Faecal Indicator Bacteria and Pseudomonas aeruginosa in Marine Coastal Waters: Is there a Relationship?
Abstract
1. Introduction
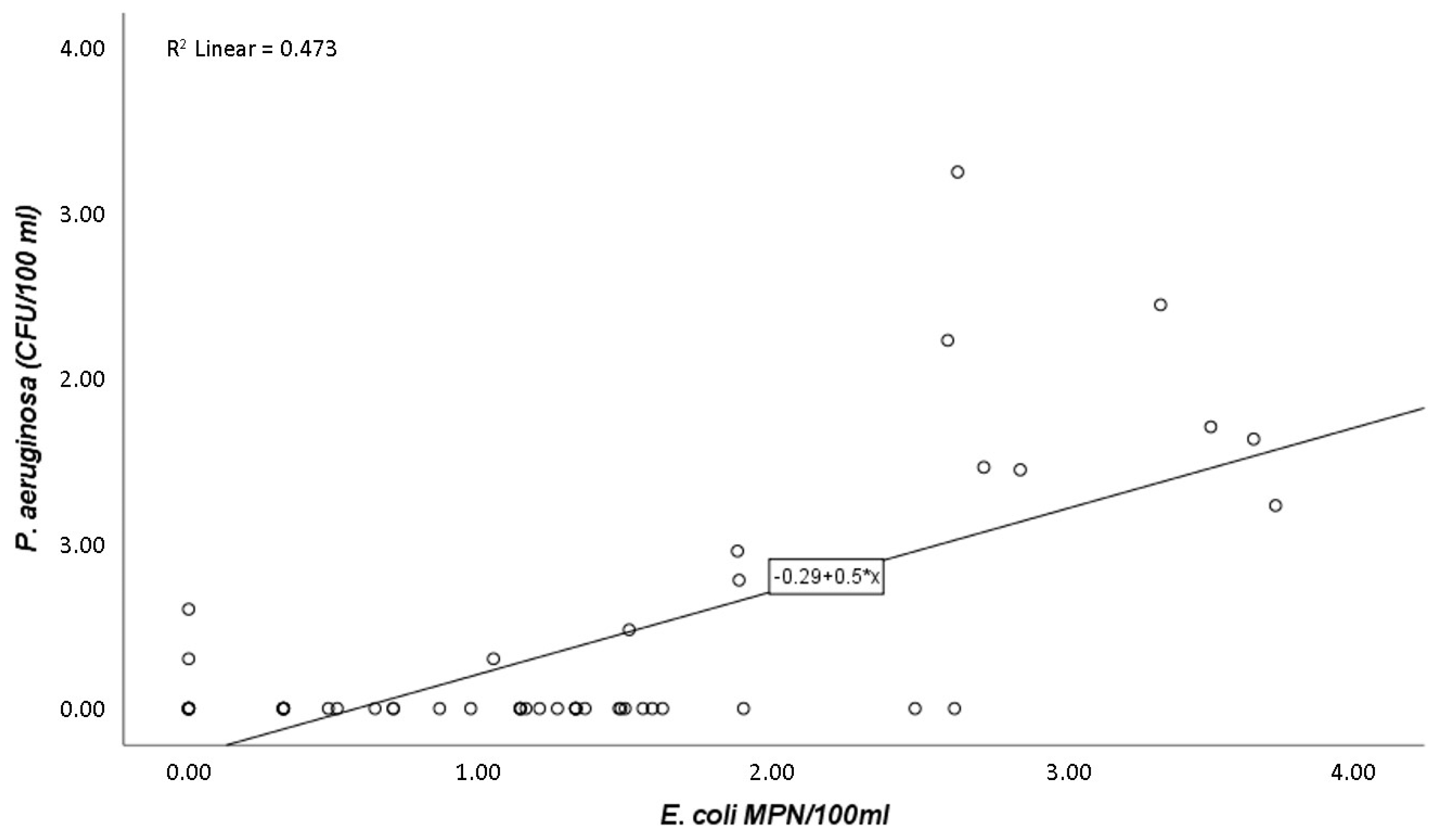
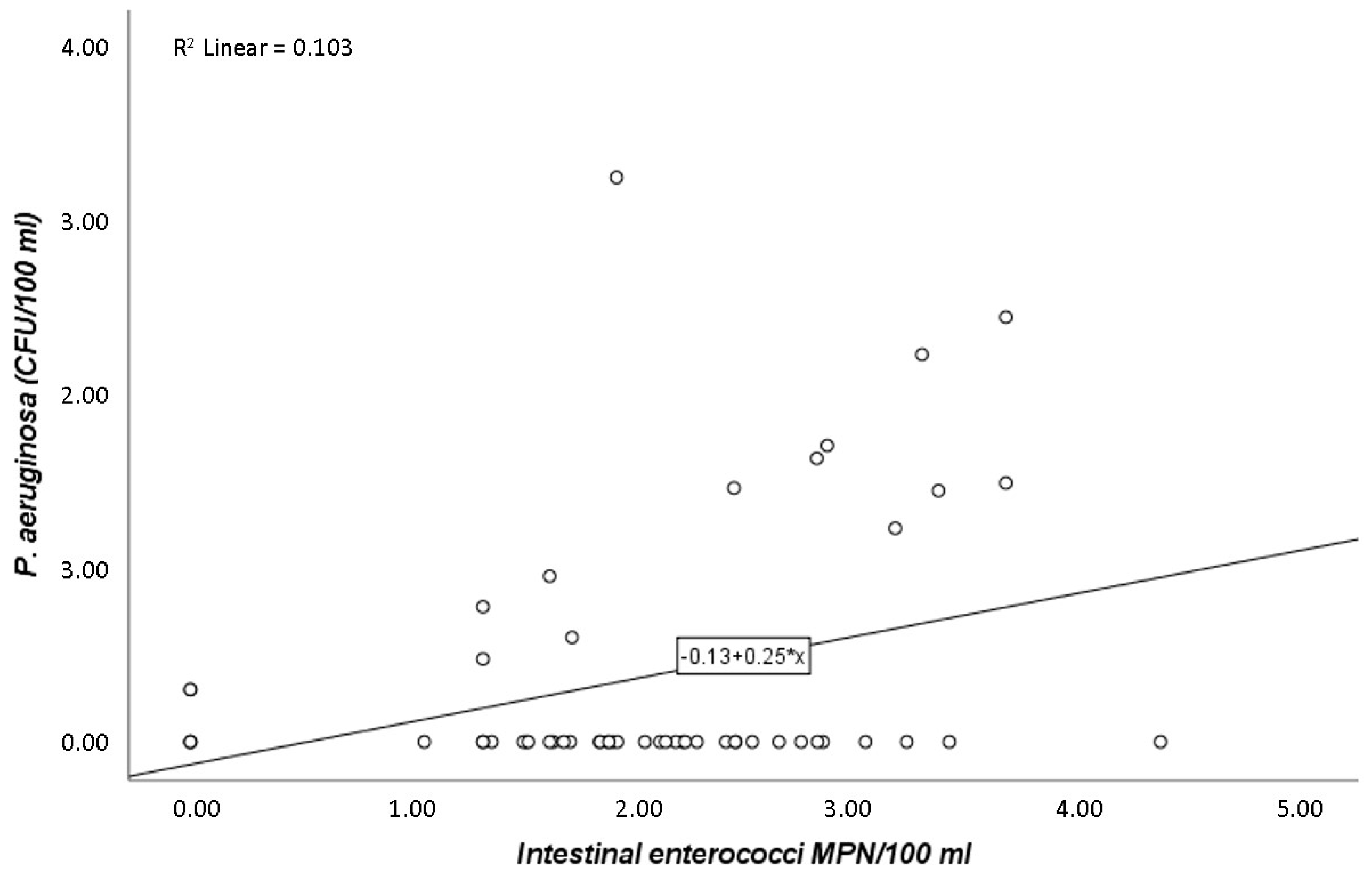
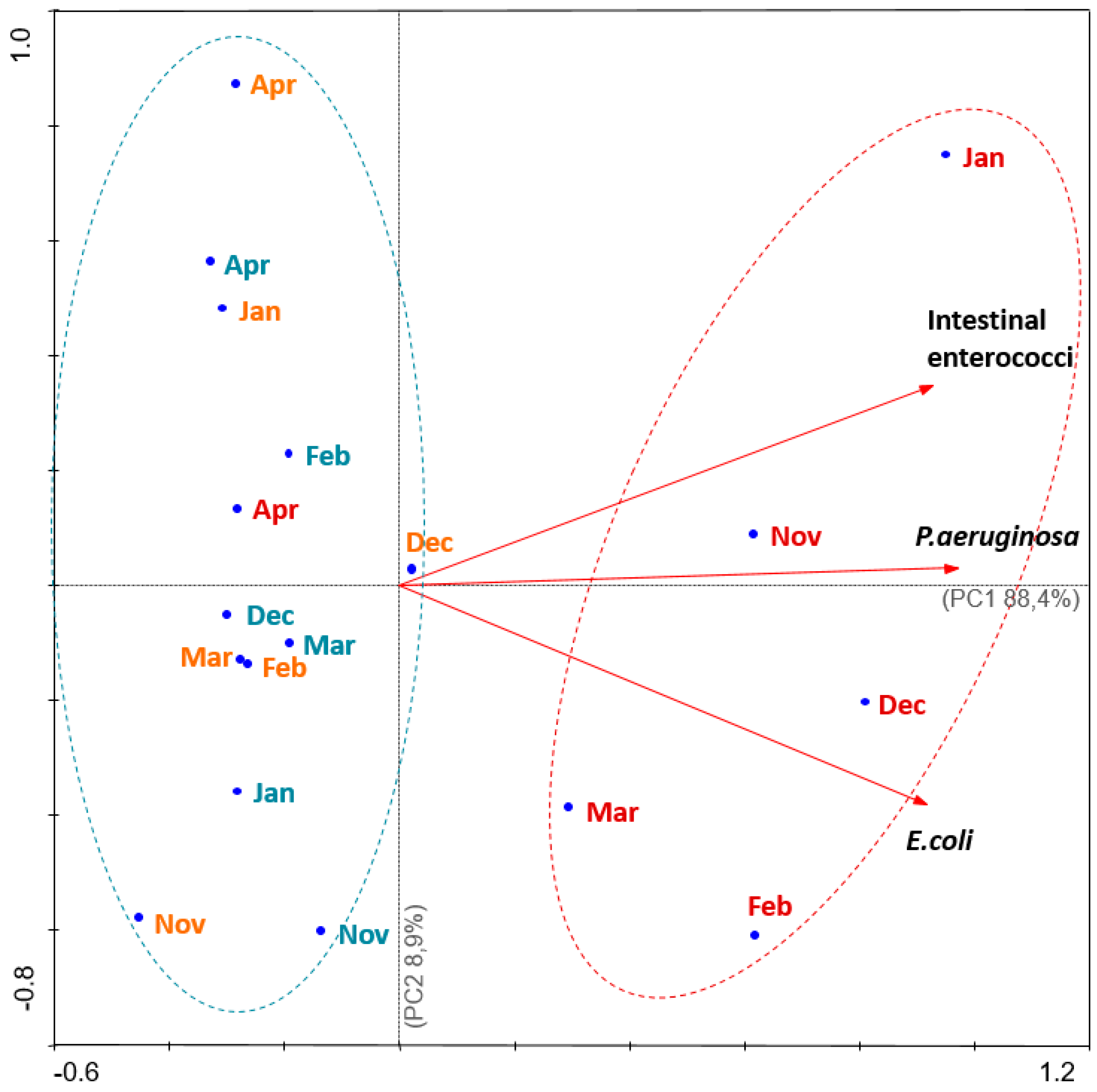
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Area and Sample Collection
4.2. Enumeration of E. coli and Intestinal Enterococci
4.3. Enumeration of Pseudomonas aeruginosa
4.4. Statistical Analysis
Author Contributions
Funding
Conflicts of Interest
References
- Semeoshenkova, V.; Newton, A.; Contin, A.; Greggio, N. Development and application of an Integrated Beach Quality Index (BQI). Ocean Coast. Manag. 2017, 143, 74–86. [Google Scholar] [CrossRef]
- Mansilha, C.R.; Coelho, C.A.; Heitor, A.M.; Amado, J.; Martins, J.P.; Gameiro, P. Bathing waters: New directive, new standards, new quality approach. Mar. Pollut. Bull. 2009, 58, 1562–1565. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.J.; Tsai, Y.L.; Lang, A.L.; Sangermano, L.R. Evaluation of colilert-marine water for detection of total coliforms and Escherichia coli in the marine-environment. Appl. Environ. Microbiol. 1993, 59, 786–790. [Google Scholar] [PubMed]
- Bartram, J.; Rees, G. Monitoring Bathing Waters—A Practical Guide to the Design and Implementation of Assessments and Monitoring Programmes; WHO: Geneva, Switzerland, 2000; ISBN 0419243801. [Google Scholar]
- Aragones, L.; Lopez, I.; Palazon, A.; Lopez-Ubeda, R.; Garcia, C. Evaluation of the quality of coastal bathing waters in Spain through fecal bacteria Escherichia coli and Enterococcus. Sci. Total Environ. 2016, 566, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Baudart, J.; Servais, P.; De Paoli, H.; Henry, A.; Lebaron, P. Rapid enumeration of Escherichia coli in marine bathing waters: Potential interference of non-target bacteria. J. Appl. Microbiol. 2009, 107, 2054–2062. [Google Scholar] [CrossRef] [PubMed]
- European Union. Directive 2006/7/EC of the European Parliament and of the Council of 15 February 2006 concerning the management of bathing water quality and repealing Directive 76/160/EEC. Off. J. Eur. Union 2006, L 064, 37–51.
- López Martínez, I.; Álvarez Díaz, C.; Gil Díaz, J.L.; Revilla Cortezón, J.A.; Juanes, J.A. The European bathing water directive: Application and consequences in quality monitoring programs. J. Environ. Monit. 2010, 12, 369–376. [Google Scholar] [CrossRef]
- López, I.; Álvarez, C.; Gil, J.L.; Revilla, J.A. Methodology to elaborate the bathing water profile on urban beaches, according to the requirements of the European Directive 2006/7/EC: The case of Santander beaches (Spain). Water Sci. Technol. 2013, 68, 1037–1047. [Google Scholar] [CrossRef][Green Version]
- Tiwari, A.; Niemela, S.I.; Vepsalainen, A.; Rapala, J.; Kalso, S.; Pitkanen, T. Comparison of Colilert-18 with miniaturised most probable number method for monitoring of Escherichia coli in bathing water. J. Water Health 2016, 14, 121–131. [Google Scholar] [CrossRef]
- Napier, M.D.; Haugland, R.; Poole, C.; Dufour, A.P.; Stewart, J.R.; Weber, D.J.; Varma, M.; Lavender, J.S.; Wade, T.J. Exposure to human-associated fecal indicators and self-reported illness among swimmers at recreational beaches: A cohort study. Environ. Health 2017, 16, 103–118. [Google Scholar] [CrossRef]
- Mohammed, R.L.; Echeverry, A.; Stinson, C.M.; Green, M.; Bonilla, T.D.; Hartz, A.; McCorquodale, D.S.; Rogerson, A.; Esiobu, N. Survival trends of Staphylococcus aureus, Pseudomonas aeruginosa, and Clostridium perfringens in a sandy South Florida beach. Mar. Pollut. Bull. 2012, 64, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Gellatly, S.L.; Hancock, R.E.W. Pseudomonas aeruginosa: New insights into pathogenesis and host defenses. Pathog. Dis. 2013, 67, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Mariño, F.J.; Moriñigo, M.A.; Martinez-Manzanares, E.; Borrego, J.J. Microbiological-epidemiological study of selected marine beaches in Malaga (Spain). Water Sci. Technol. 1995, 31, 5–9. [Google Scholar] [CrossRef]
- Trautmann, M.; Lepper, P.M.; Haller, M. Ecology of Pseudomonas aeruginosa in the intensive care unit and the evolving role of water outlets as a reservoir of the organism. Am. J. Infect. Control 2005, 33, S41–S49. [Google Scholar] [CrossRef] [PubMed]
- Ngwa, G.A.; Schop, R.; Chow, J.; Lukic, L.; McKague, K. Comparative detection and recovery of Pseudomonas aeruginosa by membrane filtration and a Most Probable Number technique. J. Microbiol. Methods 2017, 133, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Hardalo, C.; Edberg, S.C. Pseudomonas aeruginosa: Assessment of risk from drinking water. Crit. Rev. Microbiol. 1997, 23, 47–75. [Google Scholar] [CrossRef]
- Quinn, J.P. Pseudomonas aeruginosa infections in the intensive care unit. Semin. Respir. Crit. Care Med. 2003, 24, 61–68. [Google Scholar] [CrossRef]
- Mena, K.D.; Gerba, C.P. Risk Assessment of Pseudomonas aeruginosa in Water. Rev. Environ. Contam. Toxicol. 2009, 201, 71–115. [Google Scholar]
- Bedard, E.; Prevost, M.; Deziel, E. Pseudomonas aeruginosa in premise plumbing of large buildings. Microbiologyopen 2016, 5, 937–956. [Google Scholar] [CrossRef]
- Fazeli, H.; Akbari, R.; Moghim, S.; Narimani, T.; Arabestani, M.R.; Ghoddousi, A.R. Pseudomonas aeruginosa infections in patients, hospital means, and personnel’s specimens. J. Res. Med. Sci. 2012, 17, 332–337. [Google Scholar]
- Zichichi, L.; Asta, G.; Noto, G. Pseudomonas aeruginosa folliculitis after shower/bath exposure. Int. J. Dermatol. 2000, 39, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Roser, D.J.; den Akker, B.; Boase, S.; Haas, C.N.; Ashbolt, N.J.; Rice, S.A. Pseudomonas aeruginosa dose response and bathing water infection. Epidemiol. Infect. 2014, 142, 449–462. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.J.; Martins, K.; Garcia, D.; Ferreira, S.M.F.; Gonçalves, S.C.; Mendes, S.; Lemos, M.F.L. Using the mini-VIDAS® Easy Salmonella protocol to assess contamination in transitional and coastal waters. Arch. Microbiol. 2016, 198, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.S.E.; Novais, S.C.; Simões, T.; Caramalho, M.; Gravato, C.; Rodrigues, M.J.; Maranhão, P.; Lemos, M.F.L. Using biomarkers to address the impacts of pollution on limpets (Patella depressa) and their mechanisms to cope with stress. Ecol. Indic. 2018, 95, 1077–1086. [Google Scholar] [CrossRef]
- Cabral-Oliveira, J.; Pratas, J.; Mendes, S.; Pardal, M.A. Trace Elements in Edible Rocky Shore Species: Effect of Sewage Discharges and Human Health Risk Implications. Hum. Ecol. Risk Assess. 2015, 21, 135–145. [Google Scholar] [CrossRef]
- Harwood, V.J.; Staley, C.; Badgley, B.D.; Borges, K.; Korajkic, A. Microbial source tracking markers for detection of fecal contamination in environmental waters: Relationships between pathogens and human health outcomes. FEMS Microbiol. Rev. 2014, 38, 1–40. [Google Scholar] [CrossRef]
- Vergine, P.; Salerno, C.; Barca, E.; Berardi, G.; Pollice, A. Identification of the faecal indicator Escherichia coli in wastewater through the β-D-glucuronidase activity: Comparison between two enumeration methods, membrane filtration with TBX agar, and Colilert ®-18. J. Water Health 2017, 15, 209–217. [Google Scholar] [CrossRef]
- Ferguson, D.M.; Griffith, J.F.; McGee, C.D.; Weisberg, S.B.; Hagedorn, C. Comparison of enterococcus species diversity in marine water and wastewater using Enterolert and EPA method 1600. J. Environ. Public Health 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Strathmann, M.; Horstkott, M.; Koch, C.; Gayer, U.; Wingender, J. The River Ruhr—An urban river under particular interest for recreational use and as a raw water source for drinking water: The collaborative research project ‘Safe Ruhr’—Microbiological aspects. Int. J. Hyg. Environ. Health 2016, 219, 643–661. [Google Scholar] [CrossRef]
- Havelaar, A.H.; During, M.; Delfgouvanasch, E.H.M. Comparative-study of membrane filtration and enrichment media for the isolation and enumeration of Pseudomonasaeruginosa from sewage, surface-water, and swimming pools. Can. J. Microbiol. 1985, 31, 686–692. [Google Scholar] [CrossRef]
- Warburton, D.W.; Bowen, B.; Konkle, A. The survival and recovery of Pseudomonas aeruginosa and its effect upon Salmonellae in mater—Methodology to test bottled water in Canada. Can. J. Microbiol. 1994, 40, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Seyfried, P.L.; Cook, R.J. Otitis externa infections related to Pseudomonas aeruginosa levels in five Ontario lakes. Can. J. Public Health 1984, 75, 83–91. [Google Scholar] [PubMed]
- Valente, M.S.; Pedro, P.; Alonso, M.C.; Borrego, J.J.; Dionísio, L. Are the defined substrate-based methods adequate to determine the microbiological quality of natural recreational waters? J. Water Health 2010, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Noble, R.; Moore, D.; Leecaster, M.; McGee, C.; Weisberg, S. Comparison of total coliform, fecal coliform, and enterococcus bacterial indicator response for ocean recreational water quality testing. Water Res. 2003, 37, 1637–1643. [Google Scholar] [CrossRef]
- Kay, D.; Bartram, J.; Prüss, A.; Ashbolt, N.; Wyer, M.D.; Fleisher, J.M.; Fewtrell, L.; Rogers, A.; Rees, G. Derivation of numerical values for the World Health Organization guidelines for recreational waters. Water Res. 2004, 38, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
- Hoadley, A.W.; Knight, D.E. External otitis among swimmers and nonswimmers. Arch. Environ. Health 1975, 30, 445–448. [Google Scholar] [CrossRef]
- Reid, T.M.; Porter, I.A. An outbreak of otitis externa in competitive swimmers due to Pseudomonas aeruginosa. J. Hyg. 1981, 86, 357–362. [Google Scholar] [CrossRef]
- Van Asperen, I.A.; de Rover, C.M.; Schijven, J.F.; Oetomo, S.B.; Schellekens, J.F.P.; van Leeuwen, N.J.; Colle, C.; Havelaar, A.H.; Kromhout, D.; Sprenger, M.W.J. Risk of otitis externa after swimming in recreational fresh water lakes containing Pseudomonas aeruginosa. BMJ 1995, 311, 1407–1410. [Google Scholar] [CrossRef]
- Zhang, Q.; Eichmiller, J.J.; Staley, C.; Sadowsky, M.J.; Ishii, S. Correlations between pathogen concentration and fecal indicator marker genes in beach environments. Sci. Total Environ. 2016, 573, 826–830. [Google Scholar] [CrossRef]
- Zabed, H.; Suely, A.; Faruq, G.; Sahu, J.N. Water quality assessment of an unusual ritual well in Bangladesh and impact of mass bathing on this quality. Sci. Total Environ. 2014, 472, 363–369. [Google Scholar] [CrossRef]
- ISO 16266 Water quality—Detection and enumeration of Pseudomonas aeruginosa—Method by membrane filtration. Available online: https://www.iso.org/obp/ui/#iso:std:iso:16266:ed-1:v1:en (accessed on 6 December 2019).
- Legendre, L.; Legendre, P. Écologie numérique. Tome 1: Le traitement multiple des données écologiques; Collection d′Écologie no 12 XIV. Masson; Paris et les Presses de l′Université du Québec: Paris, France, 1979; p. 197. [Google Scholar]
- Zar, J.H. Biostatistical Analysis, 5th ed.; Pearson Prentice-Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Ter Braak, C.J.F.; Smilauer, P. CANOCO Reference Manual and User’s Guide to Canoco for Windows—Software for Canonical Community Ordination; Version 4; Microcomputer Power: Ithaca, NY, USA, 1998. [Google Scholar]

| STP | CJ (Beach 1) | PAS (Beach 2) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | n | Minimum | Maximum | Mean | n | Minimum | Maximum | Mean | n | Minimum | Maximum | |
| P. aeruginosa(CFU/100 mL) | 135.8 | 18 | 0.0 | 1800.0 | 0.7 | 18 | 0.0 | 8.0 | 0.3 | 18 | 0.0 | 5.0 |
| E. coli(MPN/100 mL) | 1100.1 | 16 | 0.0 | 5172.0 | 16.5 | 18 | 0.0 | 74.0 | 14.1 | 18 | 0.0 | 75.0 |
| Intestinal enterococci(MPN/100 mL) | 2685.9 | 18 | 0.0 | 24196.0 | 100.5 | 18 | 0.0 | 455.8 | 145.9 | 18 | 0.0 | 720.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Januário, A.P.; Afonso, C.N.; Mendes, S.; Rodrigues, M.J. Faecal Indicator Bacteria and Pseudomonas aeruginosa in Marine Coastal Waters: Is there a Relationship? Pathogens 2020, 9, 13. https://doi.org/10.3390/pathogens9010013
Januário AP, Afonso CN, Mendes S, Rodrigues MJ. Faecal Indicator Bacteria and Pseudomonas aeruginosa in Marine Coastal Waters: Is there a Relationship? Pathogens. 2020; 9(1):13. https://doi.org/10.3390/pathogens9010013
Chicago/Turabian StyleJanuário, Adriana P., Clélia N. Afonso, Susana Mendes, and Maria J. Rodrigues. 2020. "Faecal Indicator Bacteria and Pseudomonas aeruginosa in Marine Coastal Waters: Is there a Relationship?" Pathogens 9, no. 1: 13. https://doi.org/10.3390/pathogens9010013
APA StyleJanuário, A. P., Afonso, C. N., Mendes, S., & Rodrigues, M. J. (2020). Faecal Indicator Bacteria and Pseudomonas aeruginosa in Marine Coastal Waters: Is there a Relationship? Pathogens, 9(1), 13. https://doi.org/10.3390/pathogens9010013







