861
APA StyleClarke, C., Kerr, T. J., Warren, R. M., Kleynhans, L., Miller, M. A., & Goosen, W. J. (2022). Identification and Characterisation of Nontuberculous Mycobacteria in African Buffaloes (Syncerus caffer), South Africa. Microorganisms, 10(9), 1861. https://doi.org/10.3390/microorganisms10091861






