1. Introduction
Robots in rehabilitation are a relatively young field (beginning in the early 1990s), and currently their clinical application is increasing. The main purpose of introducing robots was to support therapy by increasing its intensity (number of repetitions per unit of time) and relieving physiotherapists [
1]. In terms of improving the lower limb, the development of robots was initiated by the LOKOMAT system as a support for gait re-education in the patient’s body relief system. In patients with damage to the central nervous system (CNS), the goal of therapy will not be to restore normal movement patterns, but to achieve the maximum mobility and daily activities of the patient. In some patients with CNS damage, motor deficits are so serious that their prognosis is poor as to their return to independence. In this case, the essence of therapy will be to counteract the effects of prolonged immobilization. The advantage of robot-assisted therapy is its repeatability, as well as the ability to plan the exact number of repetitions per unit of time, often along with the speed of the performed movement task. The assumptions of neurological rehabilitation are based on the basics of neuroanatomy and physiology. Therapy with the use of a robot is intended to help mobilize the nervous system through repetitive time summation, which is part of the process of neuroplasticity [
2,
3,
4,
5].
One of the concepts of rehabilitation in patients with CNS damage is Proprioception Neuromuscular Facilitation (PNF). This method, although created in the 1930s, is still successfully used by physiotherapists all over the world [
6,
7,
8,
9]. The concept is based on neurophysiological therapeutic interactions: proprioceptive stimulation (concerning body receptors) and neuromuscular facilitation. By restoring lost function, the physiotherapist paves the way for natural movements that run in three planes, along the diagonals. By maintaining the oblique axis of movement, as many muscles as possible from the same muscle chain are activated. Thus, it is a reproduction of the natural movement of the patient, performed during everyday activities [
10]. PNF therapy distinguishes movement patterns for the trunk, upper limbs, and lower limbs. Two patterns of the lower limb are used to teach gait, for the support phase and for the transfer phase, respectively: extension–abduction–internal rotation; and flexion–adduction–external rotation with knee flexion [
11]. So far, the “neuro-robotics” field has largely used one-plane movement, which is not identical with natural human movement.
Collaborative robots (cobots) are rapidly gaining recognition within the field of rehabilitation and provide a novel, innovative approach to assisting people with neurological conditions to regain their mobility and independence. Cobots have specifically demonstrated considerable promise in the rehabilitation of neurological diseases affecting the lower limbs, such as stroke and spinal cord injuries. Cobots are robots made specifically to cooperate with people in the workplace. They are intended to engage with humans and help them with a variety of jobs, as opposed to typical robots that are kept apart from human touch. They are frequently more flexible, lighter, and smaller than traditional robots, which makes them perfect for usage in patient care where they may assist patients in regaining their independence and mobility. With the use of cobots, patients in rehabilitation may relearn how to move their feet and legs through a technique known as gait training. Gait training entails doing various exercises and motions to assist patients in regaining control of their lower limbs, enhancing their balance, and developing strength. Cobots are perfect for this procedure because they can give patients focused support and feedback, enabling them to make the proper motions and advance in reaching their rehabilitation goals. Cobots provide a potential new approach to assisting people with neurological disorders to regain their physical capacity. They can assist patients with achieving their rehabilitation objectives and regaining their quality of life by offering focused assistance, adaptable training, and real-time feedback.
This study analyzed the possibility of adapting the universal robot to perform rehabilitation with the patient. The authors made a comparative analysis of the performance of the robot in relation to the physiotherapist. The following kinematic parameters were analyzed: hip flexion and abduction angles; knee flexion and rotation angles; ankle dorsiflexion angle; and motion cycle time. These parameters all may affect the quality of therapy.
2. Materials and Methods
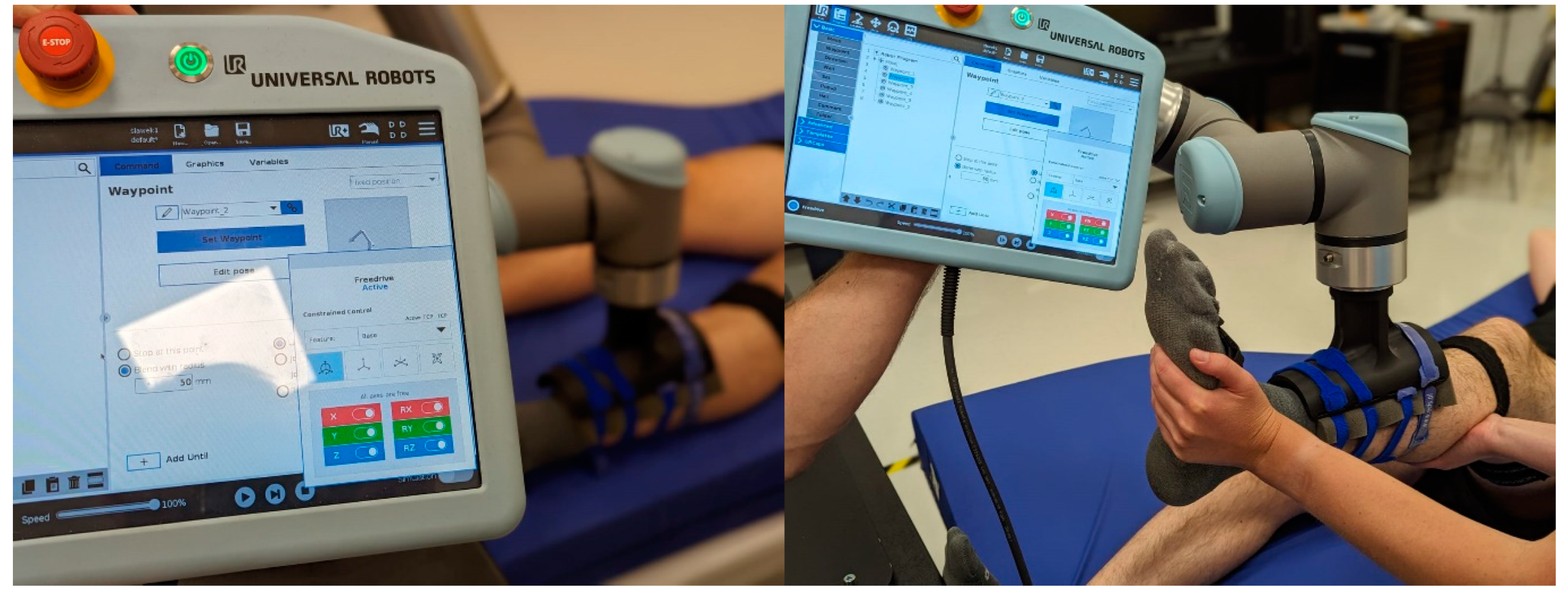
Experimental studies were carried out using the UR10e cobot and the Noraxon MyoMotion system consisting of seven sensors. The sensors were located on the pelvis and right/left feet, thighs, and lower legs. The study was conducted in two stages. Each stage consisted of ten repeated movements from PNF and was performed twice. Before each stage, the Noraxon system was calibrated. The first stage consisted of performing the PNF movement ten times with the physiotherapist. The second stage began with the positioning of the UR10e robot (
Figure 1). A specially designed brace was attached to the robot and then to the lower limb with straps. The therapist, after examining the patient and making a decision on the method of rehabilitation, programmed a repetitive movement of the robotic arm (which in the classical approach would be performed by a human). The trajectory of this movement was programmed when the robot arm was already attached to the patient’s limb. The programming is done in Freedrive mode (
Figure 2) [
12]. In this mode, it is possible to physically grab the robotic arm and pull it to any desired location. The robot joints can be moved with relatively little force because the brakes are released. During the initialization of the robot arm, minor vibrations may be observed. The trajectory of the robotic arm was determined based on seven selected points. In the final stage, the therapist set other parameters such as movement speed, strength limit, and number of repetitions. The process takes place through sensing feedback, visual feedback, and communication with the patient. During the programming of the robot trajectory, all loops are preserved because the process is guided by the therapist. During the rehabilitation, when the robot takes over the process, key couplings are also maintained: the robot’s force/torque sensor protects against exceeding the limit value, and the patient has access to the emergency switch, which allows the process to be interrupted at his demand. The robot has a range of 1300 mm and a maximum payload of 12.5 kg, and its mass is 33.5 kg. The cobot has built-in force sensors that allow for setting the threshold at which the robot will automatically stop. The threshold has been set to the least restricted with a maximum tool force of 150 N. After starting the procedure, the role of the therapist is to supervise the course of the process.
3. Results
The obtained results are presented in
Table 1. The results were determined as the mean min (minimum) and max (maximum) values of the analyzed kinematic quantities, as well as the mean RoM (Range of Motion) and motion cycle time.
The values shown in
Table 1 represent the results for the two tests recorded when the physiotherapist performed PNF therapy and the two tests performed by the cobot.
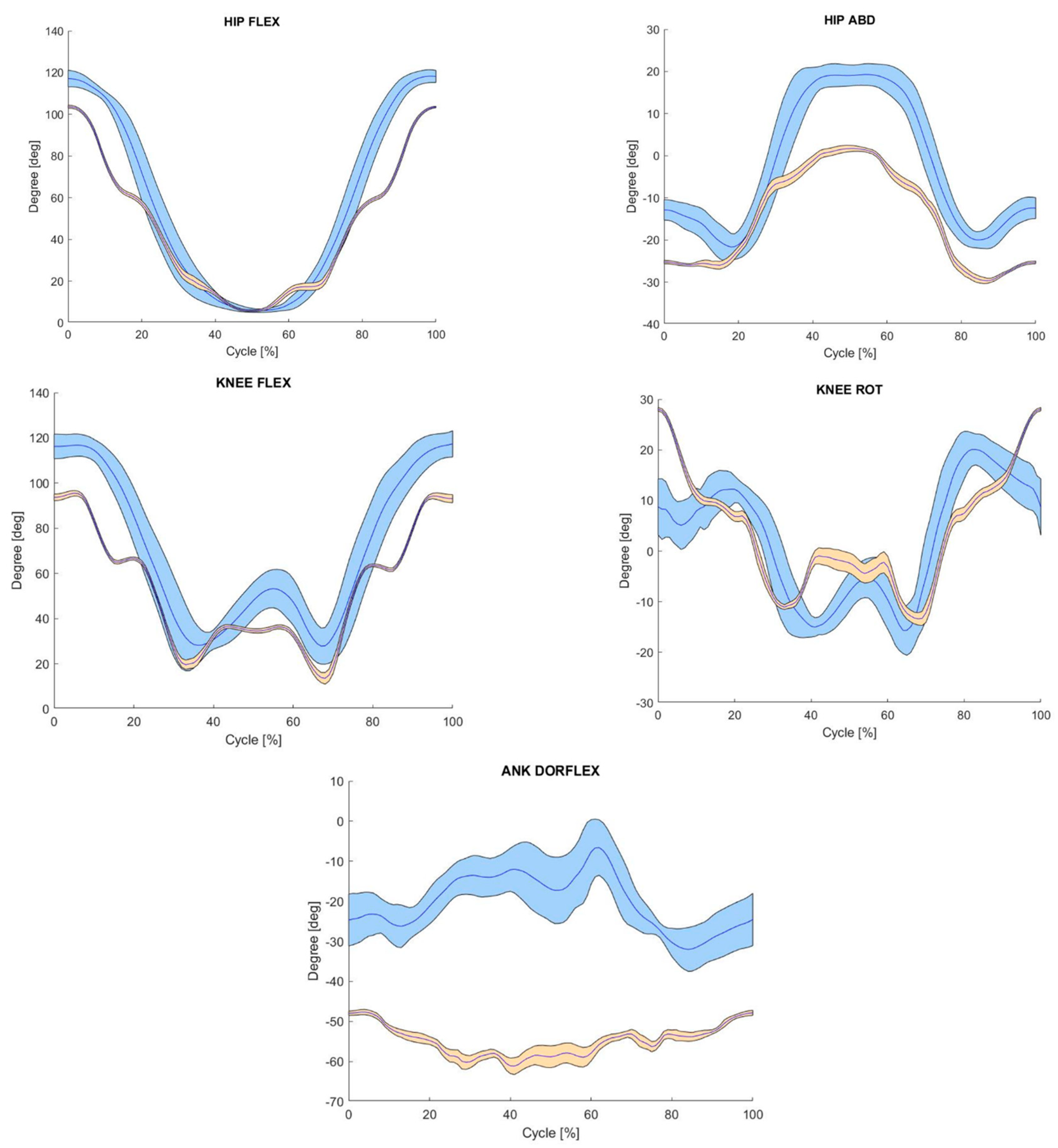
For hip flexion and extension, knee flexion, and ankle dorsiflexion, the RoM values obtained by the physiotherapist were greater than those obtained by the cobot. For hip flexion motion, the difference in range for the trials in which the mean value was highest was 13.54°, for hip flexion motion: 15.14°, while for flexion of the knee joint the differences were 9.5°. For the ankle joint, the largest differences in angular values were registered ranging from 12.25° to as much as 21.24°. These differences were due to the lack of a grasping point in this segment by the working end of the robotic arm. The ankle joint moved freely, and its movement was not forced in any way. Only in the case of knee joint rotation was a greater range of motion registered during the cobot exercise. In contrast, the value of the difference between the mean RoM was the smallest among the analyzed ranges of motion, at 3.76°. However, when comparing the ranges of motion between Test 1 and Test 2 performed by a physiotherapist or cobot, it can be seen that greater differences in values were found when exercising with a physiotherapist. Despite the assumption that the physiotherapist should perform the movements in the same way during therapy, the differences in RoM range from 1.54 ÷ 11.81°, while for the movement performed by the cobot, the range is smaller at 0.54 ÷ 6.45.
On the other hand, it is also worth noting the value of the standard deviation, which indicates the degree of repeatability of each movement cycle. For both mini-maximal, maximal, and RoM, the standard deviation was several times smaller during the movements performed by the cobot and its value was in the range of 0.23–2.36°, while for the exercises performed by the physiotherapist, the standard deviation range was 1.12–6.35°.
Comparing the duration of individual cycles in each trial, the time per cycle was four times greater for the cycle performed by the cobot compared to that performed by the physical therapist. The increased cycle time during the therapy performed by the cobot was solely due to the way it was programmed to adjust the exercise speed to the subject’s comfort. On the other hand, by comparing the cycle times between the two methods analyzed, it can be seen that the cycle time during therapy with the cobot was constant at 22.22 s, while during therapy with the physiotherapist it was 5.27 s in Test 1 and 4.78 s in Test 2 giving a difference of 0.49 s. Analyzing the standard deviation shows that during Test 1 performed by the physiotherapist, the std value was 0.15 s, suggesting that the individual cycles during this trial were performed with less temporal accuracy compared to the off-trials.
Figure 3 shows the waveforms of the averaged angular values registered at individual joints of the lower limbs. The blue waveform represents the movement performed by the physiotherapist, and the orange waveform shows the movement performed by the robot. By performing a qualitative analysis, it can be seen that the shapes of the individual waveforms are similar, which indicates the mapping of the PNF exercises by the cobot. On the other hand, a smaller range of deviation in the case of the exercises performed by the robot indicates the greater repeatability of each cycle of movement performed by the subject. In the case of the waveforms recorded during the robot tests, it can be noted that there is no smooth change of the angular values in individual joints as in the case of exercises with a physiotherapist. The occurring “staircase” visible especially during knee flexion is due to the determination of intermediate points of the movement trajectory while programming the robot.
Table 2 presents the results of the correlation analysis conducted between exercises by the physiotherapist and by the robot. The movement correlation analysis for individual joints showed similarities between human and robotic exercises. A strong correlation can be observed for the flexion movement in the hip joint, and a weak correlation for the adduction movement. The movement in the knee joint showed a moderate similarity. Ankle dorsiflexion showed a negative moderate correlation. Overall, these results are satisfactory.
The correlation of movements during the series of exercises performed by the physiotherapist (Test 1 physiotherapist vs. Test 2 physiotherapist) showed a very high similarity for each joint. An analogous comparison of a series of exercises performed by the robot (Test 1 cobot vs. Test 2 cobot) also showed a strong similarity with the exception of the hip abduction and ankle dorsiflexion movements, where a weak similarity was obtained.
This means that despite the lower repeatability of movements within a given series, a human controls the entire process better, while the robot offers very good repeatability within a series, but much depends on the stage of programming the movement. If at the programming stage there is a deviation from the expected trajectory, the robot will not correct this error but will repeat it.
4. Discussion
It is estimated that today one in three people live with a health condition that benefits from rehabilitation. This number has increased by 63% in almost 30 years (period: 1990–2019), which shows the need to increase accessibility, but also to improve and streamline the rehabilitation process [
13]. The main goals of the healthcare system include increasing the availability of rehabilitation services, increasing the efficiency of the physical therapist’s work, and especially reducing the cost of treatment [
14,
15]. One of the solutions to these problems could be the introduction of industrial cobots, suitable for performing rehabilitation exercises, for example, and integrated into the work of physical therapists.
In the literature, papers describe the use of industrial cobots in rehabilitation tasks. The authors mainly use Kuka robotic arms and universal robots. All papers deal with upper limb rehabilitation and focus on the use of robots as part of an adaptive system, even including force feedback as input into the algorithm. The mechanical interface between the patient’s limbs and the robotic arm varies in design, but interfaces based on the patient’s grip are the predominant solutions. The system presented by Papaleo, Zollo, Spedaliere et al. [
16] consists of a Kuka 7-DoF robotic arm, an adaptive interaction control system, and a patient performance evaluation module. The study goes into great detail about the adaptive interaction control system and the patient biomechanical state assessment module. Results in 2D and 3D space will be provided following experimental validation in healthy volunteers. The Universal RoboTrainer project also uses a cobot-based strategy for rehabilitation. The idea behind this technology, which uses a universal robot to train damaged upper limbs, is based on research demonstrating the value of repetitive motion in the treatment of functional disorders. Several experiments have already been conducted with this device [
17,
18]. Apollonio et al. [
19] presents an elastic system for rehabilitation that incorporates several learning algorithms. The scaled-down UR3 cobot was used for upper limb rehabilitation. The authors are satisfied with the results for 2D movements, but point out a need for improvement for 3D movements. It should be noted that no systems were found in the literature that use the cobot for lower limb rehabilitation tasks. In the projects presented, the authors also did not compare the kinematics of the limbs treated by the robot with the kinematics of the limbs during manual exercises under the guidance of a physical therapist.
In this paper, the first comparison of the kinematics of PNF exercises performed with the help of a physical therapist with movements performed with the assistance of a robot is presented. The obtained results show that the robot is able to imitate a given movement pattern (therapeutic exercise) with high accuracy and, above all, repeatability. During rehabilitation with the robot, the range of a given exercise is not affected by the human factor of the fatigue of the physical therapist. In the present study, although the maximum value of the deviation was 6.35°, it should be remembered that the tests performed included only 10 repetitions and the physical therapist was just starting work on the day of the measurements. There is evidence in the literature that the high repetition of motor tasks during learning, which we can certainly provide in robot-assisted rehabilitation, stimulates a change in organization in the cerebral cortex. These experiments suggest that simple, repetitive motor activities are sufficient to produce representative plasticity in the motor maps of the cerebral cortex [
20,
21]. The authors suggest that the timing, intensity, and approach of training determine the degree of motor regeneration after stroke [
22]. It is known that therapeutic intervention should be started as soon as possible, but the specific number of repetitions required for optimal recovery of full function has not been established. Using animal models, researchers have achieved 300–800 repetitions and shown positive results in learning a motor task [
23,
24].
Birkenmeier et al. [
25] performed an intervention in which ≥ 300 repetitions were performed. The group consisted of post-stroke patients (≥ 6 months post-stroke) who performed a specific sequence of movements (reaching/carrying a deposited can). Participation in the intervention resulted in improved upper limb function as measured by the Action Research Arm Test and in patient reports. Similar results are presented by Waddell’s team, showing that performing a highly repetitive, individually tailored intervention (289 repetitions per session) statistically significantly improved movement function [
26]. The literature seems to indicate that it is not the time spent that matters, but how often a motor task is performed [
27]. This is supported by, among others, the results presented by Auwal Abdullahi et al. [
28], where the first group performed five lower limb tasks with a total of 600 repetitions per day, while the second group performed the same tasks for 3 h per day. The protocol of the first group was found to be not only more effective in improving performance but also simpler and less time consuming. The above examples confirm that the effectiveness of rehabilitation is related to a high number of repetitions of the rehabilitation exercises. It is considered reasonable to have patients perform a certain number of repetitions—tasks known to promote recovery. The UR10e robot presented in this paper has no restrictions on the number of repetitions; it is sufficient to program the rehabilitation series accordingly and start training. The use of robots for exercises that require a high number of repetitions can be a good alternative to support the work of a physiotherapist.
In addition to the benefits such as repetitive motion, stress relief, and support from the physical therapist, there is also the economic aspect to consider. The costs associated with paying the staff result in the patient not receiving an adequate therapeutic dose. In addition, most of the financing of the patient’s improvement process comes from public funds, and the calculation of expenses is not insignificant. It should also be noted that conventional therapy for neurological patients is very energy-intensive and requires a lot of physical effort from physical therapists. Therefore, the robots in rehabilitation are designed to perform the recommended number and precision of follow-up treatments, thus relieving the physical therapy staff while reducing the funding of the process. Hesse et al. [
29] compared robot-assisted group therapy to that of patients treated individually only. The results showed that both methods of improvement were satisfactorily effective, but therapy in the robot-assisted group appeared to be less costly. Carpiono et al. [
30] emphasized that robotic-assisted therapy reduces the cost incurred for rehabilitation with the number of sessions because the cost of purchasing the device alone is high (it pays for itself over time). Lo Kenneth et al. [
31] have produced a fair systematic review with a very thorough analysis of the costs incurred in improving patients after stroke, which clearly points to a more favorable calculation of the costs incurred in improving patients through the use of a robot, with evidence of achieving comparable therapeutic effects.
Limitation of This Work and Directions of Further Research
The idea presented in this paper of using the UR10e industrial robot to perform therapeutic exercises can be a valuable direction in improving the functioning of healthcare and, in particular, the rehabilitation process. Although the purpose of this work was to analyze the possibility of using the cobot in rehabilitation by comparing the kinematics of the set motion, it should be noted that the presented solution should be modified. Certainly, one of the most important aspects is the refinement of the safety system. Currently, the research was performed based on factory-built safety systems, including sensing feedback. The safety switch was accessible to the test patient. Admittedly, the type of procedures performed did not pose a threat and were performed and supervised by two qualified therapists. However, in the target solution for cooperation with patients, the built-in safety system will need to be expanded and adapted to the relevant standards. During the therapy, the aforementioned safety systems, supplemented according to the requirements of the standards, should guarantee that there will be no injury. One of the proposed improvements to the safety system could be the introduction of sensors to monitor the failure to exceed certain ranges of motion, such as at the knee joint [
32]. In addition to the development of a safety system, further work is planned to produce handles dedicated to the robotic arm allowing both lower and upper limb rehabilitation. The literature also indicates that a potential enrichment and motivation factor during the rehabilitation process can be the use of virtual reality during therapeutic exercises [
15].
5. Conclusions
The robot performs physiotherapeutic movements more precisely and with greater repeatability. Adapting the speed of the robot to reflect the speed of movement of the physiotherapist can be achieved by adjusting the orthosis to the limb for greater comfort. The movements performed by physiotherapists are less repetitive and have a smaller range with successive repetitions (possibly due to the cause of fatigue). The robot can reproduce the movement in the hip and knee joints accurately but not in the ankle joint (this is due to the way the limb is connected to the robot); it may be necessary to introduce an additional device/accessory to better control this joint. The algorithm of moving the robot arm between the control points changes the kinematic characteristics of the limb. The subject of research can be developed in order to modify the control of the robot using EMG signals to initiate the robot’s movement. By modifying the software, the robot could initiate the movement by exceeding the appropriate force registered by the robot (only in the UR10e version), which extends the possibilities of rehabilitation.
The robot’s current limb attachment does not allow active movement of the ankle joint. At a later stage of research, it is planned to design a lower limb orthosis attached to the UR10e robot, which will allow active movement of the ankle joint to reflect the kinematics of PNF movement.
Author Contributions
Conceptualization, S.S., M.B. and M.C.; data curation, H.Z. and P.S.; funding acquisition, W.W.; investigation, S.S., M.C., J.S.-D. and D.W.-Z.; methodology, R.M., S.S., M.B., M.C., H.Z. and J.S.-D.; project administration, W.W.; resources, S.S.; software, M.B.; supervision, R.M.; visualization, P.S.; writing—original draft, S.S., M.B., H.Z., P.S., J.S.-D. and D.W.-Z.; writing—review and editing, M.C., H.Z., P.S. and D.W.-Z. All authors have read and agreed to the published version of the manuscript.
Funding
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gassert, R.; Dietz, V. Rehabilitation Robots for the Treatment of Sensorimotor Deficits: A Neurophysiological Perspective. J. Neuroeng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef]
- Hu, X.; Suresh, N.L.; Rymer, W.Z. Estimating the Time Course of Population Excitatory Postsynaptic Potentials in Motoneurons of Spastic Stroke Survivors. J. Neurophysiol. 2015, 113, 1952. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.C.; Shaw, F.Z. Progress in Sensorimotor Rehabilitative Physical Therapy Programs for Stroke Patients. World J. Clin. cases 2014, 2, 316. [Google Scholar] [CrossRef]
- Coscia, M.; Wessel, M.J.; Chaudary, U.; Millán, J.d.R.; Micera, S.; Guggisberg, A.; Vuadens, P.; Donoghue, J.; Birbaumer, N.; Hummel, F.C. Neurotechnology-Aided Interventions for Upper Limb Motor Rehabilitation in Severe Chronic Stroke. Brain 2019, 142, 2182–2197. [Google Scholar] [CrossRef] [PubMed]
- Pignolo, L. Robotics in Neuro-Rehabilitation. J. Rehabil. Med. 2009, 41, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Guiu-Tula, F.X.; Cabanas-Valdés, R.; Sitjà-Rabert, M.; Urrútia, G.; Gómara-Toldrà, N. The Efficacy of the Proprioceptive Neuromuscular Facilitation (PNF) Approach in Stroke Rehabilitation to Improve Basic Activities of Daily Living and Quality of Life: A Systematic Review and Meta-Analysis Protocol. BMJ Open 2017, 7, e016739. [Google Scholar] [CrossRef]
- Gunning, E.; Uszynski, M.K. Effectiveness of the Proprioceptive Neuromuscular Facilitation Method on Gait Parameters in Patients With Stroke: A Systematic Review. Arch. Phys. Med. Rehabil. 2019, 100, 980–986. [Google Scholar] [CrossRef]
- Sharma, V.; Kaur, J. Effect of Core Strengthening with Pelvic Proprioceptive Neuromuscular Facilitation on Trunk, Balance, Gait, and Function in Chronic Stroke. J. Exerc. Rehabil. 2017, 13, 200–205. [Google Scholar] [CrossRef]
- Nguyen, P.T.; Chou, L.W.; Hsieh, Y.L. Proprioceptive Neuromuscular Facilitation-Based Physical Therapy on the Improvement of Balance and Gait in Patients with Chronic Stroke: A Systematic Review and Meta-Analysis. Life 2022, 12, 882. [Google Scholar] [CrossRef]
- Hindle, K.; Whitcomb, T.; Briggs, W.; Hong, J. Proprioceptive Neuromuscular Facilitation (PNF): Its Mechanisms and Effects on Range of Motion and Muscular Function. J. Hum. Kinet. 2012, 31, 105–113. [Google Scholar] [CrossRef]
- Adler, S.S.; Beckers, D.; Buck, M. PNF in Practice: An Illustrated Guide; Springer: Berlin/Heidelberg, Germany, 2008; pp. 1–299. [Google Scholar]
- Universal Robots—User Manual—UR10 CB-Series—SW3.15—English International (En). Available online: https://www.universal-robots.com/download/manuals-cb-series/user/ur10/315/user-manual-ur10-cb-series-sw315-english-international-en/ (accessed on 15 June 2023).
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global Estimates of the Need for Rehabilitation Based on the Global Burden of Disease Study 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Rehabilitation. Available online: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (accessed on 19 April 2023).
- Gzik, M.; Wodarski, P.; Jurkojć, J.; Michnik, R.; Bieniek, A. Interactive System of Enginering Support of Upper Limb Diagnosis. Adv. Intell. Syst. Comput. 2017, 526, 115–123. [Google Scholar] [CrossRef]
- Papaleo, E.; Zollo, L.; Spedaliere, L.; Guglielmelli, E. Patient-Tailored Adaptive Robotic System for Upper-Limb Rehabilitation. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 3860–3865. [Google Scholar] [CrossRef]
- Universal RoboTrainer—SDU. Available online: https://www.sdu.dk/en/forskning/healthinformaticsandtechnology/significantachievements/universal-robotrainer (accessed on 19 April 2023).
- Patient—Rehabilitation Using Industrial Robots—Universal RoboTrainer. Available online: https://www.en.patientathome.dk/projects/rehabilitation-using-industrial-robots-universal-robotrainer.aspx (accessed on 19 April 2023).
- Apollonio, L. Development of a Rehabilitation Exercise for Assisted Grasping through Collaborative Robot. Master’s Thesis, Università Politecnica delle Marche, Ancona, Italy, 2023. [Google Scholar]
- Monfils, M.H.; Plautz, E.J.; Kleim, J.A. In Search of the Motor Engram: Motor Map Plasticity as a Mechanism for Encoding Motor Experience. Neuroscientist 2005, 11, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Dayan, E.; Cohen, L.G. Neuroplasticity Subserving Motor Skill Learning. Neuron 2011, 72, 443–454. [Google Scholar] [CrossRef] [PubMed]
- Zeiler, S.R.; Krakauer, J.W. The Interaction between Training and Plasticity in the Poststroke Brain. Curr. Opin. Neurol. 2013, 26, 609–616. [Google Scholar] [CrossRef]
- Nudo, R.J.; Milliken, G.W.; Jenkins, W.M.; Merzenich, M.M. Use-Dependent Alterations of Movement Representations in Primary Motor Cortex of Adult Squirrel Monkeys. J. Neurosci. 1996, 16, 785–807. [Google Scholar] [CrossRef] [PubMed]
- Kleim, J.A.; Barbay, S.; Nudo, R.J. Functional Reorganization of the Rat Motor Cortex Following Motor Skill Learning. J. Neurophysiol. 1998, 80, 3321–3325. [Google Scholar] [CrossRef] [PubMed]
- Birkenmeier, R.L.; Prager, E.M.; Lang, C.E. Translating Animal Doses of Task-Specific Training to People with Chronic Stroke in 1-Hour Therapy Sessions: A Proof-of-Concept Study. Neurorehabil. Neural Repair 2010, 24, 620–635. [Google Scholar] [CrossRef]
- Waddell, K.J.; Birkenmeier, R.L.; Moore, J.L.; Hornby, T.G.; Lang, C.E. Feasibility of High-Repetition, Task-Specific Training for Individuals with Upper-Extremity Paresis. Am. J. Occup. Ther. 2014, 68, 444–453. [Google Scholar] [CrossRef]
- Nudo, R.J.; Milliken, G.W. Reorganization of Movement Representations in Primary Motor Cortex Following Focal Ischemic Infarcts in Adult Squirrel Monkeys. J. Neurophysiol. 1996, 75, 2144–2149. [Google Scholar] [CrossRef]
- Abdullahi, A.; Aliyu, N.U.; Useh, U.; Abba, M.A.; Akindele, M.O.; Truijen, S.; Saeys, W. Effects of Two Different Modes of Task Practice during Lower Limb Constraint-Induced Movement Therapy in People with Stroke: A Randomized Clinical Trial. Neural Plast. 2021, 2021, 6664058. [Google Scholar] [CrossRef]
- Hesse, S.; Heß, A.; Werner, C.C.; Kabbert, N.; Buschfort, R. Effect on Arm Function and Cost of Robot-Assisted Group Therapy in Subacute Patients with Stroke and a Moderately to Severely Affected Arm: A Randomized Controlled Trial. Clin. Rehabil. 2014, 28, 637–647. [Google Scholar] [CrossRef] [PubMed]
- Carpino, G.; Pezzola, A.; Urbano, M.; Guglielmelli, E. Assessing Effectiveness and Costs in Robot-Mediated Lower Limbs Rehabilitation: A Meta-Analysis and State of the Art. J. Healthc. Eng. 2018, 2018, 7492024. [Google Scholar] [CrossRef]
- Lo, K.; Stephenson, M.; Lockwood, C. The Economic Cost of Robotic Rehabilitation for Adult Stroke Patients: A Systematic Review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 520–547. [Google Scholar] [CrossRef] [PubMed]
- Fay, C.D.; Mannering, N.; Jeiranikhameneh, A.; Mokhtari, F.; Foroughi, J.; Baughman, R.H.; Choong, P.F.M.; Wallace, G.G. Wearable Carbon Nanotube-Spandex Textile Yarns for Knee Flexion Monitoring. Adv. Sens. Res. 2023, 2, 2200021. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).