A New Early Predictor of Fatal Outcome for COVID-19 in an Italian Emergency Department: The Modified Quick-SOFA
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Characteristics of Patients in Relation to the Primary Outcome
3.1.1. IHM
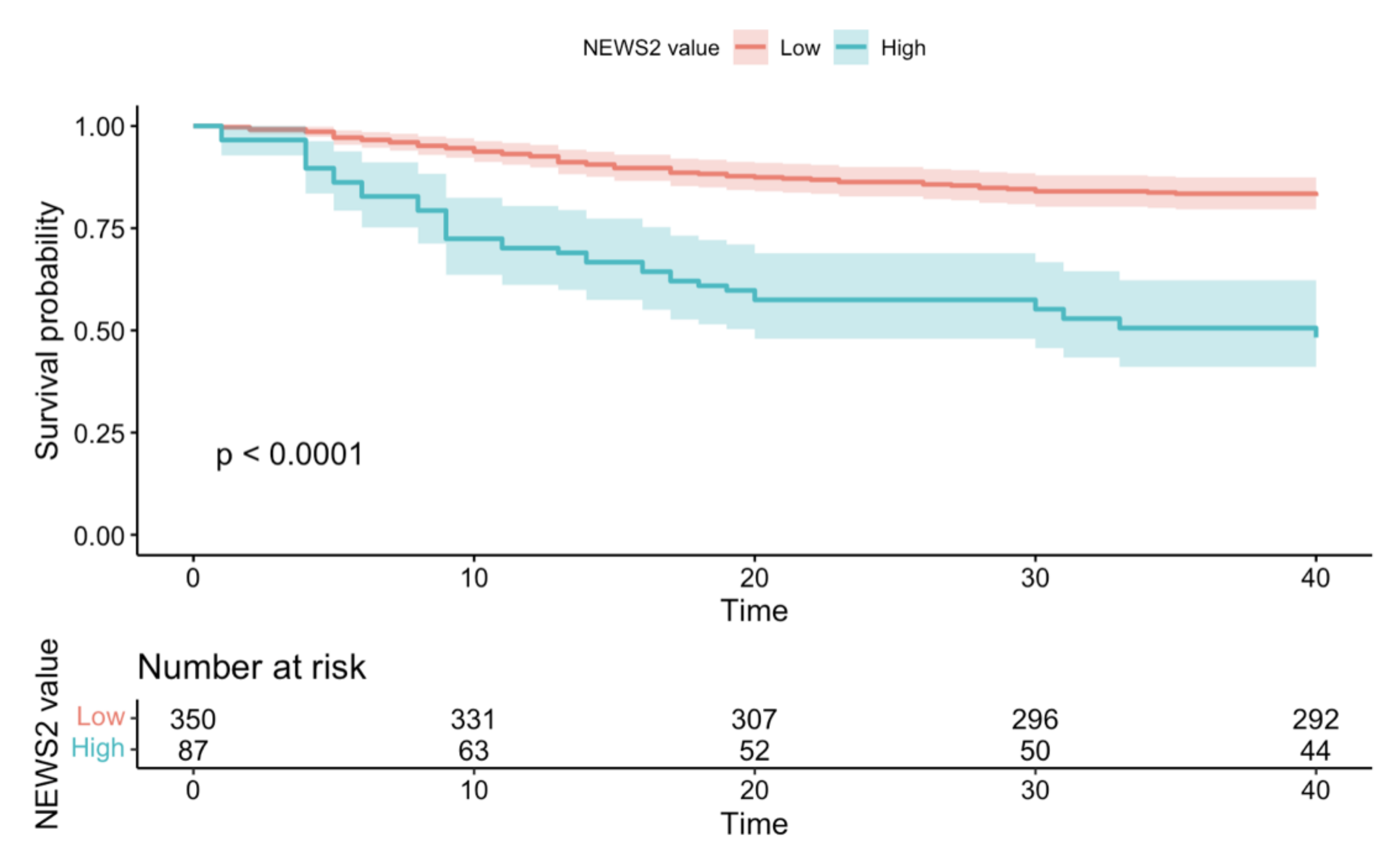
3.1.2. 30-Day Mortality
3.2. Logistic Regression and Supplementary Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| CAD | Coronary artery disease |
| CCI | Charlson comorbidity index |
| CHF | Congestive heart failure |
| CKD | Chronic kidney disease |
| COPD | Chronic obstructive pulmonary disease |
| CVA | Cerebrovascular accident |
| ED | Emergency department |
| FiO2 | Inspired fraction of oxygen |
| HR | Hazard ratio |
| ICU | Intensive care unit |
| IHM | In-hospital mortality |
| MqSOFA | Modified quick sequential organ failure assessment |
| NEWS-2 | National early warning score 2 |
| NPV | Negative predictive value |
| OR | Odds ratio |
| S/F | SpO2/FiO2 ratio |
| SD | Standard deviation |
| SpO2 | Peripheral oxygen saturation |
| PaO2 | Arterial partial pressure of oxygen |
| PPV | Positive predictive value |
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Vahidy, F.S.; Drews, A.L.; Masud, F.N.; Schwartz, R.L.; Askary, B.B.; Boom, M.L.; Phillips, R.A. Characteristics and Outcomes of COVID-19 Patients During Initial Peak and Resurgence in the Houston Metropolitan Area. JAMA 2020, 324, 998–1000. [Google Scholar] [CrossRef] [PubMed]
- Rotondo, J.C.; Martini, F.; Maritati, M.; Mazziotta, C.; Di Mauro, G.; Lanzillotti, C.; Barp, N.; Gallerani, A.; Tognon, M.; Contini, C. SARS-CoV-2 Infection: New Molecular, Phylogenetic, and Pathogenetic Insights. Efficacy of Current Vaccines and the Potential Risk of Variants. Viruses 2021, 13, 1687. [Google Scholar] [CrossRef]
- Contini, C.; Di Nuzzo, M.; Barp, N.; Bonazza, A.; De Giorgio, R.; Tognon, M.; Rubino, S. The novel zoonotic COVID-19 pandemic: An expected global health concern. J. Infect. Dev. Ctries. 2020, 14, 254–264. [Google Scholar] [CrossRef] [Green Version]
- Wolff, D.; Nee, S.; Hickey, N.S.; Marschollek, M. Risk factors for Covid-19 severity and fatality: A structured literature review. Infection 2021, 49, 15–28. [Google Scholar] [CrossRef]
- Myrstad, M.; Ihle-Hansen, H.; Tveita, A.A.; Andersen, E.L.; Nygård, S.; Tveit, A.; Berge, T. National Early Warning Score 2 (NEWS-2) on admission predicts severe disease and in-hospital mortality from Covid-19—A prospective cohort study. Scand. J. Trauma. Resusc. Emerg. Med. 2020, 28, 66. [Google Scholar] [CrossRef]
- Jang, J.G.; Hur, J.; Hong, K.S.; Lee, W.; Ahn, J.H. Prognostic Accuracy of the SIRS, qSOFA, and NEWS for Early Detection of Clinical Deterioration in SARS-CoV-2 Infected Patients. J. Korean Med. Sci. 2020, 35, e234. [Google Scholar] [CrossRef]
- Liu, S.; Yao, N.; Qiu, Y.; He, C. Predictive performance of SOFA and qSOFA for in-hospital mortality in severe novel coronavirus disease. Am. J. Emerg Med. 2020, 38, 2074–2080. [Google Scholar] [CrossRef]
- Guarino, M.; Gambuti, E.; Alfano, F.; De Giorgi, A.; Maietti, E.; Strada, A.; Ursini, F.; Volpato, S.; Caio, G.; Contini, C.; et al. Predicting in-hospital mortality for sepsis: A comparison between qSOFA and modified qSOFA in a 2-year single-centre retrospective analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 825–831. [Google Scholar] [CrossRef]
- Guarino, M.; Perna, B.; De Giorgi, A.; Gambuti, E.; Alfano, F.; Catanese, E.M.; Volpato, S.; Strada, A.; Caio, G.; Contini, C.; et al. A 2-year retrospective analysis of the prognostic value of MqSOFA compared to lactate, NEWS and qSOFA in patients with sepsis. Infection 2022. [Google Scholar] [CrossRef] [PubMed]
- Alberdi-Iglesias, A.; Martín-Rodríguez, F.; Ortega Rabbione, G.; Rubio-Babiano, A.I.; Núñez-Toste, M.G.; Sanz-García, A.; Del Pozo Vegas, C.; Castro Villamor, M.A.; Martín-Conty, J.L.; Jorge-Soto, C.; et al. Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines 2021, 9, 1036. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Wang, C.; Liu, X.; Gao, W.; Bai, X.; Li, Z. Lessons Learned Comparing Immune System Alterations of Bacterial Sepsis and SARS-CoV-2 Sepsis. Front. Immunol. 2020, 11, 598404. [Google Scholar] [CrossRef] [PubMed]
- Tuty Kuswardhani, R.A.; Henrina, J.; Pranata, R.; Anthonius Lim, M.; Lawrensia, S.; Suastika, K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2020, 14, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Available online: https://covid19.who.int/ (accessed on 13 March 2022).
- CDC COVID-19 Response Team. MMWR Morb Mortal SARS-CoV-2 B.1.1.529 (Omicron) Variant—United States, 1–8 December 2021. Wkly. Rep. 2021, 70, 1731–1734. [Google Scholar]
- Twohig, K.A.; Nyberg, T.; Zaidi, A.; Thelwall, S.; Sinnathamby, M.A.; Aliabadi, S.; Seaman, S.R.; Harris, R.J.; Hope, R.; Lopez-Bernal, J.; et al. COVID-19 Genomics UK (COG-UK) consortium. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: A cohort study. Lancet Infect. Dis. 2022, 22, 35–42. [Google Scholar] [CrossRef]
- Abdullah, F.; Myers, J.; Basu, D.; Tintinger, G.; Ueckermann, V.; Mathebula, M.; Ramlall, R.; Spoor, S.; de Villiers, T.; Van der Walt, Z.; et al. Decreased severity of disease during the first global omicron variant covid-19 outbreak in a large hospital in tshwane, South Africa. Int. J. Infect. Dis. 2022, 116, 38–42. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef] [Green Version]
- Alhazzani, W.; Evans, L.; Alshamsi, F.; Møller, M.H.; Ostermann, M.; Prescott, H.C.; Arabi, Y.M.; Loeb, M.; Ng Gong, M.; Fan, E.; et al. Surviving Sepsis Campaign Guidelines on the Management of Adults with Coronavirus Disease 2019 (COVID-19) in the ICU: First Update. Crit. Care Med. 2021, 49, e219–e234. [Google Scholar] [CrossRef]
- Carr, E.; Bendayan, R.; Bean, D.; Stammers, M.; Wang, W.; Zhang, H.; Searle, T.; Kraljevic, Z.; Shek, A.; Phan, H.T.T.; et al. Evaluation and improvement of the National Early Warning Score (NEWS-2) for COVID-19: A multi-hospital study. BMC Med. 2021, 19, 23. [Google Scholar] [CrossRef]
- Covino, M.; Sandroni, C.; Santoro, M.; Sabia, L.; Simeoni, B.; Bocci, M.G.; Ojetti, V.; Candelli, M.; Antonelli, M.; Gasbarrini, A.; et al. Predicting intensive care unit admission and death for COVID-19 patients in the emergency department using early warning scores. Resuscitation 2020, 156, 84–91. [Google Scholar] [CrossRef]
- Fan, G.; Tu, C.; Zhou, F.; Liu, Z.; Wang, Y.; Song, B.; Gu, X.; Wang, Y.; Wei, Y.; Li, H.; et al. Comparison of severity scores for COVID-19 patients with pneumonia: A retrospective study. Eur. Respir. J. 2020, 56, 2002113. [Google Scholar] [CrossRef]
- Chan, E.D.; Chan, M.M.; Chan, M.M. Pulse oximetry: Understanding its basic principles facilitates appreciation of its limitations. Respir. Med. 2013, 107, 789–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inciardi, R.M.; Adamo, M.; Lupi, L.; Cani, D.S.; Di Pasquale, M.; Tomasoni, D.; Italia, L.; Zaccone, G.; Tedino, C.; Fabbricatore, D.; et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. 2020, 41, 4591. [Google Scholar] [CrossRef] [PubMed]
- Rey, J.R.; Caro-Codón, J.; Rosillo, S.O.; Iniesta, Á.M.; Castrejón-Castrejón, S.; Marco-Clement, I.; Martín-Polo, L.; Merino-Argos, C.; Rodríguez-Sotelo, L.; García-Veas, J.M.; et al. CARD-COVID Investigators. Heart failure in COVID-19 patients: Prevalence, incidence and prognostic implications. Eur. J. Heart Fail. 2020, 22, 2205–2215. [Google Scholar] [CrossRef]
- Noor, F.M.; Islam, M.M. Prevalence and Associated Risk Factors of Mortality Among COVID-19 Patients: A Meta-Analysis. J. Community Health 2020, 45, 1270–1282. [Google Scholar] [CrossRef]
- Barros, D.; Borges-Machado, F.; Ribeiro, Ó.; Carvalho, J. Dementia and COVID-19: The Ones Not to Be Forgotten. Am. J. Alzheimers Dis. Other Demen. 2020, 35, 1533317520947505. [Google Scholar] [CrossRef] [PubMed]
- Flythe, J.E.; Assimon, M.M.; Tugman, M.J.; Chang, E.H.; Gupta, S.; Shah, J.; Sosa, M.A.; Renaghan, A.D.; Melamed, M.L.; Wilson, F.P.; et al. STOP-COVID Investigators. Characteristics and Outcomes of Individuals with Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States. Am. J. Kidney Dis. 2021, 77, 190–203. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.A.; Ma, W.; Sikavi, D.R.; Drew, D.A.; Nguyen, L.H.; Bowyer, R.C.E.; Cardoso, M.J.; Fall, T.; Freidin, M.B.; Gomez, M.; et al. COPE consortium. Cancer and Risk of COVID-19 Through a General Community Survey. Oncologist 2021, 26, e182–e185. [Google Scholar] [CrossRef]
- Leung, J.M.; Niikura, M.; Yang, C.W.T.; Sin, D.D. COVID-19 and COPD. Eur. Respir. J. 2020, 13, 2002108. [Google Scholar] [CrossRef]
- Higham, A.; Mathioudakis, A.; Vestbo, J.; Singh, D. COVID-19 and COPD: A narrative review of the basic science and clinical outcomes. Eur. Respir. Rev. 2020, 29, 200199. [Google Scholar] [CrossRef] [PubMed]

| MqSOFA | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | Points | ||||||
| Blood Pressure ≤ 100 mmHg | 1 | ||||||
| Respiratory Rate ≥ 22/min | 1 | ||||||
| Altered Mentation | 1 | ||||||
| SpO2/FiO2 ratio | ≥316 | 0 | |||||
| 236–315 | 1 | ||||||
| ≤235 | 2 | ||||||
| NEWS-2 | |||||||
| Parameter | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
| Respiratory Rate | ≤8 | 9–11 | 12–20 | 21–24 | ≥25 | ||
| O2 Saturation Scale 1 (%) | ≤91 | 92–93 | 94–95 | ≥96 | |||
| O2 Saturation Scale 2 (%) | ≤83 | 84–85 | 86–87 | 88–92 ≥ 93 on air | 93–94 on oxygen | 95–96 on oxygen | ≥97 on oxygen |
| Supplemental O2 | Yes | No | |||||
| Temperature (°C) | ≤35.0 | 35.1–36.0 | 36.1–38.0 | 38.1–39.0 | ≥39.1 | ||
| Systolic Blood Pressure (mmHg) | ≤90 | 91–100 | 101–110 | 111–219 | ≥220 | ||
| Heart Rate | ≤40 | 41–50 | 51–90 | 91–110 | 111–130 | ≥131 | |
| Level of Consciousness (AVPU) | Alert | Verbal, Pain, Unresponsive | |||||
| Patients, n | 437 |
|---|---|
| Female, n (%) | 206 (47.1) |
| Age (years), mean (SD) | 47.79 (18.53) |
| Hospital Unit, (%) | |
| Discharged | 0 (0) |
| Low-intensity care | 316 (72.3) |
| Intermediate-intensity care | 121 (27.7) |
| High-intensity care | 0 (0) |
| Comorbidities | |
| CAD (%) | 44 (10.2) |
| CHF (%) | 37 (8.5) |
| Peripheral vascular disease (%) | 11 (2.5) |
| CVA (%) | 90 (20.8) |
| Dementia (%) | 106 (24.4) |
| COPD (%) | 56 (12.8) |
| Connective tissue disease (%) | 46 (10.6) |
| Peptic ulcer disease (%) | 5 (1.2) |
| Liver disease (%) | 7 (1.6) |
| Uncomplicated diabetes mellitus (%) | 66 (15.2) |
| Diabetes mellitus with end-organ damage (%) | 25 (5.8) |
| Hemiplegia | 7 (1.6) |
| Moderate to severe CKD (%) | 40 (9.2) |
| Cancer without metastasis (%) | 41 (9.4) |
| Moderate to severe liver disease (%) | 2 (0.5) |
| Metastatic tumour (%) | 10 (2.3) |
| CCI, mean (SD) | 2.73 (2.08) |
| NEWS-2, mean (SD) | 4.75 (3.11) |
| MqSOFA, mean (SD) | 1.76 (1.04) |
| LOS, mean (SD) | 14.53 (15.48) |
| IHM | 30-Days Mortality | |||||
|---|---|---|---|---|---|---|
| Variables | Survived (n = 344) | Deceased (n = 93) | p | Survived (n = 341) | Deceased (n = 96) | p |
| Female, n (%) | 154 (44.8) | 52 (55.9) | 0.073 | 152 (44.6) | 54 (56.2) | 0.056 |
| Age (years), mean (SD) | 43.88 (18.26) | 62.25 (10.76) | <0.001 | 43.71 (18.14) | 62.29 (11.25) | <0.001 |
| Comorbidities | ||||||
| CAD (%) | 28 (8.2) | 16 (17.4) | 0.017 | 27 (8.0) | 17 (17.9) | 0.009 |
| CHF (%) | 22 (6.5) | 15 (16.1) | 0.006 | 20 (5.9) | 17 (17.7) | 0.001 |
| Peripheral vascular disease (%) | 7 (2.1) | 4 (4.3) | 0.398 | 7 (2.1) | 4 (4.2) | 0.435 |
| CVA (%) | 56 (16.5) | 34 (36.6) | <0.001 | 50 (14.8) | 40 (41.7) | <0.001 |
| Dementia (%) | 66 (19.4) | 40 (43.0) | <0.001 | 62 (18.3) | 44 (45.8) | <0.001 |
| COPD (%) | 44 (12.8) | 12 (12.9) | 1.000 | 45 (13.4) | 11 (11.5) | 0.752 |
| Connective tissue disease (%) | 35 (10.3) | 11 (11.8) | 0.814 | 33 (9.8) | 13 (13.5) | 0.388 |
| Peptic ulcer disease (%) | 4 (1.2) | 1 (1.1) | 1.000 | 3 (0.9) | 2 (2.1) | 0.674 |
| Liver disease (%) | 6 (1.8) | 1 (1.1) | 0.995 | 6 (1.8) | 1 (1.0) | 0.959 |
| Uncomplicated diabetes mellitus (%) | 48 (14.1) | 18 (19.4) | 0.279 | 46 (13.6) | 20 (20.8) | 0.117 |
| Diabetes mellitus with end-organ damage (%) | 18 (5.3) | 7 (7.5) | 0.571 | 18 (5.3) | 7 (7.3) | 0.635 |
| Hemiplegia | 7 (2.1) | 0 (0.0) | 0.352 | 7 (2.1) | 0 (0.0) | 0.335 |
| Moderate to severe CKD (%) | 21 (6.2) | 19 (20.4) | <0.001 | 20 (5.9) | 20 (20.8) | <0.001 |
| Cancer without metastasis (%) | 24 (7.0) | 17 (18.3) | 0.002 | 26 (7.7) | 15 (15.6) | 0.032 |
| Moderate to severe liver disease (%) | 0 (0.0) | 2 (2.2) | 0.065 | 0 (0.0) | 2 (2.1) | 0.072 |
| Metastatic tumour (%) | 6 (1.8) | 4 (4.3) | 0.290 | 7 (2.1) | 3 (3.1) | 0.824 |
| CCI, mean (SD) | 2.43 (1.87) | 3.86 (2.42) | <0.001 | 2.42 (1.91) | 3.86 (2.26) | <0.001 |
| NEWS-2 ≥ 7, n (%) | 46 (13.4) | 41 (44.1) | <0.001 | 46 (13.5) | 41 (42.7) | <0.001 |
| MqSOFA ≥ 2, n (%) | 42 (12.2) | 40 (43.3) | <0.001 | 42 (12.3) | 40 (41.7) | <0.001 |
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| In-hospital mortality | ||||||
| NEWS-2 | 3.56 | (2.34–5.41) | <0.001 | 2.37 | (1.53–3.66) | <0.001 |
| Age (years) | 1.08 | (1.06–1.10) | <0.001 | 1.08 | (1.05–1.10) | <0.001 |
| Sex (F) | 1.60 | (1.06–2.42) | <0.05 | 0.83 | (0.53–1.30) | 0.406 |
| CCI | 1.22 | (1.14–1.31) | <0.001 | 1.05 | (0.96–1.14) | 0.273 |
| 30-day mortality | ||||||
| NEWS-2 | 3.65 | (2.42–5.50) | <0.001 | 2.44 | (1.60–3.72) | <0.001 |
| Age (years) | 1.08 | (1.06–1.10) | <0.001 | 1.07 | (1.05–1.09) | <0.001 |
| Sex (F) | 1.58 | (1.06–2.38) | <0.05 | 0.85 | (0.55–1.32) | 0.472 |
| CCI | 1.24 | (1.16–1.33) | <0.001 | 1.08 | (0.99–1.17) | 0.077 |
| In-hospital mortality | ||||||
| MqSOFA | 3.76 | (2.47–5.72) | <0.001 | 2.19 | (1.39–3.43) | <0.001 |
| Age (years) | 1.08 | (1.06–1.10) | <0.001 | 1.07 | (1.05–1.10) | <0.001 |
| Sex (F) | 1.60 | (1.06–2.42) | <0.05 | 0.77 | (0.49–1.21) | 0.258 |
| CCI | 1.22 | (1.14–1.31) | <0.001 | 1.05 | (0.97–1.15) | 0.233 |
| 30-day mortality | ||||||
| MqSOFA | 3.86 | (2.56–5.82) | <0.001 | 2.23 | (1.45–3.44) | <0.001 |
| Age (years) | 1.08 | (1.06–1.10) | <0.001 | 1.07 | (1.05–1.09) | <0.001 |
| Sex (F) | 1.58 | (1.06–2.38) | <0.05 | 0.79 | (0.51–1.23) | 0.292 |
| CCI | 1.24 | (1.16–1.33) | <0.001 | 1.08 | (1.00–1.18) | 0.062 |
| In-Hospital Mortality | 30-Day Mortality | |||
|---|---|---|---|---|
| NEWS-2 | MqSOFA | NEWS-2 | MqSOFA | |
| Sensitivity | 85.1% | 85.1% | 84.3% | 84.2% |
| Specificity | 47.1% | 48.8% | 47.1% | 48.8% |
| PPV | 86.6% | 87.8% | 86.5% | 87.7% |
| NPV | 44.1% | 43.0% | 42.7% | 41.7% |
| Diagnostic accuracy | 77.6% | 78.3% | 76.9% | 77.6% |
| Diagnostic OR | 5.11 | 5.43 | 4.78 | 5.09 |
| Youden index | 0.32 | 0.35 | 0.31 | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guarino, M.; Perna, B.; Remelli, F.; Cuoghi, F.; Cesaro, A.E.; Spampinato, M.D.; Maritati, M.; Contini, C.; De Giorgio, R. A New Early Predictor of Fatal Outcome for COVID-19 in an Italian Emergency Department: The Modified Quick-SOFA. Microorganisms 2022, 10, 806. https://doi.org/10.3390/microorganisms10040806
Guarino M, Perna B, Remelli F, Cuoghi F, Cesaro AE, Spampinato MD, Maritati M, Contini C, De Giorgio R. A New Early Predictor of Fatal Outcome for COVID-19 in an Italian Emergency Department: The Modified Quick-SOFA. Microorganisms. 2022; 10(4):806. https://doi.org/10.3390/microorganisms10040806
Chicago/Turabian StyleGuarino, Matteo, Benedetta Perna, Francesca Remelli, Francesca Cuoghi, Alice Eleonora Cesaro, Michele Domenico Spampinato, Martina Maritati, Carlo Contini, and Roberto De Giorgio. 2022. "A New Early Predictor of Fatal Outcome for COVID-19 in an Italian Emergency Department: The Modified Quick-SOFA" Microorganisms 10, no. 4: 806. https://doi.org/10.3390/microorganisms10040806
APA StyleGuarino, M., Perna, B., Remelli, F., Cuoghi, F., Cesaro, A. E., Spampinato, M. D., Maritati, M., Contini, C., & De Giorgio, R. (2022). A New Early Predictor of Fatal Outcome for COVID-19 in an Italian Emergency Department: The Modified Quick-SOFA. Microorganisms, 10(4), 806. https://doi.org/10.3390/microorganisms10040806









