Syphilis and the Eye: Clinical Features, Diagnostic Challenges, and Evolving Therapeutic Paradigms
Abstract
1. Introduction
Epidemiology and Pathogenesis of Ocular Syphilis
2. Clinical Manifestation of Syphilis-Related Ocular Disease
2.1. Anterior Segment Manifestations
2.2. Posterior Segment Manifestation
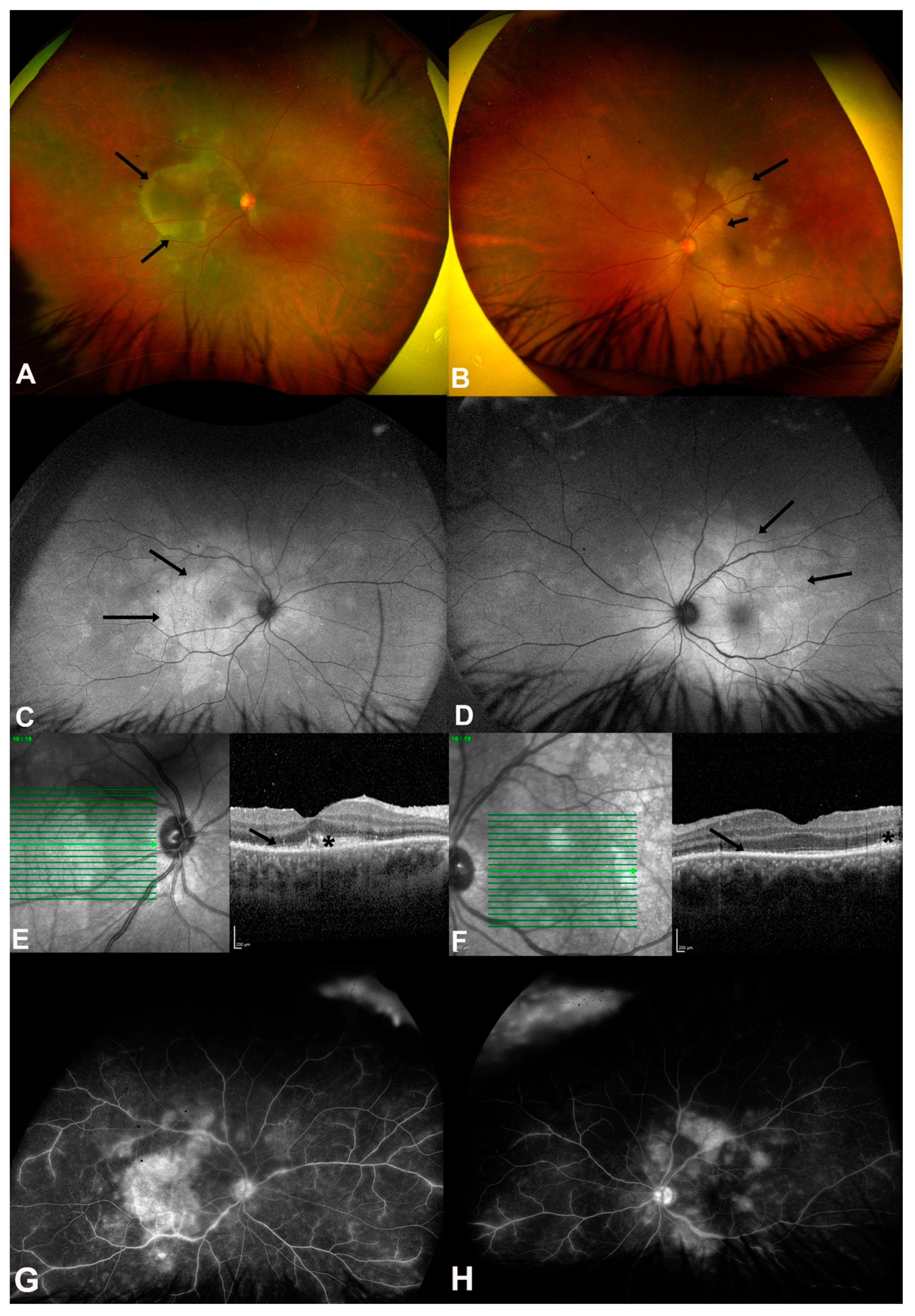
2.3. ASPPC
2.4. Neuro-Ophthalmic Complications
3. Diagnostic Challenges and Advanced Modalities
3.1. Limitations of Traditional Serology Test in Ocular Syphilis
3.2. Cerebrospinal Fluid Antibody Analysis
3.3. Imaging-Driven Diagnosis
3.4. Molecular Diagnostics
4. Therapeutic Innovations in Ocular Syphilis
4.1. Adjunctive and Alternative Strategies
4.2. Vaccine Development
5. Co-Infection with Retrovirus: Synergistic Pathogenesis and Management
5.1. HIV Co-Infection in Syphilitic Patients
5.2. HTLV-1 Co-Infection in Syphilitic Patients
6. Global Health Strategies for Ocular Syphilis
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Quilter, L.A.S.; de Voux, A.; Amiya, R.M.; Davies, E.; Hennessy, R.R.; Kerani, R.P.; Madera, R.; Matthias, J.; Pearson, V.M.; Walters, J.K.; et al. Prevalence of Self-reported Neurologic and Ocular Symptoms in Early Syphilis Cases. Clin. Infect. Dis. 2020, 72, 961–967. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Sector Strategies on, Respectively, HIV, Viral Hepatitis and Sexually Transmitted Infections for the Period 2022–2030; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Taylor, M.M.; Wi, T.; Gerbase, A.; Thwin, S.S.; Gottlieb, S.; Babovic, M.T.; Low-Beer, D.; Alonso, M.; Mello, M.B.; Ishikawa, N.; et al. Assessment of country implementation of the WHO global health sector strategy on sexually transmitted infections (2016–2021). PLoS ONE 2022, 17, e0263550. [Google Scholar] [CrossRef] [PubMed]
- Do, D.; Rodriguez, P.J.; Gratzl, S.; Cartwright, B.M.G.; Baker, C.; Stucky, N.L. Trends in Incidence of Syphilis Among US Adults from January 2017 to October 2024. Am. J. Prev. Med. 2025; Advance online publication. [Google Scholar] [CrossRef]
- World Health Organization. Data on Syphilis. Available online: https://www.who.int/data/gho/data/themes/topics/data-on-syphilis (accessed on 24 July 2025).
- U.S. Department of Health and Human Services. 2022 U.S. Syphilis Cases Reach Highest Numbers Since the 1950s. Available online: https://www.cdc.gov/nchhstp/newsroom/releases/2024/sti-surveillance-report-2022.html (accessed on 24 July 2025).
- Mathew, R.G.; Goh, B.T.; Westcott, M.C. British Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5394–5400. [Google Scholar] [CrossRef]
- Reid, G.A.; Halmagyi, G.M.; Whyte, C.; McCluskey, P.J. Ocular vs neurosyphilis. are they the same? A guide to investigation and management. Eye 2024, 38, 2337–2349. [Google Scholar] [CrossRef]
- Sun, C.B.; Liu, G.H.; Wu, R.; Liu, Z. Demographic, Clinical and Laboratory Characteristics of Ocular Syphilis: 6-Years Case Series Study From an Eye Center in East-China. Front. Immunol. 2022, 13, 910337. [Google Scholar] [CrossRef]
- Harvey, J.; Lee, I.J.; Lee, C.S.; Hinkle, D. Ocular syphilis on the rise: A 10-year analysis from 2010 to 2020. Int. Ophthalmol. 2023, 43, 4419–4426. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S.E.; Aubin, M.; Atwell, L.; Matthias, J.; Cope, A.; Mobley, V.; Goode, A.; Minnerly, S.; Stoltey, J.; Bauer, H.M.; et al. Ocular Syphilis—Eight Jurisdictions, United States, 2014–2015. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1185–1188. [Google Scholar] [CrossRef]
- Shields, M.K.; Arantes, T.E.; Lake, S.R.; Belfort, R.; Muccioli, C.; Nascimento, H.; de Pinho Queiroz, R.; Vasconcelos-Santos, D.V.; Furtado, J.M.; Smith, J.R. Influence of gender on clinical presentation, management practices and outcomes of ocular syphilis. Sci. Rep. 2024, 14, 16390. [Google Scholar] [CrossRef]
- Gu, X.; Gao, Y.; Yan, Y.; Marks, M.; Zhu, L.; Lu, H.; Guan, Z.; Shi, M.; Ni, L.; Peng, R.; et al. The importance of proper and prompt treatment of ocular syphilis: A lesson from permanent vision loss in 52 eyes. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1569–1578. [Google Scholar] [CrossRef]
- Furtado, J.M.; Simões, M.; Vasconcelos-Santos, D.; Oliver, G.F.; Tyagi, M.; Nascimento, H.; Gordon, D.L.; Smith, J.R. Ocular syphilis. Surv. Ophthalmol. 2022, 67, 440–462. [Google Scholar] [CrossRef]
- Alhawsawi, A.A.; Aljahdali, A.; Magharbil, E.; Alzuabi, A.; Albloushi, A.F.; Alhamad, D.; Alsalamah, A.K.; Alsulaiman, S.M.; Al Hammad, F.; Magliyah, M.S. The clinical spectrum and outcomes of ocular syphilis in Saudi Arabia: The emergence of a uveitic masquerader. J. Epidemiol. Glob. Health 2025, 15, 31. [Google Scholar] [CrossRef]
- Ghanem, K.G.; Ram, S.; Rice, P.A. The Modern Epidemic of Syphilis. N. Engl. J. Med. 2020, 382, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Du, Q.; Ma, F.; Lu, Y.; Wang, M.; Li, X. Characteristics of syphilitic uveitis in northern China. BMC Ophthalmol. 2017, 17, 95. [Google Scholar] [CrossRef] [PubMed]
- Radolf, J.D.; Deka, R.K.; Anand, A.; Šmajs, D.; Norgard, M.V.; Yang, X.F. Treponema pallidum, the syphilis spirochete: Making a living as a stealth pathogen. Nat. Rev. Microbiol. 2016, 14, 744–759. [Google Scholar] [CrossRef]
- Cameron, C.E.; Lukehart, S.A. Current status of syphilis vaccine development: Need, challenges, prospects. Vaccine 2014, 32, 1602–1609. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, M.; Kase, M. Retinal vasculitis due to secondary syphilis. Jpn. J. Ophthalmol. 2004, 48, 65–67. [Google Scholar] [CrossRef]
- Kiss, S.; Damico, F.M.; Young, L.H. Ocular manifestations and treatment of syphilis. Semin. Ophthalmol. 2005, 20, 161–167. [Google Scholar] [CrossRef]
- Shahid, M.M.; Neequaye, N.; Hu, W.F.; Shifera, A.S. Demographic Trends, Clinical Features, and Visual Outcomes of Ocular Syphilis from a Single Tertiary Care Center in Western New York. Investig. Ophthalmol. Vis. Sci. 2025, 66, 33. Available online: https://iovs.arvojournals.org/article.aspx?articleid=2805519 (accessed on 20 July 2025).
- Jabs, D.; Nussenblatt, R. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data: Results of the First International Workshop. Am. J. Ophthalmol. 2005, 140, 509–516. [Google Scholar] [CrossRef]
- Jeyakumar, W.; Chithra, A.; Shanmugasundararaj, A. Primary syphilis of the eyelid: Case report. Genitourin. Med. 1989, 65, 192–193. [Google Scholar] [CrossRef]
- Cillino, S.; Di Pace, F.; Trizzino, M.; Vecchi, V.L.; Di Carlo, P. Chancre of the eyelid as manifestation of primary syphilis, and precocious chorioretinitis and uveitis in an HIV-infected patient: A case report. BMC Infect. Dis. 2012, 12, 226. [Google Scholar] [CrossRef]
- Shields, M.K.; Furtado, J.M.; Lake, S.R.; Smith, J.R. Syphilitic scleritis and episcleritis: A review. Asia Pac. J. Ophthalmol. 2024, 13, 100073. [Google Scholar] [CrossRef]
- Wilhelmus, K.R.; Yokoyama, C.M. Syphilitic episcleritis and scleritis. Am. J. Ophthalmol. 1987, 104, 595–597. [Google Scholar] [CrossRef]
- Watson, P.; Hayreh, S.S. Scleritis and episcleritis. Br. J. Ophthalmol. 1976, 60, 163–191. [Google Scholar] [CrossRef]
- Jabs, D.A.; Mudun, A.; Dunn, J.; Marsh, M.J. Episcleritis and scleritis: Clinical features and treatment results. Am. J. Ophthalmol. 2000, 130, 469–476. [Google Scholar] [CrossRef]
- Lee, M.E.; Lindquist, T.D. Syphilitic interstitial keratitis. JAMA 1989, 262, 2921. [Google Scholar] [CrossRef]
- Tsan, G.L.; Claiborne, R.T. Ocular syphilis. Clin. Exp. Optom. 2021, 104, 756–759. [Google Scholar] [CrossRef]
- Knox, C.M.; Holsclaw, D.S. Interstitial keratitis. Int. Ophthalmol. Clin. 1998, 38, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.S.; Vitale, A.T.; Shakoor, A.; Larochelle, M.; Sassalos, T.; Elner, S.G.; Jayasundera, T.; Conrady, C.D. Pyramidal inflammatory deposits of the retinal pigment epithelium and outer retina in ocular syphilis. Ophthalmol. Retin. 2022, 6, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Jiang, Y.; Shi, Y.; Zheng, B.; Xu, Z.; Jia, W. Clinical manifestations and treatment outcomes of syphilitic uveitis in HIV-negative patients in China: A retrospective case study. Medicine 2017, 96, e8376. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.L. Ocular syphilis. Curr. Opin. Ophthalmol. 2014, 25, 513–518. [Google Scholar] [CrossRef]
- Eandi, C.M.; Neri, P.; Adelman, R.A.; Yannuzzi, L.A.; Cunningham, E.T.J. Acute Syphilitic Posterior Placoid Chorioretinitis: Report of a Case Series and Comprehensive Review of the Literature. Retina 2012, 32, 1915–1941. [Google Scholar] [CrossRef]
- Jabbehdari, S.; Oganov, A.; Uwaydat, S.H. From Retinal Vasculitis to Stroke, from Systemic Findings to Diagnosis, the Necessity of Multidisciplinary Management in Behçet’s Disease: A Case Report. Case Rep. Ophthalmol. 2025, 16, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Du, K.-F.; Li, H.-Y.; Wang, X.-D.; Li, X.-N.; Kong, W.-J.; Xie, L.-Y.; Zhang, M.; Yan, Z.-Z.; Weng, W.-J.; Dong, H.-W. Assessment of Syphilitic Optic Neuropathy: A Prospective Cross-Sectional Study. Ocul. Immunol. Inflamm. 2025; Advance online publication. [Google Scholar] [CrossRef]
- Jumper, J.M.; Machemer, R.; Gallemore, R.P.; Jaffe, G.J. Exudative retinal detachment and retinitis associated with acquired syphilitic uveitis. Retina 2000, 20, 190–194. [Google Scholar] [CrossRef]
- Shughoury, A.; Carr, E.W.; Moorthy, R.S. Rhegmatogenous retinal detachment in syphilitic uveitis: A case series and comprehensive review of the literature. Ocul. Immunol. Inflamm. 2024, 32, 1302–1313. [Google Scholar] [CrossRef]
- Smith, G.; Goldmeier, D.; Migdal, C. Neurosyphilis with optic neuritis: An update. Postgrad. Med. J. 2006, 82, 36–39. [Google Scholar] [CrossRef]
- Moore, D.B.; Jaffe, G.J.; Asrani, S. Retinal nerve fiber layer thickness measurements: Uveitis, a major confounding factor. Ophthalmology 2015, 122, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Pichi, F.; Ciardella, A.P.; Cunningham, E.T., Jr.; Morara, M.; Veronese, C.; Jumper, J.M.; Albini, T.A.; Sarraf, D.; McCannel, C.; Voleti, V.; et al. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina 2014, 34, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Wai, K.M.; Gong, D.; Rodriguez, M.; Cunningham, E.T., Jr.; Vavvas, D.G.; Eliott, D. Acute syphilitic posterior placoid chorioretinitis with subfoveal choroidal neovascularization managed with anti-VEGF therapy. J. Vitr. Dis. 2022, 6, 246–250. [Google Scholar] [CrossRef]
- Herbort, C.P., Jr.; Papasavvas, I.; Mantovani, A. Choriocapillaris involvement in acute syphilis posterior placoid chorioretinitis is responsible for functional impairment and points towards an immunologic mechanism: A comprehensive clinicopathological approach. J. Curr. Ophthalmol. 2020, 32, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.; Agorogiannis, E. The Rise of Syphilitic Placoid Chorioretinitis: A Literature Review with Data from 286 Published Cases. Ocul. Immunol. Inflamm. 2025; Advance online publication. [Google Scholar] [CrossRef]
- Arora, S.; Dudani, S.; Mohan, C.; Shankar, M.M.; Chaturvedi, P.; Kumar, A.H. Ocular and Neuro-ophthalmic Conditions Causing Visual Impairment in Human Immunodeficiency Virus: A Case Series. J. Med. Acad. 2023, 6, 61–65. [Google Scholar] [CrossRef]
- Bhatti, M.T. Optic neuropathy from viruses and spirochetes. Int. Ophthalmol. Clin. 2007, 47, 37–66. [Google Scholar] [CrossRef]
- Rizvi, I.; Garg, R.K. Infectious Optic Neuropathies. In A Clinical Approach to Neuro-Ophthalmic Disorders; CRC Press: Boca Raton, FL, USA, 2022; pp. 99–107. [Google Scholar]
- Chauhan, K.; Fonollosa, A.; Giralt, L.; Artaraz, J.; Randerson, E.L.; Goldstein, D.A.; Furtado, J.M.; Smith, J.R.; Sudharshan, S.; Ahmed, A.S. Demystifying ocular syphilis–A major review. Ocul. Immunol. Inflamm. 2023, 31, 1425–1439. [Google Scholar] [CrossRef] [PubMed]
- Sivabalan, P.; Haider, A.; Palmer, C.; Bursle, E.; Hutchinson, K. An unusual presentation of neuro-ophthalmic syphilis. Intern. Med. J. 2021, 51, 610–612. [Google Scholar] [CrossRef]
- Levy, J.H.; Liss, R.A.; Maguire, A.M. Neurosyphilis and ocular syphilis in patients with concurrent human immunodeficiency virus infection. Retina 1989, 9, 175–180. [Google Scholar] [CrossRef]
- Dutta Majumder, P.; Chen, E.J.; Shah, J.; Ching Wen Ho, D.; Biswas, J.; See Yin, L.; Gupta, V.; Pavesio, C.; Agrawal, R. Ocular syphilis: An update. Ocul. Immunol. Inflamm. 2017, 27, 117–125. [Google Scholar] [CrossRef]
- Kiani, R.; Ahmady, A.; Luhadia, K.; Abugrin, M.; Virk, J.; Yashi, K. Blurry Diagnosis of Ocular Syphilis. Cureus 2022, 14, 10. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, A.; Castledine, R.; Rogers, D.; Burke, T. Ocular syphilis presenting as panuveitis: A management approach for the non-uveitis specialist. BMJ Case Rep. 2025, 18, e260699. [Google Scholar] [CrossRef]
- Mohareb, A.M.; Barshak, M.B.; Papaliodis, G.N.; Sobrin, L.; Durand, M.L. Ocular Syphilis in Patients with Nonreactive Rapid Plasma Reagin and Positive Treponemal Serologies: A Retrospective Observational Cohort Study. Clin. Infect. Dis. 2024; Advance online publication. [Google Scholar] [CrossRef]
- Nair, N.; Sudharshan, S.; Anand, A.R.; Biswas, J.; Therese, K.L. Utility of treponemal testing from aqueous fluid in the diagnosis of ocular syphilis in patients with HIV/AIDS. Ocul. Immunol. Inflamm. 2022, 30, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Silpa-Archa, S.; Hoopholerb, T.; Foster, C.S. Appraisal of vitreous syphilis antibody as a novel biomarker for the diagnosis of syphilitic uveitis: A prospective case-control study. Eye 2023, 37, 146–154. [Google Scholar] [CrossRef]
- Moore, M.B., Jr.; Knox, J.M. Sensitivity and Specificity in Syphilis Serology: Clinical Implications. South. Med. J. 1965, 58, 963–968. [Google Scholar] [CrossRef]
- Papp, J.R.; Park, I.U.; Fakile, Y.; Pereira, L.; Pillay, A.; Bolan, G.A. CDC Laboratory Recommendations for Syphilis Testing, United States. 2024. Available online: https://www.cdc.gov/mmwr/volumes/73/rr/rr7301a1.htm?utm_medium=email&utm_source=govdelivery (accessed on 20 July 2025).
- Sarraf, D. Ocular imaging in the Canadian Journal of Ophthalmology. Can. J. Ophthalmol. 2019, 54, 410. [Google Scholar] [CrossRef]
- Luo, Y.; Xie, Y.; Xiao, Y. Laboratory diagnostic tools for syphilis: Current status and future prospects. Front. Cell Infect. Microbiol. 2021, 10, 574806. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Thorpe, P.G.; O’Callaghan, K.; Kersh, E.N. Advantages and limitations of current diagnostic laboratory approaches in syphilis and congenital syphilis. Expert. Rev. Anti Infect. Ther. 2023, 21, 1339–1354. [Google Scholar] [CrossRef] [PubMed]
- Marra, C.M.; Maxwell, C.L.; Dunaway, S.B.; Sahi, S.K.; Tantalo, L.C. Cerebrospinal Fluid Treponema pallidum Particle Agglutination Assay for Neurosyphilis Diagnosis. J. Clin. Microbiol. 2017, 55, 1865–1870. [Google Scholar] [CrossRef] [PubMed]
- Workowski, K.A.; Berman, S. Sexually Transmitted Diseases Treatment Guidelines. 2010. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5912a1.htm (accessed on 16 July 2025).
- Harding, A.S.; Ghanem, K.G. The Performance of Cerebrospinal Fluid Treponemal-Specific Antibody Tests in Neurosyphilis: A Systematic Review. Sex. Transm. Dis. 2012, 39, 291–297. [Google Scholar] [CrossRef]
- Workowski, K.A. Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clin. Infect. Dis. 2015, 61, S759–S762. [Google Scholar] [CrossRef]
- Sandoval Gonzalez, S.; Song, W.; Privratsky, J.K.; Lemon, J.; Tsui, E. Swept-Source Anterior Segment Optical Coherence Tomography of a Vascularized Syphilitic Iris Lesion. Ocul. Immunol. Inflamm. 2025; Advance online publication. [Google Scholar] [CrossRef]
- Chen, A.; Seddon, I.; Rhead, J.; Browning, D.J. Near Infrared Reflectance Imaging Changes in Acute Syphilitic Outer Retinitis. Ophthalmol. Retin. 2025; Advance online publication. [Google Scholar] [CrossRef]
- Sverdlichenko, I.; McDonald, H.M.; Xie, J.S.C.; Margolin, E.A. Macular Optical Coherence Tomography Findings in Patients with Syphilitic Optic Neuropathy-A Case Series and Systematic Review. J. Neuroophthalmol. 2025, 45, 137–144. [Google Scholar] [CrossRef]
- Méndez-Rodríguez, L.; Nocua-Báez, L.; Mejía-Salgado, G.; de-la-Torre, A.; Álvarez-Moreno, C. Infectious uveitis: Epidemiology, etiology, diagnostic test performance and treatment. Arch. Soc. Española Oftalmol. (Engl. Ed.) 2025, 100, 397–420. [Google Scholar] [CrossRef]
- Tuddenham, S.; Katz, S.S.; Ghanem, K.G. Syphilis laboratory guidelines: Performance characteristics of nontreponemal antibody tests. Clin. Infect. Dis. 2020, 71, S21–S42. [Google Scholar] [CrossRef]
- Sena, A.C.; Wolff, M.; Martin, D.H.; Behets, F.; Van Damme, K.; Leone, P.; Langley, C.; McNeil, L.; Hook, E.W. Predictors of serological cure and serofast state after treatment in HIV-negative persons with early syphilis. Clin. Infect. Dis. 2011, 53, 1092–1099. [Google Scholar] [CrossRef]
- Rhoton, E. Using the Reverse Testing Algorithm to Detect a Case of Ocular Syphilis. Available online: https://dc.etsu.edu/boland-research-day/2025/presentations/199/ (accessed on 18 July 2025).
- Gu, X.; Lu, H.; Yang, Y.; Zhu, L.; Shi, M.; Guan, Z.; Ni, L.; Peng, R.; Zhao, W.; Wu, J. Could ceftriaxone be a viable alternative to penicillin for the treatment of ocular syphilis? Antimicrob. Agents Chemother. 2024, 68, e0008024. [Google Scholar] [CrossRef]
- Du, F.-Z.; Wu, M.-Z.; Zhang, X.; Zhang, R.-L.; Wang, Q.-Q. Ceftriaxone compared with penicillin G for the treatment of neurosyphilis: Study protocol for a multicenter randomized controlled trial. Trials 2022, 23, 835. [Google Scholar] [CrossRef] [PubMed]
- Workowski, K.A. Sexually Transmitted Infections Treatment Guidelines. 2021. Available online: https://www.cdc.gov/mmwr/volumes/70/rr/RR7004a1.htm?s_cid=RR7004a1_w (accessed on 10 July 2025).
- Bao, Y.K.; Hwang, J.; Long, C.; Davar, K.; Kapadia, N.; Spellberg, B.; Wong, B.; Rao, N.; Toy, B.C. Outpatient Oral Doxycycline Therapy for Ocular Syphilis. JAMA Netw. Open 2024, 7, e2449364. [Google Scholar] [CrossRef]
- Janier, M.; Unemo, M.; Dupin, N.; Tiplica, G.S.; Potočnik, M.; Patel, R. 2020 European guideline on the management of syphilis. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 574–588. [Google Scholar] [CrossRef]
- Nau, R.; Sörgel, F.; Eiffert, H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin. Microbiol. Rev. 2010, 23, 858–883. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.d.S.; Rangel, I.d.C.; Soane, M.M.; Bacarov, N.B.; Herbst, V.; Ferry, F.R. Cerebrospinal fluid CXCL13 concentration for diagnosis and monitoring of neurosyphilis in people with HIV. AIDS 2024, 38, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Waugh, S.; Ranasinghe, A.; Gomez, A.; Houston, S.; Lithgow, K.V.; Eshghi, A.; Fleetwood, J.; Conway, K.M.E.; Reynolds, L.A.; Cameron, C.E. Syphilis and the host: Multi-omic analysis of host cellular responses to Treponema pallidum provides novel insight into syphilis pathogenesis. Front. Microbiol. 2023, 14, 1254342. [Google Scholar] [CrossRef]
- Lithgow, K.V.; Tsao, E.; Schovanek, E.; Gomez, A.; Swayne, L.A.; Cameron, C.E. Treponema pallidum Disrupts VE-Cadherin Intercellular Junctions and Traverses Endothelial Barriers Using a Cholesterol-Dependent Mechanism. Front. Microbiol. 2021, 12, 691731. [Google Scholar] [CrossRef]
- Lukehart, S.A.; Molini, B.; Gomez, A.; Godornes, C.; Hof, R.; Fernandez, M.C.; Pitner, R.A.; Gray, S.A.; Carter, D.; Giacani, L. Immunization with a tri-antigen syphilis vaccine significantly attenuates chancre development, reduces bacterial load, and inhibits dissemination of Treponema pallidum. Vaccine 2022, 40, 7676–7692. [Google Scholar] [CrossRef]
- Jeyanathan, M.; Afkhami, S.; Smaill, F.; Miller, M.S.; Lichty, B.D.; Xing, Z. Immunological considerations for COVID-19 vaccine strategies. Nat. Rev. Immunol. 2020, 20, 615–632. [Google Scholar] [CrossRef]
- Mathew, D.; Smit, D. Clinical and laboratory characteristics of ocular syphilis and neurosyphilis among individuals with and without HIV infection. Br. J. Ophthalmol. 2021, 105, 70–74. [Google Scholar] [CrossRef]
- Tran, T.H.; Cassoux, N.; Bodaghi, B.; Fardeau, C.; Caumes, E.; Lehoang, P. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch. Clin. Exp. Ophthalmol. 2005, 243, 863–869. [Google Scholar] [CrossRef]
- Amaratunge, B.C.; Camuglia, J.E.; Hall, A.J. Syphilitic uveitis: A review of clinical manifestations and treatment outcomes of syphilitic uveitis in human immunodeficiency virus-positive and negative patients. Clin. Exp. Ophthalmol. 2010, 38, 68–74. [Google Scholar] [CrossRef]
- Dutta Majumder, P.; Agarwal, S.; Shah, M.; Srinivasan, B.; Priyadarshini, K.; Iyer, G.; Sharma, N.; Biswas, J.; McCluskey, P. Necrotizing Scleritis: A Review. Ocul. Immunol. Inflamm. 2024, 32, 1405–1419. [Google Scholar] [CrossRef]
- Wu, L.Z.; Orlowski, T.M.; Karunatilake, M.; Lee, S.; Mondal, P.; Kogilwaimath, S.; Bursztyn, L. Prognostic effect of HIV on visual acuity in ocular syphilis: A systematic review. Eye 2023, 37, 3271–3281. [Google Scholar] [CrossRef] [PubMed]
- Nunes, D.; Boa-Sorte, N.; Grassi, M.F.R.; Pimentel, K.; Teixeira, M.G.; Barreto, M.L.; Dourado, I.; Galvão-Castro, B. Evidence of a predominance of sexual transmission of HTLV-1 in Salvador, the city with the highest prevalence in Brazil. Retrovirology 2015, 12, O3. [Google Scholar] [CrossRef]
- Ayerdi, O.; Benito, R.; Ortega, D.; Aguilera, A.; Montiel, N.; Pintos, I.; Díaz de Santiago, A.; Baza, B.; Soriano, V.; De Mendoza, C. HTLV infection in persons with sexually transmitted diseases in Spain. Front. Immunol. 2023, 14, 1277793. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Human T-Cell Lymphotropic Virus-1. Available online: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/htlv-1 (accessed on 27 July 2025).
- Sagara, Y.; Nakamura, H.; Satake, M.; Watanabe, T.; Hamaguchi, I. Increasing horizontal transmission of human T-cell leukemia virus type 1 in adolescents and young adults in Japan. J. Clin. Virol. 2022, 157, 105324. [Google Scholar] [CrossRef]
- Kamoi, K.; Horiguchi, N.; Kurozumi-Karube, H.; Hamaguchi, I.; Yamano, Y.; Uchimaru, K.; Tojo, A.; Watanabe, T.; Ohno-Matsui, K. Horizontal transmission of HTLV-1 causing uveitis. Lancet Infect. Dis. 2021, 21, 578. [Google Scholar] [CrossRef]
- Kamoi, K.; Uchimaru, K.; Nannya, Y.; Tojo, A.; Watanabe, T.; Ohno-Matsui, K. Sexual transmission of HTLV-1 resulting in uveitis with short-term latency and low proviral load. J. Med. Virol. 2024, 96, e70000. [Google Scholar] [CrossRef] [PubMed]
- Bollig, E.R.; Hirsch, E.B.; Bueno, I.; Lynfield, R.; Granick, J.L.; Gens, K.D.; Rashid, A.; Harris, K.; Boeser, K.; Beaudoin, A.L. Minnesota One Health Antibiotic Stewardship Collaborative: A Reproducible Approach to Facilitate Antimicrobial Stewardship Progress. In Open Forum Infectious Diseases; Oxford University Press: Oxford, UK, 2022; p. ofac602. [Google Scholar]
- World Health Organization. Implementing the Global Health Sector Strategies on HIV, Viral Hepatitis and Sexually Transmitted Infections, 2022–2030: Report on Progress And Gaps 2024; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Sittivarakul, W.; Aramrungroj, S.; Seepongphun, U. Clinical features and incidence of visual improvement following systemic antibiotic treatment in patients with syphilitic uveitis. Sci. Rep. 2022, 12, 12553. [Google Scholar] [CrossRef] [PubMed]

| Study | Clinical Entity | Key Signs | Common Pitfalls | Key Differentials | Imaging Correlates | Evolution After Treatment |
|---|---|---|---|---|---|---|
| Alhawsawi et al. [15] | Anterior uveitis | Blurred vision, floaters, red eye with pain, conjunctival injection | Misdiagnosed as autoimmune uveitis | HLA-B27 anterior uveitis and viral uveitis | Slit-lamp; OCT | Responsive to IV penicillin; VA recovery varies |
| Shahid et al. [22] | Anterior uveitis | Similar prevalence to posterior uveitis; 25.9% anterior vs. 22.4% posterior | Mistaken for idiopathic cases | Idiopathic uveitis and sarcoidosis | OCT; FA | Improves with systemic antibiotics |
| Cillino et al. [25] | Eyelid chancre with HIV co-infection | Painless eyelid ulcer, resolving lesion at lateral canthus → later bilateral chorioretinitis | Misdiagnosed as chalazion | Viral keratitis and chalazion | Fundus photo; FA | Lesions resolved after penicillin |
| Zhu et al. [34] | Syphilitic scleritis | Painful red eye, nodular anterior scleritis, necrotizing form is rare | Misdiagnosed as rheumatoid scleritis | RA, TB scleritis, HSV | Anterior segment OCT | Responds to IV penicillin; superficial type; good prognosis |
| Knox et al. [32] | Interstitial keratitis (congenital syphilis) | Keratitis, deafness, Hutchinson’s teeth (Hutchinson’s triad) | Misdiagnosed as herpetic keratitis | HSV keratitis and autoimmune IK | OCT: stromal haze and outer retina changes) | Response to antibiotics; vision recovery possible |
| Study | Clinical Entity | Key Signs | Common Pitfalls | Key Differentials | Imaging Correlates | Evolution After Treatment |
|---|---|---|---|---|---|---|
| Oliver et al. (2016) [11]; Zhang et al. (2017) [17] | Posterior uveitis/panuveitis | Blurred vision, foveal involvement, vitreous haze | Misdiagnosed as autoimmune posterior uveitis | Tuberculous uveitis; sarcoid uveitis | OCT/FA: vitritis and chorioretinal lesions | Responds to IV penicillin, with partial visual acuity recovery |
| Jabbehdari et al. (2017) [37]; Alhawsawi et al. (2025) [15] | Retinal vasculitis | Perivascular sheathing and vascular leakage on FA | Mistaken for TB or idiopathic vasculitis | Behçet’s disease; TB uveitis | FA: vascular leakage; OCT: retinal edema | Improves with systemic antibiotics ± corticosteroids |
| Du et al.(2025) [38]; JUMPER et al.(2000) [39]; Shughoury et al.(2024) [40] | Retinal detachment | Exudative or rhegmatogenous detachment, often with uveitis/retinitis | Misdiagnosed as autoimmune retinopathy | Vogt–Koyanagi–Harada disease; CMV retinitis | OCT: subretinal fluid; FA: pooling | Exudative detachment resolves with penicillin; RRD often needs surgery |
| Du et al.(2025) [38]; Smith et al.(2006) [41]; Moore et al.(2015) [42] | Optic neuropathies | Optic neuritis, disc edema, papilledema | Misdiagnosed as demyelinating optic neuritis | Multiple sclerosis, NMO, ischemic optic neuropathy | OCT: RNFL changes; MRI: optic nerve enhancement | Variable recovery; poorer outcomes in HIV+ |
| Eandi et al.(2012) [36]; Pichi et al.(2014) [43]; Wai et al.(2022) [44]; Herbort et al.(2020) [45] | ASPPC | Macular placoid yellow lesions, RPE disruption, vitreous inflammation | Mistaken for APMPPE or serpiginous choroiditis | APMPPE; MEWDS | OCT: EZ loss and RPE nodules; FAF: hyperautofluorescence; FA/ICGA: choroidal hypoperfusion | Usually resolves with antibiotics; anatomical recovery common |
| Modality | Sensitivity/Specificity (Reported Ranges) | Key Limitations | References |
|---|---|---|---|
| Non-treponemal tests (NTT: RPR and VDRL) | Sensitivity 48.7–76.1% vs. dark-field microscopy; CSF-VDRL sensitivity 50–78.4% | False-negative results (esp. ocular/neuro involvement); up to 40% of ocular syphilis patients with low/negative RPR; poor sensitivity for neurosyphilis | [56,58,59,60,61] |
| Treponemal tests (TT: TPHA and FTA-ABS) | High sensitivity; lifelong positivity | Cannot distinguish active vs. past infection; not reliable for follow-up or isolated ocular disease | [58,62,63] |
| CSF-VDRL | Highly specific but insensitive | Negative result does not exclude neurosyphilis; invasive | [64,65] |
| CSF-FTA-ABS | Highly sensitive, less specific than CSF-VDRL | Not recommended for monitoring treatment; may yield false positives | [64,65,66] |
| Intraocular antibody index | Adjunctive diagnostic tool (no standardized sensitivity) | Limited validation; may be negative in immunocompromised patients | [56,64] |
| Aqueous/vitreous PCR (Treponema pallidum DNA) | Sensitivity > 85% in active phase; high specificity; qPCR can monitor bacterial load | Requires invasive sample; limited lab availability | [71,72,73] |
| OCT (SD-OCT and SS-ASOCT) | Detects retinal/choroidal inflammatory changes; macular OCT valuable in optic neuropathy | Nonspecific; cannot directly confirm syphilis | [17,43,68,70] |
| Near-infrared reflectance (NIR) | Sensitive to syphilitic outer retinitis, detects subtle retinal lesions | Adjunctive only; not specific | [68,69] |
| Fundus autofluorescence (FAF) and OCT angiography (OCTA) | Described as adjunctive, useful for structural/vascular changes | Lack of standardized sensitivity data | [68,70] |
| Regimen | Dose and Duration | Pros/Cons | Evidence Level | Special Situations |
|---|---|---|---|---|
| IV Penicillin G | 18–24 million units/day (3–4 million units q4h or continuous infusion), 10–14 days | Gold standard; excellent CNS penetration; proven efficacy. Limited by need for hospitalization or IV access. | High (CDC guidelines, RCTs, cohort studies) | First-line for all patients, including pregnancy and HIV co-infection [75,77]. |
| Ceftriaxone | 2 g IV/IM daily, 10–14 days | Alternative in penicillin allergy; good CNS penetration. Limited evidence in ocular syphilis; efficacy not fully established. | Moderate (observational studies and case reports) | Consider only if penicillin cannot be given. Use with caution in HIV [75,77]. |
| Doxycycline | 100 mg orally twice daily, 28 days | Oral route convenient; accessible in resource-limited areas. Poor CSF penetration; limited evidence in ocular/neurosyphilis. Not equivalent to penicillin. | Low (small case series and expert opinion) | Not recommended except when penicillin/ceftriaxone unavailable. Contraindicated in pregnancy; limited efficacy in HIV [78,79]. |
| Adjunctive Corticosteroids | Prednisone (short taper course; variable dose) | May reduce inflammation and Jarisch–Herxheimer reaction; evidence is empirical. No effect on pathogen clearance. | Low (case series and expert consensus) | Used cautiously to control uveitis or severe inflammation [80]. |
| Experimental/Emerging Approaches | Intravitreal antibiotics; immunomodulators; biomarker-guided retreatment (e.g., CSF CXCL13) | Potential for refractory cases; biomarkers may help monitor treatment. Not validated by large trials. | Very low (pilot studies and animal models) | Consider in HIV-associated neurosyphilis or retreatment contexts [81]. |
| Feature/Outcome | HIV-Negative Patients | HIV-Positive Patients | References |
|---|---|---|---|
| Frequency of ocular involvement | Lower frequency of ocular symptoms in syphilis patients | Nearly 2× higher risk of ocular symptoms among syphilis patients with HIV | [43,86] |
| Common ocular phenotype | More anterior/intermediate uveitis; focal retinitis; placoid chorioretinitis | Higher frequency of posterior uveitis, panuveitis, and optic neuropathy | [87,88,89] |
| CSF abnormalities | Less frequent; lumbar puncture performed in ~61% | More frequent (pleocytosis and protein elevation); lumbar puncture performed in ~83% | [87,88] |
| Serological response | Conventional NTT/TT more reliable, but false negatives occur | Serological response altered; atypical or discordant serology under HIV-induced immune dysregulation | [56,62,63,87] |
| Treatment response | Generally favorable with IV penicillin | Suboptimal response; higher risk of incomplete clearance; possible need for retreatment; CSF CXCL13 may persist | [75,81,87,88] |
| Visual prognosis | Good if treated early; favorable outcomes in many cases | Prognosis often poorer; systematic reviews show higher recurrence and worse visual recovery | [57,90] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye, Z.; Yang, M.; Zou, Y.; Zhang, J.; Deng, J.; Zong, Y.; Ohno-Matsui, K.; Kamoi, K. Syphilis and the Eye: Clinical Features, Diagnostic Challenges, and Evolving Therapeutic Paradigms. Pathogens 2025, 14, 852. https://doi.org/10.3390/pathogens14090852
Ye Z, Yang M, Zou Y, Zhang J, Deng J, Zong Y, Ohno-Matsui K, Kamoi K. Syphilis and the Eye: Clinical Features, Diagnostic Challenges, and Evolving Therapeutic Paradigms. Pathogens. 2025; 14(9):852. https://doi.org/10.3390/pathogens14090852
Chicago/Turabian StyleYe, Zizhen, Mingming Yang, Yaru Zou, Jing Zhang, Jiaxin Deng, Yuan Zong, Kyoko Ohno-Matsui, and Koju Kamoi. 2025. "Syphilis and the Eye: Clinical Features, Diagnostic Challenges, and Evolving Therapeutic Paradigms" Pathogens 14, no. 9: 852. https://doi.org/10.3390/pathogens14090852
APA StyleYe, Z., Yang, M., Zou, Y., Zhang, J., Deng, J., Zong, Y., Ohno-Matsui, K., & Kamoi, K. (2025). Syphilis and the Eye: Clinical Features, Diagnostic Challenges, and Evolving Therapeutic Paradigms. Pathogens, 14(9), 852. https://doi.org/10.3390/pathogens14090852






