Transstadial Transmission from Nymph to Adult of Coxiella burnetii by Naturally Infected Hyalomma lusitanicum
Abstract
1. Introduction
2. Results and Discussion
3. Materials and Methods
3.1. Ticks
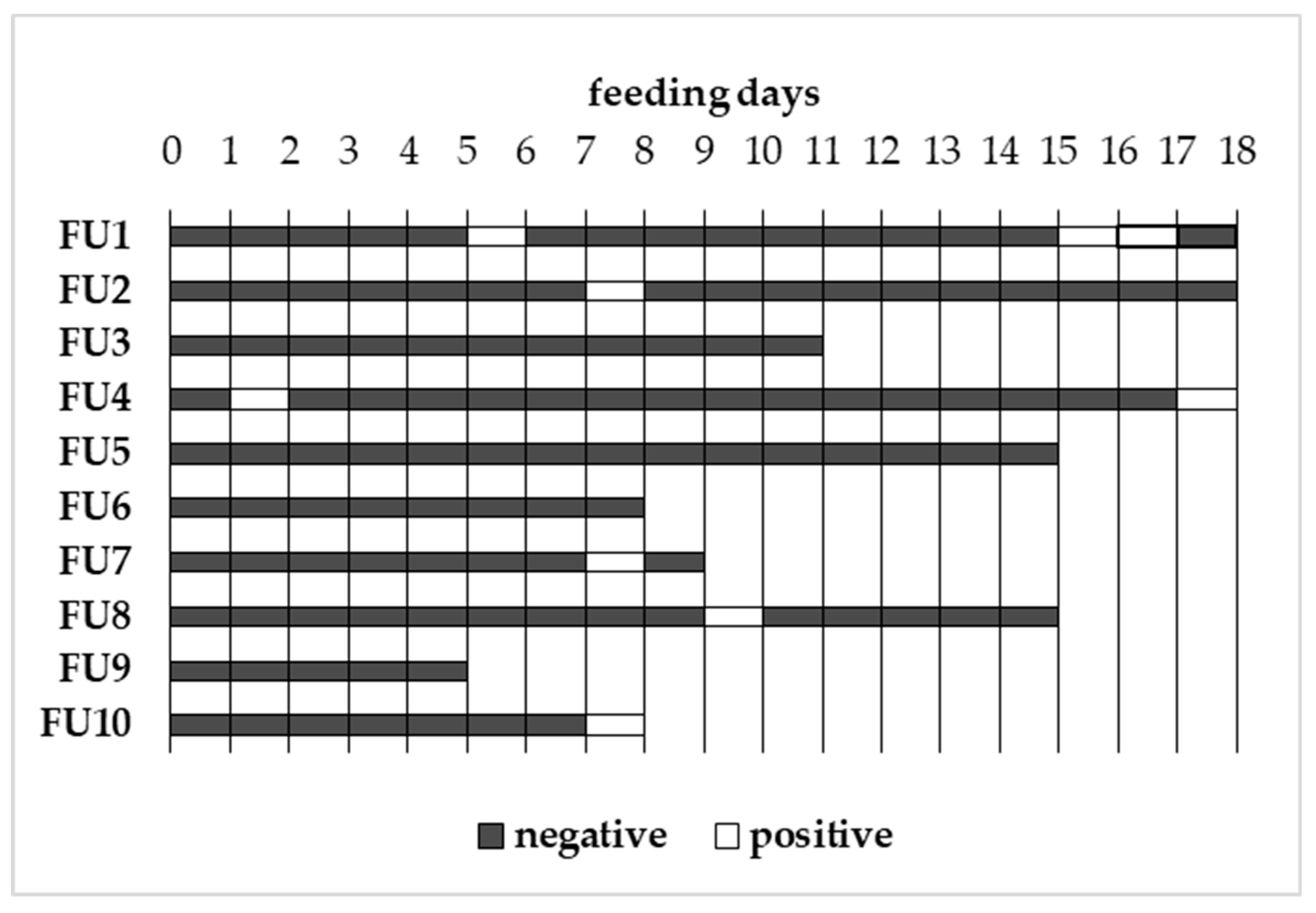
3.2. Artificial Tick Feeding
3.3. Sample Preparation and PCR Analysis
3.4. Data Analyses
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maurin, M.; Raoult, D. Q Fever. Clin. Microbiol. Rev. 1999, 12, 518–553. [Google Scholar] [CrossRef] [PubMed]
- Gürtler, L.; Bauerfeind, U.; Blümel, J.; Burger, R.; Drosten, C.; Gröner, A.; Heiden, M.; Hildebrandt, M.; Jansen, B.; Offergeld, R.; et al. Coxiella burnetii - Pathogenic Agent of Q (Query) Fever. Transfus. Med. Hemother. 2014, 41, 60–72. [Google Scholar] [PubMed]
- Duron, O.; Sidi-Boumedine, K.; Rousset, E.; Moutailler, S.; Jourdain, E. The Importance of Ticks in Q Fever Transmission: What Has (and Has Not) Been Demonstrated? Trends Parasitol. 2015, 31, 536–552. [Google Scholar] [CrossRef] [PubMed]
- Eldin, C.; Mélenotte, C.; Mediannikov, O.; Ghigo, E.; Million, M.; Edouard, S.; Mege, J.L.; Maurin, M.; Raoult, D. From Q Fever to Coxiella burnetii Infection: A Paradigm Change. Clin. Microbiol. Rev. 2017, 30, 115–190. [Google Scholar] [CrossRef]
- Barandika, J.F.; Hurtado, A.; García-Sanmartín, J.; Juste, R.A.; Anda, P.; García-Pérez, A.L. Prevalence of tick-borne zoonotic bacteria in questing adult ticks from northern Spain. Vector Borne Zoonotic Dis. 2008, 8, 829–835. [Google Scholar] [CrossRef]
- Astobiza, I.; Barral, M.; Ruiz-Fons, F.; Barandika, J.F.; Gerrikagoitia, X.; Hurtado, A.; García-Pérez, A.L. Molecular investigation of the occurrence of Coxiella burnetii in wildlife and ticks in an endemic area. Vet. Microbiol. 2011, 147, 190–194. [Google Scholar] [CrossRef]
- Toledo, A.; Jado, I.; Olmeda, A.S.; Casado-Nistal, M.A.; Gil, H.; Escudero, R.; Anda, A.P. Detection of Coxiella burnetii in Ticks Collected from Central Spain. Vector Borne Zoonotic Dis. 2009, 9, 465–468. [Google Scholar] [CrossRef]
- González, J.; González, M.G.; Valcárcel, F.; Sánchez, M.; Martín-Hernández, R.; Tercero, J.M.; Olmeda, A.S. Prevalence of Coxiella burnetii (Legionellales: Coxiellaceae) Infection Among Wildlife Species and the Tick Hyalomma lusitanicum (Acari: Ixodidae) in a Meso-Mediterranean Ecosystem. J. Med. Entomol. 2020, 57, 551–556. [Google Scholar] [CrossRef]
- González-Barrio, D.; Maio, E.; Vieira-Pinto, M.; Ruiz-Fons, F. European Rabbits as Reservoir for Coxiella burnetii. Emerg. Infect. Dis. 2015, 21, 1055–1058. [Google Scholar] [CrossRef]
- González-Barrio, D.; Almería, S.; Caro, M.R.; Salinas, J.; Ortiz, J.A.; Gortázar, C.; Ruiz-Fons, F. Coxiella burnetii Shedding by Farmed Red Deer (Cervus elaphus). Transbound. Emerg. Dis. 2015, 62, 572–574. [Google Scholar] [CrossRef]
- Bonnet, S.; Liu, X.Y. Laboratory artificial infection of hard ticks: A tool for the analysis of tick-borne pathogen transmission. Acarologia 2012, 52, 453–464. [Google Scholar] [CrossRef]
- Körner, S.; Makert, G.R.; Mertens-Scholz, K.; Henning, K.; Pfeffer, M.; Starke, A.; Nijhof, A.M.; Ulbert, S. Uptake and fecal excretion of Coxiella burnetii by Ixodes ricinus and Dermacentor marginatus ticks. Parasites Vectors 2020, 13, 75. [Google Scholar] [CrossRef] [PubMed]
- Kröber, T.; Guerin, P.M. In vitro feeding assays for hard ticks. Trends Parasitol. 2007, 23, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Duron, O. The IS1111 insertion sequence used for detection of Coxiella burnetii is widespread in Coxiella -like endosymbionts of ticks. Fems Microbiol. Lett. 2015, 362, fnv132. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.F.; Burgdorfer, W.; Aeschlimann, A. Sexual Transmission of Spotted Fever Group Rickettsiae by Infected Male Ticks: Detection of Rickettsiae in Immature Spermatozoa of Ixodes ricinus. Infect. Immun. 1980, 27, 638–642. [Google Scholar] [CrossRef]
- Gonzalez, J.P.; Camicas, J.L.; Cornet, J.P.; Faye, O.; Wilson, M.L. Sexual and transovarian transmission of Crimean-Congo haemorrhagic fever virus in Hyalomma truncatum ticks. Res. Virol. 1992, 143, 23–28. [Google Scholar] [CrossRef]
- Alekseev, A.N.; Dubinina, H.V.; Rijpkema, S.G.T.; Schouls, L.M. Sexual transmission of Borrelia garinii by male Ixodes persulcatus ticks (Acari, Ixodidae). Exp. Appl. Acarol. 1999, 23, 165–169. [Google Scholar] [CrossRef]
- Sakamoto, J.M.; Ng, T.F.F.; Suzuki, Y.; Tsujimoto, H.; Deng, X.; Delwart, E.; Rasgon, J.L. Bunyaviruses are common in male and female Ixodes scapularis ticks in central Pennsylvania. PeerJ 2016, 4, e2324. [Google Scholar] [CrossRef]
- González, J.; Valcárcel, F.; Aguilar, A.; Olmeda, A.S. In vitro feeding of Hyalomma lusitanicum ticks on artificial membranes. Exp. Appl. Acarol. 2017, 72, 449–459. [Google Scholar] [CrossRef]
- Hoogstraal, H. Ticks. In Parasites, Pests and Predators; Gaafar, S.M., Howard, W.E., Marsh, R.E., Eds.; Elsevier Science Publishers: Amsterdam, The Netherlands, 1985; Volume 3, pp. 347–370. [Google Scholar]
- Reuben Kaufman, W. Tick-host interaction: A synthesis of current concepts. Parasitol. Today 1989, 5, 47–56. [Google Scholar] [CrossRef]
- Richards, S.; Langley, R.; Apperson, C.; Watson, E. Do Tick Attachment Times Vary between Different Tick-Pathogen Systems? Environments 2017, 4, 37. [Google Scholar] [CrossRef]
- WHO. Report of WHO Workshop on Q Fever, Giessen, 2–5 September 1986. Available online: https://apps.who.int/iris/handle/10665/59435 (accessed on 11 August 2020).
- Voordouw, M.J. Co-feeding transmission in Lyme disease pathogens. Parasitology 2015, 142, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Tilburg, J.J.H.C.; Melchers, W.J.G.; Pettersson, A.M.; Rossen, J.W.A.; Hermans, M.H.A.; van Hannen, E.J.; Nabuurs-Franssen, M.H.; de Vries, M.C.; Horrevorts, A.M.; Klaassen, C.H. Interlaboratory Evaluation of Different Extraction and Real-Time PCR Methods for Detection of Coxiella burnetii DNA in Serum. J. Clin. Microbiol. 2010, 48, 3923–3927. [Google Scholar] [CrossRef]
- SPSS Inc. IBM SPSS Statistics 20; IBM Company: Armonk, NY, USA, 2011. [Google Scholar]
| Feeding Unit | Number of Ticks | Number of Females | Number of Males | Feeding Rate 1 (%) | Degree of Engorgement 2 | ||
|---|---|---|---|---|---|---|---|
| GF | EF | UF | |||||
| 1 | 6 | 3 | 3 | 100.0 | 3 | ||
| 2 | 10 | 6 | 4 | 33.3 | 2 | 1 | 3 |
| 3 | 8 | 4 | 4 | 25.0 | 1 | 1 | 2 |
| 4 | 8 | 4 | 4 | 25.0 | 1 | 3 | |
| 5 | 10 | 6 | 4 | 16.7 | 1 | 1 | 4 |
| 6 | 8 | 4 | 4 | 0 | 1 | 3 | |
| 7 | 7 | 5 | 2 | 0 | 1 | 4 | |
| 8 | 9 | 6 | 3 | 0 | 6 | ||
| 9 | 7 | 4 | 3 | 0 | 4 | ||
| 10 | 7 | 5 | 2 | 0 | 1 | 4 | |
| Feeding Units | Mean Feeding Rate 1 (%) | Positive Ticks (%) | Positive Females (%) | Positive Males (%) |
|---|---|---|---|---|
| With GF (N = 5) | 40.0 | 26.2a | 39.1a | 10.5a |
| Without GF (N = 5) | 0 | 47.4b | 54.2a | 35.7a |
| Total | 20.0 | 36.2 | 46.8 | 21.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
González, J.; González, M.G.; Valcárcel, F.; Sánchez, M.; Martín-Hernández, R.; Tercero, J.M.; Olmeda, A.S. Transstadial Transmission from Nymph to Adult of Coxiella burnetii by Naturally Infected Hyalomma lusitanicum. Pathogens 2020, 9, 884. https://doi.org/10.3390/pathogens9110884
González J, González MG, Valcárcel F, Sánchez M, Martín-Hernández R, Tercero JM, Olmeda AS. Transstadial Transmission from Nymph to Adult of Coxiella burnetii by Naturally Infected Hyalomma lusitanicum. Pathogens. 2020; 9(11):884. https://doi.org/10.3390/pathogens9110884
Chicago/Turabian StyleGonzález, Julia, Marta G. González, Félix Valcárcel, María Sánchez, Raquel Martín-Hernández, José M. Tercero, and A. Sonia Olmeda. 2020. "Transstadial Transmission from Nymph to Adult of Coxiella burnetii by Naturally Infected Hyalomma lusitanicum" Pathogens 9, no. 11: 884. https://doi.org/10.3390/pathogens9110884
APA StyleGonzález, J., González, M. G., Valcárcel, F., Sánchez, M., Martín-Hernández, R., Tercero, J. M., & Olmeda, A. S. (2020). Transstadial Transmission from Nymph to Adult of Coxiella burnetii by Naturally Infected Hyalomma lusitanicum. Pathogens, 9(11), 884. https://doi.org/10.3390/pathogens9110884






