Staphylococcus aureus Nasal Colonization among Children with Sickle Cell Disease at the Children’s Hospital, Accra: Prevalence, Risk Factors, and Antibiotic Resistance
Abstract
1. Introduction
2. Methodology
2.1. Study Site, Design, and Sampling
2.2. Laboratory Analysis
2.3. Data Analysis
2.4. Ethical Approval
3. Results
3.1. Demographic, Household, and Clinical Features of the Study Participants
3.2. Relationship between Sickle Cell Disease and Staphylococcal Carriage
3.3. Risk Factors for Colonization with S. aureus and MRSA among the Study Participants
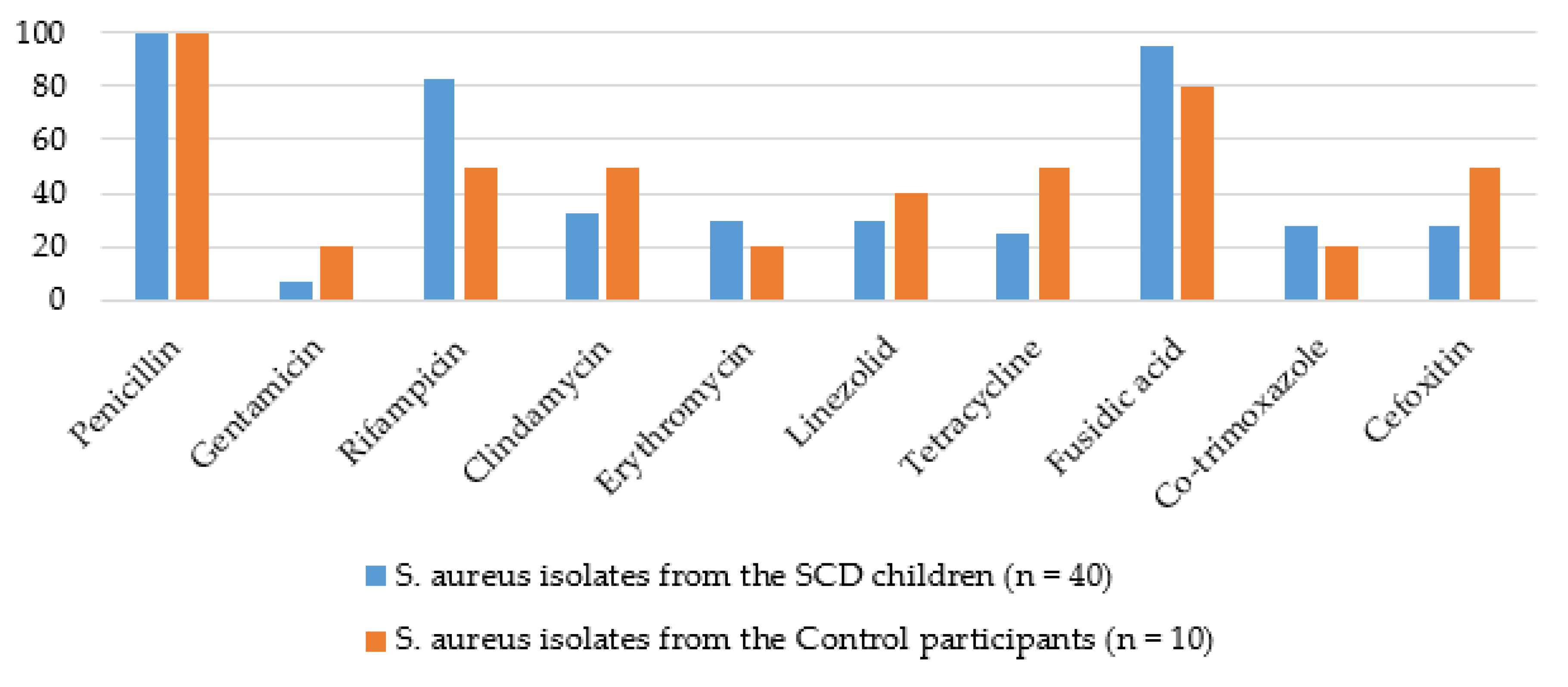
3.4. Patterns of Antimicrobial Resistance among the S. aureus and MRSA Isolates
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fowler, V.; Olsen, M.K.; Corey, G.R.; Woods, C.W.; Cabell, C.H.; Reller, L.B.; Cheng, A.; Dudley, T.; Oddone, E.Z. Clinical Identifiers of Complicated Staphylococcus aureus Bacteremia. Arch. Intern. Med. 2003, 163, 2066. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S.; Newman, M.J.; Oliver-Commey, J.; Bannerman, E.; Dayie, N.T.K.D.; Badoe, E.V. Invasive disease and paediatric carriage of Streptococcus pneumoniae in Ghana. Scand. J. Infect. Dis. 2010, 42, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, J.; Mehl, A.; Askim, Å.; Solligård, E.; Åsvold, B.O.; Damås, J.K. Epidemiology and outcome of Staphylococcus aureus bloodstream infection and sepsis in a Norwegian county 1996–2011: An observational study. BMC Infect. Dis. 2015, 15, 116. [Google Scholar] [CrossRef] [PubMed]
- Todar, K. Todar’s Online Textbook of Bacteriology; Department of Bacteriology, University of Wisconsin-Madison: Madison, WI, USA, 2006. [Google Scholar]
- Kluytmans, J.; van Belkum, A.; Verbrugh, H. Nasal carriage of Staphylococcus aureus: Epidemiology, underlying mechanisms, and associated risks. Clin. Microbiol. Rev. 1997, 10, 505–520. [Google Scholar] [CrossRef] [PubMed]
- Wertheim, H.F.L.; Melles, D.C.; Vos, M.C.; Van Leeuwen, W.; Van Belkum, A.; Verbrugh, H.A.; Nouwen, J.L. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 5, 751–762. [Google Scholar] [CrossRef]
- Eriksen, N.H.; Espersen, F.; Rosdahl, V.; Jensen, K. Carriage of Staphylococcus aureus among 104 healthy persons during a 19-month period. Epidemiol. Infect. 1995, 115, 51–60. [Google Scholar] [CrossRef]
- Hu, L.; Umeda, A.; Kondo, S.; Amako, K. Typing of Staphylococcus aureus colonising human nasal carriers by pulsed-field gel electrophoresis. J. Med. Microbiol. 1995, 42, 127–132. [Google Scholar] [CrossRef]
- Nouwen, J.; Boelens, H.; Van Belkum, A.; Verbrugh, H. Human Factor in Staphylococcus aureus Nasal Carriage. Infect. Immun. 2004, 72, 6685–6688. [Google Scholar] [CrossRef]
- Moran, G.J.; Krishnadasan, A.; Gorwitz, R.J.; Fosheim, G.E.; McDougal, L.K.; Carey, R.B.; Talan, D.A. Methicillin-ResistantS. aureusInfections among Patients in the Emergency Department. N. Engl. J. Med. 2006, 355, 666–674. [Google Scholar] [CrossRef]
- Haenni, M.; Saras, E.; Chatre, P.; Médaille, C.; Bes, M.; Madec, J.-Y.; Laurent, F. A USA300 variant and other human-related methicillin-resistant Staphylococcus aureus strains infecting cats and dogs in France. J. Antimicrob. Chemother. 2011, 67, 326–329. [Google Scholar] [CrossRef]
- Camargo, C.; Cunha, M.; Bonesso, M.F.; Da Cunha, F.P.; Barbosa, A.N.; Fortaleza, C.M.C.B. Systemic CA-MRSA infection following trauma during soccer match in inner Brazil: Clinical and molecular characterization. Diagn. Microbiol. Infect. Dis. 2013, 76, 372–374. [Google Scholar] [CrossRef] [PubMed]
- Quitoco, I.M.Z.; Ramundo, M.S.; Silva-Carvalho, M.C.; Souza, R.R.; Beltrame, C.O.; De Oliveira, T.F.; Araújo, R.; Del Peloso, P.F.; Coelho, L.; Figueiredo, A.M.S. First report in South America of companion animal colonization by the USA1100 clone of community-acquired meticillin-resistant Staphylococcus aureus (ST30) and by the European clone of methicillin-resistant Staphylococcus pseudintermedius (ST71). BMC Res. Notes 2013, 6, 336. [Google Scholar] [CrossRef]
- Casey, J.A.; Cosgrove, S.E.; Stewart, W.F.; Pollak, J.; Schwartz, B.S. A population-based study of the epidemiology and clinical features of methicillin-resistant Staphylococcus aureus infection in Pennsylvania, 2001-2010. Epidemiol. Infect. 2013, 141, 1166–1179. [Google Scholar] [CrossRef] [PubMed]
- Hsueh, P.-R.; Liu, C.-Y.; Luh, K.-T. Current Status of Antimicrobial Resistance in Taiwan. Emerg. Infect. Dis. 2002, 8, 132–137. [Google Scholar] [CrossRef]
- National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am. J. Infect. Control. 2004, 32, 470–485. [Google Scholar] [CrossRef]
- Tiemersma, E.W.; Bronzwaer, S.L.; Lyytikäinen, O.; Degener, J.E.; Schrijnemakers, P.; Bruinsma, N.; Monen, J.; Witte, W.; Grundmann, H. Methicillin-resistant Staphylococcus aureus in Europe, 1999–2002. Emerg. Infect. Dis. 2004, 10, 1627–1634. [Google Scholar] [CrossRef] [PubMed]
- Amaral, M.M.; Coelho, L.; Flores, R.P.; Souza, R.R.; Silva-Carvalho, M.C.; Teixeira, L.; Ferreira-Carvalho, B.T.; Figueiredo, A.M.S. The Predominant Variant of the Brazilian Epidemic Clonal Complex of Methicillin?Resistant Staphylococcus aureus Has an Enhanced Ability to Produce Biofilm and to Adhere to and Invade Airway Epithelial Cells. J. Infect. Dis. 2005, 192, 801–810. [Google Scholar] [CrossRef]
- European Antimicrobial Resistance Surveillance System: Annual Report 2006. Available online: http://www.rivm.nl/earss/Images/EARSS%202006%20Def_tcm61-44176.pdf (accessed on 11 October 2016).
- Centers for Disease Control and Prevention. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus Aureus. 2014. Available online: www.cdc.gov/abcs/reports-findings/survreports/mrsa14.html (accessed on 26 September 2016).
- Elixhauser, A.; Steiner, C. Infections with Methicillin-Resistant Staphylococcus Aureus (MRSA) in U.S. Hospitals, 1993–2005: Statistical Brief #35; Agency for Health Care Policy and Research: Rockville, MD, USA, 2007.
- Klevens, R.M.; Morrison, M.A.; Nadle, J.; Petit, S.; Gershman, K.; Ray, S.; Harrison, L.H.; Lynfield, R.; Dumyati, G.; Townes, J.M.; et al. Invasive Methicillin-Resistant Staphylococcus aureus Infections in the United States. JAMA 2007, 298, 1763. [Google Scholar] [CrossRef]
- Saraf, S.L.; Molokie, R.E.; Nouraie, M.; Sable, C.A.; Luchtman-Jones, L.; Ensing, G.J.; Campbell, A.; Rana, S.R.; Niu, X.M.; Machado, R.; et al. Differences in the clinical and genotypic presentation of sickle cell disease around the world. Paediatr. Respir. Rev. 2013, 15, 4–12. [Google Scholar] [CrossRef]
- Seybold, U.; Supthut-Schröder, B.; Draenert, R.; Hogardt, M.; Bogner, M.J. Prevalence and risk factors of nasal colonization with Staphylococcus aureus–Association with HIV infection in older patients. Scand. J. Infect. Dis. 2009, 41, 63–66. [Google Scholar] [CrossRef]
- Popovich, K.J.; Hota, B.; Aroutcheva, A.; Kurien, L.; Patel, J.; Lyles-Banks, R.; Grasso, A.E.; Spec, A.; Beavis, K.G.; Hayden, M.K.; et al. Community-Associated Methicillin-Resistant Staphylococcus aureus Colonization Burden in HIV-Infected Patients. Clin. Infect. Dis. 2013, 56, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S.; Jamrozy, D.; Mills, R.O.; Dankwah, T.; Amoo, P.K.; Egyir, B.; Badoe, E.V.; Twasam, J.; Bentley, S.D. A genomic infection control study for Staphylococcus aureus in two Ghanaian hospitals. Infect. Drug Resist. 2018, 11, 1757–1765. [Google Scholar] [CrossRef] [PubMed]
- Kateete, D.; Kajumbula, H.; Kaddu-Mulindwa, D.H.; Ssevviri, A.K. Nasopharyngeal carriage rate of Streptococcus pneumoniae in Ugandan children with sickle cell disease. BMC Res. Notes 2012, 5, 28. [Google Scholar] [CrossRef]
- Dayie, N.T.K.D.; Tetteh-Ocloo, G.; Labi, A.-K.; Olayemi, E.; Slotved, H.-C.; Lartey, M.; Donkor, E.S. Pneumococcal carriage among sickle cell disease patients in Accra, Ghana: Risk factors, serotypes and antibiotic resistance. PLoS ONE 2018, 13, e0206728. [Google Scholar] [CrossRef]
- Okuonghae, H.O.; Nwankwo, M.U.; Offor, E.C. Pattern of bacteremia in febrile children with sickle cell anemia. Ann. Trop. Pediatr. 1993, 13, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Akuse, R.M. Variation in the pattern of bacterial infection in patients with sickle cell disease requiring admission. J. Trop. Pediatr. 1996, 42, 318–323. [Google Scholar] [CrossRef]
- Aken’Ova, Y.A.; Bakare, R.A.; Okunade, M.A. Septicaemia in sickle cell anaemia patients: The Ibadan experience. Central Afr. J. Med. 1998, 44, 102–104. [Google Scholar]
- Thanni, L.O. Bacterial osteomyelitis in major sickling haemoglobinopathies: Geographic difference in pathogen prevalence. Afr. Health Sci. 2006, 6, 236–239. [Google Scholar]
- Kizito, M.E.; Mworozi, E.; Ndugwa, C.; Serjeant, G.R. Bacteraemia in homozygous sickle cell disease in Africa: Is pneumococcal prophylaxis justified? Arch. Dis. Child. 2006, 92, 21–23. [Google Scholar] [CrossRef]
- Egyir, B.; Guardabassi, L.; Nielsen, S.S.; Larsen, J.; Addo, K.K.; Newman, M.J.; Larsen, A.R. Prevalence of nasal carriage and diversity of Staphylococcus aureus among inpatients and hospital staff at Korle Bu Teaching Hospital, Ghana. J. Glob. Antimicrob. Resist. 2013, 1, 189–193. [Google Scholar] [CrossRef]
- Egyir, B.; Guardabassi, L.; Esson, J.; Nielsen, S.S.; Newman, M.J.; Addo, K.K.; Larsen, A.R. Insights into Nasal Carriage of Staphylococcus aureus in an Urban and a Rural Community in Ghana. PLoS ONE 2014, 9, e96119. [Google Scholar] [CrossRef]
- Eibach, D.; Nagel, M.; Hogan, B.; Azuure, C.; Krumkamp, R.; Dekker, D.; Gajdiss, M.; Brunke, M.; Sarpong, N.; Owusu-Dabo, E.; et al. Nasal Carriage of Staphylococcus aureus among Children in the Ashanti Region of Ghana. PLoS ONE 2017, 12, e0170320. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S.; Nartey, E. Nasal colonisation of antibiotic resistant bacteria in Ghanaian children less than five years of age. Internet J. Microbiol. 2007, 5, 1–5. [Google Scholar]
- Egyir, B.; Oteng, A.A.; Owusu, E.; Newman, M.J.; Addo, K.K.; Larsen, A.R. Characterization of Staphylococcus aureus from Human Immunodeficiency Virus (HIV) patients in Accra, Ghana. J. Infect. Dev. Ctries. 2016, 10, 453–456. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S.; Badoe, E.V.; Annan, J.A.; Nii-Trebi, N. Colonisation of antibiotic resistant bacteria in a cohort of HIV infected children in Ghana. Pan Afr. Med. J. 2017, 26, 1–7. [Google Scholar]
- Donkor, E.S.; Kotey, F.C.N.; Dayie, N.T.K.D.; Duodu, S.; Tetteh-Quarcoo, P.B.; Osei, M.-M.; Tette, E.M.A. Colonization of HIV-Infected Children with Methicillin-Resistant Staphylococcus aureus. Pathogens 2019, 8, 35. [Google Scholar] [CrossRef]
- Labi, A.-K.; Obeng-Nkrumah, N.; Addison, N.O.; Donkor, E.S. Salmonella blood stream infections in a tertiary care setting in Ghana. BMC Infect. Dis. 2014, 14, 3857. [Google Scholar] [CrossRef]
- Donkor, E.S.; Foster-Nyarko, E.; Enweronu-Laryea, C.C. Relationship between antibiotic resistance and sickle cell anemia: Preliminary evidence from a pediatric carriage study in Ghana. Infect. Drug Resist. 2013, 6, 71–77. [Google Scholar] [CrossRef][Green Version]
- Schaumburg, F.; Biallas, B.; Feugap, E.N.; Alabi, A.; Mordmüller, B.; Kremsner, P.; Grobusch, M.; Lell, B.; Van Der Linden, M.; Peters, G.; et al. Carriage of encapsulated bacteria in Gabonese children with sickle cell anaemia. Clin. Microbiol. Infect. 2013, 19, 235–241. [Google Scholar] [CrossRef]
- Schaumburg, F.; Alabi, A.; Peters, G.; Becker, K. New epidemiology of Staphylococcus aureus infection in Africa. Clin. Microbiol. Infect. 2014, 20, 589–596. [Google Scholar] [CrossRef]
- Ngoa, U.A.; Schaumburg, F.; Adegnika, A.A.; Kösters, K.; Möller, T.; Fernandes, J.F.; Alabi, A.; Issifou, S.; Becker, K.; Grobusch, M.P.; et al. Epidemiology and population structure of Staphylococcus aureus in various population groups from a rural and semi urban area in Gabon, Central Africa. Acta Trop. 2012, 124, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Ebruke, C.; Dione, M.; Walter, B.; Worwui, A.; Adegbola, R.A.; Roca, A.; Antonio, M. High genetic diversity of Staphylococcus aureus strains colonising the nasopharynx of Gambian villagers before widespread use of pneumococcal conjugate vaccines. BMC Microbiol. 2016, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Marriott, I.; Huet-Hudson, Y.M. Sexual Dimorphism in Innate Immune Responses to Infectious Organisms. Immunol. Res. 2006, 34, 177–192. [Google Scholar] [CrossRef]
- Luzar, M.A.; Coles, G.A.; Faller, B.; Slingeneyer, A.; Dah, G.D.; Briat, C.; Wone, C.; Knefati, Y.; Kessler, M.; Peluso, F. Staphylococcus aureus Nasal Carriage and Infection in Patients on Continuous Ambulatory Peritoneal Dialysis. N. Engl. J. Med. 1990, 322, 505–509. [Google Scholar] [CrossRef]
- Cole, A.M.; Dewan, P.; Ganz, T. Innate Antimicrobial Activity of Nasal Secretions. Infect. Immun. 1999, 67, 3267–3275. [Google Scholar] [CrossRef]
- Olsen, K.; Falch, B.M.; Danielsen, K.; Johannessen, M.; Sollid, J.U.E.; Thune, I.; Grimnes, G.; Jorde, R.; Simonsen, G.S.; Furberg, A.-S. Staphylococcus aureus nasal carriage is associated with serum 25-hydroxyvitamin D levels, gender and smoking status. The Tromsø Staph and Skin Study. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 31, 465–473. [Google Scholar] [CrossRef]
- Winters, A.C.; Kethman, W.; Kruse-Jarres, R.; Kanter, J. Vitamin D Insufficiency is a Frequent Finding in Pediatric and Adult Patients with Sickle Cell Disease and Correlates with Markers of Cell Turnover. J. Nutr. Disord. Ther. 2014, 4, 140. [Google Scholar] [CrossRef]
- Lemma, M.T.; Zenebe, Y.; Tulu, B.; Mekonnen, D.; Mekonnen, Z. Methicillin Resistant Staphylococcus aureus among HIV Infected Pediatric Patients in Northwest Ethiopia: Carriage Rates and Antibiotic Co-Resistance Profiles. PLoS ONE 2015, 10, e0137254. [Google Scholar] [CrossRef]
- Fritz, S.A.; Garbutt, J.; Elward, A.; Shannon, W.; Storch, G.A. Prevalence of and Risk Factors for Community-Acquired Methicillin-Resistant and Methicillin-Sensitive Staphylococcus aureus Colonization in Children Seen in a Practice-Based Research Network. Pediatrics 2008, 121, 1090–1098. [Google Scholar] [CrossRef]
- Bogaert, D.; van Belkum, A.; Sluijter, M.; Luijendijk, A.; de Groot, R.; Rumke, H.C.; Verbrugh, H.A.; Hermans, P.W. Colonization by Streptococcus pneumoniae and Staphylococcus aureus in healthy children. Lancet 2004, 363, 1871–1872. [Google Scholar] [CrossRef]
- Donkor, E.S.; Dayie, N.T.; Tette, E.M.A. Methicillin-Resistant Staphylococcus aureus in Ghana: Past, Present, and Future. Microb. Drug Resist. 2019, 25, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, I.H.; Koken, R.; Bukulmez, A.; Özdemir, M.; Safak, B.; Cetinkaya, Z. Nasal carriage ofStaphylococcus aureusin 4-6 age groups in healthy children in Afyonkarahisar, Turkey. Acta Paediatr. 2007, 96, 1043–1046. [Google Scholar] [CrossRef] [PubMed]
- Zanelli, G.; Sansoni, A.; Zanchi, A.; Cresti, S.; Pollini, S.; Rossolini, G.M.; Cellesi, C. Staphylococcus aureus nasal carriage in the community: A survey from central Italy. Epidemiol. Infect. 2002, 129, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Halablab, M.A.; Hijazi, S.M.; Fawzi, M.A.; Araj, G.F. Staphylococcus aureus nasal carriage rate and associated risk factors in individuals in the community. Epidemiol. Infect. 2009, 138, 702–706. [Google Scholar] [CrossRef]
- Miller, M.; Cook, H.A.; Furuya, E.Y.; Bhat, M.; Lee, M.-H.; Vavagiakis, P.; Visintainer, P.; Vasquez, G.; Larson, E.; Lowy, F.D. Staphylococcus aureus in the Community: Colonization Versus Infection. PLoS ONE 2009, 4, e6708. [Google Scholar] [CrossRef]
- Regev-Yochay, G.; Raz, M.; Carmeli, Y.; Shainberg, B.; Navon-Venezia, S.; Pinco, E.; Leavitt, A.; Keller, N.; Rahav, G.; Malley, R.; et al. Parental Staphylococcus aureus Carriage is Associated With Staphylococcal Carriage in Young Children. Pediatr. Infect. Dis. J. 2009, 28, 960–965. [Google Scholar] [CrossRef]
- Madani, T.A.; Al-Abdullah, N.A.; Al-Sanousi, A.A.; Ghabrah, T.M.; Afandi, S.Z.; Bajunid, H.A. Methicillin-Resistant Staphylococcus aureus in Two Tertiary-Care Centers in Jeddah, Saudi Arabia. Infect. Control. Hosp. Epidemiol. 2001, 22, 211–216. [Google Scholar] [CrossRef]
- Köck, R.; Winner, K.; Schaumburg, F.; Jurke, A.; Rossen, J.W.; Friedrich, A.W. Admission prevalence and acquisition of nasal carriage of methicillin-resistant Staphylococcus aureus (MRSA) in German rehabilitation centres. J. Hosp. Infect. 2014, 87, 115–118. [Google Scholar] [CrossRef]
- Creech, C.B.; Kernodle, D.S.; Alsentzer, A.; Wilson, C.; Edwards, K.M. Increasing Rates of Nasal Carriage of Methicillin-Resistant Staphylococcus aureus in Healthy Children. Pediatr. Infect. Dis. J. 2005, 24, 617–621. [Google Scholar] [CrossRef]
- Dekker, D.; Wolters, M.; Mertens, E.; Boahen, K.G.; Krumkamp, R.; Eibach, D.; Schwarz, N.G.; Adu-Sarkodie, Y.; Rohde, H.; Chistner, M.; et al. Antibiotic resistance and clonal diversity of invasive Staphylococcus aureus in the rural Ashanti Region, Ghana. BMC Infect. Dis. 2016, 16, 720. [Google Scholar] [CrossRef]
- Howe, R.A.; Noel, A.; Bowker, K.E.; Enne, V.I.; Walsh, T.R.; MacGowan, A.P. Emergence of linezolid (LIN) resistance in Staphylococcus aureus can be associated with loss of erythromycin (ERY) resistance. In Program and Abstracts of the Forty-Second Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, CA, USA, 2002; American Society for Microbiology: Washington, DC, USA, 2002; p. 75. [Google Scholar]
- Morales, G.; Baos, E.; Arribi, A.; Andrade, R.; Picazo, J.J.; Candel, F.J.; Peláez, B.; De La Torre, M.-Á.; Fereres, J.; Sánchez-García, M. Resistance to Linezolid Is Mediated by the cfr Gene in the First Report of an Outbreak of Linezolid?Resistant Staphylococcus aureus. Clin. Infect. Dis. 2010, 50, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Long, K.S.; Vester, B. Resistance to Linezolid Caused by Modifications at Its Binding Site on the Ribosome. Antimicrob. Agents Chemother. 2011, 56, 603–612. [Google Scholar] [CrossRef]
- Shore, A.C.; Lazaris, A.; Kinnevey, P.; Brennan, O.M.; Brennan, G.I.; O’Connell, B.; Feßler, A.T.; Schwarz, S.; Coleman, D.C. First Report of cfr-Carrying Plasmids in the Pandemic Sequence Type 22 Methicillin-Resistant Staphylococcus aureus Staphylococcal Cassette Chromosome mec Type IV Clone. Antimicrob. Agents Chemother. 2016, 60, 3007–3015. [Google Scholar] [CrossRef] [PubMed]
- A Mitchison, D. Role of individual drugs in the chemotherapy of tuberculosis. Int. J. Tuberc. Lung Dis. 2000, 4, 796–806. [Google Scholar] [PubMed]
- Cartwright, E.; Paterson, G.K.; Raven, K.E.; Harrison, E.M.; Gouliouris, T.; Kearns, A.; Pichon, B.; Edwards, G.; Skov, R.L.; Larsen, A.R.; et al. Use of Vitek 2 antimicrobial susceptibility profile to identify mecC in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 2013, 51, 2732–2734. [Google Scholar] [CrossRef] [PubMed]
- Paterson, G.K.; Morgan, F.J.E.; Harrison, E.M.; Cartwright, E.J.P.; Torok, E.; Zadoks, R.N.; Parkhill, J.; Peacock, S.J.; Holmes, M.A. Prevalence and characterization of human mecC methicillin-resistant Staphylococcus aureus isolates in England. J. Antimicrob. Chemother. 2013, 69, 907–910. [Google Scholar] [CrossRef]
- Donkor, E.S.; Tetteh-Quarcoo, P.B.; Nartey, P.; Agyeman, I.O. Self-Medication Practices with Antibiotics among Tertiary Level Students in Accra, Ghana: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2012, 9, 3519–3529. [Google Scholar] [CrossRef]
- Donkor, E.S.; Newman, M.J.; Yeboah-Manu, D. Epidemiological aspects of non-human antibiotic usage and resistance: Implications for the control of antibiotic resistance in Ghana. Trop. Med. Int. Health 2012, 17, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 1–10. [Google Scholar] [CrossRef] [PubMed]
| Demographic and Household Characteristics | SCD Group | Control Group | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Gender | ||||
| Male | 58 | 48.3 | 50 | 50.0 |
| Female | 62 | 51.7 | 50 | 50.0 |
| Current school enrolment | ||||
| Yes | 104 | 86.7 | 97 | 97.0 |
| No | 16 | 13.3 | 3 | 3.0 |
| Type of residence | ||||
| Self-contained | 37 | 30.8 | 38 | 38.0 |
| Compound | 83 | 69.2 | 61 | 61.0 |
| Presence of health worker in household | ||||
| Yes | 3 | 2.5 | 0 | 0 |
| No | 117 | 97.5 | 100 | 100 |
| Hand washing with soap | ||||
| Rarely | 50 | 41.7 | 45 | 45.0 |
| Often | 70 | 58.3 | 55 | 55.0 |
| Clinical Features | SCD Group | Control Group | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Self-reported self-medication * | ||||
| Yes | 24 | 20 | 23 | 23.0 |
| No | 96 | 80 | 77 | 77.0 |
| Penicillin prophylaxis | ||||
| Yes | 116 | 96.7 | 0 | 0 |
| No | 4 | 3.3 | 100 | 100 |
| History of hospitalization in the past year | ||||
| Yes | 49 | 40.8 | 8 | 8.0 |
| No | 71 | 59.2 | 92 | 92.0 |
| Chronic skin condition | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 120 | 100 | 100 | 100 |
| History of pneumonia | ||||
| Yes | 8 | 6.7 | 0 | 0 |
| No | 112 | 93.3 | 100 | 100 |
| History of TB | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 120 | 100 | 100 | 100 |
| History of surgery | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 120 | 100 | 100 | 100 |
| Underlying disease | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 120 | 100 | 100 | 100 |
| History of blood transfusion | ||||
| Yes | 42 | 35 | 0 | 0 |
| No | 78 | 65 | 100 | 100 |
| SCD Group | Control Group | |||
|---|---|---|---|---|
| Risk Factor | OR (95% CI) | p Value | OR (95% CI) | p Value |
| Age | 1.275 (1.084–1.499) | 0.003 | N/A | N/A |
| Male gender | 0.344 (0.142–0.833) | 0.018 | N/A | N/A |
| Living in SC apartments | 3.632 (1.108–11.906) | 0.033 | N/A | N/A |
| Practice of self-medication | 0.233 (0.059–0.927) | 0.039 | N/A | N/A |
| Hospitalization in the past year | N/A | N/A | 14.333 (1.023–200.907) | 0.048 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Appiah, V.A.; Pesewu, G.A.; Kotey, F.C.N.; Boakye, A.N.; Duodu, S.; Tette, E.M.A.; Nyarko, M.Y.; Donkor, E.S. Staphylococcus aureus Nasal Colonization among Children with Sickle Cell Disease at the Children’s Hospital, Accra: Prevalence, Risk Factors, and Antibiotic Resistance. Pathogens 2020, 9, 329. https://doi.org/10.3390/pathogens9050329
Appiah VA, Pesewu GA, Kotey FCN, Boakye AN, Duodu S, Tette EMA, Nyarko MY, Donkor ES. Staphylococcus aureus Nasal Colonization among Children with Sickle Cell Disease at the Children’s Hospital, Accra: Prevalence, Risk Factors, and Antibiotic Resistance. Pathogens. 2020; 9(5):329. https://doi.org/10.3390/pathogens9050329
Chicago/Turabian StyleAppiah, Vera A., George A. Pesewu, Fleischer C. N. Kotey, Alahaman Nana Boakye, Samuel Duodu, Edem M. A. Tette, Mame Y. Nyarko, and Eric S. Donkor. 2020. "Staphylococcus aureus Nasal Colonization among Children with Sickle Cell Disease at the Children’s Hospital, Accra: Prevalence, Risk Factors, and Antibiotic Resistance" Pathogens 9, no. 5: 329. https://doi.org/10.3390/pathogens9050329
APA StyleAppiah, V. A., Pesewu, G. A., Kotey, F. C. N., Boakye, A. N., Duodu, S., Tette, E. M. A., Nyarko, M. Y., & Donkor, E. S. (2020). Staphylococcus aureus Nasal Colonization among Children with Sickle Cell Disease at the Children’s Hospital, Accra: Prevalence, Risk Factors, and Antibiotic Resistance. Pathogens, 9(5), 329. https://doi.org/10.3390/pathogens9050329





