A Probiotic-Based Sanitation System for the Reduction of Healthcare Associated Infections and Antimicrobial Resistances: A Budget Impact Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Outcomes
2.3. Healthcare Resource Consumption and Costs
2.4. Budget Impact Analysis
3. Results
3.1. Target Population, Pharmaceutical Treatments, HAI and Antibiotic-Resistance Rates, HAIs Outcomes
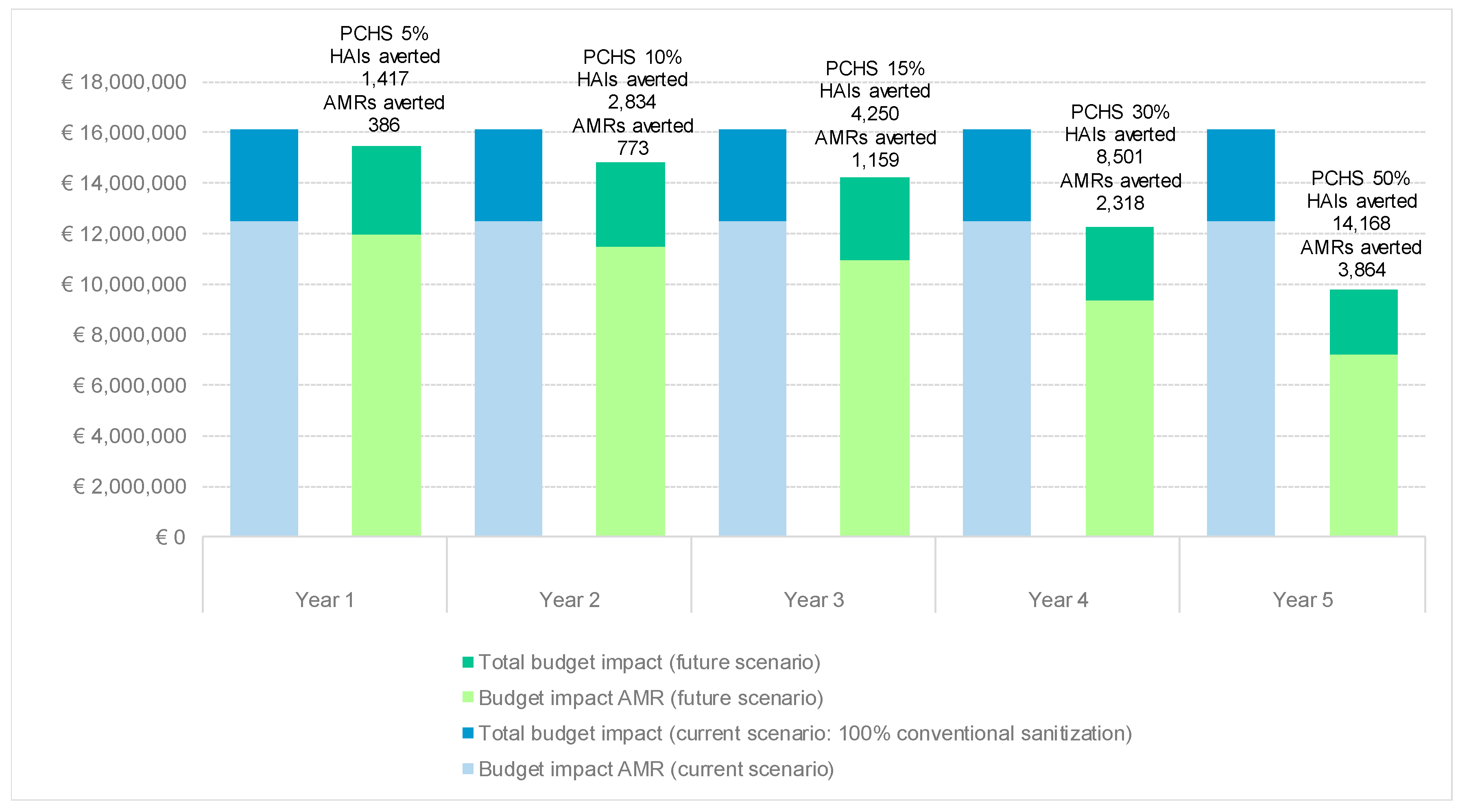
3.2. Budget Impact Analysis
3.3. Risk Assessment Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Level | €/Hour | Employment | Value €/Hour |
|---|---|---|---|
| 2° level | €15.88 | 85.00% | €13.50 |
| 3° level | €16.65 | 12.00% | €2.00 |
| 4° level | €17.52 | 3.00% | €0.53 |
| TOTAL | €16.02 | ||
| Item | Cost component | VALUE €/HOUR | |
| Analysis of “material” needs | |||
| Machinery | 1.40% | €0.22 | |
| Equipment | 1.80% | €0.29 | |
| Cleaning products | 2.50% | €0.40 | |
| Consumables | 2.00% | €0.32 | |
| Treasury | 4.00% | €0.64 | |
| Analysis of “ancillary” needs | |||
| Overheads | 7.00% | €1.12 | |
| Profit | 3.00% | €0.48 | |
| €/hour GROSS REVENUE | €19.50 | ||
| Area Code | Description | Locations Included |
|---|---|---|
| MR1 | Ward with hospitalization—Medium risk | Inpatient rooms, medication room, ward depot, nurses’ work room, herbal tea room, ward kitchen, dining room, related to the following departments: First aid or ER, day hospital, and other departments not included in the homogeneous area AR0 |
| MR3 | Corridors and waiting rooms—Medium risk | Corridors, waiting rooms inside the wards and medium-risk diagnosis areas, lifts for patient transport, living rooms inside the wards |
| MR4 | Hospital toilets, staff toilets or in any case open 7 days a week | Toilets inside the wards, operating departments and diagnostic areas, (regardless of the risk area they belong to) drains, and other similar rooms open 7 days a week |
| Activity Description | Frequency | CCC Time Spent | PCHS Time Spent | |
|---|---|---|---|---|
| Emptying of waste bins with closure and transport to the solid or similar waste collection point and replacement of the bag and/or container | 2 per day | 0.025 | 0.025 | |
| Wet dusting and cleaning including the removal of stains on horizontal and vertical surfaces up to 180 cm, on furnishings, sanitary facilities (beds, bedside tables, bed headboards, dividing curtains, IV stands including wheels, serving tables, trolleys, stretchers, prams, walkers, supports, etc.) and common contact points (telephones, switches and push-button panels, audiovisual equipment, handles, handrails, etc.) light points, fan coils, internal windowsills, doors, windows and other washable surfaces | daily | 0.1917 | 0.1917 | |
| Wet sweeping with removal of dust and waste from all floors, with disposable and/or suction gauze. | daily | 0.0208 | * | |
| Floor washing, after moving the easily removable furnishings. Reposition on dry floor of what was previously moved. If using a washer dryer, finish with manual cleaning the points not reached by washing by machine. | daily | 0.05 | 0.05 | |
| Cleansing and disinfection of waste bins, bag carriages and waste bins. | weekly | 0.0143 | 0.0143 | |
| Maintenance of protective floor treatments (spray cleaning or spray buffing). | monthly | 0.0033 | 0.0033 | |
| Debinding with total or partial removal of the film and subsequent waxing of the floors. | de-waxing | every six months | 0.0046 | 0.0046 |
| waxing | 0.0009 | 0.0009 | ||
| Cleaning the external side of the fixtures, including glass surfaces, bins and external window sills if accessible from the inside in compliance with safety regulations. | every three months | 0.0003 | 0.0003 | |
| Total working hours CONTINUOUS ACTIVITIES on a day basis (7/7) | 0.2875 | 0.2667 | ||
| Total working hours PERIODIC ACTIVITIES (from weekly to annual) on a day basis (7/7) | 0.0234 | 0.0234 | ||
| TOTAL DAILY HOURS | 0.3109 | 0.29 | ||
| Activity Description | Frequency | CCC Time Spent | PCHS Time Spent | |
|---|---|---|---|---|
| Emptying of waste bins with closure and transport to the solid or similar waste collection point and replacement of the bag and/or container | 2 per day | 0.0083 | 0.0083 | |
| Wet dusting and cleaning including the removal of stains of horizontal and vertical surfaces up to 180 cm, on furniture, and common contact points (telephones switches and push-button panels, handles, handrails, etc.), fan coils, window sills, doors, internal parts of the fixtures including glass surfaces, and other washable surfaces. | 2 per day | 0.0333 | 0.0333 | |
| Wet sweeping with removal of dust and waste from all floors, with disposable and/or suction gauze. | 2 per day | 0.0376 | 0.0188 * | |
| Floor washing, after moving the easily removable furnishings. Reposition on dry floor of what was previously moved. If using a washer dryer, finish with manual cleaning the points not reached by washing by machine. | daily | 0.05 | 0.05 | |
| Cleansing and disinfection of waste bins, bag carriages and waste bins. | weekly | 0.0048 | 0.0048 | |
| Maintenance of protective floor treatments (spray cleaning or spray buffing). | monthly | 0.004 | 0.004 | |
| Debinding with total or partial removal of the film and subsequent waxing of the floors. | de-waxing | every six months | 0.0055 | 0.0055 |
| waxing | 0.0011 | 0.0011 | ||
| Cleaning the external side of the fixtures, including glass surfaces, bins and external window sills if accessible from the inside in compliance with safety regulations. | every three months | 0.0003 | 0.0003 | |
| Total working hours CONTINUOUS ACTIVITIES on a day basis (7/7) | 0.1292 | 0.1104 | ||
| Total working hours PERIODIC ACTIVITIES (from weekly to annual) on a day basis (7/7) | 0.0156 | 0.0156 | ||
| TOTAL DAILY HOURS | 0.1448 | 0.126 | ||
| Activity Description | Frequency | CCC Time Spent | CCC Time Spent |
|---|---|---|---|
| Emptying of waste bins with closure and transport to the solid or similar waste collection point and replacement of the bag and/or container | 2 per day | 0.0167 | 0.0167 |
| Cleaning and disinfection of sanitary fixtures, showers, shower cubicles, washable walls and all the accessories and sanitary furnishings present in these areas (including pipe cleaners and brush holders). | 2 per day | 0.3 | 0.3 |
| 0.15 | 0.15 | ||
| Cleaning of soap dispensers, wipes, toilet paper. | 2 per day | 0.15 | 0.15 |
| 0.075 | 0.075 | ||
| Wet dusting with the help of specific products of horizontal surfaces and up to 180 cm, radiators, fan coils, internal windowsills, push-button panels, handles, crystals, mirrors, shelves, furnishings, etc. | 2 per day | 0.1833 | 0.1833 |
| Wet rubbish with removal of dust and waste from the floors. | 2 per day | 0.0033 | * |
| 0.0033 | * | ||
| Floor washing and disinfection. | 2 per day | 0.008 | 0.008 |
| 0.008 | 0.008 | ||
| Descaling of sanitary ware, taps and neighboring areas | 2 per week | 0.0714 | 0.0714 |
| Spiderweb removals | weekly | 0.001 | 0.001 |
| Cleaning of rubbish bins, bag holder trolleys for laundry | weekly | 0.0095 | 0.0095 |
| Thorough cleaning of floors, if necessary carry out descaling. Previously transport any furniture and furnishings, after thorough cleaning, outside the room. | monthly | 0.0012 | 0.0012 |
| Wet dusting of convector heaters, heaters, air conditioning appliances, air vents, bins. | monthly | 0.0066 | 0.0066 |
| Mechanical aspiration of all areas not manually accessible beyond cm. 180 including lighting fixtures, convectors, heaters, conduits, bins, air vents, etc. | every four months | 0.0005 | 0.0005 |
| Cleaning the external side of the fixtures, including glass surfaces, bins and external window sills if accessible from the inside in compliance with safety regulations | every three months | 0.0002 | 0.0002 |
| Total working hours CONTINUOUS ACTIVITIES on a day basis (7/7) | 0.9691 | 0.9624 | |
| Total working hours PERIODIC ACTIVITIES (from weekly to annual) on a day basis (7/7) | 0.019 | 0.019 | |
| TOTAL DAILY HOURS | 0.9881 | 0.9815 | |
| Description | CCC | PCHS | |
|---|---|---|---|
| Total working hours CONTINUOUS ACTIVITIES on a day basis (7/7) (MR1+MR3+MR4) | 1.3858 | 1.3395 | |
| Total working hours PERIODIC ACTIVITIES (from weekly to annual) on a day basis (7/7) (MR1+MR3+MR4) | 0.058 | 0.058 | |
| TOTAL DAILY HOURS | 1.4438 | 1.3975 | |
| HOURLY COST | €19.50 | €19.50 | |
| MONETIZATION DAY SERVICE | €28.15 | €27.25 | |
| SAVINGS | €0.90 (=3.20%) | ||
References
- World Health Organization. Antimicrobial Resistance. Available online: https://www.who.int/health-topics/antimicrobial-resistance (accessed on 20 May 2020).
- Organisation for Economic Cooperation and Development. Stemming the Superbug Tide: Just a Few Dollars More; OECD publishing: Paris, France, 2018; ISBN 92-64-31139-4. [Google Scholar]
- Limmathurotsakul, D.; Dunachie, S.; Fukuda, K.; Feasey, N.A.; Okeke, I.N.; Holmes, A.H.; Moore, C.E.; Dolecek, C.; van Doorn, H.R.; Shetty, N. Improving the estimation of the global burden of antimicrobial resistant infections. Lancet Infect. Dis. 2019, 19, e392–e398. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- Chokshi, A.; Sifri, Z.; Cennimo, D.; Horng, H. Global contributors to antibiotic resistance. J. Glob. Infect. Dis. 2019, 11, 36. [Google Scholar]
- Ministry of Health. Antibiotico Resistenza Nell’uomo. Available online: http://www.salute.gov.it/portale/antibioticoresistenza/dettaglioContenutiAntibioticoResistenza.jsp?lingua=italiano&id=5282&area=antibiotico-resistenza&menu=vuoto&tab=1 (accessed on 20 May 2020).
- Allegranzi, B.; Nejad, S.B.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Anderson, M.; Clift, C.; Schulze, K.; Sagan, A.; Nahrgang, S.; Ouakrim, D.A.; Mossialos, E. Averting the AMR crisis. What are the avenues for policy action for countries in Europe? In European Observatory Policy Briefs; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2019. [Google Scholar]
- Collignon, P.; Beggs, J.J.; Walsh, T.R.; Gandra, S.; Laxminarayan, R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance: A univariate and multivariable analysis. Lancet Planet. Health 2018, 2, e398–e405. [Google Scholar] [CrossRef]
- Anderson, D.J.; Chen, L.F.; Weber, D.J.; Moehring, R.W.; Lewis, S.S.; Triplett, P.F.; Blocker, M.; Becherer, P.; Schwab, J.C.; Knelson, L.P. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium difficile (the Benefits of Enhanced Terminal Room Disinfection study): A cluster-randomised, multicentre, crossover study. Lancet 2017, 389, 805–814. [Google Scholar] [CrossRef]
- Almatroudi, A.; Gosbell, I.B.; Hu, H.; Jensen, S.O.; Espedido, B.A.; Tahir, S.; Glasbey, T.O.; Legge, P.; Whiteley, G.; Deva, A. Staphylococcus aureus dry-surface biofilms are not killed by sodium hypochlorite: Implications for infection control. J. Hosp. Infect. 2016, 93, 263–270. [Google Scholar] [CrossRef]
- Dancer, S.J. Controlling hospital-acquired infection: Focus on the role of the environment and new technologies for decontamination. Clin. Microbiol. Rev. 2014, 27, 665–690. [Google Scholar] [CrossRef]
- Wand, M.E.; Bock, L.J.; Bonney, L.C.; Sutton, J.M. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of Klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob. Agents Chemother. 2017, 61, e01162-16. [Google Scholar] [CrossRef]
- Donskey, C.J. Does improving surface cleaning and disinfection reduce health care-associated infections? Am. J. Infect. Control 2013, 41, S12–S19. [Google Scholar] [CrossRef]
- La Fauci, V.; Costa, G.B.; Anastasi, F.; Facciolà, A.; Go, C.; Squeri, R. An innovative approach to hospital sanitization using probiotics: In vitro and field trials. Microb. Biochem. Technol. 2015, 7, 160–164. [Google Scholar] [CrossRef]
- Vandini, A.; Temmerman, R.; Frabetti, A.; Caselli, E.; Antonioli, P.; Balboni, P.G.; Platano, D.; Branchini, A.; Mazzacane, S. Hard surface biocontrol in hospitals using microbial-based cleaning products. PLoS ONE 2014, 9, e108598. [Google Scholar] [CrossRef] [PubMed]
- Caselli, E. Hygiene: Microbial strategies to reduce pathogens and drug resistance in clinical settings. Microb. Biotechnol. 2017, 10, 1079–1083. [Google Scholar] [CrossRef]
- Caselli, E.; Arnoldo, L.; Rognoni, C.; D’Accolti, M.; Soffritti, I.; Lanzoni, L.; Bisi, M.; Volta, A.; Tarricone, R.; Brusaferro, S. Impact of a probiotic-based hospital sanitation on antimicrobial resistance and HAI-associated antimicrobial consumption and costs: A multicenter study. Infect. Drug Resist. 2019, 12, 501. [Google Scholar] [CrossRef]
- Caselli, E.; Brusaferro, S.; Coccagna, M.; Arnoldo, L.; Berloco, F.; Antonioli, P.; Tarricone, R.; Pelissero, G.; Nola, S.; La Fauci, V. Reducing healthcare-associated infections incidence by a probiotic-based sanitation system: A multicentre, prospective, intervention study. PLoS ONE 2018, 13, 0199616. [Google Scholar] [CrossRef]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Rosenbaum, P.R.; Rubin, D.B. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am. Stat. 1985, 39, 33–38. [Google Scholar]
- Peikes, D.N.; Moreno, L.; Orzol, S.M. Propensity score matching: A note of caution for evaluators of social programs. Am. Stat. 2008, 62, 222–231. [Google Scholar] [CrossRef]
- Leuven, E.; Sianesi, B. PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing. 2003. Available online: https://econpapers.repec.org/software/bocbocode/s432001.htm (accessed on 20 May 2020).
- Thorpe, K.E.; Joski, P.; Johnston, K.J. Antibiotic-resistant infection treatment costs have doubled since 2002, now exceeding $2 billion annually. Health Aff. 2018, 37, 662–669. [Google Scholar] [CrossRef]
- Currie, C.J.; Berni, E.; Jenkins-Jones, S.; Poole, C.D.; Ouwens, M.; Driessen, S.; de Voogd, H.; Butler, C.C.; Morgan, C.L. Antibiotic treatment failure in four common infections in UK primary care 1991–2012: Longitudinal analysis. BMJ 2014, 349, g5493. [Google Scholar] [CrossRef] [PubMed]
- Longo, C.; Bartlett, G.; MacGibbon, B.; Mayo, N.; Rosenberg, E.; Nadeau, L.; Daskalopoulou, S.S. The effect of obesity on antibiotic treatment failure: A historical cohort study. Pharmacoepidemiol. Drug Saf. 2013, 22, 970–976. [Google Scholar] [CrossRef]
- Hess, G.; Hill, J.W.; Raut, M.K.; Fisher, A.C.; Mody, S.; Schein, J.R.; Chen, C.-C. Comparative antibiotic failure rates in the treatment of community-acquired pneumonia: Results from a claims analysis. Adv. Ther. 2010, 27, 743–755. [Google Scholar] [CrossRef] [PubMed]
- Runciman, W.B. Lessons from the Australian Patient Safety Foundation: Setting up a national patient safety surveillance system—Is this the right model? BMJ Qual. Saf. 2002, 11, 246–251. [Google Scholar] [CrossRef] [PubMed]
- European Union. Services—505366-2019. Available online: https://ted.europa.eu/udl?uri=TED:NOTICE:505366-2019:TEXT:EN:HTML (accessed on 20 May 2020).
- Ministry of Health. Rapporto Annuale Sull’attività Di Ricovero Ospedaliero. Dati SDO 2018. Available online: http://www.salute.gov.it/portale/documentazione/p6_2_8_3_1.jsp?lingua=italiano&id=33 (accessed on 20 May 2020).
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Hughes, G.; Hinder, S.; Fahy, N.; Procter, R.; Shaw, S. Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J. Med. Internet Res. 2017, 19, e367. [Google Scholar] [CrossRef] [PubMed]
- Ciani, O.; Armeni, P.; Boscolo, P.R.; Cavazza, M.; Jommi, C.; Tarricone, R. De innovatione: The concept of innovation for medical technologies and its implications for healthcare policy-making. Health Policy Technol. 2016, 5, 47–64. [Google Scholar] [CrossRef]
- Smith, B.D.; Tarricone, R.; Vella, V. The role of product life cycle in medical technology innovation. J. Med. Mark. 2013, 13, 37–43. [Google Scholar] [CrossRef]
- Sullivan, S.D.; Mauskopf, J.A.; Augustovski, F.; Caro, J.J.; Lee, K.M.; Minchin, M.; Orlewska, E.; Penna, P.; Barrios, J.-M.R.; Shau, W.-Y. Budget impact analysis—Principles of good practice: Report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health 2014, 17, 5–14. [Google Scholar] [CrossRef]
- Caselli, E.; Antonioli, P.; Mazzacane, S. Safety of probiotics used for hospital environmental sanitation. J. Hosp. Infect. 2016, 94, 193. [Google Scholar] [CrossRef]
- Caselli, E.; D’Accolti, M.; Vandini, A.; Lanzoni, L.; Camerada, M.T.; Coccagna, M.; Branchini, A.; Antonioli, P.; Balboni, P.G.; Di Luca, D. Impact of a probiotic-based cleaning intervention on the microbiota ecosystem of the hospital surfaces: Focus on the resistome remodulation. PLoS ONE 2016, 11, 0148857. [Google Scholar] [CrossRef]
- Clift, C. Review of Progress on Antimicrobial Resistance; Chatham House: London, UK, 2019. [Google Scholar]
- Bock, L.J.; Wand, M.E.; Sutton, J.M. Varying activity of chlorhexidine-based disinfectants against Klebsiella pneumoniae clinical isolates and adapted strains. J. Hosp. Infect. 2016, 93, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Piano Nazionale Di Contrasto Dell’antimicrobico-Resistenza (PNCAR) 2017–2020. 2017. Available online: http://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=2660 (accessed on 20 May 2020).
- Ricchizzi, E. Studio Di Prevalenza Europeo Su Infezioni Correlate All’assistenza e Uso Di Antibiotici Negli Ospedali per Acuti. Rapporto nazionale. Available online: https://assr.regione.emilia-romagna.it/pubblicazioni/rapporti-documenti/studio-prevalenza-europeo-ICA-ospedali-acuti (accessed on 20 May 2020).
- Istituto Superiore di Sanità. Infezioni Correlate All’assistenza. Available online: https://www.epicentro.iss.it/infezioni-correlate/epidemiologia (accessed on 20 May 2020).
- The European House-Ambrosetti XIII Rapporto Meridiano Sanità. 2018. Available online: https://eventi.ambrosetti.eu/forum-meridiano-sanita-13/wp-content/uploads/sites/79/2018/11/MS13-Report-def-completo.pdf (accessed on 20 May 2020).
- Berger, M.L.; Sox, H.; Willke, R.J.; Brixner, D.L.; Eichler, H.-G.; Goettsch, W.; Madigan, D.; Makady, A.; Schneeweiss, S.; Tarricone, R.; et al. Good practices for real-world data studies of treatment and/or comparative effectiveness: Recommendations from the joint ISPOR-ISPE Special Task Force on real-world evidence in health care decision making. Pharm. Drug Saf 2017, 26, 1033–1039. [Google Scholar]
- Patrini, E. Le Infezioni ospedaliere. Analisi dei sinistri nella sanità pubblica. 2019. Available online: https://www.quotidianosanita.it/allegati/allegato8049683.pdf (accessed on 20 May 2020).
- Linea Guida Sulla Valutazione Del Processo Di Sanificazione Ambientale Nelle Strutture Ospedaliere e Territoriali Per Il Controllo Delle Infezioni Correlate All’assistenza (ICA). Available online: https://www.anmdo.org/wp-content/uploads/2019/01/libro-uno-finzi-1.pdf (accessed on 20 May 2020).
- Pasquarella, C.; Ciorba, V.; Arnoldo, L.; Auxilia, F.; Baldovin, T.; Barchitta, M.; Bianco, A.; Calagreti, G.; Casini, B.; Cristina, M.L. Hospital hygiene in Italy: The GISIO-SItI survey. Ann. Di Igiene Med. Prev. E Di Comunita 2018, 30, 7–14. [Google Scholar]
- Allegato 22 al Capitolato d’Oneri “Servizi” per l’abilitazione dei Prestatori di “Servizi di Pulizia degli Immobili, Disinfestazione e Sanificazione Impianti” ai fini della partecipazione al Mercato Elettronico della Pubblica Amministrazione Vers. 5.0—May 2019”. Available online: http://www.consip.it (accessed on 20 May 2020).
- AFIDAMP (for conventional cleaning timing procedures). Available online: https://www.afidamp.it/it/shop/vademecum-della-pulizia-professionale-detail.html (accessed on 20 May 2020).
| Drug | Intravenous (€) | Inhalation (€) | Oral (€) | Parenteral (€) |
|---|---|---|---|---|
| Ambisome * | 246.71 | |||
| Amikacin | 1.2–3.06 | |||
| Amoxicillin | 0.09–0.6 | |||
| Amoxicillin/clavulanate | 2.58–5.9 | 0.05–0.33 | ||
| Ampicillin | 1.96–3.93 | 0.99 | ||
| Ampicillin/sulbactam | 4.44–7.86 | |||
| Anidulafungin * | 354 | |||
| Caspofungin * | 560.99 | |||
| Cefixim | 1.14–2.01 | |||
| Cefotaxim | 1.76 | |||
| Ceftazidime | 3.37 | 3.37 | ||
| Ceftriaxone | 0.9–1.32 | |||
| Ciprofloxacin | 0.11–3.96 | 0.11–0.88 | ||
| Clarithromycin | 8.7 | 0.88 | ||
| Clindamicin | 1.64 | 0.84 | ||
| Colistin | 27 | 8.95 | ||
| Daptomicin * | 107.2 | |||
| Fluconazole | 0.54–2 | 0.99–1.54 | ||
| Fosfomycin | 1.2–5.68 | |||
| Ganciclovir * | 13.6 | |||
| Gentamicin | 0.99–1.24 | |||
| Imipenem | 9.24 | |||
| Imipenem/cilast | 9.4–13.58 | |||
| Levofloxacin | 0.7–0.96 | 0.2–1.2 | ||
| Linezolid | 10–151.32 | |||
| Meropenem | 9.9–13.16 | |||
| Metronidazole | 0.9–1.8 | 0.09–0.23 | ||
| Nystatin * | 0.45 | |||
| Oxacillin * | 2.99 | |||
| Piperacillin/tazobactam | 4.43–6.6 | |||
| Teicoplanin | 5.16–57.75 | 5.16 | 36.8 | |
| Tigecycline | 98.27–107.8 | |||
| Trimethoprim/sulfamethoxazole | 13.89 | 0.14–0.22 | ||
| Vancomycin | 2.5–3.06 | 3–3.69 | ||
| Voriconazole | 96.72–96.72 | 18.84–18.84 |
| Populations Characteristics | Unmatched/Matched | PCHS Mean Value | CCC Mean Value | % Bias | % Bias Reduction |
|---|---|---|---|---|---|
| Age | U | 73.000 | 71.804 | 7.4 | |
| M | 73.465 | 73.465 | 0 | 100 | |
| Gender (proportion of males) | U | 0.471 | 0.498 | −5.5 | |
| M | 0.483 | 0.483 | 0 | 100 | |
| Proportion of patients with urinary catheter | U | 0.211 | 0.231 | −4.8 | |
| M | 0.200 | 0.200 | 0 | 100 | |
| Proportion of patients with self-sufficiency | U | 0.649 | 0.626 | 4.9 | |
| M | 0.678 | 0.678 | 0 | 100 | |
| Proportion of patients with pressure sores | U | 0.045 | 0.064 | −8.3 | |
| M | 0.024 | 0.024 | 0 | 100 | |
| Proportion of patients with mechanical ventilation | U | 0.027 | 0.039 | −6.8 | |
| M | 0.010 | 0.010 | 0 | 100 | |
| Proportion of patients with use of antibiotics in the last two weeks | U | 0.058 | 0.091 | −12.7 | |
| M | 0.032 | 0.032 | 0 | 100 | |
| Proportion of patients with parenteral nutrition | U | 0.023 | 0.036 | −7.1 | |
| M | 0.008 | 0.008 | 0 | 100 | |
| Proportion of patients with presence at admission of multi-drug resistant organisms | U | 0.015 | 0.022 | −5.0 |
| Drug | CCC (No HAIs = 191) | PCHS (No HAIs = 100) | PCHS vs. CCC | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Days of Treatment | N. of Treated Pts | Mean Days of Treatment per Pt with HAI | Mean Days of Treatment per Pt with HAI per Specific Drug | Days of Treatment | N. of Treated Pts | Mean Days of Treatment per Pt with HAI | Mean Days of Treatment per Pt with HAI per Specific Drug | Variation in Days of Treatment (%) | |
| Piperacillin/tazobactam | 395 | 45 | 2.07 | 8.78 | 406 | 39 | 4.06 | 10.41 | 96% |
| Levofloxacin | 269 | 42 | 1.41 | 6.40 | 15 | 4 | 0.15 | 3.75 | −89% |
| Ciprofloxacin | 239 | 33 | 1.25 | 7.24 | 55 | 11 | 0.55 | 5.00 | −56% |
| Teicoplanin | 183 | 15 | 0.96 | 12.20 | 63 | 6 | 0.63 | 10.50 | −34% |
| Ceftriaxone | 176 | 22 | 0.92 | 8.00 | 90 | 14 | 0.90 | 6.43 | −2% |
| Meropenem | 158 | 14 | 0.83 | 11.29 | 61 | 6 | 0.61 | 10.17 | −26% |
| Vancomycin | 133 | 15 | 0.70 | 8.87 | 38 | 4 | 0.38 | 9.50 | −45% |
| Colistin | 79 | 5 | 0.41 | 15.80 | 40 | 2 | 0.40 | 20.00 | −3% |
| Fluconazole | 76 | 7 | 0.40 | 10.86 | 16 | 3 | 0.16 | 5.33 | −60% |
| Fosfomycin | 63 | 9 | 0.33 | 7.00 | 2 | 1 | 0.02 | 2.00 | −94% |
| Anidulafungin | 51 | 5 | 0.27 | 10.20 | 0 | 0 | 0.00 | 0.00 | −100% |
| Metronidazole | 45 | 7 | 0.24 | 6.43 | 25 | 3 | 0.25 | 8.33 | 6% |
| Ampicillin/sulbactam | 40 | 5 | 0.21 | 8.00 | 8 | 1 | 0.08 | 8.00 | −62% |
| Amoxicillin/clavulanate | 34 | 5 | 0.18 | 6.80 | 104 | 11 | 1.04 | 9.45 | 484% |
| Imipenem | 30 | 2 | 0.16 | 15.00 | 26 | 3 | 0.26 | 8.67 | 66% |
| Linezolid | 30 | 2 | 0.16 | 15.00 | 58 | 4 | 0.58 | 14.50 | 269% |
| Tigecycline | 28 | 3 | 0.15 | 9.33 | 18 | 2 | 0.18 | 9.00 | 23% |
| Cefixim | 23 | 1 | 0.12 | 23.00 | 3 | 1 | 0.03 | 3.00 | −75% |
| Trimethoprim/sulfamethoxazole | 22 | 3 | 0.12 | 7.33 | 0 | 0 | 0.00 | 0.00 | −100% |
| Ambisome | 21 | 1 | 0.11 | 21.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Gentamicin | 20 | 2 | 0.10 | 10.00 | 2 | 1 | 0.02 | 2.00 | −81% |
| Voriconazole | 19 | 3 | 0.10 | 6.33 | 0 | 0 | 0.00 | 0.00 | −100% |
| Ampicillin | 18 | 3 | 0.09 | 6.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Imipenem/cilast | 16 | 2 | 0.08 | 8.00 | 8 | 1 | 0.08 | 8.00 | −5% |
| Amikacin | 15 | 2 | 0.08 | 7.50 | 25 | 1 | 0.25 | 25.00 | 218% |
| Caspofungin | 13 | 1 | 0.07 | 13.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Ganciclovir | 12 | 1 | 0.06 | 12.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Clarithromycin | 11 | 3 | 0.06 | 3.67 | 14 | 2 | 0.14 | 7.00 | 143% |
| Penicillin | 10 | 1 | 0.05 | 10.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Daptomicin | 9 | 2 | 0.05 | 4.50 | 0 | 0 | 0.00 | 0.00 | −100% |
| Amoxicillin | 8 | 2 | 0.04 | 4.00 | 7 | 2 | 0.07 | 3.50 | 67% |
| Nystatin | 7 | 1 | 0.04 | 7.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Ceftazidime | 6 | 1 | 0.03 | 6.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Clindamicin | 5 | 1 | 0.03 | 5.00 | 0 | 0 | 0.00 | 0.00 | −100% |
| Cefotaxim | 0 | 0 | 0.00 | 0.00 | 11 | 1 | 0.11 | 11.00 | 100% |
| Oxacillin | 0 | 0 | 0.00 | 0.00 | 9 | 1 | 0.09 | 9.00 | 100% |
| Total | 2264 | 1104 | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarricone, R.; Rognoni, C.; Arnoldo, L.; Mazzacane, S.; Caselli, E. A Probiotic-Based Sanitation System for the Reduction of Healthcare Associated Infections and Antimicrobial Resistances: A Budget Impact Analysis. Pathogens 2020, 9, 502. https://doi.org/10.3390/pathogens9060502
Tarricone R, Rognoni C, Arnoldo L, Mazzacane S, Caselli E. A Probiotic-Based Sanitation System for the Reduction of Healthcare Associated Infections and Antimicrobial Resistances: A Budget Impact Analysis. Pathogens. 2020; 9(6):502. https://doi.org/10.3390/pathogens9060502
Chicago/Turabian StyleTarricone, Rosanna, Carla Rognoni, Luca Arnoldo, Sante Mazzacane, and Elisabetta Caselli. 2020. "A Probiotic-Based Sanitation System for the Reduction of Healthcare Associated Infections and Antimicrobial Resistances: A Budget Impact Analysis" Pathogens 9, no. 6: 502. https://doi.org/10.3390/pathogens9060502
APA StyleTarricone, R., Rognoni, C., Arnoldo, L., Mazzacane, S., & Caselli, E. (2020). A Probiotic-Based Sanitation System for the Reduction of Healthcare Associated Infections and Antimicrobial Resistances: A Budget Impact Analysis. Pathogens, 9(6), 502. https://doi.org/10.3390/pathogens9060502






