Mycobacterium bovis PknG R242P Mutation Results in Structural Changes with Enhanced Virulence in the Mouse Model of Infection
Abstract
1. Introduction
2. Materials and Methods
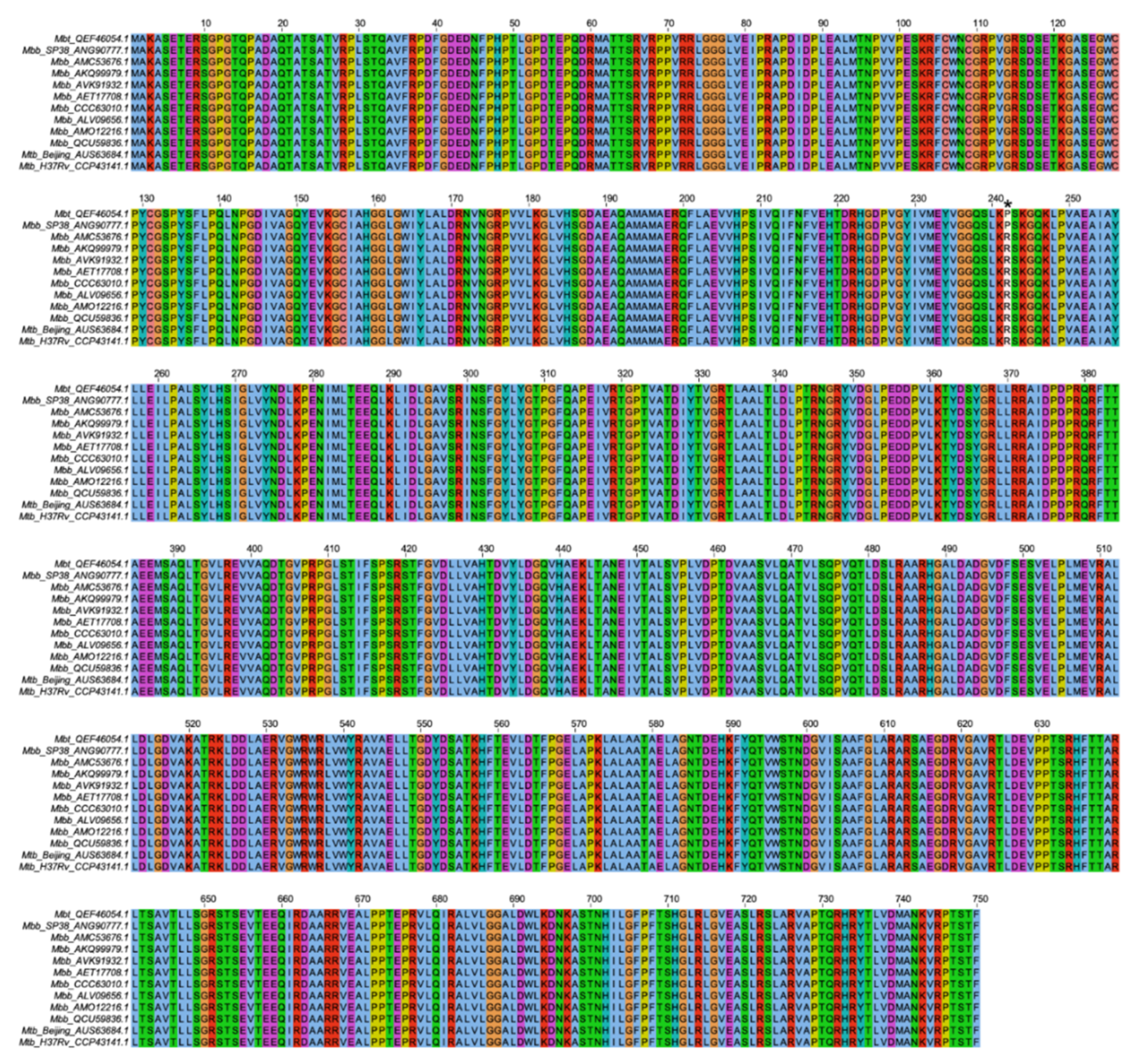
2.1. Alignment of PknG Protein Sequences from M. bovis Genome Sequences
2.2. Mycobacterium bovis Isolation
2.3. Mycobacterial Isolate Preparation
2.4. Mycobacterium bovis Mbt Isolate Genome Sequencing and Annotation
2.5. Confirmation of pknG Gene Mutation by Partial Gene Sequencing
2.6. Molecular Dynamics Simulations
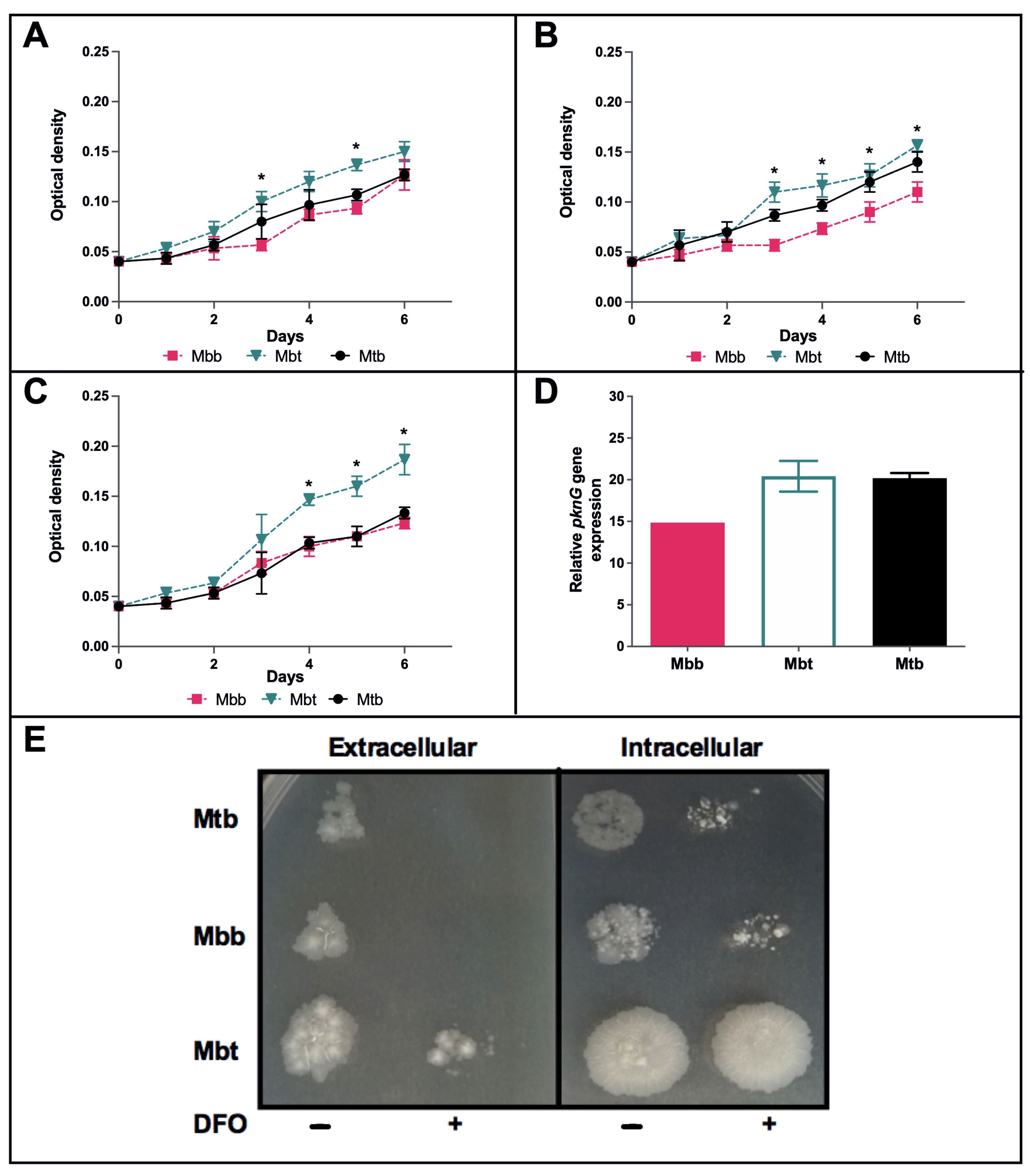
2.7. Evaluation of M. bovis Isolates Growth under In Vitro Stress Conditions
2.8. Infection of Bone Marrow-Derived Macrophages (BMDM)
2.9. Animals
2.10. Animal Infection, Survival, and Bacterial Load Determination
2.11. Evaluation of Pulmonary Pathology
2.12. Flow Cytometry Analysis
2.13. Statistical Analysis
3. Results
3.1. M. bovis PknG Sequences Alignment and Tertiary Structures
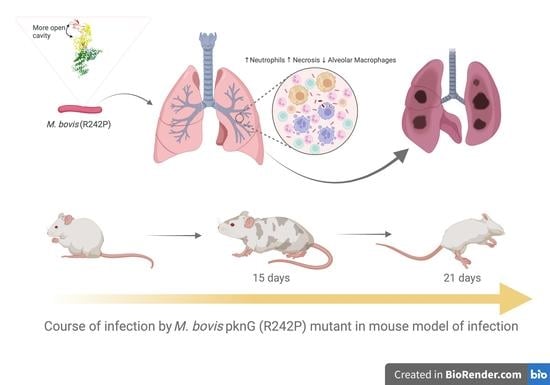
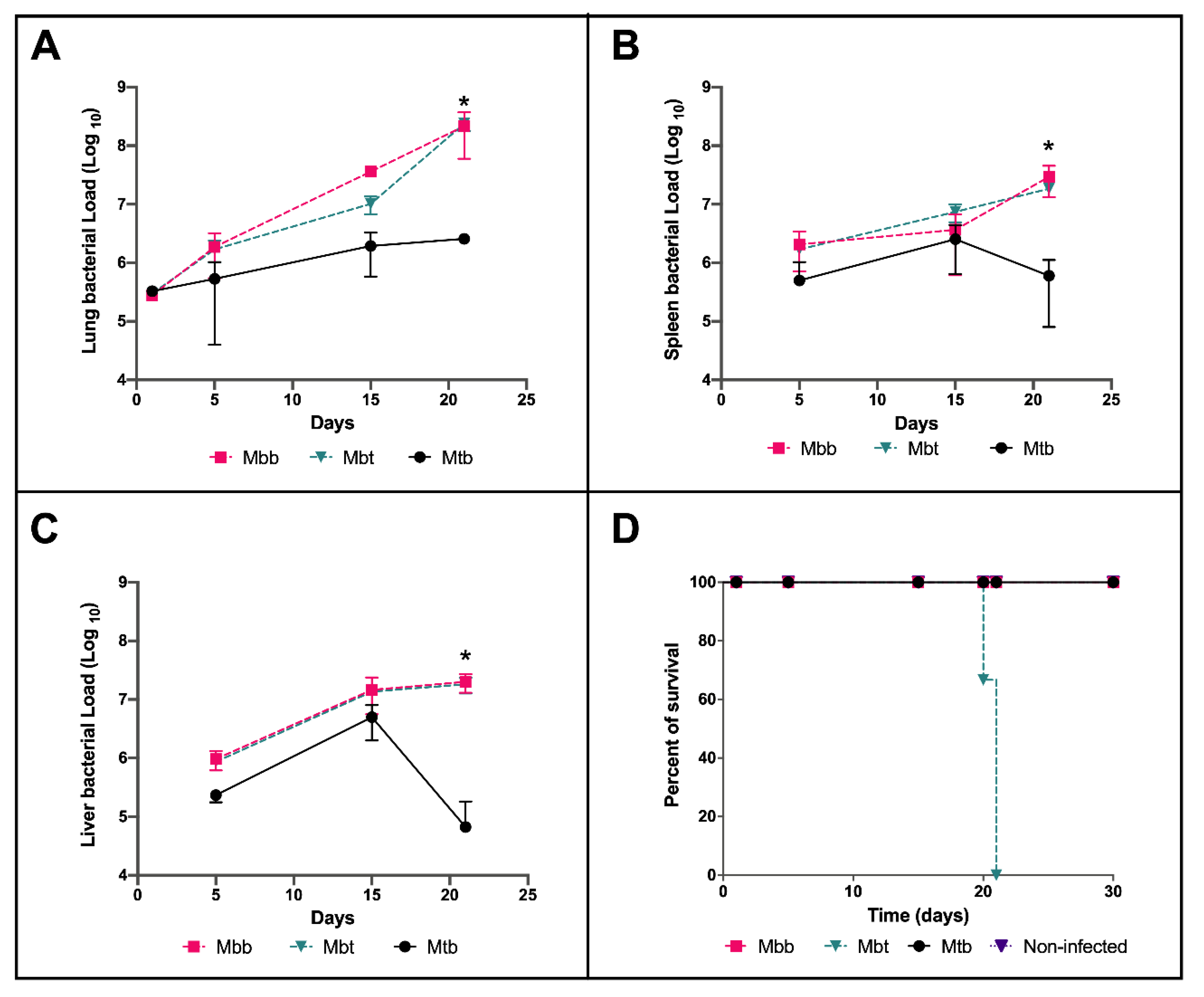
3.2. M. bovis Mbt Isolate (R242P) Have Increased Virulence in the Murine Model of Infection
3.3. Innate Immune Responses Evoked by M. bovis Presenting Different PknG Proteins
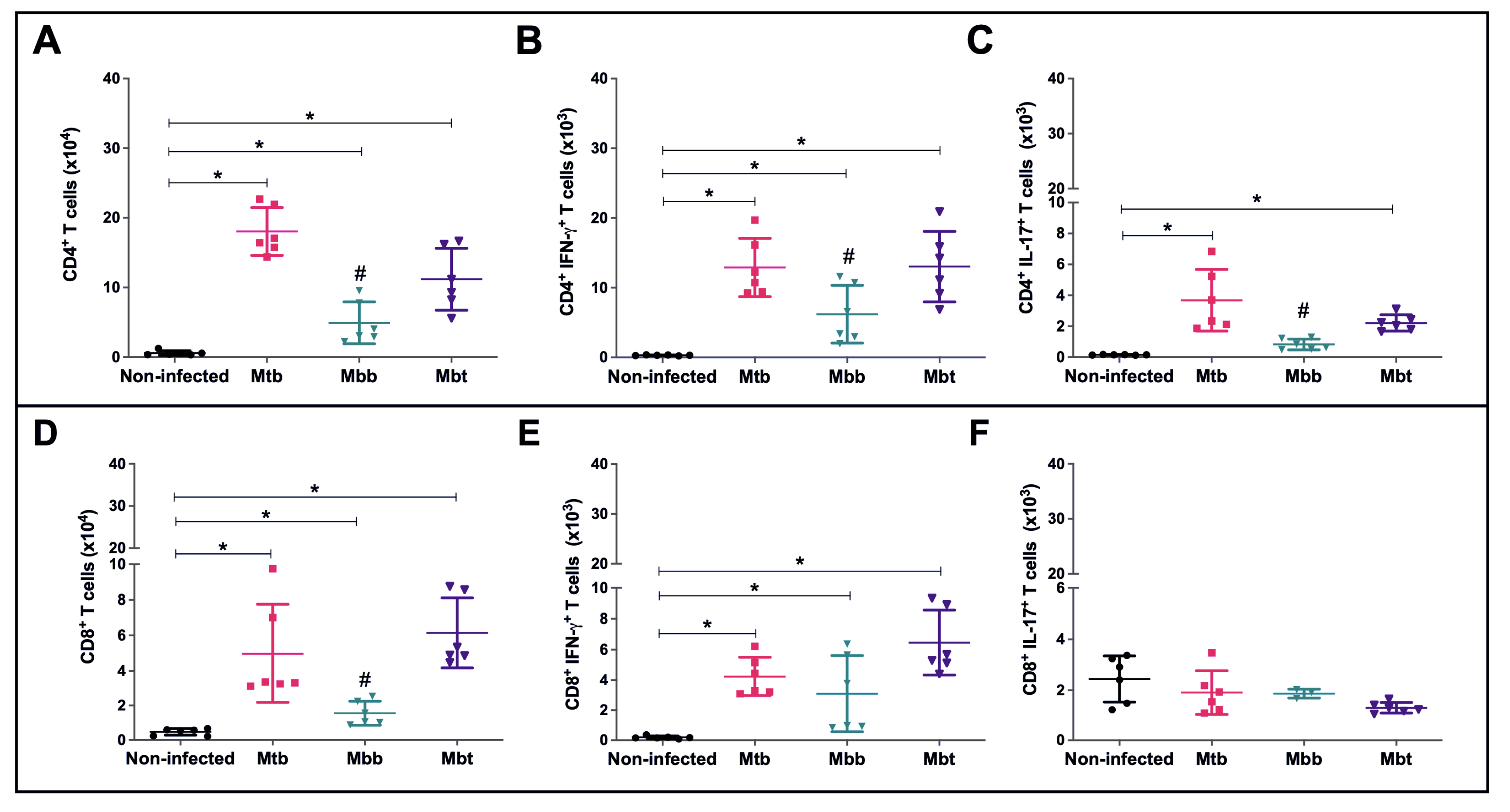
3.4. Modulation of the Acquired Immune Response
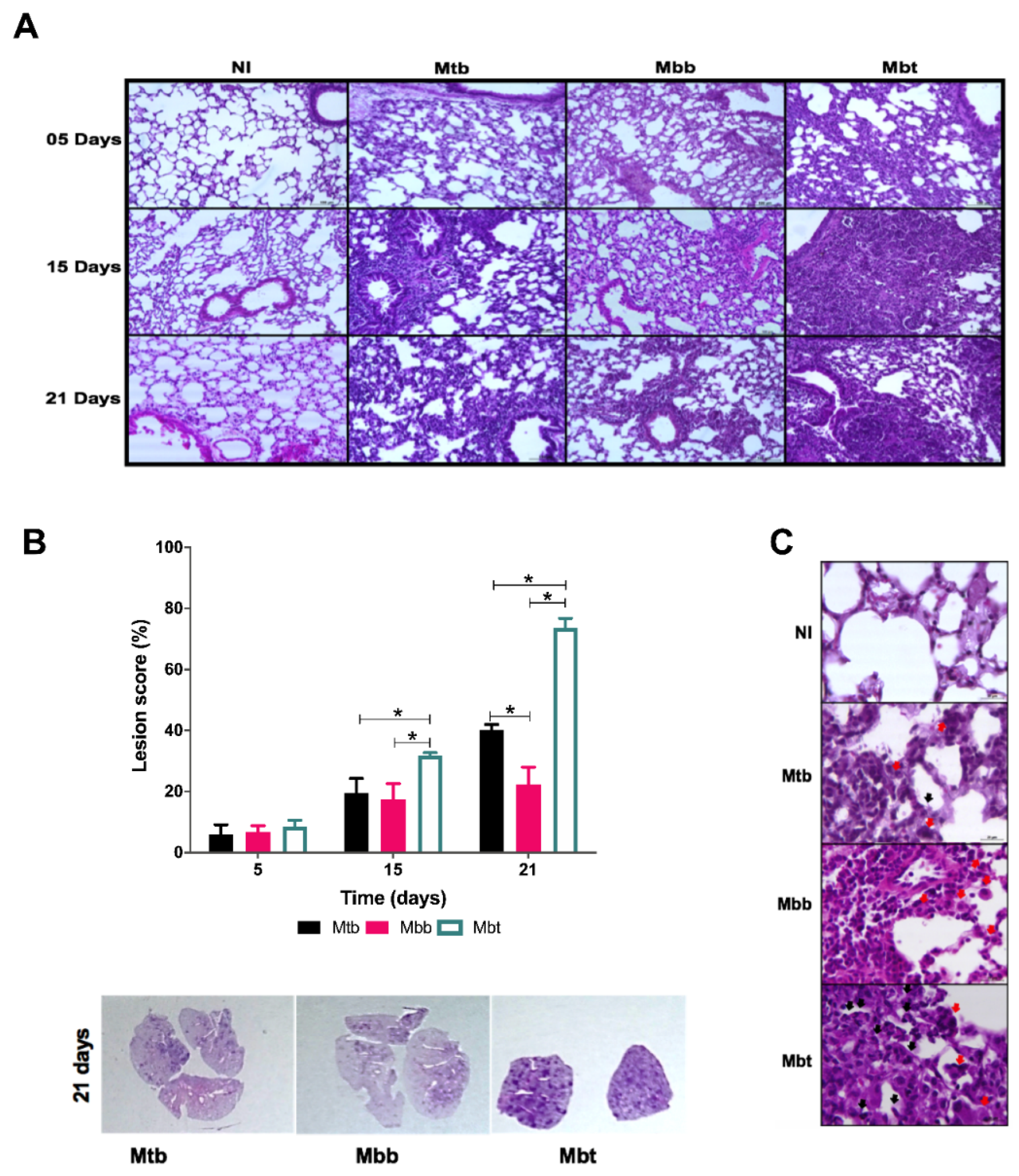
3.5. Kinetics of Pulmonary Pathology in Infection with M. bovis Isolates with Different PknG Proteins
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alber, T. Signaling mechanisms of the Mycobacterium tuberculosis receptor Ser/Thr protein kinases. Curr. Opin. Struct. Biol. 2009, 19, 650–657. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Scherr, N.; Honnappa, S.; Kunz, G.; Mueller, P.; Jayachandran, R.; Winkler, F.; Pieters, J.; Steinmetz, M.O. Structural basis for the specific inhibition of protein kinase G, a virulence factor of Mycobacterium tuberculosis. Proc. Natl. Acad. Sci. USA 2007, 104, 12151–12156. [Google Scholar] [CrossRef] [PubMed]
- Reckel, S.; Hantschel, O. Kinase Regulation in Mycobacterium tuberculosis: Variations on a Theme. Structure 2015, 23, 975–976. [Google Scholar] [CrossRef][Green Version]
- Wittwer, M.; Dames, S.A. Expression and purification of the natively disordered and redox sensitive metal binding regions of Mycobacterium tuberculosis protein kinase G. Protein Expr. Purif. 2015, 111, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Zulauf, K.E.; Sullivan, J.T.; Braunstein, M. The SecA2 pathway of Mycobacterium tuberculosis exports effectors that work in concert to arrest phagosome and autophagosome maturation. PLoS Pathog. 2018, 14, e1007011. [Google Scholar] [CrossRef]
- O’Hare, H.M.; Durán, R.; Cerveñansky, C.; Bellinzoni, M.; Wehenkel, A.M.; Pritsch, O.; Obal, G.; Baumgartner, J.; Vialaret, J.; Johnsson, K.; et al. Regulation of glutamate metabolism by protein kinases in mycobacteria. Mol. Microbiol. 2008, 70, 1408–1423. [Google Scholar] [CrossRef]
- Khan, M.Z.; Bhaskar, A.; Upadhyay, S.; Kumari, P.; Rajmani, R.S.; Jain, P.; Singh, A.; Kumar, D.; Bhavesh, N.S.; Nandicoori, V.K. Protein kinase G confers survival advantage to Mycobacterium tuberculosis during latency-like conditions. J. Biol Chem. 2017, 292, 16093–16108. [Google Scholar] [CrossRef]
- Wong, D.; Bach, H.; Sun, J.; Hmama, Z.; Av-Gay, Y. Mycobacterium tuberculosis protein tyrosine phosphatase (PtpA) excludes host vacuolar-H+-ATPase to inhibit phagosome acidification. Proc. Natl. Acad. Sci. USA 2011, 108, 19371–19376. [Google Scholar] [CrossRef]
- Mariotti, S.; Pardini, M.; Gagliardi, M.C.; Teloni, R.; Giannoni, F.; Fraziano, M.; Lozupone, F.; Meschini, S.; Nisini, R. Dormant Mycobacterium tuberculosis Fails To Block Phagosome Maturation and Shows Unexpected Capacity To Stimulate Specific Human T Lymphocytes. J. Immunol. 2013, 191, 274–282. [Google Scholar] [CrossRef]
- Pradhan, G.; Shrivastva, R.; Mukhopadhyay, S. Mycobacterial PknG Targets the Rab7l1 Signaling Pathway to Inhibit Phagosome-Lysosome Fusion. J. Immunol. 2018, 201, 1421–1433. [Google Scholar] [CrossRef]
- Nakedi, K.C.; Calder, B.; Banerjee, M.; Giddey, A.; Nel, A.J.M.; Garnett, S.; Blackburn, J.M.; Soares, N.C. Identification of Novel Physiological Substrates of Mycobacterium bovis BCG Protein Kinase G (PknG) by Label-free Quantitative Phosphoproteomics. Mol. Cell Proteom. 2018, 17, 1365–1377. [Google Scholar] [CrossRef] [PubMed]
- Caminiti, A.; Pelone, F.; LaTorre, G.; De Giusti, M.; Saulle, R.; Mannocci, A.; Sala, M.; Della Marta, U.; Scaramozzino, P. Control and eradication of tuberculosis in cattle: A systematic review of economic evidence. Vet. Rec. 2016, 179, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Thoen, C.; LoBue, P.; Kantor, I. The importance of Mycobacterium bovis as a zoonosis. Vet. Microbiol. 2006, 112, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Comas, I.; Coscolla, M.; Luo, T.; Borrell, S.; Holt, K.E.; Kato-Maeda, M.; Parkhill, J.; Malla, B.; Berg, S.; Thwaites, G.; et al. Out-of-Africa migration and Neolithic coexpansion of Mycobacterium tuberculosis with modern humans. Nat. Genet. 2013, 45, 1176–1182. [Google Scholar] [CrossRef] [PubMed]
- Medina, E.; Ryan, L.; LaCourse, R.; North, R.J. Superior virulence of Mycobacterium bovis over Mycobacterium tuberculosis (Mtb) for Mtb-resistant and Mtb-susceptible mice is manifest as an ability to cause extrapulmonary disease. Tuberculosis 2006, 86, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Aguilar León, D.; Zumárraga, M.J.; Jiménez Oropeza, R.; Gioffré, A.K.; Bernardelli, A.; Orozco Estévez, H.; Cataldi, A.A.; Hernández Pando, R. Mycobacterium bovis with different genotypes and from different hosts induce dissimilar immunopathological lesions in a mouse model of tuberculosis. Clin. Exp. Immunol. 2009, 157, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Lv, Y.; Sreevatsan, S.; Zhao, D.; Zhou, X. Differences in pathogenicity of three animal isolates of Mycobacterium species in a mouse model. PLoS ONE 2017, 12, e0183666. [Google Scholar] [CrossRef]
- Cheng, G.; Hussain, T.; Sabir, N.; Ni, J.; Li, M.; Zhao, D.; Zhou, X. Comparative study of the molecular basis of pathogenicity of M. bovis strains in a mouse model. Int. J. Mol. Sci. 2018, 20, 5. [Google Scholar] [CrossRef]
- Bigi, M.; Vazquez, C.L.; Castelão, A.B.C.; García, E.A.; Cataldi, A.A.; Jackson, M.; McNeil, M.; Soria, M.; Zumárraga, M.J.; Cabruja, M.; et al. Analysing nonsynonymous mutations between two Mycobacterium bovis strains with contrasting pathogenic profiles. Vet. Microbiol. 2019, 239, 108482. [Google Scholar] [CrossRef]
- Zerbino, D.R.; Birney, E. Velvet: Algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008, 18, 821–829. [Google Scholar] [CrossRef]
- Tsai, I.J.; Otto, T.D.; Berriman, M. Improving draft assemblies by iterative mapping and assembly of short reads to eliminate gaps. Genome Biol. 2010, 11, R41. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, A.; Saveliev, V.; Vyahhi, N.; Tesler, G. QUAST: Quality assessment tool for genome assemblies. Bioinformatics 2013, 29, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, Y. I-TASSER server: New development for protein structure and function predictions. Nucleic Acids Res. 2015, 43, 174–181. [Google Scholar] [CrossRef]
- Chen, V.B.; Arendall, W.B., 3rd; Headd, J.J.; Keedy, D.A.; Immormino, R.M.; Kapral, G.J.; Murray, L.W.; Richardson, J.S.; Richardson, D.C. MolProbity: All-atom structure validation for macromolecular crystallography. Acta Cryst. D Biol. Cryst. 2010, 66, 12–21. [Google Scholar] [CrossRef]
- Olsson, M.H.M.; Søndergaard, C.R.; Rostkowski, M.; Jensen, J.H. PROPKA3: Consistent Treatment of Internal and Surface Residues in Empirical p K a Predictions. J. Chem. Theory Comput. 2011, 7, 525–537. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. GROMACS: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX 2015, 1, 19–25. [Google Scholar] [CrossRef]
- Miyamoto, S.; Kollman, P.A. Settle: An analytical version of the SHAKE and RATTLE algorithm for rigid water models. J. Comput. Chem. 1992, 13, 952–962. [Google Scholar] [CrossRef]
- Hess, B. P-LINCS: A Parallel Linear Constraint Solver for Molecular Simulation. J. Chem. Theory. Comput. 2008, 4, 16–122. [Google Scholar] [CrossRef]
- Berendsen, H.J.C.; Postma, J.P.M.; van Gunsteren, W.F.; DiNola, A.; Haak, J.R. Molecular dynamics with coupling to an external bath. J. Chem. Phys. 1984, 81, 3684–3690. [Google Scholar] [CrossRef]
- Parrinello, M.; Rahman, A. Polymorphic transitions in single crystals: A new molecular dynamics method. J. Appl. Phys. 1981, 52, 7182–7190. [Google Scholar] [CrossRef]
- Essmann, U.; Perera, L.; Berkowitz, M.L.; Darden, T.; Lee, H.; Pedersen, L.G. A smooth particle mesh Ewald method. J. Chem. Phys. 1995, 103, 8577–8593. [Google Scholar] [CrossRef]
- Hockney, R.W.; Goel, S.P.; Eastwood, J.W. Quiet high-resolution computer models of a plasma. J. Comput. Phys. 1974, 14, 148–158. [Google Scholar] [CrossRef]
- Oliveira, F.M.; da Costa, A.C.; Procopio, V.O.; Garcia, W.; Araújo, J.N.; Silva, R.A.; Junqueira-Kipnis, A.P.; Kipnis, A. Mycobacterium abscessus subsp. massiliense mycma_0076 and mycma_0077 genes code for ferritins that are modulated by iron concentration. Front. Microbiol. 2018, 9, 1072. [Google Scholar] [CrossRef]
- Gonzalez-Juarrero, M.; Shim, T.S.; Kipnis, A.; Junqueira-Kipnis, A.P.; Orme, I.M. Dynamics of macrophage cell populations during murine pulmonary tuberculosis. J. Immunol. 2003, 171, 3128–3135. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, A.C.; de Resende, D.P.; Santos, B.P.O.; Zoccal, K.F.; Faccioli, L.H.; Kipnis, A.; Junqueira-Kipnis, A.P. Modulation of Macrophage Responses by CMX, a Fusion Protein Composed of Ag85c, MPT51, and HspX from Mycobacterium tuberculosis. Front. Microbiol. 2017, 8, 623. [Google Scholar] [CrossRef]
- Lisa, M.N.; Gil, M.; André-Leroux, G.; Barilone, N.; Durán, R.; Biondi, R.M.; Alzari, P.M. Molecular Basis of the Activity and the Regulation of the Eukaryotic-like S/T Protein Kinase PknG from Mycobacterium tuberculosis. Structure 2015, 23, 1039–1048. [Google Scholar] [CrossRef]
- Wang, J.; Ge, P.; Lei, Z.; Lu, Z.; Qiang, L.; Chai, Q.; Zhang, Y.; Zhao, D.; Li, B.; Su, J.; et al. Mycobacterium tuberculosis protein kinase G acts as an unusual ubiquitinating enzyme to impair host immunity. EMBO Rep. 2021, 22, e52175. [Google Scholar] [CrossRef]
- Wittwer, M.; Luo, Q.; Kaila, V.R.; Dames, S.A. Oxidative Unfolding of the Rubredoxin Domain and the Natively Disordered N-terminal Region Regulate the Catalytic Activity of Mycobacterium tuberculosis Protein Kinase G. J. Biol. Chem. 2016, 291, 27062–27072. [Google Scholar] [CrossRef]
- Li, Y.; Wei, C.; Xu, H.; Jia, J.; Wei, Z.; Guo, R.; Jia, Y.; Wu, Y.; Li, Y.; Qi, X.; et al. The Immunoregulation of Th17 in Host against Intracellular Bacterial Infection. Mediat. Inflamm. 2018, 2018, 6587296. [Google Scholar] [CrossRef]
- Lopez, P.M.; Golby, P.; Wooff, E.; Garcia, J.N.; Garcia Pelayo, M.C.; Conlon, K.; Gema Camacho, A.; Hewinson, R.G.; Polaina, J.; Suárez García, A.; et al. Characterization of the transcriptional regulator Rv3124 of Mycobacterium tuberculosis identifies it as a positive regulator of molybdopterin biosynthesis and defines the functional consequences of a non-synonymous SNP in the Mycobacterium bovis BCG orthologue. Microbiology 2010, 156, 2112–2123. [Google Scholar] [CrossRef][Green Version]
- Biek, R.; O’Hare, A.; Wright, D.; Mallon, T.; McCormick, C.; Orton, R.J.; McDowell, S.; Trewby, H.; Skuce, R.A.; Kao, R.R. Whole Genome Sequencing Reveals Local Transmission Patterns of Mycobacterium bovis in Sympatric Cattle and Badger Populations. PLoS Pathog. 2012, 8, e1003008. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, A.M.; Hill-Cawthorne, G.A.; Otto, T.D.; Coll, F.; Guerra-Assunção, J.A.; Gao, G.; Naeem, R.; Ansari, H.; Malas, T.B.; Adroub, S.A.; et al. Genomic expression catalogue of a global collection of BCG vaccine strains show evidence for highly diverged metabolic and cell-wall adaptations. Sci. Rep. 2015, 5, 15443. [Google Scholar] [CrossRef] [PubMed]
- Walburger, A.; Koul, A.; Ferrari, G.; Nguyen, L.; Prescianotto-Baschong, C.; Huygen, K.; Klebl, B.; Thompson, C.; Bacher, G.; Pieters, J. Protein kinase G from pathogenic mycobacteria promotes survival within macrophages. Science 2004, 304, 1800–1804. [Google Scholar] [CrossRef]
- Rieck, B.; Degiacomi, G.; Zimmermann, M.; Cascioferro, A.; Boldrin, F.; Lazar-Adler, N.R.; Bottrill, A.R.; le Chevalier, F.; Frigui, W.; Bellinzoni, M.; et al. PknG senses amino acid availability to control metabolism and virulence of Mycobacterium tuberculosis. PloS Pathog. 2017, 13, e1006399. [Google Scholar] [CrossRef]
- Nguyen, L.; Walburger, A.; Houben, E.; Koul, A.; Muller, S.; Morbitzer, M.; Klebl, B.; Ferrari, G.; Pieters, J. Role of protein kinase G in growth and glutamine metabolism of Mycobacterium bovis BCG. J. Bacteriol. 2005, 187, 5852–5856. [Google Scholar] [CrossRef][Green Version]
- Slayden, R.A.; Barry, C.E. The genetics and biochemistry of isoniazid resistance in Mycobacterium tuberculosis. Microbes Infect. 2000, 2, 659–669. [Google Scholar] [CrossRef]
- Pym, A.S.; Saint-Joanis, B.; Cole, S.T. Effect of katG mutations on the virulence of Mycobacterium tuberculosis and the implication for transmission in humans. Infect. Immun. 2002, 70, 4955–4960. [Google Scholar] [CrossRef]
- Cowley, S.; Ko, M.; Pick, N.; Chow, R.; Downing, K.J.; Gordhan, B.G.; Betts, J.C.; Mizrahi, V.; Smith, D.A.; Stokes, R.W.; et al. The Mycobacterium tuberculosis protein serine/threonine kinase PknG is linked to cellular glutamate/glutamine levels and is important for growth in vivo. Mol. Microbiol 2004, 52, 1691–1702. [Google Scholar] [CrossRef]
- Conrad, M.; Kagan, V.E.; Bayir, H.; Pagnussat, G.C.; Head, B.; Traber, M.G.; Stockwell, B.R. Regulation of lipid peroxidation and ferroptosis in diverse species. Genes Dev. 2018, 32, 602–619. [Google Scholar] [CrossRef]
- Cronjé, L.; Edmondson, N.; Eisenach, K.D.; Bornman, L. Iron and iron chelating agents modulate Mycobacterium tuberculosis growth and monocyte-macrophage viability and effector functions. FEMS Immunol. Med. Microbiol. 2005, 45, 103–112. [Google Scholar] [CrossRef]
- Amaral, E.P.; Costa, D.L.; Namasivayam, S.; Riteau, N.; Kamenyeva, O.; Mittereder, L.; Mayer-Barber, K.D.; Andrade, B.B.; Sher, A. A major role for ferroptosis in Mycobacterium tuberculosis–induced cell death and tissue necrosis. J. Exp. Med. 2019, 216, 556–570. [Google Scholar] [CrossRef] [PubMed]
- Lemire, J.A.; Harrison, J.J.; Turner, R.J. Antimicrobial activity of metals: Mechanisms, molecular targets and applications. Nat. Rev. Microbiol. 2013, 11, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Andrade, M.R.M.; Amaral, E.P.; Ribeiro, S.C.M.; Almeida, F.M.; Peres, T.V.; Lanes, V.; D’Império-Lima, M.R.; Lasunskaia, E.B. Pathogenic Mycobacterium bovis strains differ in their ability to modulate the proinflammatory activation phenotype of macrophages. BMC Microbiol. 2012, 12, 166. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, T.S.; Conti, B.J.; Fraga-Silva, T.F.C.; Almeida, F.; Bonato, V.L.D. Interplay between alveolar epithelial and dendritic cells and Mycobacterium tuberculosis. J. Leukoc. Biol. 2020, 108, 1139–1156. [Google Scholar] [CrossRef]
- Almeida, F.M.; Ventura, T.L.B.; Amaral, E.P.; Ribeiro, S.C.M.; Calixto, S.D.; Manhães, M.R.; Rezende, A.L.; Souza, G.S.; de Carvalho, I.S.; Silva, E.C.; et al. Hypervirulent Mycobacterium tuberculosis strain triggers necrotic lung pathology associated with enhanced recruitment of neutrophils in resistant C57BL/6 mice. PLoS ONE 2017, 12, e0173715. [Google Scholar] [CrossRef]
- Braian, C.; Hogea, V.; Stendahl, O. Mycobacterium tuberculosis-induced neutrophil extracellular traps activate human macrophages. J. Innate. Immun. 2013, 5, 591–602. [Google Scholar] [CrossRef]
- Dallenga, T.; Repnik, U.; Corleis, B.; Eich, J.; Reimer, R.; Griffiths, G.W.; Schaible, U.E. M. Tuberculosis-Induced Necrosis of Infected Neutrophils Promotes Bacterial Growth Following Phagocytosis by Macrophages. Cell Host Microbe 2017, 22, 519–530. [Google Scholar] [CrossRef]
- Sada-Ovalle, I.; Chiba, A.; Gonzales, A.; Brenner, M.B.; Behar, S.M. Innate invariant NKT cells recognize Mycobacterium tuberculosis-infected macrophages, produce interferon-γ, and kill intracellular bacteria. PLoS Pathog. 2008, 4, e1000239. [Google Scholar] [CrossRef]
- Chiba, A.; Dascher, C.C.; Besra, G.S.; Brenner, M.B. Rapid NKT Cell Responses Are Self-Terminating during the Course of Microbial Infection. J. Immunol. 2008, 181, 2292–2302. [Google Scholar] [CrossRef]
- Junqueira-Kipnis, A.P.; Kipnis, A.; Jamieson, A.; Juarrero, M.G.; Diefenbach, A.; Raulet, D.H.; Turner, J.; Orme, I.M. NK cells respond to pulmonary infection with Mycobacterium tuberculosis, but play a minimal role in protection. J. Immunol. 2003, 171, 6039–6045. [Google Scholar] [CrossRef] [PubMed]
- Andersson, M.; Lutay, N.; Hallgren, O.; Westergren-Thorsson, G.; Svensson, M.; Godaly, G. Mycobacterium bovis bacilli Calmette-Guerin regulates leukocyte recruitment by modulating alveolar inflammatory responses. Innate. Immun. 2012, 18, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Trentini, M.; Oliveira, F.M.; Kipnis, A.; Junqueira-Kipnis, A.P. The Role of Neutrophils in the Induction of Specific Th1 and Th17 during Vaccination against Tuberculosis. Front. Microbiol. 2016, 10, 7:898. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, F.M.d.; Procopio, V.O.; de Lima Menezes, G.; Silva, R.A.d.; Kipnis, A.; Junqueira-Kipnis, A.P. Mycobacterium bovis PknG R242P Mutation Results in Structural Changes with Enhanced Virulence in the Mouse Model of Infection. Microorganisms 2022, 10, 673. https://doi.org/10.3390/microorganisms10040673
Oliveira FMd, Procopio VO, de Lima Menezes G, Silva RAd, Kipnis A, Junqueira-Kipnis AP. Mycobacterium bovis PknG R242P Mutation Results in Structural Changes with Enhanced Virulence in the Mouse Model of Infection. Microorganisms. 2022; 10(4):673. https://doi.org/10.3390/microorganisms10040673
Chicago/Turabian StyleOliveira, Fábio Muniz de, Victor Oliveira Procopio, Gabriela de Lima Menezes, Roosevelt Alves da Silva, André Kipnis, and Ana Paula Junqueira-Kipnis. 2022. "Mycobacterium bovis PknG R242P Mutation Results in Structural Changes with Enhanced Virulence in the Mouse Model of Infection" Microorganisms 10, no. 4: 673. https://doi.org/10.3390/microorganisms10040673
APA StyleOliveira, F. M. d., Procopio, V. O., de Lima Menezes, G., Silva, R. A. d., Kipnis, A., & Junqueira-Kipnis, A. P. (2022). Mycobacterium bovis PknG R242P Mutation Results in Structural Changes with Enhanced Virulence in the Mouse Model of Infection. Microorganisms, 10(4), 673. https://doi.org/10.3390/microorganisms10040673