A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance
Abstract
1. Introduction
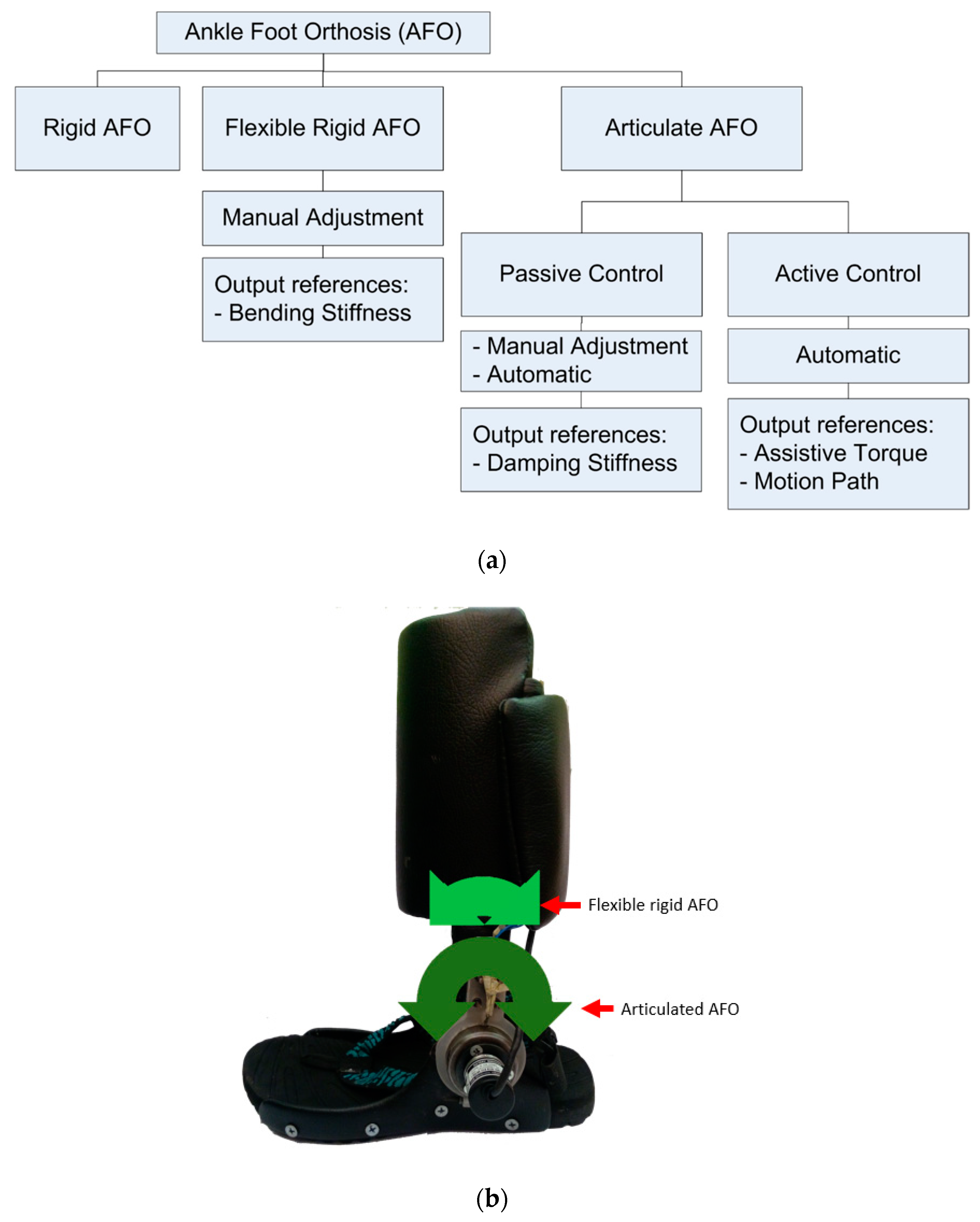
2. Types of AFO Structures
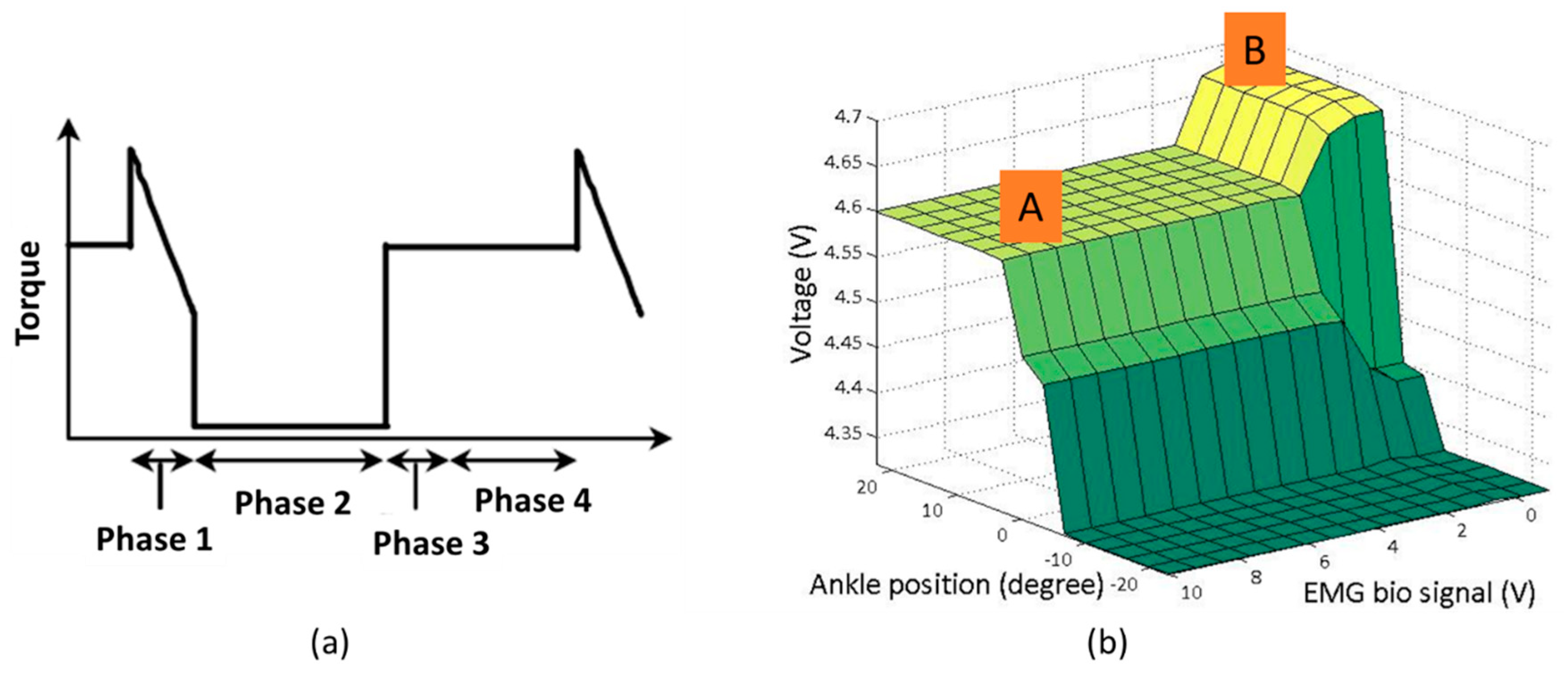
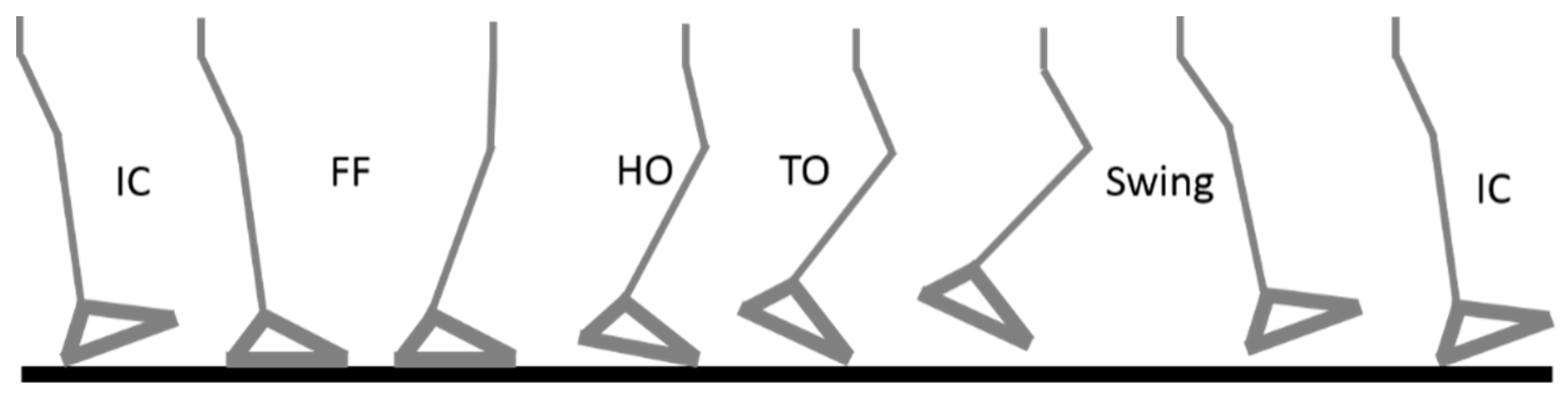
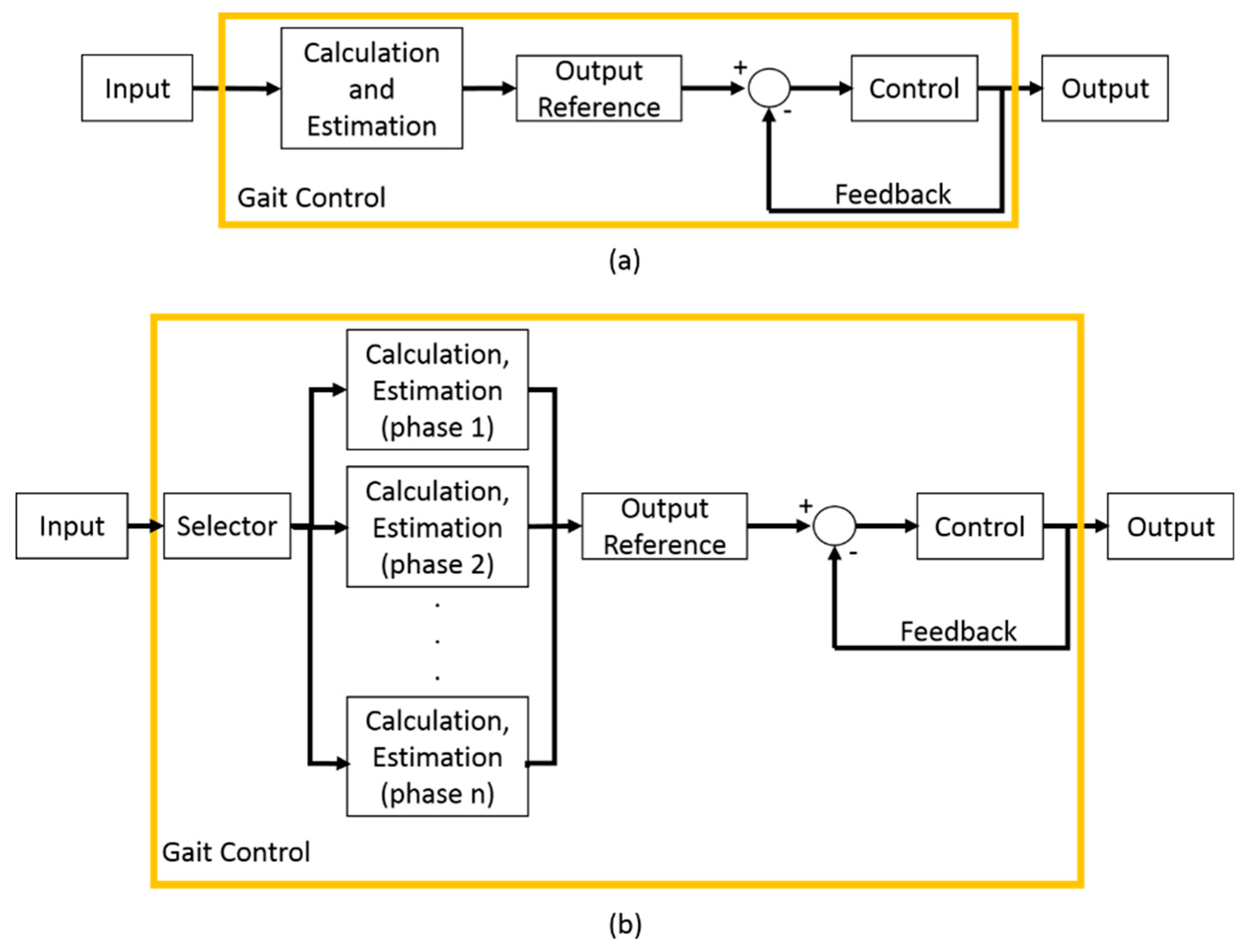
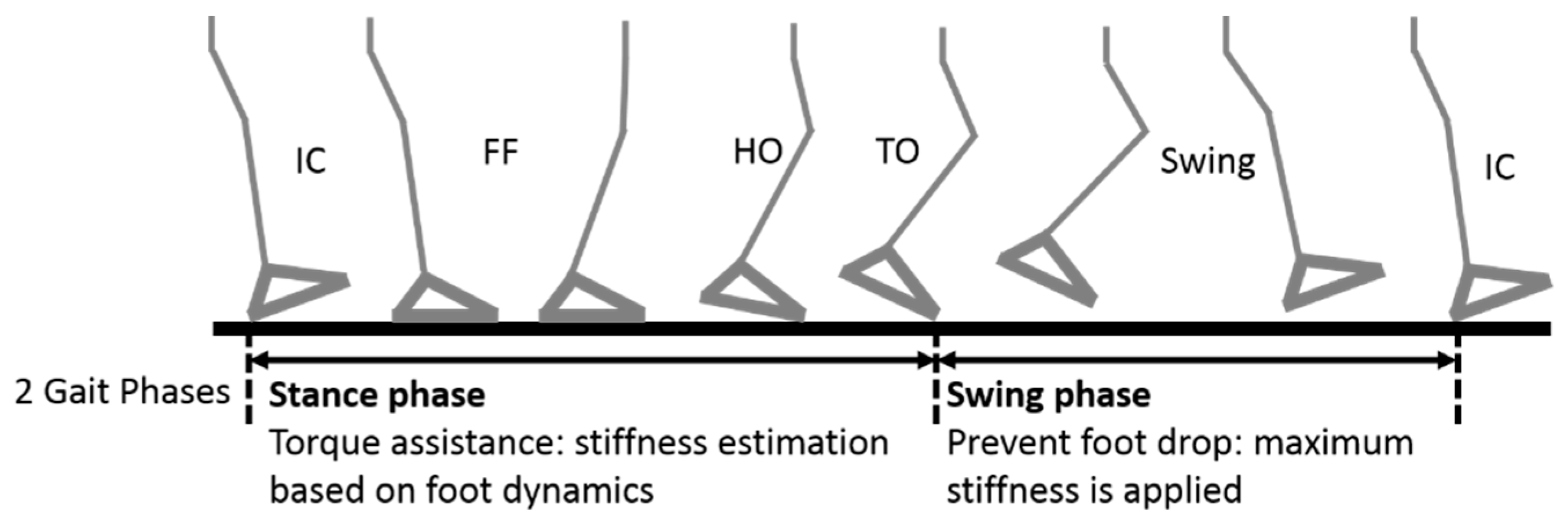
3. Input and Gait Phases
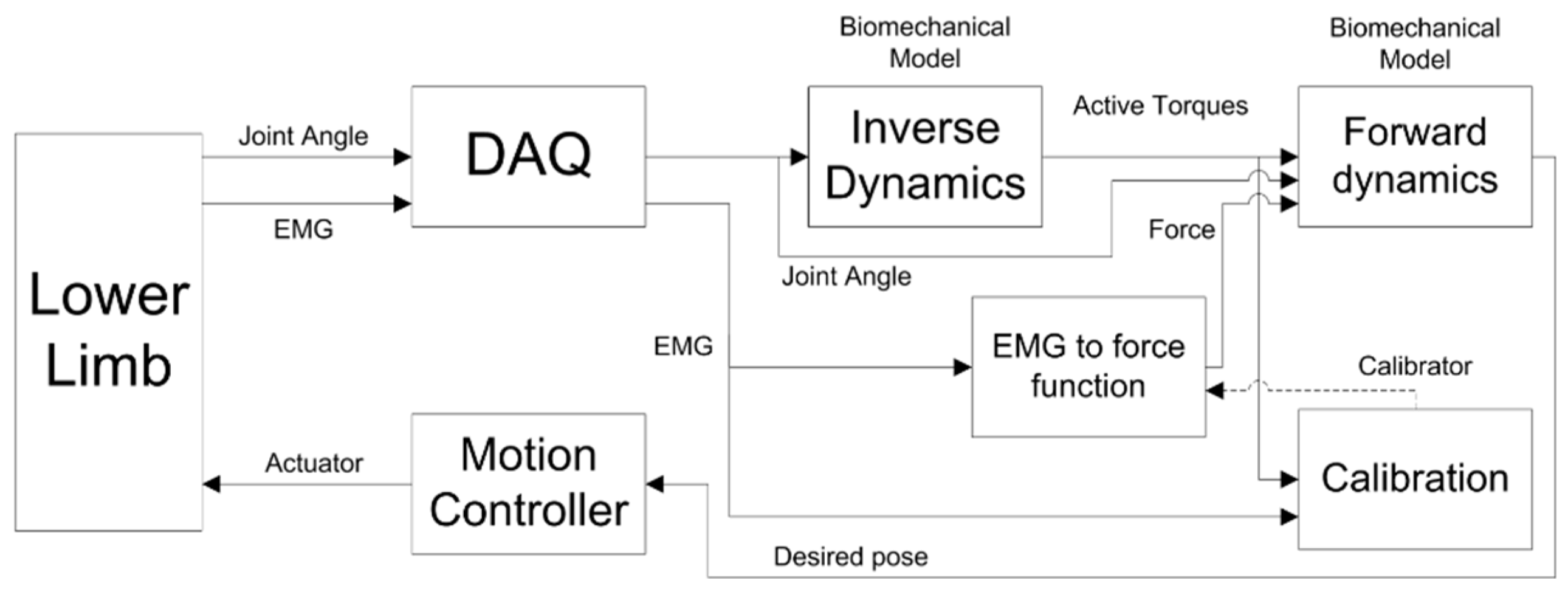
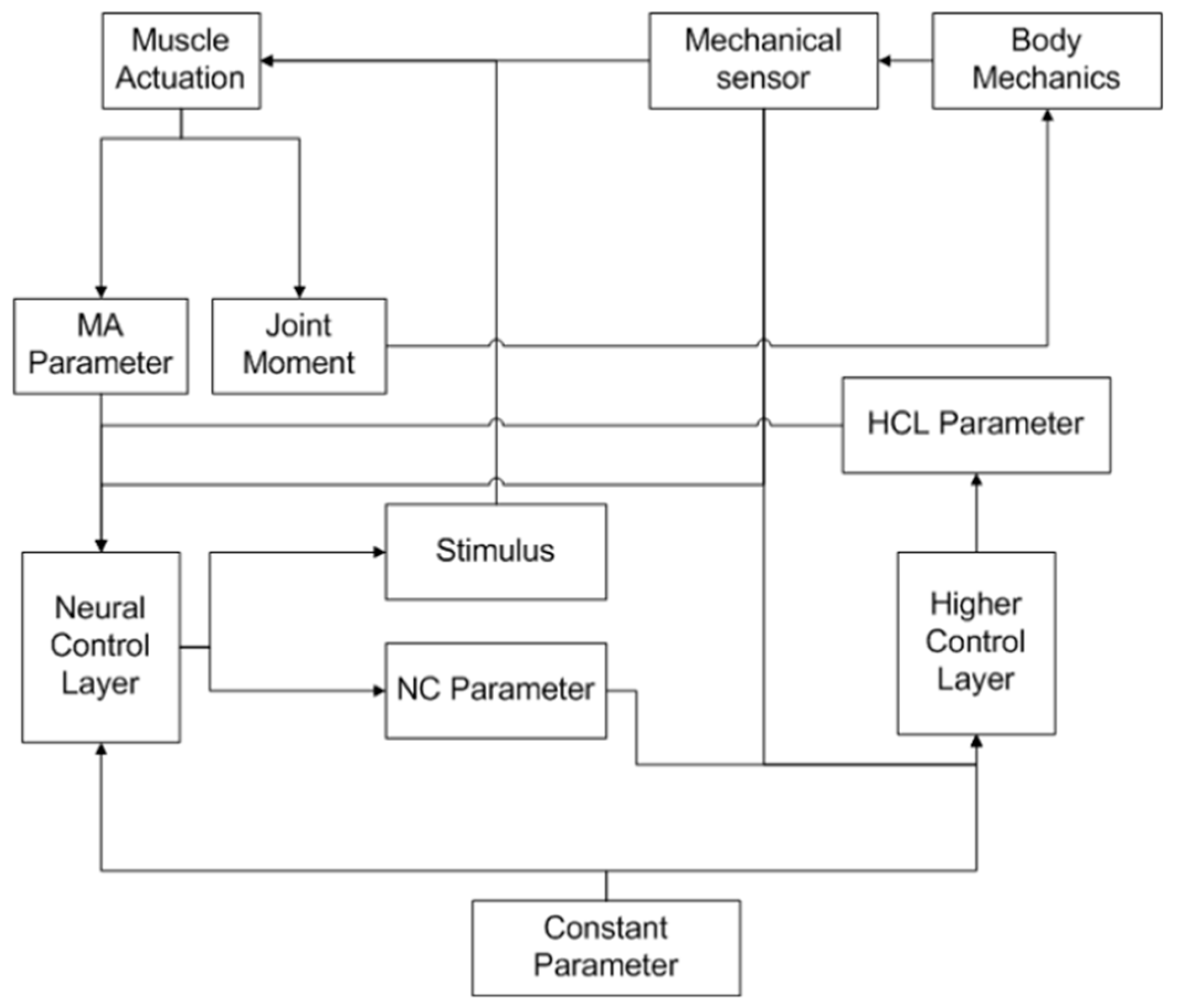
4. Output Reference Estimation and Control
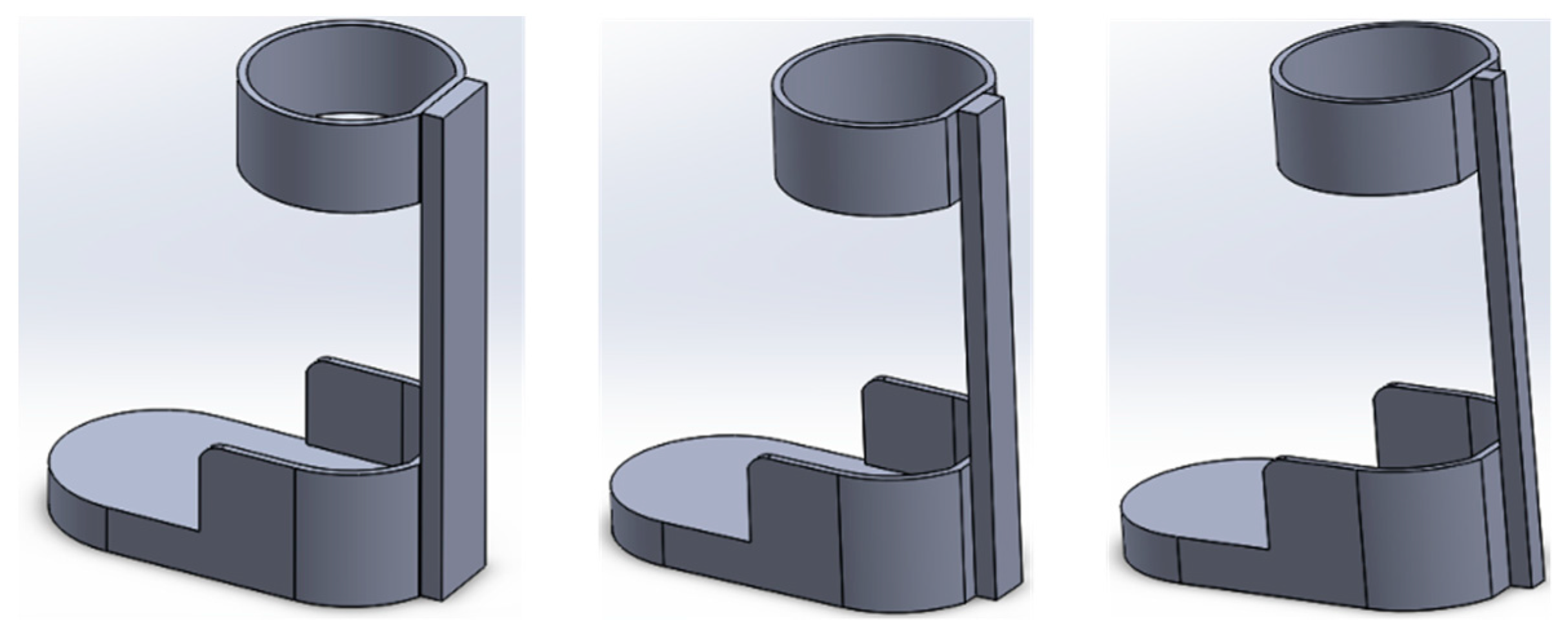
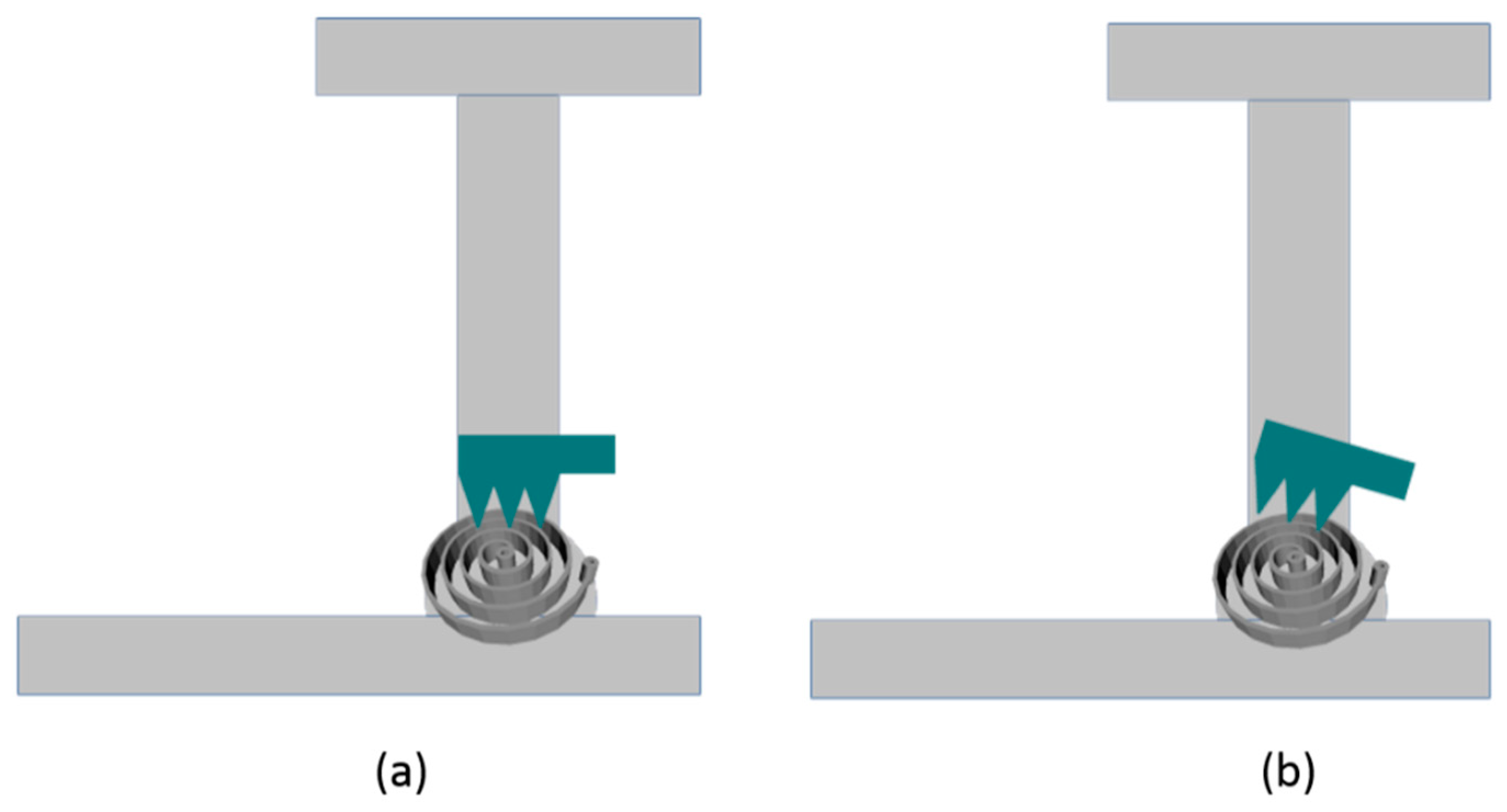
4.1. Bending Stiffness Control
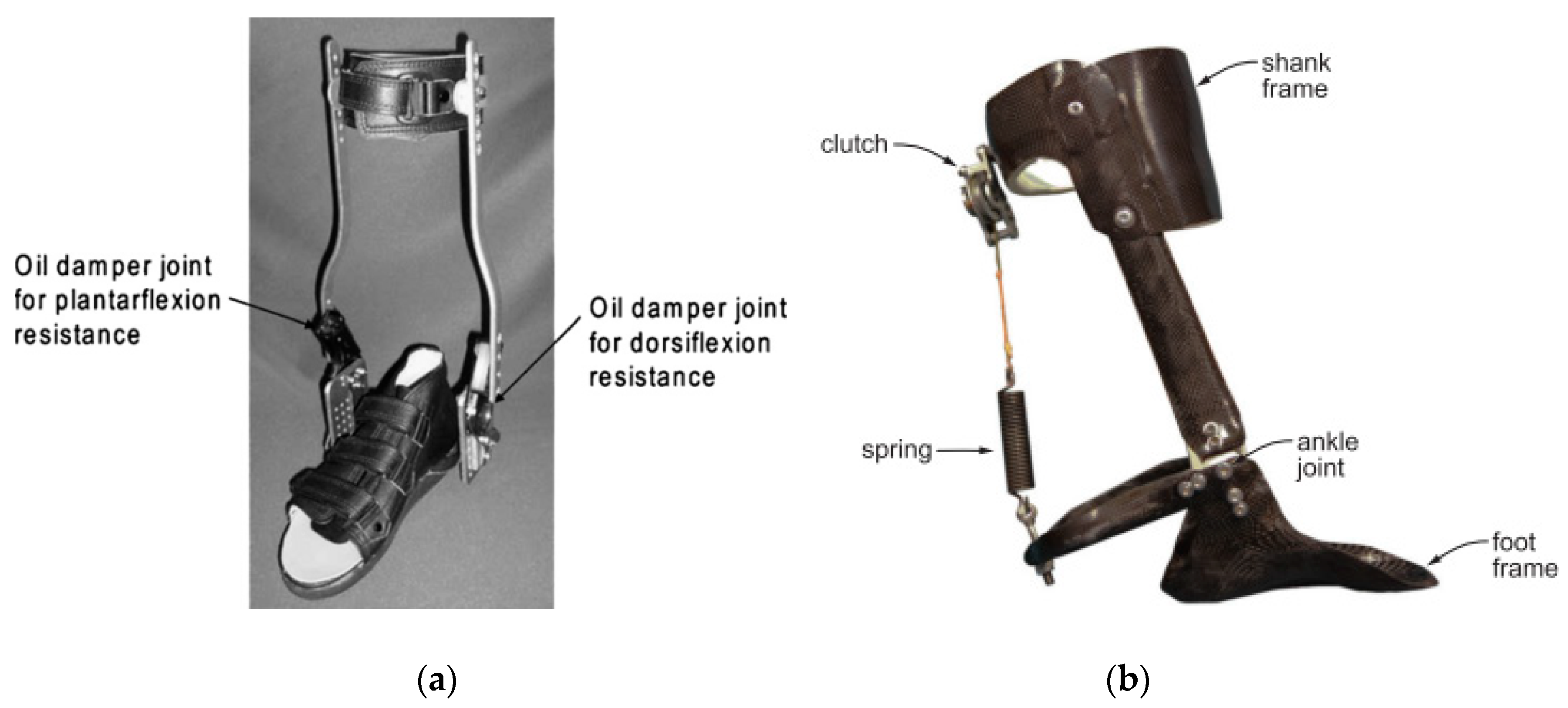
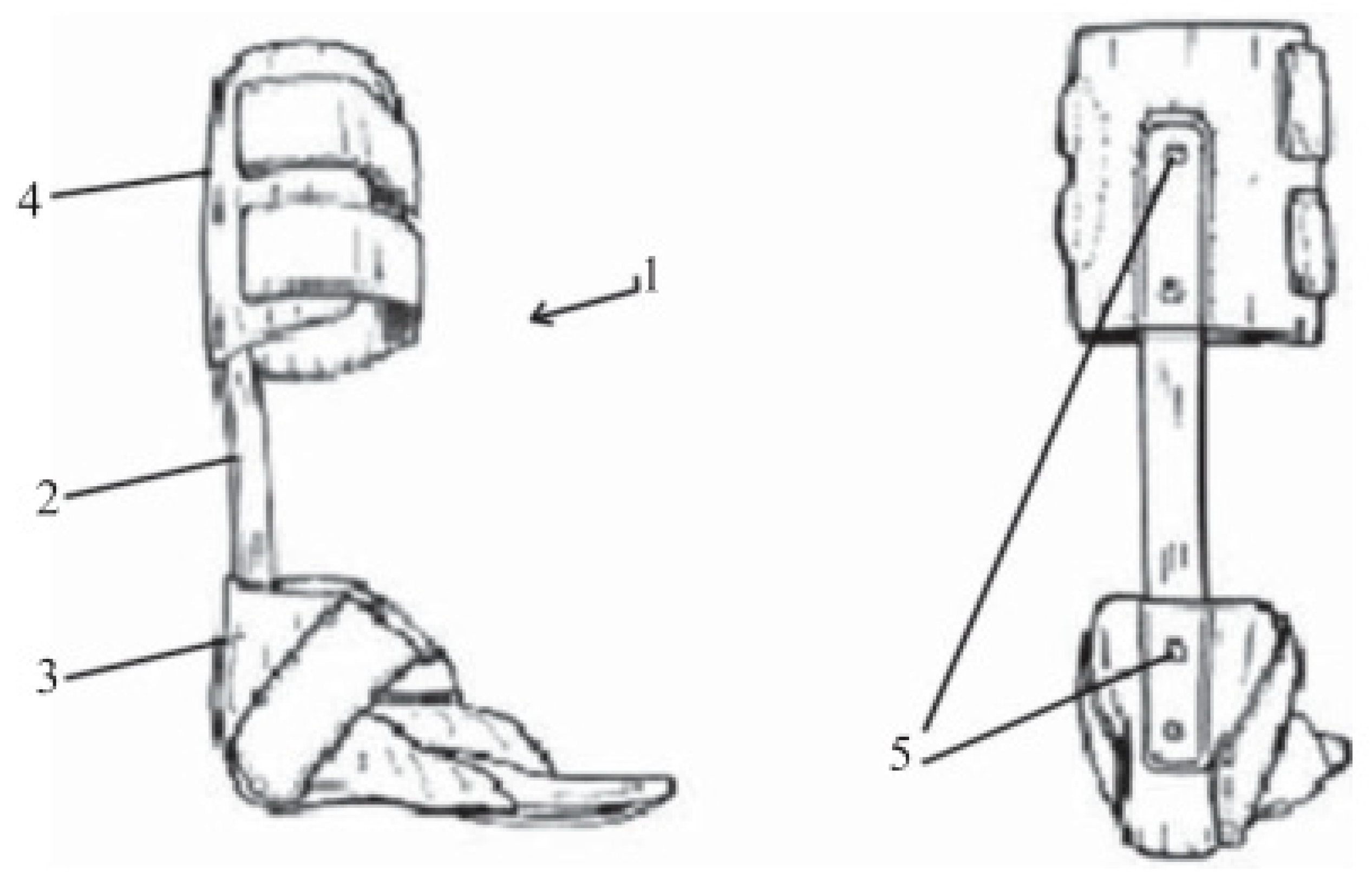
4.2. Damping Stiffness Control
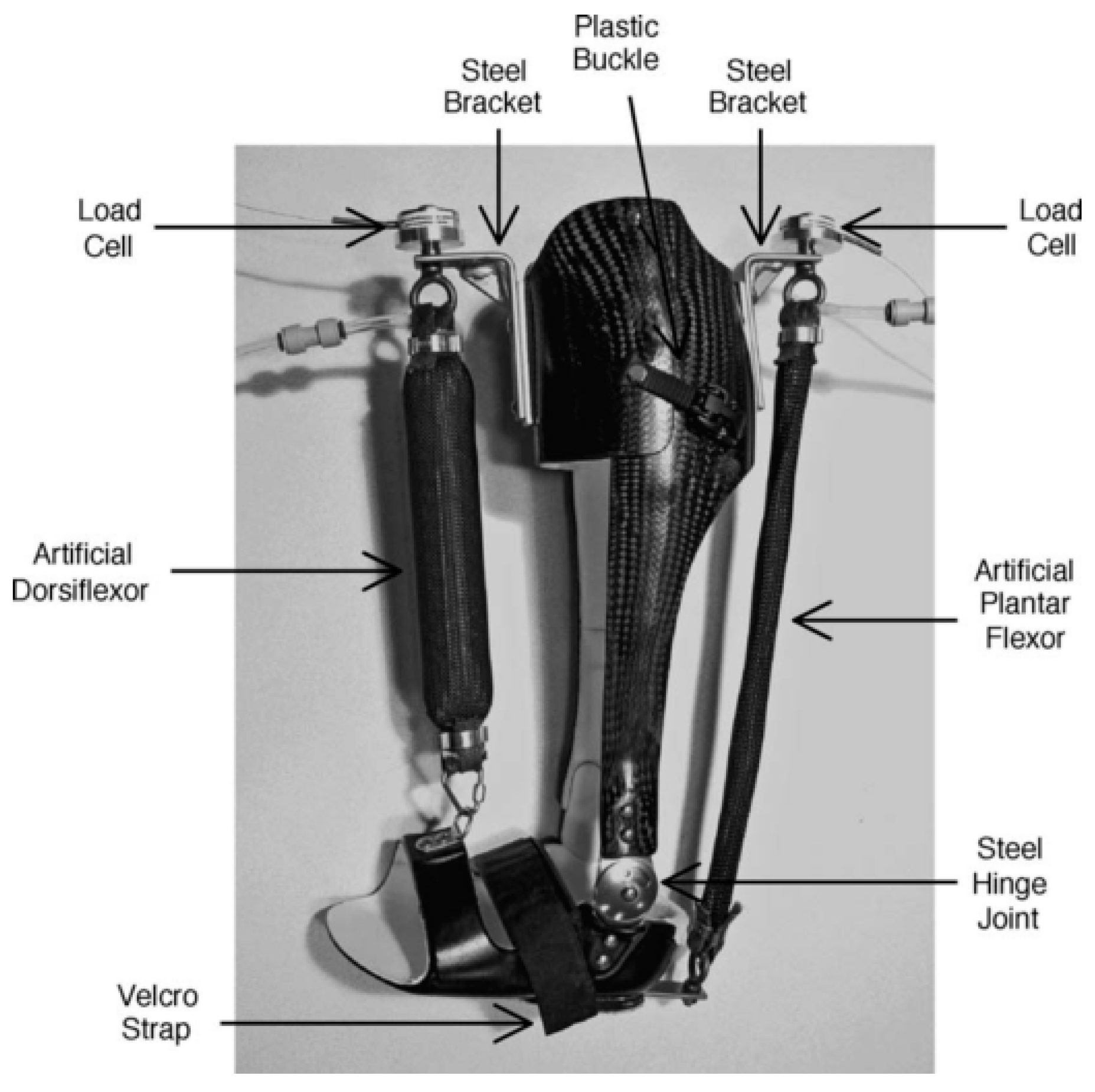
4.3. Assistive Torque
4.4. Motion Path Control
5. Discussion
5.1. Input Considerations for Gait Phase Classification
5.2. Output Reference: Fixed versus Adaptive
5.3. Controller Performance Evaluation
6. Future Research
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Vámos, T.; Berencsi, A.; Fazekas, G.; Kullmann, L. Precise isometric hand grip learning of hemiparetic stroke patients. Int. J. Rehabil. Res. 2018, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Bouffard, J.; Salomoni, S.E.; Mercier, C.; Tucker, K.; Roy, J.-S.; van den Hoorn, W.; Bouyer, L.J. Effect of experimental muscle pain on the acquisition and retention of locomotor adaptation: Different motor strategies for a similar performance. J. Neurophysiol. 2018, 119, 1647–1657. [Google Scholar] [CrossRef] [PubMed]
- Abedi, M.; Moghaddam, M.M.; Fallah, D. A Poincare map-based analysis of stroke patients’ walking after a rehabilitation by a robot. Math. Biosci. 2018, 299, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Huo, W.; Mohammed, S.; Moreno, J.C.; Amirat, Y. Lower Limb Wearable Robots for Assistance and Rehabilitation: A State of the Art. IEEE Syst. J. 2016, 10, 1068–1081. [Google Scholar] [CrossRef]
- Iñaki, D.; Jorge, J.G.; Emilio, S. Lower-Limb Robotic Rehabilitation: Literature Review and Challenges. J. Robot. 2011, 2011, 759764. [Google Scholar] [CrossRef]
- Edwards, M.K.; Rosenbaum, S.; Loprinzi, P.D. Differential Experimental Effects of a Short Bout of Walking, Meditation, or Combination of Walking and Meditation on State Anxiety Among Young Adults. Am. J. Health Promot. 2017. [Google Scholar] [CrossRef] [PubMed]
- Garzon, L.C.; Switzer, L.; Musselman, K.E.; Fehlings, D. The use of functional electrical stimulation to improve upper limb function in children with hemiplegic cerebral palsy: A feasibility study. J. Rehabil. Assist. Technol. Eng. 2018, 5, 1–15. [Google Scholar] [CrossRef]
- Lawton, M.; Sage, K.; Haddock, G.; Conroy, P.; Serrant, L. Speech and language therapists’ perspectives of therapeutic alliance construction and maintenance in aphasia rehabilitation post-stroke. Int. J. Lang. Commun. Disord. 2018, 1–14. [Google Scholar] [CrossRef]
- Song, S.H.; Park, J.H.; Song, G.D.; Lee, S.G.; Jo, Y.H.; Jin, M.K.; Lee, G.C. Usability of the Thera-Band® to improve foot drop in stroke survivors. Neuro Rehabil. 2018, 42, 505–510. [Google Scholar] [CrossRef]
- Williamson, P.; Lechtig, A.; Hanna, P.; Okajima, S.; Biggane, P.; Nasr, M.; Nazarian, A. Pressure Distribution in the Ankle and Subtalar Joint with Routine and Oversized Foot Orthoses. Foot Ankle Int. 2018, 39, 994–1000. [Google Scholar] [CrossRef]
- Miao, Q.; Zhang, M.; Wang, C.; Li, H. Towards optimal platform-based robot design for ankle rehabilitation: The state of the art and future prospects. J. Healthc. Eng. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Jamwal, P.K.; Ghayesh, M.H. State-of-the-art robotic devices for ankle rehabilitation: Mechanism and control review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017, 231, 1224–1234. [Google Scholar] [CrossRef] [PubMed]
- Gijon-Nogueron, G.; Ramos-Petersen, L.; Ortega-Avila, A.B.; Morales-Asencio, J.M.; Garcia-Mayor, S. Effectiveness of foot orthoses in patients with rheumatoid arthritis related to disability and pain: A systematic review and meta-analysis. Qual. Life Res. 2018, 27, 3059–3069. [Google Scholar] [CrossRef] [PubMed]
- Requier, B.; Bensoussan, L.; Mancini, J.; Delarque, A.; Viton, J.M.; Kerzoncuf, M. Knee-ankle-foot orthoses for treating posterior knee pain resulting from genu recurvatum: Efficiency, patients’ tolerance and satisfaction. J. Rehabil. Med. 2018, 50, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Pongpipatpaiboon, K.; Mukaino, M.; Matsuda, F.; Ohtsuka, K.; Tanikawa, H.; Yamada, J.; Saitoh, E. The impact of ankle-foot orthoses on toe clearance strategy in hemiparetic gait: A cross-sectional study. J. Neuro Eng. Rehabil. 2018, 15, 1–12. [Google Scholar] [CrossRef]
- Vistamehr, A.; Kautz, S.A.; Neptune, R.R. The influence of solid ankle-foot-orthoses on forward propulsion and dynamic balance in healthy adults during walking. Clin. Biomech. 2014, 29, 583–589. [Google Scholar] [CrossRef]
- Adiputra, D.; Ubaidillah Mazlan, S.A.; Zamzuri, H.; Rahman, M.A.A. Fuzzy Logic Control for Ankle Foot Orthoses Equipped with Magnetorheological Brake. Jurnal Teknol. 2016, 78, 2016. [Google Scholar] [CrossRef]
- Arch, E.S.; Stanhope, S.J.; Higginson, J.S. Passive-dynamic ankle–foot orthosis replicates soleus but not gastrocnemius muscle function during stance in gait: Insights for orthosis prescription. Prosthet. Orthot. Int. 2016, 40, 606–616. [Google Scholar] [CrossRef]
- Tavernese, E.; Petrarca, M.; Rosellini, G.; Di Stanislao, E.; Pisano, A.; Di Rosa, G.; Castelli, E. Carbon Modular Orthosis (Ca. M.O.): An innovative hybrid modular ankle-foot orthosis to tune the variable rehabilitation needs in hemiplegic cerebral palsy. Neuro Rehabil. 2017, 40, 447–457. [Google Scholar] [CrossRef]
- Collins, S.H.; Bruce Wiggin, M.; Sawicki, G.S. Reducing the energy cost of human walking using an unpowered exoskeleton. Nature 2015, 522, 212–215. [Google Scholar] [CrossRef]
- Kikuchi, T.; Tanida, S.; Yasuda, T.; Fujikawa, T. Automatic adjustment of initial drop speed of foot for intelligently controllable ankle foot orthosis. In Proceedings of the 2013 6th IEEE/SICE International Symposium on System Integration, Kobe, Japan, 15–17 December 2013; pp. 276–281. [Google Scholar] [CrossRef]
- Delafontaine, A.; Gagey, O.; Colnaghi, S.; Do, M.-C.; Honeine, J.-L. Rigid Ankle Foot Orthosis Deteriorates Mediolateral Balance Control and Vertical Braking during Gait Initiation. Front. Hum. Neurosci. 2017, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bregman, D.J.J.; De Groot, V.; Van Diggele, P.; Meulman, H.; Houdijk, H.; Harlaar, J. Polypropylene ankle foot orthoses to overcome drop-foot gait in central neurological patients: A mechanical and functional evaluation. Prosthet. Orthot. Int. 2010, 34, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Nikamp, C.D.M.; Hobbelink, M.S.H.; Palen, J.; Van Der Hermens, H.J.; Rietman, J.S.; Buurke, J.H. A randomized controlled trial on providing ankle-foot orthoses in patients with (sub-)acute stroke: Short-term kinematic and spatiotemporal effects and effects of timing. Gait Posture 2017. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, P.N.F.; Hamzaid, N.A.; Usman, J.; Islam, M.A.; Kean, V.S.P.; Wahab, A.K.A.; Davis, G.M. Variations of ankle-foot orthosis-constrained movements increase ankle range of movement while maintaining power output of recumbent cycling. Biomed. Tech. 2017. [Google Scholar] [CrossRef] [PubMed]
- Tyson, S.F.; Vail, A.; Thomas, N.; Woodward-Nutt, K.; Plant, S.; Tyrrell, P.J. Bespoke versus off-the-shelf ankle-foot orthosis for people with stroke: Randomized controlled trial. Clin. Rehabil. 2018, 32, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Daryabor, A.; Arazpour, M.; Aminian, G. Effect of different designs of ankle-foot orthoses on gait in patients with stroke: A systematic review. Gait Posture 2018, 62, 268–279. [Google Scholar] [CrossRef] [PubMed]
- Mazumder, O.; Kundu, A.; Lenka, P.; Bhaumik, S. Robotic AFO to enhance walking capacity: Initial development. Electron. Lett. 2016, 52, 1840–1841. [Google Scholar] [CrossRef]
- Sawicki, G.S.; Ferris, D.P. A pneumatically powered knee-ankle-foot orthosis (KAFO) with myoelectric activation and inhibition. J. Neuro Eng. Rehabil. 2009, 6, 1–16. [Google Scholar] [CrossRef]
- Chen, B.; Zhao, X.; Ma, H.; Qin, L.; Liao, W.-H. Design and characterization of a magnetorheological series elastic actuator for a lower extremity exoskeleton. Smart Mater. Struct. 2017, 26, 105008. [Google Scholar] [CrossRef]
- Naito, H.; Akazawa, Y.; Tagaya, K.; Matsumoto, T.; Tanaka, M. An ankle-foot orthosis with a variable-resistance ankle joint using a magnetorheological-fluid rotary damper. J. Biomech. Sci. Eng. 2009, 4, 182–191. [Google Scholar] [CrossRef]
- Van Der Wilk, D.; Reints, R.; Postema, K.; Gort, T.; Harlaar, J.; Hijmans, J.M.; Verkerke, G.J. Development of an ankle-foot orthosis that provides support for flaccid paretic plantarflexor and dorsiflexor muscles. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Frascarelli, F.; Masia, L.; Di Rosa, G.; Cappa, P.; Petrarca, M.; Castelli, E.; Krebs, H.I. The impact of robotic rehabilitation in children with acquired or congenital movement disorders. Eur. J. Phys. Rehabil. Med. 2009, 45, 135–141. [Google Scholar] [PubMed]
- Emmens, A.R.; Van Asseldonk, E.H.F.; Van Der Kooij, H. Effects of a powered ankle-foot orthosis on perturbed standing balance. J. Neuro Eng. Rehabil. 2018, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Fabián, R.; Verlinden, O. Review of control algorithms for robotic ankle systems in lower-limb orthoses, prostheses, and exoskeletons. Med. Eng. Phys. 2012, 34, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Hong, Z.; Sui, M.; Zhuang, Z.; Liu, H.; Zheng, X.; Cai, C.; Jin, D. Effectiveness of Neuromuscular Electrical Stimulation on Lower Limbs of Patients with Hemiplegia After Chronic Stroke: A Systematic Review. Arch. Phys. Med. Rehabil. 2018, 99, 1011.e1–1022.e1. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Or, Y. Modelling the dynamics and control of rehabilitative exoskeleton with robotic crutches. Int. J. Adv. Robot. Syst. 2018, 15, 1–14. [Google Scholar] [CrossRef]
- Shih, L.-Y.; Wu, J.-J.; Lo, W.-H. Changes in Gait and Maximum Ankle Torque in Patients with Ankle Arthritis. Foot Ankle 1993, 14, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.; Docherty, C.L.; Schrader, J.; Applegate, T. Eccentric plantar-flexor torque deficits in participants with functional ankle instability. J. Athl. Train. 2008, 43, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, T.; Tanida, S.; Otsuki, K.; Yasuda, T.; Furusho, J. Development of third-generation intelligently controllable ankle-foot orthosis with compact MR fluid brake. In Proceedings of the IEEE International Conference on Robotics and Automation, Anchorage, AK, USA, 3–7 May 2010; pp. 2209–2214. [Google Scholar] [CrossRef]
- Tanida, S.; Kikuchi, T.; Kakehashi, T.; Otsuki, K.; Ozawa, T.; Fujikawa, T.; Hashimoto, Y. Intelligently controllable Ankle Foot Orthosis (I-AFO) and its application for a patient of Guillain-Barre syndrome. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, ICORR, Kyoto, Japan, 23–26 June 2009; pp. 857–862. [Google Scholar] [CrossRef]
- Tamburella, F.; Moreno, J.C.; Iosa, M.; Pisotta, I.; Cincotti, F.; Mattia, D.; Molinari, M. Boosting the traditional physiotherapist approach for stroke spasticity using a sensorized ankle foot orthosis: A pilot study. Top. Stroke Rehabil. 2017, 24, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, J.; Morin, E.; Mousavi, P.; Mountjoy, K.; Hashtrudi-zaad, K. EMG—Force modelling using parallel cascade identification. J. Electromyogr. Kinesiol. 2012, 22, 469–477. [Google Scholar] [CrossRef]
- Liu, P.; Liu, L.; Martel, F.; Rancourt, D.; Clancy, E.A. Influence of joint angle on EMG—Torque model during constant-posture, quasi-constant-torque contractions. J. Electromyogr. Kinesiol. 2013, 23, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Liu, L.; Clancy, E.A.; Member, S. Influence of Joint Angle on EMG-Torque Model During Constant-Posture, Torque-Varying Contractions. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Fleischer, C.; Hommel, G. EMG-Driven Human Model for Orthosis Control. Hum. Interact. Mach. 2006, 69–76. [Google Scholar] [CrossRef]
- Ferris, D.P.; Gordon, K.E.; Sawicki, G.S.; Peethambaran, A. An improved powered ankle-foot orthosis using proportional myoelectric control. Gait Posture 2006, 23, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Adiputra, D.; Mazlan, S.A.; Zamzuri, H.; Rahman, M.A.A. Development of Controller for Passive Control Ankle Foot Orthoses (PICAFO) based on Electromyography (EMG) Signal and Angle. In Proceedings of the Joint International Conference on Electric Vehicular Technology and Industrial, Mechanical, Electrical, and Chemical Engineering (ICEVT & IMECE), Surakarta, Indonesia, 4–5 November 2015; pp. 200–206. [Google Scholar] [CrossRef]
- Adiputra, D.; Rahman, M.A.A.; Ubaidillah Tjahjana, D.D.D.P.; Widodo, P.J.; Imaduddin, F. Controller Development of a Passive Control Ankle Foot Orthosis. In Proceedings of the International Conference on Robotics, Automation and Sciences, Melaka, Malaysia, 27–29 November 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Alam, M.; Choudhury, I.A.; Mamat, A.B. Mechanism and Design Analysis of Articulated Ankle Foot Orthoses for Drop-Foot. Sci. World J. 2014, 1–14. [Google Scholar] [CrossRef]
- Boehler, A.W.; Hollander, K.W.; Sugar, T.G.; Shin, D. Design, implementation and test results of a robust control method for a powered ankle foot orthosis (AFO). In Proceedings of the IEEE International Conference on Robotics and Automation, Pasadena, CA, USA, 19–23 May 2008; pp. 2025–2030. [Google Scholar] [CrossRef]
- Kikuchi, T.; Ikeda, K.; Otsuki, K.; Kakehashi, T.; Tanida, S.; Furusho, J. Basic study on prediction of initial contact for intelligently controlled ankle foot orthosis (I-AFO). In Proceedings of the 2008 IEEE International Conference on Robotics and Biomimetics, ROBIO, Bangkok, Thailand, 22–25 February 2008; pp. 86–90. [Google Scholar] [CrossRef]
- Gordon, K.E.; Sawicki, G.S.; Ferris, D.P. Mechanical performance of artificial pneumatic muscles to power an ankle-foot orthosis. J. Biomech. 2006, 39, 1832–1841. [Google Scholar] [CrossRef]
- Patane, F.; Rossi, S.; Del Sette, F.; Taborri, J.; Cappa, P. WAKE-up exoskeleton to assist children with Cerebral Palsy: Design and preliminary evaluation in level walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 906–916. [Google Scholar] [CrossRef]
- Shorter, K.A.; Li, Y.; Bretl, T.; Hsiao-Wecksler, E.T. Modeling, control, and analysis of a robotic assist device. Mechatronics 2012, 22, 1067–1077. [Google Scholar] [CrossRef]
- Svensson, W.; Holmberg, U. Ankle-foot-orthosis control in inclinations and stairs. In Proceedings of the 2008 IEEE International Conference on Robotics, Automation and Mechatronics, RAM, Chengdu, China, 21–24 September 2008; pp. 301–306. [Google Scholar] [CrossRef]
- Yeung, L.F.; Ockenfeld, C.; Pang, M.K.; Wai, H.W.; Soo, O.Y.; Li, S.W.; Tong, K.Y. Randomized controlled trial of robot-assisted gait training with dorsiflexion assistance on chronic stroke patients wearing ankle-foot-orthosis. J. Neuro Eng. Rehabil. 2018, 15, 1–12. [Google Scholar] [CrossRef]
- Stanhope, S.J.; Siegel, K.L.; Halstead, L.S. Contribution of dynamic Ankle-Foot Orthoses to ankle moments during stance in gait. In Proceedings of the ISPO World Conference, Vancouver, BC, Canada, 27 July 2007. [Google Scholar]
- Walbran, M.; Turner, K.; McDaid, A.J. Customized 3D printed ankle-foot orthosis with adaptable carbon fibre composite spring joint. Cogent Eng. 2016, 3, 1–11. [Google Scholar] [CrossRef]
- Potter, B.K.; Sheu, R.G.; Stinner, D.; Fergason, J.; Hsu, J.R.; Kuhn, K.; MacKenzie, E.J. Multisite Evaluation of a Custom Energy-Storing Carbon Fibre Orthosis for Patients with Residual Disability After Lower-Limb Trauma. J. Bone Joint Surg. Am. Vol. 2018, 100, 1781–1789. [Google Scholar] [CrossRef] [PubMed]
- Schrank, E.S.; Hitch, L.; Wallace, K.; Moore, R.; Stanhope, S.J. Assessment of a Virtual Functional Prototyping Process for the Rapid Manufacture of Passive-Dynamic Ankle-Foot Orthoses. J. Biomech. Eng. 2013, 135, 101011. [Google Scholar] [CrossRef] [PubMed]
- Aydin, L.; Kucuk, S. A method for more accurate FEA results on a medical device developed by 3D technologies. Polym. Adv. Technol. 2018, 29, 2281–2286. [Google Scholar] [CrossRef]
- Harper, N.G.; Russell, E.; Wilken, J.M.; Neptune, R.R. The influence of ankle-foot orthosis stiffness on walking performance in individuals with lower-limb impairments. J. Clin. Biomech. 2014, 29, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Waterval, N.F.J.; Nollet, F.; Harlaar, J.; Brehm, M.A. Precision orthotics: Optimising ankle foot orthoses to improve gait in patients with neuromuscular diseases; Protocol of the PROOF-AFO study, a prospective intervention study. BMJ Open 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Tanaka, S.; Motojima, N. Comparison of ankle–foot orthoses with plantar flexion stop and plantar flexion resistance in the gait of stroke patients: A randomized controlled trial. Prosthet. Orthot. Int. 2018, 42, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Ohata, K.; Yasui, T.; Tsuboyama, T.; Ichihashi, N. Effects of an ankle-foot orthosis with oil damper on muscle activity in adults after stroke. Gait Posture 2011, 33, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Leung, A.K.L.; Akazawa, Y.; Hutchins, S.W. Design of a stiffness-adjustable ankle-foot orthosis and its effect on ankle joint kinematics in patients with stroke. Gait Posture 2011, 33, 721–723. [Google Scholar] [CrossRef]
- Yamamoto, S.; Fuchi, M.; Yasui, T. Change of rocker function in the gait of stroke patients using an ankle foot orthosis with an oil damper: Immediate changes and the short-term effects. Prosthet. Orthot. Int. 2011, 35, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Leung, A.K.L.; Akazawa, Y.; Naito, H.; Tanaka, M.; Hutchins, S.W. Design of an automated device to measure sagittal plane stiffness of an articulated ankle-foot orthosis. Prosthet. Orthot. Int. 2010, 34, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Singer, M.L.; Gao, F.; Hunt, G.; Foreman, K.B. Effect of plantarflexion resistance of an ankle-foot orthosis on ankle and knee joint power during gait in post-stroke individuals. J. Biomech. 2018, 75, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Bolus, N.B.; Teague, C.N.; Inan, O.T.; Kogler, G.F. Instrumented ankle-foot orthosis: Toward a clinical assessment tool for patient-specific optimization of orthotic ankle stiffness. IEEE/ASME Trans. Mechatron. 2017, 22, 2492–2501. [Google Scholar] [CrossRef]
- Kerkum, Y.L.; Buizer, A.I.; Noort, J.C.; Van, D.; Becher, J.G. The Effects of Varying Ankle Foot Orthosis Stiffness on Gait in Children with Spastic Cerebral Palsy Who Walk with Excessive Knee Flexion. PLoS ONE 2015, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Hunt, G.; Lincoln, L.S.; Gao, F.; Lecursi, N.; Foreman, K.B. An articulated ankle–foot orthosis with adjustable plantarflexion resistance, dorsiflexion resistance and alignment: A pilot study on mechanical properties and effects on stroke hemiparetic gait. Med. Eng. Phys. 2017, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Hunt, G.; Gao, F.; LeCursi, N.; Lincoln, L.S.; Foreman, K.B. The effects of an articulated ankle-foot orthosis with resistance-adjustable joints on lower limb joint kinematics and kinetics during gait in post-stroke individuals. Clin. Biomech. 2018, 59, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Pott, P.P.; Wolf, S.I.; Block, J.; van Drongelen, S.; Grün, M.; Heitzmann, D.W.; Hielscher, J.; Horn, A.; Müller, R.; Rettig, O.; et al. Knee-ankle-foot orthosis with powered knee for support in the elderly. Proc. Inst. Mech. Eng.Part H J. Eng. Med. 2017, 231, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Arazpour, M.; Ahmadi Bani, M.; Baniasad, M.; Samadian, M.; Golchin, N. Design, construction, and evaluation of “sensor lock”: An electromechanical stance control knee joint. Disabil. Rehabil. Assist. Technol. 2018, 13, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Braun, J.-M.; Wörgötter, F.; Manoonpong, P. Modular Neural Mechanisms for Gait Phase Tracking, Prediction, and Selection in Personalizable Knee-Ankle-Foot-Orthoses. Front. Neurorobot. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, T.; Tanida, S.; Otsuki, K.; Yasuda, T.; Furusho, J. A novel estimating method of the gait state and velocity control in the initial stance phase for the intelligent ankle foot orthosis with compact MR fluid brake(i-AFO). J. Jpn. Soc. Exp. Mech. 2010, 10, 240–246. [Google Scholar] [CrossRef]
- Zhang, M.; Cao, J.; Xie, S.Q.; Zhu, G.; Zeng, X.; Huang, X.; Xu, Q. A Preliminary Study on Robot-Assisted Ankle Rehabilitation for the Treatment of Drop Foot. J. Intell. Robot. Syst. Theory Appl. 2018, 91, 207–215. [Google Scholar] [CrossRef]
- Guerrero-Castellanos, J.F.; Rifaï, H.; Arnez-Paniagua, V.; Linares-Flores, J.; Saynes-Torres, L.; Mohammed, S. Robust Active Disturbance Rejection Control via Control Lyapunov Functions: Application to Actuated-Ankle–Foot-Orthosis. Control Eng. Pract. 2018, 80, 49–60. [Google Scholar] [CrossRef]
- Santos, C.P.; Alves, N.; Moreno, J.C. Biped Locomotion Control through a Biomimetic CPG-based Controller. J. Intell. Robot. Syst. Theory Appl. 2017, 85, 47–70. [Google Scholar] [CrossRef]
- Nachstedt, T.; Tetzlaff, C.; Manoonpong, P. Fast dynamical coupling enhances frequency adaptation of oscillators for robotic locomotion control. Front. Neurorobot. 2017, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tropea, P.; Vitiello, N.; Martelli, D.; Aprigliano, F.; Micera, S.; Monaco, V. Detecting Slipping-Like Perturbations by Using Adaptive Oscillators. Ann. Biomed. Eng. 2015, 43, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Ronsse, R.; Lenzi, T.; Vitiello, N.; Koopman, B.; Van Asseldonk, E.; De Rossi, S.M.M.; Ijspeert, A.J. Oscillator-based assistance of cyclical movements: Model-based and model-free approaches. Med. Biol. Eng. Comput. 2011, 49, 1173–1185. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Garate, V.; Parri, A.; Yan, T.; Munih, M.; Molino Lova, R.; Vitiello, N.; Ronsse, R. Walking Assistance Using Artificial Primitives: A Novel Bioinspired Framework Using Motor Primitives for Locomotion Assistance Through a Wearable Cooperative Exoskeleton. IEEE Robot. Autom. Mag. 2016, 23, 83–95. [Google Scholar] [CrossRef]
- Eilenberg, M.F.; Geyer, H.; Herr, H. Control of a powered ankle-foot prosthesis based on a neuromuscular model. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.R.; Dzeladini, F.; Brug, T.J.H.; Tamburella, F.; Tagliamonte, N.L.; Van Asseldonk, E.H.F.; Ijspeert, A.J. An adaptive neuromuscular controller for assistive lower-limb exoskeletons: A preliminary study on subjects with spinal cord injury. Front. Neurorobot. 2017, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Geyer, H.; Thatte, N.; Duan, H. Toward Balance Recovery with Active Leg Prostheses Using Neuromuscular Model Control. IEEE Trans. Biomed. Eng. 2017, 15, 649–652. [Google Scholar] [CrossRef]
- Geyer, H.; Herr, H. A Muscle-reflex model that encodes principles of legged mechanics produces human walking dynamics and muscle activities. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 263–273. [Google Scholar] [CrossRef]
- Song, S.; Geyer, H. A neural circuitry that emphasizes spinal feedback generates diverse behaviours of human locomotion. J. Physiol. 2015, 593, 3493–3511. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Geyer, H. Evaluation of a Neuromechanical Walking Control Model Using Disturbance Experiments. Front. Comput. Neurosci. 2017, 11. [Google Scholar] [CrossRef] [PubMed]
- Nazmi, N.; Azizi, M.; Rahman, A. Electromyography (EMG) based Signal Analysis for Physiological Device Application in Lower Limb Rehabilitation. In Proceedings of the 2nd International Conference on Biomedical Engineering, Penang, Malaysia, 30–31 March 2015. [Google Scholar]
- Villa-Parra, A.C.; Delisle-Rodriguez, D.; Lima, J.S.; Frizera-Neto, A.; Bastos, T. Knee impedance modulation to control an active orthosis using insole sensors. Sensors 2017, 17, 2751. [Google Scholar] [CrossRef] [PubMed]
- Healy, A.; Farmer, S.; Pandyan, A.; Chockalingam, N. A systematic review of randomised controlled trials assessing effectiveness of prosthetic and orthotic interventions. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Abtahi, S.M.A.; Jamshidi, N.; Ghaziasgar, A. The effect of Knee-Ankle-Foot orthosis stiffness on the parameters of walking. Comput. Methods Biomech. Biomed. Eng. 2018, 21, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Katsuhira, J.; Yamamoto, S.; Machida, N.; Ohmura, Y.; Fuchi, M.; Ohta, M.; Matsudaira, K. Immediate synergistic effect of a trunk orthosis with joints providing resistive force and an ankle–foot orthosis on hemiplegic gait. Clin. Interv. Aging 2018, 13, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Moltedo, M.; Baček, T.; Verstraten, T.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Powered ankle-foot orthoses: The effects of the assistance on healthy and impaired users while walking. J. Neuro Eng. Rehabil. 2018. [Google Scholar] [CrossRef] [PubMed]
- Sadeghian, F.; Zakerzadeh, M.R.; Karimpour, M.; Baghani, M. Compliant orthoses for repositioning of knee joint based on super-elasticity of shape memory alloys. J. Intell. Mater. Syst. Struct. 2018, 29, 3136–3150. [Google Scholar] [CrossRef]
- Nalam, V.; Lee, H. Environment-Dependent Modulation of Human Ankle Stiffness and its Implication for the Design of Lower Extremity Robots. In Proceedings of the 2018 15th International Conference on Ubiquitous Robots, Honolulu, HI, USA, 27–30 June 2018; pp. 112–118. [Google Scholar] [CrossRef]
- Shakti, D.; Mathew, L.; Kumar, N.; Kataria, C. Effectiveness of robo-assisted lower limb rehabilitation for spastic patients: A systematic review. Biosens. Bioelectron. 2018, 117, 403–415. [Google Scholar] [CrossRef] [PubMed]
| Name | Control Orientation | References | Input | Gait Phases | Output Reference | Estimation Method | Control | Actuator | Performance |
|---|---|---|---|---|---|---|---|---|---|
| Rigid AFO | Subject-Oriented | 16, 22, 23, 38, 42 | - | - | Bending stiffness | - | Manufacturer | Thermoplastic |
|
| Flexible Rigid AFO | 18, 25, 26, 57, 58, 61, 63 | Motion | - | Bending stiffness | Model | Manufacturer | Thermoplastic |
| |
| 19, 59, 60, 64 | Motion | - | Bending stiffness | - | Modular | Carbon fiber |
| ||
| 62 | Bending Stiffness | Model | Manufacturer | Acrylonitrile Butadine Styrene (ABS) Polymer |
| ||||
| Articulated AFO | 28, 34 | GRF, Motion | - | Motion | Direct | PID | DC motor |
| |
| 80 | GRF, Motion | - | Motion | Direct | Lyapunov Control | DC motor |
| ||
| 29, 47, 53 | EMG | - | Assistive Torque | Direct | PID | Pneumatic |
| ||
| 20, 71, 72, 70, 73, 74 | Motion | - | Damping stiffness | - | Screw mechanism | Spring |
| ||
| 65, 66, 67, 68 | - | - | Damping Stiffness | - | Screw Mechanism | Oil damper |
| ||
| 79 | Motion | - | Motion | - | PID | Pneumatic |
| ||
| Phase-Oriented | 17, 48, 49 | EMG, Motion | 2 | Damping stiffness | Fuzzy Logic | - | MR brake |
| |
| 31, 56 | Foot Switch, Motion | 3 | Damping stiffness | Fix look-up table | - | MR damper |
| ||
| 32 | Motion | 3 | Damping stiffness | Model | On/off | Solenoid |
| ||
| 21 | Motion | 3 | Motion | Model | PID | MR brake |
| ||
| 40, 78 | Motion | 3 | Motion | Direct | PID | MR brake |
| ||
| 41, 52 | Foot Switch, Motion | 4 | Damping stiffness | Fix look up table | - | MR brake |
| ||
| 55 | Motion | 3 | Motion | Direct | PID | Solenoid |
| ||
| KAFO | Subject-Oriented | 46 | EMG, Motion | - | Motion | Model | PID | Motor |
|
| KAFO | 75 | GRF | - | Damping stiffness | Model | PID | SEA |
| |
| KAFO | Phase-Oriented | 51, 54, 76 | GRF, Motion | 3 | Assistive torque | Direct | PID | SEA |
|
| KAFO | 77 | GRF, motion | 2 | Damping stiffness | Model | Neural Network | Hydraulic Damper |
| |
| Exoskeleton | 30 | GRF, Motion | 3 | Motion | Direct | PID | MRSEA |
| |
| Exoskeleton | Subject Oriented | 84, 87 | GRF, Motion | - | Motion | Model | - | SEA |
|
| Active Pelvis Orthosis | 85 | GRF, Motion | - | Motion | Model | - | Motor |
| |
| Prosthesis | 86 | GRF, Motion | - | Motion | Model | PID | SEA |
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adiputra, D.; Nazmi, N.; Bahiuddin, I.; Ubaidillah, U.; Imaduddin, F.; Abdul Rahman, M.A.; Mazlan, S.A.; Zamzuri, H. A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance. Actuators 2019, 8, 10. https://doi.org/10.3390/act8010010
Adiputra D, Nazmi N, Bahiuddin I, Ubaidillah U, Imaduddin F, Abdul Rahman MA, Mazlan SA, Zamzuri H. A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance. Actuators. 2019; 8(1):10. https://doi.org/10.3390/act8010010
Chicago/Turabian StyleAdiputra, Dimas, Nurhazimah Nazmi, Irfan Bahiuddin, Ubaidillah Ubaidillah, Fitrian Imaduddin, Mohd Azizi Abdul Rahman, Saiful Amri Mazlan, and Hairi Zamzuri. 2019. "A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance" Actuators 8, no. 1: 10. https://doi.org/10.3390/act8010010
APA StyleAdiputra, D., Nazmi, N., Bahiuddin, I., Ubaidillah, U., Imaduddin, F., Abdul Rahman, M. A., Mazlan, S. A., & Zamzuri, H. (2019). A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance. Actuators, 8(1), 10. https://doi.org/10.3390/act8010010