Abstract
People with disabilities often face challenges like moving around independently and depending on personal caregivers for daily life activities. Traditional assistive devices are universally accepted by these communities, but they are designed with one-size-fits-all approaches that cannot adjust to individual human sizes, are not easily customized, and are made from rigid materials that do not adapt as a person’s condition changes over time. This systematic review examines the integration of smart materials, sensors, actuators, and 3D/4D printing technologies in advancing assistive devices, with a particular emphasis on mobility aids. In this work, the authors conducted a comparative analysis of traditional devices with commercially available innovative prototypes and research stage assistive devices by focusing on smart adaptable materials and sustainable additive manufacturing techniques. The results demonstrate how artificial intelligence drives smart assistive devices in hospital decentralized additive manufacturing, and policy frameworks agree with the Sustainable Development Goals, representing the future direction for adaptive assistive technology. Also, by combining 3D/4D printing and AI, it is possible to produce adaptive, affordable, and patient centered rehabilitation with feedback and can also provide predictive and preventive healthcare strategies. The successful commercialization of adaptive assistive devices relies on cost effective manufacturing techniques clinically aligned development supported by cross disciplinary collaboration to ensure scalable, sustainable, and universally accessible smart solutions. Ultimately, it paves the way for smart, sustainable, and clinically viable assistive devices that outperform conventional solutions and promote equitable access for all users.
1. Introduction
People having mobility challenges and physical disabilities such as Parkinson’s disease, spinal cord injuries (SCI), multiple sclerosis, amyotrophic lateral sclerosis, cerebral palsy, and muscular dystrophy have to live a hard life with less confidence and complex challenges like pressure sores and endure chronic pain and fatigue. It includes impaired mobility and muscle control, making routine activities, such as sitting, standing, dressing, eating, and moving independently, difficult without assistance. Patients with mobility impairments generally experience one of two basic types of disability: progressive disabilities, which involve a gradual physical decline over time, and static disabilities, which remain stable but still necessitate ongoing adaptation [1]. Additionally, societal misconceptions [2], employment barriers, and financial hardship further erode their quality of life, whereas assistive technologies (ATs) [3], tailored rehabilitation, and inclusive policies are crucial in empowering individuals to regain autonomy [4]. Actual equity demands not just providing medical help but also eliminating the unfair attitudes and systems that strip people of their dignity and choice of career [5,6].
There is a need to study and evaluate a wide range of devices, software, support, and assistive services designed to improve lifestyle, daily activities, manage chronic conditions, enhance health, and promote functional independence for individuals with disabilities and chronic conditions [7]. Assistive devices (ADs) [8,9], including mobility aids, communication devices, hearing aids, and adaptive equipment, have increased control in daily life activities for patients with disabilities. In recent times, smart materials (SMs) and artificial intelligence (AI) have transformed these technologies.
Beyond physical devices, for effective adoption and long term usability, personalized assessments, training, cost, aesthetics, comfort, ease of maintenance, and control are critical fields that need to be focused on. After addressing gaps in mobility [10], communication, and self-care assistive devices, users will be able to overcome barriers and actively participate in education, employment, and social life without relying on others for support. However, to unlock the transformative potential of AT, there is a need for inclusive policies and equitable distribution. The United Nation’s convention on the rights of persons with disabilities [11] strongly supports the opportunities for exercising personal choice and living independently within the community for persons with disabilities. Rehabilitation and treatment of disabled patients, even with minor injuries and disabilities, is an essential yet underestimated aspect of global healthcare. During 2019 alone, approximately 2.41 billion individuals, representing one third of the world’s population, required rehabilitation services, marking a striking 63% rise since 1990 [12]. Musculoskeletal disorders, notably low back pain, sports injuries, and military rehabilitation, emerged as the main reason for rehabilitation practices. To address this issue, three key actions should be undertaken: elevating rehabilitation within health policy agendas, securing sustainable funding, and integrating rehabilitation services into primary healthcare departments.
Previous reviews have mainly focused on material development, fabrication strategies, and general biomedical applications of 3D/4D printing [13,14]. In contrast, this work addresses a specific research gap by integrating both 3D and 4D printing with their application domains, emphasizing their role in ADs. This perspective provides a user centered and clinical focus that distinguishes this review from [13], which concentrates on magnetically responsive memory polymers, and [14], which discusses 4D printing primarily as a technology.
1.1. Statistics on Global Disability
The World Health Organization (WHO) [15] has extensively documented the global crisis in access to ADs. According to the 2022 global report on AT, almost one billion people with minor or major disabilities are living without any access to AT, whereas an estimated 2.5 billion people need at least one device for assisting in motion, such as wheelchairs, prosthetics, and hearing aids; yet nearly 1 billion people remain without access to these products. This gap is severe in countries having low and middle incomes, where healthcare systems often lack the infrastructure and funding to provide these life changing technologies. The report emphasizes that if no action is taken, the issue will continue to grow, particularly as aging populations increase the demand for mobility and sensory aid.
The WHO identifies 50 essential assistive products, such as wheelchairs, hearing aids, and communication devices, from the priority assistive products list [16] to meet global needs, yet despite the critical role of these technologies, 80% of countries still lack national policies to ensure their role in providing accessibility of these devices to all age groups. There is a report on disability in 2011 [17] by the WHO, which was later updated in 2023, highlighting that 50% of individuals with disabilities cannot afford essential ADs. As a result, many are forced to rely on outdated, inexpensive, and makeshift solutions, which restrict their independence, thereby limiting their adaptability, and provide only limited support. Additionally, the report emphasizes how societal stigma and poor policies marginalize disabled individuals.
Certain types of minor disabilities are becoming common in children; as per the report [18], an estimated 240 million children worldwide are living with disabilities. However, 75% of them lack access to basic ADs. Hence, 50% of them will not attend school, as they require ADs for mobility and psychological support. UNICEF and WHO call for global action on inclusive policies, increased funding, and strengthened international cooperation to ensure that no child is left behind.
In May 2018, there was a resolution, World Health Assembly 71.8 [19], passed by an assembly representing health professionals, urging countries to improve access to AT. This resolution calls for its inclusion in universal health coverage and the creation of a global report on access to AT, utilizing worldwide research and experience. WHO must also report progress made in 2022 and future purposes for 2026 and 2030. These reports will highlight the large gap in access to AT but also show a way to improve the situation. They call on governments, researchers, and industry leaders to focus on creating affordable solutions, making policies more inclusive, and ensuring that AT is part of universal healthcare. By working together, they can help more people obtain the devices and provide moral, ethical, and financial support for better lives.
1.2. Limitations of Traditional Assistive Devices
The traditional ADs, shown in Figure 1, such as manual wheelchairs, basic hearing aids, white canes, and bare prosthetic limbs, have long been used by individuals with disabilities [20]. These devices are affordable and straightforward, with prices ranging from as low as USD 20 for white canes to several thousand dollars for prosthetic limbs. These traditional aids, which had a greater impact in the past, now have numerous limitations. As technology advances, there is a corresponding need for the development of these devices as well. For example, manual wheelchairs [21] require physical strength to propel, whereas basic hearing aids merely amplify sound without offering advanced features such as Bluetooth connectivity and noise cancellation. Similarly, white canes are effective for basic navigation but lack the real time feedback and navigation assistance found in modern bright canes. Prosthetic limbs, though offering basic functionality, do not offer the precision, adaptability, and control provided by advanced bionic and myoelectric limbs [22]. Devices like raised toilet seats and walkers, while providing essential support, offer limited customization and are fixed in their design. In contrast, advanced technologies such as smart toilets and robotic walkers are more adaptable, utilizing sensors, AI, and SMs. Grab bars and crutches, although reliable, often work without the aid of smart sensors (SSs). In contrast, ergonomic innovations, such as bright grab bars and crutches, reduce strain. Bed rails and shower chairs are also effective but lack the motorized and automated adjustments seen in modern solutions. Devices like long reach grabbers and sock aids are simple and cost effective but do not offer the precision and motorized control found in advanced ADs; also, button hooks and utensil cuffs are functional but lack the multi-functionality available in modern adaptive wearables. Braille books, while still crucial, are bulky compared to digital Braille displays [23], having greater flexibility. Pill organizers and transfer boards remain useful, but they are far less sophisticated compared to bright medication dispensers and motorized lift systems.
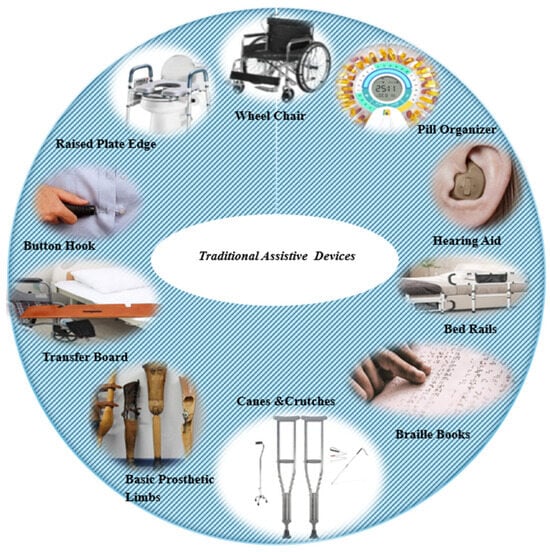
Figure 1.
Traditional ADs.
Overall, traditional ADs (see Table 1), while foundational and accessible, cannot compete with the flexibility, adaptability, and customization offered by advanced technologies. New technologies, such as SMs and SSs, and customized 3D-printed devices [24,25] are helping people with disabilities live more independently and comfortably in ways that traditional ADs were never able to [26]. However, globally, access to smart ADs [27], durability, customer satisfaction, cost, and acceptance by healthcare professionals and patients still need to be addressed.

Table 1.
Widely adopted traditional ADs.
The challenges of high costs and limited accessibility in ADs are often due to the expensive materials, technology, and manufacturing processes involved [28]. Additionally, the distribution networks in these regions can be inefficient, and a lack of local suppliers may lead individuals to rely on expensive imports. In terms of static designs, many traditional ADs are based on one-size-fits-all models that do not account for the unique and evolving needs of individual users. These devices often have limited customization options, meaning that once a device is purchased, it cannot be easily adjusted and adapted to changes in the patient’s condition and preferences. For example, a wheelchair with a fixed seat and armrest configuration might not be comfortable for all users, especially as their mobility needs change over time [29,30]. Similarly, prosthetic limbs, which often come in fixed designs, may not provide sufficient flexibility to adapt to the varying levels of activity and functionality required by the user. The lack of adaptability in these devices results in a situation where users may have to settle for a suboptimal solution, leading to decreased comfort, functionality, and independence. Both the high costs and limited access of advanced, customizable, and adaptive ATs pose significant barriers for people having disabilities.
The combination of these factors makes it even more challenging for individuals with disabilities to lead independent, dignified lives, highlighting the need for innovation in both affordable pricing and more adaptable, user required designs [28].
1.3. Commercially Used Advanced ADs: Current Functioning, Limitations and Future Implementations
This subsection discusses several commercially available ADs, examining their current functionalities, limitations, and potential future developments aimed at improving and expanding their applications. These ADs have undergone rigorous industry validation, secured patent protection, and are now subject to continuous annual enhancements. An overview of these devices is also presented in Table 2.
1. The EksoNR [31] exoskeleton has been utilized to assist patients with neurological impairments in regaining mobility through guided standing and walking rehabilitation (Figure 2a). The most important characteristics include sensor adaptive algorithms, which ensure safe and effective therapy but also involve high costs, limiting accessibility for smaller clinics and those treating diverse patient anatomies [32,33]. Due to advancements in manufacturing techniques, users and health professionals also demand human body dimension based exoskeleton components, AI-controlled tele-rehabilitation, and 4D-printed SMs, which pose future challenges.
2. The ReWalk [34,35] is a motorized, wearable exoskeleton enabling mobility, walking, stair climbing, and ramp navigation for people with spinal problems. Adaptive gait control, clearance by the Food and Drug Administration (FDA) for personal use, and overground mobility are essential performance parameters. In contrast, limited battery life, restricted adaptability for varying levels of paralysis, uneven terrain, and fast transitions from sitting to standing are challenges for future researchers [36]. Stroke patients were trained with a soft exosuit (Figure 2b) for almost two months to test the effects of gait training. Clinical and biomechanical performance were measured and paved the way for adopting exosuits for post-rehabilitation of stroke patients [37]. At the same time, real-time adaptability to muscle fatigue can be improved by using 4D-printed shape memory alloys (SMAs) and self-adjusting structures. Modular designs of brain controlled exoskeletons could also revolutionize mobility for individuals with paralysis.
3. Carbon hand (Figure 2c) is a soft robotic glove, which is designed to provide grip strength for individuals with hand weakness. It utilizes flexible actuators and pressure sensors to detect grip intent and provide proportional assistance, enabling tasks such as holding utensils, tools, and domestic items. It also features intuitive control over shelf sizing. Soft materials wear out over time, have a moderate grip force, which is unsuitable for heavy lifting, and lack finger independence, which are the current challenges [38]. Personalized glove liners for deformed and atrophied hands, 4D smart textiles that integrate haptic feedback, and AI-controlled grip prediction sensors for individual finger movement could bridge current gaps, making it viable for high precision and critical tasks.
4. Neuro Node [39] can control AT with the help of muscle signals and head/limb motions. It is a wireless wearable sensor designed for patients with extremely critical SCI. It is a universal control interface for all digital devices. A study [40] uses neuro node technology (Figure 2d) to test the speed and accuracy of an eye gaze augmentative and alternative communication system with dwell selection (extended gaze) compared to eye gaze combined with electromyography switching, a method designed for users with disabilities that limit independence and communication. Limited precision for multiple tasks, dependence on residual muscle and neck movement, skin irritation, grip assistance problems, and relying on external devices for physical function are current challenges. Eye-tracking hybrid modes, combined with 3D-printed, softer, and more breathable materials, as well as durable direct neural interfaces, can enable seamless control for users with paralysis.
5. LUKE Arm [41] is an advanced prosthetic limb, that is designed for upper arm amputees, focusing on replacing limb function rather than rehabilitating movement, offering multi-articulating joints and intuitive control. Weight and bulkiness compared to biological arms, as well as the lack of full tactile feedback, can restrict fine motor tasks, such as handling fragile items, which are the functional improvements required in the most recent model of 3D- and 4D-printed materials, touch sensation, and closing. A modern six degree of freedom (DOF) LUKE Arm (Figure 2e) is used in a study to achieve natural and precise control of the arm using a modified Kalman filter (a smart control system) [42]. Predictive motion control and battery free power solutions, as well as brain machine interfaces, serve as future challenges. If researchers succeed in solving these issues, it will enable the LUKE Arm to behave more like a real human arm.
6. The HERO (Hand Extension Robot Orthosis) glove (Figure 2f) is an assistive device for heart patients with severe hand impairment, using artificial tendons driven by a linear actuator to enable finger grasping and assisting users in relearning hand movements through automated finger flexion triggered by inertial sensors. Insufficient force for heavy objects, lack of individual finger control, dependency on residual arm movement, and severe spasticity are current trends missing in this glove [43,44]. Three-dimensional printed tendon systems, 4D printed self-stiffening materials, and hybrid control for users with minimal limb mobility, learning user specific movement patterns with the help of AI, could personalize rehabilitation and make this device a modern and adaptive control.
7. Myo suit [45] is a soft exo muscle that uses artificial tendons and elastic bands, and it is designed for users with lower limb weakness who retain some walking ability but fatigue quickly. It lacks adaptive AI control, and no ankle support is available [46]. A study involved experimental evaluation of lower limb joint kinematics and electromyography patterns in healthy subjects walking with and without the Myo suit (Figure 2g) during level overground and incline treadmill walking [47]. Three-dimensional printed elastic actuators and sensors, such as neuro nodes, could improve responsiveness by combining Myo suit’s soft robotics with functional electrical stimulation, among other future challenges for this device.
8. Exo glove is a tendon driven actuation system embedded in flexible polymers. The most important drawback is the dependency on residual muscle signals, which is challenging for high level amputations [48,49]. Advances in pressure sensitive skin, which enhance sensory feedback, and neural lace interfaces may enable direct brain control, serving as a viable alternative for advanced prosthetic hands. Similarly, in order to achieve effective finger rehabilitation, lightweight exo gloves (Figure 2h) using nitinol shape memory alloy (SMA) actuators have been fabricated [50], then numerically simulated and experimentally verified as well. Hence, remote therapy will be achieved using smart actuators combined with telerehabilitation to print small, efficient wearable devices that can help patients recover better.
9. Qolo rehabilitation system is a mobility aid designed for individuals with difficulties in walking and standing. These rehabilitation devices consist of numerous sensors that help in adjusting supports. The human machine interface has been used for rehabilitation sessions. Currently, due to the high-level of advanced digital technology, it has limited home use [51]. Although this system is advanced, personalized rehabilitation based on patient progress, affordable modular supports utilizing 3D and 4D materials, and remote therapist monitoring via cloud data are some improvements that can be made to make this device completely compatible with all kinds of digital advancements needed according to modern digital protocols. To achieve quality of life for children with cerebral palsy, dynamic standing and static standing designs (Figure 2i) were studied over a 4-month period, and dynamic standing was preferred, while more personalized standing care was preferred for each patient [52].
10. The able chair is a hybrid mobility device that transitions from wheelchairs to assisted walking. It consists of a seated support system with motorized walking actuators and balance aids to prevent falls. It promotes rehabilitation, reduces pressure sores, and improves cardiovascular health. It is not designed for long distance mobility, such as wheelchairs; that is why it is less portable than soft exosuits. Additionally, it requires residual leg strength, which is also suitable for cases of complete paralysis, although with some limited applications [53]. Seat and walker components are tailored to individual body shapes using advanced 3D and 4D printed materials and shapes, then adjust support levels based on real time fatigue and terrain data from neural network predictions, serving as a foundation for future modifications in this hybrid chair. Standing up is always a problem for elderly patients; a compact design prototype (Figure 2j) was developed and experimentally validated with four volunteers involved. This design supports the arms of elderly patients using the lifting mechanism allows simple hand and arm engagement after standing [54].
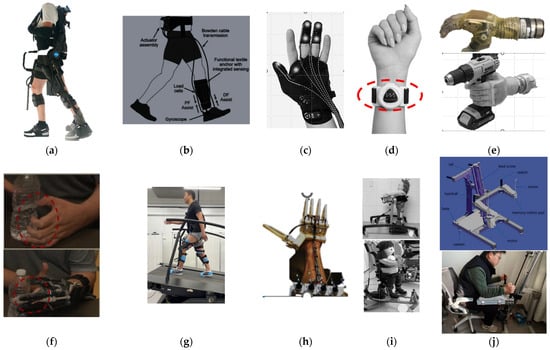
Figure 2.
Commercially available ADs: (a) Ekso NR exoskeleton [33]; (b) ReWalk exosuit [37]; (c) Carbon hand [38]; (d) A neuro node device placed on the forearm to measure when the index finger bends [40]; (e) LUKE Arm [42]; (f) HERO glove assistive tasks for paralyzed patient [43]; (g) Myo suit [47]; (h) Fabricated SMA actuator exo glove [50]; (i) Static and dynamic standing design assistive device [52]; (j) Sit to stand movement AD (CAD and experimental model) [54]. (Figures reproduced from external sources retain their original copyright. Reuse permissions were granted under the creative commons licenses (CC BY 4.0).) (https://creativecommons.org/licenses/by/4.0/ accessed on 10 April 2025).

Table 2.
Commercially available ADs.
Table 2.
Commercially available ADs.
| No. | Type of Device (Year Updated) | Potential Application of 3D/4D Printing Technologies | Material | Actuator, Sensors, Applications |
|---|---|---|---|---|
| 1 | Ekso NR [31] is a robotic exoskeleton for limbs (2023) | Limited 3D shell with future 4D potential with smart materials application. | Aluminum, carbon fiber | Motion sensors, AI-linked circuits |
| 2 | ReWalk personal 6.0 [35] is an exoskeleton for paraplegic patients (2022) | 3D printed braces are possible | Aluminum, polycarbonate | Gyroscope, tilt sensors |
| 3 | Carbon hand [38] is smart grip assist glove. (2024) | 3D glove shells; soft robotics future | Silicone, textile blend | Pneumatic actuators, sensors |
| 4 | Neuro node trilogy [39] is a neural input interface (2022) | Minimal 3D use, flexible PCBs in future | Composite plastic, medical gel | Electromyography sensors, capacitive electronics |
| 5 | LUKE Arm [41] is an advanced prosthetic arm (2023) | 3D sockets; 4D joints future applications | Titanium, silicone, carbon fiber | Neural interfaces, pressure sensors |
| 6 | HERO glove [43,44] is a rehab glove (2022) | 3D finger modules; 4D soft robotics future | Neoprene, nylon | Flex sensors, IMU tracking |
| 7 | Myo suit [45] soft exosuit for legs (2024) | 3D fit shells; 4D fabrics in research | Smart textiles, carbon fabric | Smart stretch sensors, textile circuits |
| 8 | Exo glove poly II [49] is a soft hand exosuit (2023) | Fully 3D printable; 4D in exploration | TPU, nylon, silicone | Pneumatic actuators, embedded sensors |
| 9 | Qolo [51] rehabilitation system is used for sit to stand movements (2022) | 3D frame; 4D seat research ongoing | Aluminum, plastic | McKibben type soft, compliant actuators, load sensors, IMU and pressure sensors |
| 10 | Able chair [53] is a smart power wheelchair (2023) | 3D seat shells; 4D cushion materials in R and D | Aluminum, memory foam | Electric motors, joint position and EMG sensors |
1.4. Breakthroughs in ADs from Academia and Lab Studies
The devices listed in Table 2 represent commercially established technologies. There are some other studies that focused on optimization methodology, such as in [55], where a step approach was employed: first, Kano model is used to identify user demands; second, design elements are obtained using the analytic hierarchy process; and last, a fuzzy comprehensive evaluation technique is used to obtain the best-performing scheme. Another novel omnidirectional Ex robot, WANDER [56], is developed using a preference optimization method for walking aids with multifunctional properties.
On the other hand, Table 3 provides a brief comparison of devices that are currently emerging technologies. The details of these devices are primarily sourced from recent research publications and prototypes. As innovation in manufacturing processes is increasing, there are a lot of prototypes being developed and tested in research institutions and in medical facilities. Some of the applications related to our study will be discussed here.
- SEM glove (Figure 3a) is a motor assisted glove designed for patients with upper limb movement deficiencies [57]. This glove increased the pinch strength of patients when tested on almost 30 hospitalized patients.
- A pilot study [58] was performed on a soft and light textile based exo boot designed to reduce the metabolic effort during walking. A comparative study involving the torque generated by this innovative lightweight assistive device at different pressures and ankle angles is also being performed. In order to enhance the naturalness of single DOF commercial devices, a lightweight, autonomous two DOF ankle prosthesis (Figure 3b) consisting of a screw drive actuator and microcontroller has been developed and tested [59]. Experimental and FEA simulations pave the way for real-world locomotion, whereas future work will focus on fatigue and impacts.
- Neurobotics [60] elbow exoskeleton is designed for patients recovering from stroke and has also been verified with experimental studies. In order to drive a multi DOF anthropomorphic prosthetic hand emulator (Figure 3c), a novel two DOF myoelectric controller using principal components analysis was employed [61]. Twelve participants used two differential EMG (electromyography) channels to grasp, move, and release different objects. They also measured how well and how fast they completed tasks and tracked their improvement over three consecutive days.
- A unique heat cured rubber silicon fabrication process is used to fabricate a voice-controlled flex tendon glove-III, a hand exoskeleton designed for holding and grasping objects. This study also involved a mobile phone app controlled by voice control an object based admittance controller for gripping and grasping. This device was also validated with experimental verification on a healthy user [62]. Similarly, for developing a new rehabilitation glove, a novel actuator design [63] aligned with human finger anatomy and motion was created and tested using soft materials with 3D printed manufacturing technology (Figure 3d). Kinematic models for the index and little finger actuators were developed from pressure and link lengths, and forward kinematics was used for workspace estimation. Finally, the results were verified with anatomical motion and experiments, and glove ergonomics were assessed.
- SPEXOR [64] is an exoskeleton design for improving workplace ergonomics for healthy patients. This exoskeleton is designed to support the spinal cord, unlike other exoskeletons, which were designed for limb assistance and rehabilitation. So, this study focuses on preventive medical assistance. So, in order to manage and prevent low back pain, biomechanical principles have been studied [65]. This research consists of modeling and optimization of spinal exoskeleton interaction (Figure 3e) with the human body, and also the design and development of a passive system with effective control system assistance has been evaluated.
- A novel bio inspired fish like structure having a bionic spine with variable stiffness [66] can be used to create a bionic spine for more natural and energy efficient movement in ADs such as soft exoskeletons and prosthetic limbs. This novel study demonstrates the effectiveness of bio-inspired structures with advantages of adaptability, responsiveness, and better natural motion efficiency. So, by using a flexible bionic spine that can adjust stiffness depending on patient requirements, ADs offer a valuable solution. There is another study in which a multi-stable origami exoskeleton (Figure 3f) is developed, inspired by shrimp exoskeletons, in order to achieve flexible, rigid arrangements [67].
- Power knee [68] is one of the advanced prosthetic knees available with the first microprocessor motor power, so it will give smooth, natural motion, as this advanced prosthetic consists of sensors as well, so it will also reduce user effort and can be used for climbing as well. A novel strategy has been developed by integrating a powered knee prosthesis (Figure 3g) with a control system [69]. This system provides passive behavior during activities requiring minimal power and delivers powered assistance for movements demanding active knee actuation. This intelligent control system is also verified experimentally by making a comparison of a nominally passive system with a conventional passive microprocessor-controlled knee prosthesis.
- The multifunctional elbow brace is designed to treat elbow joint problems with both heat therapy and mechanical pressure. This device [70] is also being experimentally verified on human participants. Knitted SMA fabric provides comfort for daily use, and SMA changes shape when heated, giving smart properties to the fabric, so heating therapy, muscle contraction for joint movement, and mobility assistance to the elbow are achieved after testing on human participants, satisfying the aim of achieving multiple functional outputs. Since COVID-19, numerous strategies and studies have been implemented for increasing the role of robotic technologies in healthcare while keeping patient care, safety, and clinical efficiency as priorities. Recent studies have explored the potential application of knitted shape memory alloys in soft wearable robots, where a flexible knitted shape memory alloy actuator has been developed for a rehabilitation glove [71]. Also, to achieve a realistic patient’s finger range of motion (Figure 3h), both plain and double-knit modules were used.
- Similarly, robots have been used in spinal surgeries to perform simple tasks, but this robotic system (Figure 3i) performs autonomous laminectomy (spinal bone removal to release pressure from the spinal cord). In an experimental approach [72], an advanced robotic system is being used to perform surgeries on four human bodies donated for research, performance metrics were measured and compared with professional surgeons’ outcomes and standards; hence, precise execution is reported.
Below mentioned Table 3 provides a brief comparison of devices explained above, concerning advanced additive manufacturing techniques that are currently emerging, their working principle, and SMs’ potential in these devices.
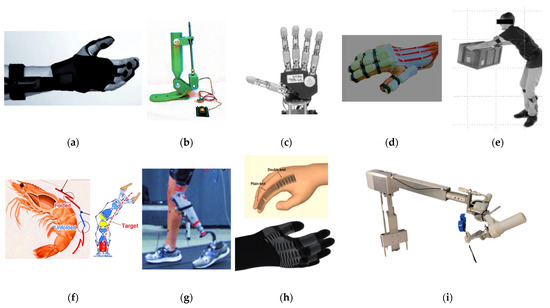
Figure 3.
ADs from academia and lab studies. (a) SEM glove [57]; (b) Two DOF ankle prosthesis [59]; (c) robotic hand [61]; (d) 3D-printed rehabilitation glove [63]; (e) SPEXOR monitoring system [65]; (f) multi-stable origami exoskeleton [67]; (g) power knee and control system [69]; (h) knitted SMA actuator rehabilitation glove [71]; (i) robotic arm with a Jamshidi needle for spinal surgery [73]. (Figures reproduced from external sources retain their original copyright.) Reuse permissions were granted under creative commons licenses (CC BY 4.0).) (https://creativecommons.org/licenses/by/4.0/ accessed on 20 April 2025).

Table 3.
Innovative prototypes and research stage ADs.
Table 3.
Innovative prototypes and research stage ADs.
| No. | Type of Device | Working Principle | Limitations | 3D Printing Material Potential and Application | SMs Potential | Potential Applications of 3D/4D Printing Technologies | Advantages Over Conventional Materials |
|---|---|---|---|---|---|---|---|
| 1 | SEM Glove [57] works as a hand rehab device for stroke patients | Soft actuators for finger motion | Limited grip force, no tactile feedback | TPU/Elastomers | Shape memory polymers | Self-stiffening finger joints for variable resistance | Patient required design and size, adaptive grips |
| 2 | Exo Boot [58] is ankle rehab device | Portable assistance | Bulky, short battery life | Carbon fiber composites | Piezoelectric polymers | Energy-harvesting sole foams | Adjustable strap systems, Solar powered gait adaptation |
| 3 | Powered elbow exo skeleton [60] works for arm rehab for SCI disabilities | Torque-controlled spasticity management | Rigid joints restrict motion | Titanium alloys | Liquid crystal elastomers | Stiffness adjusting cuffs based on EMG signals | Torque personalization, neural interface integration |
| 4 | Flexo tendon glove [62] gives hand rehab | Fluidic tendons for adaptive grip | Slow response, leakage risks | Flexible photopolymers | Self-healing hydrogels | Microfluidic channels with leak proof coatings | Predefined grip modes, closed loop pressure control |
| 5 | SPEXOR [64] spinal exoskeleton provides spinal support | Passive lower back load reduction | No active assistance | Nylon 12 | Auxetic metamaterials | Lattice structures for dynamic spinal alignment | Sizing only |
| 6 | Bionic spine [66] helps in full-body mobility | Neural implant for exoskeleton control | Invasive surgery | Biocompatible resins | Conductive 4D hydrogels | Self-expanding electrode arrays | Surgical precision |
| 7 | Power knee [68,74,75] provides knee rehab | Energy recycling exosuit | Heavy, noisy | PETG/PLA composites | Electroactive polymers | Energy harvesting knee hinges | Gait pattern tuning, Silent piezoelectric actuation |
| 8 | Smart braces [70,76] provides knee and ankle support | SMA dynamic bracing | Slow response | NiTi alloys | Thermo-responsive polymers | Terrain-responsive stiffness modulation | Joint specific tuning, predicted stiffness adjustment |
| 9 | Spine surgery assists robotic system for works [72,77] | Robotic scoliosis correction | Restricted mobility | PEEK polymers | Growth adaptive scaffolds | Expandable braces for child development | Curve specific correction, pediatric growth accommodation |
As discussed in Section 1, this review first establishes the global statistics on disability and the urgent need for assistive technologies (ATs), followed by an assessment of the limitations of traditional devices. It then examines commercially established smart devices and subsequently highlights recent laboratory breakthroughs, each addressed in separate sections to provide clarity on material usage, technological adoption, and functional capabilities. By structuring the discussion in this way, the study not only compares devices across different stages of maturity but also emphasizes how materials, design innovations, and policy frameworks interact to shape accessibility. Unlike previous reviews, which often focus narrowly on sensor actuator integration, material combinations, and isolated performance parameters, this work presents a comprehensive synthesis that bridges global policy perspectives, affordability, and patient centered design with technical advancements. In doing so, it provides a holistic roadmap for how innovations in advanced materials and additive technologies can be aligned with policy and accessibility goals, paving the way for more inclusive and scalable AT solutions. As a result, this review performs a critical comparative analysis that explicitly connects material properties and manufacturing techniques to functional outcomes, accessibility, and scalability. We identify and analyze a crucial paradigm shift: the move away from rigid, centralized manufacturing towards AI-driven, decentralized, and on demand production models (e.g., 3D/4D printing in hospitals) as the key to overcoming the systemic barriers of cost, customization, and equitable access detailed in Section 1.1 and Section 1.2. By evaluating both commercial devices (Section 1.3) and academic breakthroughs (Section 1.4) against this same framework, this review reveals previously unrecognized trends and critical gaps, most notably the disconnect between high performance laboratory innovations and the requirements for sustainable, policy aligned, and globally scalable commercialization. Ultimately, this work provides a unique roadmap for guiding future research, development, and policy toward creating clinically viable and universally accessible adaptive assistive technologies.
2. Methodology
2.1. Research Questions
The PICO framework has been used to explore the role of emerging technologies, such as materials adaptive behavior properties, sensors, actuators, and 3D and 4D printing, in the design and performance of ADs. In this phase, population (P) represents users of ADs, exposure and intervention (I) are the current available ADs, the comparison (C) are the alternatives, such as smart materials, 3D/4D printing, sensors, and actuators (C), whereas outcome (O) represents improved customization, performance, cost efficiency, adaptability, biomechanical alignment, and accessibility to all kinds of people. Depending on this framework, we have developed the following research questions for our systematic review.
- How can 3D and 4D printing technologies improve the traditional ADs by considering customization, cost, adaptability factors, and performance for mobility assistance such as walking, standing, and grasping? And how will these technologies be able to fully replace conventional devices in the healthcare industry?
- How can smart sensors (SSs) be integrated into ADs with a focus on recent research prototypes and commercial applications? How do different types of actuators increase smart functionality and self-regulated motion in ATs to ensure smooth and efficient mobility support?
- How do different 3D printing technologies used for producing ADs affect their quality and performance? How is decentralized additive manufacturing of ADs in hospitals possible, patient acceptance, and overall productivity in digital healthcare systems improved?
- What kind of smart materials are essential for mobility aids and prosthetics? Are there any successful applications of smart materials in mobility aids with improved adaptability and biomechanical performance?
- In what ways can actuators, sensors, and 3D/4D printing be harnessed to design adaptive and affordable ADs aligned with individual biomechanics?
- What are the primary technical, economic, and regulatory barriers that exist for establishing 3D and 4D printing technologies in healthcare facilities? Smart material (SM) reliability, lab scale success vs. scalability, performance metrics of ADs, small decentralized economic production, availability in rural regions, and FDA/CE approvals are key factors to be followed.
- How effective are commercially available smart ADs, such as prosthetic and orthotic devices, in achieving improved gait, posture, and quality of life, and how can emerging technologies push these outcomes further?
- Which design strategies and engineering models best support the co-optimization of mechanical and biomechanical performance in ATs, integrating 3D/4D printing, sensors, and actuators, through collaborative, multidisciplinary approaches and data sharing?
2.2. Development of Research Objectives and Methodology for Research Studies Analysis
The research questions outlined above aim to clearly define our objectives in exploring recent advancements in ATs. They emphasize evolution beyond traditional ADs by focusing on enhanced customization, cost-effectiveness, adaptability, and biomechanical performance. We also want to evaluate the performance of laboratory scale innovations and their potential for full scale adoption in the healthcare industry. Figure 4 illustrates an overview of the methodology adopted during the systematic review process to facilitate a clearer, unbiased understanding of our study and ensure its accuracy. This will result in comprehensive research, enabling healthcare professionals, engineers, and industrialists to make decisions based on reliable information. To implement a medical device, specific protocols must be met. Additionally, we require research evidence, clinical proficiency, and patient preferences, which is why evidence based and experimentally verified digital health devices are our focus. We will discuss advanced ADs produced in research hospitals, commercially available and laboratory success comparisons, with a focus on ATs that are easily implemented, customer-satisfied devices, and their components, such as sensors, adaptable materials, actuators, and advancements in 3D/4D printing in recent years.
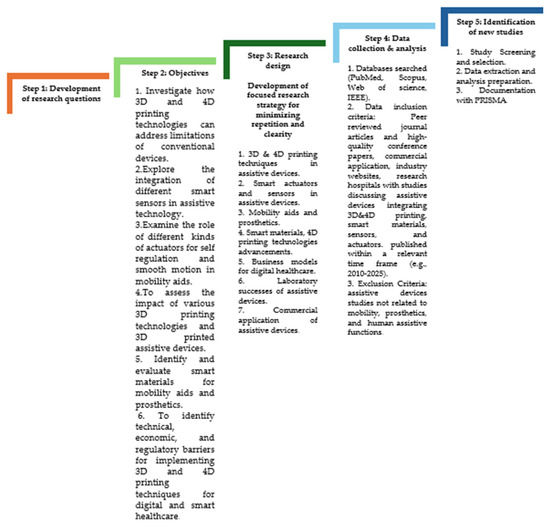
Figure 4.
Steps for the methodology adopted for review.
2.3. Inclusion/Exclusion Criteria of Research Studies and Reports
This review was built on a foundation of primary research evidence. To ensure our findings were comprehensive and robust, we used a multifaceted strategy for collecting data: Core Evidence (Primary Research): The main body of our analysis is based on 130 primary research articles. These provided the original data that we synthesized to draw our conclusions. Supporting Context (Review Articles): We consulted 33 existing review articles, but only to help shape our research question and provide background context in the introduction and discussion. Their data was not included in our final analysis to avoid simply repeating previous summaries. Mitigating Bias (Grey Literature): To capture valuable data that is not always published in academic journals, we included 53 pieces of “grey literature,” such as technical reports from universities and documents from agencies like the WHO and UNICEF. These sources were only used when they contained unique, unpublished information (e.g., specific performance metrics, internal program data, or policy guidelines) relevant to our research question. In these cases, they were treated as primary evidence. This approach, recommended by the Cochrane Handbook, helps minimize publication bias and ensures a more complete picture of the available evidence.
2.4. PRISMA Flow Chart
Figure 5 reports the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart, which represents the screening process of this study. To make this process transparent, a mapped research approach in the form of a flowchart has been implemented. It consists of steps that represent how many studies were processed, identified at the start, then screened for the final analysis, along with reasons for inclusion and exclusion. Grey literature, including technical reports, theses, and institutional documents, was considered when it provided original data relevant to our research question. While excluded from the final evidence synthesis, these sources helped to shape the research framework, identify gaps, and ensure a comprehensive overview of the field.
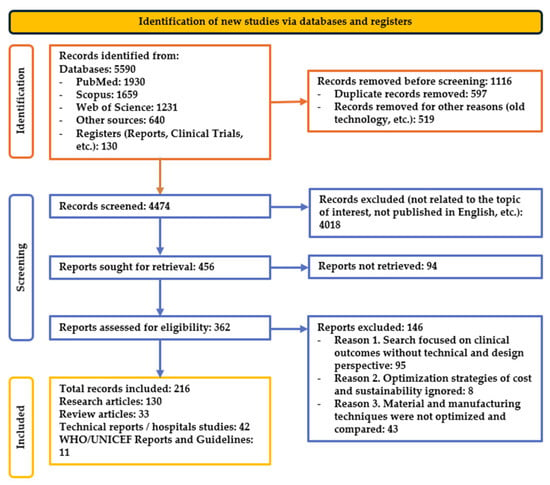
Figure 5.
PRISMA flow chart.
3. Functional Components in ADs: Recent Advancements
3.1. Actuators in ADs
Actuators help components in ADs to move, control, and interact by converting an input, depending on application type, such as electrical energy, hydraulic energy, and pneumatic energy, into an output, which is mechanical energy. In ADs, actuators assist human motion, thereby improving independence and performance in daily life activities, including prosthetics, orthotics, mobility aids, and rehabilitation robotics. Powered prosthetic limbs, motorized wheelchairs, and robotic exoskeletons work with the help of electrical actuators, named as electrical motors, DC motors, and servo motors. Another essential type of actuator for high force output in heavy-duty exoskeletons and advanced prosthetic knees is hydraulic actuators; as their name suggests, they use hydraulic fluid pressure to create strong but smooth movements. However, most of the time, they require pumps and reservoirs, which typically consist of large bulk quantities of actuators. Pneumatic actuators are lighter than hydraulic actuators because they use compressed air, which is commonly found in wearable ADs for flexible motion. The force output of McKibben pneumatic artificial muscles is analyzed to achieve efficient muscle design by a detailed comparison of design parameters. Finite element simulation and artificial neural network techniques were used to verify real test data [78]. There have been examples of actuators being developed using SMs in clinical studies. Most of the actuators have used SMAs and piezoelectric materials. SMAs can change shape in response to a heat stimulus within their designed working environment, making them adaptable and multifunctional. In contrast, piezoelectric materials produce small displacements in response to an electrical stimulus. These types of smart actuators generate the required actuation without needing any external power. Soft actuators represent another type of actuator that is commonly found in ADs that utilize soft materials, such as polymers. In order to achieve flexibility, strength, and speed, a novel bioinspired soft actuator design is experimentally validated, showing an excellent biomimetic design, paving the way for future applications in soft robotic limbs [79]. Soft actuators have four further types: pneumatic, hydraulic, tendon-driven, and dielectric elastomer systems that help patients with mobility assistance and also in later stages of rehabilitation [80]. In addition to these, there are some other emerging actuator technologies as well, like ionic polymer metal composites [81], bend easily when a small amount of electricity is applied because ions move inside them, offering advantages like biocompatibility and silent operation, but have some drawbacks like low force output, slow response, and environmental sensitivity. Twisted and coiled polymer actuators [82], usually made from nylon and polyethylene fibers, change shape in response to heat, their contracting ability is fast when exposed to heat; providing high stroke and low cost, but complex thermal management is one of the key problems in these devices. Liquid crystal elastomers (LCEs) [83] are one of the most advanced and efficient actuators, having reversible significant shape changes directly in response to changes in heat and light, making them highly sensitive and with impressive theoretical work density, but complex fabrication and significant control challenges are limiting these to research laboratories. The overall comparison of these actuators explains that actuators in soft hand exoskeletons have improved the range of motion for patients. Adaptive ankle-foot orthoses have reduced walking effort by 12% for patients with cerebral palsy. As this is the next generation phase of ADs, energy inefficiency, control delays, material durability, and cost are key challenges for advanced actuators. Actuators are the backbone of ADs; therefore, for next-generation ADs, there is a need to transform them from passive devices to smart, interactive ones. In Table 4 below is reported a brief comparison of some advanced actuators in ADs.

Table 4.
Advanced actuators in ADs.
Figure 6a illustrates the bi-directional soft pneumatic actuator [87], produced using 3D-printed molds and silicone rubber, reinforced with polyethylene rings, lightweight, and sized to match human fingers. Integrated with sensors and control, it enables safe, controllable, and bidirectional motion for assistive hand robotics. Figure 6b presents a series elastic tendon actuator (SETA) [88], where linear springs and wire actuation provide smooth, controlled knee assistance in an exosuit. This elastic tendon actuator generates torque through front and rear wires during knee flexion, also measuring forces with wire tension. Compliance is introduced through linear springs, allowing slight joint movement, and a single motor drives both wires with two series elastic components sliding along linear shafts. Each SEC, preloaded to 50% of maximum deformation with four compression springs, transmits motor power from the input to the front or rear wires. Figure 6c presents shape memory alloy spring-shaped, muscle-like actuators [89] that contract when heated electrically, providing actuation without bulky motors. In Figure 6c, actuators are placed strategically around the wrist; contraction of actuators on the palm side (4, 5) produces flexion, while those on the dorsal side (1, 2, 3) cause extension. Similarly, actuators near the little finger side (1, 4) generate ulnar deviation, and those near the thumb side (3, 5) induce radial deviation. By selectively activating combinations of these actuators, the device enables not only single-axis movements but also complex wrist motions.
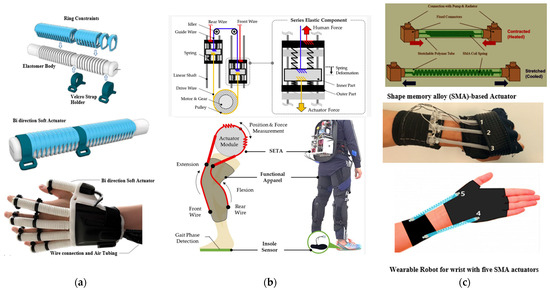
Figure 6.
Actuators in ADs. (a) Bi-directional pneumatic soft actuator in wearable soft robotic hand [87]; (b) series elastic tendon actuator (SETA) in knee exosuit actuator using linear springs and encoder feedback for compliant, adaptive stair climbing assistance [88]; (c) SMA coil actuator with coil shaped SMA for high contraction and force in soft wrist assistive device [89].
While actuators independently serve as the backbone of advanced ADs, their true potential emerges when integrated with sensors and produced using sustainable advanced fabrication technologies. For example, actuators alone can enable motion, but when coupled with sensor feedback, for example, using EMG, pressure, and motion sensors, they allow for adaptive control in prosthetics and exoskeletons. Furthermore, 3D printing technologies enable the customization and lightweight design of actuator housings and transmission systems, ensuring improved comfort and usability for patients. Emerging smart actuators based on shape memory alloys (SMA), dielectric elastomers, and liquid crystal elastomers can be directly integrated with sensor arrays, resulting in self-regulating, adaptive ADs. This integration represents the shift from passive mechanical components to smart, interactive systems that dynamically respond to user needs and environmental contexts. This concept promotes some components of actuators to be printed with conventional 3D-printed materials and then some with smart materials for a combination of active and passive motion. In order to explain this concept in detail, some advanced sensors and manufacturing techniques are explained in further sections.
3.2. Sensors in ADs
Sensors typically operate by detecting changes in their environment and converting them into readable values [90]. Sensors detect physical changes and convert them into analog and digital outputs, which can be displayed, monitored, and processed by other devices, depending on the application. Sensors provide a link between the physical parameters, as input values, and the logical parameters, as output values [91]. It works for IoT [92] by collecting, analyzing, and processing environmental data, then providing efficient monitoring, management, and control with the help of other devices. So, almost every assistive device consists of transducers that convert the signal from input to output, and then we have actuators that use these outputs as their input to perform required tasks, such as motion or force transfer. In ADs, sensors are used for different applications; even 3D printing technology has been used to produce smart sensors as well [93]. There are various types of sensor classification, classified by power requirement as active sensors that require external power for operation. In contrast, passive sensors work without external power. Another type of sensor depends on how they detect changes in the environment, meaning their detection principle, such as chemical, electrical, and radioactive methods for measuring environmental changes. Sensors are also classified on the working principle of conversions, meaning how they convert input into output, with massive applications in ADs, for example, converting heat to voltage in thermoelectric sensors. However, the last classification type encompasses both analog and digital sensors, depending on the type of output required from them. ADs used in neurological, musculoskeletal, cardiopulmonary, and pediatric rehabilitation are using accelerometers, gyroscopes, and magnetometers as sensors. All three types are inertial measurement units, strain sensors, and pressure sensors, such as those found in the insoles of ADs, on mats, in wearable devices and exoskeletons [94], and electromyography sensors for intramuscular devices. Electrocardiography (ECG), electrodermal activity, photoplethysmography, temperature sensors, and respiration sensors are utilized in the field of physiology, alongside haptic, auditory, and visual modalities, which operate on the principle of biofeedback [95]. Also during grasping action [96], a Bayesian sensor fusion algorithm was used to analyze the data from each sensor independently. Four surface EMG sensors (Figure 7a) were utilized to measure muscular signals during sequential grasping actions, resulting in a more reliable and easier-to-maintain design, providing a flexible design while still providing intent detection precision and reduced maintenance requirements. In electronic travel aids, sensors such as cameras, sonar, and laser scanners [97,98] have been utilized. In order to measure the force applied and to detect the user’s intention to stand, researcher [99] involves initial feasibility testing of sit-to-stand devices that utilize pressure sensors, thereby promoting adaptive assistance. This resulted in the sensor-integrated device being feasible, offering promising usability and providing potential benefits for safer and easier standing. An advanced wearable electronic patch [100] is also used, which adheres directly to the skin of the forearm and hand, and it is composed of an array of tiny sensors made from laser-induced graphene (Figure 7b). When patients move their fingers and hands, sensors will detect sensitive muscle movements and skin deformations (myography). To track the complex poses and gestures of the entire hand and forearm, data is recorded and then processed. There is another advanced camera, the Intel RealSense D400f depth camera [101], that can be used for advanced detection techniques. It consists of an IR pass filter that blocks visible light and captures only infrared. It will increase depth sensitivity in challenging environments, such as obstacle detection and navigation for smart wheelchairs in bright outdoor settings. This promotes contactless gesture control for mobility limited users, visually impaired navigation systems for spatial mapping, and home lighting that prevents patients from falling. To achieve comfortable and real time wearable gait monitoring, a novel, flexible microchannel pressure sensor (Figure 7c) has been designed from a soft elastomer containing a microchannel filled with liquid metal Galinstan [102]. This sensor features a flexible electrode that changes capacitance when a footstep deforms the microchannel, resulting in highly sensitive and stable pressure values. These advanced sensors can work very efficiently in rehabilitation and other mobility ADs due to their excellent step timing, pressure patterns, and center of pressure trajectory compared to piezoresistive alternatives and other rigid sensors.
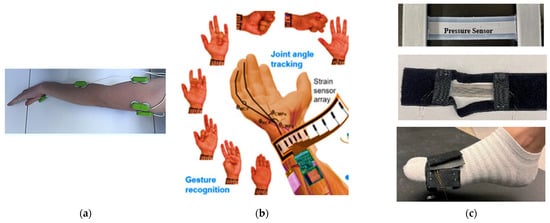
Figure 7.
Sensors in ADs. (a) EMG sensors (green boxes) on participants arms [96]; (b) laser-induced graphene sensors for sensitive hand movements and gesture detection [100]; (c) microchannel pressure sensor application in a gait monitoring system [102].
The functionality of sensors in ADs is amplified when integrated with smart actuators and sustainable advanced fabrication methods. Sensors provide the critical feedback loop by monitoring biomechanical signals, physiological parameters, and environmental changes, which actuators then convert into precise motion and assistance. For instance, pressure sensors in gait-monitoring devices can guide actuators in exoskeletons to adjust step assistance in real time. Similarly, 3D printing allows for embedding flexible, lightweight sensors directly into wearable devices, enhancing comfort and accuracy while minimizing bulk. When combined with smart materials, such as piezoelectric and graphene sensors, the integration fosters the development of ADs that are not only responsive but also predictive, enabling proactive rehabilitation and assistance tailored to individual users.
3.3. D-Printed ADs
3D printing technology is revolutionizing ATs by enabling highly customizable, affordable, and functional replacements for the human body [25]. Three-dimensional printing produces digital scanning and modeling, ensuring a comfortable fit with 3D-printed sensors [93], user-specified components, and actuators [32,103]. It utilizes lightweight, durable materials and rapid prototyping, enabling quick adjustments and iterative improvements [104], hence increasing enhanced mobility and responsiveness. In [105], a case report is studied using a comparative approach to examine a 3D-printed transradial prosthesis (Figure 8a) compared to a standard one. The wrist–hand orthoses (Figure 8b) and lattice geometries were fabricated using material extrusion technology equipped with a direct drive extruder suitable for soft materials, which are melted and extruded through a nozzle to create custom lattice geometries and orthoses layer by layer [106]. There is also research that revolutionizes the production of lower limb prostheses by using 3D printing combined with digital design and structural optimization. In this study a single monocoque device (Figure 8c) is printed using fused filament fabrication, with careful selection of materials for prototyping and load bearing applications, enabling rapid iteration and patient-specific customization. Ultimately, the study provides a practical roadmap for making prosthetic devices accessible to underserved populations, reducing both economic and geographic barriers while maintaining quality, comfort, and functionality [107]. The standard device performed better functionally, offering strength, durability, and fine control. In contrast, the 3D-printed prosthesis offered significantly higher patient satisfaction due to its comfort, lighter weight, and customizable appearance. Also, a brief comparison of 3D-printed technologies is presented, highlighting applications and potential in ADs.
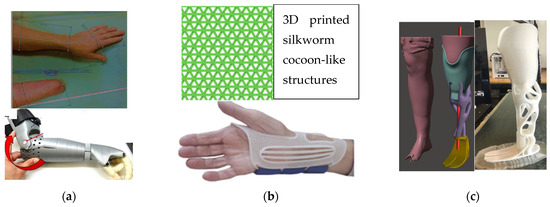
Figure 8.
Three-dimensional printed ADs. (a) 3D-printed arm prosthesis produced using photogrammetry [105]; (b) 3D-printed orthosis [106]; (c) 3D-printed monocoque design transtibial prosthesis (unibody structure instead of multiple parts) [107].
3.3.1. Fused Deposition Modeling (FDM)
It is a widely used additive manufacturing technique in which a heated nozzle fabricates 3D ADs by extruding thermoplastic filaments, depositing material layer by layer. FDM techniques have significant importance in ADs and prosthetics [108], where customization, lightweight designs, and cost-effectiveness are paramount [109]. Examples include prosthetic sockets, ankle–foot orthoses, and exoskeletons, which feature variable patient-specific design [110] and sizing tailored with the help of 3D scanning and FDM’s design flexibility [111]. FDM also offers great transformative potential, achieving consistent quality demands, rigorous parameter control, and material innovation. Nozzle temperature, thickness, and interlayer bonding are critical processing parameters. Material selection, primarily composed of PLA, ABS, and TPU, among others, significantly influences mechanical performance, including warping, residual stresses, and poor interlayer adhesion [112]. However, there are several limitations, such as reduced strength along layer lines due to anisotropic behavior and surface roughness, necessitating postprocessing. AI-driven parameter optimization, as well as carbon fiber reinforced filaments, are future improvements that are needed to make ADs printed by FDM stronger and more durable.
3.3.2. Selective Laser Sintering and Melting (SLS and SLM)
It is a powder-based manufacturing method that produces ADs with complex geometries without support structures. It uses a laser to selectively polymerize powders, such as polyamide, polypropylene, and composites, layer by layer. Material properties, printing orientation, and inherent porosity resulting from incomplete sintering impact the mechanical performance of 3D-printed ADs [113]. SLS-printed ADs have better strength and surface finish compared to FDM, although they face challenges such as limited material options, high costs, and the need for parameter optimization [114]. Selective laser melting (SLM) and electron beam melting (EBM) were used to fabricate titanium frameworks for implant supported fixed prostheses [115].
Factors, such as laser power, thickness of layer, and speed, critically affect the mechanical behavior of 3D-printed ADs [116], while also assessing defects like incomplete sintering, which results in incomplete durability. To achieve robust additive manufacturing practices, there is a need for advanced material models, future advancements in polymer blends, powder recycling, process refinement, and simulation techniques to bridge the gap between SLS fabrication and functional performance.
3.3.3. Stereolithography and Digital Light Processing
SLA (stereolithography) and DLP (digital light processing) use UV and laser to cure liquid photopolymer resin layer by layer into a solid 3D-printed assistive device. DLP has been used to fabricate complex, customized structures for tissue engineering, prosthetics, and implants [117]. Eco-friendly materials reduce environmental impact by developing bio-based, recyclable, and biodegradable photopolymer resins, as well as innovations such as vitrimers and water-soluble supports, to minimize waste [118]. This technique has great potential for producing advanced assistive technology.
3.3.4. Material Jetting (MJ)
It is a high-precision additive manufacturing technology that deposits and cures droplets of photopolymers to create a 3D-printed assistive device [119]. It includes material diversity, including photopolymers, waxes, and emerging composites, with advantages such as exceptional resolution, multimaterial capabilities, and easy support removal [120]. Limitations, such as material brittleness, post-processing requirements, and high costs, are key points to consider for future applications of ADs printed with quality and strength [121]. Customized pediatric and prosthetic limb socket liners, anatomical fitting models, and other assistive devices have been produced by using material jetting techniques in research laboratories [119]. Improved printhead precision and novel material formulations are state-of-the-art advancements needed to make this technology sustainable in biomedical applications.
3.3.5. Laser Powder Bed Fusion (LPBF)
LPBF builds parts, layer by layer, from metal powder to produce complex ADs. This technique offers excellent design flexibility with minimal waste and the ability to produce strong prosthetic sockets and hand frameworks, wheelchair components, and cranial implants [122]. LPBF is ideal for customized, low-volume, and highly complex prosthetics and mobility aids, with hybrid approaches emerging to combine their strengths. Factors such as material, design complexity, production volume, and post-processing requirements need to be discussed and addressed [123]. There is research [123] that discusses LPBF and electron beam melting (EBM) [124]; these techniques are being used to create bone replacements. LPBF provides precise and smoother surfaces, while EBM results in parts with reduced internal stress and the ability to handle more challenging metals, such as titanium. In Table 5 below is reported a global impact of 3D printing in academic hospitals.

Table 5.
Global impact of 3D printing in academic hospitals.
3D printing technologies extend beyond structural customization to serve as a platform for integrating actuators and sensors within a single device. For example, prosthetic sockets produced through 3D printing can be directly integrated with flexible pressure sensors, while actuator housings and transmission components can be printed simultaneously using lightweight and durable polymers. This approach reduces assembly complexity and cost accommodates users’ aesthetic preferences, since many wear these devices on a daily basis, hence improving overall reliability. Furthermore, 3D printing supports iterative prototyping of sensor actuator combinations, enabling rapid personalization for users. The future of ADs lies in merging these printed structures with smart materials that inherently provide sensing and actuation, creating multifunctional devices that are lightweight, affordable, and patient-specific. Thus, 3D printing acts as the convergence hub for bringing actuators, sensors, and smart materials together into integrated, intelligent AD systems. Thus, 3D printing serves as a convergence hub for integrating actuators, sensors, and smart materials into cohesive and intelligent assistive device systems. Beyond the technical advantages, the adoption of this approach also calls for supportive policy frameworks that enable in-hospital production, streamline regulatory approval, and ensure patient safety. At the same time, advances in smart materials such as self-healing polymers and biocompatible composites can further enhance device performance, durability, and user comfort, highlighting the need for coordinated efforts between engineering innovation and healthcare policy.
3.3.6. Challenges
One of the primary challenges in developing and implementing new devices is navigating complex regulatory frameworks, which can delay approval and market entry. Additionally, ensuring high manufacturing quality and minimizing defects remain critical hurdles, particularly when scaling up production from laboratory prototypes to commercial products. Moreover, the long-term success of these innovations depends on establishing sustainable and economically viable business models [132] that support widespread adoption while addressing environmental and societal impacts.
Agencies like the FDA and the European Medicines Agency (EMA) are the primary regulatory bodies overseeing medical products, innovations, new devices, and testing protocols, including 3D-printed medical devices and pharmaceuticals [133]. Advancing medical innovations while balancing patient safety is a critical factor; however, delays in approval methods and standards can impact the global adoption of 3D-printed medical solutions. A study [134] discusses the FDA’s guidance, which classifies 3D-printed medical devices by risk and requires process validation and good manufacturing practices even in research hospital laboratories [135]. According to the available literature and regulatory bodies, a lack of clear pathways and old strategies are the key challenges for new device approvals.
The requirements, such as time-intensive biocompatibility testing and dependency on historically safe materials, necessitate the use of limited, available FDA-approved polymers with less flexible material properties, including durability, sterilization compatibility, high development costs, degradation, and biocompatibility issues. Additionally, there are limited approved data available for specialized fields, such as heart valves and bone grafts. These barriers hinder innovation and favor well-established polymers, despite their potential limitations.
Layer by layer manufacturing processes, such as FDM and SLA, create steplike rough structures that can disturb the surrounding tissues. These rough surfaces affect mechanical performance by creating stress concentrations. Processes such as chemical vapor smoothing, mechanical polishing, and plasma treatment serve as post-processing techniques to ensure smooth surfaces for devices like prosthetics [136,137].
If the removal of support material is not performed carefully, it can introduce sharp protrusions that damage tissue and internal arteries [138]. Manual trimming, ultrasonic cleaning, and solvent baths are finishing techniques. There is a common challenge in printing techniques that are using resin printed devices contain toxic uncured monomers and metal particles from the nozzles, which can lead to inflammation and cytotoxicity. Heat treatments and washing in isopropanol are required to eliminate harmful residues [139].
Weak interlayer bonding results in weak anisotropic strength, consequently unsuitable for loading applications, such as orthopedic implants [140]. Annealing, epoxy infiltration, and hydrothermal aging are techniques required to post-process these defects after printing. Degradation of polymers under standard sterilization methods is also a significant issue for 3D-printed devices used in the human body. Autoclaving and gamma irradiation result in warping of thermoplastics and embrittling of materials. To address these issues, methods include using sterilization resistant polymers (e.g., PEEK), applying ethylene oxide gas for heat-sensitive devices, and adding surface coatings to seal and protect the material.
Devices like cranial plates and dental aligners sometimes have poor fit and functional failure, which are mostly due to shrinkage, warping, and swelling during printing [141]. Hydrostatic pressurization for reshaping warped parts, precision machining, and design software compensation improve the dimensional and size fit errors for customized devices. Most biomedical devices require bioactive properties for tissue integration; however, materials like PLA and ABS are inert and lack these properties [142,143]. To introduce bioactivity, coating a 3D-printed device with materials like hydroxyapatite, which promotes bone growth, immersing devices in collagen solutions, and plasma treatment have been used as finishing techniques. There are two types of porosity expected in 3D-printed ADs: porosity resulting from printing defects and intentional porosity, such as in scaffolds. For refining pore size and shape, chemical etching is performed, along with surface modifications such as RGD peptide coatings and infiltration with biocompatible sealants, which will provide mechanical strength and biological performance [144].
Aesthetic defects, such as visible layer lines, uneven color distribution, and textures, may be unacceptable for some patients, particularly in the case of prosthetics and wearable devices. Biocompatible painting, dyeing, and coating enhance aesthetics while maintaining functionality. Most of the time, patients need prosthetic limbs with smooth, skin-like finishes for psychological impact. Hence, post-processing techniques and finishing methods are indispensable for devices like ADs, as these devices are used daily by patients. Additionally, these techniques convert raw 3D ADs into safe, functional, and regulatory compliant medical devices, so post-processing remains a cornerstone of biomedical device fabrication and application.
Smart service models are revolutionizing healthcare by effectively integrating medical resources. Decentralization of any 3D-printed medical facility promotes flexibility, resulting in lower costs, easier access, and increased sustainability and competition from decentralized small manufacturing units. On-demand production, combined with a small investment, motivates healthcare departments to shift production technology from centralized factories to research teaching hospitals and laboratories, producing user-friendly, customized, and perfectly sized ADs. To streamline workflows, we need collaborative ecosystems that include hospitals, engineers, material experts, and policy regulators, as well as effective digital platforms for sharing data and knowledge. Additionally, reduced costs and improved accessibility can be achieved through subscription models for digital innovation and updates, as well as outsourcing small mobile 3D printing units and on-demand manufacturing. Advanced materials like biocompatible polymers and bioinks improve functionality and economic efficiencies, also converting complex, expensive processes into sustainable processes economically, like the real-life example of Align Technology [145], which uses 3D printing to make custom-fit clear braces for teeth, and Stryker [146], which uses 3D printing to design as well as to test medical device.
Intellectual property disputes over open-source designs, standardization gaps in achieving effective decentralized production, and regulatory hurdles remain significant challenges. Sustainability, achieved by using recyclable materials, ensuring secure data sharing, and scaling bioprinting, is a future recommendation for a digital sustainable healthcare business. Complex innovations have been achieved by utilizing hybrid systems that combine robotics and nanotechnology, as exemplified by the case of drug-eluting stents. Collaborative policy frameworks, an ethical approach, training, and the satisfaction of healthcare professionals are necessary to realize the full potential behind [147].
3.4. Four-Dimensional Printing Technology in ADs
A significant amount of research and studies has been conducted to make 3D printing more sustainable and accessible, which is opening doors for strategies like interdisciplinary research, detailed approaches to studying new material properties like smart and adaptive properties, and process design, ultimately leading to the evolution of 4D printing. Four-dimensional printing is an additive manufacturing process where products like ADs dynamically transform over time, concerning the fourth dimension, in response to stimuli, types of stimuli depending on the type of materials and applications, such as temperature, position, moisture, and light. Hence, 4D printing revolves around stimuli-responsive materials, also known as smart materials (SMs), such as thermal activation, pH changes, humidity, and light driven actuation, as well as composite systems that enable multi-responsive behavior for unique applications.
Four-dimensional printing produces self-adjusting and self-assembling structures and smart structures, making 4D-printed ADs the most advanced next-generation medical devices. However, there are numerous challenges, as with every new technology, such as scalability, biocompatibility, precise spatiotemporal control, and material durability. Multi-responsive materials, computational modeling, integration for intelligent systems, and interdisciplinary innovation are key factors to consider for future advancements in 4D printing [148]. Applications such as adaptive tissue engineered scaffolds, drug delivery systems triggered by physiological conditions, self-adjusting implants, and invasive surgical tools are key examples of the transformative potential of 4D printing for ADs [149]. The combination of electroactive polymers and ionic polymers, along with advanced 3D printing methods, produces structures with smart properties that can change their shape and then adapt their functions in response to electrical signals. These materials can allow programmable, voltage-driven movement, such as bending, twisting, and expanding, which can be tailored for various applications, including the manipulation of delicate objects in soft robotic grippers, stents that adjust to human body conditions, and airplane wings that morph mid-flight [150]. Biomimetic materials, such as those that mimic collagen and bone, are being used in training hospitals and research institutions [151]. These materials include hydrogels, which are water responsive, shape memory polymers, which are temperature responsive; and stimuli responsive ceramics. Stents produced with SMs can expand and contract in response to vascular conditions and release drugs to prevent restenosis, whereas as traditional stents are static scaffolds. Implants that release therapeutics in response to biomarkers work as glucose-sensitive insulin drug delivery systems, and adaptive pacemakers and neural interfaces that adjust to physiological signals work as neurological and cardiac devices are some recent examples of 4D printing applications across medical sectors.
3.5. Smart Materials (SMs)
SMs are advanced forms of engineered materials that can perform multiple tasks by responding intelligently to stimuli available in their working environment. These kinds of materials sense specific external signals, such as temperature, pressure, and light, and can actuate themselves to perform defined tasks. Distinguished by transiency, immediacy, self-actuation intelligence, selectivity, and directness, they respond and act inherently in place. They have two main types, depending on their functions. The first one transfers energy as a passive type, like fiber optics. Active types of SMs, which can be further categorized into two types depending on their functions, changing properties functions (such as SMAs) and converting energy functions, like solar cells, both exhibit reversibility and can intelligently sense and respond to their environment. Smart materials transform energy from specific environmental stimuli into functional responses. SMAs convert thermal and mechanical energy into shape changes. Materials that convert electrical energy to mechanical strain are piezoelectric in behavior. Magnetostrictive materials convert magnetic field energy into mechanical strain, while chromic materials convert energy from various stimuli (light, heat, etc.) into color changes. Electrorheological fluids convert electrical field energy into changes in viscosity, and magnetorheological fluids convert magnetic field energy into changes in viscosity. Recent applications of smart materials (Figure 9) in AT will be discussed comparatively with conventional materials.
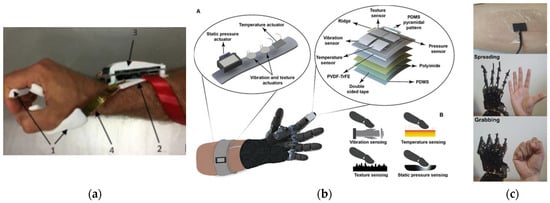
Figure 9.
Examples of smart material applications in ADs. (a) Shape memory alloy in ADS, personalized anti-spastic orthosis, combining 3D-printed polyamide and TPU passive parts with active Nitinol SMA actuators, consists of a passive framework including the finger section (1) and the forearm section (2), a control unit (3), and an active component made of SMA actuators (4) [152]; (b) (A) E-skin system (whole picture), (B) Two sensor pixels (zoomed-in view)Piezoelectric materials in ADs, a flexible, multiplexed piezoelectric-capacitive electronic skin (e-skin) for upper limb prostheses that detects pressure, temperature, vibration, and texture. To replicate human skin’s vibration sensitivity (40–400 Hz), a piezoelectric-based vibration sensor using PVDF-TrFE in a parallel plate configuration was designed [153]; (c) self-healing polymer in ADs, A conductive composite electrode is created by combining a self-healing polymer (SHP) with graphene. This material can repair itself automatically and quickly regain electrical function even after being damaged repeatedly, this electrode is attached to the skin, and a demonstration of a human robot interface with stretchable and self-healable electrodes for grasping and spreading is measured and tested [154].
3.5.1. Shape Memory Alloys (SMAs) in ADs
SMAs retain their shape and exhibit two distinct basic phases and can switch or transition between these phases in response to external changes. The austenite phase is a form of SMAs in which it remembers its original shape. If, by any application in a working environment, they are deformed, they can transition to their original stable state when exposed to other stimuli. This change occurs due to the shape memory transformation property of the material. There is a study that uses a lightweight wearable exo-glove for hand tele-rehabilitation using NiTi shape memory alloy (SMA) actuators to control all five fingers, resulting in compact, efficient, and remotely controllable solutions for improving hand rehabilitation outcomes. In Table 6 there are some recent applications of SMAs in ADs with future potential and comparison.

Table 6.
SMAs’ application and comparison with conventional materials in ADs.
3.5.2. Piezoelectric Material in ADs
Piezoelectric materials are smart materials that generate an electric field when subjected to mechanical strain [93]. Due to their smart properties, these materials [162] have applications in biosensors [163], actuators, ultrasound transducers, energy harvesters, and implantable devices. As a result, these materials provide diagnostics, monitoring, and self-powered systems [94] that are biocompatible, flexible, and functional in next-generation medical applications. Table 7 shows several examples of piezoelectric materials and their applications in sustainable digital healthcare systems.

Table 7.
Piezoelectric materials application and comparison with conventional materials in ADs.
3.5.3. Self-Healing Polymers (SHP) in ADs
Biological tissues in the human body have the natural ability to heal with time, as in the case of a wound on the human body, which heals with time. So, a lot of materials have been developed by inspiring this biological property of human skin and tissue. Self-healing materials are materials that automatically repair structural damage by using physical, chemical, and biological mechanisms, thereby maintaining structural properties, hence increasing the lifespan and restoring structural functionality. In order to have sustainable and durable polymers [187], reversible coordination bonds have been used to increase mechanical properties and dynamic repair properties. Also, high performance polymers have been created using materials like polyurethanes, polyacrylates, and epoxy resins. As a result, supramolecular polymers have been produced for reversible interactions using methods like metal ligand coordination and hydrogen bonding. To have increased healing and high strength, hybrid materials have been engineered using covalent and non-covalent bond methods, having durability, flexibility, and automatic repair properties [188,189].
3.5.4. Smart Materials Integration in ADs
Smart materials application is pivotal for advancing multifunctional and durable ADs. SMAs, such as NiTi, are primarily employed as compact, high strength actuators that respond to thermal stimuli, exemplified by their use in wearable exo-gloves for hand tele-rehabilitation, where they provide the actuation force for finger movement. In contrast, piezoelectric materials serve a dual purpose, functioning both as self-powered sensors that convert mechanical strain from body movement into electrical signals for biosensing and monitoring and as precise micro actuators in systems like ultrasound transducers. Concurrently, SHPs are engineered not as active elements but as robust structural matrices often incorporating polyurethanes and supramolecular networks that utilize reversible covalent and non-covalent bonds to autonomously repair mechanical damage, thereby significantly enhancing the durability, safety, and lifespan of 3D-printed wearable devices. As a result, we have more adaptive, resilient, and functionally integrated ADs.
Table 8 mentioned below represents SHP comparison with conventional materials applications.

Table 8.
SHP materials application and comparison with conventional materials in ADs.
3.6. Potential vs. Reality of 4D Printing Techniques in ADs
Four-dimensional printing produces next-generation smart ADs that are personalized to fit and adapt to patients’ customized needs. In the absence of industrial standards, material incompatibilities pose a significant scalability barrier for larger-scale and unoptimized stimulus response control mechanisms, particularly in smart materials (see Table 8) and 4D-printed mobility aids. MIT [199] research laboratories produce innovations in self-assembly and programmable materials, creating systems that autonomously adapt and transform. For example, shape shifting 4D knit dresses, liquid metal printing for rapid fabrication, active shoes with a customizable fit, and rock printing using granular jamming are notable lab successes. Still, they need a collaborative approach for scalable outcomes. A collaboration between MIT’s self-assembly lab [199], Stratasys [203], and Autodesk, produces multi-material 3D objects that respond to stimuli like water and heat, resulting in self transforming applications, for example, shape shifting objects like adaptive wearables, adaptive functionality, biomedical devices, and climate responsive textiles without electronics [172]. Mars Ice Home [204] is another example of an SM application of NASA’s adaptive space habitat concepts. Transformers for lunar extremes align with 4D printing principles to provide smart responses to environmental stimuli such as temperature and radiation, whereas current prototypes do not utilize 4D printing. SMs that harness Martian ice to self-thicken radiation shielding, apply modular lunar structures that fold under temperature shifts, and use self-healing polymers to repair micrometeorite damage. Merging 4D printing’s programmable material logic with NASA’s need for lightweight, self-sustaining systems will result in reduced dependency on mechanical components and promote habitats that can adapt to harsh space environments. In recent years, numerous ADs have been developed in research and teaching hospitals; however, 4D printing still struggles to create scalable industrial applications due to reasons such as material limitations, material degradation, patient and doctor acceptance rates, a lack of industrial standards, and scalability gaps. ADs with advanced 3D and 4D printing technologies (see Table 9), such as mobility aids, medical implants, and adaptive devices, face significant barriers. These barriers include sustainable design tools for modeling time-dependent material responses and traditional ABAQUS version 2022 software for predicting dynamic shape transformations [205]. Standardized protocols for stimulus responses, the challenge of safely handling light, and photo responsive materials implanted in the body are process control challenges [206]. In load bearing prosthetics, quality assurance compromises repeatability, resulting in inconsistent performance. The FDA and ISO standards require empirical data on fatigue and stimulus response consistency under real world conditions, like in hospitals and on patients. Therefore, for shape memory implants and adaptive orthotics to achieve precise temporal control and biocompatibility, the current lack of clinical translation and industrial adoption remains a significant barrier [207]. There are numerous devices with limited data on the durability of materials and devices, such as shape memory polymers, used in pediatric scoliosis braces. However, for certification, they require durability testing. Slow printing speeds can delay the mass production of customized ADs, such as ankle–foot orthoses, for patients with cerebral palsy [208,209].

Table 9.
Common 3D/4D materials FDA data.
4. Discussion: Future of ADs, Merging SMs with 3D and 4D Printing Techniques
4.1. Smart Synergies
We will discuss the next generation of ADs, which combines the positive impacts of 3D and 4D printing with smart materials for customization, adaptability, and multifunctionality. Three-dimensional printing produces customized designs, while 4D printing allows for dynamic behavior in response to stimulus changes. For example, 3D-printed lightweight sockets are designed for residual limbs, while 4D printing provides properties that adjust to temperature changes, promoting a better fit during activity. In commercial applications, such as in teaching hospitals and small industries, affordable 3D printing technology has been utilized to produce prosthetics, while 4D printing can better serve the users by developing adaptive ADs that respond to environmental stimuli. Adaptive knee braces with hydrogels and electroactive polymers automatically adjust in response to movement, while 4D-printed spinal braces also reshape as posture changes. Multi-material orthotics operate on the principle of alignment feedback with pressure stimulus effect, while commercial applications utilize lattice structures for enhanced breathability. In energy efficient exoskeleton actuators, dielectric elastomers and magnetorheological fluids provide lightweight actuation, while 4D-printed joints adapt to gait patterns. Increasing the lifespan of self-healing polymers and developing pressure points in thermochromic materials to prevent ulcers are among the future recommendations. To achieve mass production, industrial and digital healthcare are adopting human centered solutions by focusing on personalization, functionality, and accessibility.
4.2. Functional Limitations
Several technical barriers exist when integrating 3D and 4D multi-material combinations in prosthetics; numerous manufacturing complexities affect sensor sensitivity and reproducibility. Hence, there is a need for precise control to prevent delamination and ensure consistent layer resolution. Prosthetic upper limb sockets [210], using 3D-printed capacitive pressure sensors, have been developed; however, challenges remain in terms of biocompatibility, durability, and compatibility between conductive and dielectric inks and structural thermoplastics, which hinder successful mass production. To achieve optimal performance from sensors, it is essential to consider temperature, humidity, and other environmental factors, as well as signal noise and calibration challenges. Material fatigue and hysteresis, among other factors, affect mechanical stress and cyclic loading, which collectively contribute to reduced operational lifespan. Embedding power sources and coordinating software and hardware for pressure monitoring are some other challenges. Four-dimensional-printed scoliosis braces produced with shape memory polymers (SMPs) and rigid nylon face technical challenges due to thermal incompatibility. SMPs require heat for shape activation, but nylon’s higher glass transition temperature causes warping during thermal cycles [211]. Layer delamination due to uneven cooling rates between the two materials and weakened structural interfaces are challenges. However, thermal stress can be minimized by using gradient printing to radially transition materials, and carbon fiber layers stabilize a hybrid structure; these steps have reduced warping by 70%. Hence, these steps resulted in increased production complexity because material deposition requires precise control as well as accurate control of curing parameters. This thermal incompatibility in multi-material 4D printing highlights the need to carefully match material properties.
There is poor adhesion between the ink and the flexible polymer base in 3D-printed wearable knee braces [212] with embedded silver conductive ink circuits for strain sensing; hence, circuits detachment occurs when the braces are bent. Processes such as plasma surface treatment and aerosol jet printing have been adopted to address these issues; however, these processes increase the cost of additive manufacturing, which in turn results in less commercial acceptance. Weak structural challenges exist for a durable ankle orthotic due to thermoplastic polyurethane (TPU), as embedded microcapsules of healing agents reduce the tensile strength. For SM applications, balancing between smart responsive stimuli and mechanical strength is a future upgrade that needs to be addressed. As electrodes wore out quickly at high voltages of 2000–5000 V, when stretchy, metal electrodes were replaced with a hydrogel [213], electricity-powered materials (dielectric elastomer actuators) were added to exoskeleton joints. Hence, after cutting the voltage, this device becomes safer. As an output to this change, a 30% weaker exoskeleton would be produced so that it could not help with heavier patients and strong applications.
5. Challenges and Future Directions
5.1. Comparative Approach: 3D/4D Printing in ADs
Traditional ADs with static, rigid geometries and passive materials such as plastics and metals have limited functionality, adaptability, and customization. However, 3D-printed ADs resolve the issue of traditional ADs, but complex CAD modeling requirements, material waste, a passive response to the environment, and post-processing demands for multipart assemblies result in functionality challenges for 3D technologies in healthcare. Whereas 4D printing overcomes some of the limitations by integrating smart materials that change in response to the environment, making them adaptable for desired tasks, for example, controlled dynamic shape change, self-assembly, and self-healing in response to stimuli like heat, moisture, and light, so manual assembly would be removed, resulting in less design complexity, and also sustainability is increased in controlled use of material application. Advanced medical stents automatically change their geometry in response to tissue growth, and textiles that respond to temperature-controlled degradation and reconfiguration are examples of successful 4D-printed devices. So, 4D-printed ADs are adaptive, multifunctional, and sustainable, although retaining electroactive properties of materials like polymers, high voltage requirements for actuation, embedding conductive electrodes into ADs, optimizing computational modeling for predicting deformation, anisotropic material design approaches for controlled shape changes, maintaining performance even for all sizes of geometries, and long-term material degradation studies for fatigue electrical loads are current gaps, some of which have already been addressed in some devices, but others remain unsolved. By addressing these challenges, we can achieve a revolutionary step towards smart, responsive ADs, where structures autonomously interact with their environment.
Smart, optimized material responses, such as precise spatiotemporal control and material stability against unwanted stimuli, remain a mystery for researchers. However, scalable fabrication and biocompatibility can be achieved if manufacturing techniques and technical errors are reduced because these are the steps to establish standards; once these are completed, investment will follow.
The transition and acceptance of 3D and 4D-printed ADs from research laboratories to clinical applications will revolutionize healthcare. However, the most critical step is navigating the regulatory hurdles for FDA and EMA approvals. There is a need for interdisciplinary collaboration among engineering, materials, and medical professionals to achieve successful scalability and clinical practice, such as customized cranial plates, bio-printed skin grafts for burns, and smart stents that expand in response to bodily fluids [144]. Other challenges, such as organ bioprinting, necessitate an ethical and regulatory framework, as well as social acceptance protocols, alongside advanced biomaterials for sustainable applications. Additionally, integrating AI and automation to address precision and control needs is crucial for future innovations. Less dependency on donor organs, on demand medical solutions, personalized care, patient specific outcomes, and clinical historical data are key advancements, in addition to the others already discussed. Now, advanced 4D-printed technologies are readily accessible and can be printed in urban areas, while in contrast, small hospitals and clinics in rural areas are hundreds of kilometers away from these technologies, including even basic 3D printers. So progressive methodology is required. In the first step, rural regions require internet access to utilize cloud-based 3D printing software platforms for downloading design files and to support decentralized manufacturing processes. The high costs of 3D printers, along with delivery and maintenance expenses, exclude rural communities from accessing this technology. Additionally, limited availability of advanced materials and insufficient technical training are the barriers to the adoption of additive manufacturing in both urban and rural populations. In Table 10 are detailed SWOT analyses comparing the use of 4D printing in ADs across three classes of smart materials: SMAs, PMs, and SHPs. This qualitative assessment highlights the strengths, weaknesses, opportunities, and threats of each material, providing a structured perspective despite the scarcity of quantitative benchmarking data, particularly for prototypes at the academic or laboratory level.

Table 10.
SWOT analysis of 4D printing in assistive devices for SMAs, PMs, and SHPs.
5.2. Future Trends
To create advanced ADs, professionals from engineering, manufacturing, and medical fields must collaborate. As in the case of a simple new manufacturing process, it starts with strengthening the basics, then gradually building toward more advanced, efficient processes. First, we need to develop strong, sustainable, smart materials, depending on the application requirement. Next, produce ADs by using sustainable additive manufacturing techniques with minimized energy consumption and cost. The data analysis by optimization techniques, testing prototypes, user feedback, and finally advanced steps for building these technologies efficiently. These steps need to involve experts from each field for fast transition and for approvals. This is a simple and easily understandable mechanism that has been used in the past to develop new technologies. Proposed solutions should also include subsidized marketplaces, offline 3D printing toolkits, mobile labs, and educational initiatives that teach communities about additive manufacturing. Hence, to improve the impact and adoption of ADs, it is essential to ensure affordability digital literacy and increase awareness by involving nongovernmental organizations (NGOs), healthcare departments, and educational institutions. There is a critical roadmap for adopting and involving these technologies in clinical practice, which outlines short-term and long-term goals, first by improving technical parameters of manufacturing techniques, industrial scalability, bio-inspired systems, and AI for patient data analyzing and predicting exercises, then using machine learning algorithms for predicting rehabilitation steps for patients with similar symptoms, reduced waste, and ethical considerations. If all these goals were achieved successfully in stages, we would be successful in developing biocompatible, AI-assisted, smart, and affordable medical devices. To quantify the research landscape and active scholars in 4D printing, a bibliometric analysis was conducted. The field is characterized by the significant contributions of an active group of researchers, whose primary research interests with respect to rank are summarized in Table 11. Geographically, research activity is concentrated in a few key nations, with the top ten contributing countries ranked by publication volume presented in Figure 10, underscoring the global interest in this advanced manufacturing technology.

Table 11.
Most active scholars in 4D printing research (based on Scopus Data (2010–2025)).
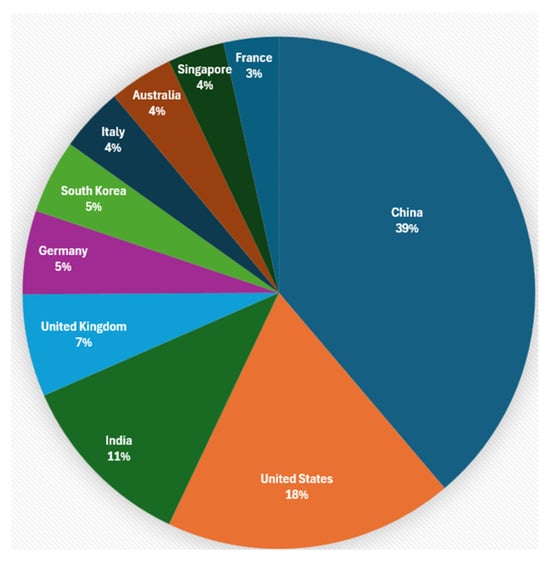
Figure 10.
Geographical research activity in the field of 4D printing as per Scopus (2010–2025).
5.3. AI and Digital Healthcare
The future of assistive technology lies in combining smart materials, AI-based design algorithms, and modern sustainable manufacturing methods. Stimuli responsive materials act as self-adjusting and self-healing, such as in prosthetics and other mobility aids. The inherent adaptability of smart materials without external input can be further increased and optimized by using generative algorithms. To achieve optimized biomechanical efficiency and comfort, exoskeletons with a special lattice design [214] are developed, customized to how each person walks, and prosthetic sockets are designed to balance rigidity and cushioning using patient data, pressure map prediction, and history analysis. Four-dimensional printing uses time as an active feature, enabling wearable systems [215] to change shape autonomously over time. AI [216] will store this data, and then these systems can adapt intelligently. AI predictive analysis with 4D adaptability will function as closed-loop systems, for example, preventing falls in patients wearing smart exoskeletons and diabetic socks that contain hydrogel releasing therapeutics in response to inflammation. AI systems can monitor data from the body in real time, recognize early patterns of inflammation, and control when and how much therapeutic agent is released. AI will make these ADs more precise, adaptive, sustainable, and customized and help in preventive treatment for critical patients. Three-dimensional and 4D printing enable the rapid creation of innovative rehabilitation tools. In contrast, AI will store data from different patients in the cloud, allowing customized smart devices in practice to predict the best geometrical designs and identify problems before they occur. So adjusting treatments and providing instant feedback to medical professionals about device performance is crucial for continuous improvement. Hence, to achieve accelerated healing, a patient centered rehabilitation process ensures that each technique grows and adjusts as the patient’s condition changes with time while avoiding the need for attendant and expensive medical guidance.
5.4. Sustainability and Digital Healthcare
Four-dimensional printing utilizes sustainable, smart materials for biodegradable SMPs, such as PLA-PCL blends and lignin composites, while producing ADs that naturally decompose after their functional lifespan, hence preserving the ecology. AI algorithms can optimize smart material formulations and compositions as an advanced material engineering tool, while machine learning models will also predict degradation rates to balance durability and sustainability. Hybrid materials, such as sustainable polymers derived from algae self-healing and enzyme activated recyclable smart materials, will promote the lifespans of medical devices, resulting in fewer replacements. All these smart properties will result in lower carbon footprints. Another breakthrough is low temperature 4D printing, which will make production more accessible, with a working principle that focuses on safe and biodegradable effects. Advanced energy autonomous systems, such as humidity and light actuated joints, can also be developed. For aligning medical innovation with planetary health goals, biohybrid devices are crucial, as they utilize living cells to enable them to respond and adapt to changes in their surroundings.
6. Conclusions
The process of integrating SMs, advanced 3D and 4D printing techniques, eco-friendly materials, and AI strategies provides a practical, transformative solution for customized, flexible, and sustainable smart ADs, such as biodegradable prosthetics, self-adjusting orthoses, and lightweight exoskeletons. To realize this potential on an industrial scale, critical and technically sensitive parameters must be addressed. Policy frameworks that focus on standardizing safety, biodegradability certifications, and ethical guidelines are essential, ensuring these solutions support global sustainability goals. Another important factor is focusing on cost effective techniques, so balancing technological innovations, device effectiveness, sustainability, and accessibility is the goal. To achieve this long term goal, the first step should be to develop customized, effective smart ADs within hospital premises, making clinical practices and healthcare professionals independent, after that, develop historical technical data, user’s feedback, and performance metrics. It is also vital for engineers, doctors, material experts, and policymakers to work together and harmonize technical innovation with clinical needs. Researchers should transform ADs from laboratory successes into commercially viable and acceptable devices. Public acceptance can be improved through the involvement of social and medical professionals, which could accelerate regulatory approvals and market adoption. By combining all these challenges, we can develop more effective solutions and translate them into a successful adaptive assistive device. The goal should be to have ADs that offer superior functionality compared to conventional devices, possess ecologically regenerative functions, and are universally accessible and economically viable.
Author Contributions
Conceptualization, M.A.S. and N.S.; methodology, M.A.S., N.S. and M.U.; formal analysis, M.A.S. and N.S.; investigation, M.A.S.; resources, M.A.S.; data curation, M.A.S.; writing—original draft preparation, M.A.S., N.S. and M.U.; writing—review and editing, M.A.S., N.S. and M.U.; visualization, M.U.; supervision, N.S.; project administration, N.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Drum, C.E. Chapter 3 Models and Approaches to Disability. In Disability and Public Health; American Public Health Association: Washington, DC, USA, 2012. [Google Scholar]
- Yusif, S.; Soar, J.; Hafeez-Baig, A. Older people, assistive technologies, and the barriers to adoption: A systematic review. Int. J. Med. Inform. 2016, 94, 112–116. [Google Scholar] [CrossRef]
- Cook, A.M.; Polgar, J.M.; Encarnação, P. Assistive Technologies: Principles & Practice; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Schur, L.; Kruse, D.; Blanck, P. People with Disabilities: Sidelined or Mainstreamed? Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Rimmerman, A. Social Inclusion of People with Disabilities: National and International Perspectives; Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Dawes, P.; Emsley, R.; Cruickshanks, K.J.; Moore, D.R.; Fortnum, H.; Edmondson-Jones, M.; McCormack, A.; Munro, K.J. Hearing loss and cognition: The role of hearing AIDS, social isolation and depression. PLoS ONE 2015, 10, e0119616. [Google Scholar] [CrossRef]
- WHO. World Health Organization Glossary. Available online: https://www.who.int/docs/default-source/documents/health-systems-strengthening-glossary.pdf (accessed on 10 March 2025).
- Yong, C.Y.; Chew, K.M.; Mahmood, N.H.; Sudirman, R.; Omar, C. Prosthetics: Health quality of life effects of limb loss. In Proceedings of the 2011 4th International Conference on Biomedical Engineering and Informatics (BMEI), Shanghai, China, 15–17 October 2011; pp. 1333–1337. [Google Scholar]
- Boot, F.H.; Owuor, J.; Dinsmore, J.; MacLachlan, M. Access to assistive technology for people with intellectual disabilities: A systematic review to identify barriers and facilitators. J. Intellect. Disabil. Res. 2018, 62, 900–921. [Google Scholar] [CrossRef]
- Cowan, R.E.; Fregly, B.J.; Boninger, M.L.; Chan, L.; Rodgers, M.M.; Reinkensmeyer, D.J. Recent trends in assistive technology for mobility. J. Neuroeng. Rehabil. 2012, 9, 20. [Google Scholar] [CrossRef]
- U.N. Convention on the Rights of Persons with Disabilities. U.Nations, Editor. 2006. Available online: https://www.un.org/esa/socdev/enable/rights/convtexte.htm (accessed on 10 March 2025).
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021, 396, 2006–2017. [Google Scholar] [CrossRef]
- Mirasadi, K.; Yousefi, M.A.; Jin, L.; Rahmatabadi, D.; Baniassadi, M.; Liao, W.-H.; Bodaghi, M.; Baghani, M. 4D Printing of Magnetically Responsive Shape Memory Polymers: Toward Sustainable Solutions in Soft Robotics, Wearables, and Biomedical Devices. Adv. Sci. 2024, 77, e13091. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Virrueta, C.; Zhang, S.; Mao, C.; Wang, J. 4D printing: The spotlight for 3D printed smart materials. Mater. Today 2024, 77, 66–91. [Google Scholar] [CrossRef]
- WHO. Global Report on Assistive Technology. 2023. Available online: https://www.who.int/publications/i/item/9789240049451 (accessed on 10 March 2025).
- WHO; Standards, HPPA (WHO). Assistive Product List. WHO. 2016. Available online: https://www.who.int/teams/health-product-policy-and-standards/assistive-and-medical-technology/assistive-technology/promoting-access (accessed on 10 March 2025).
- WHO & World Bank. World Report on Disability. WHO & World Bank. 2011. Available online: https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/world-report-on-disability (accessed on 10 March 2025).
- UNICEF. The Future of Childhood in a Changing World. UNICEF. 2024. Available online: https://www.unicef.org/reports/state-of-worlds-children/2024 (accessed on 20 March 2025).
- WHO (World Health Organization). WHA 71.8—Progress Indicators for Access to Assistive Technology. World Health Organization. 2018. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-ATM-2022.01 (accessed on 20 March 2025).
- Andrysek, J. Lower-limb prosthetic technologies in the developing world: A review of literature from 1994–2010. Prosthet. Orthot. Int. 2010, 34, 378–398. [Google Scholar] [CrossRef] [PubMed]
- Flemmer, C.L.; Flemmer, R.C. A review of manual wheelchairs. Disabil. Rehabil. Assist. Technol. 2016, 11, 177–187. [Google Scholar] [CrossRef]
- Manero, A.; Smith, P.; Sparkman, J.; Dombrowski, M.; Courbin, D.; Kester, A.; Womack, I.; Chi, A. Implementation of 3D printing technology in the field of prosthetics: Past, present, and future. Int. J. Environ. Res. Public Health 2019, 16, 1641. [Google Scholar] [CrossRef]
- Gikandi, J.; Kimaru, S.; Mwangi, J.; Mugwe, M. Assessment of the Benefits and Challenges of Digital Braille Assistive Devices in Promoting Inclusivity of Learners with Visual Impairment in Kenya. Acitya J. Teach. Educ. 2025, 7, 258–289. [Google Scholar] [CrossRef]
- Silva, R.; Silva, B.; Fernandes, C.; Morouço, P.; Alves, N.; Veloso, A. A review on 3D scanners studies for producing customized orthoses. Sensors 2024, 24, 1373. [Google Scholar] [CrossRef] [PubMed]
- Vennam, S.; Vijayasankar, K.; Pati, F. 3D printed personalized assistive devices: A material, technique, and medical condition perspective. Appl. Mater. Today 2024, 40, 102403. [Google Scholar] [CrossRef]
- Mahmoudi-Dehaki, M.; Nasr-Esfahani, N.; Vasan, S. The transformative role of assistive technology in enhancing quality of life for individuals with disabilities. In Assistive Technology Solutions for Aging Adults and Individuals with Disabilities; IGI Global Scientific Publishing: Hershey, PA, USA, 2025; pp. 45–72. [Google Scholar]
- Mishra, S.; Laplante-Levesque, A.; Barbareschi, G.; Witte, L.D.; Abdi, S.; Spann, A.; Khasnabis, C.; Allen, M. Assistive technology needs, access and coverage, and related barriers and facilitators in the WHO European region: A scoping review. Disabil. Rehabil. Assist. Technol. 2024, 19, 474–485. [Google Scholar] [CrossRef]
- Lourenço, J.W.; de Jesus, P.A.C.; Schaefer, J.L.; Canciglieri Junior, O. Challenges and strategies for the development and diffusion of assistive technologies. Disabil. Rehabil. Assist. Technol. 2025, 1–14. [Google Scholar] [CrossRef]
- Fasipe, G.; Goršič, M.; Rahman, M.H.; Rammer, J. Community mobility and participation assessment of manual wheelchair users: A review of current techniques and challenges. Front. Hum. Neurosci. 2024, 17, 1331395. [Google Scholar] [CrossRef]
- Pedroza-Santiago, E.A.; Quiroz-Ibarra, J.E.; Bojorges-Valdez, E.R.; Padilla-Castañeda, M.Á. Comparison of Manual, Automatic, and Voice Control in Wheelchair Navigation Simulation in Virtual Environments: Performance Evaluation of User and Motion Sickness. Sensors 2025, 25, 530. [Google Scholar] [CrossRef]
- EksoNR Technology (ECTRON). The EksoNR Exoskeleton. ECTRON. Available online: https://www.ectron.co.uk/eksonr (accessed on 20 March 2025).
- Zolfagharian, A.; Kouzani, A.Z.; Khoo, S.Y.; Moghadam, A.A.A.; Gibson, I.; Kaynak, A. Evolution of 3D printed soft actuators. Sens. Actuators A Phys. 2016, 250, 258–272. [Google Scholar] [CrossRef]
- Wiśniowska-Szurlej, A.; Wołoszyn, N.; Brożonowicz, J.; Ciąpała, G.; Pietryka, K.; Grzegorczyk, J.; Leszczak, J.; Sozańska, A.; Sozański, B.; Korczowski, B. Enhanced Rehabilitation Outcomes of Robotic-Assisted Gait Training with EksoNR Lower Extremity Exoskeleton in 19 Stroke Patients. Med. Sci. Monit. 2023, 29, e940511. [Google Scholar] [CrossRef]
- LIFEWARD Rewalk Ex oskeleton. ReWalk Robotics’ Exo-Suit. 2024. Available online: https://golifeward.com/products/rewalkpersonal-exoskeleton/ (accessed on 20 March 2025).
- Progettiamo Autonomia. REWALK Exoskelton. 2022. Available online: https://progettiamoautonomia.it/prodotto/rewalk (accessed on 20 March 2025).
- Siviy, C.; Baker, L.M.; Quinlivan, B.T.; Porciuncula, F.; Swaminathan, K.; Awad, L.N.; Walsh, C.J. Opportunities and challenges in the development of exoskeletons for locomotor assistance. Nat Biomed Eng 2023, 7, 456–472. [Google Scholar] [CrossRef]
- Shin, S.Y.; Hohl, K.; Giffhorn, M.; Awad, L.N.; Walsh, C.J.; Jayaraman, A. Soft robotic exosuit augmented high intensity gait training on stroke survivors: A pilot study. J. Neuroeng. Rehabil. 2022, 19, 51. [Google Scholar] [CrossRef]
- Bioservo. Carbonhand. 2024. Available online: https://www.bioservo.com/products/carbonhand (accessed on 20 March 2025).
- Control Bionics. NeuroNode Trilogy. 2022. Available online: https://www.controlbionics.com/products/how-it-works/ (accessed on 20 March 2025).
- Lo, L. Does Eye Gaze Combined with EMG Switching Outperform Traditional Eye Gaze AAC Systems? RMIT University: Melbourne, Australia, 2022. [Google Scholar]
- Mobius Bionics. LUKE Arm. 2023. Available online: https://mobiusbionics.com/luke-arm/ (accessed on 20 March 2025).
- George, J.A.; Davis, T.S.; Brinton, M.R.; Clark, G.A. Intuitive neuromyoelectric control of a dexterous bionic arm using a modified Kalman filter. J. Neurosci. Methods 2020, 330, 108462. [Google Scholar] [CrossRef] [PubMed]
- Yurkewich, A.; Hebert, D.; Wang, R.; Mihailidis, A. Hand Extension Robot Orthosis (HERO) Glove: Development and Testing With Stroke Survivors With Severe Hand Impairment. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 916–926. [Google Scholar] [CrossRef] [PubMed]
- Landori-Hoffmann, D.; Mihalache, J.; Aziegbe, O.; Vella, M.; Charest-Finn, M.; Yurkewich, A. HERO Glove Insight: Utilizing Computer Vision and Force Sensors for Object-Specific Force Control. In Proceedings of the 2025 International Conference on Rehabilitation Robotics (ICORR), Chicago, IL, USA, 12–16 May 2025; pp. 614–619. [Google Scholar]
- Progettiamo Autonomia. MYOSUIT. 2024. Available online: https://progettiamoautonomia.it/prodotto/myosuit/ (accessed on 20 March 2025).
- Polzin, M.; Guan, Q.; Hughes, J. Robotic locomotion through active and passive morphological adaptation in extreme outdoor environments. Sci. Robot. 2025, 10, eadp6419. [Google Scholar] [CrossRef]
- Kim, J.; Kim, Y.; Kang, S.; Kim, S.-J. Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait. Sensors 2022, 22, 6127. [Google Scholar] [CrossRef]
- BrainRobotics. BrainRobotics AI Prosthetic Hand. 2024. Available online: https://www.brainrobotics.com/ (accessed on 20 March 2025).
- Kang, B.B.; Choi, H.; Lee, H.; Cho, K.J. Exo-Glove Poly II: A Polymer-Based Soft Wearable Robot for the Hand with a Tendon-Driven Actuation System. Soft Robot 2019, 6, 214–227. [Google Scholar] [CrossRef]
- Sadeghi, M.; Abbasimoshaei, A.; Kitajima Borges, J.P.; Kern, T.A. Numerical and Experimental Study of a Wearable Exo-Glove for Telerehabilitation Application Using Shape Memory Alloy Actuators. Actuators 2024, 13, 409. [Google Scholar] [CrossRef]
- Honoree in Digital Health. Qolo Rehabilitation. Available online: https://www.ces.tech/ces-innovation-awards/2025/qolo-rehabilitation/ (accessed on 20 March 2025).
- Lauruschkus, K.; Jarl, J.; Fasth Gillstedt, K.; Tornberg, Å.B. Dynamic Standing Exercise in a Novel Assistive Device Compared with Standard Care for Children with Cerebral Palsy Who Are Non-Ambulant, with Regard to Quality of Life and Cost-Effectiveness. Disabilities 2022, 2, 73–85. [Google Scholar] [CrossRef]
- AbleChair. 2023. Available online: https://ablechair.com/ (accessed on 27 March 2025).
- Xu, Y.; Zhang, B.; Li, Y.; Guo, R.; Cao, P.; Zhu, X.; Zhu, S. Design and Evaluation of the Sit-to-Stand Movement Assistive Device for Elderly. Actuators 2024, 13, 102. [Google Scholar] [CrossRef]
- Wang, T.; Zhao, Y.; Zhang, X.; Xie, Y.; Pang, L.L.L. Design of walking aids for the elderly based on the Kano-AHP-FEC method. Sci. Rep. 2025, 15, 2663. [Google Scholar] [CrossRef]
- Fortuna, A.; Lorenzini, M.; Leonori, M.; Gandarias, J.M.; Balatti, P.; Cho, Y.; De Momi, E.; Ajoudani, A. A personalizable controller for the walking assistive omni-directional exo-robot (WANDER). In Proceedings of the 2024 IEEE International Conference on Robotics and Automation (ICRA), Yokohama, Japan, 13–17 May 2024; pp. 3212–3218. [Google Scholar]
- Hashida, R.; Matsuse, H.; Bekki, M.; Omoto, M.; Morimoto, S.; Hino, T.; Harano, Y.; Iwasa, C.; Miyamoto, K.; Haraguchi, M.; et al. Evaluation of Motor-Assisted Gloves (SEM Glove) for Patients with Functional Finger Disorders: A Clinical Pilot Study. Kurume Med. J. 2019, 65, 63–70. [Google Scholar] [CrossRef]
- Chung, J.; Heimgartner, R.; Neill, C.T.O.; Phipps, N.S.; Walsh, C.J. ExoBoot, a Soft Inflatable Robotic Boot to Assist Ankle During Walking: Design, Characterization and Preliminary Tests. In Proceedings of the 2018 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), Enschede, The Netherlands, 26–29 August 2018; pp. 509–516. [Google Scholar]
- Akhmejanov, S.; Zhetenbayev, N.; Sultan, A.; Zhauyt, A.; Nurgizat, Y.; Ozhikenov, K.; Ayazbay, A.-A.; Uzbekbayev, A. Design and Analysis of an Autonomous Active Ankle–Foot Prosthesis with 2-DoF. Sensors 2025, 25, 4881. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, N.; Lenzi, T.; Roccella, S.; De Rossi, S.M.M.; Cattin, E.; Giovacchini, F.; Vecchi, F.; Carrozza, M.C. NEUROExos: A Powered Elbow Exoskeleton for Physical Rehabilitation. IEEE Trans. Robot. 2013, 29, 220–235. [Google Scholar] [CrossRef]
- Matrone, G.C.; Cipriani, C.; Carrozza, M.C.; Magenes, G. Real-time myoelectric control of a multi-fingered hand prosthesis using principal components analysis. J. Neuroeng. Rehabil. 2012, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.; Jeong, S.; Lyu, F.; Herrin, K.; Bhatia, S.; Elliott, D.; Kozin, S.; Desai, J.P. FLEXotendon Glove-III: Voice-Controlled Soft Robotic Hand Exoskeleton With Novel Fabrication Method and Admittance Grasping Control. IEEE/ASME Trans. Mechatron. 2022, 27, 3920–3931. [Google Scholar] [CrossRef]
- Bazina, T.; Kladarić, M.; Kamenar, E.; Gregov, G. Development of Rehabilitation Glove: Soft Robot Approach. Actuators 2024, 13, 472. [Google Scholar] [CrossRef]
- SPEXOR. Spinal Exoskeletal Robot for Low Back Pain Prevention and Vocational Reintegration. Available online: https://spexor.eu/ (accessed on 27 March 2025).
- Babič, J.; Petrič, T.; Mombaur, K.; Kingma, I.; Bornmann, J.; González-Vargas, J.; Baltrusch, S.; Šarabon, N.; Houdijk, H. SPEXOR: Design and development of passive spinal exoskeletal robot for low back pain prevention and vocational reintegration. SN Appl. Sci. 2019, 1, 262. [Google Scholar] [CrossRef]
- Zhu, C.; Zhou, C.; Zou, Q.; Wang, X.; Deng, L.; Wang, J.; Fan, J. A variable stiffness fishlike propeller with compressible flexible bionic spine. Ocean Eng. 2025, 316, 119780. [Google Scholar] [CrossRef]
- Fu, K.; Wu, X.; Yu, S.; Zhang, Q.; Yang, Y.; Xu, T.; Yao, W.; Yi, T.; Li, H.; Chen, Y.; et al. Origami exoskeletons for enhanced soft robotic manipulation. Sci. Adv. 2025, 11, eadv6629. [Google Scholar] [CrossRef]
- Ossur. Power Knee. Available online: https://www.ossur.com/en-us/prosthetics/knees/power-knee (accessed on 2 April 2025).
- Culver, S.C.; Vailati, L.G.; Morgenroth, D.C.; Goldfarb, M. A new approach to a powered knee prosthesis: Layering powered assistance onto strictly passive prosthesis behavior. Wearable Technol. 2023, 4, e21. [Google Scholar] [CrossRef]
- Jung, W.-K.; Lee, S.-M.; Ahn, S.-H.; Park, J. Development and assessment of a knitted shape memory alloy-based multifunctional elbow brace. J. Ind. Text. 2022, 51, 1989S–2009S. [Google Scholar] [CrossRef]
- Lee, S.-M.; Park, J. A soft wearable exoglove for rehabilitation assistance: A novel application of knitted shape-memory alloy as a flexible actuator. Fash. Text. 2024, 11, 14. [Google Scholar] [CrossRef]
- Li, Z.; Wang, C.; Song, X.; Liu, S.; Zhang, Y.; Jiang, S.; Ji, X.; Zhang, T.; Xu, F.; Hu, L.; et al. Accuracy Evaluation of a Novel Spinal Robotic System for Autonomous Laminectomy in Thoracic and Lumbar Vertebrae: A Cadaveric Study. JBJS 2023, 105, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Burström, G.; Balicki, M.; Patriciu, A.; Kyne, S.; Popovic, A.; Holthuizen, R.; Homan, R.; Skulason, H.; Persson, O.; Edström, E.; et al. Feasibility and accuracy of a robotic guidance system for navigated spine surgery in a hybrid operating room: A cadaver study. Sci. Rep. 2020, 10, 7522. [Google Scholar] [CrossRef]
- Madden, K.; Flood, B.; Malek, M.; Milantoni, V.; Astephen Wilson, J.L.; Tarride, J.-E.; Khanna, V.; Adili, A.; Madden, K.; Adili, A.; et al. Robot-assisted partial knee replacement versus standard total knee replacement (RoboKnees): A protocol for a pilot randomized controlled trial. Pilot Feasibility Stud. 2024, 10, 39. [Google Scholar] [CrossRef]
- Sun, Y.; Tang, H.; Tang, Y.; Zheng, J.; Dong, D.; Chen, X.; Liu, F.; Bai, L.; Ge, W.; Xin, L.; et al. Review of Recent Progress in Robotic Knee Prosthesis Related Techniques: Structure, Actuation and Control. J. Bionic Eng. 2021, 18, 764–785. [Google Scholar] [CrossRef]
- Du, H.; Li, G.; Sun, J.; Zhang, Y.; Bai, Y.; Qian, C.; Liang, Y. A review of shape memory alloy artificial muscles in bionic applications. Smart Mater. Struct. 2023, 32, 103001. [Google Scholar] [CrossRef]
- Davidar, A.D.; Jiang, K.; Weber-Levine, C.; Bhimreddy, M.; Theodore, N. Advancements in Robotic-Assisted Spine Surgery. Neurosurg. Clin. 2024, 35, 263–272. [Google Scholar] [CrossRef]
- Antonelli, M.G.; Beomonte Zobel, P.; Sarwar, M.A.; Stampone, N. Mechanical Design of McKibben Muscles Predicting Developed Force by Artificial Neural Networks. Actuators 2025, 14, 153. [Google Scholar] [CrossRef]
- Antonelli, M.G.; Beomonte Zobel, P.; Sarwar, M.A.; Stampone, N. Seahorse-tail-inspired soft pneumatic actuator: Development and experimental characterization. Biomimetics 2024, 9, 264. [Google Scholar] [CrossRef]
- Pan, M.; Yuan, C.; Liang, X.; Dong, T.; Liu, T.; Zhang, J.; Zou, J.; Yang, H.; Bowen, C. Soft Actuators and Robotic Devices for Rehabilitation and Assistance. Adv. Intell. Syst. 2022, 4, 2100140. [Google Scholar] [CrossRef]
- Wang, H.; Yang, L.; Yang, Y.; Zhang, D.; Tian, A. Highly flexible, large-deformation ionic polymer metal composites for artificial muscles: Fabrication, properties, applications, and prospects. Chem. Eng. J. 2023, 469, 143976. [Google Scholar] [CrossRef]
- Wang, Q.; Ghrayeb, A.; Kim, S.; Cheng, L.; Tawfick, S. The mechanics and physics of twisted and coiled polymer actuators. Int. J. Mech. Sci. 2024, 280, 109440. [Google Scholar] [CrossRef]
- Min, J.; Wu, Z.; Zhang, W.; Liu, Y.; Luo, D. Intelligent Liquid Crystal Elastomer Actuators with High Mechanical Strength, Self-Sensing, and Automatic Control. Adv. Sens. Res. 2024, 3, 2300117. [Google Scholar] [CrossRef]
- Cyberdyne HAL. Available online: https://www.cyberdyne.jp/english/products/HAL/ (accessed on 2 April 2025).
- WYSS. Harvard Harvard Soft Robotic Glove. Available online: https://wyss.harvard.edu/technology/soft-robotic-glove/ (accessed on 2 April 2025).
- Simonds, E.; Colton, J.; Kogler, G.; Chang, Y.H. Design and testing of a prototype foot orthosis that uses the principle of granular jamming. Prosthetics Orthot. Int. 2021, 45, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Heung, K.H.; Li, H.; Wong, T.W.; Ng, S.S. Assistive robotic hand with bi-directional soft actuator for hand impaired patients. Front. Bioeng. Biotechnol. 2023, 11, 1188996. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.D.; Park, H.; Hong, D.H.; Kang, T.H. Development of a Series Elastic Tendon Actuator (SETA) Based on Gait Analysis for a Knee Assistive Exosuit. Actuators 2022, 11, 166. [Google Scholar] [CrossRef]
- Jeong, J.; Yasir, I.B.; Han, J.; Park, C.H.; Bok, S.-K.; Kyung, K.-U. Design of Shape Memory Alloy-Based Soft Wearable Robot for Assisting Wrist Motion. Appl. Sci. 2019, 9, 4025. [Google Scholar] [CrossRef]
- Vetelino, J.; Reghu, A. Introduction to Sensors; CRC press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Javaid, M.; Haleem, A.; Rab, S.; Singh, R.P.; Suman, R. Sensors for daily life: A review. Sens. Int. 2021, 2, 100121. [Google Scholar] [CrossRef]
- Sehrawat, D.; Gill, N.S. Smart sensors: Analysis of different types of IoT sensors. In Proceedings of the 2019 3rd International Conference on Trends in Electronics and Informatics (ICOEI), Tirunelveli, India, 23–25 April 2019; pp. 523–528. [Google Scholar]
- Han, T.; Kundu, S.; Nag, A.; Xu, Y. 3D printed sensors for biomedical applications: A review. Sensors 2019, 19, 1706. [Google Scholar] [CrossRef]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and Actuation Technologies in Exoskeletons: A Review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Russell, J.; Bergmann, J.H.M. Real-Time Intent Sensing for Assistive Devices with Implications for Minimising Maintenance. Prosthesis 2023, 5, 453–466. [Google Scholar] [CrossRef]
- Liu, J.; Liu, J.; Xu, L.; Jin, W. Electronic travel aids for the blind based on sensory substitution. In Proceedings of the 2010 5th International Conference on Computer Science & Education, Hefei, China, 24–27 August 2010; pp. 1328–1331. [Google Scholar]
- Sánchez, J.; Elías, M. Guidelines for designing mobility and orientation software for blind children. In Proceedings of the IFIP Conference on Human-Computer Interaction, Rio de Janeiro, Brazil, 10–14 September 2007; pp. 375–388. [Google Scholar]
- Lee, K.; Ha, S.; Lee, K.; Hong, S.; Shin, H.; Lee, G. Development of a sit-to-stand assistive device with pressure sensor for elderly and disabled: A feasibility test. Phys. Eng. Sci. Med. 2021, 44, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Kammarchedu, V.; AlSiyabi, M.; Ebrahimi, A. Skin-Conformal Myography for Real-Time Hand Tracking Using a Laser-Induced Graphene Strain Sensor Array. Adv. Intell. Syst. 2025, 7, 2400812. [Google Scholar] [CrossRef]
- Intel RealSense D400f Depth Camera. Available online: https://www.intelrealsense.com/stereo-depth-with-ir/ (accessed on 10 April 2025).
- Ahn, J.-B.; Yoo, B.; Pines, D.J.; Kuo, C.-Y.; Wang, M.; Bejjanki, N.S.G.; Kim, S. Microchannel pressure sensor for continuous and real-time wearable gait monitoring. Commun. Mater. 2024, 5, 136. [Google Scholar] [CrossRef]
- Haghiashtiani, G.; Habtour, E.; Park, S.-H.; Gardea, F.; McAlpine, M.C. 3D printed electrically-driven soft actuators. Extrem. Mech. Lett. 2018, 21, 1–8. [Google Scholar] [CrossRef]
- Tawk, C.; Alici, G. A review of 3D—Printable soft pneumatic actuators and sensors: Research challenges and opportunities. Adv. Intell. Syst. 2021, 3, 2000223. [Google Scholar] [CrossRef]
- Copeland, C.; Reyes, C.C.; Peck, J.L.; Srivastava, R.; Zuniga, J.M. Functional performance and patient satisfaction comparison between a 3D printed and a standard transradial prosthesis: A case report. Biomed. Eng. Online 2022, 21, 7. [Google Scholar] [CrossRef]
- Badini, S.; Regondi, S.; Lammi, C.; Bollati, C.; Donvito, G.; Pugliese, R. Computational Mechanics of Form-Fitting 3D-Printed Lattice-Based Wrist-Hand Orthosis for Motor Neuron Disease. Biomedicines 2023, 11, 1787. [Google Scholar] [CrossRef]
- De Vivo Nicoloso, L.G.; Pelz, J.; Barrack, H.; Kuester, F. Towards 3D printing of a monocoque transtibial prosthesis using a bio-inspired design workflow. Rapid Prototyp. J. 2021, 27, 67–80. [Google Scholar] [CrossRef]
- Răduică, F.-F.; Simion, I. Development of a Low-Cost 3D-Printed Upper Limb Prosthetic Device with Hybrid Actuation for Partial Hand Amputees. Appl. Sci. 2024, 14, 8929. [Google Scholar] [CrossRef]
- Risad, R.H.; Ahmed, M.H.; Basher, A.; Rashid, S.; Shishir, M.M.A.; Hossain, K.R. FDM printing process and its Biomedical Application. Chem. Res. Technol. 2024, 1, 138–149. [Google Scholar]
- Yousif, L.E.; Abed, M.S.; Al-Zubidi, A.B.; Resan, K.K. Innovations in prosthetic foot design enhancing durability, functionality and comfort through PLA composite filament 3D printing. Pigment Resin Technol. 2025, 54, 378–389. [Google Scholar] [CrossRef]
- Ott, M.; Jung, P.; Bödger, C.; Koch, R.; Mozgova, I.; Tröster, T. Fused Deposition Modeling and its Extension Through Metal-Filled Filaments as a Means of Self-Help for Individuals with Physical Disabilities. In Proceedings of the Workshop on Innovative Product Development by Additive Manufacturing, Stuttgart, Germany, 12 September 2023; pp. 117–127. [Google Scholar]
- Solomon, I.J.; Sevvel, P.; Gunasekaran, J. A review on the various processing parameters in FDM. Mater. Today Proc. 2021, 37, 509–514. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Espera, A.H.; Chen, Q.; Advincula, R.C. Mechanical characterization of 3D-printed polymers. Addit. Manuf. 2018, 20, 44–67. [Google Scholar] [CrossRef]
- Polozov, I.; Nefyodov, V.; Zolotarev, A.; Sokolova, V.; Gracheva, A.; Popovich, A. Process-structure–property relationships in selective laser melting of Ti-15Ta alloy for biomedical applications. Int. J. Adv. Manuf. Technol. 2025, 139, 3391–3406. [Google Scholar] [CrossRef]
- Velôso, D.V.; Barbin, T.; Del Rio Silva, L.; Barão, V.A.R.; Mesquita, M.F.; Borges, G.A. Additive manufacturing of CAD-CAM complete arch fixed implant restorations supported by six implants: Prosthetic screw stability and marginal precision under masticatory simulation. J. Prosthet. Dent. 2025, 134, 783.e1–783.e9. [Google Scholar] [CrossRef]
- van Roo, T.; Mager, C.J. Mechanical Behavior of SLS-Printed Parts and Their Structural Simulation. J. Manuf. Mater. Process. 2025, 9, 83. [Google Scholar] [CrossRef]
- Zhang, J.; Hu, Q.; Wang, S.; Tao, J.; Gou, M. Digital Light Processing Based Three-dimensional Printing for Medical Applications. Int. J. Bioprint. 2020, 6, 242. [Google Scholar] [CrossRef]
- Maines, E.M.; Porwal, M.K.; Ellison, C.J.; Reineke, T.M. Sustainable advances in SLA/DLP 3D printing materials and processes. Green Chem. 2021, 23, 6863–6897. [Google Scholar] [CrossRef]
- Chokshi, S.; Gangatirkar, R.; Kandi, A.; DeLeonibus, M.; Kamel, M.; Chadalavada, S.; Gupta, R.; Munigala, H.; Tappa, K.; Kondor, S. Medical 3D Printing Using Material Jetting: Technology Overview, Medical Applications, and Challenges. Bioengineering 2025, 12, 249. [Google Scholar] [CrossRef]
- Bezek, L.B.; Chatham, C.A.; Dillard, D.A.; Williams, C.B. Mechanical properties of tissue-mimicking composites formed by material jetting additive manufacturing. J. Mech. Behav. Biomed. Mater. 2022, 125, 104938. [Google Scholar] [CrossRef]
- Gülcan, O.; Günaydın, K.; Tamer, A. The State of the Art of Material Jetting—A Critical Review. Polymers 2021, 13, 2829. [Google Scholar] [CrossRef]
- Adelmann, B.; Hellmann, R. Mechanical Properties of LPBF-Built Titanium Lattice Structures—A Comparative Study of As-Built and Hot Isostatic Pressed Structures for Medical Implants. Metals 2022, 12, 2072. [Google Scholar] [CrossRef]
- Khorasani, M.; Gibson, I.; Ghasemi, A.H.; Hadavi, E.; Rolfe, B. Laser subtractive and laser powder bed fusion of metals: Review of process and production features. Rapid Prototyp. J. 2023, 29, 935–958. [Google Scholar] [CrossRef]
- Sing, S.L.; An, J.; Yeong, W.Y.; Wiria, F.E. Laser and electron—Beam powder—Bed additive manufacturing of metallic implants: A review on processes, materials and designs. J. Orthop. Res. 2016, 34, 369–385. [Google Scholar] [CrossRef] [PubMed]
- Boston Children’s Hospital. Cardiovascular 3D Modeling and Simulation Program. 2020. Available online: https://www.childrenshospital.org/programs/cardiovascular-3d-modeling-and-simulation (accessed on 10 April 2025).
- Mayo Clinic. Neurosurgical Simulation. 2020. Available online: https://www.mayo.edu/research/labs/neurosurgery-simulation-innovations/overview (accessed on 10 April 2025).
- Wang, L.; Huang, L.; Li, X.; Zhong, D.; Li, D.; Cao, T.; Yang, S.; Yan, X.; Zhao, J.; He, J.; et al. Three-Dimensional Printing PEEK Implant: A Novel Choice for the Reconstruction of Chest Wall Defect. Ann. Thorac. Surg. 2019, 107, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Hospital for Special Surgery. 3D-Printed Scoliosis Braces. 2022. Available online: https://www.hss.edu/conditions_scoliosis-bracing.asp (accessed on 20 April 2025).
- Li, J.; Zhou, G.; Xu, N.; Sun, P.; Chang, S.; Zhang, Y.; Du, C.; Li, W.; Zeng, Y.; Yu, M. Patient-specific 3D-printed Brace for Adolescent Idiopathic Scoliosis: A Prospective Cohort Study. World Neurosurg. 2024, 189, e69–e79. [Google Scholar] [CrossRef]
- 3D Printed Device for Babies with Rare Respiratory Disease. 2025. Available online: https://medresearch.umich.edu/news-release/clinical-trial-opens-study-groundbreaking-3d-printed-device-babies-rare-respiratory-disease?pk_vid=30f812cc173a32bf17450695024bb6ad (accessed on 10 April 2025).
- Petruzzi, G.; De Virgilio, A.; Pichi, B.; Mazzola, F.; Zocchi, J.; Mercante, G.; Spriano, G.; Pellini, R. COVID-19: Nasal and oropharyngeal swab. Head Neck 2020, 42, 1303–1304. [Google Scholar] [CrossRef]
- Sujatha, S.; Bapat, G.M.; Dash, S.S. GRID: A model for the development of assistive devices in developing countries. Disabil Rehabil Assist Technol 2021, 16, 317–323. [Google Scholar] [CrossRef]
- Ng, W.L.; An, J.; Chua, C.K. Process, material, and regulatory considerations for 3D printed medical devices and tissue constructs. Engineering 2024, 36, 146–166. [Google Scholar] [CrossRef]
- Beitler, B.G.; Abraham, P.F.; Glennon, A.R.; Tommasini, S.M.; Lattanza, L.L.; Morris, J.M.; Wiznia, D.H. Interpretation of regulatory factors for 3D printing at hospitals and medical centers, or at the point of care. 3D Print. Med. 2022, 8, 7. [Google Scholar] [CrossRef]
- FDA. DataBase for FDA. 2025. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm (accessed on 20 April 2025).
- Baran, E.H.; Erbil, H.Y. Surface Modification of 3D Printed PLA Objects by Fused Deposition Modeling: A Review. Colloids Interfaces 2019, 3, 43. [Google Scholar] [CrossRef]
- Zhang, Y. Post-printing surface modification and functionalization of 3D-printed biomedical device. Int. J. Bioprint. 2017, 3, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Guoqing, Z.; Junxin, L.; Xiaoyu, Z.; Anmin, W. Optimization design of support structure based on 3D printing technology. Sci. Rep. 2024, 14, 18225. [Google Scholar] [CrossRef] [PubMed]
- Dizon, J.R.C.; Gache, C.C.L.; Cascolan, H.M.S.; Cancino, L.T.; Advincula, R.C. Post-processing of 3D-printed polymers. Technologies 2021, 9, 61. [Google Scholar] [CrossRef]
- Nguyen, P.; Stanislaus, I.; McGahon, C.; Pattabathula, K.; Bryant, S.; Pinto, N.; Jenkins, J.; Meinert, C. Quality assurance in 3D-printing: A dimensional accuracy study of patient-specific 3D-printed vascular anatomical models. Front. Med. Technol. 2023, 5, 1097850. [Google Scholar] [CrossRef]
- Lotz, O.; McKenzie, D.R.; Bilek, M.M.; Akhavan, B. Biofunctionalized 3D printed structures for biomedical applications: A critical review of recent advances and future prospects. Prog. Mater. Sci. 2023, 137, 101124. [Google Scholar] [CrossRef]
- Jose, J.; Sultan, S.; Kalarikkal, N.; Thomas, S.; Mathew, A.P. Fabrication and functionalization of 3D-printed soft and hard scaffolds with growth factors for enhanced bioactivity. RSC Adv. 2020, 10, 37928–37937. [Google Scholar] [CrossRef]
- Buj-Corral, I.; Bagheri, A.; Petit-Rojo, O. 3D printing of porous scaffolds with controlled porosity and pore size values. Materials 2018, 11, 1532. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Petrescu, F.I.T.; Ungureanu, L.M.; Munteanu, I.S. Post-production finishing processes utilized in 3D printing technologies. Processes 2024, 12, 595. [Google Scholar] [CrossRef]
- Invisalign System for Straighting Teeth. AlignTech’s Invisalign®. 2023 (Patent Pending). Available online: https://www.aligntech.com/solutions (accessed on 1 May 2025).
- STRYKER. 2025. Available online: https://www.stryker.com/it/it/index.html (accessed on 15 April 2025).
- Chen, J.K.C.; Do, H.T.T. Perspective of the 3D Printing Technology Applied on Medical Resource Integration and Service Innovation Business Model. In Proceedings of the 2017 Portland International Conference on Management of Engineering and Technology (PICMET), Portland, OR, USA, 9–13 July 2017; pp. 1–11. [Google Scholar]
- Kuang, X.; Roach, D.J.; Wu, J.; Hamel, C.M.; Ding, Z.; Wang, T.; Dunn, M.L.; Qi, H.J. Advances in 4D Printing: Materials and Applications. Adv. Funct. Mater. 2019, 29, 1805290. [Google Scholar] [CrossRef]
- Mandal, A.; Chatterjee, K. 4D printing for biomedical applications. J. Mater. Chem. B 2024, 12, 2985–3005. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.Y.; Pegg, E.; Chen, A.; Jin, Z.; Gu, G.X. 4D Printing of Electroactive Materials. Adv. Intell. Syst. 2021, 3, 2100019. [Google Scholar] [CrossRef]
- Kantaros, A.; Petrescu, F.I.T.; Ganetsos, T. From Stents to Smart Implants Employing Biomimetic Materials: The Impact of 4D Printing on Modern Healthcare. Biomimetics 2025, 10, 125. [Google Scholar] [CrossRef]
- Toth, L.; Schiffer, A.; Nyitrai, M.; Pentek, A.; Told, R.; Maroti, P. Developing an anti-spastic orthosis for daily home-use of stroke patients using smart memory alloys and 3D printing technologies. Mater. Des. 2020, 195, 109029. [Google Scholar] [CrossRef]
- Awais, M.; AliAbbasi, E.; Atik, A.Y.; Bathaei, M.J.; Ali, M.; Das, R.; Dag, C.; Ullah, A.; Singh, R.; Turker, K.S.; et al. Multiplexed Piezoelectric Electronic Skin with Haptic Feedback for Upper Limb Prosthesis. Adv. Sens. Res. 2024, 3, 2400100. [Google Scholar] [CrossRef]
- Song, J.; Kim, Y.; Kang, K.; Lee, S.; Shin, M.; Son, D. Stretchable and Self-Healable Graphene–Polymer Conductive Composite for Wearable EMG Sensor. Polymers 2022, 14, 3766. [Google Scholar] [CrossRef]
- Mohd Jani, J.; Leary, M.; Subic, A.; Gibson, M.A. A review of shape memory alloy research, applications and opportunities. Mater. Des. 2014, 56, 1078–1113. [Google Scholar] [CrossRef]
- Ottobock Professionals. Early Stage Prototype. 2023. Available online: https://www.ottobock.com/en-us/home (accessed on 16 April 2025).
- Medtronic. MicraAV Leadless Pacemaker (SMA Components). 2023. Available online: https://www.medtronic.com/me-en/healthcare-professionals/products/cardiac-rhythm/pacemakers/micra-av2.html (accessed on 16 April 2025).
- Esplora. Dentsply Sirona’s SmartTrack® Aligners (SMA-Enhanced). 2023. Available online: https://www.dentsplysirona.com/en (accessed on 16 April 2025).
- Xiao, M.; Yao, Y.; Fan, C.; Xu, Z.; Liu, Y.; Liu, B.; Li, J.; Zhang, X.; Jin, X.; Yang, J.; et al. Multiple H-bonding chain extender-based polyurethane: Ultrastiffness, hot-melt adhesion, and 3D printing finger orthosis. Chem. Eng. J. 2022, 433, 133260. [Google Scholar] [CrossRef]
- BASF. BASF’s 4D-Printed Orthopedic Supports (Research Collaboration). Available online: https://promotions.basf.com/news-and-releases/orthopaedic-insoles-made-of-elastollan-more-comfortable-sustainable-and-individual (accessed on 16 April 2025).
- Intuitive Surgical’s Da Vinci (SMA-Enhanced Forceps). 2023. Available online: https://www.intuitive.com/en-us/products-and-services/da-vinci (accessed on 20 April 2025).
- Haberland, C.; Elahinia, M.H. Fabricating NiTi SMA Components. In Shape Memory Alloy Actuators: Design, Fabrication and Experimental Evaluation; John Wiley & Sons: Hoboken, NJ, USA, 2015; p. 191. [Google Scholar]
- Zaszczyńska, A.; Gradys, A.; Sajkiewicz, P. Progress in the Applications of Smart Piezoelectric Materials for Medical Devices. Polymers 2020, 12, 2754. [Google Scholar] [CrossRef] [PubMed]
- SolePower. Smart Boots (Military Use, Charges Batteries Via Walking). 2020. Available online: https://solepowertech.com/smartboot/ (accessed on 20 April 2025).
- Pan, Q.; Long, Z.; Zheng, Y.; Yang, Z. Characterization of Foot Strike Motion and Biomechanical Energy Harvesting for Footwear. IEEE Internet Things J. 2025, 12, 22989–22999. [Google Scholar] [CrossRef]
- Starr, M.B.; Wang, X. Coupling of piezoelectric effect with electrochemical processes. Nano Energy 2015, 14, 296–311. [Google Scholar] [CrossRef]
- Deng, J.; Jiang, W.; Gao, H.; Li, M.; Shi, Y. Active Power Assist with Equivalent Force on Connection for Lower Limb Exoskeleton Robots. Actuators 2024, 13, 212. [Google Scholar] [CrossRef]
- Google Jacquard™ (Prototype Piezoelectric Touch-Sensitive Fabric). 2019. Available online: https://www.carlosterminel.com/jacquard (accessed on 22 April 2025).
- Lou, Z.; Li, L.; Wang, L.; Shen, G. Recent progress of self—Powered sensing systems for wearable electronics. Small 2017, 13, 1701791. [Google Scholar] [CrossRef]
- University of Bern Piezoelectric Pacemaker Prototypes (University of Bern, 2023). Available online: https://www.unibe.ch/ (accessed on 22 April 2025).
- Almouahed, S.; Hamitouche, C.; Stindel, E. Optimized prototype of instrumented knee implant: Experimental validation. IRBM 2017, 38, 250–255. [Google Scholar] [CrossRef]
- ReTiSense™. ReTiSense™ Smart Knee Brace (Energy Harvesting + Pressure Sensing). Available online: https://www.retisense.com/ (accessed on 22 April 2025).
- Yoo, H.-J.; Lee, S.; Kim, J.; Park, C.; Lee, B. Development of 3D-printed myoelectric hand orthosis for patients with spinal cord injury. J. Neuroeng. Rehabil. 2019, 16, 162. [Google Scholar] [CrossRef]
- Teslasuit® Gloves (Piezoelectric Tactile Feedback). 2023. Available online: https://teslasuit.io/ (accessed on 22 April 2025).
- Fu, Y.; Liu, J.; Li, X.; Sun, X. A haptic feedback glove for virtual piano interaction. Virtual Real. Intell. Hardw. 2025, 7, 95–110. [Google Scholar] [CrossRef]
- Xenoma. E-Skin (for Prosthetics). 2023. Available online: https://www.xenoma.com/ (accessed on 1 May 2025).
- Li, M.; Miao, C.; Zou, M.; Guo, J.; Wang, H.; Gao, M.; Zhang, H.; Deng, Z. The development of stretchable and self-repairing materials applied to electronic skin. Front. Chem. 2023, 11, 1198067. [Google Scholar] [CrossRef]
- SpryFlex® Medical Braces (Concept). 2022. Available online: https://www.thuasneusa.com/sprystep-flex/ (accessed on 1 May 2025).
- Zhang, X.; Wang, D.; Lv, D.; Lv, J.; Tang, H.; Qian, J.; Liao, B. Reducing the Brace Correction Stress on the Secondary Lumbar Curve Results in Excellent Muscle, Bone, and Disc Mechanical Performance: A Musculoskeletal Finite Element Simulation of AIS Patient With Rigo A3. Orthop. Surg. 2025, 17, 525–539. [Google Scholar] [CrossRef]
- Coloplast. Coloplast’s SureFlo® (R&D Phase). Available online: https://www.coloplast.com/ (accessed on 1 May 2025).
- He, Q.; Huang, C.; Lu, Y.; Zhao, Y.; Xing, M.; Wang, X.; Sun, B.; Zhu, Y. Developing an anticoagulant microfibrous vascular graft with enhanced kink resistance and self-sealing capabilities. Biomater. Adv. 2025, 173, 214290. [Google Scholar] [CrossRef] [PubMed]
- Frengopoulos, C.; Fuller, K.; Payne, M.W.; Viana, R.; Hunter, S.W. Rehabilitation outcomes after major lower limb amputation in the oldest old: A systematic review. Prosthet. Orthot. Int. 2021, 45, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Össur Power Feet. Healable Foot Prosthetics. 2023. Available online: https://www.ossur.com/en-us/prosthetics/products/feet (accessed on 1 May 2025).
- Siren Care’s Neurofabric® (Diabetic Socks). 2022. Available online: https://www.siren.care/ (accessed on 1 May 2025).
- Sikka, M.; Garg, S.; Kumari, N. Bandages (Compression, Retention, and Support). In Textile Materials for Good Health and Wellbeing: Design and Applications; Springer: Berlin/Heidelberg, Germany, 2024; pp. 155–170. [Google Scholar]
- Cenzato, N.; Di Iasio, G.; Martìn Carreras-Presas, C.; Caprioglio, A.; Del Fabbro, M. Materials for Clear Aligners—A Comprehensive Exploration of Characteristics and Innovations: A Scoping Review. Appl. Sci. 2024, 14, 6533. [Google Scholar] [CrossRef]
- Li, C.-H.; Zuo, J.-L. Self-Healing Polymers Based on Coordination Bonds. Adv. Mater. 2020, 32, 1903762. [Google Scholar] [CrossRef]
- Peng, Y.; Gu, S.; Wu, Q.; Xie, Z.; Wu, J. High-Performance Self-Healing Polymers. Acc. Mater. Res. 2023, 4, 323–333. [Google Scholar] [CrossRef]
- Blaiszik, B.J.; Kramer, S.L.B.; Olugebefola, S.C.; Moore, J.S.; Sottos, N.R.; White, S.R. Self-Healing Polymers and Composites. Annu. Rev. Mater. Res. 2010, 40, 179–211. [Google Scholar] [CrossRef]
- Zhu, Z.; Tian, Z.; Zhang, F.; Li, Z.; Yang, D. Self-Healing Waterborne Polyurethane-Based Wearable Sensors with Excellent Thermal Management and Electromagnetic Interference Shielding for Advanced Biometric Gait Recognition. Adv. Funct. Mater. 2025, e11461. [Google Scholar] [CrossRef]
- Jung, J.; Lee, S.; Kim, H.; Lee, W.; Chong, J.; You, I.; Kang, J. Self-healing electronic skin with high fracture strength and toughness. Nat. Commun. 2024, 15, 9763. [Google Scholar] [CrossRef]
- Rahman, M.W.; Shefa, N.R. Minireview on Self-Healing Polymers: Versatility, Application, and Prospects. Adv. Polym. Technol. 2021, 2021, 7848088. [Google Scholar] [CrossRef]
- Sun, M.; Lu, T.; Zhou, Y.; Chen, Y.; Tu, W.; Zhang, C.; Ni, Z.; Li, X.; Hu, T. Structural engineering and 3D printing of highly stretchable strain sensors for smart wearable systems. Chem. Eng. J. 2025, 518, 164611. [Google Scholar] [CrossRef]
- Liu, P.; Chu, C.; Qiu, W.; Cheng, L.; Gu, J.; Mao, Z.; Zhao, Z.; He, X.; Liu, G.; Peng, C.; et al. 3D/4D printed versatile fibre-based wearables for embroidery, AIE-chemosensing, and unidirectional draining. Aggregate 2024, 5, e521. [Google Scholar] [CrossRef]
- XSensio. Lab-on-Skin™ for Next-Generation Wearables. Available online: https://xsensio.com/lab-on-skin-technology/ (accessed on 5 July 2025).
- Zeng, L.; Chen, L.; Lin, J.; Lin, J.; Wu, Y.; Wang, Y.; Luo, Z.; Huang, F.; Chen, D. Glow-Worm-Inspired Fluorescent Self-Healing Actuators for Soft Robot and Reconfigurable Information Encryption. Adv. Mater. 2025, 37, 2501007. [Google Scholar] [CrossRef] [PubMed]
- Sheikhi, M.; Vakili, S.; Karimi, N.; Rafiemanzelat, F.; Maleki, A.; Taheri, A.; Mohamadnia, Z.; Ramazani, A. 4D printing of self-healing, thermally, and near-infrared light-responsive granular hydrogels with segmental directed movement for soft robotic. ACS Appl. Polym. Mater. 2025, 7, 1717–1728. [Google Scholar] [CrossRef]
- Aydin, G.; Abdullah, T.; Okay, O. 4D printing of self-healing and shape-memory hydrogels sensitive to body temperature. Eur. Polym. J. 2025, 223, 113651. [Google Scholar] [CrossRef]
- Massachusetts Institute of Technology, Self-Assembly Lab. A Research Lab at MIT Inventing Self-Assembly and Programmable Material Technologies. Available online: https://selfassemblylab.mit.edu/ (accessed on 11 May 2025).
- Zhao, M.; Zhou, Z.; Sherchan, A.; Yuan, W.; Xie, X.; Li, M. An Innovative Delivery System of Oxygen-Releasing Nanospheres and Self-Healing Hydrogels Enhances the Therapeutic Effectiveness of Bone Marrow Mesenchymal Stem Cells for Chronic Limb-Threatening Ischemia. Int. J. Nanomed. 2024, 19, 12153–12170. [Google Scholar] [CrossRef]
- Creager, M.A.; Kaufman, J.A.; Conte, M.S. Acute limb ischemia. New Engl. J. Med. 2012, 366, 2198–2206. [Google Scholar] [CrossRef]
- Lin, D.; Li, M.; Wang, L.; Cheng, J.; Yang, Y.; Wang, H.; Ye, J.; Liu, Y. Multifunctional Hydrogel Based on Silk Fibroin Promotes Tissue Repair and Regeneration. Adv. Funct. Mater. 2024, 34, 2405255. [Google Scholar] [CrossRef]
- SFU. Stratasys US & Canada. Available online: https://www.stratasys.com/en/ (accessed on 11 May 2025).
- Project NASA Langley Research Center. Mars Ice Home. Available online: https://www.spacexarch.com/mars-ice-home (accessed on 11 May 2025).
- Athinarayanarao, D.; Prod’hon, R.; Chamoret, D.; Qi, H.J.; Bodaghi, M.; André, J.-C.; Demoly, F. Computational design for 4D printing of topology optimized multi-material active composites. NPJ Comput. Mater. 2023, 9, 1. [Google Scholar] [CrossRef]
- Amisha; Thakur, S.; Singh, A. Photo Responsive Material for 4D Printing in Tissue Engineering. In Engineered Biomaterials: Synthesis and Applications; Springer: Berlin/Heidelberg, Germany, 2023; pp. 429–463. [Google Scholar]
- Momeni, F.; Hassani, S.M.M.; Liu, X.; Ni, J. A review of 4D printing. Mater. Des. 2017, 122, 42–79. [Google Scholar] [CrossRef]
- Bodaghi, M.; Wang, L.; Zhang, F.; Liu, Y.; Leng, J.; Xing, R.; Dickey, M.D.; Vanaei, S.; Elahinia, M.; Hoa, S.V.; et al. 4D printing roadmap. Smart Mater. Struct. 2024, 33, 113501. [Google Scholar] [CrossRef]
- Emelogu, A.; Marufuzzaman, M.; Thompson, S.M.; Shamsaei, N.; Bian, L. Additive manufacturing of biomedical implants: A feasibility assessment via supply-chain cost analysis. Addit. Manuf. 2016, 11, 97–113. [Google Scholar] [CrossRef]
- Lee, S.; Kwon, H.; Jung, S.-Y.; Shin, H.-J.; Kwon, C.-Y.; Kim, J.-H. Pressures monitored by 3D printed capacitive pressure sensor embedded on prosthetic upper-limb socket; a case study. J. Biomech. Sci. Eng. 2021, 16, 21-00077. [Google Scholar] [CrossRef]
- Rafiee, M.; Farahani, R.D.; Therriault, D. Multi—Material 3D and 4D printing: A survey. Adv. Sci. 2020, 7, 1902307. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Wu, W. Ink-Based Additive Nanomanufacturing of Functional Materials for Human-Integrated Smart Wearables. Adv. Intell. Syst. 2020, 2, 2000117. [Google Scholar] [CrossRef]
- Zhang, H.; Wen, H.; Zhu, J.; Xia, Z.; Zhang, Z. 3D printing dielectric elastomers for advanced functional structures: A mini-review. J. Appl. Polym. Sci. 2024, 141, e55015. [Google Scholar] [CrossRef]
- Quan, R.; Chinchilla, S.C.; Nassehi, A.; Liu, F. Machine Learning-Driven Optimization of 3D Printing Parameters for PLA Bone Scaffolds with Enhanced Mechanical Properties. Procedia CIRP 2024, 125, 255–259. [Google Scholar] [CrossRef]
- Steer, J.; Grudniewski, P.; Browne, M.; Worsley, P.; Sobey, A.; Dickinson, A. Predictive prosthetic socket design: Part 2—Generating person-specific candidate designs using multi-objective genetic algorithms. Biomech. Model. Mechanobiol. 2020, 19, 1347–1360. [Google Scholar] [CrossRef]
- Mikołajewska, E.; Mikołajewski, D.; Mikołajczyk, T.; Paczkowski, T. A Breakthrough in Producing Personalized Solutions for Rehabilitation and Physiotherapy Thanks to the Introduction of AI to Additive Manufacturing. Appl. Sci. 2025, 15, 2219. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).