Abstract
Salmonella spp. are among the most frequent causes of foodborne diseases, and the increasing occurrence of MDR strains is an additional cause for concern. In the three-year period 2019–2021, we collected Salmonella spp. strains isolated from different food categories analysed in the context of Regulation (EC) No 2073/2005 in order to assess their antibiotic susceptibility profiles and ESBL production. To determine the susceptibility profiles and identify MDR strains, we used the Kirby–Bauer method to test 17 antibiotics. Double-disc and PCR testing then allowed us to assess the production of ESBLs and the presence of beta-lactamase resistance genes. Phenotypic tests showed that 36 out of 67 strains were MDR and 52.7% of these were ESBL producers. Finally, molecular investigations conducted on ESBL-producing strains revealed the presence of blaSHV, blaCTX-M and blaTEM genes. Our results confirmed the prevalence of S. Infantis, an MDR strain and ESBL producer, in chicken meat. This suggests that further research on the prevalence of antibiotic resistance genes (ARGs) in foodborne strains is needed, especially from a One Health perspective.
1. Introduction
Salmonellosis is a commonly reported gastrointestinal infection in humans, and an important cause of foodborne outbreaks. In the European Union (EU) in 2019, the number of confirmed salmonellosis cases was 87,923; in 2020, the number was 57,702, which was the lowest recorded number since 2007 because of the impacts of the withdrawal of the United Kingdom from the EU and the COVID-19 pandemic [1]. The main route of infection is ingestion of food or water contaminated with Salmonella spp., Gram-negative, facultative anaerobic bacilli belonging to the Enterobacteriaceae family [2,3]. Salmonella is ubiquitous in the human food chain and is one of the most important foodborne pathogens in the world. In particular, S. Enteritidis, S. Typhimurium, monophasic S. Typhimurium, S. Infantis and S. Derby are the five serotypes most commonly involved in human infections [1]. In the EU, microbiological food controls carried out in the context of Regulation (EC) No. 2073/2005 found the highest percentages of Salmonella-positive samples in egg products, poultry meat and poultry products, which are the most critical sources of Salmonella spp. transmission to humans [1,4].
Although salmonellosis is generally self-limited and usually does not require specific treatment, antibiotic therapy with quinolones, beta-lactams, aminoglycosides, tetracyclines or sulfamethoxazole–trimethoprim is necessary in severe cases [5]. However, the overuse of antibiotics has contributed to the selection of MDR Salmonella strains, i.e., resistant simultaneously to three or more classes of antibiotics, including those most commonly prescribed for the treatment of salmonellosis [6]. The spread of MDR Salmonella represents a significant health problem, as it causes longer hospitalisations, prolonged illnesses and higher mortality rates than susceptible strains [7,8]. The World Health Organization estimates that of the 100,000 cases of salmonellosis each year, a large number are caused by MDR Salmonella [9], with the majority acquired through the consumption of contaminated food of animal origin, particularly beef, pork and poultry products [10,11].
In Enterobacteriaceae such as Salmonella, the main mechanism of resistance to beta-lactams is the acquisition of genes (bla gene) that encode for beta-lactamase hydrolytic enzymes, which inactivate the antibiotic [12]. Extended-spectrum beta-lactamases (ESBLs), which hydrolyse first-, second-, and third-generation penicillins and cephalosporins, are encoded by genes belonging to the TEM, SHV, and CTX-M families, including multiple variants of the blaTEM, blaSHV and blaCTX-M genes [13]. These ESBL genes have been identified in bacteria isolated from animals and food products of animal origin [7,14], as well as from other types of foods, such as seafood [15], raw vegetables [16] and ready-to-eat (RTE) foods [17], suggesting the possible role of the food production chain as a reservoir for this group of bacteria. Indeed, factors such as selective pressure in animal and environmental microbiomes, the circulation of bacteria between animals and environment and ineffective food safety management can contribute to the presence and persistence of antibiotic-resistant bacteria (ARB) and antibiotic resistance genes (ARGs) in the food production context [18].
The aim of this study was to evaluate the MDR potential of Salmonella strains isolated in the period from January 2019 to December 2021 from food samples analysed in the context of the Regulation (EC) No 2073/2005 [4]. Furthermore, for every MDR Salmonella strain, ESBL production and ESBL gene presence were determined by double-disc diffusion and PCR tests, respectively.
2. Materials and Methods
2.1. Salmonella Isolation
From January 2019 to December 2021, 493 food samples, subjected to controls according to European Community legislation, were analysed [4]. Specifically, these samples were poultry meat (n = 145), pig meat (n = 106), beef (n = 54), bivalve molluscs (n = 109), eggs (n = 43) and sprouted seeds (n = 36).
Isolation according to ISO 6579-1:2017 was performed, and strains were then identified by biochemical enzymatic assays and serotyping, according to the Kauffmann–White–Le Minor scheme (Supplementary Materials Table S1) [19].
2.2. Antibiotic Susceptibility Profile Determination
Antibiotic susceptibility was assessed using the Kirby–Bauer method on Mueller Hinton agar medium (Oxoid, Milan, Italy), testing 17 antibiotics: kanamycin (30 µg), gentamicin (10 µg), streptomycin (10 µg), tobramycin (10 µg), ampicillin (10 µg), amoxicillin/clavulanic acid (30 µg), cefotaxime (30 µg), ceftriaxone (30 µg), ceftazidime (30 µg), imipenem (10 µg), nalidixic acid (30 µg), ciprofloxacin (5 µg), enrofloxacin (5 µg), levofloxacin (5 µg), sulfamethoxazole/trimethoprim (25 µg), tetracycline (30 µg) and chloramphenicol (30 µg).
Interpretation of inhibition zones and classification of isolates as susceptible (S), intermediate (I) or resistant (R), was done in accordance with CLSI guidelines [20].
2.3. ESBL Production Evaluation by Double-Disc Test
The double-disc test (DDT) was conducted on 36 MDR Salmonella strains to phenotypically assess ESBL production. Discs containing cephalosporins (cefotaxime 30 µg, ceftazidime 30 µg, cefepime 30 µg) were placed next to a disc with clavulanic acid (30 µg amoxicillin–clavulanic acid), as recommended by EUCAST [21]. When zones of inhibition around any of the cephalosporin discs were increased or there was a ‘keyhole’ in the direction of amoxicillin–clavulanic acid disc, the test was considered positive.
2.4. Detection of Beta-Lactamase Genes
The beta-lactamase gene detection was conducted on the 19 strains that were found by the double-disc test to be ESBL-producing. Bacterial DNA was extracted using 100 µL of PrepMan™ ultra Sample Preparation Reagent (Thermo Fisher Scientific, Waltham, MA, USA), according to the procedure recommended by the manufacturer. Real Time PCR reactions were performed using 10 ng of DNA template and 0.5 µM of the forward and reverse primers listed in Table 1, for a total volume of 25 µL of 1X of Advanced Universal SYBR Green Supermix (Bio-Rad Laboratories, Hercules, CA, USA), in order to amplify blaTEM, blaCTX-M, blaSHV and blaOXA genes.

Table 1.
Primers used in this study.
The amplification program included an initial denaturation at 94 °C for 10 min, followed by 32 cycles of 94 °C for 30 s, 60 °C for 30 s, 72 °C for 15 s, and a final extension at 72 °C for 10 min. Subsequently, 10 µL of the PCR product were used for electrophoresis on 2% E-Gel™ Go! Agarose Gels (Thermo Fisher Scientific, Waltham, MA, USA) to determine the size of the product. In each Real Time PCR reaction, a positive and a negative control were used. The positive one was represented by DNA belonging to a strain of Salmonella in which the presence of the bla gene was previous confirmed by sequencing; the negative control was represented by a Not Template Control (NTC), in which the reaction volume with DNase free water was obtained.
3. Results
3.1. Isolation Results
Microbiological analysis of the 493 food samples resulted in the isolation of 67 strains of Salmonella spp. (15 out of 172 were isolated in 2019, 17 out of 132 in 2020 and 35 out of 189 in 2021). Supplementary Materials Table S1 shows the samples that tested positive for the presence of Salmonella spp. and the serotypes identified. Notably, poultry meat was the main source of Salmonella, showing a prevalence of 40%, 52.9% and 71.4% in 2019, 2020 and 2021, respectively (Figure 1).
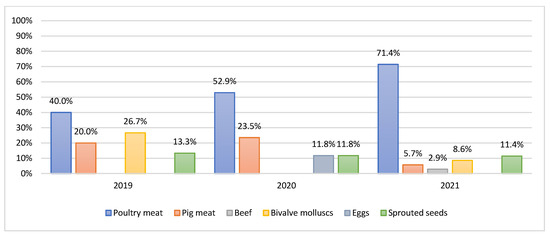
Figure 1.
Prevalence per year of Salmonella based on food.
S. Infantis was the predominant serotype (48%), present in 32 poultry meat samples. Instead, S. Typhimurium (9%), S. Derby (6%) and S. Enteritidis (3%) serotypes were found to have a low prevalence (Figure 2).
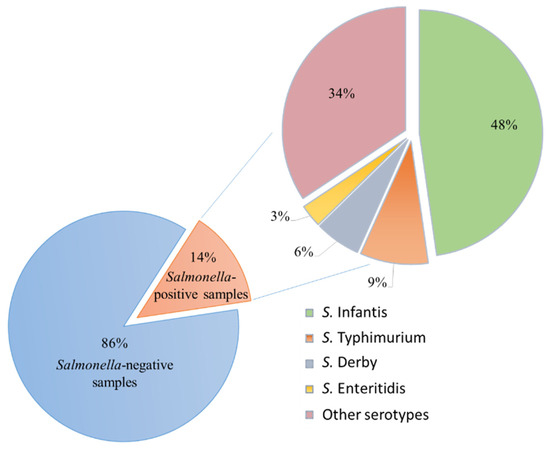
Figure 2.
Salmonella spp. research results and serotypes identified in the 2019–2021 three-year period.
3.2. Antibiotic Susceptibility and ESBL Production Test Results
Antibiotic susceptibility testing conducted on the 67 Salmonella strains showed the absence of resistance in 24 of these strains, whereas 43 strains (64%) were resistant to one or more of the tested antibiotics. Supplementary Materials Table S1 provides an overview of these strains and their resistances.
Notably, 31.3% of these strains were resistant to kanamycin, 43.2% to sulphonamides, 47.7% to nalidixic acid, 49.2% to ampicillin and 50.7% to tetracycline. Few strains showed resistance to levofloxacin (5%) or chloramphenicol (6%), whereas no resistance against imipenem, ciprofloxacin or enrofloxacin was detected.
An MDR profile was found in 36 strains that showed resistance to three (n = 4), four (n = 22) and five (n = 10) antibiotic classes (Supplementary Materials Table S1). Specifically, the most frequent MDR profiles were: aminoglycosides, beta-lactams, quinolones, sulphonamides and tetracyclines; resistance to these was found in eight S. Infantis, one S. Salamae and one S. Kentucky. Resistance to beta-lactams, quinolones, sulphonamides and tetracyclines was found in nine S. Infantis and one S. Cerro.
Finally, the double-disc test allowed detection of ESBL production in 19 strains. Indeed, for these strains, an increase in the zones of inhibition in the direction of amoxicillin or clavulanic acid was recorded around the tested cephalosporins (Table 2).

Table 2.
Resistance and ESBL production test results of the 36 MDR Salmonella strains.
3.3. Detection of Beta-Lactamase Genes
Genes responsible for beta-lactamase activity in 19 ESBL-producing Salmonella strains were screened by PCR. The presence of beta-lactamase genes was detected in all tested strains, confirming the phenotypic results of ESBL production tests (Table 3).

Table 3.
Beta-lactamase resistance gene detection results.
The most frequently identified genes were blaSHV and blaCTX-M, which were present in 68.4% and 47.3% of strains, respectively. Furthermore, the blaTEM gene was harboured by only one strain, while blaOXA was not detected. Specifically, nine strains harboured only the blaSHV gene, six strains harboured only the blaCTX-M gene, three strains harboured the blaCTX-M and blaSHV genes together, and one strain harboured the blaTEM and blaSHV genes together.
4. Discussion
Salmonella spp. are among the most frequent causes of foodborne diseases, and the increasing occurrence of MDR strains is an additional cause for concern. Thus, in the three-year period 2019–2021, we collected Salmonella spp. strains isolated from different food categories analysed in the context of Regulation (EC) No 2073/2005 [4], in order to assess their antibiotic susceptibility profiles and ESBL production.
Our data show that among the different food categories analysed, poultry meat was a relevant source of Salmonella. Moreover, regarding poultry meat, it is possible to note that the prevalence of Salmonella significantly increased over the three-year period, rising from 40% in 2019 to 71.4% in 2021; the prevalent serovar was S. Infantis (48%).
We performed a screening test using the Kirby–Bauer method to estimate the antibiotic susceptibility profiles of these strains, and we found a very high rate of strains showing at least one phenotypic resistance (64%). Among these, the highest rates of resistance were found against sulphonamides (43.2%), a class of antibiotics used in severe Salmonella infections, but also against nalidixic acid (47.7%) and kanamycin (31.3%). In addition, a high percentage of strains showed resistance to tetracyclines (50.7%), despite the fact that, in 2006, the European Union, in an attempt to counteract this trend, imposed a ban on the non-therapeutic use of antibiotics of human importance, such as tetracyclines, in farm animal feed. However, resistance to these drugs in Salmonella from food samples continues to be of concern [8,23]. This observation may be related to the human manipulation of these kinds of foods [24].
Of the strains tested, 53.7% showed an MDR profile with resistance to four or five classes in the majority of strains. These data are alarming, not only because of the real risk for consumers of becoming infected with an MDR strain, but also because many of these strains showed resistance to antibiotic classes important in human medicine, such as beta-lactamases. Thus, in order to obtain a complete overview of the resistance profiles of all the MDR strains isolated, we conducted a double-disc test (DDT) for ESBL phenotype detection. This test is one of the four different methods for confirming the ESBL phenotype recommended by EUCAST [21]. Despite the EFSA 2018/2019 report’s observation of resistance to third-generation cephalosporins at the overall low levels of 1.8% and 1.2% for cefotaxime and ceftazidime, respectively, for Salmonella spp., our experiment indicated that 52% of all MDR strains had an ESBL phenotype [8]. Finally, because these phenotypes could be conferred by several ARGs [25], the detection of beta-lactamase genes was performed in order to confirm phenotypic pattern. The PCRs we conducted allowed us to identify at least one gene encoding for β-lactamase enzymes in each strain that had an ESBL profile (Table 3). The blaCTX-M gene was present in 9 out of 19 ESBL strains, and in three of these, it was in association with the blaSHV gene, which was found to be the most prevalent gene among our isolates, because of its detection in 12 out of 19 ESBL strains. The blaCTX-M genes encode for extended-spectrum β-lactamases (ESBLs) frequently identified in Gram-negative pathogens. These types of enzymes are active against cephalosporins and monobactams (but not cephamycins or carbapenems), and are currently of great epidemiological and clinical interest [26]. The blaSHV gene has been identified mainly in Enterobacteriaceae causing nocosomal infections, but also in isolates from different contexts (human, animal and environment) [27,28]. Probably originating from a chromosomal penicillinase of Klebsiella pneumoniae, SHV β-lactamases currently comprise a large number of allelic variants, including extended-spectrum β-lactamases (ESBLs), non-ESBLs and several unclassified variants [29]. Our isolates showed an ESBL phenotype, so we have probably identified blaSHV genes encoded for extended-spectrum β-lactamases.
These data are certainly alarming, since all of our strains came from food samples, particularly poultry, intended for human consumption. Indeed, although cooking these products may reduce the risk of foodborne disease, ARGs can resist high temperatures and, once ingested, can be transferred to the gut microbiota and confer resistance to other bacteria [30]. Therefore, our data are in line with the latest EFSA recommendations, which confirm how important it is in the monitoring and surveillance of antibiotic resistance (AMR) to assess the presence of ARGs in foodborne strains, especially in a One Health approach that recognises the circularity of human, animal and environmental health.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microorganisms10040780/s1. Table S1: Analysed strains and their phenotypic resistances.
Author Contributions
Conceptualisation, V.G., D.G. and A.C.; methodology, V.G., C.P., M.P., C.C. and D.G.; formal analysis, D.G., V.G. and G.B.; investigation, D.G., V.G., S.S., G.O. and G.B.; resources, A.C.; data curation, V.G. and D.G.; writing—original draft preparation, V.G., D.G. and G.B.; writing—review and editing, V.G., D.G., S.S., C.C. and A.C.; visualisation, D.V.; supervision, G.C., D.V. and A.C.; project administration, A.C.; funding acquisition, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by IZS SI 07/20 RC: “Study on the correlation between pesticides and antimicrobial resistance in bacteria isolated from plants”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data discussed are contained in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- European Food Safety Authority; European Centre for Disease Prevention and Control. The European Union One Health 2020 Zoonoses Report. EFSA J. 2021, 19, e06971. [Google Scholar] [CrossRef]
- Liu, H.; Whitehouse, C.A.; Li, B. Presence and Persistence of Salmonella in Water: The Impact on Microbial Quality of Water and Food Safety. Front. Public Health 2018, 6, 159. [Google Scholar] [CrossRef] [PubMed]
- Ehuwa, O.; Jaiswal, A.K.; Jaiswal, S. Salmonella, Food Safety and Food Handling Practices. Foods 2021, 10, 907. [Google Scholar] [CrossRef] [PubMed]
- Commission of the European Communities Regulation (EC) No 2073/2005 of 15 November 2005 on Microbiological Criteria for Foodstuffs. 2005. Available online: http://data.europa.eu/eli/reg/2005/2073/oj (accessed on 14 December 2021).
- Eng, S.-K.; Pusparajah, P.; Ab Mutalib, N.-S.; Ser, H.-L.; Chan, K.-G.; Lee, L.-H. Salmonella: A Review on Pathogenesis, Epidemiology and Antibiotic Resistance. Front. Life Sci. 2015, 8, 284–293. [Google Scholar] [CrossRef] [Green Version]
- Elnekave, E.; Hong, S.L.; Lim, S.; Boxrud, D.; Rovira, A.; Mather, A.E.; Perez, A.; Alvarez, J. Transmission of Multidrug-Resistant Salmonella Enterica Subspecies Enterica 4,[5],12:I:- Sequence Type 34 between Europe and the United States. Emerg. Infect. Dis. 2020, 26, 3034–3038. [Google Scholar] [CrossRef] [PubMed]
- Proietti, P.C.; Stefanetti, V.; Musa, L.; Zicavo, A.; Dionisi, A.M.; Bellucci, S.; Mensa, A.L.; Menchetti, L.; Branciari, R.; Ortenzi, R.; et al. Genetic Profiles and Antimicrobial Resistance Patterns of Salmonella Infantis Strains Isolated in Italy in the Food Chain of Broiler Meat Production. Antibiotics 2020, 9, 814. [Google Scholar] [CrossRef]
- European Food Safety Authority; European Centre for Disease Prevention and Control. The European Union Summary Report on Antimicrobial Resistance in Zoonotic and Indicator Bacteria from Humans, Animals and Food in 2018/2019. EFSA J. 2021, 19, e06490. [Google Scholar] [CrossRef]
- Antimicrobial Resistance: Global Report on Surveillance; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92-4-156474-8.
- Castro-Vargas, R.E.; Herrera-Sánchez, M.P.; Rodríguez-Hernández, R.; Rondón-Barragán, I.S. Antibiotic Resistance in Salmonella Spp. Isolated from Poultry: A Global Overview. Vet. World 2020, 13, 2070–2084. [Google Scholar] [CrossRef]
- Campos, J.; Mourão, J.; Peixe, L.; Antunes, P. Non-Typhoidal Salmonella in the Pig Production Chain: A Comprehensive Analysis of Its Impact on Human Health. Pathogens 2019, 8, 19. [Google Scholar] [CrossRef] [Green Version]
- Iredell, J.; Brown, J.; Tagg, K. Antibiotic Resistance in Enterobacteriaceae: Mechanisms and Clinical Implications. BMJ 2016, 352, h6420. [Google Scholar] [CrossRef]
- Philippon, A.; Slama, P.; Dény, P.; Labia, R. A Structure-Based Classification of Class A β-Lactamases, a Broadly Diverse Family of Enzymes. Clin. Microbiol. Rev. 2016, 29, 29–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, Q.; Wu, Q.; Zhang, S.; Zhang, J.; Yang, G.; Wang, J.; Xue, L.; Chen, M. Characterization of Extended-Spectrum β-Lactamase-Producing Enterobacteriaceae From Retail Food in China. Front. Microbiol. 2018, 9, 1709. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.T.A.; Kanki, M.; Nguyen, P.D.; Le, H.T.; Ngo, P.T.; Tran, D.N.M.; Le, N.H.; Dang, C.V.; Kawai, T.; Kawahara, R.; et al. Prevalence, Antibiotic Resistance, and Extended-Spectrum and AmpC β-Lactamase Productivity of Salmonella Isolates from Raw Meat and Seafood Samples in Ho Chi Minh City, Vietnam. Int. J. Food Microbiol. 2016, 236, 115–122. [Google Scholar] [CrossRef]
- Colosi, I.A.; Baciu, A.M.; Opriș, R.V.; Peca, L.; Gudat, T.; Simon, L.M.; Colosi, H.A.; Costache, C. Prevalence of ESBL, AmpC and Carbapenemase-Producing Enterobacterales Isolated from Raw Vegetables Retailed in Romania. Foods 2020, 9, 1726. [Google Scholar] [CrossRef]
- Kim, H.-S.; Chon, J.-W.; Kim, Y.-J.; Kim, D.-H.; Kim, M.; Seo, K.-H. Prevalence and Characterization of Extended-Spectrum-β-Lactamase-Producing Escherichia Coli and Klebsiella Pneumoniae in Ready-to-Eat Vegetables. Int. J. Food Microbiol. 2015, 207, 83–86. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Biological Hazards (BIOHAZ); Koutsoumanis, K.; Allende, A.; Álvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; Davies, R.; De Cesare, A.; Herman, L.; et al. Role Played by the Environment in the Emergence and Spread of Antimicrobial Resistance (AMR) through the Food Chain. EFSA J. 2021, 19, 6651. [Google Scholar] [CrossRef]
- ISO 6579-1:2017; Microbiology of the Food Chain—Horizontal Method for the Detection, Enumeration and Serotyping of Salmonella—Part 1: Detection of Salmonella spp. International Organization for Standardization; AFNOR: Saint-Denis, France, 2017.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility: Supplement M100, 31st ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2021; ISBN 978-1-68440-105-5. [Google Scholar]
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Guideline for the Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance, Version 2.0; 2017. Available online: https://www.eucast.org/resistance_mechanisms/ (accessed on 14 December 2021).
- Zhao, X.; Hu, M.; Zhang, Q.; Zhao, C.; Zhang, Y.; Li, L.; Qi, J.; Luo, Y.; Zhou, D.; Liu, Y. Characterization of Integrons and Antimicrobial Resistance in Salmonella from Broilers in Shandong, China. Poult. Sci. 2020, 99, 7046–7054. [Google Scholar] [CrossRef] [PubMed]
- Gargano, V.; Sciortino, S.; Gambino, D.; Costa, A.; Agozzino, V.; Reale, S.; Alduina, R.; Vicari, D. Antibiotic Susceptibility Profile and Tetracycline Resistance Genes Detection in Salmonella Spp. Strains Isolated from Animals and Food. Antibiotics 2021, 10, 809. [Google Scholar] [CrossRef] [PubMed]
- Gargano, V.; Gambino, D.; Migliore, S.; Vitale, M.; Sciortino, S.; Costa, A.; Vicari, D. Can Human Handling Increase the Presence of Multidrug Resistance (MDR) in Salmonella Spp. Isolated from Food Sources? Microorganisms 2021, 9, 2018. [Google Scholar] [CrossRef] [PubMed]
- Dhanani, A.S.; Block, G.; Dewar, K.; Forgetta, V.; Topp, E.; Beiko, R.G.; Diarra, M.S. Genomic Comparison of Non-Typhoidal Salmonella Enterica Serovars Typhimurium, Enteritidis, Heidelberg, Hadar and Kentucky Isolates from Broiler Chickens. PLoS ONE 2015, 10, e0128773. [Google Scholar] [CrossRef]
- Cantón, R.; Coque, T.M. The CTX-M β-Lactamase Pandemic. Curr. Opin. Microbiol. 2006, 9, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Alcalá, L.; Alonso, C.A.; Simón, C.; González-Esteban, C.; Orós, J.; Rezusta, A.; Ortega, C.; Torres, C. Wild Birds, Frequent Carriers of Extended-Spectrum β-Lactamase (ESBL) Producing Escherichia Coli of CTX-M and SHV-12 Types. Microb. Ecol. 2016, 72, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Liakopoulos, A.; Mevius, D.; Ceccarelli, D. A Review of SHV Extended-Spectrum β-Lactamases: Neglected Yet Ubiquitous. Front. Microbiol. 2016, 7, 1374. [Google Scholar] [CrossRef] [PubMed]
- Bush, K. Past and Present Perspectives on β-Lactamases. Antimicrob. Agents Chemother. 2018, 62, e01076-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groussin, M.; Poyet, M.; Sistiaga, A.; Kearney, S.M.; Moniz, K.; Noel, M.; Hooker, J.; Gibbons, S.M.; Segurel, L.; Froment, A.; et al. Elevated Rates of Horizontal Gene Transfer in the Industrialized Human Microbiome. Cell 2021, 184, 2053–2067.e18. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).