Global Burden and Incidence Trends in Cancers Associated with Human Papillomavirus Infection: A Population-Based Systematic Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Population
2.2. Statistical Analysis
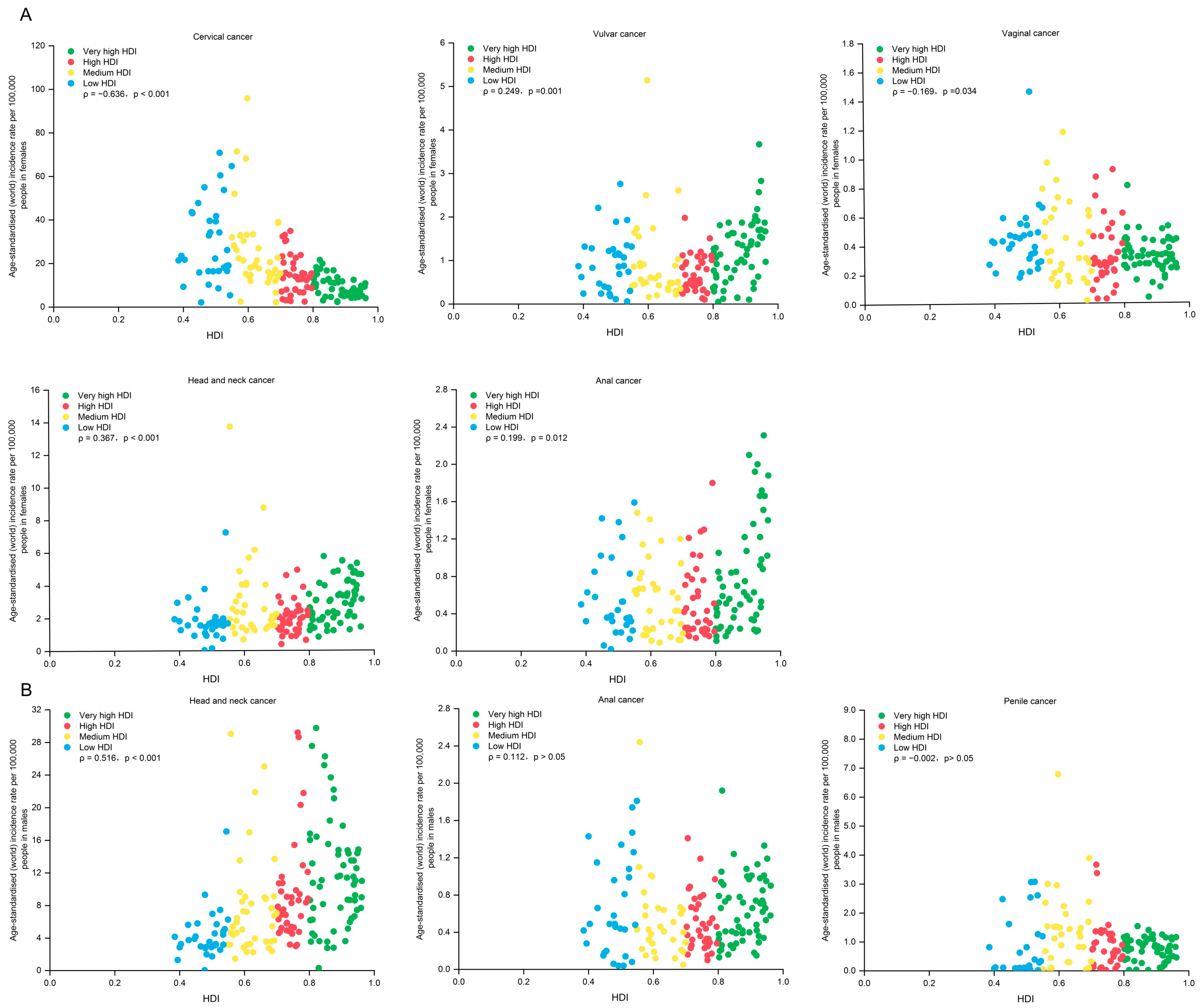
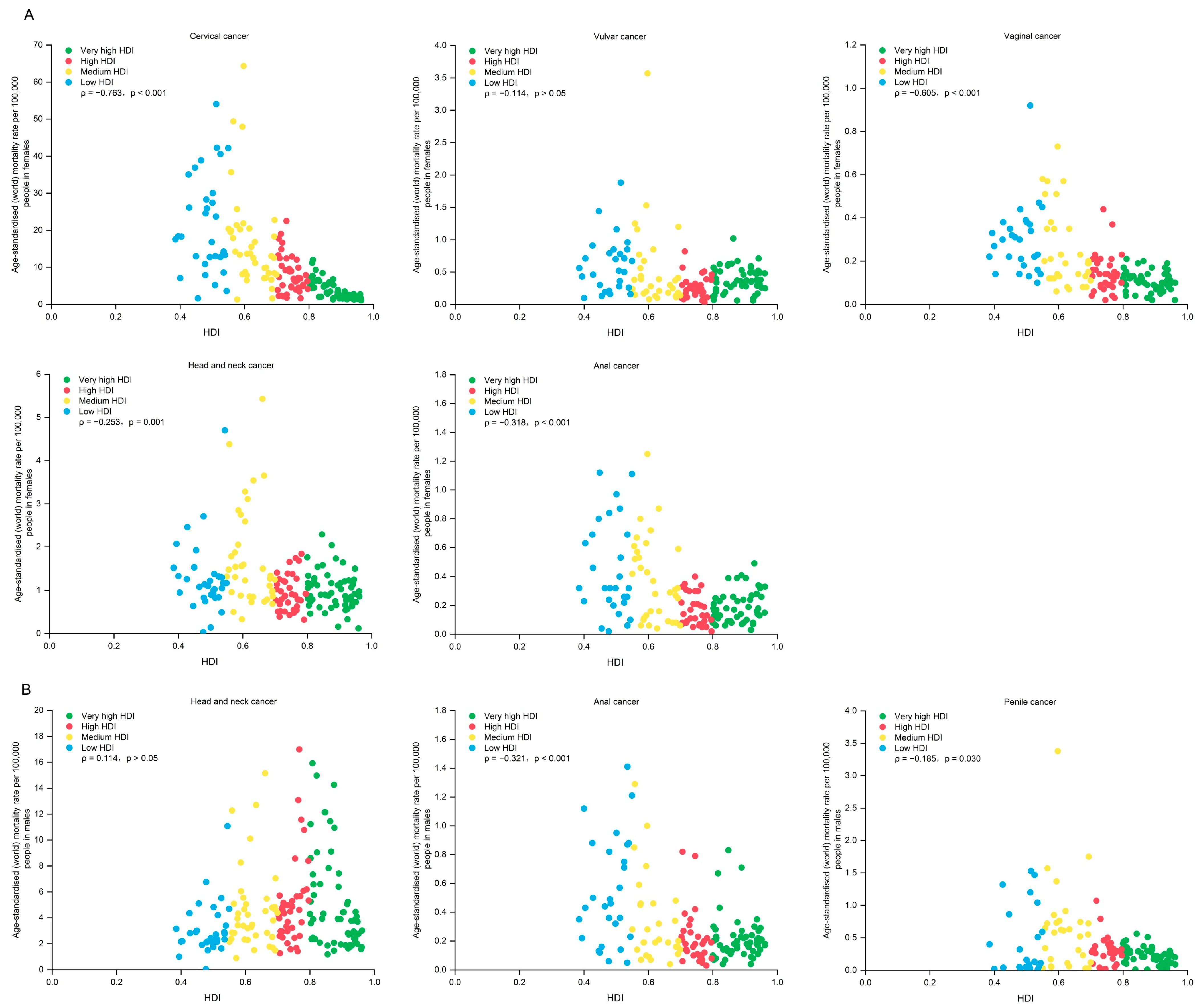
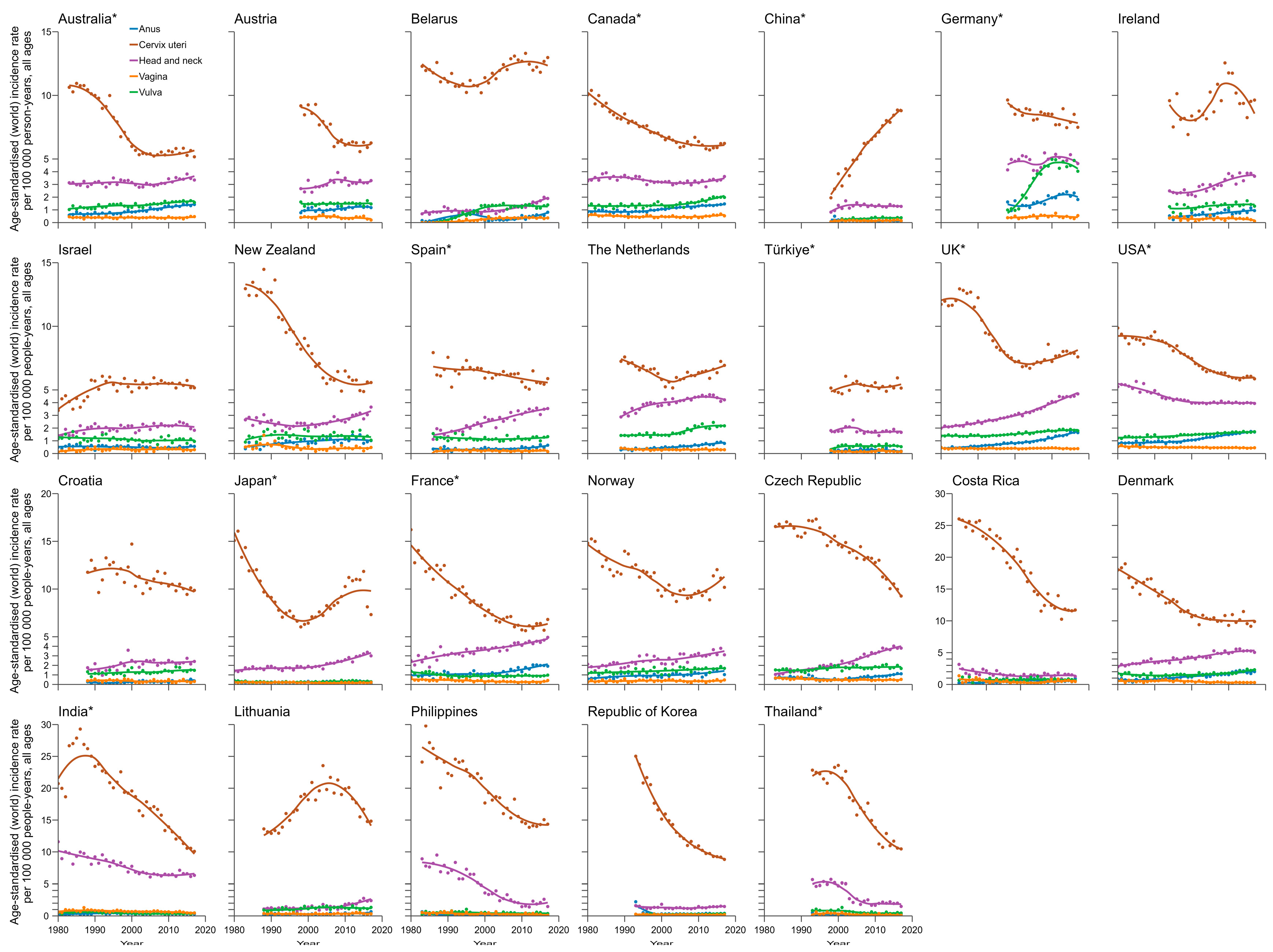
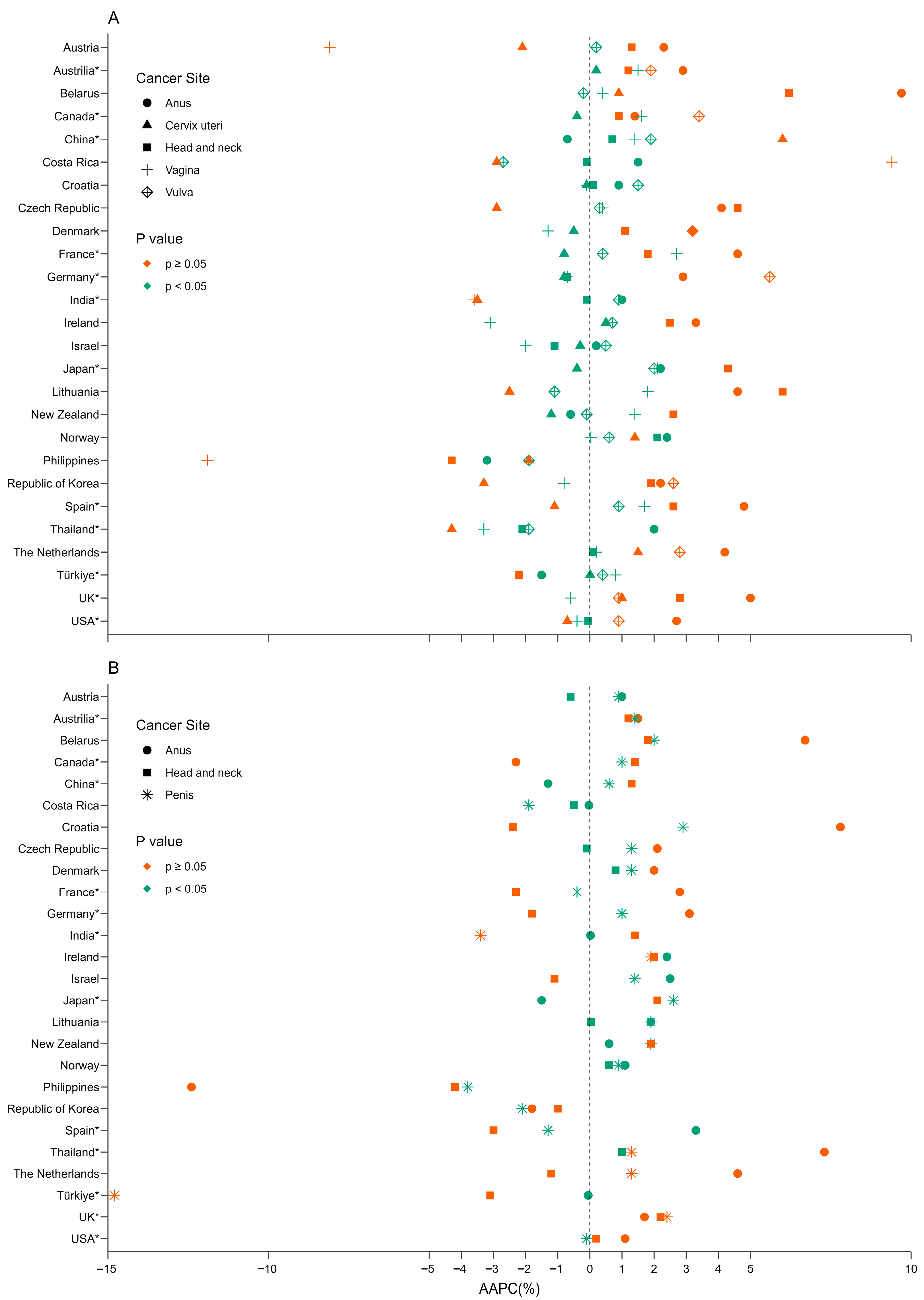
3. Results
4. Discuss
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAPC | average annual percent change |
| APC | annual percent change |
| ASIR | age-standardized incidence |
| ASMR | age-standardized mortality rate |
| CI5 | Cancer Incidence in Five Continents |
| HDI | Human Development Index |
| HNC | head and neck cancer |
| HPV | human papillomavirus |
| ICD-10 | International Classification of Diseases, Tenth Edition |
| LMICs | low-and middle-income countries |
| MSM | men having sex with men |
| NCCSPRAf | National Cervical Cancer Screening Program in Rural Areas |
| PLHIV | people living with HIV |
| WHO | World Health Organization |
References
- Jensen, J.E.; Becker, G.L.; Jackson, J.B.; Rysavy, M.B. Human Papillomavirus and Associated Cancers: A Review. Viruses 2024, 16, 680. [Google Scholar] [CrossRef]
- Muñoz, N.; Bosch, F.X.; de Sanjosé, S.; Herrero, R.; Castellsagué, X.; Shah, K.V.; Snijders, P.J.F.; Meijer, C.J.L.M. Epidemiologic Classification of Human Papillomavirus Types Associated with Cervical Cancer. N. Engl. J. Med. 2003, 348, 518–527. [Google Scholar] [CrossRef]
- Szymonowicz, K.A.; Chen, J. Biological and clinical aspects of HPV-related cancers. Cancer Biol. Med. 2020, 17, 864–878. [Google Scholar] [CrossRef] [PubMed]
- Trias-Llimós, S.; Rentería, E.; Rutigliano, R.; Aggarwal, A.; Moodley, J.; Unger-Saldaña, K.; Soerjomataram, I. Deciphering the sex gap in global life expectancy: The impact of female-specific cancers 1990-2019. J. Natl. Cancer Inst. 2024, 116, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Du, J.; Lu, H.; Xiang, F.; Mei, H.; Xiao, H. Global trends and age-specific incidence and mortality of cervical cancer from 1990 to 2019: An international comparative study based on the Global Burden of Disease. BMJ Open 2022, 12, e055470. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Available online: https://www.who.int/initiatives/cervical-cancer-elimination-initiative (accessed on 18 December 2024).
- de Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G.M. Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob. Health 2020, 8, e180–e190. [Google Scholar] [CrossRef] [PubMed]
- Yun, B.S.; Park, E.H.; Ha, J.; Lee, J.-Y.; Lee, K.H.; Lee, T.S.; Lee, K.J.; Kim, Y.J.; Jung, K.-W.; Roh, J.-W. Incidence and survival of gynecologic cancer including cervical, uterine, ovarian, vaginal, vulvar cancer and gestational trophoblastic neoplasia in Korea, 1999–2019: Korea Central Cancer Registry. Obstet. Gynecol. Sci. 2023, 66, 545–561. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute of the United States. Cancer Statistics Factsheets: Vulvar Cancer. Available online: https://seer.cancer.gov/statfacts/html/vulva.html (accessed on 20 November 2024).
- Douglawi, A.; Masterson, T.A. Penile cancer epidemiology and risk factors. Curr. Opin. Urol. 2019, 29, 145–149. [Google Scholar] [CrossRef]
- Amini, A.P.; Brookes, T.S.; Shah, H.; Bhate, K.; Alnajjar, H.; Muneer, A.; Kravvas, G.; Bunker, C.B. The association between penile cancer and HIV infection: A literature review. Int. J. STD AIDS 2023, 34, 214–228. [Google Scholar] [CrossRef]
- Serrano, B.; Brotons, M.; Bosch, F.X.; Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 14–26. [Google Scholar] [CrossRef]
- National Cancer Institute of the United States. Cancer Statistics Factsheets: Anal Cancer. Available online: https://seer.cancer.gov/statfacts/html/anus.html (accessed on 25 November 2024).
- Syrjanen, S.; Rautava, J.; Syrjanen, K. HPV in Head and Neck Cancer-30 Years of History. Recent Results Cancer Res. 2017, 206, 3–25. [Google Scholar]
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. A Review of Human Carcinogens; International Agency for Research on Cancer: Lyon, France, 2012. [Google Scholar]
- D’Souza, G.; Westra, W.H.; Wang, S.J.; van Zante, A.; Wentz, A.; Kluz, N.; Rettig, E.; Ryan, W.R.; Ha, P.K.; Kang, H.; et al. Differences in the Prevalence of Human Papillomavirus (HPV) in Head and Neck Squamous Cell Cancers by Sex, Race, Anatomic Tumor Site, and HPV Detection Method. JAMA Oncol. 2017, 3, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Segi, M.F.S.; Kurihara, M. Geographical observation on cancer mortality by selected sites on the basis of standardised death rate. Gann 1957, 48, 219–225. [Google Scholar] [PubMed]
- Powell, S.F.; Vu, L.; Spanos, W.C.; Pyeon, D. The Key Differences between Human Papillomavirus-Positive and -Negative Head and Neck Cancers: Biological and Clinical Implications. Cancers 2021, 13, 5206. [Google Scholar] [CrossRef]
- Castellsagué, X.; Alemany, L.; Quer, M.; Halec, G.; Quirós, B.; Tous, S.; Clavero, O.; Alòs, L.; Biegner, T.; Szafarowski, T.; et al. HPV Involvement in Head and Neck Cancers: Comprehensive Assessment of Biomarkers in 3680 Patients. J. Natl. Cancer Inst. 2016, 108, djv403. [Google Scholar] [CrossRef]
- Zhang, J.; Qin, Z.; Lou, C.; Huang, J.; Xiong, Y. The efficacy of vaccination to prevent human papilloma viruses infection at anal and oral: A systematic review and meta-analysis. Public Health 2021, 196, 165–171. [Google Scholar] [CrossRef]
- El Hussein, M.T.; Dhaliwal, S. HPV vaccination for prevention of head and neck cancer among men. Nurse Pract. 2023, 48, 25–32. [Google Scholar] [CrossRef]
- Singh, D.; Vignat, J.; Lorenzoni, V.; Eslahi, M.; Ginsburg, O.; Lauby-Secretan, B.; Arbyn, M.; Basu, P.; Bray, F.; Vaccarella, S. Global estimates of incidence and mortality of cervical cancer in 2020: A baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob. Health 2023, 11, e197–e206. [Google Scholar] [CrossRef]
- Guo, M.; Xu, J.; Du, J. Trends in cervical cancer mortality in China from 1989 to 2018: An age-period-cohort study and Joinpoint analysis. BMC Public Health 2021, 21, 1329. [Google Scholar] [CrossRef]
- Sun, K.; Zheng, R.; Lei, L.; Zhang, S.; Zeng, H.; Wang, S.; Li, L.; Chen, R.; Han, B.; Peng, J.; et al. Trends in Incidence Rates, Mortality Rates, and Age-Period-Cohort Effects of Cervical Cancer—China, 2003–2017. CN CDC Wkly. 2022, 4, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Simms, K.T.; Steinberg, J.; Caruana, M.; Smith, M.A.; Lew, J.-B.; Soerjomataram, I.; Castle, P.E.; Bray, F.; Canfell, K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–2099: A modelling study. Lancet Oncol. 2019, 20, 394–407. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, A.R.; Palefsky, J.M.; Goldstone, S.; Moreira, E.D.; Penny, M.E.; Aranda, C.; Vardas, E.; Moi, H.; Jessen, H.; Hillman, R.; et al. Efficacy of Quadrivalent HPV Vaccine against HPV Infection and Disease in Males. N. Engl. J. Med. 2011, 364, 401–411. [Google Scholar] [CrossRef]
- Zhu, B.; Gu, H.; Mao, Z.; Beeraka, N.M.; Zhao, X.; Anand, M.P.; Zheng, Y.; Zhao, R.; Li, S.; Manogaran, P.; et al. Global burden of gynaecological cancers in 2022 and projections to 2050. J. Glob. Health 2024, 14, 4155. [Google Scholar] [CrossRef]
- Stier, E.A.; Clarke, M.A.; Deshmukh, A.A.; Wentzensen, N.; Liu, Y.; Poynten, I.M.; Cavallari, E.N.; Fink, V.; Barroso, L.F.; Clifford, G.M.; et al. International Anal Neoplasia Society’s consensus guidelines for anal cancer screening. Int. J. Cancer 2024, 154, 1694–1702. [Google Scholar] [CrossRef]
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M.; et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Human Papillomavirus Vaccines: WHO Position Paper (2022 Update). Available online: https://www.who.int/publications/i/item/who-wer9750-645-672 (accessed on 11 November 2024).
- Fu, L.; Tian, T.; Wang, B.; Lu, Z.; Gao, Y.; Sun, Y.; Lin, Y.-F.; Zhang, W.; Li, Y.; Zou, H. Global patterns and trends in Kaposi sarcoma incidence: A population-based study. Lancet Glob. Health 2023, 11, e1566–e1575. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.; Williams, J.; Townsend, N.; Mikkelsen, B.; Roberts, N.; Foster, C.; Wickramasinghe, K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob. Health 2017, 5, e277–e289. [Google Scholar] [CrossRef]
- Lu, J.G. Cultural differences in humor: A systematic review and critique. Curr. Opin. Psychol. 2023, 53, 101690. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, X.; Yang, B.; Yin, H.; Chen, J.; Ma, W.; Xu, Z.; Shen, Y. Global Burden and Incidence Trends in Cancers Associated with Human Papillomavirus Infection: A Population-Based Systematic Study. Pathogens 2025, 14, 880. https://doi.org/10.3390/pathogens14090880
Meng X, Yang B, Yin H, Chen J, Ma W, Xu Z, Shen Y. Global Burden and Incidence Trends in Cancers Associated with Human Papillomavirus Infection: A Population-Based Systematic Study. Pathogens. 2025; 14(9):880. https://doi.org/10.3390/pathogens14090880
Chicago/Turabian StyleMeng, Xiaojun, Bolin Yang, Hanlu Yin, Jibiao Chen, Wenjuan Ma, Zhuping Xu, and Yuan Shen. 2025. "Global Burden and Incidence Trends in Cancers Associated with Human Papillomavirus Infection: A Population-Based Systematic Study" Pathogens 14, no. 9: 880. https://doi.org/10.3390/pathogens14090880
APA StyleMeng, X., Yang, B., Yin, H., Chen, J., Ma, W., Xu, Z., & Shen, Y. (2025). Global Burden and Incidence Trends in Cancers Associated with Human Papillomavirus Infection: A Population-Based Systematic Study. Pathogens, 14(9), 880. https://doi.org/10.3390/pathogens14090880




