Vaccinations for Expecting Mothers to Improve Pregnancy Care in Middle Tennessee
Abstract
1. Introduction
2. Methods
2.1. The 15 Tennessee Counties Included in This Study
2.2. Data Analysis Plan
2.2.1. Power Analysis
2.2.2. Analysis Plan
2.2.3. Analysis Plan for Quantitative Data
2.2.4. Analysis Plan for Qualitative Data
3. Results
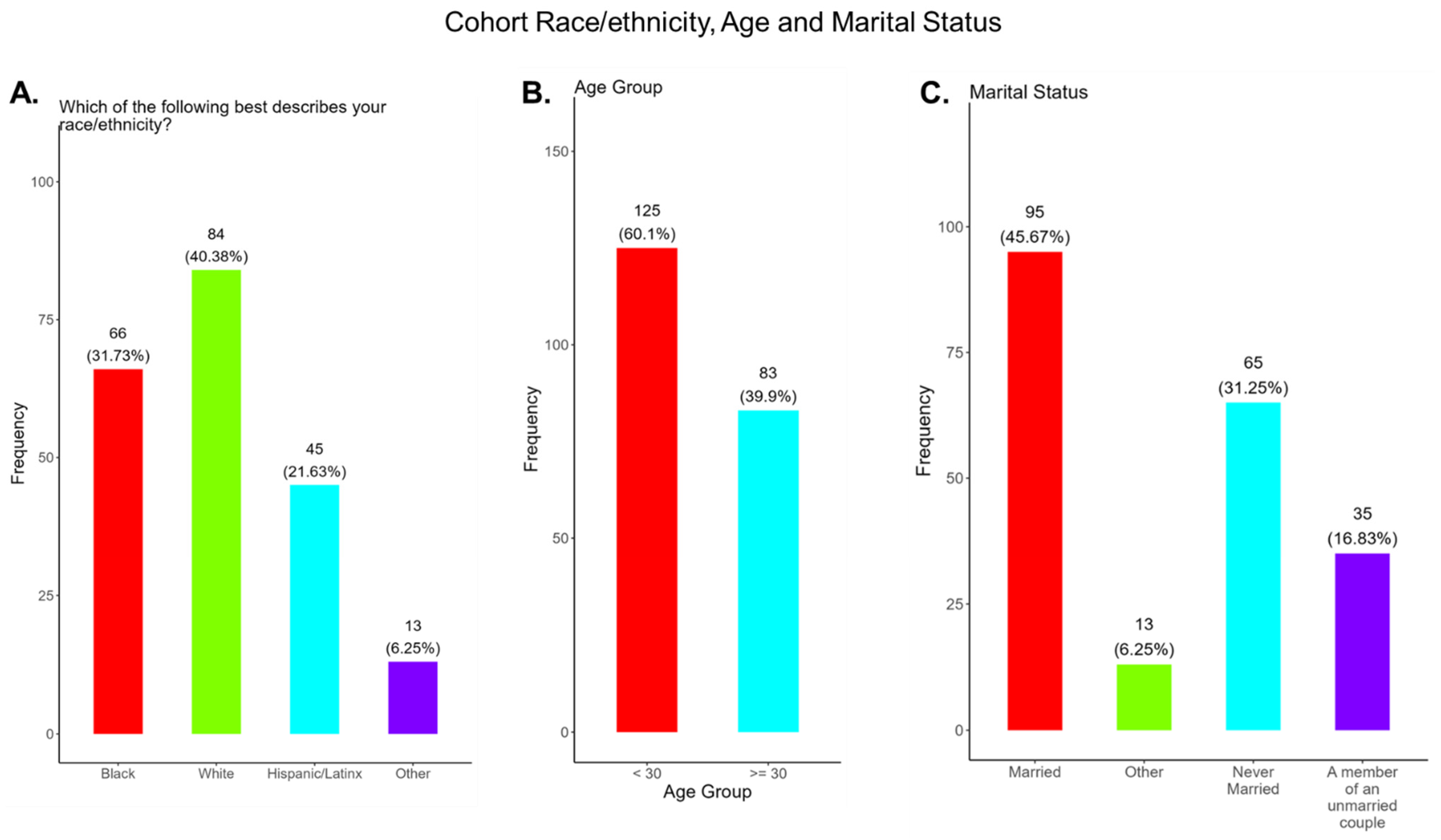
3.1. Cohort Demographics
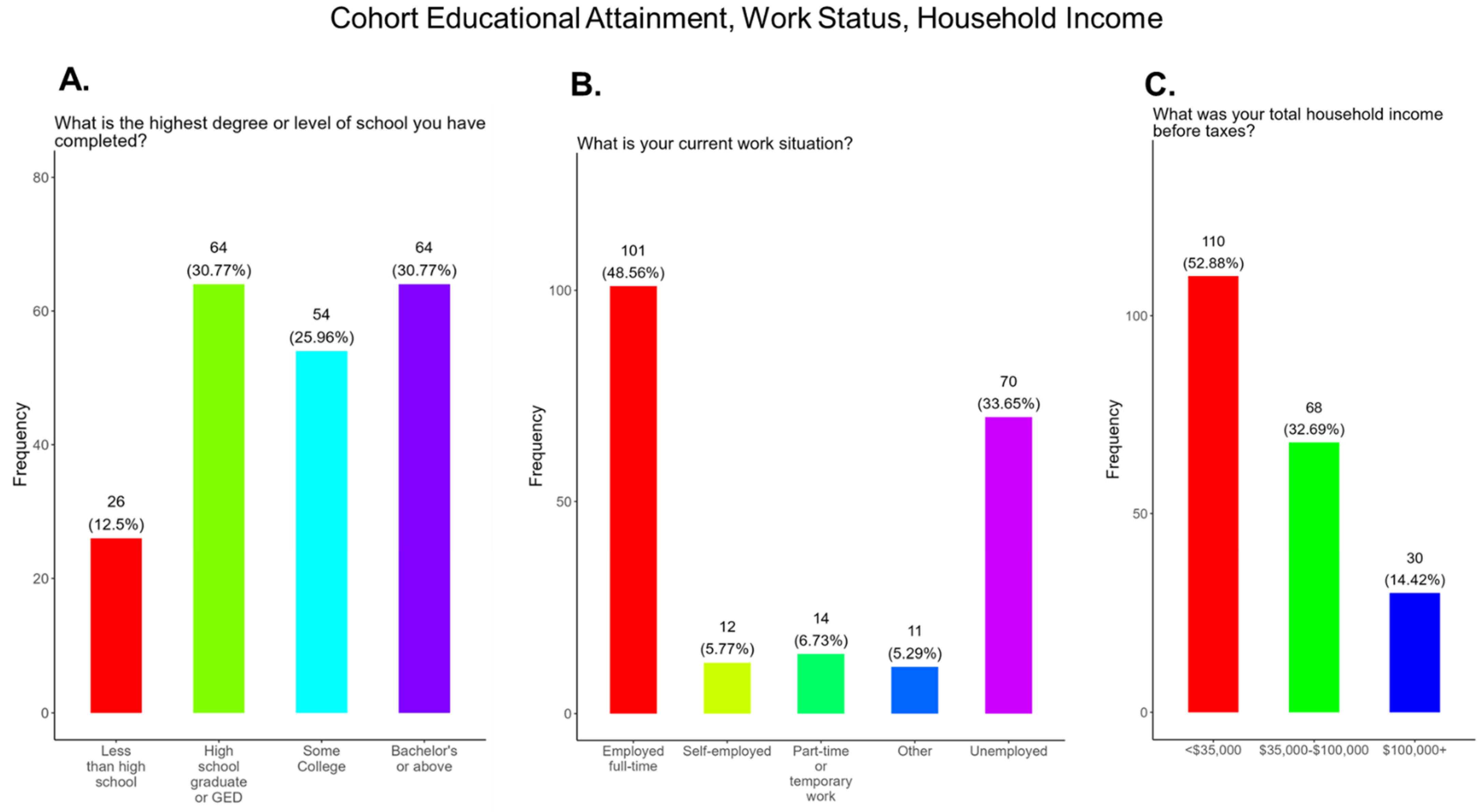
3.2. Differences in Cohort Educational Attainment and Socioeconomic Status
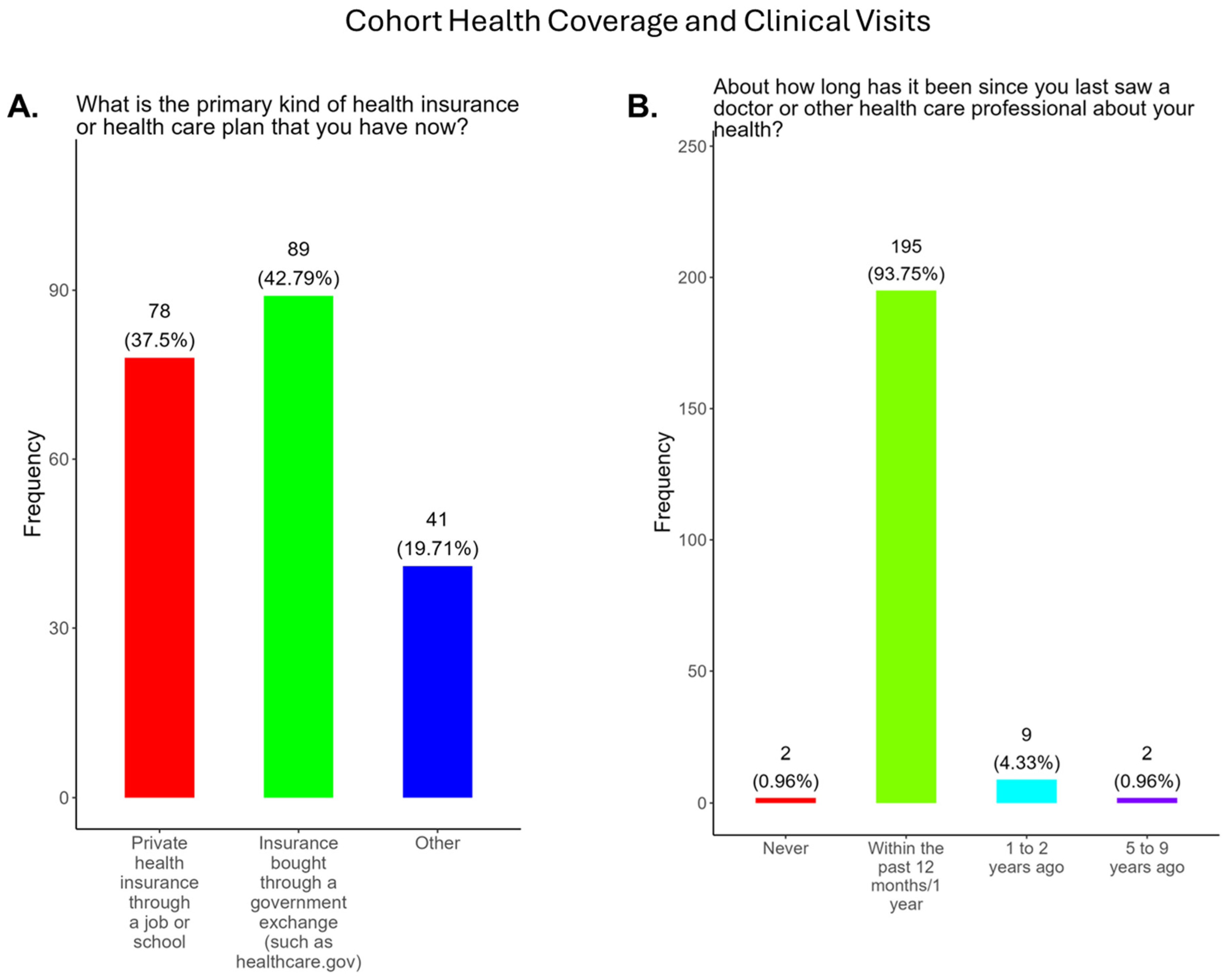
3.3. Strong Supportive Health Coverage and Prenatal Care for Expecting Mothers in Tennessee
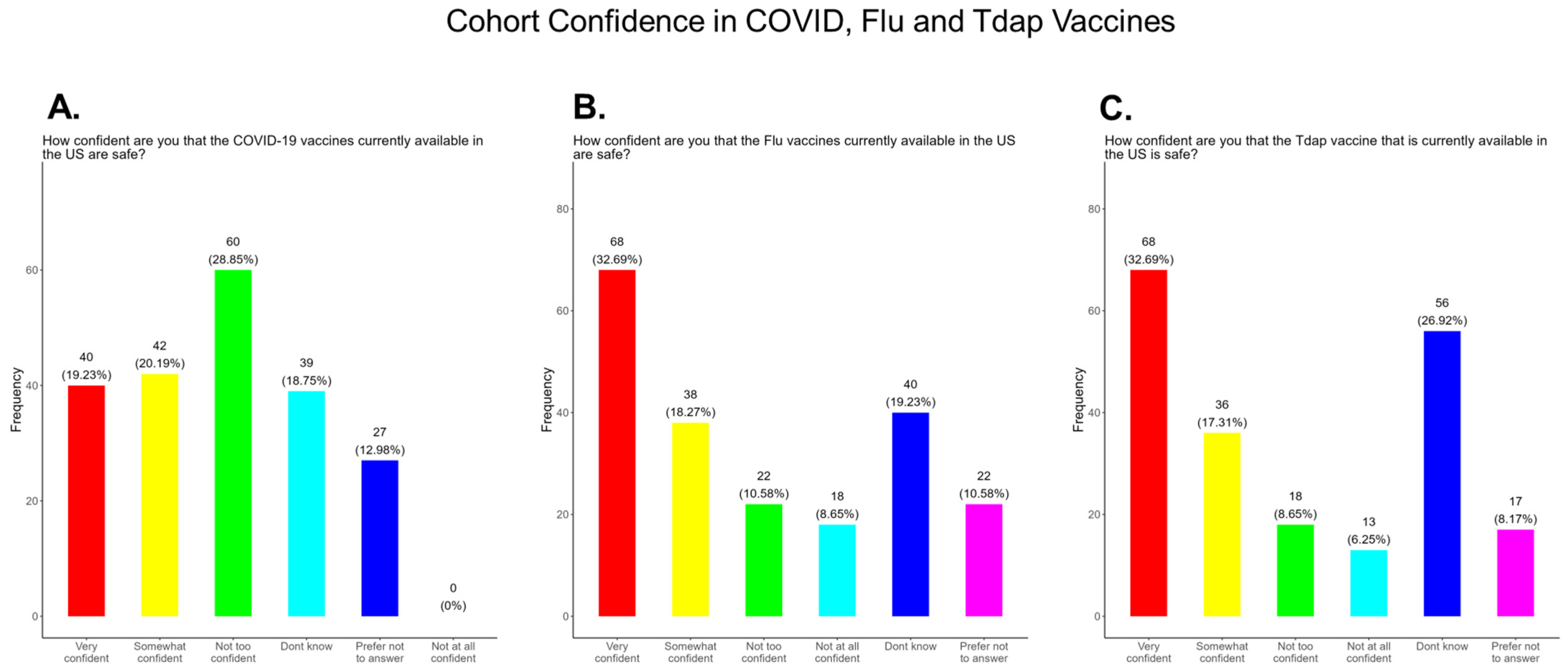
3.4. Poor Confidence in the COVID-19 Vaccine Compared to Flu and Tdap Vaccines
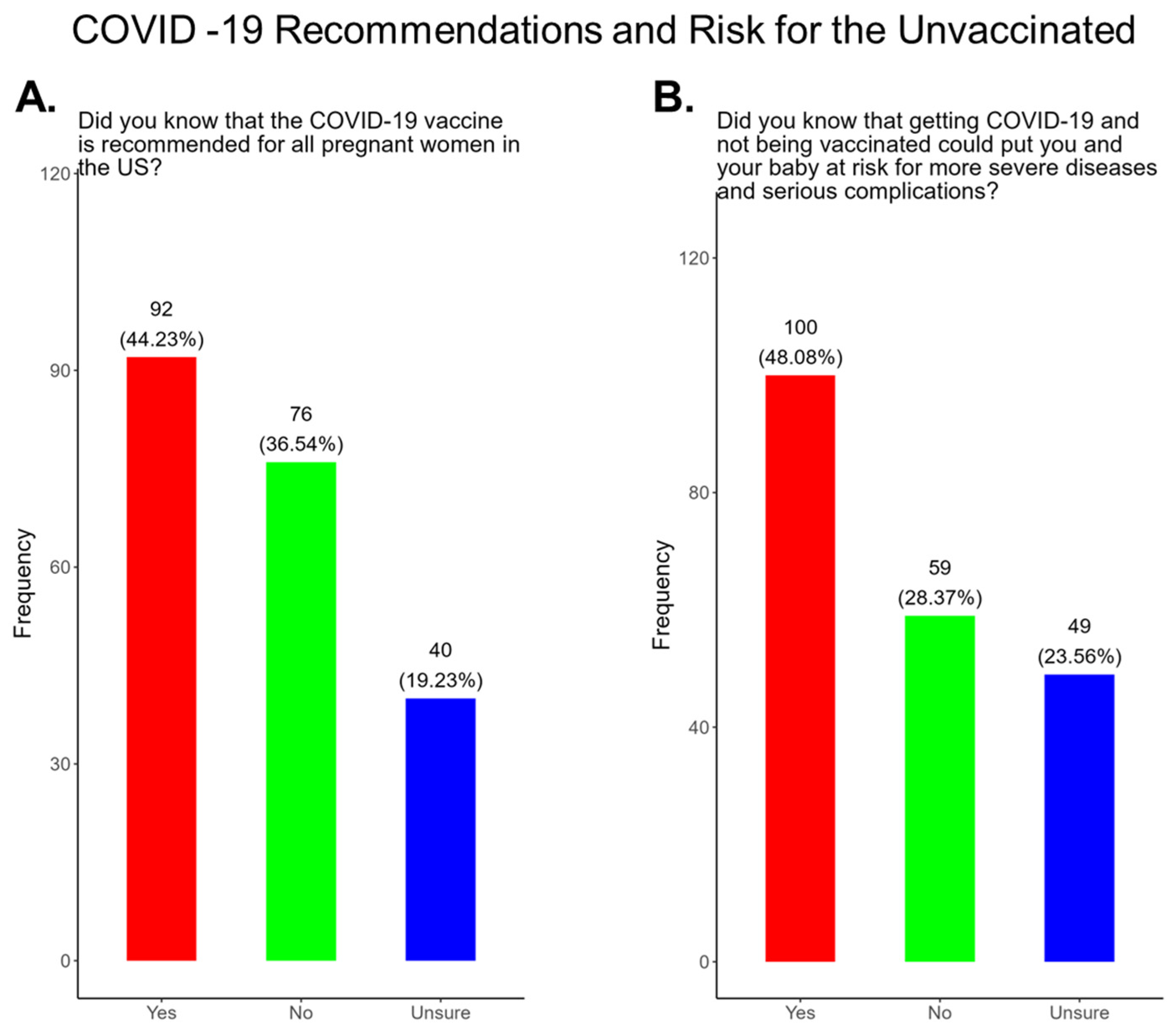
3.5. Most Pregnant Women in the Study Were Not Aware That the COVID-19 Vaccine Was Recommended for All Pregnant Women and Were Not Aware of the Health Risks Associated with Being Unvaccinated
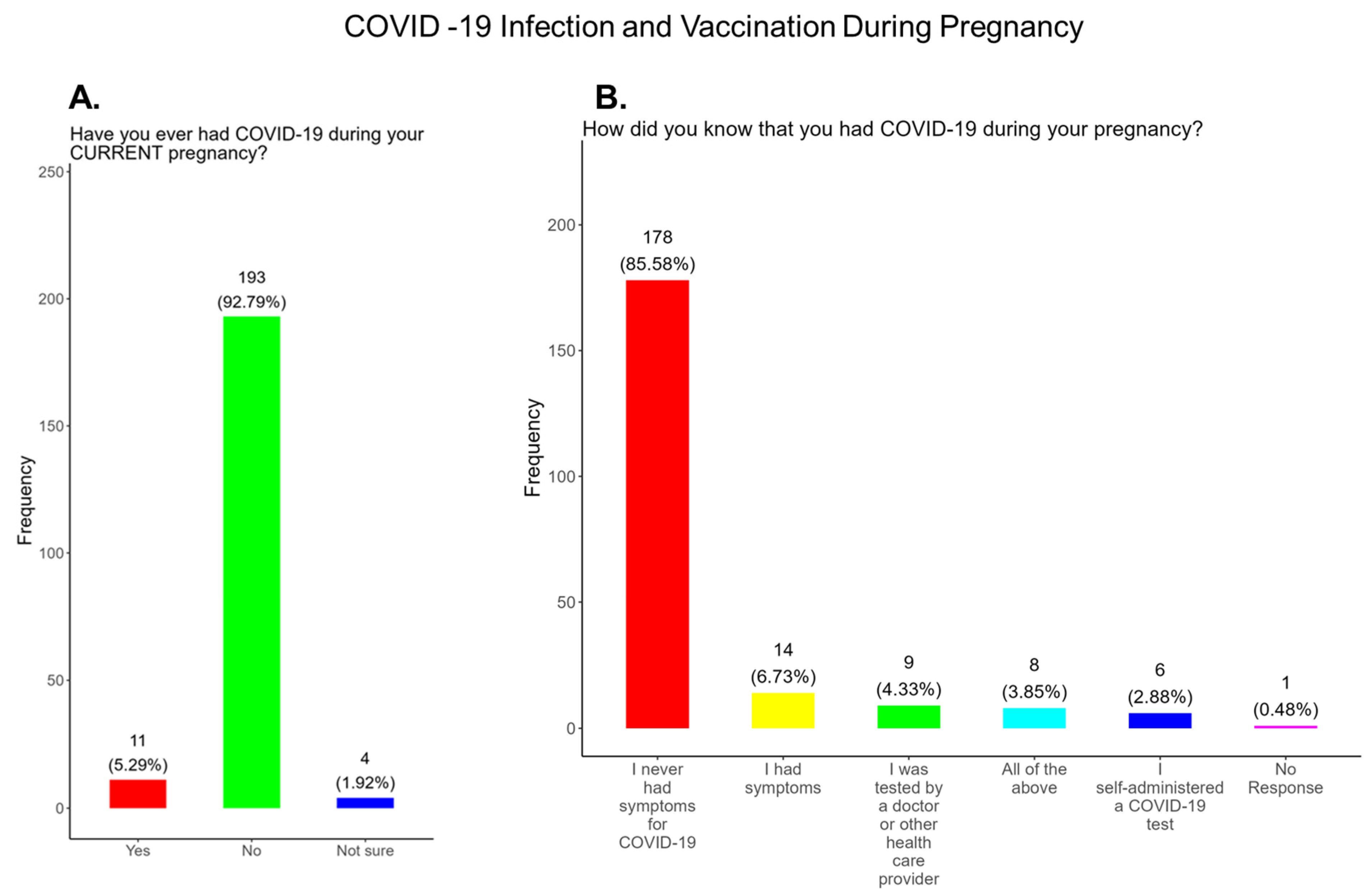
3.6. Poor Vaccine Confidence and Uptake of the COVID-19 Vaccine for Mothers and Babies and the Need for Health Literacy Surrounding Long COVID-19
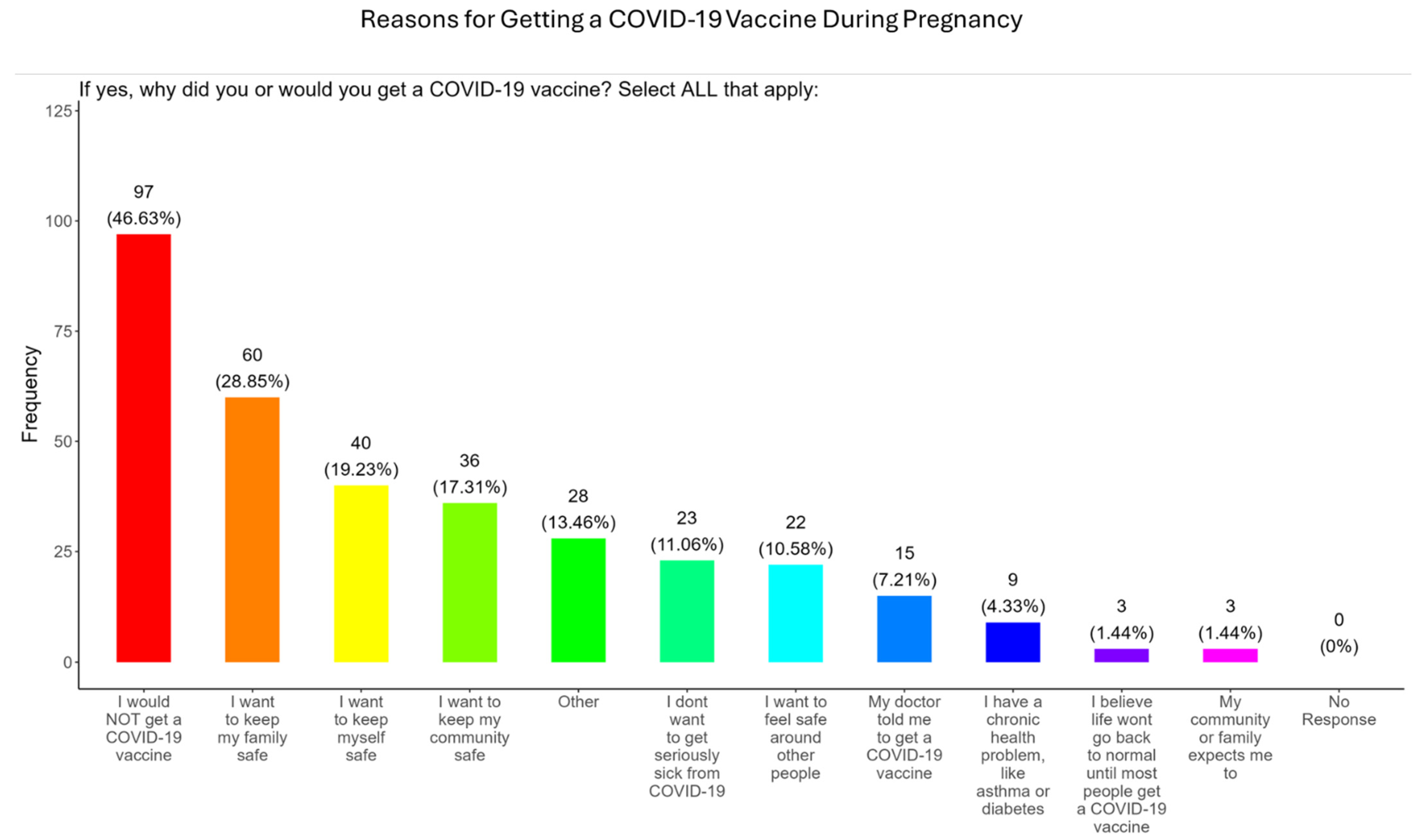
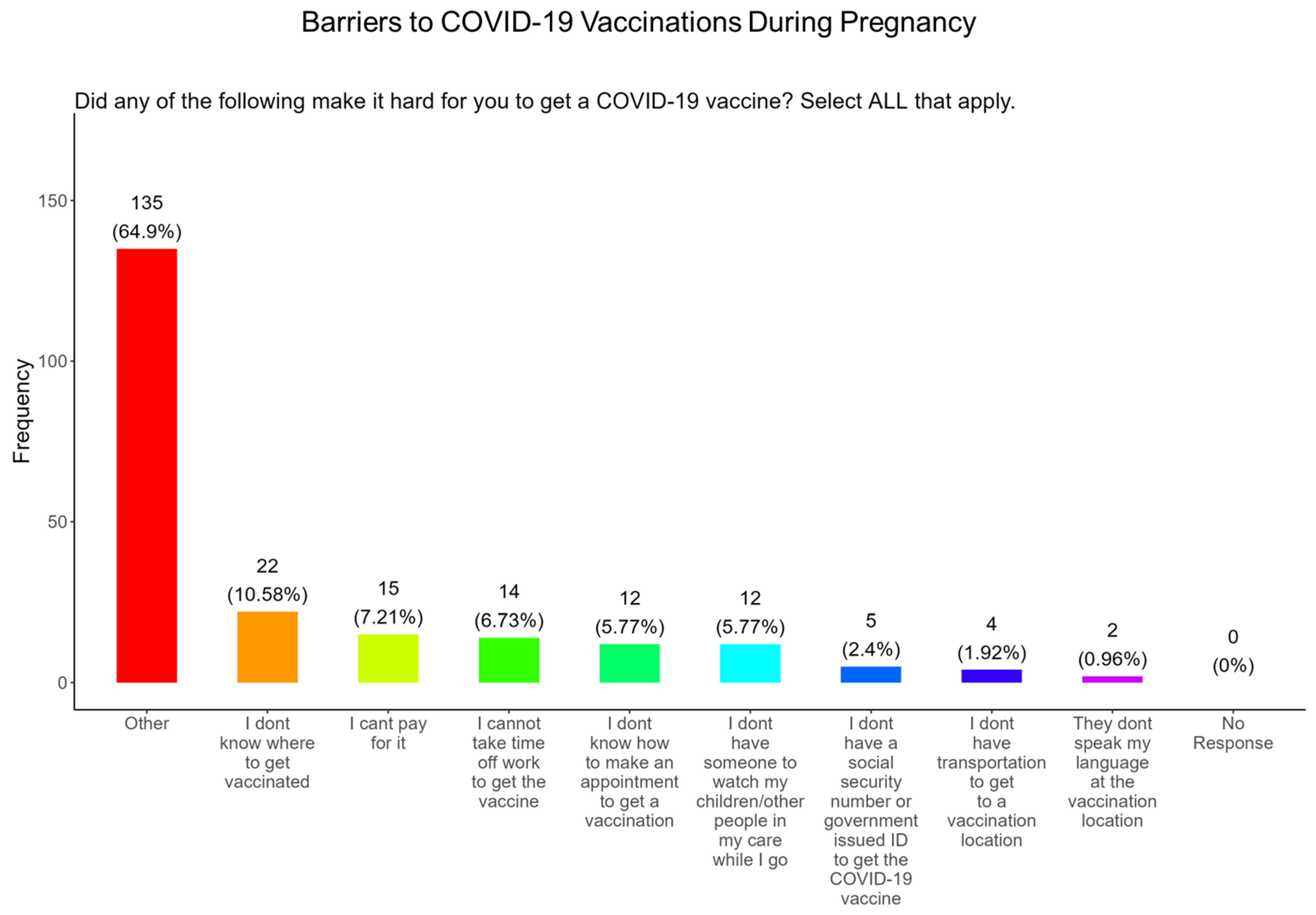
3.7. Participant Reasons for and Against Receiving COVID-19 Vaccine and Barriers to Vaccination
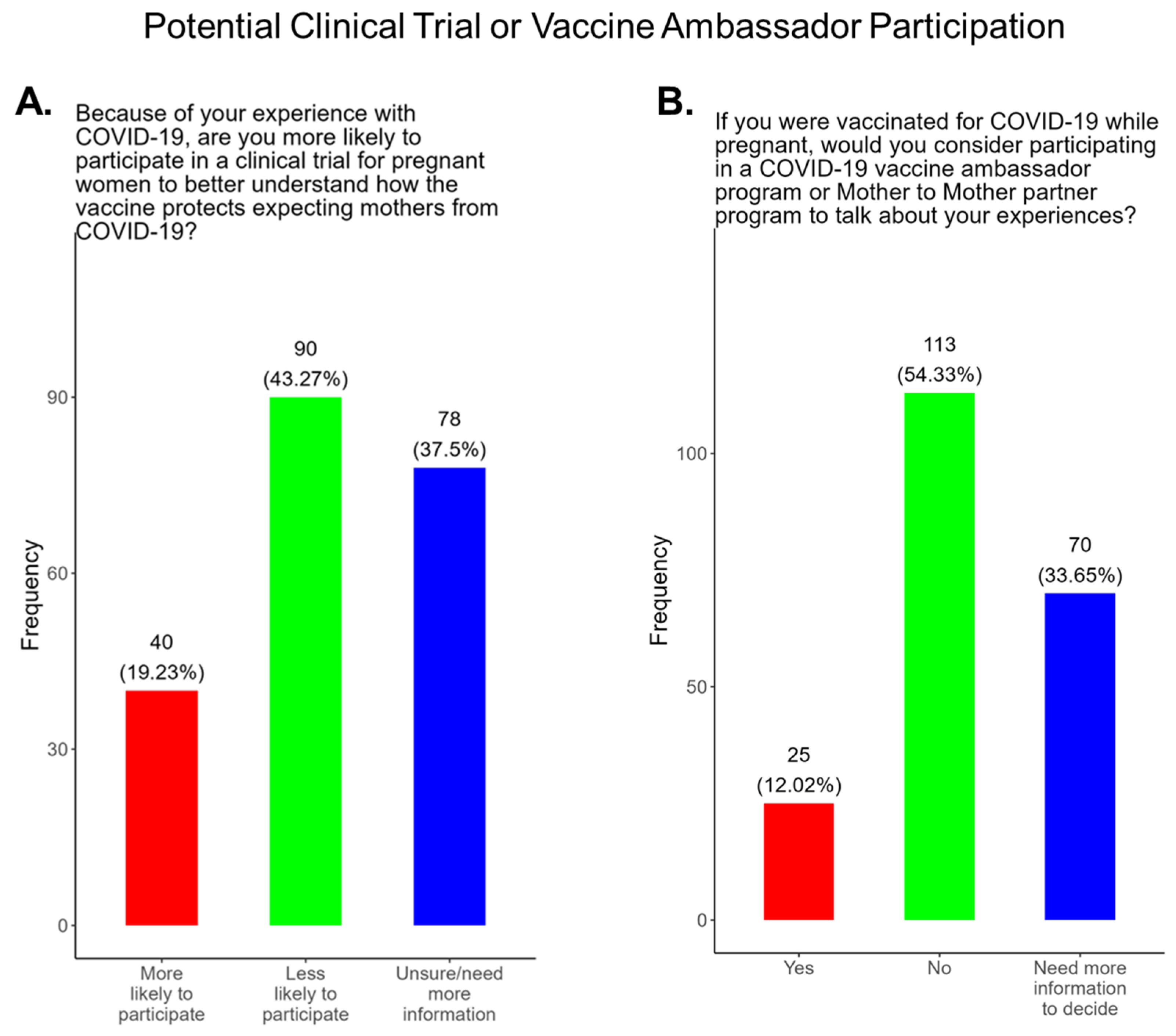
3.8. Study Participants Were Unlikely to Participate in COVID-19 Clinical Trials or Ambassador Programs to Support COVID-19-Related Studies
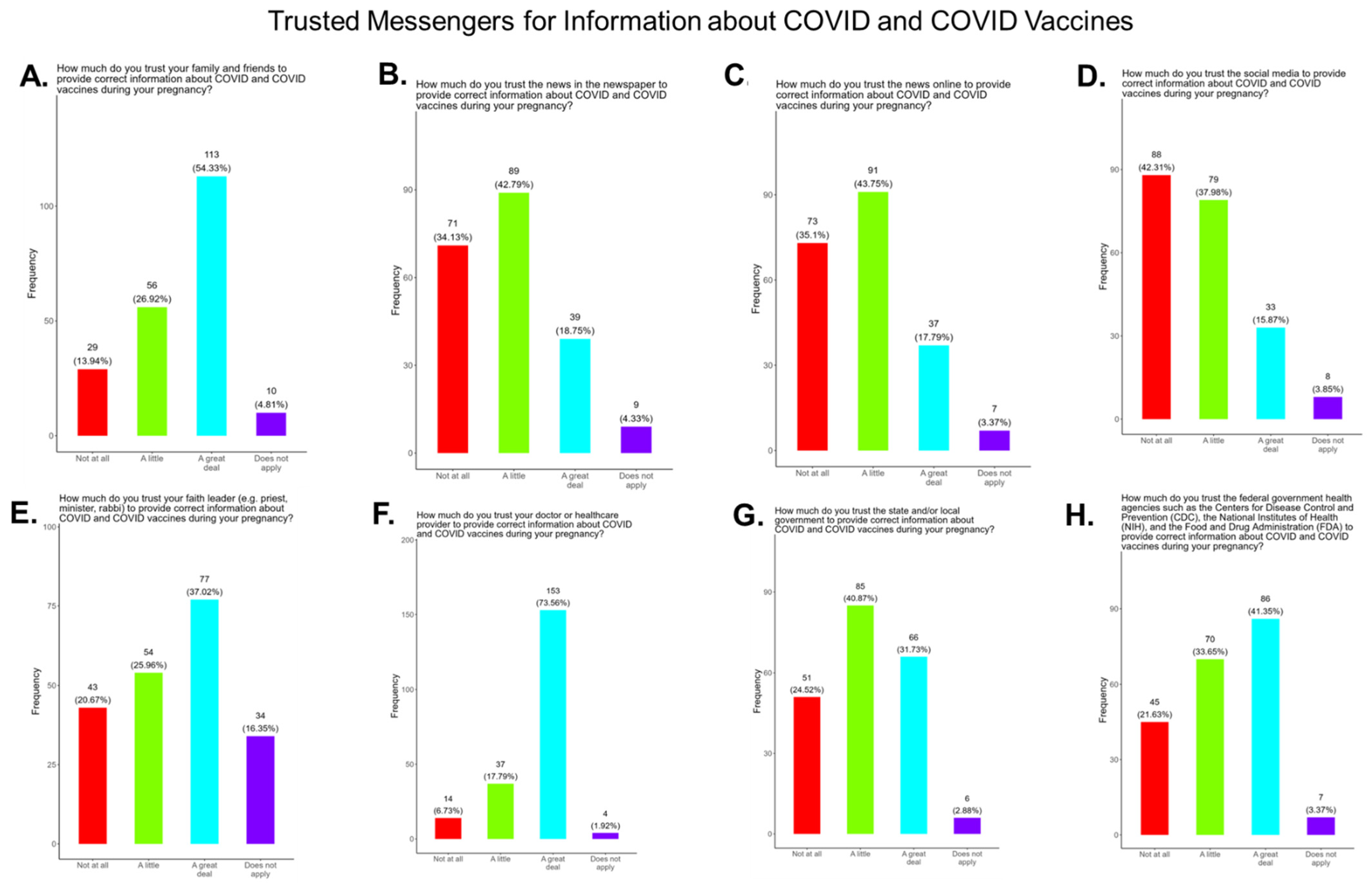
3.9. Assessment of the Level of Trust in COVID-19 Information Sources
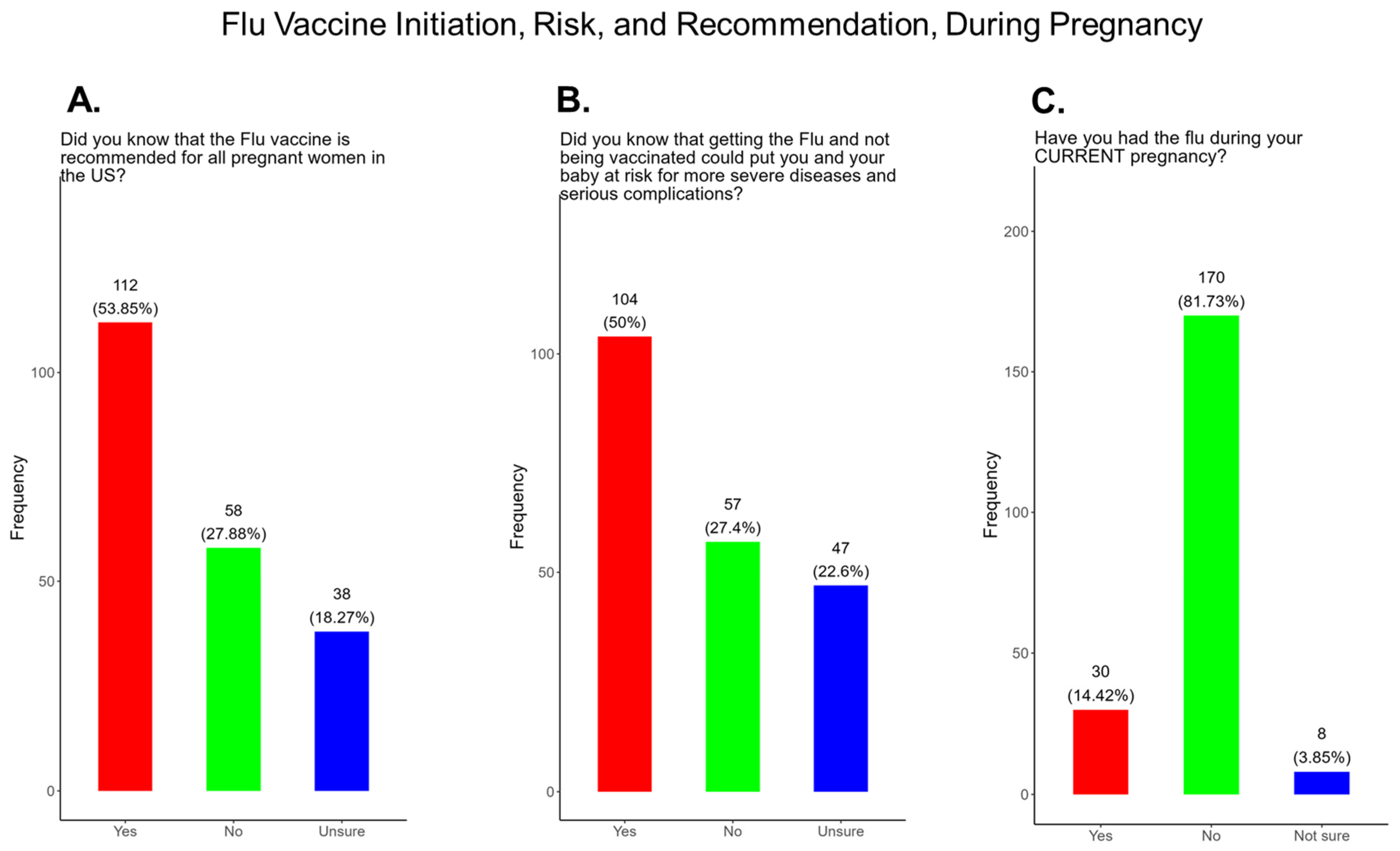
3.10. Flu Vaccine Initiation, Risk, and Recommendation During Pregnancy
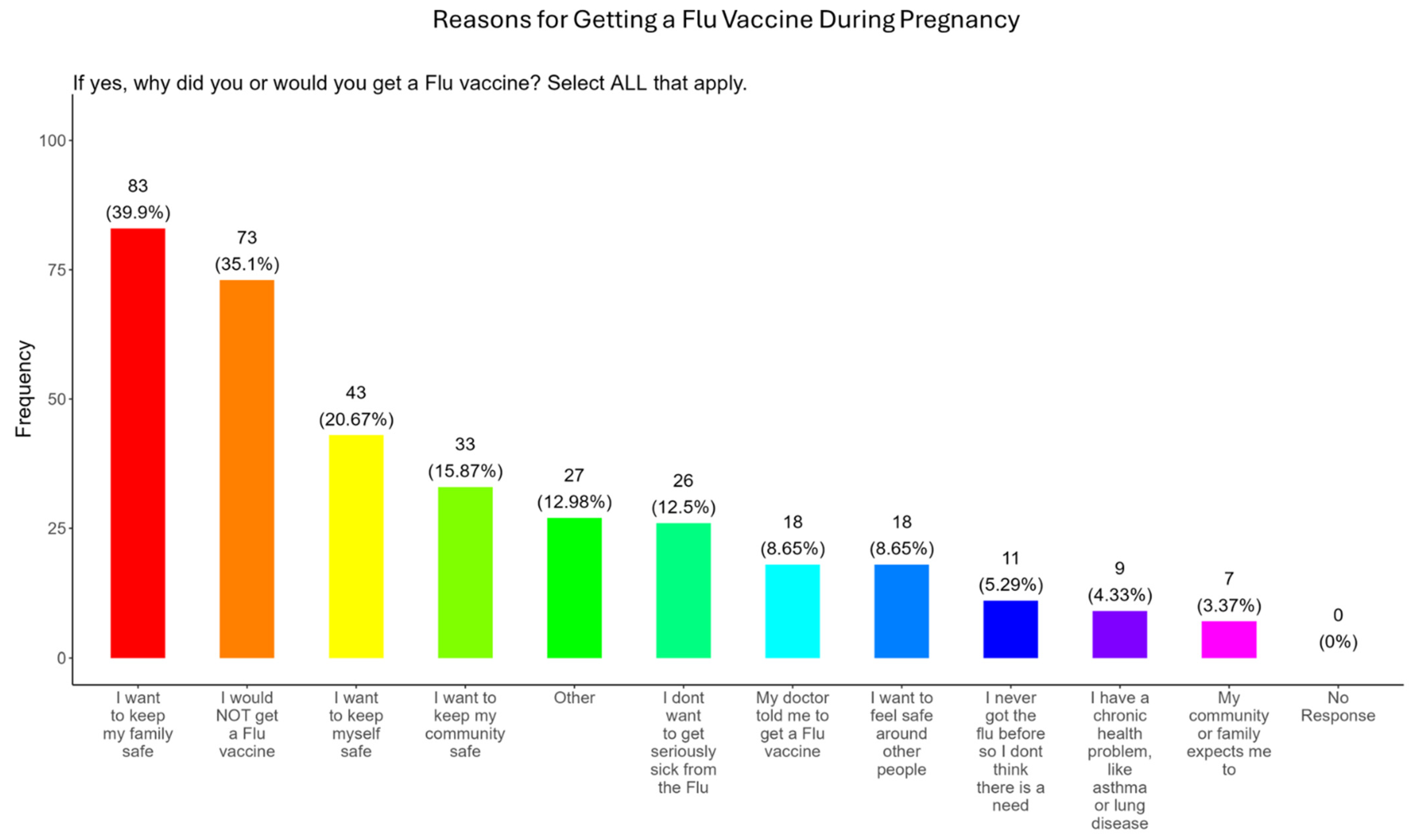
3.11. Family and Personal Safety Were the Most Important Reason for Participants Receiving the Flu Vaccine During Pregnancy
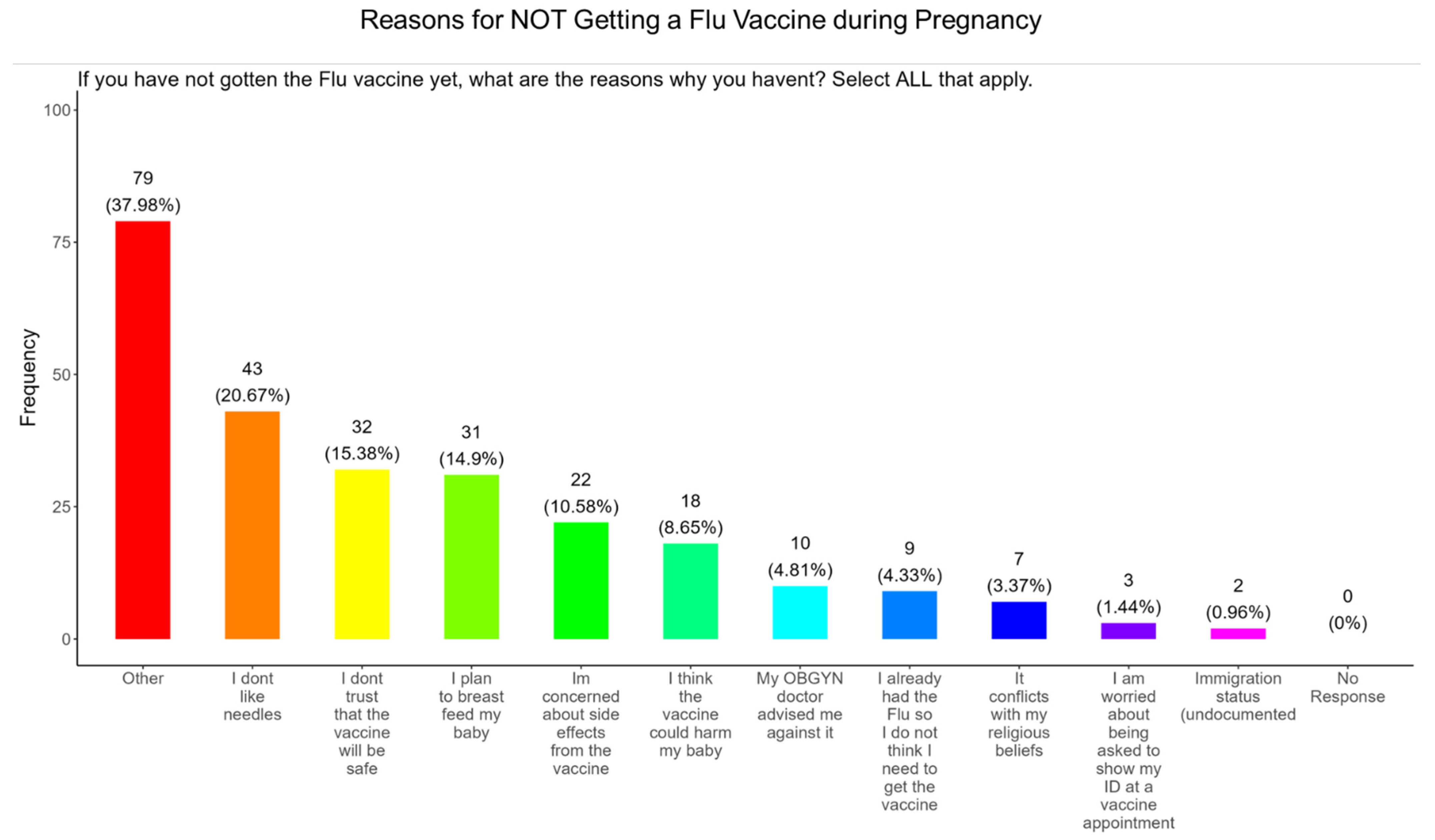
3.12. Needle Phobias and Distrust in Vaccine Safety Were the Most Important Reasons for Participants Not Receiving the Flu Vaccine During Pregnancy
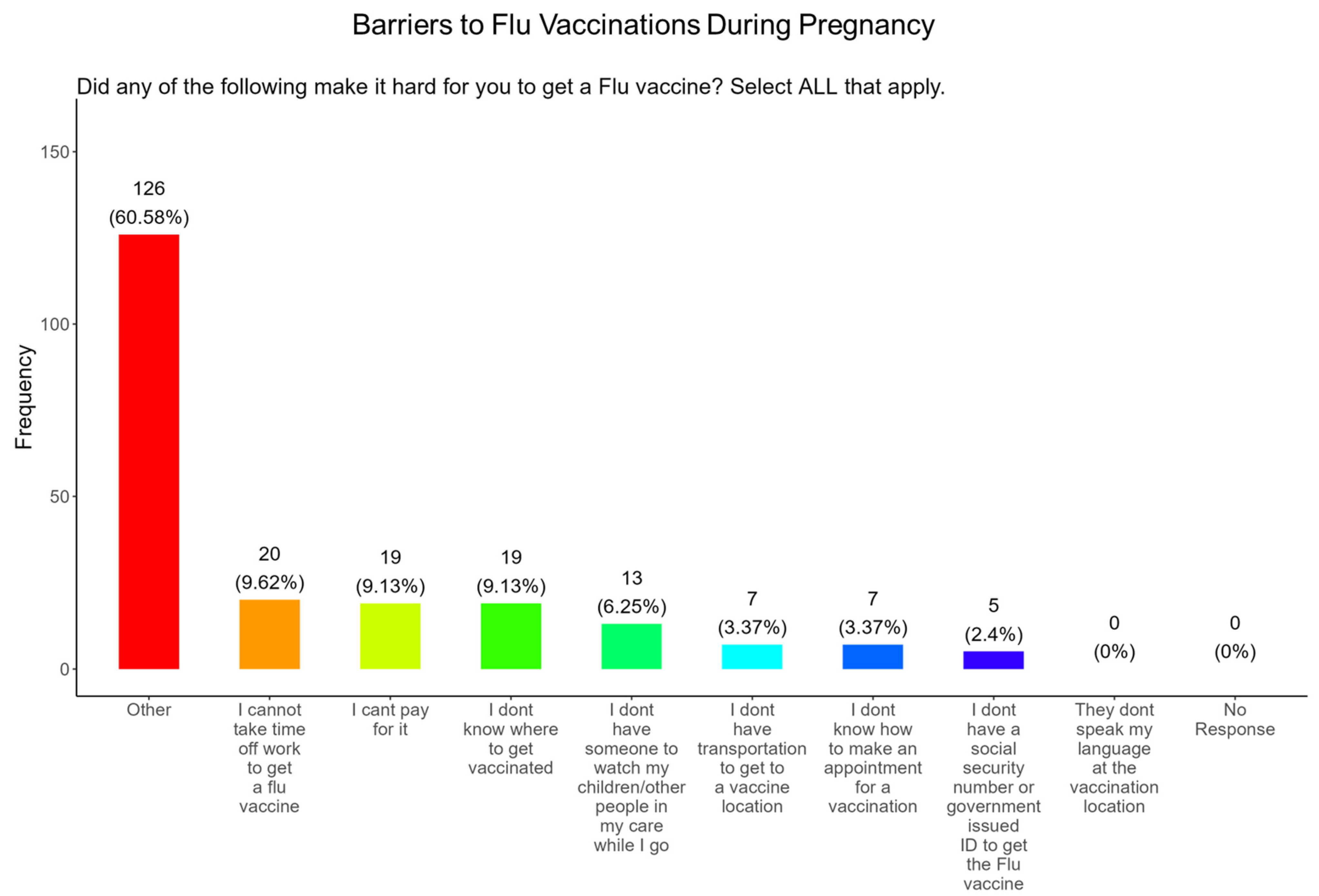
3.13. Time off from Work and the Affordability of the Vaccine Were the Most Important Barriers to Participants Receiving a Flu Vaccine During Pregnancy
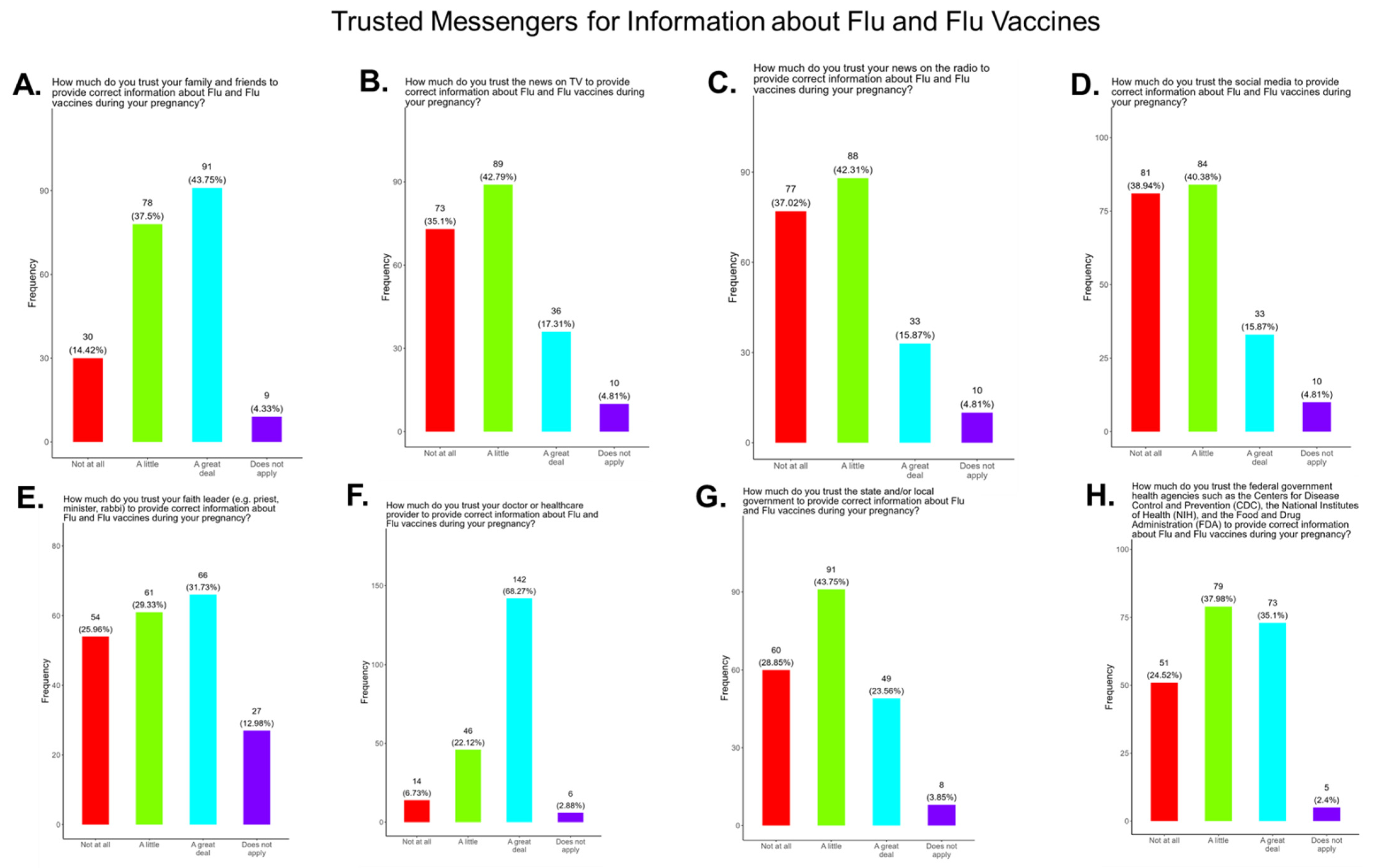
3.14. Assessment of the Level of Trust in Flu Information Sources
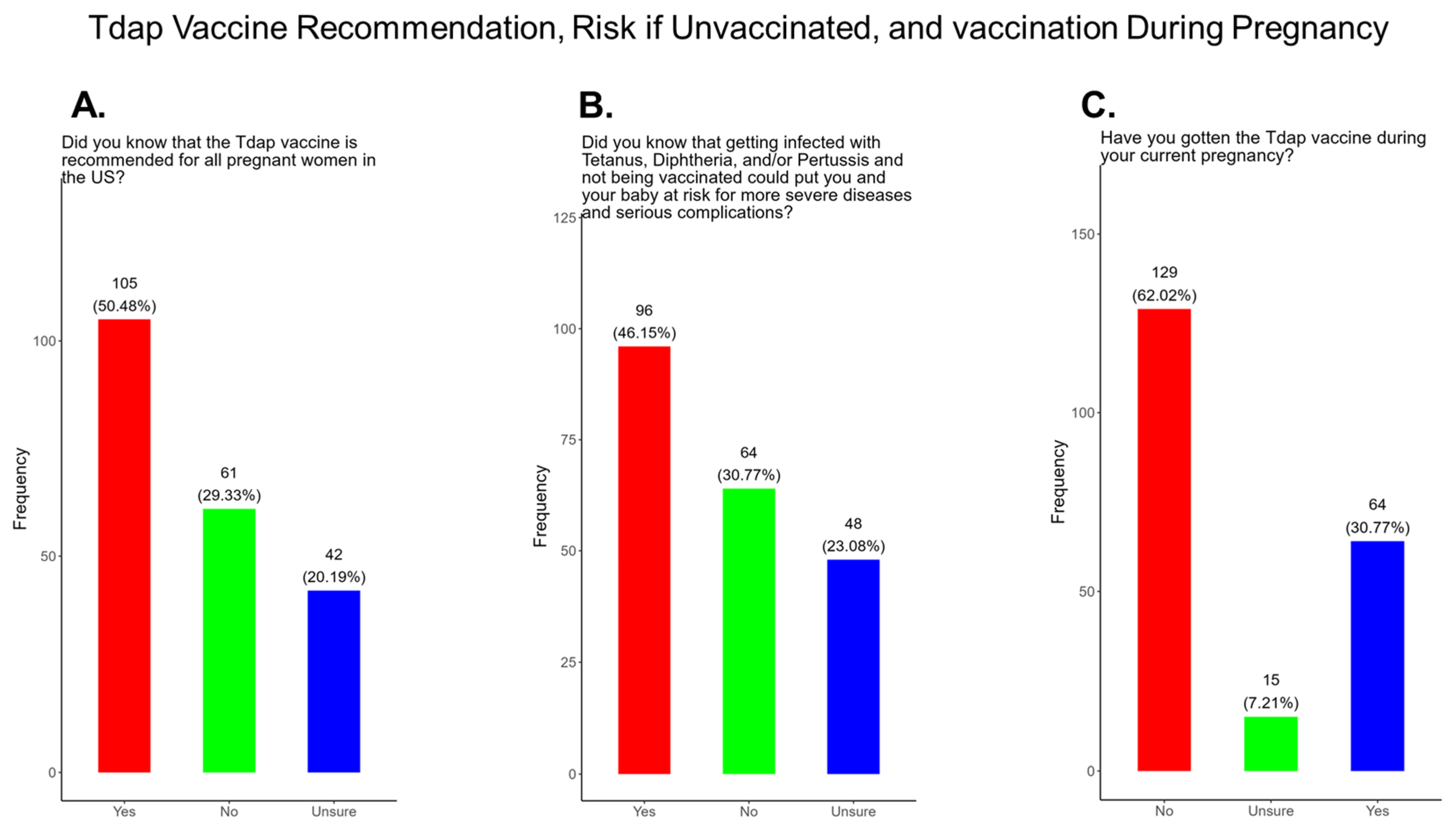
3.15. Only Half of the Expecting Mothers in the Study Were Aware That the Tdap Vaccine Was Recommended for All Pregnant Women, as Well as the Risk of Being Unvaccinated
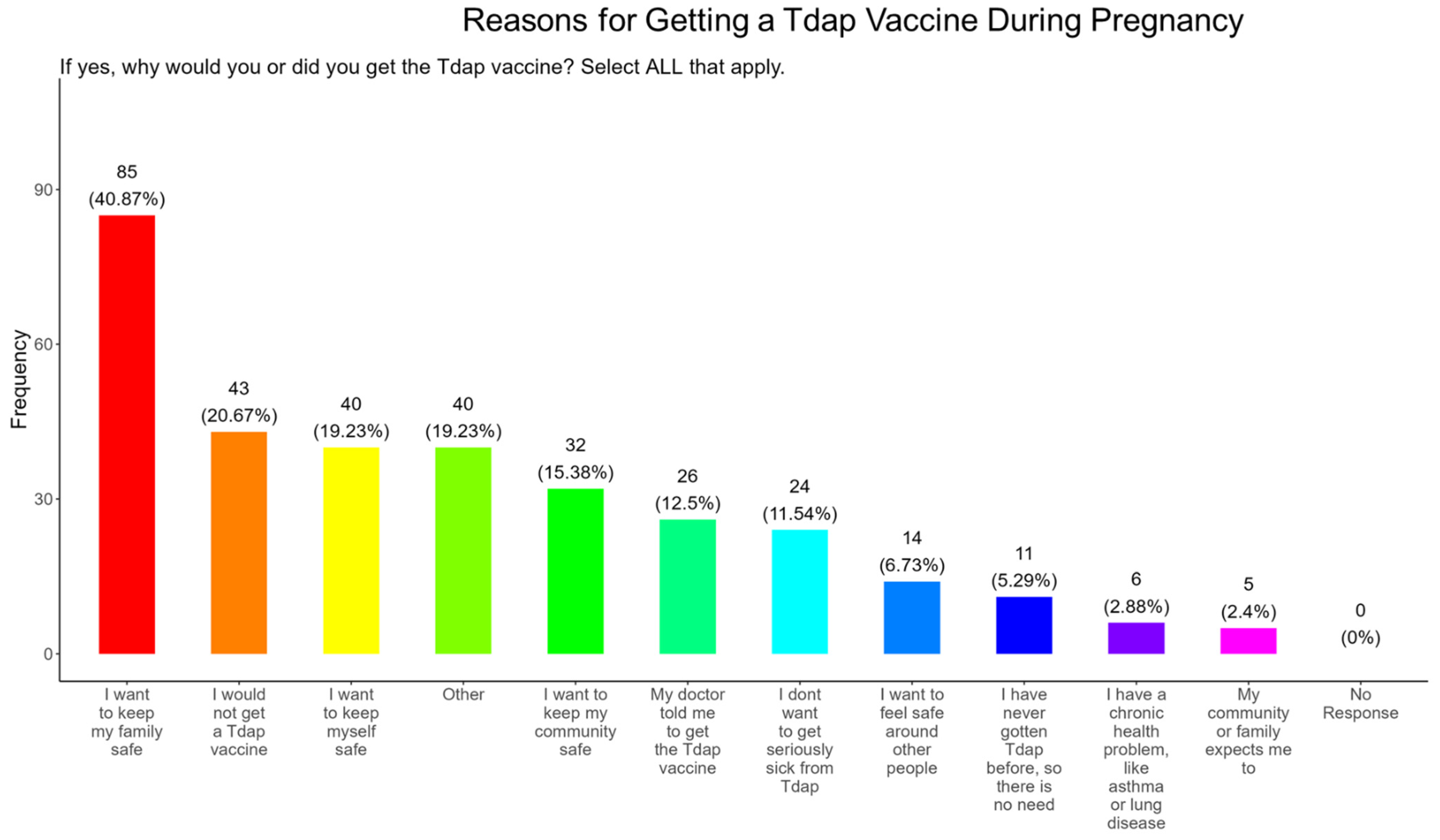
3.16. Family and Personal Safety Were the Most Important Reason for Participants Receiving the Tdap Vaccine During Pregnancy
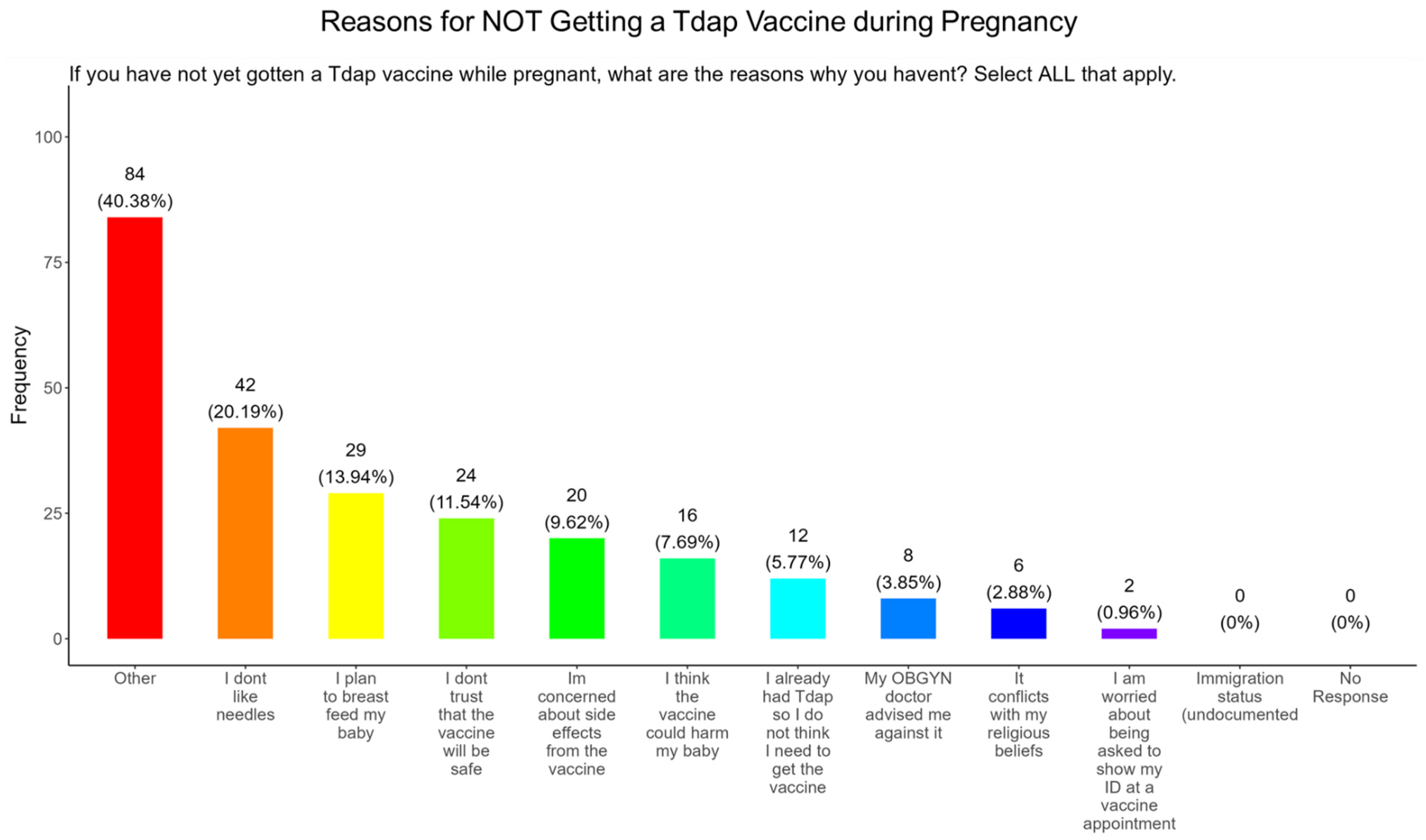
3.17. Needle Phobias and Plans to Breastfeed Their Infants Were the Most Important Reasons for Participants Not Receiving the Tdap Vaccine During Pregnancy
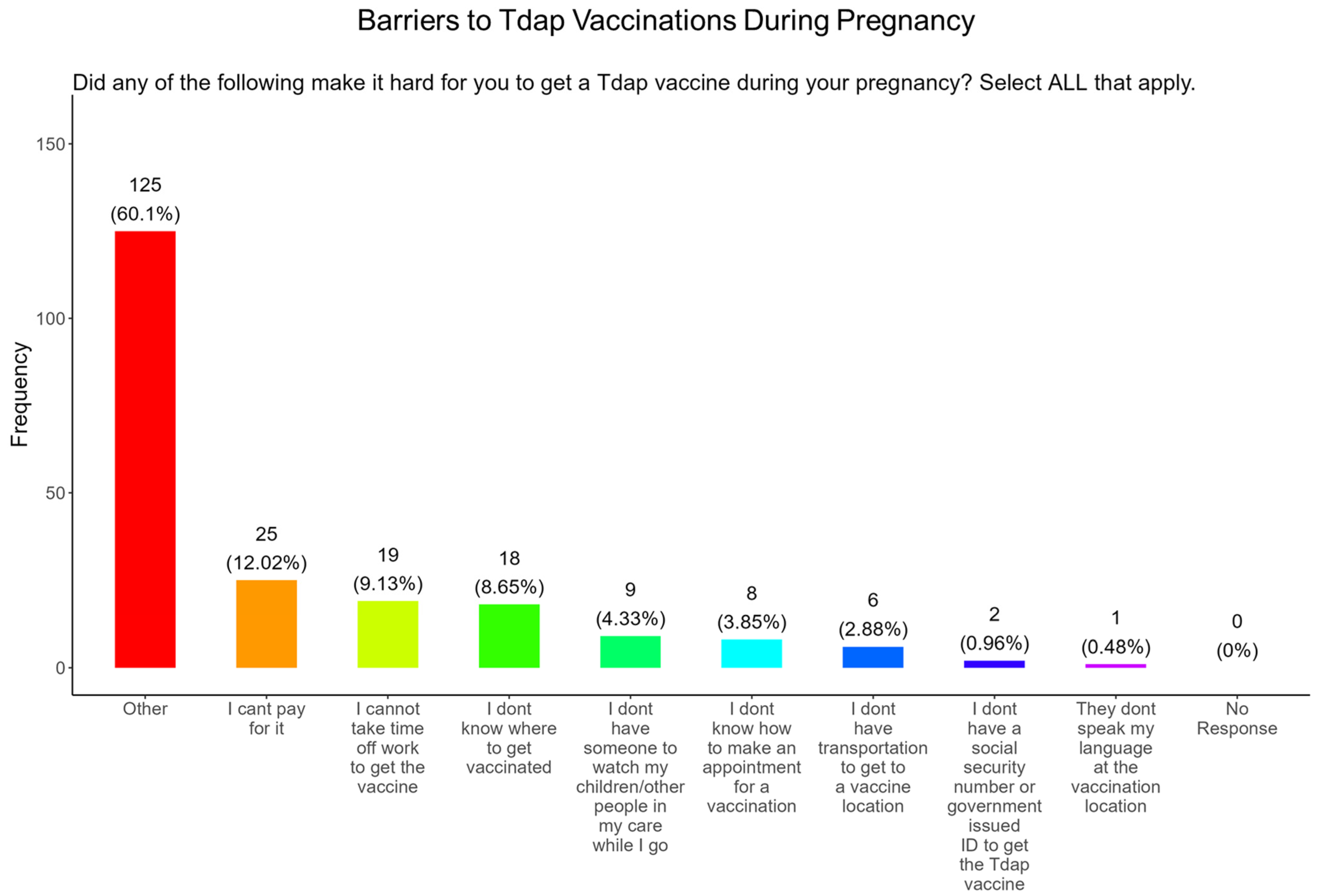
3.18. Vaccine Affordability and Time off from Work Were the Most Important Barriers to Participants Receiving a Tdap Vaccine During Pregnancy
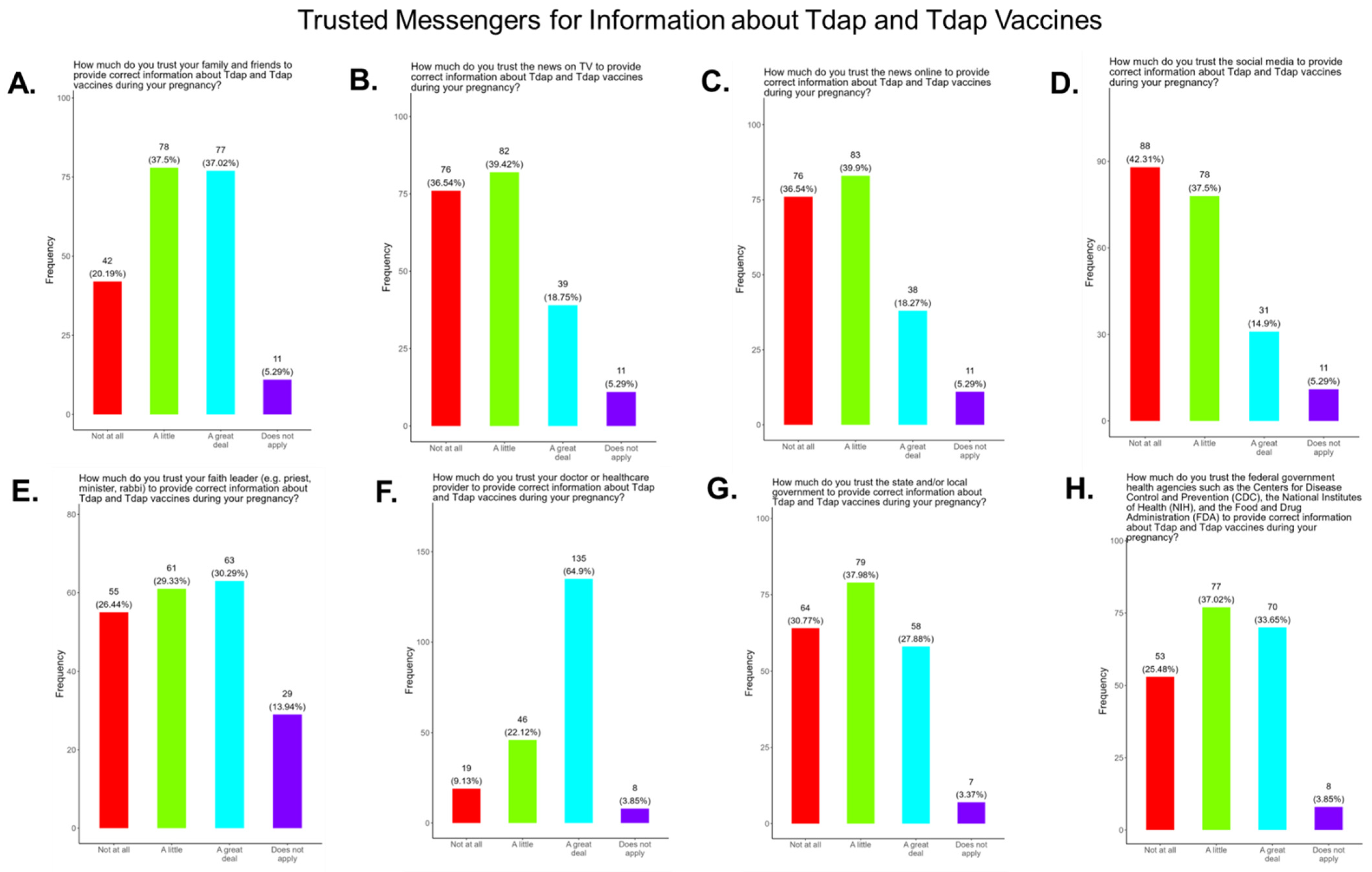
3.19. Assessing Trust in Tdap Information Sources, Primary Care Providers Were the Most Trusted Source
4. Discussion and Conclusions
5. Analysis of Study Findings with Previous Studies
6. Limitations of the Study
7. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meghani, M.; Razzaghi, H.; Kahn, K.E.; Hung, M.C.; Srivastav, A.; Lu, P.J.; Ellington, S.; Zhou, F.; Weintraub, E.; Black, C.L.; et al. Surveillance Systems for Monitoring Vaccination Coverage with Vaccines Recommended for Pregnant Women, United States. J. Women’s Health 2023, 32, 260–270. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG and SMFM Recommend COVID-19 Vaccination for Pregnant Individuals. 2021. Available online: https://www.acog.org/news/news-releases/2021/07/acog-smfm-recommend-covid-19-vaccination-for-pregnant-individuals (accessed on 30 November 2021).
- Centers for Disease Control and Prevention. COVID-19 Vaccines While Pregnant or Breastfeeding. 2021. Available online: https://stacks.cdc.gov/view/cdc/111391 (accessed on 30 November 2021).
- Lindley, M.C.; Kahn, K.E.; Bardenheier, B.H.; D’Angelo, D.V.; Dawood, F.S.; Fink, R.V.; Havers, F.; Skoff, T.H. Vital Signs: Burden and Prevention of Influenza and Pertussis Among Pregnant Women and Infants–United States. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 885–892. [Google Scholar] [CrossRef]
- Schwartz, J.L. Revised Recommendations for Covid-19 Vaccines—U.S. Vaccination Policy Under Threat. N. Engl. J. Med. 2025, 393, 417–419. [Google Scholar] [CrossRef]
- Anderer, S. Breaking from CDC, ACOG Continues Recommending COVID-19 Vaccine During Pregnancy. JAMA 2025, 334, 1131–1132. [Google Scholar] [CrossRef]
- Prasad, V.; Makary, M.A. An Evidence-Based Approach to Covid-19 Vaccination. N. Engl. J. Med. 2025, 392, 2484–2486. [Google Scholar] [CrossRef]
- Alcendor, D.J.; Matthews-Juarez, P.; Smoot, D.; Hildreth, J.E.K.; Tabatabai, M.; Wilus, D.; Brown, K.Y.; Juarez, P.D. The COVID-19 Vaccine and Pregnant Minority Women in the US: Implications for Improving Vaccine Confidence and Uptake. Vaccines 2022, 10, 2122. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Jamieson, D.J. Pregnancy, postpartum care, and COVID-19 vaccination in 2021. JAMA 2021, 325, 1099–1100. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Information about COVID-19 Vaccines for People Who Are Pregnant or Breastfeeding. 2022. Available online: https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html (accessed on 20 October 2022).
- American College of Obstetricians and Gynecologists. COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care. 2021. Available online: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care (accessed on 16 November 2022).
- Moro, P.L.; Getahun, A.; Romanson, B.; Marquez, P.; Tepper, N.K.; Olson, C.K.; Jones, J.M.; Nair, N.; Broder, K.R. Safety monitoring of Pfizer’s Respiratory Syncytial Virus Vaccine in pregnant women in the Vaccine Adverse Event Reporting System (VAERS), 2023–2024, United States. Vaccine 2025, 62, 127497. [Google Scholar] [CrossRef] [PubMed]
- Zaman, K.; Roy, E.; Arifeen, S.E.; Rahman, M.; Raqib, R.; Wilson, E.; Omer, S.B.; Shahid, N.S.; Breiman, R.F.; Steinhoff, M.C. Effectiveness of maternal influenza immunization in mothers and infants. N. Engl. J. Med. 2008, 359, 1555–1564. [Google Scholar] [CrossRef] [PubMed]
- Winter, K.; Nickell, S.; Powell, M.; Harriman, K. Effectiveness of Prenatal Versus Postpartum Tetanus, Diphtheria, and Acellular Pertussis Vaccination in Preventing Infant Pertussis. Clin. Infect. Dis. 2017, 64, 3–8. [Google Scholar] [CrossRef]
- Tapia, M.D.; Sow, S.O.; Tamboura, B.; Tégueté, I.; Pasetti, M.F.; Kodio, M.; Onwuchekwa, U.; Tennant, S.M.; Blackwelder, W.C.; Coulibaly, F.; et al. Maternal immunization with trivalent inactivated influenza vaccine for prevention of influenza in infants in Mali: A prospective, active-controlled, observer-blind, randomised phase 4 trial. Lancet Infect. Dis. 2016, 16, 1026–1035. [Google Scholar] [CrossRef]
- Laenen, J.; Roelants, M.; Devlieger, R.; Vandermeulen, C. Influenza and pertussis vaccination coverage in pregnant women. Vaccine 2015, 33, 2125–2131. [Google Scholar] [CrossRef] [PubMed]
- Etti, M.; Calvert, A.; Galiza, E.; Lim, S.; Khalil, A.; Le Doare, K.; Heath, P.T. Maternal vaccination: A review of current evidence and recommendations. Am. J. Obstet. Gynecol. 2022, 226, 459–474. [Google Scholar] [CrossRef] [PubMed]
- Shook, L.L.; Fallah, P.N.; Silberman, J.N.; Edlow, A.G. COVID-19 Vaccination in Pregnancy and Lactation: Current Research and Gaps in Understanding. Front. Cell. Infect. Microbiol. 2021, 11, 735394. [Google Scholar] [CrossRef]
- Razzaghi, H.; Kahn, K.E.; Black, C.L.; Lindley, M.C.; Jatlaoui, T.C.; Fiebelkorn, A.P.; Havers, F.P.; D’Angelo, D.V.; Cheung, A.; Ruther, N.A.; et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women—United States, April 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1391–1397. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG: COVID-19 Vaccines and Pregnancy: Conversation Guide. Available online: https://www.acog.org/programs/immunization-infectious-disease-public-health/tools-and-resources/covid-19-vaccines-and-pregnancy-conversation-guide-for-clinicians (accessed on 22 August 2025).
- CDC: COVID-19 Vaccination for Women Who Are Pregnant or Breastfeeding. Available online: https://www.cdc.gov/covid/vaccines/pregnant-or-breastfeeding.html (accessed on 10 September 2024).
- Kalafat, E.; Heath, P.; Prasad, S.; O Brien, P.; Khalil, A. COVID-19 vaccination in pregnancy. Am. J. Obstet. Gynecol. 2022, 227, 136–147. [Google Scholar] [CrossRef]
- Alcendor, D.J.; Matthews-Juarez, P.; Williams, N.; Wilus, D.; Tabatabai, M.; Hopkins, E.; George, K.; Leon, A.H.; Santiago, R.; Lee, A.; et al. COVID-19 Vaccine Hesitancy and Uptake Among Minority Populations in Tennessee. Vaccines 2023, 11, 1073. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccin. Immunother. 2013, 8, 1763–1773. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Tolbert, J.; Bell, C.; Cervantes, S.; Rakesh, S. The Uninsured Population and Health Coverage. In Health Policy 101; Altman, D., Ed.; KFF: San Francisco, CA, USA, 2025; Available online: https://www.kff.org/health-policy-101-the-uninsured-population-and-health-coverage/ (accessed on 8 October 2025).
- Tennessee Association of Health Care Journalist: Sources of Insurance Coverage KFF, Health Insurance Coverage of the Total Population. 2023. Available online: https://healthjournalism.org/wp-content/uploads/2025/01/TennesseeFor-AHCJ2024.pdf (accessed on 22 August 2025).
- Shearn, C.; Krockow, E.M. Reasons for COVID-19 vaccine hesitancy in ethnic minority groups: A systematic review and thematic synthesis of initial attitudes in qualitative research. SSM Qual. Res. Health 2023, 3, 100210. [Google Scholar] [CrossRef]
- Zimmerman, T.; Shiroma, K.; Fleischmann, K.R.; Xie, B.; Jia, C.; Verma, N.; Lee, M.K. Misinformation and COVID-19 vaccine hesitancy. Vaccine 2023, 41, 136–144. [Google Scholar] [CrossRef]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef]
- Alcendor, D.J. Targeting COVID Vaccine Hesitancy in Rural Communities in Tennessee: Implications for Extending the COVID-19 Pandemic in the South. Vaccines 2021, 9, 1279. [Google Scholar] [CrossRef]
- Van Spall, H.G.C. Exclusion of pregnant and lactating women from COVID-19 vaccine trials: A missed opportunity. Eur. Heart J. 2021, 42, 2724–2726. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, S.; Logan, R.; Marshall, C.; Kerns, J.; Diamond-Smith, N. Predictors of COVID-19 Vaccination Likelihood Among Reproductive-Aged Women in the United States. Public Health Rep. 2022, 137, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Goldshtein, I.; Steinberg, D.M.; Kuint, J.; Chodick, G.; Segal, Y.; Shapiro Ben David, S.; Ben-Tov, A. Association of BNT162b2 COVID-19 Vaccination During Pregnancy With Neonatal and Early Infant Outcomes. JAMA Pediatr. 2022, 176, 470–477. [Google Scholar] [CrossRef]
- Chaubey, I.; Vijay, H.; Govindaraj, S.; Babu, H.; Cheedarla, N.; Shankar, E.M.; Vignesh, R.; Velu, V. Impact of COVID-19 Vaccination on Pregnant Women. Pathogens 2023, 12, 431. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Sivan, M.; Perlowski, A.; Nikolich, J.Ž. Long COVID: A clinical update. Lancet 2024, 404, 707–724. [Google Scholar] [CrossRef] [PubMed]
- Georgakopoulou, V.E.; Taskou, C.; Spandidos, D.A.; Sarantaki, A. Long COVID-19 and pregnancy: A systematic review. Biomed. Rep. 2024, 22, 15. [Google Scholar] [CrossRef]
- Twanow, J.E.; McCabe, C.; Ream, M.A. The COVID-19 Pandemic and Pregnancy: Impact on Mothers and Newborns. Semin. Pediatr. Neurol. 2022, 42, 100977. [Google Scholar] [CrossRef]
- Yao, Y.; Sun, L.; Luo, J.; Qi, W.; Zuo, X.; Yang, Z. The effect of long-term COVID-19 infection on maternal and fetal complications: A retrospective cohort study conducted at a single center in China. Sci. Rep. 2024, 14, 17273. [Google Scholar] [CrossRef]
- McGovern, I.; Bogdanov, A.; Cappell, K.; Whipple, S.; Haag, M. Influenza Vaccine Uptake in the United States before and during the COVID-19 Pandemic. Vaccines 2022, 10, 1610. [Google Scholar] [CrossRef]
- Health Care.Gov: Department of Health and Human Services, Federal Poverty Level (FPL). Available online: https://www.healthcare.gov/glossary/federal-poverty-level-fpl/ (accessed on 2 September 2025).
- Metz, T.D.; Reeder, H.T.; Clifton, R.G.; Flaherman, V.; Aragon, L.V.; Baucom, L.C.; Beamon, C.J.; Braverman, A.; Brown, J.; Cao, T.; et al. Post-Acute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) After Infection During Pregnancy. Obstet. Gynecol. 2024, 144, 411–420. [Google Scholar] [CrossRef]
- Alarcón Garavito, G.A.; Gilchrist, K.; Ciurtin, C.; Khanna, S.; Chambers, P.; McNally, N.; Merivale, E.; Carr, E.; Yu, R.; Vindrola-Padros, C. Enablers and barriers of clinical trial participation in adult patients from minority ethnic groups: A systematic review. Trials 2025, 26, 65. [Google Scholar] [CrossRef] [PubMed]
- Bierer, B.E.; Meloney, L.G.; Ahmed, H.R.; White, S.A. Advancing the inclusion of underrepresented women in clinical research. Cell Rep. Med. 2022, 3, 100553. [Google Scholar] [CrossRef] [PubMed]
- Whyte, J. Racial and Ethnic Representation of Participants in US Clinical Trials of New Drugs and Biologics. JAMA 2022, 327, 985. [Google Scholar] [CrossRef]
- Searing, K.; Baukus, M.; Stark, M.A.; Morin, K.H.; Rudell, B. Needle phobia during pregnancy. J. Obstet. Gynecol. Neonatal Nurs. JOGNN 2006, 35, 592–598. [Google Scholar] [CrossRef]
- McAllister, N.; Elshtewi, M.; Badr, L.; Russell, I.F.; Lindow, S.W. Pregnancy outcomes in women with severe needle phobia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 162, 149–152. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG: The Tdap Vaccine and Pregnancy. Available online: https://www.acog.org/womens-health/faqs/the-tdap-vaccine-and-pregnancy (accessed on 15 May 2024).
- Shi, Q.; Li, J.; Hu, Q.; Cheng, C.; Yang, K.; Li, X.; Song, X.; Chen, S.; Duan, G. Efficacy, Immunogenicity, and Safety of Pertussis Vaccine During Pregnancy: A Meta-Analysis. Vaccines 2025, 13, 666. [Google Scholar] [CrossRef] [PubMed]
- Vilajeliu, A.; Goncé, A.; López, M.; Costa, J.; Rocamora, L.; Ríos, J.; Teixidó, I.; Bayas, J.M. Combined tetanus-diphtheria and pertussis vaccine during pregnancy: Transfer of maternal pertussis antibodies to the newborn. Vaccine 2015, 33, 1056–1062. [Google Scholar] [CrossRef]
- Hardy-Fairbanks, A.J.; Pan, S.J.; Decker, M.D.; Johnson, D.R.; Greenberg, D.P.; Kirkland, K.B.; Talbot, E.A.; Bernstein, H.H. Immune responses in infants whose mothers received Tdap vaccine during pregnancy. Pediatr. Infect. Dis. J. 2013, 32, 1257–1260. [Google Scholar] [CrossRef]
- Lindsey, B.; Kampmann, B.; Jones, C. Maternal immunization as a strategy to decrease susceptibility to infection in newborn infants. Curr. Opin. Infect. Dis. 2013, 26, 248–253. [Google Scholar] [CrossRef]
- Munoz, F.M.; Jamieson, D.J. Maternal Immunization. Obstet. Gynecol. 2019, 133, 739–753. [Google Scholar] [CrossRef]
- Dancewicz, H.; Kwiatkowska, A.; Gebarowska, J.; Bienkowski, C.; Pokorska-Spiewak, M. The attitudes of pregnant or breastfeeding polish women towards COVID-19 vaccinations: A cross-sectional survey study. Ginekol. Pol. 2025, 96, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Mierzwa, G.; Jurga, J.; Kuciel, J.; Kolak, M.; Jaworowski, A.; Huras, H. Pregnant women’s knowledge of and attitudes toward pertussis, influenza and COVID-19 vaccination. Ginekol. Pol. 2025, 96, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Cubizolles, C.; Barjat, T.; Chauleur, C.; Bruel, S.; Botelho-Nevers, E.; Gagneux-Brunon, A. Evaluation of intentions to get vaccinated against influenza, COVID 19, pertussis and to get a future vaccine against respiratory syncytial virus in pregnant women. Vaccine 2023, 41, 7342–7347. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.T.; Bae, Y.; Birkett, R.; Sharma, A.M.; Zhang, R.; Fisch, K.M.; Funk, W.; Mestan, K.K. Cord Blood Adductomics Reveals Oxidative Stress Exposure Pathways of Bronchopulmonary Dysplasia. Antioxidants 2024, 13, 494. [Google Scholar] [CrossRef] [PubMed]
- Funk, W.E.; Montgomery, N.; Bae, Y.; Chen, J.; Chow, T.; Martinez, M.P.; Lurmann, F.; Eckel, S.P.; McConnell, R.; Xiang, A.H. Human Serum Albumin Cys34 Adducts in Newborn Dried Blood Spots: Associations with Air Pollution Exposure During Pregnancy. Front. Public Health 2021, 9, 730369. [Google Scholar] [CrossRef]
- Mestan, K.; Gotteiner, N.; Porta, N.; Grobman, W.; Su, E.J.; Ernst, L.M. Cord Blood Biomarkers of Placental Maternal Vascular Underperfusion Predict Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension. J. Pediatr. 2017, 185, 33–41. [Google Scholar] [CrossRef]
- Voller, S.B.; Chock, S.; Ernst, L.M.; Su, E.; Liu, X.; Farrow, K.N.; Mestan, K.K. Cord blood biomarkers of vascular endothelial growth (VEGF and sFlt-1) and postnatal growth: A preterm birth cohort study. Early Hum. Dev. 2014, 90, 195–200. [Google Scholar] [CrossRef]
- Afrose, D.; Alfonso-Sánchez, S.; McClements, L. Targeting oxidative stress in preeclampsia. Hypertens. Pregnancy 2025, 44, 2445556. [Google Scholar] [CrossRef]
- Brooker, I.A.; Fisher, J.J.; Sutherland, J.M.; Pringle, K.G. Understanding the impact of placental oxidative and nitrative stress in pregnancies complicated by fetal growth restriction. Placenta 2024, 158, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Zhao, Y.; Chen, W.; Niu, Y.; Wang, D.; Jin, Z. Hierarchical metal exposure in umbilical cord blood in relation to oxidative stress and AMPK/NF-κB signaling in preterm membrane rupture. Sci. Rep. 2025, 15, 26434. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Shen, J.; Fang, R.; Huang, H.; Lai, Y.; Hu, Y.; Zheng, J. The impact of environmental and dietary exposure on gestational diabetes mellitus: A comprehensive review emphasizing the role of oxidative stress. Front. Endocrinol. 2025, 16, 1393883. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Gao, J.; Yang, L.; Feng, X.; Yuan, X. Oxidative stress and its role in recurrent pregnancy loss: Mechanisms and implications. J. Mol. Histol. 2024, 56, 55. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harvey, A.; Tabatabai, M.; Wilus, D.; Thomas, S.; Hildreth, J.E.K.; Alcendor, D.J. Vaccinations for Expecting Mothers to Improve Pregnancy Care in Middle Tennessee. Pathogens 2025, 14, 1255. https://doi.org/10.3390/pathogens14121255
Harvey A, Tabatabai M, Wilus D, Thomas S, Hildreth JEK, Alcendor DJ. Vaccinations for Expecting Mothers to Improve Pregnancy Care in Middle Tennessee. Pathogens. 2025; 14(12):1255. https://doi.org/10.3390/pathogens14121255
Chicago/Turabian StyleHarvey, Alphonso, Mohammad Tabatabai, Derek Wilus, Sofia Thomas, James E. K. Hildreth, and Donald J. Alcendor. 2025. "Vaccinations for Expecting Mothers to Improve Pregnancy Care in Middle Tennessee" Pathogens 14, no. 12: 1255. https://doi.org/10.3390/pathogens14121255
APA StyleHarvey, A., Tabatabai, M., Wilus, D., Thomas, S., Hildreth, J. E. K., & Alcendor, D. J. (2025). Vaccinations for Expecting Mothers to Improve Pregnancy Care in Middle Tennessee. Pathogens, 14(12), 1255. https://doi.org/10.3390/pathogens14121255







