Abstract
Invasive candidiasis (IC) is a systemic life-threatening infection of immunocompromised humans, but remains a relatively neglected disease among public health authorities. Ongoing assessments of disease epidemiology are needed to identify and map trends of importance that may necessitate improvements in disease management and patient care. Well-established incidence increases, largely due to expanding populations of patients with pre-disposing risk factors, has led to increased clinical use and pressures on antifungal drugs. This has been exacerbated by a lack of fast, accurate diagnostics that have led treatment guidelines to often recommend preventative strategies in the absence of proven infection, resulting in unnecessary antifungal use in many instances. The consequences of this are multifactorial, but a contribution to emerging drug resistance is of primary concern, with high levels of antifungal use heavily implicated in global shifts to more resistant Candida strains. Preserving and expanding the utility and number of antifungals should therefore be of the highest priority. This may be achievable through the development and use of biomarker tests, bringing about a new era in improved antifungal stewardship, as well as novel antifungals that offer favorable profiles by targeting Candida pathogenesis mechanisms over cell viability.
1. Introduction
Until relatively recently, fungi were a rare cause of life-threatening human disease. Since the early 1980s, invasive fungal diseases (IFDs) have been an increasing occurrence in healthcare environments due to an ever-expanding population susceptible to infection [1,2]. This has largely been driven by the advent of more aggressive interventions and treatments in modern healthcare, placing patients in prolonged states of severe immunosuppression [3,4].
Invasive candidiasis (IC), caused by yeast species in the fungal genus Candida, is one of the main systemic, opportunistic fungal diseases of immunocompromised patients. It is associated with significant global burden, with an estimated 750,000 cases occurring annually [5] and unacceptably high mortality rates of up to 30% [6,7]. More than 15 Candida species have now been described as etiologic agents of IC, but >90% of cases are attributed to just five: C. albicans, C. glabrata, C. parapsilosis, C. tropicalis and C. krusei. Of these, C. albicans is predominant [1,8]. The term invasive candidiasis is used to describe two distinct disease entities: candidemia bloodstream infection (BSI) and deep-seated tissue candidiasis (Figure 1), which may occur independently or concomitantly [9].
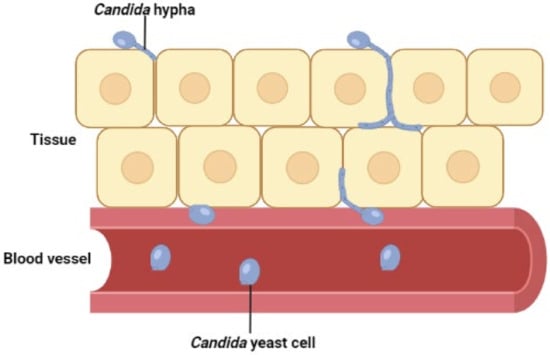
Figure 1.
Invasive candidiasis involves rapid dissemination of Candida yeast cells in the bloodstream (candidemia BSI) and/or tissue penetration by invasive hypha (deep-seated candidiasis). Hematogenous seeding of Candida yeast from blood-borne candidemia is often a key source of tissue candidiasis and vice versa [9]. Although hyphal extension is a well-described mechanism of C. albicans tissue invasion, its role is less clear for other clinically important Candida species such as C. glabrata where other mechanisms of invasion may be involved.
Despite being an increasing cause of morbidity and mortality in healthcare settings, IC is still a somewhat neglected topic among public health authorities. Consequently, improvements in disease management and patient care are urgently needed [1,5]. Of particular importance is a lack of fast, accurate diagnostics, with clinicians continuing to rely on suggestive clinical findings and the use of culture-based diagnostics with sub-optimal sensitivity to inform decision making [10]. It is suggested that up to 50% of disease episodes may go undiagnosed by these conventional methods, resulting in delayed treatment initiation and markedly worse patient outcomes [9,10,11]. To mitigate this, current treatment guidelines recommend that prophylactic or empirical preventative strategies be initiated in high-risk populations in the absence of proven infection [12,13]. Whilst some patients will benefit from these measures, non-specific implementation leads to unnecessary use of precious antifungals in many instances. This has led many to raise concerns about the risks of widespread drug resistance among Candida spp., particularly given the already limited availability of front-line antifungals [14,15].
Overall, IC represents a major global public health concern. A robust understanding of ongoing disease epidemiology is therefore of importance to identify concerning trends that may inform policy decisions and necessitate the need for improvements in disease management and patient care. In this review, a critical appraisal of the current IC epidemiologic landscape is made, focusing on prospective surveillance studies that assess patient pre-disposing risk factors, incidence, Candida spp. distribution and antifungal susceptibility patterns both spatially and temporally. Particular attention will be given to the interplay between these factors. Antifungal treatment and diagnostics are outlined as two key components of IC management, with the influence of current practices on disease epidemiology considered. Viable improvements in the implementation of these clinical activities are then proposed, offering the potential for a new era in disease management and patient care through improved antifungal stewardship and availability.
2. Pre-Disposing Risk Factors
As a commensal fungus that is part of the normal human microbiota, Candida very rarely causes invasive infections in healthy individuals [16]. Classically, life-threatening IC infections are found in patients with compromised immune systems [3,17,18,19], broadly influenced by healthcare and host-related risk factors [4,20].
2.1. Healthcare Factors
Healthcare-related pre-disposing risks for IC often involve cutaneous or mucosal barrier disruption and broad-spectrum antimicrobials, common interventions in healthcare. Cutaneous barrier disruption is often a result of subcutaneous medical devices, such as central venous catheters (CVCs) and portacaths, implanted for long-term intravenous drug infusion or parenteral nutrition [4]. Subcutaneous implanted medical devices into the vasculature are a common source of candidemia BSI. This is due to the ability of Candida to form biofilms on such indwelling abiotic surfaces and subsequent release of Candida yeast cells into circulation [16].
Disruption of the mucosal barrier in the gastrointestinal tract through surgery or transplantation is also an important risk factor for invasive infection, resulting in increased translocation of gut-dwelling Candida into the vasculature [21]. Administration of broad-spectrum antimicrobials increases colonisation and pathogenic capabilities of Candida spp. by altering the interactions and dynamics of the microbiome. A distinct shift is seen from mutualism and colonisation in commensal Candida to competition and infection in IC [22,23]. Others postulate that chemotherapy agents may have similar effects on the gut microbiome [24]. Together with their immunosuppressive activity, chemotherapeutic agents represent a major risk factor by acting through multiple channels.
2.2. Host Factors
Underlying host conditions can bring about immunocompromised states that increase the likelihood of opportunistic infection. This may occur directly, such as in HIV infection, some cancers, renal disease, liver cirrhosis and diabetes mellitus among others [4,25,26], or indirectly through immunosuppressive treatment (e.g., chemotherapy, corticosteroids and, more recently, immunotherapy) for underlying conditions such as solid and haematological malignancies [3]. These populations of the immunosuppressed have expanded in recent decades with the advent of longer treatment regimens and newer therapeutics with greater cytotoxic payloads and potency [2,27]. Of particular importance is the increasing number of neutropenic individuals, defined as a neutrophil blood count <0.5 × 109/L, who are extremely vulnerable to infection due to their inability to mount an effective immune response to invasive Candida [24,28]. Despite this, others have found a lack of correlation between immunocompromised individuals and IC prevalence [29,30,31]. Considered in isolation, the state of being immunocompromised may be a small contributor to IC risk, but the simultaneous presence of other healthcare risk factors, acting as an initial source of systemic Candida, may act to increase the relative risk of immunosuppression. This may explain the disparity in studies on pre-disposing risk factors and outlines the difficulty in defining the relative risk posed by one individual factor when, clinically, interplay exists, with multiple risk factors often observed together [4,31]. Therefore, a holistic approach may be more appropriate, taking account of all major risk factors in combination.
3. Incidence
Globally, IC incidence has generally increased over the last decades as the populations susceptible to infection have expanded [2,32,33], with increases in both hospital- and community-acquired infections observed. Candida is now responsible for ~10% of nosocomial BSIs in the United States (US) [1,2,34,35], and up to one-third of episodes are also thought to be community-acquired due to the increasing at-home management of patients with CVCs [8]. Despite a well-described incidence increase, recent studies suggest that this may be stabilising or reversing in certain settings [36,37,38,39,40]. The reasons for these observations are not well-defined, but improvements in the management of patient pre-disposing risk factors [36,37], and increasing uptake in biomarker and prediction tool use (e.g., T2 Candida, Colonisation Index and Acute Physiology and Chronic Health Evaluation II score) that allow for targeted preventative treatment strategies in identified high-risk patients have been suggested [41]. Importantly, to date, studies reporting this decline are limited, with a greater number of data sets required to establish these observations as an ongoing trend more widely. Specifically, the importance of improved risk factor management, as well as biomarker and prediction tool use that have already been suggested in these declines, should be investigated further. If a causal relationship is widely established, this should act to drive broad changes in IC disease management strategies that implement these healthcare activities.
When assessing IC incidence, several limitations must be acknowledged. First is the use of different denominators in incidence calculations, making it challenging to draw meaningful comparisons. Population-based studies report incidence as cases per 100,000 persons, whilst hospital-centre-based studies often report it as cases per 10,000 patient days or 1000 admissions [42]. Comparisons of incidence are also challenged by the variable sensitivity of blood culture, influenced by numerous factors that are not standardised across healthcare settings. These include the blood culture system in use, blood culture volume and whether antifungals were in use at the time of blood draw [36,43]. Of primary importance is that most surveillance studies are inherently flawed. This is because they look only at a partial disease spectrum, focusing on candidemia BSI and often disregarding deep-seated tissue candidiasis. This is due to the current difficulties in diagnosing deep-seated infection, meaning these disease events are largely under-ascertained [9,10]. Furthermore, suboptimal sensitivity of current diagnostics for IC infection generally means that candidemia BSI cases are also underdetermined, albeit to a lesser extent.
Inaccuracies and underestimation in IC cases and incidences are inevitable as estimates are based upon a partial clinical disease spectrum, diagnostics with poor sensitivity and factors that are not standardised across healthcare settings. Acknowledging these limitations, here an assessment of disease incidence will focus on prospective population-based surveillance data from the US and Europe, allowing for comparisons at the entire population level across the whole spectrum of clinical settings [44].
3.1. United States
Current estimates point to a higher disease incidence in the US than Europe [6,36,39,40,45], but since data are scarce and estimates vary greatly on a centre-to-centre basis such conclusions may not be nationally representative [6]. US data also suggest that whilst incidence has increased over the past decades, there may now be signs of reversal [6,36].
A series of studies aiming to provide accurate epidemiology data by conducting ongoing prospective population-based surveillance for candidemia BSI in metropolitan regions of four US states have been undertaken, with data available from 1992 to 2016 (Table 1) [6,36,44,46,47].

Table 1.
Overall candidemia population-based incidence rates expressed as the number of cases per 100,000 population across 4 metropolitan sites in four US states from 1992 to 2016.
Incidence estimates varied greatly across the four sites during the surveillance period. In Georgia, incidence increased from 9.1 to 13.3 from 1992 to 2011 [44,46] before declining to 7.5 in 2016, respectively [6,36]. Similarly, in Maryland, incidence increased from 1998–2011, albeit to a lesser extent from 24.2 to 26.2 before declining significantly to approximately 13.0 in 2016 [6,44,47]. Data from Oregon and Tennessee are only available from a later date as these two sites were added to the CDC’s Emerging Infections Program [EIP] for candidemia surveillance in 2011. In Oregon, incidence remained relatively stable and significantly lower than other sites at 3.0–3.5 whilst in Tennessee incidence rose markedly in a short 4-year period by 4.5 cases per 100,000 [6].
The main drivers of both increasing and decreasing incidences were identified. Adults aged >65 in ICUs were of greatest importance in observed increases, with this demographic now representing the largest contribution to total cases with an incidence of 25.5 per 100,000 persons [6,44,46,47]. Increasing numbers of total patients >65 in ICUs may be implicated, where invasive procedures that put elderly patients at risk for opportunistic IC infection are particularly common. IC was previously known to be most prevalent among those aged ≤1 year, driven by low-birthweight and pre-term infants. Although this age demographic still represents an important contributor to IC caseload, drastic declines in incidence have been observed (Figure 2) [6,44,48].
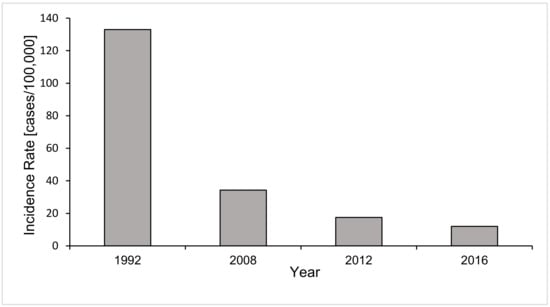
Figure 2.
Annual candidemia incidence rates in infants aged ≤1 year described from surveillance at a metropolitan site in Georgia in 1992, 2008, 2012 and 2016 [6,44,46]. Candidemia incidence in this age demographic shows a declining trend, with incidence decreasing markedly from 133.0 to 12.0 cases per 100,000 population in 1992 and 2016, respectively.
Low-birthweight and pre-term infants aged ≤1 year often require implanted medical devices, such as CVCs to be fitted, an important pre-disposing risk factor for IC infection. Therefore, improvements in infection control practices around hand hygiene and maintenance of these devices have been implicated in this trend [44,48]. Widespread implementation of standard-of-care antifungal prophylaxis may also be contributory [48]. In addition to age-specific declines, incidence decreases have been described overall from 2011 at sites in Georgia and Maryland [36]. Again, improvements in the management of patient risk factors are thought to be important, with CVC-associated candidemia almost halving from 2008 to 2013 whilst cases in patients without CVCs remained constant [36]. In the US, increasing incidence therefore appears to have been driven largely by the >65 age demographic in ICU whilst recent incidence declines result from improved management of patient pre-disposing risk factors, particularly among infants.
State- and site-specific incidences vary considerably, with the influence of varying risk factor prevalence in underlying populations and implementation of disease management strategies considered. It was found that 77% and 73% of culture positive candidemia cases were associated with systemic antimicrobial administration and patients with CVCs, respectively [6], outlining the major infection risk that they pose. Differences in the patterns of use of these healthcare factors will therefore influence the population susceptible to infection and subsequent IC incidence. The impact of underlying conditions such as solid/haematological malignancies that require prolonged immunosuppressive treatment is apparently negligible given that these patients account for a small proportion of the total population susceptible to IC (~5% of total cases only [1,6,49]). Varying implementation of preventative treatment and other disease management strategies that might reduce group-specific incidence in these high-risk populations may be important [36,37,41,50]. Surprisingly, 10% of disease events were associated with patients that had a history of injection drug use (IDU), a risk factor previously considered to be of less prominence. It is hypothesised that the current opioid crisis in the US and associated increased IDU rates might be responsible [51,52]. Importantly, while several factors are outlined here, defining the impact that any one factor has on incidence of IC is problematic. Furthermore, it must be acknowledged that there will be many other contributory factors that are currently not well-defined.
3.2. Europe
Since the first population-based European incidence data were described in 1980 [53], estimates have ranged from 1.4 to 10.05 cases per 100,000 population [39,40,45,53,54,55,56,57,58,59,60], outlining the considerable temporal and spatial variation that exists. Despite this large variation, available estimates to date are generally lower than those described in the US.
As two of the few countries that have ongoing national prospective surveillance for candidemia, Iceland and Denmark will be examined here to assess potential trends and enable comparisons with US data. Incidence in Iceland increased steadily from 1980 to 2009, where it peaked at 7.5 cases/100,000 [39,53]. In the subsequent two years, incidence declined markedly to 4.0 cases/100,000 persons, consistent with trends observed in the US and other European countries [6,36,39,40]. In these countries, declines were attributed to improved management of patient pre-disposing risk factors. However, in Iceland, it is noted that the volume of blood cultures performed at this time also reduced considerably due to an ongoing economic recession, and that this may invalidate these findings somewhat. Further readouts of incidence from Iceland are therefore required to accurately assess whether declines have truly occurred [39].
Denmark represents an outlier in European IC incidence estimates which, through its national surveillance programme for candidemia BSI, has consistently reported some of the highest regional incidences over 15 years [40,59,60], peaking at 10.05 cases/100,000 persons in 2011 [60]. The reasons suggested for this are two-fold. Danish surveillance may be more accurately ascertaining disease episodes, or the true disease burden may be greater with increased/different antibacterial drug use suggested as a cause for this [54]. Specifically, one Danish study observed that IC risk was disproportionately increased in critically ill ICU patients exposed to ciprofloxacin containing antibiotics compared with other antibacterial regimens such as cefuroxime and piperacillin [61]. Differences in national IC disease burdens will exist but are unlikely to account entirely for the significantly higher incidence in Denmark compared to neighbouring countries. Therefore, the more important factor might be the presence of robust national surveillance for candidemia that yields a more accurate ascertainment of total IC caseload across Danish healthcare than elsewhere. This highlights the importance of robust national surveillance systems for IC in understanding disease epidemiology and may be used as an appropriate model for other countries and regions to follow.
4. Antifungal Treatment
Antifungal agents (Table 2) are limited because their development relies on the identification of fungus-specific targets, which is challenged by the phylogenetic similarities between the fungal and animal kingdoms, both being eukaryotes [15]. As a life-threatening invasive mycosis, prompt initiation of intravenous antifungal treatment in suspected IC cases affects prognosis markedly [11]. Treatment guidelines therefore often recommend prophylactic and empirical strategies, due to a lack of fast, accurate diagnostics [12,13]. Prophylaxis involves preventative antifungal treatment for high-risk populations in the absence of infection signs and symptoms whilst empirical treatment is initiated in patients with suggestive clinical findings of infection in the absence of a clear diagnosis [13,62]. Given the implications of delayed treatment and the difficulties associated with making a fast and accurate diagnosis, these pre-emptive strategies have been the preferred means of managing patients at risk for IC with antifungal drugs.

Table 2.
Current antifungal agents licensed for the treatment of IC are limited to just three drug classes: the polyenes, triazoles and echinocandins [63].
4.1. Polyenes
Polyenes were the first mainstay antifungal class approved for IC treatment [63], acting as fungicidal agents by irreversibly binding ergosterol in the Candida cytoplasmic membrane and forming aqueous pores that lead to ion leakage and cell death [64]. Despite excellent efficacy against species of the Candida genus, severe dose-limiting toxicities, most notably nephrotoxicity, meant that amphotericin B deoxycholate was never fully exploited clinically [65,66]. Now, reformulated lipid-based preparations termed ‘AmBisome’ (liposomal amphotericin B) benefit from an improved therapeutic index and toxicity profile by altering distribution to organs, although significant toxicity is still persistent [67,68,69]. Furthermore, as efficacy is not compromised, Ambisome is used under specific indications, particularly on haematology and oncology wards [67,70].
4.2. Triazoles
Triazoles represent the largest group of antifungals for IC treatment [15], displaying fungistatic activity by binding and inhibiting lanosterol-14α-demethylase, leading to ergosterol depletion in the Candida membrane [71]. As with polyenes, severe toxicities are well-documented, with hepatotoxicity often implicated in use. Additionally, a high risk for drug–drug interactions is of concern, which may adversely affect treatment responses if not managed correctly [62]. Despite this, triazoles still represent key therapeutic options due predominantly to limited alternatives, excellent efficacy and availability in both intravenous and oral preparations. For years, fluconazole was the primary treatment option for IC [12,14], but continuing emergence of resistance has now limited its clinical utility [12,13]. Drivers of resistance are not fully defined, but widespread clinical overuse of fluconazole is thought to be key, exerting strong selection pressures for Candida resistance [72]. The emergence of resistance means guidelines are increasingly recommending alternate drug classes for first-line therapy [12,13].
4.3. Echinocandins
Echinocandins are the newest antifungal class despite being introduced 20 years ago, exhibiting important advantages over the different drug classes [2]. Owing to their fungus-specific target of β-D-glucan synthesis inhibition, they have markedly improved safety and toxicity profiles [73,74]. In addition, they exhibit few drug–drug interactions [13] and boast broad activity, remaining highly effective against Candida spp. displaying triazole tolerance. Importantly, C. parapsilosis and C. guilliermondii, due to a naturally occurring proline-to-alanine amino acid change in the Fks1 protein (Fks1p), are likely candidates for future echinocandin resistance and therefore should be monitored closely [75]. Fks1p represents the catalytic subunit of the β-1,3-glucan synthase complex, the target of echinocandins, meaning such amino acid polymorphisms in Fks1p may bestow resistance by evading echinocandin activity [76,77]. Superior toxicity profiles and minimal resistance to date mean that echinocandins are being increasingly favoured over triazoles and polyenes for IC treatment, except where C. parapsilosis is implicated in infection [12,13].
4.4. Antifungal Stewardship
Echinocandins represent a vital drug class in IC treatment. Few licensed drugs, unacceptable toxicities, triazole resistance and a relatively dry drug pipeline contribute to the scarcity of available alternatives [15]. The management of echinocandin use should therefore be of the highest priority. It is important that clinicians learn from mistakes made with fluconazole, aiming to reduce unnecessary echinocandin use where possible and limit emerging drug resistance [14]. A particular focus should be prophylactic antifungal practices in the absence of proven infection. More accurately, defining high-risk patients that might or might not benefit from such preventative treatment is highly desirable, and achievable through the development and use of biomarker tests that allow clinicians to accurately identify or rule out infection [9,10]. This could represent a new era, bringing improvements in disease management and patient care through improved antifungal stewardship. Given their potential importance, the applications and implications of different biomarker tests will be discussed in greater depth in Section 7.
5. Species Distribution and Antifungal Susceptibilities
Globally, more than 15 Candida spp. are known etiologic agents of IC [78,79], but the majority (>90%) of infections are attributed to just five: C. albicans, C. glabrata, C. parapsilosis, C. tropicalis and C. krusei [2,6,36,38,40,80]. As such, they will be the focus here. Candida albicans has long been and remains the predominant species present as clinical isolates from infected patients [1], but an ongoing global shift towards non-albicans Candida (NAC) species that exhibit decreased antifungal susceptibility is well-established [2,33,81]. Emerging multi-drug-resistant strains such as C. auris, first described in 2009, represent a serious public health threat and highlight further the concerning global divergence of Candida spp. implicated in IC to more resistant strains [82].
As with incidence, when assessing IC species distributions and antifungal susceptibilities, limitations in data must be considered. First is the sub-optimal sensitivity of blood culture, meaning data represent only the testing of isolates from disease events that were culture-positive [83], a partial spectrum of the total IC disease events. Furthermore, although undefined, inevitably not all culture positive cases will undergo species identification and antifungal susceptibility testing. However, as testing is common and even compulsory in some countries and healthcare settings [6,40], the volume of testing may be considered adequate and representative of the species distribution and antifungal susceptibility landscape. Comparisons are also challenged by factors that are not standardised across healthcare settings, with the use of different blood culture systems notable. For example, C. glabrata positivity rates have been shown to be higher where the BacT/Alert culture system is used [55,84]. Although this is clinically significant, quantification of differences between culture systems shows inconsistencies and will be impacted by other currently contested confounding factors [84,85]. As such, acceptable concordance will be assumed between blood culture systems in the isolation rates of Candida spp.
Here, an assessment of Candida spp. distribution and antifungal susceptibility will focus on spatial and temporal data shifts at the continental level. Additionally, specific consideration will be given to the role of patient pre-disposing risk factors in species distribution as well as the interaction between increased use of antifungals and shifts towards strains with less susceptibility [72].
5.1. Influence of Pre-Disposing Risk Factors
Pre-disposing risks for IC, both host and healthcare related factors, can influence the Candida spp. implicated in infection [6,72,86]. Increasing patient age, transplant procedures and prior fluconazole exposure are well-documented factors for increased isolation of C. glabrata [72,87,88,89,90]. The latter may point towards an applied selection pressure from fluconazole use, driving C. glabrata-implicated infection with greater drug resistance [91]. C. parapsilosis is renowned for its high prevalence among pre-term and low-birthweight infants [48,92,93,94]. This may be due to an elevated ability to form biofilms on indwelling devices, which are commonly used in this patient group [95,96]. Another key driver of C. parapsilosis infection is its ability for nosocomial spread, notably by hand carriage, leading to hospital outbreaks and persistence [94,97]. With the advent of at-home CVC management, C. parapsilosis may therefore also be responsible for the rise in community-acquired IC [8,98]. C. tropicalis and C. krusei have a heightened presence among severely neutropenic patients on oncology wards [99,100,101]. Oncology-specific C. tropicalis incidence now appears to be declining in certain settings, with widespread fluconazole prophylaxis and improved management of CVCs likely determinants in these observations [36,72]. Conversely, as with C. glabrata, fluconazole exposure is cited as a selection pressure that has acted in the emergence of resistant C. krusei, particularly among the oncology patient population [72]. However, reported increases in C. krusei prevalence pre-date widespread prophylaxis regimens [102], suggesting other factors have also influenced its emergence. These may include oncology-specific risk factors such as the long-term use of subcutaneous portacaths and CVCs as well as administration of certain chemotherapy agents [24].
5.2. Geographical Trends
Species distribution and antifungal susceptibility shows considerable geographical variation between individual countries, but trends can generally be elucidated at the continental level, such as the Americas and Europe (Figure 3). Across some continents (Asia, Africa and Oceania), few distinctive trends are observed and are not well-defined due to limited and contrasting data from mostly single-institution studies [103,104,105,106,107,108]. As a result, data from Asia will be assessed briefly and Africa and Oceania will be excluded from this review.
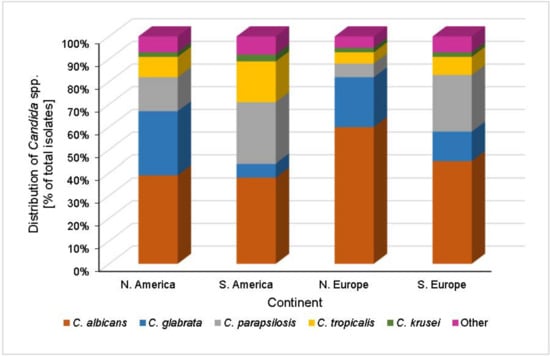
Figure 3.
Distributions of Candida spp. as a percentage of total IC case counts across North America, South America, North Europe and South Europe [6,54,109,110,111]. In North America, C. albicans is the most prevalent Candida species, accounting for ~39% of IC episodes. The most common NAC species, representing just under 30% of cases, is C. glabrata with sequentially lower case contributions from C. parapsilosis, C. tropicalis and C. krusei. European IC species distribution shows two clear trends, split broadly between the north and south of the continent. Northern Europe typically exhibits a similar species distribution to North America, although a greater contribution from C. albicans is seen, accounting for 60% of cases. In contrast, the species landscape in southern Europe is more akin to that in South America, where C. parapsilosis is the most common NAC species. Across these four regions, <10% of total cases are attributed to species outside of the five described.
5.2.1. United States
Candida glabrata is of the highest concern in the US due to a combination of increasing incidence and high levels of resistance to front-line antifungals [6]. Up until the late 1990s, C. albicans accounted for ~50% of all Candida BSIs in the US [46], but its contribution has since decreased [6,36,44], with a concurrent increase in NAC incidence observed [1,6,36,44,46]. C. glabrata has emerged as the most frequent NAC species, making up 12% of isolates in 1999 [46] but now consistently accounting for just under 30% [6,36,44]. The significance of this trend is justified as C. glabrata exhibits high levels of triazole tolerance and emerging echinocandin resistance, albeit to a lesser extent [47,81]. Importantly, resistance shows considerable state variation perhaps due to differing patterns of population pre-disposing factors at a local level, outlining the importance of robust surveillance in local healthcare settings more widely. C. glabrata fluconazole resistance has been as high as 20% in selected US states (Georgia), but a gradual decline to ~10% has been observed since the 1990s [6,36]. Echinocandin resistance has increased simultaneously, with around 4% of C. glabrata isolates now displaying elevated MIC90 values (minimum concentration of antifungal required to inhibit growth of 90% of Candida cells) from susceptibility testing [6]. Decreasing clinical use of fluconazole in place of echinocandin as a first-choice treatment option is thought to be driving this shift, as selection pressures resulting from the use of these two drug classes change [44]. Candida echinocandin resistance remains low in most settings, but careful monitoring is required as clinical use inevitably increases [112]. Candida parapsilosis, C. tropicalis and C. krusei are much less frequently isolated, with events largely concentrated in specialist neonatal and oncology units. However, these NAC species also exhibit higher levels of antifungal resistance [91], suggesting the rapid emergence of C. glabrata in the US was mediated by several confounding risk factors in addition to selection for antifungal tolerant strains as the predominant factor [46]. It is noteworthy that C. krusei consistently exhibits fluconazole MIC90 values >64 μg/mL worldwide, rendering this antifungal of little use in C. krusei-implicated infections [44,46]. A more comprehensive national surveillance is required to track species-specific incidence and antifungal resistance trends.
5.2.2. Europe
Candida species distribution varies across the European continent. Northern Europe experiences a high contribution from C. albicans [54], whilst in central Europe, C. glabrata is of increasing prominence [113,114]. Regions of southern Europe consistently report C. parapsilosis as the most prevalent NAC strain [98,109,110].
Across northern Europe, C. albicans accounts for up to 70% of total IC cases, and C. glabrata is the most prevalent NAC species, contributing 10–20% of episodes [39,40,45,53,54,55,56,57]. However, an expected shift towards increasing isolation of more resistant NAC species with increased widespread antifungal use, as seen in the US, has not occurred [39]. A lower disease incidence in the overall population and thus reduced clinical use of antifungals to treat patients with IC may be responsible, limiting the selection pressure posed by such drugs [40]. In Denmark, observations differ and are more akin to the US, where continuing shifts to C. glabrata at the expense of C. albicans are seen [40,54,59,60]. Data from 2018 show that these species now account for 32.1% and 42.1% of culture confirmed cases, respectively [40]. Higher and combination use of numerous antifungals, notably fluconazole and itraconazole, in Danish healthcare may have driven the observed species disparity with other Nordic countries [54,59,60].
It might be expected that Danish Candida isolates would exhibit greater resistance resulting from higher antifungal use and associated selection pressures across Denmark (Figure 4). In fact, the opposite is observed whereby neighbouring countries (e.g., Norway) with lower antifungal use report Candida isolates with greater resistance levels, most notably for C. glabrata [54]. Explanations for this observation are not available, but it may be due to data contributing to these findings representing a small number of isolates (23 C. glabrata isolates from Norway compared to 165 from Denmark); hence, resistance rates calculated from susceptibility testing may not be nationally representative [54,115].
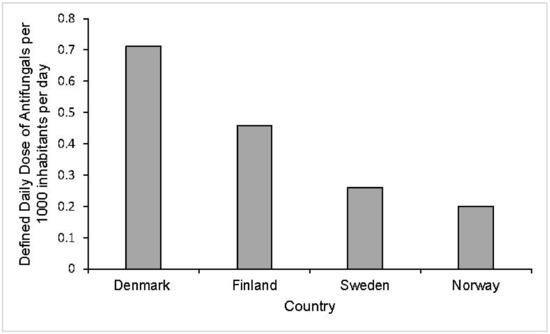
Figure 4.
Defined daily dosage (DDD) of antifungal drugs for systemic use per 1000 inhabitants per day in 2011 in healthcare settings across Denmark, Finland, Sweden and Norway. The total use of systemic antifungal drugs is significantly higher across healthcare settings in Denmark than Norway, Sweden and Finland. In Denmark, the DDD per 1000 inhabitants per day was approximately 0.712 compared to 0.459, 0.26 and 0.2 for Finland, Sweden and Norway, respectively [54].
Across central and southern Europe, species and antifungal susceptibility data are comparatively scarce and rely on single/multi-centre studies rather than national programmes. Species distribution trends analogous to the US and Denmark have been reported from institutions across central Europe [113,114,116]. A multi-decade survey by the Fungal Infection Network of Switzerland emphasizes the role of antifungals in these observations, noting that increases in C. glabrata isolation and triazole use occurred concomitantly [114]. Studies by others in the region describe a potential reversal of epidemiologic trends, with a marked increase in C. albicans and simultaneous decrease in NAC species, driven mostly by reductions in C. parapsilosis and C. tropicalis prevalence [117,118]. Confirmatory data readouts are required, with important implications if these findings represent ongoing trends. Elsewhere, antifungal use has acted to increase incidence of more resistant NAC species, leading researchers to suggest that recent changes in antifungal practices that favour echinocandin use over triazoles may be implicated [119]. In southern Europe, C. parapsilosis is the most common NAC species [98,109,110], with fluconazole-resistant C. parapsilosis increasing in prevalence and responsible for a considerably higher neonatal candidemia incidence in the region [92,94,109]. Additionally, C. parapsilosis nosocomial transmission is common [97], and therefore outbreaks in an endemic situation cannot be ruled out and may contribute to its increasing isolation further [98]. Overall, given the increasing use of echinocandins in place of triazoles as first-line treatment for IC across Europe, potential changes in species distributions and associated echinocandin resistance should be monitored closely.
5.2.3. South America
In South America, Candida species distribution is characterised by high proportions of C. parapsilosis, C. tropicalis and C. albicans, contributing >80% of the total IC caseload [111]. C. parapsilosis is the predominant NAC species and accounts for ~26.5% of cases across the continent, comparable to observations from southern Europe [109,110,111]. In addition, data from certain countries (Colombia and Venezuela) suggest that C. parapsilosis might now be the most common species implicated in infection, surpassing C. albicans as the primary causative agent [111]. This may be explained as C. parapsilosis is isolated across all age strata whilst on other continents its frequency is heavily concentrated in infant candidiasis.
C. glabrata, of major concern in the US and Europe, accounts for just 6% of IC cases across the South American continent. Additionally, low levels of overall antifungal resistance are seen, and it is thought that lower antifungal use might be implicated in both these trends [111,120,121]. C. glabrata is of greater prominence in Brazil, increasing in prevalence and currently accounting for 10% of disease events. Interestingly, differences in antifungal (particularly fluconazole) use were found to be negligible in this increase, with defined daily doses (DDD) consistent with those in neighbouring countries. Therefore, it is suggested that an ageing Brazilian population might be the cause, with increasing age a pre-disposing risk for C. glabrata infection specifically [111]. This has important implications, because as other South American countries develop an ageing population in the future, they may expect to see increasing C. glabrata isolation with inherent resistance. In fact, more recent data from Peru support these claims with C. glabrata now approaching 10% of cases there also [120]. Of note, C. guilliermondii was found to have a higher incidence than both C. glabrata and C. krusei, driven by an exceptionally high prevalence in Honduras, accounting for 28% of candidemia cases. High prevalence of C. parapsilosis overall and C. guilliermondii in specific regions warrants important considerations for antifungal stewardship in South America, as these species contain naturally occurring polymorphisms that increase the likelihood of emerging echinocandin resistance [75,76].
At present, triazoles are still recommended as the first-line therapy for IC. With potential for future increasing isolation of C. glabrata and associated triazole resistance, as seen in Brazil, this may change. If this trend continues, treatment guidelines may increasingly recommend echinocandin use over triazoles. In this scenario, additional surveillance will be required to promptly identify trends that may arise in C. parapsilosis and C. guilliermondii echinocandin resistance specifically.
5.2.4. Asia
Across the Asian continent, few distinctive trends in current species distribution and antifungal susceptibility can be concluded due to limited, contrasting data from mostly single-institution retrospective surveillance studies. Generally, C. tropicalis might be the primary etiologic agent of IC across west Asia (e.g., Pakistan, India) whilst in east Asia (e.g., China), C. albicans remains the most prevalent species with widely varied contributions from NAC species [103,104,105,106,107,108]. This is unsurprising given that China covers a land area of 9.38 million km2 and has a population of nearly 1.5 billion, which will inevitably show regional variations in pre-disposing population dynamics and risk factors that influence species distribution.
6. Diagnostics
Invasive candidiasis encompasses two distinct disease entities, candidemia BSI and deep-seated tissue candidiasis, with their distinction having important implications for diagnosis [9]. Diagnostics will be considered and split separately here into culture and non-culture-based methods, with blood culture representing the primary diagnostic choice to inform clinicians when IC infection is suspected [122,123]. Increasing development, availability and use of non-culture biomarker tests will likely complement rather than replace culture methods in the future, with combined use promising a new paradigm in patient care and disease management [10,123,124,125,126,127].
6.1. Culture-Based Diagnostics
Culture-based diagnostics, involving the detection and growth of viable Candida cells predominantly from blood, has been the primary diagnostic tool for decades [122,123]. Culture accurately diagnoses the majority of active candidemia BSI cases, with non-culture diagnostics unlikely to offer significantly lower thresholds of detection [128]. However, ~50% of total IC infection episodes are thought to go undiagnosed by blood culture, reflecting insufficient or absent viable Candida cells in circulation for detection [10,83]. These missed diagnoses are largely due to low detection rates and false-negative results for deep-seated tissue candidiasis [9,126,129], resulting from intermittent release of cells from infected tissue sites into circulation or deep-seated candidiasis that is independent of blood-borne candidemia [9,10,126,130]. Sensitivity is also influenced by Candida spp., mode of infection and antifungal drugs with C. glabrata-implicated candidemia, infection stemming from extravascular sources and use of antifungals at the time of blood draw associated with lower burdens of the pathogen and decreased likelihood of positive culture [83,131,132]. In addition to sub-optimal sensitivity for deep-seated infection and non-active candidemia, blood cultures are associated with highly variable and slow turnaround times, taking up to 8 days until positive culture [83,130]. Sub-optimal sensitivity and slow turnaround times mean that blood culture has limited utility as a definitive diagnostic, with clinicians usually utilising culture for confirmatory purposes and often taking account of multiple suggestive clinical findings to inform clinical decision making instead.
6.2. CHROMagar for Species Identification
Widely used mediums for the isolation and growth of Candida, such as Sabouraud dextrose agar (SDA) and potato dextrose agar (PDA), are unable to differentiate between Candida spp. commonly implicated in IC [133,134]. CHROMagar Candida offers a solution, a selective and differential chromogenic isolation medium allowing for presumptive identification of some Candida strains of clinical importance through observations of contrasting colony morphology and colour [134,135,136,137]. Contrasting colony colours result from reactions of species-specific enzymes with a proprietary chromogenic substrate [134]. Studies indicate that C. albicans, C. tropicalis, C. krusei [135,138] and sometimes C. glabrata [135,139] can be differentiated based on these characteristics when grown on this chromogenic medium. Of note, C. parapsilosis, due to a wide range of colony colours and morphologies, cannot be distinguished using CHROMagar [140].
The use of CHROMagar medium to identify Candida strains implicated in infection, particularly NAC species, can assist clinicians in selecting appropriate antifungal drugs that will be effective and thus may yield significant patient benefit. However, in settings where C. parapsilosis is the predominant NAC species, such as in South America and Southern Europe, the utility of CHROMagar will be more limited.
6.3. Disease Management and Patient Care Impacts
Culture-based diagnostics have important implications for the patient care and management of IC in healthcare settings, resulting from their poor sensitivity and slow turnaround times that lead to limited clinical utility and gaps in our understanding of the clinical disease spectrum [9,10,122]. Resulting delayed or missed diagnosis of these infections are therefore common and may negatively influence patient prognosis by hindering the initiation of treatment [11]. To mitigate this, current treatment guidelines recommend that early empirical and prophylactic therapy be initiated in high-risk individuals in the absence of an active infection or prior to culture diagnosis [12,13]. Although some individuals will benefit from this practice, its implementation across whole populations of high-risk patients leads to unnecessary use of precious antifungals in many instances, with important implications [12,141]. Of primary concern are the risks of emerging antifungal-resistant strains, as outlined previously, resulting from the high selection pressures caused by widespread, high levels of antifungal use. This may decrease drug efficacy in an already limited number of licensed antifungal agents for IC treatment. Furthermore, the significant healthcare costs implicated in high antifungal use as well as severe side effects endured by recipients are also important [15,72,91]. Antifungal toxicities have both direct and indirect effects on patient health [15]. Indirect impacts may relate to patients’ underlying conditions, with waning compliance to oral medication regimens due to antifungal-induced nausea and vomiting of particular concern among paediatrics [142].
Poor sensitivity of culture-based diagnostics for IC and slow turnaround times have ultimately meant that clinicians must balance the benefits of early empirical or prophylactic therapy in selected high-risk individuals with the risks posed by an increased propensity for emerging antifungal resistance, severe side effects and substantial healthcare costs.
7. Future Directions
7.1. Non-Culture-Based Diagnostics
Non-culture-based diagnostics or biomarker tests do not rely upon the detection and culture of viable Candida cells. As such, they are generally characterised by superior sensitivity and quicker turnaround times, although their clinical use in patient care is still undefined and highly limited [9]. Biomarker tests for IC typically depend upon the detection of Candida cell or cell wall components such as DNA, β-D-glucan (BDG) or mannan using PCR, colorimetric tests and immunoassays, respectively, or via host immune responses such as with anti-mannan and C. albicans germ tube antibody immunoassays [124,143,144,145]. The T2 Candida platform, approved by the US Food and Drug Administration (FDA) in 2014, represents such a test for detecting Candida DNA via cell lysis, DNA amplification using PCR and T2 magnetic resonance measurements [146,147]. In addition to superior turnaround times and sensitivity over culture-based methods, the presence of antifungals has been shown to have a negligible impact on T2 Candida test performance [132]. The high cost of the T2 Candida test may go some way as to explaining why its clinical use in patient care remains relatively limited. As for antibody assays, an important consideration is the immune status of patients, with immunocompromised individuals potentially unable to mount a strong antibody response, which could negatively impact test sensitivity [123,148]. For BDG assays, differentiation between fungi species is not possible given that BDG is a conserved cell wall component of most pathogenic fungi other than the Mucorales and Cryptococcus, which lack this carbohydrate in their cell walls [149]. Although these are important considerations, all non-culture-based diagnostics have potentially important uses in future disease management and may ultimately have their greatest impact when used in combination [146,150], increasing the overall probability of promptly diagnosing an IC disease event.
7.2. Diagnosis of Deep-Seated Tissue Candidiasis
An advantage of non-culture-based biomarker tests over culture-based methods may be the increased likelihood of detecting deep-seated tissue IC, although some events will remain undiagnosed [141]. This is evidenced by Nguyen et al. [128], where the combined use of PCR and BDG tests identified deep-seated candidiasis in 60% of patients deemed negative for tissue infections based on blood cultures alone [128]. In the same study, PCR biomarker tests elicited superior sensitivity for deep-seated IC over other non-culture-based diagnostics. However, the heterogeneity of available assays means that such findings must be approached with caution and may not be widely applicable [126].
Detecting a larger proportion of deep-seated infections will allow for earlier initiation of antifungal therapy in such instances, bringing about improvements in patient prognosis. This will also expand our understanding of the clinical disease spectrum, mapping IC epidemiology more accurately and providing further insights into Candida pathogenesis [9,124]. This includes better defining relationships between the two disease entities, such as the roles of hematogenous seeding in initiating deep-seated infection and the release of Candida cells from infected tissue into circulation [125].
However, the clinical utility of non-culture-based biomarker tests as definite diagnostics for IC is restrained by variable positive predictive values (PPVs), referring to the proportion of positive tests that are true-positive results [9,143]. The PPV is heavily dependent upon the pre-test probability of infection, and therefore disease prevalence, in the patient population being tested [126,143,151]. As a result, the use of current biomarker tests as diagnostics will likely be limited to patient populations where the pre-test probability of deep-seated IC is particularly high, such as in ICU patients with mucosal–cutaneous barrier disruption [126].
Combined use of several rapid biomarker tests for Candida infections may help broaden our understanding of the IC clinical spectrum by diagnosing a higher proportion of IC disease events, particularly deep-seated infections that were previously missed by conventional blood cultures. However, the utility of these tests as definitive diagnostics is poorly defined and may be limited to specific patient populations with a particularly high pre-test probability of infection.
7.3. Biomarker Tests as Prognostic Indicators of Infection
The uncertain performance of biomarker tests as diagnostics means that their precise roles in the management of IC are currently poorly defined [141]. It has therefore been proposed that such tests be used as adjunct prognostic indicators of Candida infections rather than providing a definitive diagnosis, with clinicians using other microbiological tests such as culture, and patient risk factors, to inform decision making [126,141]. Biomarker tests may therefore have an important role to play in guiding earlier empirical and prophylactic antifungal treatment [126,141,152]. The utility of biomarkers may also be expanded to antifungal discontinuation in high-risk individuals previously initiated on prophylactic regimens. This is due to high negative predictive values of up to 99% for these tests, meaning that up to 99% of negative tests are true-negative results, allowing clinicians to rule out infection [127,153]. In practice, the feasibility of using biomarker tests to cease antifungal treatment will be determined by the physician. If such an approach is adopted, it has the potential to prevent high-risk patients from receiving drugs that they would not benefit from, restricting antifungal usage where pre-emptive criteria are not met [9]. The use of biomarker tests as outlined has important implications for patient care and IC management, providing an opportunity for reduced unnecessary use of antifungal agents without compromising patient care and individual IC risk. It is hoped that this will allow for a marked reduction in the selection pressure posed by antifungal agents, which is thought to be a key driver in emerging resistance among some clinically important Candida spp. Furthermore, biomarker-assisted treatment will reduce the burden of antifungal-induced toxicities by limiting drug use in identified patients who do not require preventative treatment. However, a practical limitation of these biomarker-driven strategies will be the requirement for regular testing of high-risk patients to monitor IC risk over time, something that would be of considerable cost to the healthcare service [152].
The future combined use of blood culture and biomarker tests represents a potential new era in mapping Candida diseases in different patient groups by enabling earlier and more accurate detection of blood-borne candidemia and deep-seated candidiasis, as well as transforming patient care and disease management through improved antifungal stewardship [126,127].
7.4. Novel Antifungal Targets
In addition to improved antifungal stewardship aimed at preserving the utility of antifungals through the combined use of blood culture and biomarker tests, there is precedence for new antifungal drugs given the paucity of currently available treatment options [15,74]. Novel antifungals that target Candida pathogenesis mechanisms, such as hyphal morphogenesis and biofilm formation, are of particular interest compared to current agents that target cell viability via fungistatic or fungicidal activity [74,154,155]. By targeting pathogenesis rather than cell viability itself, future antifungals adopting this framework may benefit from reduced toxicities and subsequent improvements in therapeutic index as well as decreased risks of drug resistance [155]. As described previously, these are some of the main limiting factors associated with current treatments. These antifungals will likely have a narrower spectrum of activity than current broad-spectrum drugs due to their species-specific target of pathogenesis mechanisms. Clinical utility will therefore rely heavily on accurate diagnosis of IC, an area continuing to rely predominantly on the use of slow, insensitive culture-based systems [156,157]. However, increasing development and use of biomarker tests that offer faster, more sensitive disease diagnosis and indications may help realise the potential of such novel antifungals. To date, research has focused on preclinical studies with several compounds showing strong efficacy and promise in vivo in mouse challenge models [156,158,159]. Therefore, although these novel antifungals hold promise, it is likely to be some time before any such agent is available for use in the clinic.
8. Conclusions
Invasive candidiasis (IC) is the most common IFD worldwide and represents a continuing public health problem. With shifting patterns of epidemiology largely resulting from healthcare activities, changes in disease management and patient care are urgently needed.
Elucidated from population-based surveillance, increases in overall disease incidence are well-established as the population of immunocompromised individuals susceptible to life-threatening infection has expanded. However, recent data do suggest that in certain settings this trend may be reversing, with improvements in patient risk factor management implicated in these findings. As disease incidence has generally increased, so too have the requirement and clinical use of appropriate antifungal treatments. This has been exacerbated by the use of slow, insensitive culture-based diagnostics, meaning treatment guidelines often recommend empirical or prophylactic strategies for high-risk patients in the absence of proven infection. Many patients therefore receive unnecessary antifungals, with important consequences for their care and disease management more widely, such as severe toxicities and increased risks of drug resistance in an already limited antifungal arsenal. Widespread overuse of antifungals through non-specific preventative strategies is one of the key drivers in Candida spp. distribution shifts towards more resistant strains [112,114,160,161]. In particular, an increasing contribution from non-albicans Candida spp. at the expense of C. albicans is observed globally.
Ever-increasing susceptible populations for opportunistic IC infection and global epidemiologic shifts towards species with greater drug resistance mean that changes in disease management and patient care to preserve and expand the utility of antifungals are of paramount importance. Decreasing unnecessary use of antifungals and their associated selective pressures is an important factor in this, achievable through the use of biomarker tests that allow clinicians to promptly identify and rule out infection. Combined use of biomarker tests and current culture-based diagnostics may therefore yield transformations in disease management and patient care through improved antifungal stewardship. Furthermore, the development of novel antifungals with improved characteristics, targeting Candida pathogenesis mechanisms over cell viability, represents a longer-term strategy to expand the repertoire of treatment options beyond the limited number licensed today.
Author Contributions
Conceptualisation, B.Y.P. and C.R.T.; writing—original draft preparation, B.Y.P.; writing—review and editing, B.Y.P. and C.R.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
This study did not generate any new data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Primers 2018, 11, 18026. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of invasive candidiasis: A persistent public health problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.C.; Gurr, S.J.; Cuomo, C.A.; Blehert, D.S.; Jin, H.; Stukenbrock, E.H.; Stajich, J.E.; Kahmann, R.; Boone, C.; Denning, D.W.; et al. Threats posed by the fungal kingdom to humans, wildlife and agriculture. mBio 2020, 11, e00449-20. [Google Scholar] [CrossRef] [PubMed]
- Yapar, N. Epidemiology and risk factors for invasive candidiasis. Ther. Clin. Risk Manag. 2014, 10, 95–105. [Google Scholar] [CrossRef]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and multi-national prevalence of fungal diseases—Estimate precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Toda, M.; Williams, S.R.; Berkow, E.L.; Farley, M.M.; Harrison, L.H.; Bonner, L.; Marceaux, K.M.; Hollick, R.; Zhang, A.Y.; Schaffner, W.; et al. Population-based active surveillance for culture confirmed candidemia—Four sites, United States, 2012–2016. MMWR Surveill. Summ. 2019, 68, 1–15. [Google Scholar] [CrossRef]
- Saville, S.P.; Lazzell, A.L.; Monteagudo, C.; Lopez-Ribot, J. Engineered control of cell morphology in vivo reveals distinct roles for yeast and filamentous forms of Candida albicans during infection. Eukaryot. Cell 2003, 2, 1053–1060. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Moet, G.J.; Messer, S.A.; Jones, R.N.; Castanheira, M. Candida bloodstream infections: Comparison of species distributions and antifungal resistance patterns in community-onset and nosocomial isolates in the SENTRY Antimicrobial Surveillance Program, 2008–2009. Antimicrob. Agents Chemother. 2011, 55, 561–566. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Finding the “missing 50%” of invasive candidiasis: How nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin. Infect. Dis. 2013, 56, 1284–1292. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Diagnosing invasive candidiasis. J. Clin. Microbiol. 2018, 56, e01909-17. [Google Scholar] [CrossRef]
- Garey, K.W.; Rege, M.; Pai, M.P.; Mingo, D.E.; Suda, K.J.; Turpin, R.S.; Bearden, D.T. Time to initiation of fluconazole therapy impacts mortality in patients with candidemia: A multi-institutional study. Clin. Infect. Dis. 2006, 43, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical practice guideline for the management of candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef] [PubMed]
- Cornely, O.A.; Bassetti, M.; Calandra, T.; Garbino, J.; Kullberg, B.J.; Lortholary, O.; Meersseman, W.; Akova, M.; Arendrup, M.C.; Arikan-Akdagli, S.; et al. ESCMID Guideline for the diagnosis and management of Candida diseases 2012: Non-neutropenic adult patients. Clin. Microbiol. Infect. 2012, 7, 19–37. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Righi, E.; Montravers, P.; Cornely, O.A. What has changed in the treatment of invasive candidiasis? A look at the past 10 years and ahead. J. Antimicrob. Chemother. 2018, 73, i14–i25. [Google Scholar] [CrossRef] [PubMed]
- Ostrosky-Zeichner, L.; Casadevall, A.; Galgiani, J.N.; Odds, F.C.; Rex, J.H. An insight into the antifungal pipeline: Selected new molecules and beyond. Nat. Rev. Drug Discov. 2010, 9, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Thomas-Rüddel, D.; Schalttmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk factors for invasive candida infection in critically ill patients—a systematic review and meta-analysis. Chest 2021, 21, 04112. [Google Scholar]
- Eggimann, P.; Pittet, D. Candida colonization index and subsequent infection in critically ill surgical patients: 20 years later. Intensive Care Med. 2014, 40, 1429–1448. [Google Scholar] [CrossRef]
- Pittet, D.; Monod, M.; Suter, P.M.; Frenk, E.; Auckenthaler, R. Candida colonization and subsequent infections in critically ill surgical patients. Ann. Surg. 1994, 220, 751–758. [Google Scholar] [CrossRef]
- Charles, P.E.; Dalle, F.; Aube, H.; Doise, J.M.; Queno, J.P.; Aho, L.S.; Chavanet, P.; Blettery, B. Candida spp. colonization significance in critically ill medical patients: A prospective study. Intensive Care Med. 2015, 31, 393–400. [Google Scholar] [CrossRef]
- Ostrosky-Zeichner, L.; Pappas, P.G. Invasive candidiasis in the intensive care unit. Crit. Care Med. 2006, 34, 857–863. [Google Scholar] [CrossRef]
- Kumamoto, C.A. Inflammation and gastrointestinal Candida colonization. Curr. Opin. Microbiol. 2011, 14, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Guinan, J.; Wang, S.; Hazbun, T.R.; Yadav, H.; Thangamani, S. Antibiotic-induced decreases in the levels of microbial-derived short-chain fatty acids correlate with increased gastrointestinal colonization of Candida albicans. Sci. Rep. 2019, 9, 8872. [Google Scholar] [CrossRef] [PubMed]
- Seelbinder, B.; Chen, J.; Brunke, S.; Vazquez-Uribe, R.; Santhaman, R.; Meyer, A.C.; Lino, F.; Chan, K.F.; Loos, D.; Imamovic, L.; et al. Antibiotics create a shift from mutualism to competition in human gut communities with a longer-lasting impact on fungi than bacteria. Microbiome 2020, 8, 133. [Google Scholar] [CrossRef]
- Teoh, F.; Pavelka, N. How chemotherapy increases the risk of systemic candidiasis in cancer patients: Current paradigm and future directions. Pathogens 2016, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of immune dysfunction in end-stage renal disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.F.; Rodrigues, M.E.; Henriques, M. Candida spp. infections in patients with diabetes mellitus. J. Clin. Med. 2019, 8, 76. [Google Scholar] [CrossRef] [PubMed]
- Nucci, M.; Marr, K.A. Emerging fungal diseases. Clin. Infect. Dis. 2005, 41, 521–526. [Google Scholar] [CrossRef]
- Boxer, L.A. How to Approach Neutropenia; Hematology, ASH Education Program: Washington, DC, USA, 2012; pp. 174–182. [Google Scholar]
- Paphitou, N.I.; Ostrosky-Zeichner, L.; Rex, J.H. Rules for identifying patients at increased risk for candidal infections in the surgical intensive care unit: Approach to developing practical criteria for systemic use in antifungal prophylaxis trials. Med. Mycol. 2005, 43, 235–243. [Google Scholar] [CrossRef]
- Agvald-Ohman, C.; Klingspor, L.; Hjelmqvist, H.; Edlund, C. Invasive candidiasis in long-term patients at a multidisciplinary intensive care unit: Candida colonization index, risk factors, treatment and outcome. Scand. J. Infect. Dis. 2008, 40, 145–153. [Google Scholar] [CrossRef]
- Jorda-Marcos, R.; Alvarez-Lerma, F.; Jurado, M.; Palomar, M.; Nolla-Salas, J.; Leon, M.A.; Leon, C. Risk factors for candidemia in critically ill patients: A prospective surveillance study. Mycoses 2007, 50, 302–310. [Google Scholar] [CrossRef]
- Pappas, P.G. Invasive candidiasis. Infect. Dis. Clin. N. Am. 2006, 20, 485–506. [Google Scholar] [CrossRef] [PubMed]
- Lass-Flörl, C. The changing face of epidemiology of invasive fungal disease in Europe. Mycoses 2009, 52, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Sievert, D.M.; Ricks, P.; Edwards, J.R.; Schneider, A.; Patel, J.; Srinivasan, A.; Kallen, A.; Limbago, B.; Fridkin, S. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect. Control Hosp. Epidemiol. 2013, 34, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Wisplinghoff, H.; Bischoff, T.; Tallent, S.M.; Seifert, H.; Wenzel, R.P.; Edmond, M.B. Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 2004, 39, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Cleaveland, A.A.; Harrison, L.H.; Farley, M.M.; Hollick, R.; Stein, B.; Chiller, T.M.; Lockhart, S.R.; Park, B.J. Declining incidence of candidemia and the shifting epidemiology of Candida resistance in two US metropolitan areas, 2008—2013: Results from population-based surveillance. PLoS ONE 2015, 10, e0120452. [Google Scholar] [CrossRef]
- Ota, K.V.; McGowan, K.L. Declining incidence of candidemia in a tertiary inpatient paediatric population. J. Clin. Microbiol. 2012, 50, 1048–1050. [Google Scholar] [CrossRef]
- Magill, S.S.; Edwards, J.R.; Bamberg, W.; Beldavs, Z.G.; Dumyati, G.; Kainer, M.A.; Lynfield, R.; Maloney, M.; McAllister-Hollod, L.; Nadle, J.; et al. Multistate point-prevalence survey of healthcare associated infections. N. Engl. J. Med. 2014, 370, 1198–1208. [Google Scholar] [CrossRef]
- Asmundsdottir, L.R.; Erlendsdottir, H.; Gottfredsson, M. Nationwide study of candidemia, antifungal use, and antifungal drug resistance in Iceland, 2000 to 2011. J. Clin. Microbiol 2013, 51, 841–848. [Google Scholar] [CrossRef]
- Risum, M.; Astvad, K.; Johansen, H.K.; Schonheyder, H.C.; Rosenvinge, F.; Knudsen, J.D.; Hare, R.; Datcu, R.; Roder, B.L.; Antsupova, V.S.; et al. Update 2016–2018 of the nationwide Danish Fungaemia Surveillance Study: Epidemiologic changes in a 15-year perspective. J. Fungi 2021, 7, 491. [Google Scholar] [CrossRef]
- Eggimann, P.; Que, Y.; Revelly, J.P.; Pagani, J.L. Preventing invasive Candida infections. Where could we do better? J. Hosp. Infect. 2015, 89, 302–308. [Google Scholar] [CrossRef]
- Enoch, D.A.; Yang, H.; Aliyu, S.H.; Micallef, C. The changing epidemiology of invasive fungal infections. Methods Mol. Biol. 2017, 1508, 17–65. [Google Scholar] [PubMed]
- Kami, M.; Machida, U.; Okuzumi, K.; Matsumura, T.; Si, S.M.; Hori, A.; Kashima, T.; Kanda, Y.; Takaue, Y.; Sakamaki, H.; et al. Effects of fluconazole prophylaxis on fungal blood cultures: An autopsy-based study involving 720 patients with haematological malignancy. Br. J. Haemotol. 2002, 117, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Cleaveland, A.A.; Farley, M.M.; Harrison, L.H.; Stein, B.; Hollick, R.; Lockhart, S.R.; Magill, S.S.; Derado, G.; Park, B.J.; Chiller, T.M. Changes in incidence and antifungal drug resistance in candidemia: Results from population-based laboratory surveillance in Atlanta and Baltimore, 2008-2011. Clin. Infect. Dis. 2012, 55, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Poikonen, E.; Lyytikäinen, O.; Anttila, V.J.; Koivula, I.; Lumio, J.; Kotilainen, P.; Syrjälä, H.; Ruutu, P. Secular trend in candidemia and the use of fluconazole in Finland, 2004–2007. BMC Infect. Dis. 2010, 10, 312. [Google Scholar] [CrossRef]
- Kao, A.S.; Brandt, M.E.; Pruitt, W.R.; Conn, L.A.; Perkins, B.A.; Stephens, D.S.; Baughman, W.S.; Reingold, A.L.; Rothrock, G.A.; Pfaller, M.A.; et al. The epidemiology of candidemia in two United States cities: Results of a population based active surveillance. Clin. Infect. Dis. 1999, 29, 1164–1170. [Google Scholar] [CrossRef] [PubMed]
- Hajjeh, R.A.; Sofair, A.N.; Harrison, L.H.; Lyon, G.M.; Arthington-Skaggs, B.A.; Mirza, S.A.; Phelan, M.; Morgan, J.; Lee-Yang, W.; Ciblak, M.A.; et al. Incidence of bloodstream infections due to Candida species and in vitro susceptibilities of isolates collected from 1998 to 2000 in a population-based active surveillance program. J. Clin. Microbiol. 2004, 42, 1519–1527. [Google Scholar] [CrossRef]
- Oeser, C.; Lamagni, T.; Heath, P.T.; Sharland, M.; Ladhani, S. The epidemiology of neonatal and pediatric candidemia in England and Wales, 2000–2009. Pediatr. Infect. Dis. J. 2013, 32, 23–26. [Google Scholar] [CrossRef]
- Alp, S.; Arikan-Akdagli, S.; Gulmez, D.; Ascioglu, S.; Uzun, O.; Akova, M. Epidemiology of candidemia in a tertiary care university hospital: 10-year experience with 381 candidemia episodes between 2001 and 2010. Mycoses 2015, 58, 498–505. [Google Scholar] [CrossRef]
- Segal, B.H.; Almyroudis, N.G.; Battiwalla, M.; Herbrecht, R.; Perfect, J.R.; Walsh, T.J.; Wingard, J.R. Prevention and early treatment of invasive fungal infection in patients with cancer and neutropenia and in stem cell transplant recipients in the era of newer broad-spectrum antifungal agents and diagnostic adjuncts. Clin. Infect. Dis. 2007, 44, 402–409. [Google Scholar] [CrossRef]
- Vivolo-Kantor, A.M.; Seth, P.; Gladden, R.M.; Mattson, C.L.; Baldwin, G.T.; Kite-Powell, A.; Coletta, M.A. Vital signs: Trends in emergency department visits for suspected opioid overdoses—United States, July 2016–September 2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 279–285. [Google Scholar] [CrossRef]
- Seth, P.; Scholl, L.; Rudd, R.A.; Bacon, S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Asmundsdottir, L.R.; Erlendsdottir, H.; Gottfredsson, M. Increasing incidence of candidemia: Results from a 20-year nationwide study in Iceland. J. Clin. Microbiol. 2002, 40, 3482–3492. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hesstvedt, L.; Arendrup, M.C.; Poikonen, E.; Klingpor, L.; Friman, V.; Nordoy, I. Differences in epidemiology of candidemia in the Nordic countries—What is to blame? Mycoses 2017, 60, 11–19. [Google Scholar] [CrossRef]
- Sandven, P.; Bevanger, L.; Digranes, A.; Haukland, H.H.; Mannsaker, T.; Gaustad, P. Candidemia in Norway (1991–2003): Results from a nationwide study. J. Clin. Microbiol. 2006, 44, 1977–1981. [Google Scholar] [CrossRef] [PubMed]
- Poikonen, E.; Lyytikäinen, O.; Anttila, V.J.; Ruutu, P. Candidemia in Finland, 1995–1999. Emerg. Infect. Dis. 2003, 9, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, J.; Chryssanthou, E.; Klingspor, L.; Johansson, A.G.; Ljungman, P.; Svensson, E.; Sjölin, J. Candidemia in Sweden: A nationwide prospective observational study. Clin. Microbiol. Infect. 2013, 19, E218–E221. [Google Scholar] [CrossRef]
- Almirante, B.; Rodriguez, D.; Park, B.J.; Cuenca-Estrella, M.; Planes, A.M.; Almela, M.; Mensa, J.; Sanchez, F.; Ayats, J.; Gimenez, M.; et al. Epidemiology and predictors of mortality in cases of Candida bloodstream infection: Results from population-based surveillance, Barcelona, Spain, from 2002 to 2003. J. Clin. Microbiol. 2005, 43, 1829–1835. [Google Scholar] [CrossRef]
- Arendrup, M.C.; Bruun, B.; Christensen, J.J.; Fuursted, K.; Johansen, H.K.; Kjaeldgaard, P.; Knudsen, J.D.; Kristensen, L.; Moller, J.; Nielsen, L.; et al. National surveillance of fungemia in Denmark (2004–2009). J. Clin. Microbiol. 2010, 49, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Arendrup, M.C.; Dzajic, E.; Jensen, R.H.; Johansen, H.K.; Kjaeldgaard, P.; Knudsen, J.D.; Kristensen, L.; Leitz, C.; Lemming, L.E.; Nielsen, L.; et al. Epidemiological changes with potential implication for antifungal prescription recommendations for fungaemia: Data from a nationwide fungaemia surveillance programme. Clin. Microbiol. Infect. 2013, 19, E343–E353. [Google Scholar] [CrossRef]
- Jensen, J.S.; Hein, L.; Lundgren, B.; Bestle, M.H.; Mohr, T.; Andersen, M.H.; Loken, J.; Tousi, H.; Soe-Jensen, P.; Lauritsen, A.; et al. Invasive Candida infections and the harm from antibacterial drugs in critically ill patients: Data from a randomized, controlled trial to determine the role of ciprofloxacin, piperacillin-tazobactam, meropenem, and cefuroxime. Crit. Care Med. 2015, 43, 594–602. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.; Benjamin, D.K.; Calandra, T.F.; Edwards, J.E.; Filler, S.G.; Fisher, J.F.; Kullberg, B.J.; Ostrosky-Zeichner, L.; et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Disease Society of America. Clin. Infect. Dis. 2009, 48, 503–535. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ami, R. Treatment of invasive candidiasis: A narrative review. J. Fungi 2018, 4, 97. [Google Scholar] [CrossRef] [PubMed]
- Gruszecki, W.I.; Gagos, M.; Herec, M.; Kernen, P. Organisation of antibiotic amphotericin B in model lipid membranes: A mini review. Cell Mol. Biol. Lett. 2003, 8, 161–170. [Google Scholar] [PubMed]
- Bates, D.W.; Su, L.; Yu, D.T.; Chertow, G.M.; Seger, D.L.; Gomes, D.R.; Dasbach, E.J.; Platt, R. Mortality and cost of acute renal failure associated with amphotericin B therapy. Clin. Infect. Dis. 2001, 32, 686–693. [Google Scholar] [CrossRef]
- Fanos, V.; Cataldi, L. Amphotericin B-induced nephrotoxicity: A review. J. Chemother. 2000, 12, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.J.; Finberg, R.W.; Arndt, C.; Hiemenz, J.; Schwartz, C.; Bodensteiner, D.; Pappas, P.; Seibel, N.; Greenberg, R.N.; Dummer, S.; et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N. Engl. J. Med. 1999, 340, 764–771. [Google Scholar] [CrossRef]
- Garnacho-Montero, J.; Ortiz-Leyba, C.; Garmendia, J.L.; Jimenez, F. Life-threatening adverse event after amphotericin B lipid complex treatment in a patient treated previously with amphotericin B deoxycholate. Clin. Infect. Dis. 1998, 26, 1016. [Google Scholar] [CrossRef]
- Saravolatz, L.D.; Ostrosky-Zeichner, L.; Marr, K.A.; Rex, J.H.; Cohen, S.H. Amphotericin B: Time for a new “gold standard”. Clin. Infect. Dis. 2003, 37, 415–425. [Google Scholar] [CrossRef]
- Dupont, B. Overview of the lipid formulations of amphotericin B. J. Antimicrob. Chemother. 2002, 49, 31–36. [Google Scholar] [CrossRef]
- Hitchcock, C.A.; Dickinson, K.; Brown, S.B.; Evans, E.G.; Adams, D.J. Interaction of azole antifungal antibiotics with cytochrome P-450-dependent 14 alpha-sterol demethylase purified from Candida albicans. Biochem. J. 1990, 266, 475–480. [Google Scholar] [CrossRef]
- Abi-Said, D.; Anaissie, E.; Uzun, O.; Raad, I.; Pinzcowski, H.; Vartivarian, S. The epidemiology of hematogenous candidiasis caused by different Candida species. Clin. Infect. Dis. 1997, 24, 1122–1128. [Google Scholar] [CrossRef] [PubMed]
- Dennin, D.W. Echinocandin antifungal drugs. Lancet 2003, 362, 1142–1151. [Google Scholar] [CrossRef]
- Odds, F.C.; Brown, A.J.; Gow, N.A. Antifungal agents: Mechanisms of action. Trends Microbiol. 2003, 11, 272–279. [Google Scholar] [CrossRef]
- Garcia-Effron, G.; Katiyar, S.K.; Park, S.; Edlind, T.D.; Perlin, D.S. A naturally occurring proline-to-alanine amino acid change in Fks1p in Candida parapsilosis, Candida orthopsilosis, and Candida metapsilosis accounts for reduced echinocandin susceptibility. Antimicrob. Agents Chemother. 2008, 52, 2305–2312. [Google Scholar] [CrossRef]
- Douglas, C.M.; D’Ippolito, J.A.; Shei, G.J.; Meinz, M.; Onishi, J.; Marrinan, J.A.; Li, W.; Abruzzo, G.K.; Flattery, A.; Bartizal, K.; et al. Identification of the FKS1 gene of candida albicans as the essential target of 1,3-beta-D-glucan synthase inhibitors. Antimicrob. Agents Chemother. 1997, 41, 2471–2479. [Google Scholar] [CrossRef]
- Perlin, D.S. Resistance to echinocandin-class antifungal drugs. Drug Resist. Update 2007, 10, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Hazen, K.C. New and emerging yeast pathogens. Clin. Microbiol. Rev. 1995, 8, 462–478. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Rare and emerging opportunistic fungal pathogens: Concern for resistance beyond Candida albicans and Aspergillus fumigatus. J. Clin. Microbiol. 2004, 42, 4419–4431. [Google Scholar] [CrossRef]
- Banerjee, S.N.; Emori, T.G.; Culver, D.H.; Gaynes, R.P.; Jarvis, W.R.; Horan, T.; Edwards, J.R.; Tolson, J.; Henderson, T.; Martone, W.J. Secular trends in nosocomial primary bloodstream infections in the United States, 1980–1989. Am. J. Med. 1991, 91, S86–S89. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Castanheira, M.; Messer, S.A.; Moet, G.J.; Jones, R.N. Echinocandin and triazole antifungal susceptibility profiles for Candida spp., Cryptococcus neoformans, and Aspergillus fumigatus: Application of new CLSI clinical breakpoints and epidemiologic cut-off values to characterise resistance in the SENTRY Antimicrobial Surveillance Program (2009). Diagn. Microbiol. Infect. Dis. 2011, 69, 45–50. [Google Scholar]
- Satoh, K.; Makimura, K.; Hasumi, Y.; Nishiyama, Y.; Uchida, K.; Yamaguchi, H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 2009, 53, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.D.; Samsa, G.P.; Schell, W.A.; Reller, L.B.; Perfect, J.R.; Alexander, B.D. Quantification of Candida CFU in initial positive blood cultures. J. Clin. Microbiol. 2011, 49, 2878–2883. [Google Scholar] [CrossRef] [PubMed]
- Horvath, L.L.; George, B.J.; Murray, C.K.; Harrison, L.S.; Hospenthal, D.R. Direct comparison of the BACTEC 9240 and BacT/Alert 3D automated blood culture systems for Candida growth detection. J. Clin. Microbiol. 2004, 42, 115–118. [Google Scholar] [CrossRef]
- Horvath, L.L.; Hospenthal, D.R.; Murray, C.K.; Dooley, D.P. Detection of simulated candidemia by the BACTEC 9240 system with plus aerobic/F and anaerobic/F blood culture bottles. J. Clin. Microbiol. 2003, 41, 4714–4717. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCarty, T.P.; Pappas, P.G. Invasive candidiasis. Infect. Dis. Clin. North Am. 2016, 30, 103–124. [Google Scholar] [CrossRef]
- Alexander, B.D.; Schell, W.A.; Miller, J.L.; Long, G.D.; Perfect, J.R. Candida glabrata fungemia in transplant patient receiving voriconazole after fluconazole. Transplantation 2005, 80, 868–871. [Google Scholar] [CrossRef] [PubMed]
- Baran, J.; Muckatira, B.; Khatib, R. Candidemia before and during the fluconazole era: Prevalence, type of species and approach to treatment in a tertiary care community hospital. Scand. J. Infect. Dis. 2001, 33, 137–139. [Google Scholar]
- Lin, M.Y.; Carmeli, Y.; Zumsteg, J.; Flores, E.L.; Tolentino, J.; Sreeramoju, P.; Weber, S.G. Prior antimicrobial therapy and risk for hospital-acquired Candida glabrata and Candida krusei fungemia: A case-case-control study. Antimicrob. Agents Chemother. 2005, 49, 4555–4560. [Google Scholar] [CrossRef]
- Blumberg, H.M.; Jarvis, W.R.; Soucie, J.M.; Edwards, J.E.; Patterson, J.E.; Pfaller, M.A.; Rangel-Frausto, M.S.; Rinaldi, M.G.; Saiman, L.; Wiblin, R.T.; et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: The NEMIS prospective multicentre study. The National Epidemiology of Mycosis Survey. Clin. Infect. Dis. 2001, 33, 177–186. [Google Scholar] [CrossRef]
- White, M.H. The contribution of fluconazole to the changing epidemiology of invasive candidal infections. Clin. Infect. Dis. 1997, 24, 1129–1130. [Google Scholar] [CrossRef][Green Version]
- Oeser, C.; Vergnano, S.; Naidoo, R.; Anthony, M.; Chang, J.; Chow, P.; Clarke, P.; Embleton, N.; Kennea, N.; Pattnayak, S.; et al. Neonatal invasive fungal infection in England 2004–2010. Clin. Microbiol. Infect. 2014, 20, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Rubin, L.G.; Vasishtha, S.; Tucci, V.; Sood, S.K. Emergence of Candida parapsilosis as the predominant species causing candidemia in children. Clin. Infect. Dis. 1998, 26, 1086–1088. [Google Scholar] [CrossRef] [PubMed]
- Lupetti, A.; Tavanti, A.; Davini, P.; Ghelardi, E.; Corsini, V.; Merusi, I.; Boldrini, A.; Campa, M.; Senesi, S. Horizontal transmission of Candida parapsilosis candidemia in a neonatal intensive care unit. J. Clin. Microbiol. 2002, 40, 2363–2369. [Google Scholar] [CrossRef] [PubMed]
- Branchini, M.L.; Pfaller, M.A.; Rhine-Chalberg, J.; Frempong, T.; Isenberg, H.D. Genotypic variation and slime production among blood and catheter isolates of Candida parapsilosis. J. Clin. Microbiol. 1994, 32, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.A.; Slavinski, S.A.; Morgan, J.; Lott, T.; Arthington-Skaggs, B.A.; Brandt, M.E.; Webb, R.M.; Currier, M.; Flowers, R.H.; Fridkin, S.K.; et al. Epidemiologic and molecular characterization of an outbreak of Candida parapsilosis bloodstream infections in a community hospital. J. Clin. Microbiol. 2004, 42, 4468–4472. [Google Scholar] [CrossRef] [PubMed]
- Fridkin, S.K. The changing face of fungal infections in healthcare settings. Clin. Infect. Dis. 2005, 41, 1455–1460. [Google Scholar]
- Almirante, B.; Rodriguez, D.; Cuenca-Estrella, M.; Almela, M.; Sanchez, F.; Ayats, J.; Alonso-Tarres, C.; Rodriquez-Tudela, J.L.; Pahissa, A. Epidemiology, risk factors, and prognosis of Candida parapsilosis bloodstream infections: Case-control population-based surveillance study of patients in Barcelona, Spain, from 2002–2003. J. Clin. Microbiol 2006, 44, 1681–1685. [Google Scholar] [CrossRef]
- Kontoyiannis, D.P.; Vaziri, I.; Hanna, H.A.; Boktour, M.; Thornby, J.; Hachem, R.; Bodey, G.P.; Raad, I.I. Risk factors for Candida tropicalis fungemia in patients with cancer. Clin. Infect. Dis. 2001, 33, 1676–1681. [Google Scholar] [CrossRef]
- Marr, K.A.; Seidel, K.; White, T.C.; Bowden, R.A. Candidemia in allogenic blood and marrow transplant recipients: Evolution of risk factors after the adoption of prophylactic fluconazole. J. Infect. Dis. 2000, 181, 309–316. [Google Scholar] [CrossRef]
- Castanheira, M.; Messer, S.A.; Rhomberg, P.R.; Pfaller, M.A. Antifungal susceptibility patterns of a global collection of fungal isolates: Results of the SENTRY Antifungal Surveillance Program (2013). Diagn. Microbiol. Infect. Dis. 2016, 85, 200–204. [Google Scholar] [CrossRef]
- Merz, W.G.; Karp, J.E.; Schron, D.; Saral, R. Increased incidence of fungemia caused by Candida krusei. J. Clin. Microbiol. 1986, 24, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Singh, S.; Rudramurthy, S.M.; Ghosh, A.K.; Jayashree, M.; Narayana, Y.; Ray, P.; Chakrabarti, A. Candidemia in a tertiary care centre of developing country: Monitoring possible change in spectrum of agents and antifungal susceptibility. Indian J. Med. Microbiol. 2020, 38, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Ding, Y.; Tian, G.; Yang, K.; Deng, J.; Li, G.; Liu, J. A seven-year surveillance study of the epidemiology, antifungal susceptibility, risk factors and mortality of candidemia among paediatric and adult inpatients in a tertiary teaching hospital in China. Antimicrob. Resist. Infect. Control 2020, 9, 133. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Tiang, G.; Ding, Y.; Yang, K.; Liu, J.; Deng, J. Surveillance study of the prevalence, species distribution, antifungal susceptibility, risk factors and mortality of invasive candidiasis in a tertiary teaching hospital in Southwest China. BMC Infect. Dis. 2019, 19, 939. [Google Scholar] [CrossRef]
- Xiao, Z.; Wang, Q.; Zhu, F.; An, Y. Epidemiology, species distribution, antifungal susceptibility and mortality risk factors of candidemia among critically ill patients: A retrospective study from 2011–2017 in a teaching hospital in China. Antimicrob. Resist. Infect. Control 2019, 8, 89. [Google Scholar] [CrossRef]
- Boonslip, S.; Homkaew, A.; Phumisantiphong, U.; Nutalai, D.; Wongsuk, T. Species distribution, antifungal susceptibility and molecular epidemiology of candida species causing candidemia in a tertiary care hospital in Bangkok, Thailand. J. Fungi 2021, 7, 577. [Google Scholar] [CrossRef]
- Yamin, D.; Husin, A.; Harun, A. Distribution of candidemia in a Malaysian tertiary care hospital revealed predominance of Candida parapsilosis. Trop. Biomed. 2020, 37, 903–910. [Google Scholar]
- Puig-Asensio, M.; Padilla, B.; Garnacho-Montero, J.; Zaragoza, O.; Aguado, J.M.; Zaragoza, R.; Montejo, M.; Munoz, P.; Ruiz-Camps, I.; Cuenca-Estrella, M.; et al. Epidemiology and predictive factors for early and late mortality in Candida bloodstream infections: A population-based surveillance in Spain. Clin. Microbiol. Infect. 2014, 20, O245–O254. [Google Scholar] [CrossRef]
- Barchiesi, F.; Orsetti, E.; Gesuita, R.; Skrami, E.; Manso, E. Epidemiology, clinical characteristics, and outcome of candidemia in a tertiary referral center in Italy from 2010–2014. Infection 2016, 44, 205–213. [Google Scholar] [CrossRef]
- Nucci, M.; Queiroz-Telles, F.; Alvarado-Matute, T.; Tiraboschi, I.N.; Cortes, J.; Zurita, J.; Guzman-Blanco, M.; Santolaya, M.E.; Thompson, L.; Sifuentes-Osornio, J.; et al. Epidemiology of candidemia in Latin America: A laboratory-based survey. PLoS ONE 2013, 8, e59373. [Google Scholar] [CrossRef]
- Perlin, D.S. Echinocandin resistance in Candida. Clin. Infect. Dis. 2015, 61, S612–S617. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, O.; Bille, J.; Fluckiger, U.; Eggimann, P.; Ruef, C.; Garbino, J.; Calandra, T.; Glauser, M.; Tauber, M.G.; Pittet, D. Epidemiology of candidemia in Swiss tertiary care hospitals: Secular trends, 1991–2000. Clin. Infect. Dis. 2004, 38, 311–320. [Google Scholar] [CrossRef]
- Adam, K.; Osthoff, M.; Lamoth, F.; Conen, A.; Erard, V.; Boggian, K.; Schreiber, P.W.; Zimmerli, S.; Bochud, P.; Neofytos, D.; et al. Trends of the epidemiology of candidemia in Switzerland: A 15-year FUNGINOS survey. Open Forum Infect. Dis. 2021, 8, ofab471. [Google Scholar] [CrossRef] [PubMed]
- Hesstvedt, L.; Gaustad, P.; Andersen, C.T.; Haarr, E.; Hannula, R.; Haukland, H.H.; Hermansen, N.-O.; Larssen, K.W.; Mylvaganam, H.; Ranheim, T.E.; et al. Twenty-two years of candidemia surveillance: Results from a Norwegian national study. Clin. Microbiol. Infect. 2015, 21, 938–945. [Google Scholar] [CrossRef]
- Chalmers, C.; Gaur, S.; Chew, J.; Wright, T.; Kumar, A.; Mathur, S.; Wan, W.Y.; Gould, I.M.; Leanord, A.; Bal, A.M. Epidemiology and management of candidemia—A retrospective, multicentre study in five hospitals in the UK. Mycoses 2011, 54, e795–e800. [Google Scholar] [CrossRef] [PubMed]
- Vannini, M.; Emery, S.; Lieutier-Colas, F.; Legueult, K.; Mondain, V.; Retur, N.; Gastaud, L.; Pomares, C.; Hasseine, L. Epidemiology of candidemia in NICE area, France: A five-year study of antifungal susceptibility and mortality. J. Mycol. Med. 2022, 32, 101210. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, M.; Weber, T.; Denker, T.; Winterland, S.; Wichmann, D.; Rohde, H.; Ozga, A.-K.; Fischer, M.; Kluge, S. Epidemiology, clinical characteristics, and outcome of candidemia in critically ill patients in Germany: A single-centre retrospective 10-year analysis. Ann. Intensive Care 2020, 10, 142. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Ansaldi, F.; Nicolini, L.; Malfatto, E.; Molinari, M.P.; Mussap, M.; Rebesco, B.; Pallavicini, F.B.; Icardi, G.; Viscoli, C. Incidence of candidemia and relationship with fluconazole use in an intensive care unit. J. Antimicrob. Chemother. 2009, 64, 625–629. [Google Scholar] [CrossRef]
- Rodriguez, L.; Bustamante, B.; Huaroto, L.; Agurto, C.; Illescas, R.; Ramirez, R.; Diaz, A.; Hidalgo, J. A multi-centric study of Candida bloodstream infection in Lima-Callao, Peru: Species distribution, antifungal resistance and clinical outcomes. PLoS ONE 2017, 12, e0175172. [Google Scholar] [CrossRef]
- Rodrigues, D.K.B.; Bonfietti, L.X.; Garcia, R.A.; Araujo, M.R.; Rodrigues, J.S.; Gimenes, V.M.F.; Melhem, M.S.C. Antifungal susceptibility profile of Candida clinical isolates from 22 hospitals of Sao Paulo state, Brazil. Braz. J. Med. Biol. Res. 2021, 54, e10928. [Google Scholar]
- Jones, J.M. Laboratory diagnosis of invasive candidiasis. Clin. Microbiol. Rev. 1990, 3, 32–45. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ellepola, A.; Morrison, C. Laboratory diagnosis of invasive candidiasis. J. Microbiol. 2005, 43, 65–84. [Google Scholar] [PubMed]
- Leon, C.; Ruiz-Santana, S.; Saavedra, P.; Castro, C.; Loza, A.; Zakariya, I.; Ubeda, A.; Parra, M.; Macias, D.; Tomas, J.I.; et al. Contribution of Candida biomarkers and DNA detection for the diagnosis of invasive candidiasis in ICU patients with severe abdominal conditions. Crit. Care 2016, 20, 149. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Rapid diagnosis of invasive candidiasis: Ready for prime-time? Curr. Opin, Infect. Dis. 2019, 32, 546–552. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Nguyen, M.H. Non-culture diagnostics for invasive candidiasis: Promise and unintended consequences. J. Fungi 2018, 4, 27. [Google Scholar] [CrossRef]
- Clancy, C.J.; Shields, R.K.; Nguyen, M.H. Invasive candidiasis in various patient populations: Incorporating non-culture diagnostic tests into rational management strategies. J Fungi 2016, 2, 10. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.H.; Wissel, M.C.; Shields, R.K.; Salomoni, M.A.; Hao, B.; Press, E.G.; Shields, R.M.; Cheng, S.; Mitsani, D.; Vadnerkar, A.; et al. Performance of Candida real-time polymerase chain reaction, β-D-glucan assay, and blood cultures in the diagnosis of invasive candidiasis. Clin. Infect. Dis. 2012, 54, 1240–1248. [Google Scholar] [CrossRef]
- Cuenca-Estrella, M.; Verweij, P.E.; Arendrup, M.C.; Arikan-Akdagli, S.; Bille, J.; Donnelly, J.P.; Jensen, H.E.; Lass-Flörl, C.; Richardson, M.D.; Akova, M.; et al. ESCMID guideline for the diagnosis of Candida diseases 2012: Diagnostic procedures. Clin. Microbiol. Infect. 2012, 18, 9–18. [Google Scholar] [CrossRef]
- Ness, M.J.; Vaughan, W.P.; Woods, G.L. Candida antigen latex test for detection of invasive candidiasis in immunocompromised patients. J. Infect. Dis. 1989, 159, 495–502. [Google Scholar] [CrossRef]
- Telenti, A.; Steckelberg, J.M.; Stockman, L.; Edson, R.S.; Roberts, G.D. Quantitative blood cultures in candidemia. Mayo Clin. Proc. 1991, 66, 1120–1123. [Google Scholar] [CrossRef]
- Beyda, N.D.; Amadio, J.; Rodriguez, J.R.; Malinowski, K.; Garey, K.W.; Wanger, A.; Ostrosky-Zeichner, L. In vitro evaluation of BacT/Alert FA blood culture bottles and T2 Candida assay for detection of Candida in the presence of antifungals. J. Clin. Microbiol. 2018, 56, e00471-18. [Google Scholar] [CrossRef]
- Odds, F.C. Sabouraud(’s) agar. J. Med. Vet. Mycol. 1991, 29, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Odds, F.C.; Bernaerts, R. CHROMagar Candida, a new differential isolation medium for presumptive isolation of clinically important Candida species. J. Clin. Microbiol. 1994, 32, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Horvath, L.L.; Hospenthal, D.R.; Murray, C.K.; Dooley, D.P. Direct isolation of Candida spp. from blood cultures on the chromogenic medium CHROMagar Candida. J. Clin. Microbiol. 2003, 41, 2629–2632. [Google Scholar] [CrossRef] [PubMed]
- Bernal, S.; Mazuelos, E.M.; Garcia, M.; Aller, A.I.; Martinez, M.A.; Gutierrez, M.J. Evaluation of CHROMagar Candida medium for the isolation and presumptive identification of species of Candida of clinical importance. Diagn. Microbiol. Infect. Dis. 1996, 24, 201–204. [Google Scholar] [CrossRef]
- Hospenthal, D.R.; Murray, C.K.; Beckius, M.L.; Green, J.A.; Dooley, D.P. Persistence of pigment production by yeast isolates grown on CHROMagar Candida medium. J. Clin. Microbiol. 2002, 40, 4768–4770. [Google Scholar] [CrossRef] [PubMed]
- Powell, H.L.; Sand, C.A.; Rennie, R.P. Evaluation of CHROMagar Candida for presumptive identification of clinically important Candida species. Diagn. Microbiol. Infect. Dis. 1998, 32, 201–204. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Houston, A.; Coffmann, S. Application of CHROMagar Candida for rapid screening of clinical specimens for Candida albicans, Candida tropicalis, Candida krusei, and Candida (Torulopsis) glabrata. J. Clin. Microbiol. 1996, 34, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Hospenthal, D.R.; Beckius, M.L.; Floyd, K.L.; Horvath, L.L.; Murray, C.K. Presumptive identification of Candida species other than C. albicans, C. krusei, and C. tropicalis with the chromogenic medium CHROMagar Candida. Ann. Clin. Microbiol. Antimicrob. 2006, 5, 1. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Undiagnosed invasive candidiasis: Incorporating non-culture diagnostics into rational prophylactic and pre-emptive antifungal strategies. Expert Rev. Anti Infect. Ther. 2014, 12, 731–734. [Google Scholar] [CrossRef]
- Matsui, D. Current issues in pediatric medication adherence. Paediatr. Drugs 2007, 9, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Monday, L.M.; Acosta, T.P.; Alangaden, G. T2 Candida for the diagnosis and management of invasive candida infections. J. Fungi 2021, 7, 178. [Google Scholar] [CrossRef] [PubMed]
- Diez, A.; Carrano, G.; Bregon-Villahoz, M.; Cuetara, M.S.; Garcia-Ruiz, J.C.; Fernandez-de-Larrinoa, I.; Moragues, M.D. Biomarkers for the diagnosis of invasive candidiasis in immunocompetent and immunocompromised patients. Diagn. Microbiol. Infect. Dis. 2021, 101, 115509. [Google Scholar] [CrossRef] [PubMed]
- Moragues, M.D.; Ortiz, N.; Iruretagoyena, J.R.; Garcia-Ruiz, J.C.; Amutio, E.; Rojas, A.; Mendoza, J.; Quindos, G.; Emeterio, J. Evaluation of a new commercial test (Candida albicans IFA IgG) for the serodiagnosis of invasive candidiasis. Enferm. Infecc. Microbiol. Clin. 2004, 22, 83–88. [Google Scholar] [CrossRef]
- Zervou, F.N.; Zacharioudakis, I.M.; Kurpewski, J.; Mylonakis, E. T2 Magnetic Resonance for fungal diagnosis. Methods Mol. Biol. 2017, 1508, 305–319. [Google Scholar] [PubMed]
- Beyda, N.D.; Alam, M.J.; Garey, K.W. Comparison of the T2Dx instrument with T2 Candida assay and automated blood culture in the detection of Candida species using seeded blood samples. Diagn. Microbiol. Infect. Dis. 2013, 77, 324–326. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Nguyen, M.L.; Cheng, S.; Huang, H.; Fan, G.; Jaber, R.A.; Wingard, J.R.; Cline, C.; Nguyen, M.H. Immunoglobulin G responses to a panel of Candida albicans antigens as accurate and early markers for the presence of systemic candidiasis. J. Clin. Microbiol. 2008, 46, 1647–1654. [Google Scholar] [CrossRef][Green Version]
- Budhavari, S. What’s new in diagnostics? Fungitell®: 1,3 beta-D glucan assay. South Afr. Epidemiol. Infect. 2009, 24, 37–38. [Google Scholar] [CrossRef]
- Mikulska, M.; Calandra, T.; Sanguinetti, M.; Poulain, D.; Viscoli, C. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: Recommendations from the Third European Conference on Infections in Leukemia. Crit. Care 2010, 14, R222. [Google Scholar] [CrossRef]
- Wheat, L.J. Approach to the diagnosis of invasive aspergillosis and candidiasis. Clin. Chest Med. 2009, 30, 367–377. [Google Scholar] [CrossRef]
- Hanson, K.E.; Pfeiffer, C.D.; Lease, E.D.; Balch, A.H.; Zaas, A.K.; Perfect, J.R.; Alexander, B.D. β-D-glucan surveillance with preemptive anidulafungin for invasive candidiasis in intensive care unit patients: A randomized pilot study. PLoS ONE 2012, 7, e42282. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, E.G.; Denning, D.W. Prophylactic echinocandin: Is there a subgroup of intensive care unit patients who benefit? Clin. Infect. Dis. 2014, 58, 1227–1229. [Google Scholar] [CrossRef] [PubMed]
- Clatworthy, A.E.; Pierson, E.; Hung, D. Targeting virulence: A new paradigm for antimicrobial therapy. Nat. Chem. Biol. 2007, 3, 541–548. [Google Scholar] [CrossRef]
- Gauwerky, K.; Borelli, C.; Korting, H. Targeting virulence: A new paradigm for antifungals. Drug Discov. Today 2009, 14, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Romo, J.A.; Pierce, C.G.; Chaturvedi, A.K.; Lazzell, A.L.; McHardy, S.F.; Saville, S.P.; Lopez-Ribot, J.L. Development of anti-virulence approaches for candidiasis via a novel series of small molecule inhibitors of Candida albicans filamentation. mBio 2017, 8, e01991-17. [Google Scholar] [CrossRef]
- Thompson, D.S.; Carlisle, P.L.; Kadosh, D. Coevolution of morphology and virulence in Candida species. Eukaryot. Cell 2011, 10, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Pierce, C.G.; Chaturvedi, A.K.; Lazzell, A.L.; Powell, A.T.; Saville, S.P.; McHardy, S.F.; Lopez-Ribot, J.L. A novel small molecule inhibitor of biofilm formation, filamentation and virulence with low potential for the development of resistance. NPJ Biofilms Microbiomes 2015, 1, 15012. [Google Scholar] [CrossRef] [PubMed]
- Shareck, J.; Belhumeur, P. Modulation of morphogenesis in Candida albicans by various small molecules. Eukaryot. Cell 2011, 10, 1004–1012. [Google Scholar] [CrossRef]
- Perlin, D.S.; Shor, E.; Zhao, Y. Update on Antifungal Drug Resistance. Curr. Clin. Microbiol. Rep. 2015, 2, 84–95. [Google Scholar] [CrossRef]
- Perlin, D.S.; Rauternaa-Richardson, R.; Alastruey-Izquierdo, A. The global problem of antifungal resistance: Prevalence, mechanisms, and management. Lancet Infect. Dis. 2017, 17, e383–e392. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).