Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks
Abstract
1. Introduction
2. Methodology
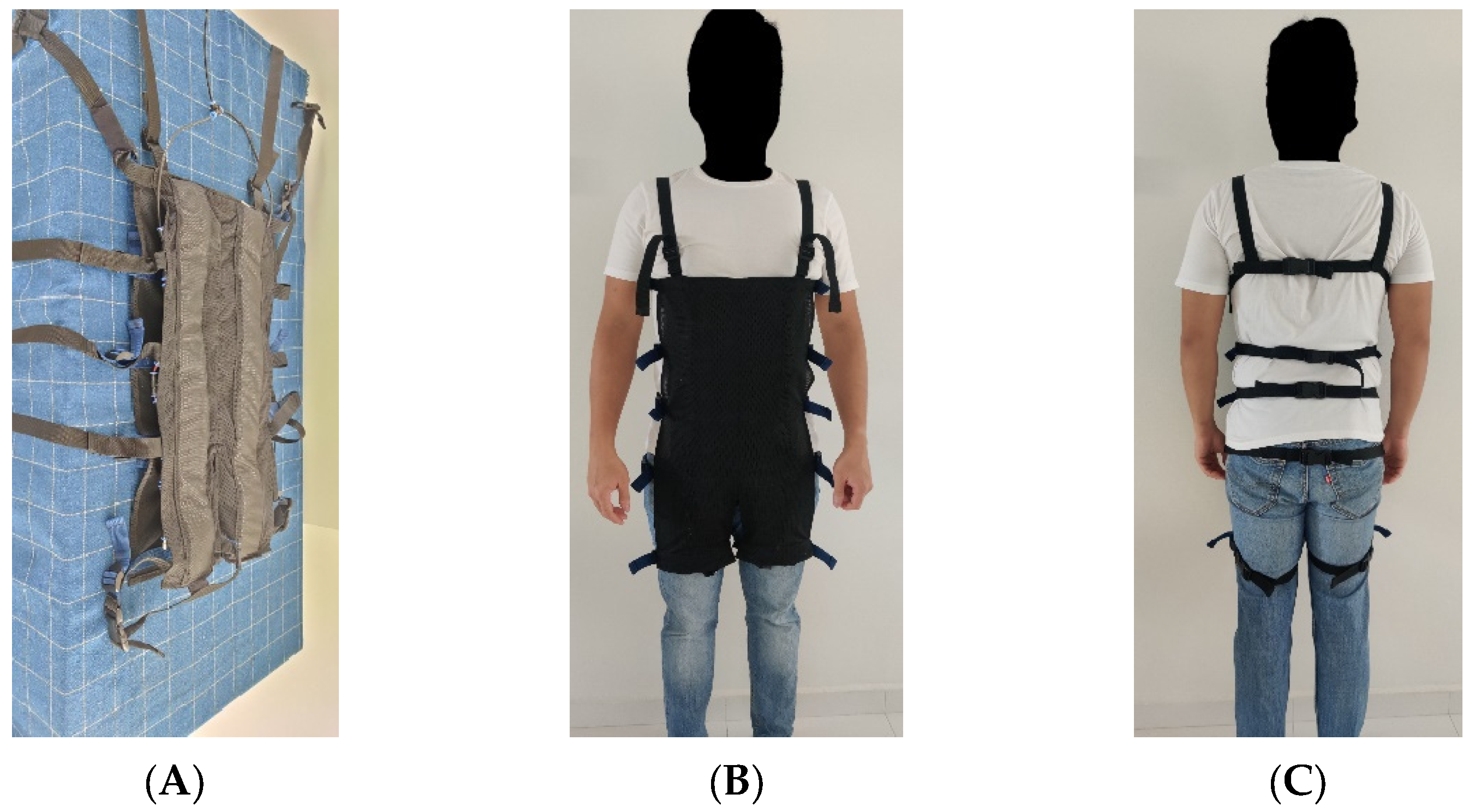
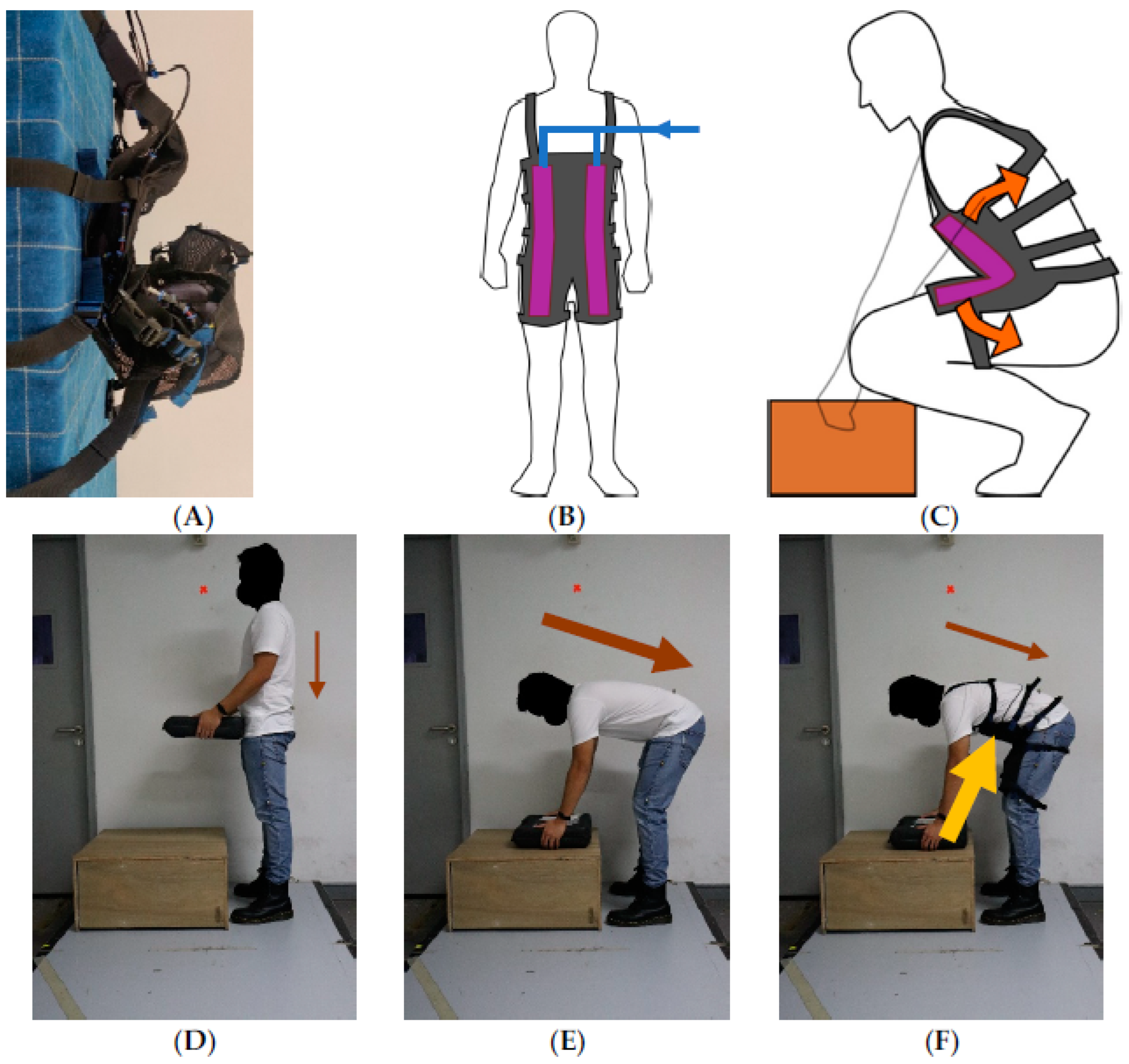
2.1. AireLevate Operation
2.2. Experiment Procedure
2.2.1. Participant Characteristics
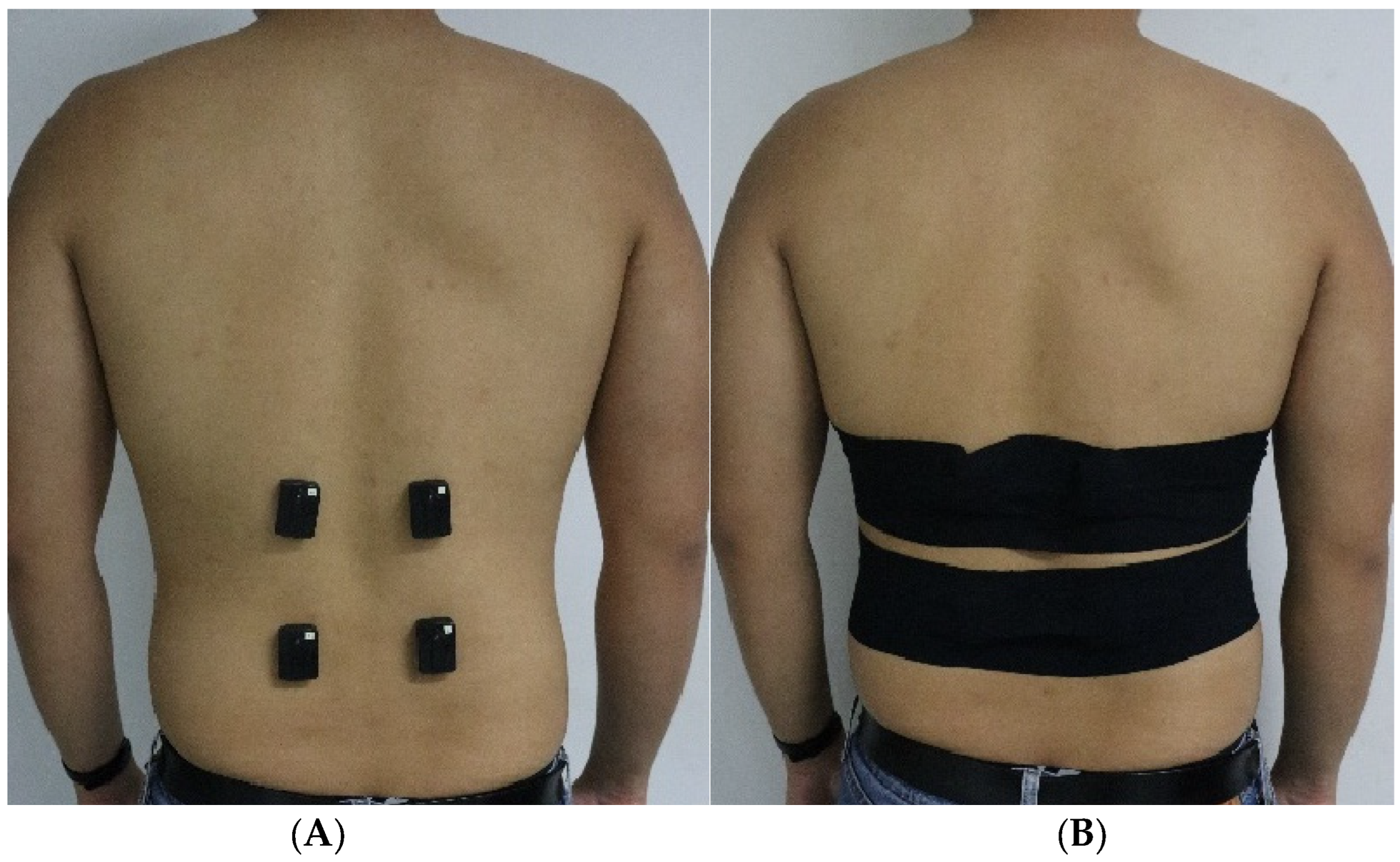
2.2.2. Application of Suit and Sensors
2.2.3. Circuit of Lifting Tasks
2.3. Data Processing
2.4. Data Analysis
3. Results
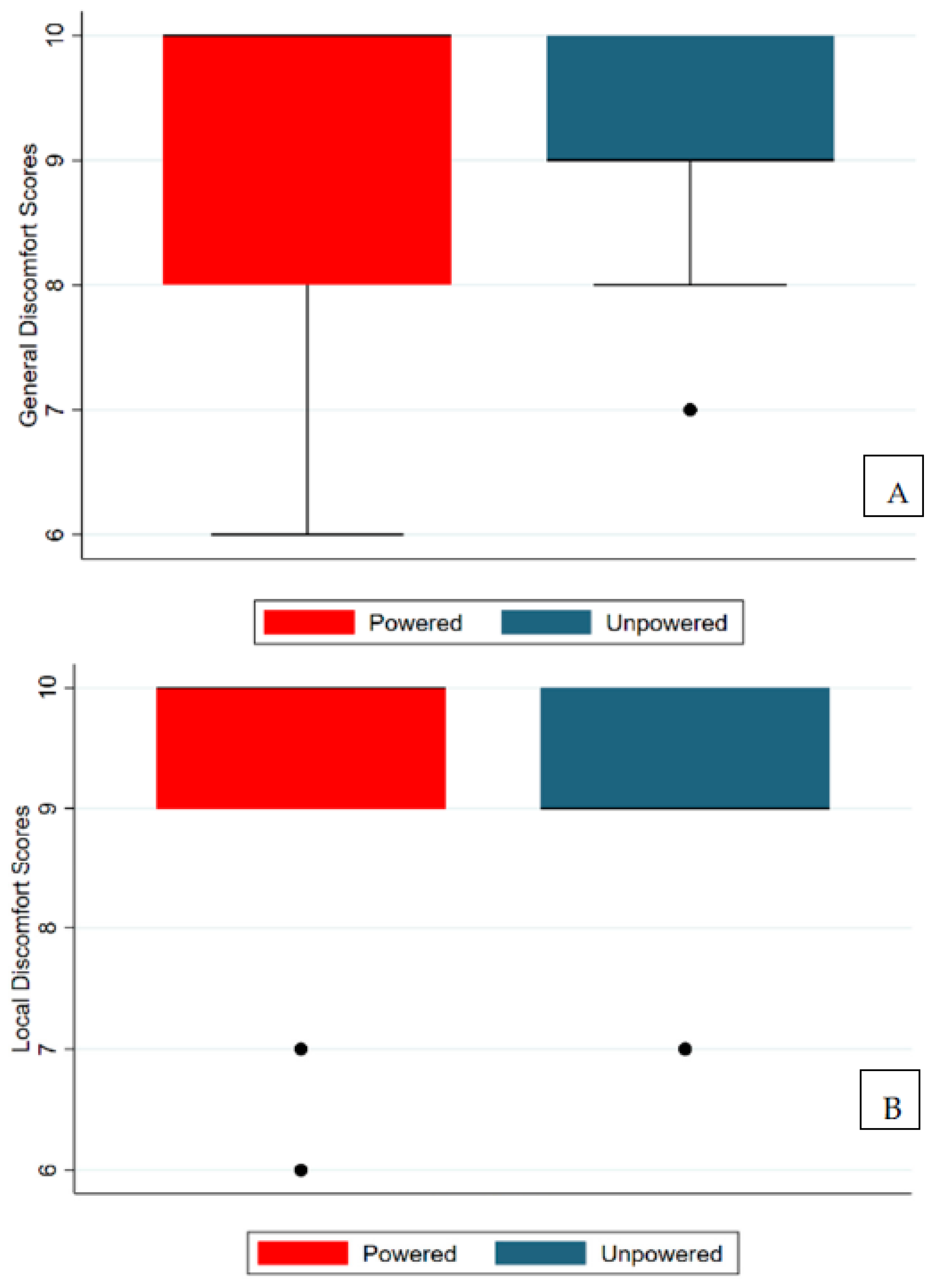
3.1. Qualitative Measures
3.2. Range of Motion
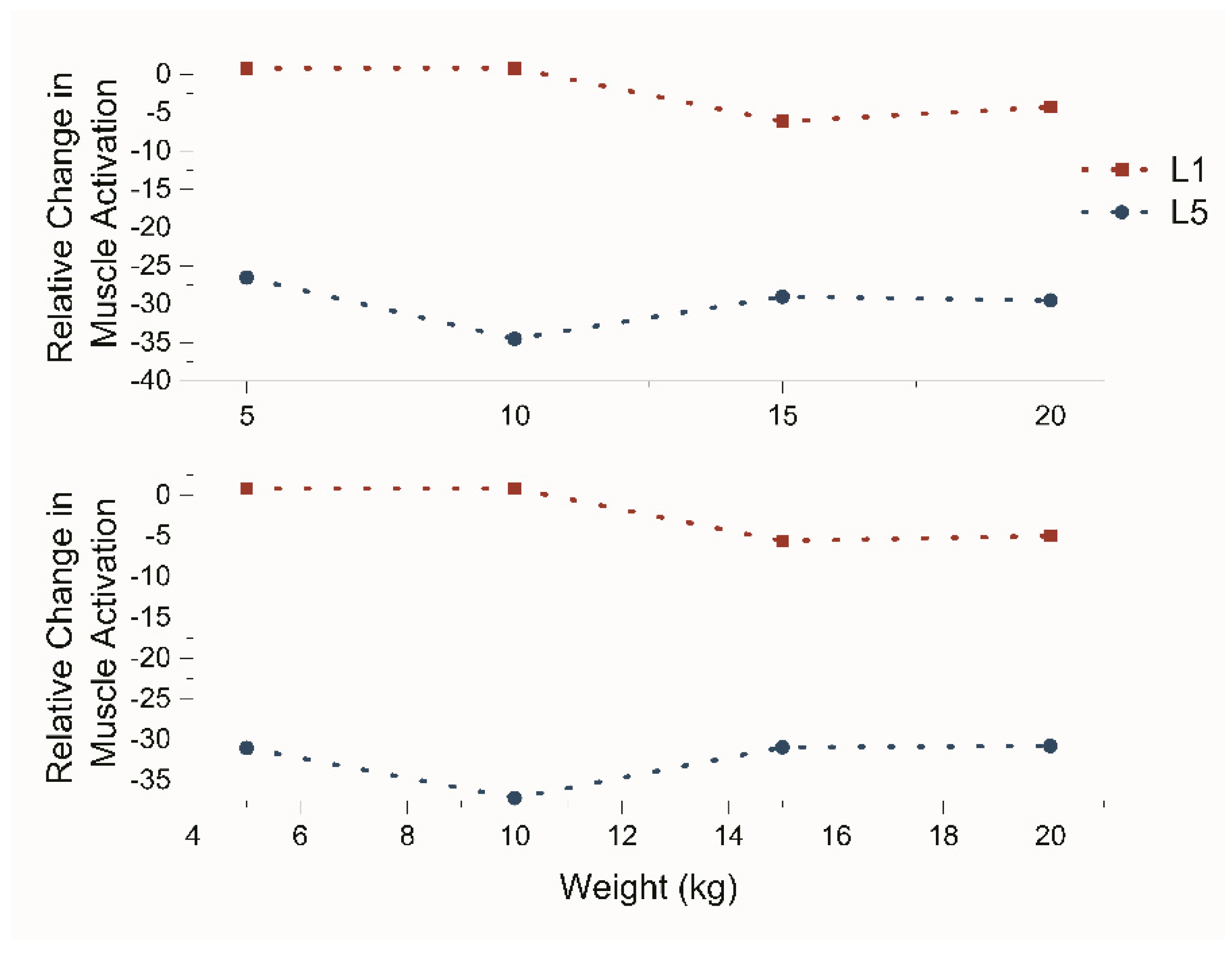
3.3. Reduction in Muscle Activation
3.4. Effect on Left Side and Right Side
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alnefaie, M.; Alamri, A.; Hariri, A.; Alsaad, M.; Alsulami, A.; Abbas, A.; Alfozan, A.; Aljiffry, M.; Abbadi, H. Musculoskeletal Symptoms Among Surgeons at a Tertiary Care Center: A Survey Based Study. Med. Arch. 2019, 73, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Abdul Monem, A.; Nizar, A.; Abdullaha, A. Prevalence and Associated Factors of Low Back Pain among Clinicians of A Major Referral Hospital. Med. J. Malays. 2015, 70, 12–17. [Google Scholar]
- Meisha, D.E.; Alsharqawi, N.S.; Samarah, A.A.; Al-Ghamdi, M.Y. Al-Ghamdi Prevalence of work-related musculoskeletal disorders and ergonomic practice among dentists in Jeddah, Saudi Arabia. Clin. Cosmet. Investig. Dent. 2019, 11, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G.; Burton, A.K.; Main, C.J. Screening to Identify People at Risk of Long-Term Incapacity for Work: A Conceptual and Scientific Review; Royal Society of Medicine Press: London, UK, 2003; Available online: www.rsmpress.co.uk (accessed on 20 August 2022).
- Punnett, L.; Prüss-Ütün, A.; Nelson, D.I.; Fingerhut, M.A.; Leigh, J.; Tak, S.; Phillips, S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am. J. Ind. Med. 2005, 48, 459–469. [Google Scholar] [CrossRef]
- Kofi, M.; Abbas, M.A.F.; Lamiaa, Z.; Abu Zaid, A.; Fiala; Alhamdan, N.A. Prevalence and Risk Factors of Low Back Pain among Nurses in Four Tertiary Care Hospitals at King Fahad Medical City, Riyadh, KSA. 2010. Available online: www.medicaljournalofcairouniversity.comwww.medicaljournalofcairouniversity.com (accessed on 20 August 2022).
- Al Dajah, S.; Abdalhamed, H.; Daghdi, A. Prevalence and risk factors of low back pain among nurses in sudayr region. Eur. Sci. J. 2013, 9, 1857–7881. [Google Scholar]
- Al-Eisa, E.; Al-Abbad, H. Occupational Back Pain among Rehabilitation Nurses in Saudi Arabia. Workplace Health Saf. 2013, 61, 401–407. [Google Scholar] [CrossRef]
- Croft, P.R.; Macfarlane, G.J.; Papageorgiou, A.C.; Thomas, E.; Silman, A.J. General practice Outcome of low back pain in general practice: A prospective study. BMJ 1998, 316, 1356–1359. Available online: www.bmj.com (accessed on 20 August 2022). [CrossRef]
- Hestbaek, L.; Leboeuf-Yde, C.; Manniche, C. Low back pain: What is the long-term course? A review of studies of general patient populations. Eur. Spine J. 2003, 12, 149–165. [Google Scholar] [CrossRef]
- Andini, F. Risk Factors of Low Back Pain in Workers. J. Major. 2015, 4. [Google Scholar]
- Publications Office of the European Union. Fifth European Working Conditions Survey—Overview Report; Publications Office of the European Union: Luxembourg, 2012. [Google Scholar]
- Iles, R.A.; Davidson, M.; Taylor, N.F. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: A systematic review. Occup. Environ. Med. 2008, 65, 507–517. [Google Scholar] [CrossRef]
- Steenstra, I.A.; Verbeek, J.H.; Heymans, M.W.; Bongers, P.M. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature. Occup. Environ. Med. 2005, 62, 851–860. [Google Scholar] [CrossRef] [PubMed]
- De Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Murashov, V.; Lowe, B.D.; Lu, M.L. Industrial exoskeletons: Need for intervention effectiveness research. Am. J. Ind. Med. 2020, 63, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Kermavnar, T.; de Vries, A.W.; de Looze, M.P.; O’Sullivan, L.W. Effects of industrial back-support exoskeletons on body loading and user experience: An updated systematic review. Ergonomics 2021, 64, 685–711. [Google Scholar] [CrossRef]
- Bosch, T.; van Eck, J.; Knitel, K.; de Looze, M. The effects of a passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Appl. Ergon. 2016, 54, 212–217. [Google Scholar] [CrossRef]
- Gopura, R.A.R.C.; Bandara, D.S.V.; Kiguchi, K.; Mann, G.K.I. Developments in hardware systems of active upper-limb exoskeleton robots: A review. Rob. Auton. Syst. 2016, 75, 203–220. [Google Scholar] [CrossRef]
- Ali, A.; Fontanari, V.; Schmoelz, W.; Agrawal, S.K. Systematic Review of Back-Support Exoskeletons and Soft Robotic Suits. Front. Bioeng. Biotechnol. 2021, 9, 1027. [Google Scholar] [CrossRef]
- Shirazi-Adl, A.; El-Rich, M.; Pop, D.G.; Parnianpour, M. Spinal muscle forces, internal loads and stability in standing under various postures and loads—Application of kinematics-based algorithm. Eur. Spine J. 2004, 14, 381–392. Available online: https://www.academia.edu/12685444/Spinal_muscle_forces_internal_loads_and_stability_in_standing_under_various_postures_and_loads_application_of_kinematics_based_algorithm (accessed on 19 September 2022). [CrossRef]
- Hara, H.; Sankai, Y. Development of HAL for Lumbar Support. In Proceedings of the Joint 5th International Conference on Soft Computing and Intelligent Systems and 11th International Symposium on Advanced Intelligent Systems (SCIS & ISIS 2010), Okayama, Japan, 8–10 December 2010; pp. 416–421. [Google Scholar]
- Yong, X.; Yan, Z.; Wang, C.; Wang, C.; Li, N.; Wu, X. Ergonomic mechanical design and assessment of a waist assist exoskeleton for reducing lumbar loads during lifting task. Micromachines 2019, 10, 463. [Google Scholar] [CrossRef]
- Ko, H.K.; Lee, S.W.; Koo, D.H.; Lee, I.; Hyun, D.J. Waist-assistive exoskeleton powered by a singular actuation mechanism for prevention of back-injury. Rob. Auton. Syst. 2018, 107, 1–9. [Google Scholar] [CrossRef]
- Technology—Verve Motion. Available online: https://vervemotion.com/technology/ (accessed on 31 August 2022).
- Madinei, S.; Alemi, M.M.; Kim, S.; Srinivasan, D.; Nussbaum, M.A. Biomechanical assessment of two back-support exoskeletons in symmetric and asymmetric repetitive lifting with moderate postural demands. Appl. Ergon. 2020, 88, 103156. [Google Scholar] [CrossRef]
- Lamers, E.P.; Yang, A.J.; Zelik, K.E. Feasibility of a biomechanically-assistive garment to reduce low back loading during leaning and lifting. In IEEE Transactions on Biomedical Engineering; IEEE Computer Society United States of America: Washington, DC, USA, 2018; Volume 65, pp. 1674–1680. [Google Scholar] [CrossRef]
- LiftSuit|Auxivo. Available online: https://www.auxivo.com/liftsuit (accessed on 31 August 2022).
- Ide, M.; Hashimoto, T.; Matsumoto, K.; Kobayashi, H. Evaluation of the Power Assist Effect of Muscle Suit for Lower Back Support. IEEE Access 2021, 9, 3249–3260. [Google Scholar] [CrossRef]
- Inose, H.; Mohri, S.; Arakawa, H.; Okui, M.; Koide, K.; Yamada, Y.; Kikutani, I.; Nakamura, T. Semi-endoskeleton-type waist assist AB-wear suit equipped with compressive force reduction mechanism. In Proceedings of the 2017 IEEE International Conference on Robotics and Automation (ICRA), Singapore, 29 May–3 June 2017; pp. 6014–6019. [Google Scholar] [CrossRef]
- Veale, A.J.; Xie, S.Q. Towards compliant and wearable robotic orthoses: A review of current and emerging actuator technologies. Med. Eng. Phys. 2016, 38, 317–325. [Google Scholar] [CrossRef]
- Natividad, R.F.; Miller-Jackson, T.; Chen-Hua, R.Y. A 2-DOF Shoulder Exosuit Driven by Modular, Pneumatic, Fabric Actuators. IEEE Trans. Med. Robot. Bionics 2020, 3, 166–178. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Vera-Garcia, F.J.; Moreside, J.M.; McGill, S.M. MVC techniques to normalize trunk muscle EMG in healthy women. J. Electromyogr. Kinesiol. 2010, 20, 10–16. [Google Scholar] [CrossRef]
- Health and Safety Executive Manual Handling at Work: A Brief Guide. 2020. Available online: https://books.hse.gov.uk/ (accessed on 20 August 2022).
- Merletti, R.; Di Torino, P.J.J.E.K. Standards for Reporting EMG Data. J. Electromyogr. Kinesiol. 1999, 9, 3–4. [Google Scholar]
- Sposito, M.; di Natali, C.; Toxiri, S.; Caldwell, D.G.; de Momi, E.; Ortiz, J. Exoskeleton kinematic design robustness: An assessment method to account for human variability. Wearable Technol. 2020, 1, e7. [Google Scholar] [CrossRef]
- Xiao, J.; Gao, J.; Wang, H.; Liu, K.; Yang, X. The Surface EMG Characteristics between Erector Spinae and Vastus Lateralis during Bending Forward and Squatting Down Tasks. Physiol. J. 2015, 2015, 537379. [Google Scholar] [CrossRef]
- Von Glinski, A.; Yilmaz, E.; Mrotzek, S.; Marek, E.; Jettkant, B.; Brinkemper, A.; Fisahn, C.; Schildhauer, T.A.; Geßmann, J. Effectiveness of an on-body lifting aid (HAL® for care support) to reduce lower back muscle activity during repetitive lifting tasks. J. Clin. Neurosci. 2019, 63, 249–255. [Google Scholar] [CrossRef]
- National Safety Council. Know the Facts about Backs [Fact Sheet]. National Safety Council, United States of America. 2019. Available online: https://injuryfacts.nsc.org/ (accessed on 20 August 2022).
- Mazis, N. Does a History of Non Specific Low Back Pain Influence Electromyographic Activity of the Erector Spinae Muscle Group during Functional Movements? J. Nov. Physiother. 2014, 4, 226. [Google Scholar] [CrossRef]
- Kordt, M.; Marschall, J.; Hildebrandt-Heene, S.; Zich, K.; Sörensen, J.; Nolting, H.-D. Deutsche Angestellten-Krankenkasse-Gesundheitsreport 2018, Medhochzwei. 2018. Available online: https://www.dak.de/dak/download/gesundheitsreport-2018-pdf-2073702.pdf (accessed on 5 April 2023).
- Mehra, M.; Hill, K.; Nicholl, D.; Schadrack, J. The burden of chronic low back pain with and without a neuropathic component: A healthcare resource use and cost analysis. J. Med. Econ. 2012, 15, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Kim, L.H.; Vail, D.; Azad, T.D.; Bentley, J.P.; Zhang, Y.; Ho, A.L.; Fatemi, P.; Feng, A.; Varshneya, K.; Desai, M.; et al. Expenditures and health care utilization among adults with newly diagnosed lowback and lower extremity pain. JAMA Netw. Open 2019, 2, e193676. [Google Scholar] [CrossRef]
- Hargreaves, M.; Spriet, L.L. Author Correction: Skeletal muscle energy metabolism during exercise. Nat. Metab. 2020, 2, 817–828, Erratum in Nat. Metab. 2020, 2, 990. [Google Scholar] [CrossRef]
- Tsianos, G.A.; MacFadden, L.N. Validated Predictions of Metabolic Energy Consumption for Submaximal Effort Movement. PLoS Comput. Biol. 2016, 12, e1004911. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Nussbaum, M.A.; Esfahani, M.I.M.; Alemi, M.M.; Jia, B.; Rashedi, E. Assessing the influence of a passive, upper extremity exoskeletal vest for tasks requiring arm elevation: Part II—‘Unexpected’ effects on shoulder motion, balance, and spine loading. Appl. Ergon. 2018, 70, 323–330. [Google Scholar] [CrossRef]
- Weston, E.B.; Alizadeh, M.; Knapik, G.G.; Wang, X.; Marras, W.S. Biomechanical evaluation of exoskeleton use on loading of the lumbar spine. Appl. Ergon. 2018, 68, 101–108. [Google Scholar] [CrossRef]


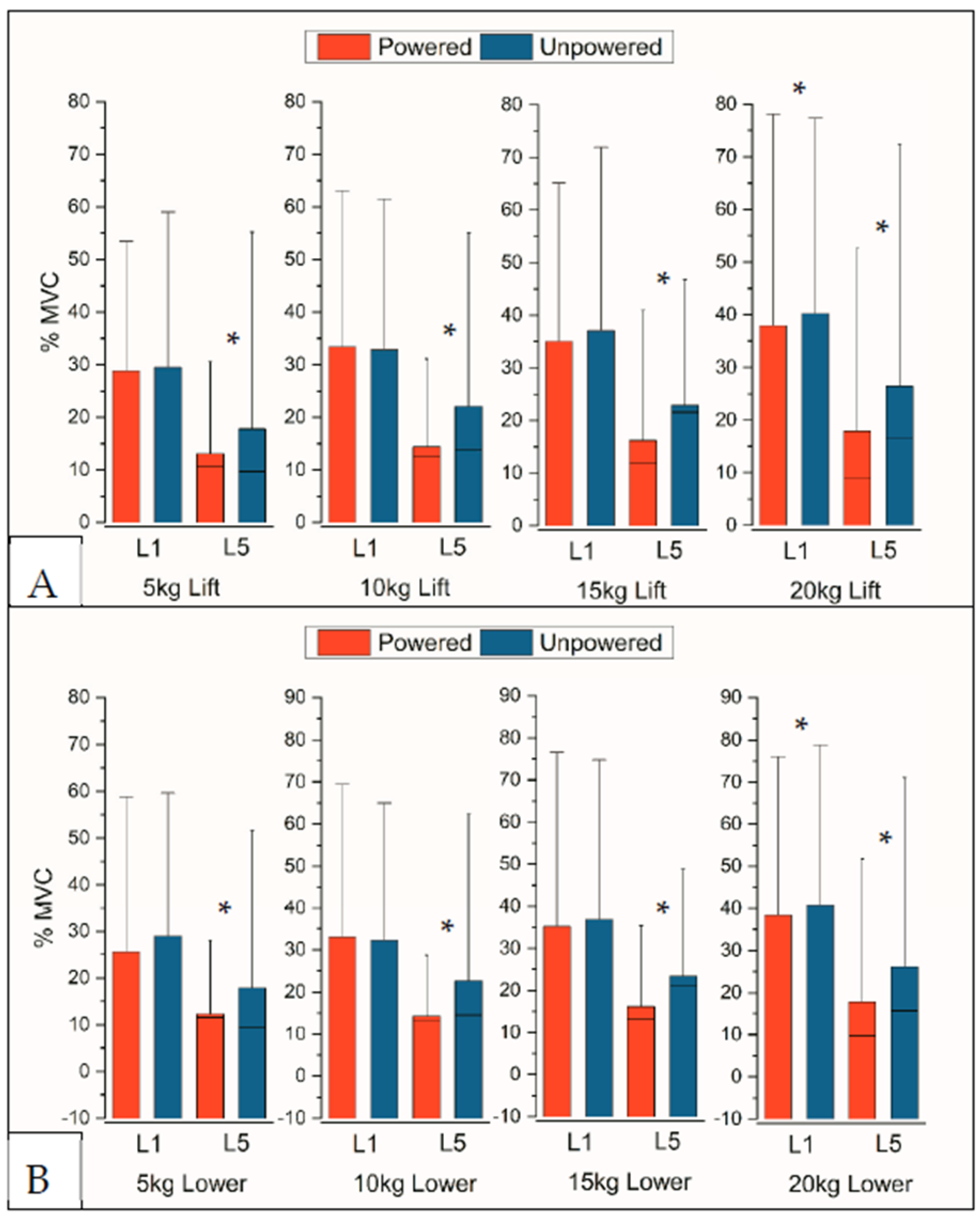
| Lifting Motions | Lowering Motions | |||
|---|---|---|---|---|
| Weight | Left L-5 | Right L-5 | Left L-5 | Right L-5 |
| 5 kg | −54% (0.01) | −9% (0.01) | −50% (0.02) | −19% (0.01) |
| 10 kg | −63% (<0.005) | −9% (0.03) | −63% (<0.005) | −14% (0.09) |
| 15 kg | −61% (<0.005) | 0% (0.07) | −61% (<0.005) | −4% (0.07) |
| 20 kg | −55% (<0.005) | −7% (0.14) | −56% (<0.005) | −8% (0.15) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuttilan, A.N.; Natividad, R.F.; Yeow, R.C.-H. Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks. Actuators 2023, 12, 273. https://doi.org/10.3390/act12070273
Cuttilan AN, Natividad RF, Yeow RC-H. Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks. Actuators. 2023; 12(7):273. https://doi.org/10.3390/act12070273
Chicago/Turabian StyleCuttilan, Amit Nirmal, Rainier F. Natividad, and Raye Chen-Hua Yeow. 2023. "Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks" Actuators 12, no. 7: 273. https://doi.org/10.3390/act12070273
APA StyleCuttilan, A. N., Natividad, R. F., & Yeow, R. C.-H. (2023). Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks. Actuators, 12(7), 273. https://doi.org/10.3390/act12070273






