Oral Ingestion of Synthetically Generated Recombinant Prion Is Sufficient to Cause Prion Disease in Wild-Type Mice
Abstract
1. Introduction
2. Results
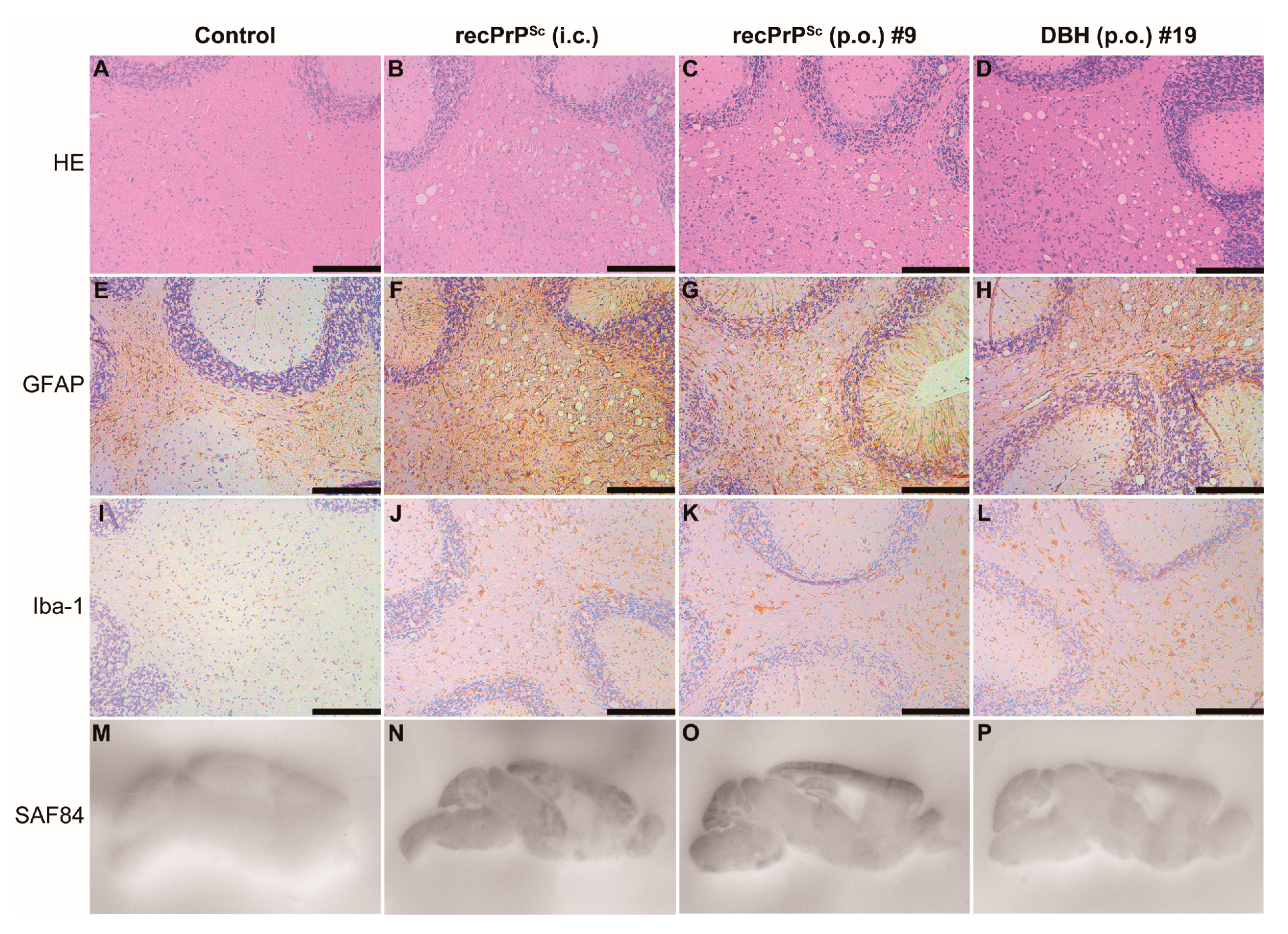
2.1. A Single Oral Feeding of RecPrPSc Causes Prion Disease in Wild-Type Mice
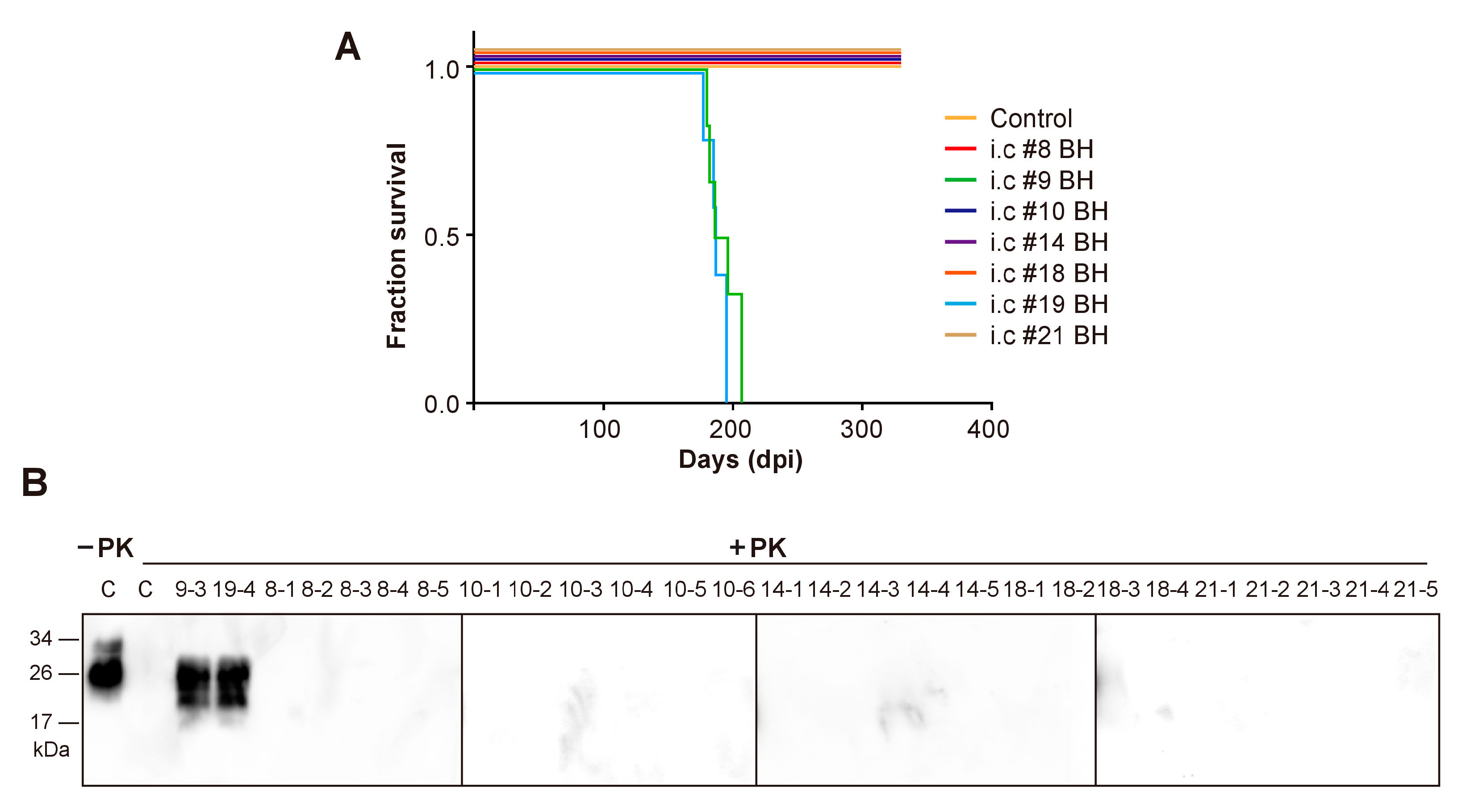
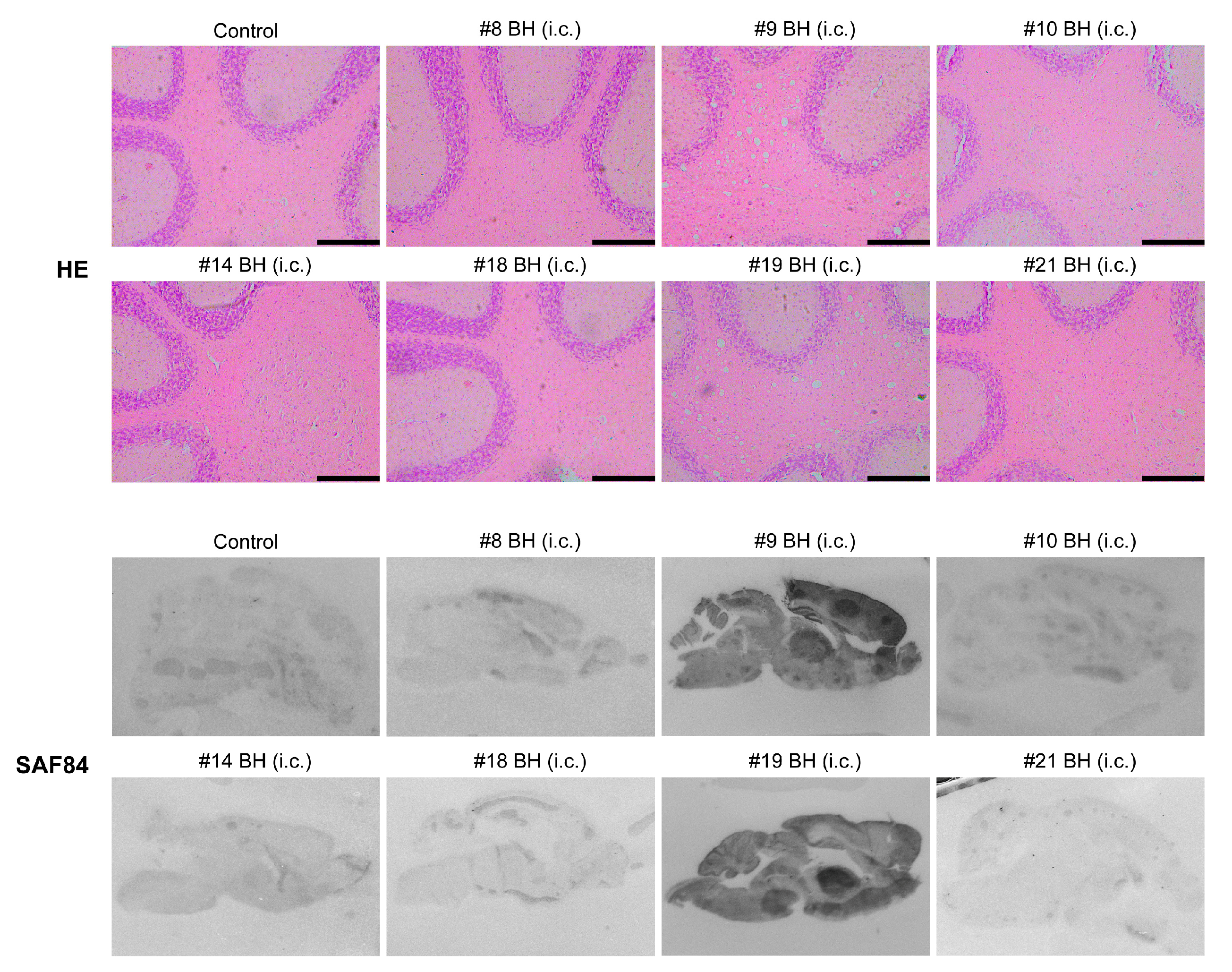
2.2. Second Round Transmission
3. Discussion
4. Materials and Methods
4.1. Mice
4.2. Prion Exposure and Disease Monitoring
4.3. Histopathological Analyses
4.4. Immunoblot Detection of PrPSc
Author Contributions
Funding
Conflicts of Interest
References
- Prusiner, S.B. Prions. Proc. Natl. Acad. Sci. USA 1998, 95, 13363–13383. [Google Scholar] [CrossRef] [PubMed]
- Mabbott, N.A. How do PrP(Sc) Prions Spread between Host Species, and within Hosts? Pathogens 2017, 6, 60. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Wang, F. Prion disease and the ‘protein-only hypothesis’. Essays Biochem. 2014, 56, 181–191. [Google Scholar] [PubMed]
- Wang, F.; Wang, X.; Yuan, C.G.; Ma, J. Generating a prion with bacterially expressed recombinant prion protein. Science 2010, 327, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, Y.; Wang, F.; Wang, X.; Xu, Y.; Yang, H.; Yu, G.; Yuan, C.; Ma, J. De novo generation of infectious prions with bacterially expressed recombinant prion protein. FASEB J. 2013, 27, 4768–4775. [Google Scholar] [CrossRef]
- Wang, X.; McGovern, G.; Zhang, Y.; Wang, F.; Zha, L.; Jeffrey, M.; Ma, J. Intraperitoneal Infection of Wild-Type Mice with Synthetically Generated Mammalian Prion. PLoS Pathog. 2015, 11, e1004958. [Google Scholar] [CrossRef]
- Wang, F.; Wang, X.; Abskharon, R.; Ma, J. Prion infectivity is encoded exclusively within the structure of proteinase K-resistant fragments of synthetically generated recombinant PrP(Sc). Acta Neuropathol. Commun. 2018, 6, 30. [Google Scholar] [CrossRef]
- Sevillano, A.M.; Fernandez-Borges, N.; Younas, N.; Wang, F.; Elezgarai, S.R.; Bravo, S.; Vazquez-Fernandez, E.; Rosa, I.; Erana, H.; Gil, D.; et al. Recombinant PrPSc shares structural features with brain-derived PrPSc: Insights from limited proteolysis. PLoS Pathog. 2018, 14, e1006797. [Google Scholar] [CrossRef]
- Wang, F.; Wang, X.; Orru, C.D.; Groveman, B.R.; Surewicz, K.; Abskharon, R.; Imamura, M.; Yokoyama, T.; Kim, Y.S.; Vander Stel, K.J.; et al. Self-propagating, protease-resistant, recombinant prion protein conformers with or without in vivo pathogenicity. PLoS Pathog. 2017, 13, e1006491. [Google Scholar] [CrossRef]
- Li, Q.; Wang, F.; Xiao, X.; Kim, C.; Bohon, J.; Kiselar, J.; Safar, J.G.; Ma, J.; Surewicz, W.K. Structural attributes of mammalian prion infectivity: Insights from studies with synthetic prions. J. Biol. Chem. 2018, 293, 18494–18503. [Google Scholar] [CrossRef]
- Thackray, A.M.; Klein, M.A.; Aguzzi, A.; Bujdoso, R. Chronic subclinical prion disease induced by low-dose inoculum. J. Virol. 2002, 76, 2510–2517. [Google Scholar] [CrossRef] [PubMed]
- Thackray, A.M.; Klein, M.A.; Bujdoso, R. Subclinical prion disease induced by oral inoculation. J. Virol. 2003, 77, 7991–7998. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.J.; Lewis, V.; Brazier, M.W.; Hill, A.F.; Lawson, V.A.; Klug, G.M.; Masters, C.L. Extended period of asymptomatic prion disease after low dose inoculation: Assessment of detection methods and implications for infection control. Neurobiol. Dis. 2005, 20, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Makarava, N.; Kovacs, G.G.; Savtchenko, R.; Alexeeva, I.; Budka, H.; Rohwer, R.G.; Baskakov, I.V. Genesis of Mammalian Prions: From Non-infectious Amyloid Fibrils to a Transmissible Prion Disease. PLoS Pathog. 2011, 7, e1002419. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, M.; Gonzalez, L.; Espenes, A.; Press, C.M.; Martin, S.; Chaplin, M.; Davis, L.; Landsverk, T.; MacAldowie, C.; Eaton, S.; et al. Transportation of prion protein across the intestinal mucosa of scrapie-susceptible and scrapie-resistant sheep. J. Pathol. 2006, 209, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Kimberlin, R.H.; Walker, C.A. Pathogenesis of scrapie in mice after intragastric infection. Virus Res. 1989, 12, 213–220. [Google Scholar] [CrossRef]
- Prusiner, S.B.; Cochran, S.P.; Alpers, M.P. Transmission of scrapie in hamsters. J. Infect. Dis. 1985, 152, 971–978. [Google Scholar] [CrossRef]
- Sigurdson, C.J.; Heikenwalder, M.; Manco, G.; Barthel, M.; Schwarz, P.; Stecher, B.; Krautler, N.J.; Hardt, W.D.; Seifert, B.; MacPherson, A.J.; et al. Bacterial colitis increases susceptibility to oral prion disease. J. Infect. Dis. 2009, 199, 243–252. [Google Scholar] [CrossRef]
- Miller, M.W.; Williams, E.S. Prion disease: Horizontal prion transmission in mule deer. Nature 2003, 425, 35–36. [Google Scholar] [CrossRef]
- Mathiason, C.K.; Hays, S.A.; Powers, J.; Hayes-Klug, J.; Langenberg, J.; Dahmes, S.J.; Osborn, D.A.; Miller, K.V.; Warren, R.J.; Mason, G.L.; et al. Infectious prions in pre-clinical deer and transmission of chronic wasting disease solely by environmental exposure. PLoS ONE 2009, 4, e5916. [Google Scholar] [CrossRef]
- Ryder, S.; Dexter, G.; Bellworthy, S.; Tongue, S. Demonstration of lateral transmission of scrapie between sheep kept under natural conditions using lymphoid tissue biopsy. Res. Vet. Sci. 2004, 76, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.J.; Pedersen, J.A.; Chappell, R.J.; McKenzie, D.; Aiken, J.M. Oral transmissibility of prion disease is enhanced by binding to soil particles. PLoS Pathog. 2007, 3, e93. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, D.S.; Sehgal, A.; Rios, D.; Williams, I.R.; Mabbott, N.A. Increased Abundance of M Cells in the Gut Epithelium Dramatically Enhances Oral Prion Disease Susceptibility. PLoS Pathog. 2016, 12, e1006075. [Google Scholar] [CrossRef] [PubMed]
- Denkers, N.D.; Telling, G.C.; Hoover, E.A. Minor oral lesions facilitate transmission of chronic wasting disease. J. Virol. 2011, 85, 1396–1399. [Google Scholar] [CrossRef]
- Wang, F.; Wang, X.; Ma, J. Conversion of bacterially expressed recombinant prion protein. Methods 2011, 53, 208–213. [Google Scholar] [CrossRef][Green Version]
- Mabbott, N.A.; Young, J.; McConnell, I.; Bruce, M.E. Follicular dendritic cell dedifferentiation by treatment with an inhibitor of the lymphotoxin pathway dramatically reduces scrapie susceptibility. J. Virol. 2003, 77, 6845–6854. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, F.; Wang, X.; Zhang, Z.; Xu, Y.; Yu, G.; Yuan, C.; Ma, J. Comparison of 2 synthetically generated recombinant prions. Prion 2014, 8, 215–220. [Google Scholar] [CrossRef]
- Choi, J.K.; Park, S.J.; Jun, Y.C.; Oh, J.M.; Jeong, B.H.; Lee, H.P.; Park, S.N.; Carp, R.I.; Kim, Y.S. Generation of monoclonal antibody recognized by the GXXXG motif (glycine zipper) of prion protein. Hybridoma (Larchmt) 2006, 25, 271–277. [Google Scholar] [CrossRef]
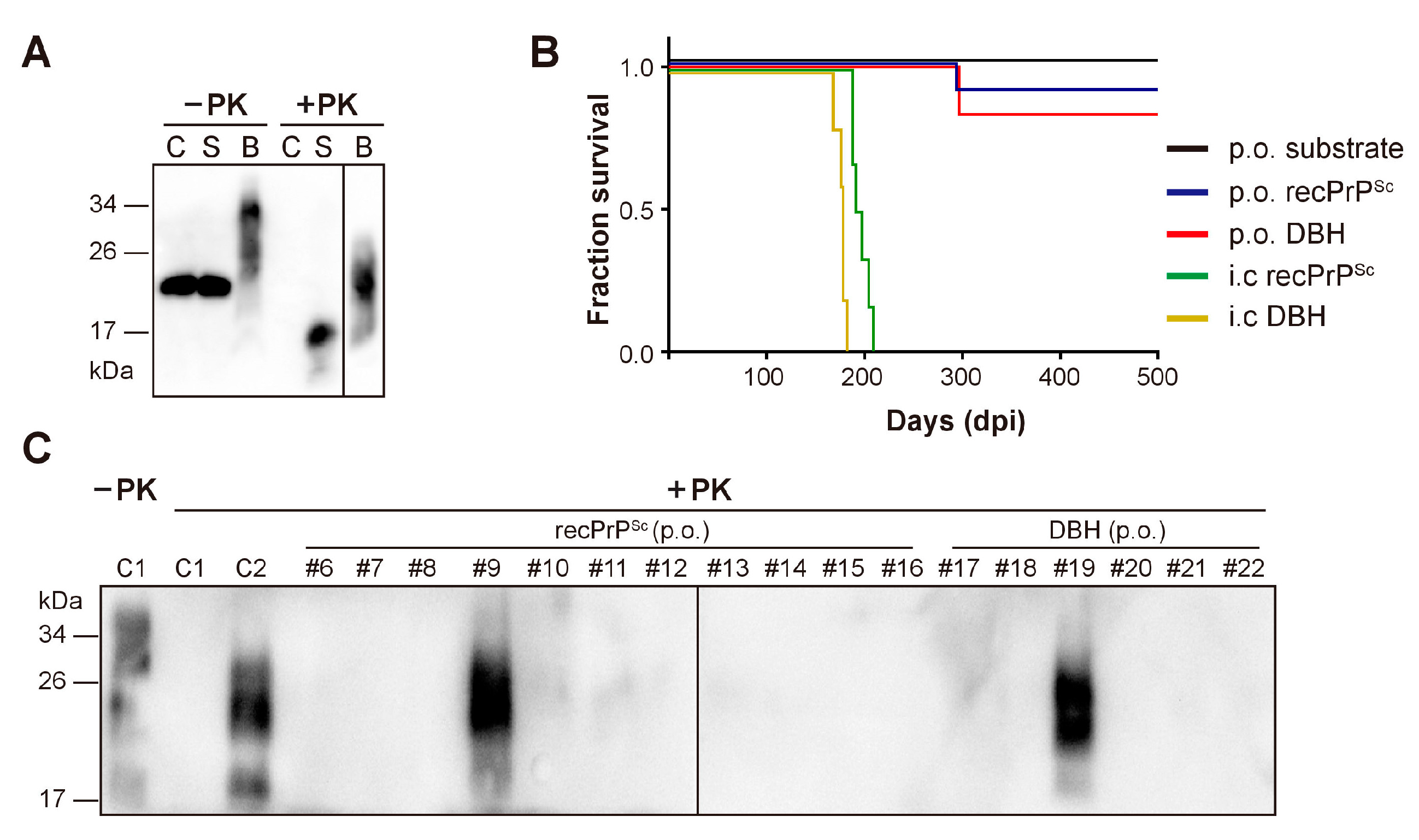
| Inoculum | Route of Transmission | Diseased/Exposed Mice | Survival (Days) (Mean ± SEM) |
|---|---|---|---|
| sPMCA substrate | Oral feeding | 0/5 | >650 |
| recPrPSc | Oral feeding | 1/11 | 294; 574 *; >650 |
| DBH | Oral feeding | 1/6 | 297; 586 *; >650 |
| recPrPSc | i.c inoculation | 6/6 | 196.2 ± 3.59 |
| DBH | i.c inoculation | 5/5 | 176.4 ± 5.17 |
| Inoculum | Route of Transmission | Diseased/Inoculated Mice | Survival (Days) (Mean ± SEM) |
|---|---|---|---|
| Control | i.c. | 0/5 | >330 |
| #8 mouse BH | i.c. | 0/5 | >330 |
| #9 mouse BH | i.c. | 6/6 | 191 ± 4.97 |
| #10 mouse BH | i.c. | 0/6 | >330 |
| #14 mouse BH | i.c. | 0/5 | >330 |
| #18 mouse BH | i.c. | 0/4 | >330 |
| #19 mouse BH | i.c. | 5/5 | 187 ± 3.38 |
| #21 mouse BH | i.c. | 0/5 | >330 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, C.; Yang, J.; Zhang, X.; Chen, Y.; Wei, S.; Yu, G.; Pan, Y.-H.; Ma, J.; Yuan, C. Oral Ingestion of Synthetically Generated Recombinant Prion Is Sufficient to Cause Prion Disease in Wild-Type Mice. Pathogens 2020, 9, 653. https://doi.org/10.3390/pathogens9080653
Pan C, Yang J, Zhang X, Chen Y, Wei S, Yu G, Pan Y-H, Ma J, Yuan C. Oral Ingestion of Synthetically Generated Recombinant Prion Is Sufficient to Cause Prion Disease in Wild-Type Mice. Pathogens. 2020; 9(8):653. https://doi.org/10.3390/pathogens9080653
Chicago/Turabian StylePan, Chenhua, Junwei Yang, Xiangyi Zhang, Ying Chen, Shunxiong Wei, Guohua Yu, Yi-Hsuan Pan, Jiyan Ma, and Chonggang Yuan. 2020. "Oral Ingestion of Synthetically Generated Recombinant Prion Is Sufficient to Cause Prion Disease in Wild-Type Mice" Pathogens 9, no. 8: 653. https://doi.org/10.3390/pathogens9080653
APA StylePan, C., Yang, J., Zhang, X., Chen, Y., Wei, S., Yu, G., Pan, Y.-H., Ma, J., & Yuan, C. (2020). Oral Ingestion of Synthetically Generated Recombinant Prion Is Sufficient to Cause Prion Disease in Wild-Type Mice. Pathogens, 9(8), 653. https://doi.org/10.3390/pathogens9080653





