Early Detection and Identification of Methylobacterium radiotolerans Bacteremia in an Early T-Cell Precursor Acute Lymphoblastic Leukemia Patient: A Rare Infection and Literature Review
Abstract
1. Introduction
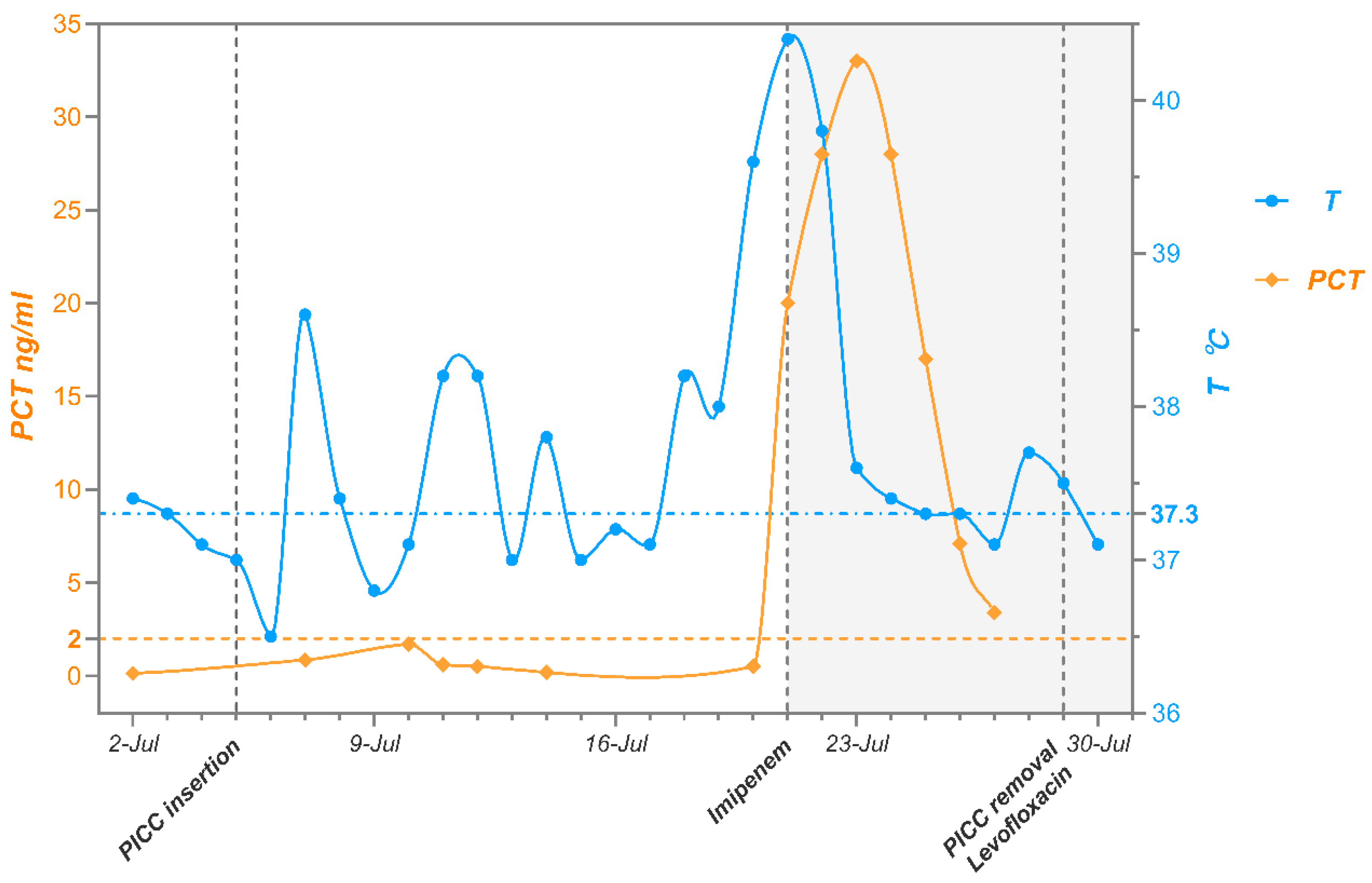
2. Case Description
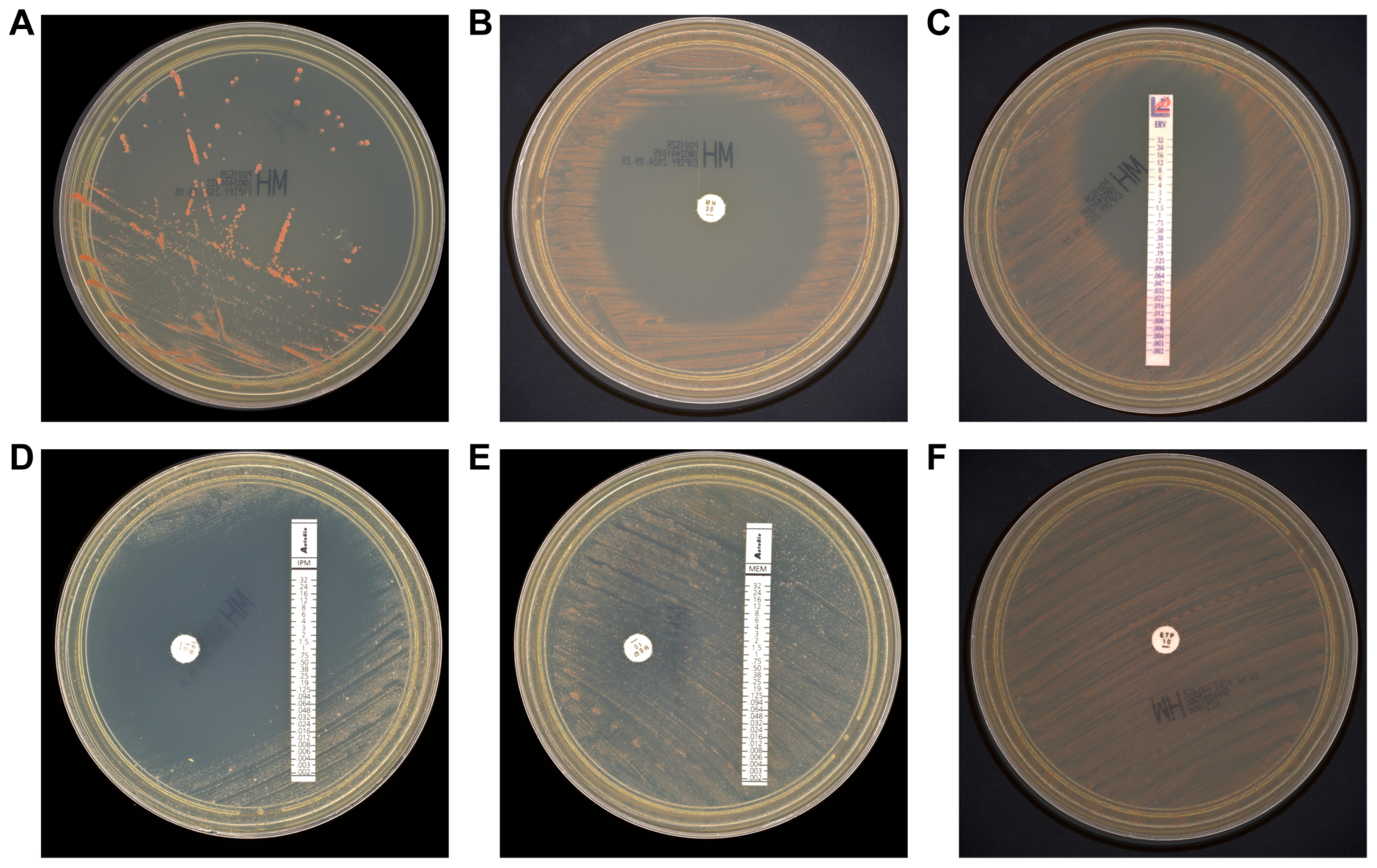
3. Additional Microbiological Studies
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| M. radiotolerans | Methylobacterium radiotolerans |
| ETP-ALL | Early T-cell precursor acute lymphoblastic leukemia |
| E-test | Epsilometer test |
| BK | Bauer-Kirby disk diffusion |
| PCT | Procalcitonin |
| PICC | Peripherally inserted central catheter |
| MALDI-TOF MS | Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry |
| AST | Antibiotic susceptibility testing |
| MH | Mueller-Hinton |
| CLSI | Clinical and Laboratory Standards Institute |
References
- Holt, J.G.; Krieg, N.R.; Sneath, P.H.A.; Staley, J.T.; Williams, S.T. Bergey’s Manual of Determinative Bacteriology, 9th ed.; Williams & Wilkins: Baltimore, MD, USA, 1994. [Google Scholar]
- Santos, M.I.S.; Brandao, E.; Santos, E.; Batista, M.V.A.; Estevam, C.S.; Alexandre, M.R.; Fernandes, M.F. Pendimethalin biodegradation by soil strains of Burkholderia sp. and Methylobacterium radiotolerans. Acad. Bras. Cienc. 2021, 93, e20210924. [Google Scholar] [CrossRef] [PubMed]
- Furuhata, K.; Kato, Y.; Goto, K.; Hara, M.; Yoshida, S.; Fukuyama, M. Isolation and identification of species from the tap water in hospitals in Japan and their antibiotic susceptibility. Microbiol. Immunol. 2006, 50, 11–17. [Google Scholar] [CrossRef] [PubMed]
- de Cal, M.; Cazzavillan, S.; Cruz, D.; Nalesso, F.; Brendolan, A.; Rassu, M.; Ronco, C. Methylobacterium radiotolerans bacteremia in hemodialysis patients. G. Ital. Nefrol. 2009, 26, 616–620. [Google Scholar] [PubMed]
- Li, L.; Tarrand, J.J.; Han, X.Y. Microbiological and clinical features of four cases of catheter-related infection by Methylobacterium radiotolerans. J. Clin. Microbiol. 2015, 53, 1375–1379. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, M.; Tominaga, Y.; Sakamoto, K.; Shikata, H. Hemodialysis vascular access infection caused by Methylobacterium radiotolerans: The first confirmed case in Japan. J. Infect. Chemother. 2020, 26, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Kovaleva, J.; Degener, J.E.; van der Mei, H.C. Methylobacterium and its role in health care-associated infection. J. Clin. Microbiol. 2014, 52, 1317–1321. [Google Scholar] [CrossRef] [PubMed]
- Cordovana, M.; Deni, A.; Kostrzewa, M.; Abdalla, M.; Ambretti, S. First report of Methylobacterium radiotolerans bacteraemia identified by MALDI-TOF mass spectrometry. New Microbes New Infect. 2019, 30, 100546. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Qi, X.; Ma, B.; Xu, P.; Yuan, Y. First case of infective endocarditis caused by Methylobacterium radiotolerans. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 1785–1788. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Desai, A.; Desai, K. A Case Report of Methylobacterium radiotolerans Bacteremia and Brain Abscesses. Infect. Microbes Dis. 2021, 3, 112–114. [Google Scholar] [CrossRef]
- Aydemir, O.; Ormanoglu, G.; Koroglu, M.; Aydemir, Y. Comparison of time-to-detection of Mindray TDR and BacT/ALERT(R)3D blood culture systems using simulated blood cultures. Acta Clin. Belg. 2024, 79, 168–173. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 15.0. 2025. Available online: https://www.eucast.org (accessed on 1 January 2025).
- Photolo, M.M.; Mavumengwana, V.; Sitole, L.; Tlou, M.G. Antimicrobial and Antioxidant Properties of a Bacterial Endophyte, Methylobacterium radiotolerans MAMP 4754, Isolated from Combretum erythrophyllum Seeds. Int. J. Microbiol. 2020, 2020, 9483670. [Google Scholar] [CrossRef]
- Lai, C.-C.; Cheng, A.; Liu, W.-L.; Tan, C.-K.; Huang, Y.-T.; Chung, K.-P.; Lee, M.-R.; Hsueh, P.-R. Infections caused by unusual Methylobacterium species. J. Clin. Microbiol. 2011, 49, 3329–3331. [Google Scholar] [CrossRef] [PubMed]
- Rit, K.; Chakraborty, B.; Mukherjee, T.; Chakrabarty, P.S.; Consultant, C.; Jo, D. A Case Report of Methylobacterium Radiotolerans Bacteremia in a Haemodialysis Patient Successfully Treated by Combination Therapy of Levofloxacin and Meropenem. World J. Pharm. Pharm. Sci. 2015, 4, 1369–1372. [Google Scholar]
- Huang, K.; Dai, M.; Li, Q.; Liu, N.; Lin, D.; Wang, Q.; Zhou, X.; Wang, Z.; Gao, Y.; Jin, H.; et al. Early T-Cell Precursor Leukemia Has a Higher Risk of Induction-Related Infection among T-Cell Acute Lymphoblastic Leukemia in Adult. Mediat. Inflamm. 2020, 2020, 8867760. [Google Scholar] [CrossRef] [PubMed]
- Forconi, F.; Moss, P. Perturbation of the normal immune system in patients with CLL. Blood 2015, 126, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Ray-Coquard, I.; Borg, C.; Bachelot, T.; Sebban, C.; Philip, I.; Clapisson, G.; Le Cesne, A.; Biron, P.; Chauvin, F.; Blay, J.Y.; et al. Baseline and early lymphopenia predict for the risk of febrile neutropenia after chemotherapy. Br. J. Cancer 2003, 88, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Patt, T.E.; Cole, G.C.; Hanson, R.S. Methylobacterium, a New Genus of Facultatively Methylotrophic Bacteria. Int. J. Syst. Bacteriol. 1976, 26, 226–229. [Google Scholar] [CrossRef]

| Category | Time Period | Reference Values | ||
|---|---|---|---|---|
| Pre-Hospitalization | Intra-Hospitalization | Post-Hospitalization | ||
| RBC, ×1012/L | 3.44 | 1.56 | 2.38 | 4.00–5.50 |
| HB, g/L | 106 | 50 | 73 | 120–160 |
| WBC, ×109/L | 98.03 | 0.28 | 5.70 | 3.50–9.50 |
| N (%) | 0 | 14.3 | 79.6 | 50.0–75.0 |
| LYM (%) | 6 | 82.1 | 7.9 | 20.0–40.0 |
| Blast (%) | 94 | - | - | - |
| PLT, ×109/L | 36 | 10 | 105 | 100–350 |
| LDH, U/L | 467 | 90 | 139 | 0–250 |
| hsCRP, mg/L | 29.70 | 311.65 | 36.19 | <3.0 |
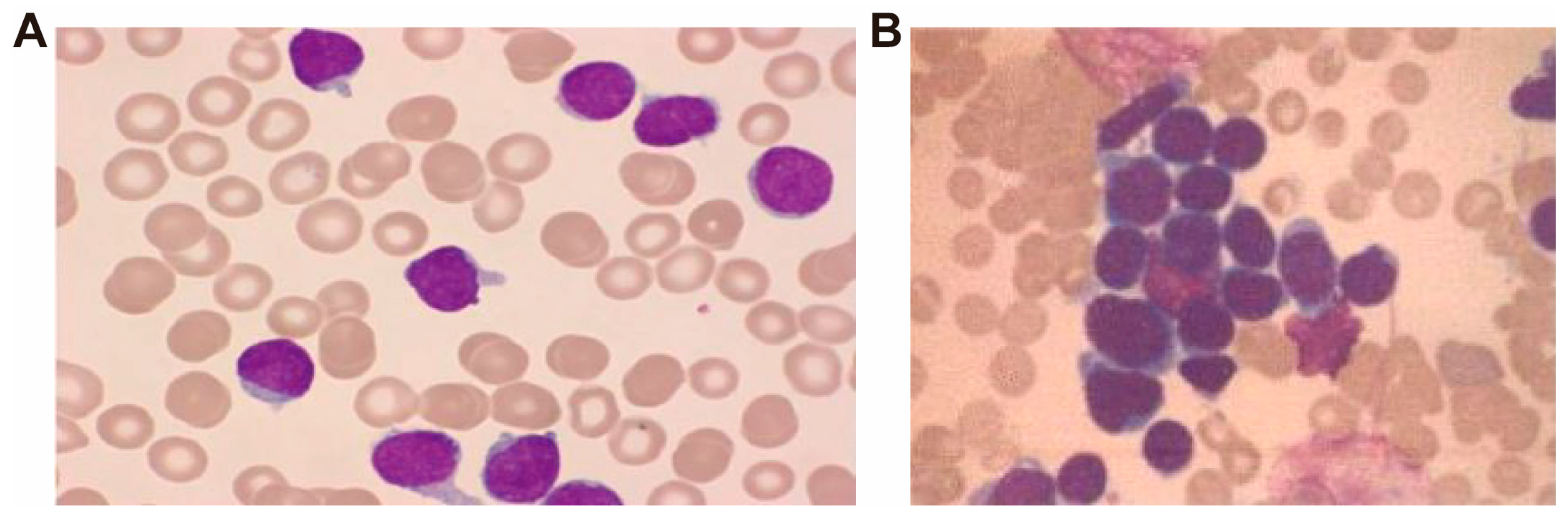
| Bone marrow flow cytometry | Abundant early abnormal T lymphocytes. | - | - | - |
| Bone marrow smear | Hypercellular proliferation, predominantly composed of prolymphoblasts (96.5%). | - | Adequate cellularity with granulocytic predominance (85%) and a relative increase in segmented neutrophils. | - |
| Class | Antibiotic | Inhibition Zone Diameter (Disc-Diffusion) (mm) | MIC (mg/mL) |
|---|---|---|---|
| Carbapenem | Imipenem | 40 | 0.75 |
| Meropenem | 6 | >=32 | |
| Ertapenem | 6 | - | |
| Aminoglycosides | Gentamicin | 31 | - |
| Amikacin | - | 1.5 | |
| 4-quinolones | Levofloxacin | 27 | 0.5 |
| Ciprofloxacin | - | 2 | |
| Tetracyclines | Minocycline | 43 | - |
| Tigecycline | 26 | - | |
| Eravacycline | - | 0.125 | |
| Cephalosporins | Ceftriaxone | - | 3 |
| Cefoxitin | 6 | - | |
| Glycopeptides | Vancomycin | 6 | - |
| Monobactams | Aztreonam | 6 | - |
| Year, [Reference] | Underlying Disease(s) | Catheter-Related | Source(s) of Isolated Bacteria | Identification Method(s) | Antibiotic Susceptibility | Therapy | Outcome |
|---|---|---|---|---|---|---|---|
| 2009 [4] | Acute/chronic renal failure | CVC | 37 patients, from blood (2.7%) or CVC (29.7%) or both (67.6%) | 16S rRNA sequencing | - | Removal and replacement of CVCs and antibiotic therapy. | Improved |
| 2011 [14] | Dilated cardiomyopathy, end-stage renal disease | DLC | Blood from DLC | 16S rRNA sequencing | Resistant to aztreonam, ceftazidime, cefepime, and piperacillin-tazobactam. | Removal of DLC, cefepime and ciprofloxacin | Improved |
| Leukemia, febrile neutropenia | CVC | Blood from CVC | Removal of CVC, ciprofloxacin and gentamicin | ||||
| 2015 [5] | AML | PICC | Blood from PICC | 16S rRNA sequencing | - | Levofloxacin | Improved |
| AML | PICC | Blood from PICC | Clindamycin, levofloxacin and cefepime | ||||
| AML | PICC | Blood from PICC | Levofloxacin and linezolid | ||||
| ALL, GVHD | CVC | Blood from CVC | Ciprofloxacin and piperacillin-tazobactam | ||||
| 2015 [15] | End-stage renal failure, COPD | CVC | Blood | 16S rRNA sequencing | Susceptible to amikacin, netilmicin, gentamicin, levofloxacin, piperacillin-tazobactam and meropenem. | Removal and replacement of CVC, levofloxacin and meropenem. | Improved |
| 2019 [8] | End-stage renal failure | CVC | Peripheral blood and CVC | MALDI-TOF MS, 16S rRNA sequencing | Susceptible to gentamycin, levofloxacin, rifampicin and imipenem. | Not known | Improved |
| 2019 [6] | Peripheral T-cell lymphoma, sick sinus syndrome | Hemodialysis vascular access | Peripheral blood and the vascular access line blood | MALDI-TOF MS, 16S rRNA sequencing | Susceptible to imipenem, amikacin, tobramycin and levofloxacin. | Removal and replacement of the vascular access line, meropenem and rifampicin for 14 days, and oral levofloxacin and rifampicin subsequently for 8 weeks. | Improved |
| 2020 [9] | After spinal cord surgery | None | Valvar (aortic and mitral valves) vegetation tissue homogenate | MALDI-TOF MS, 16S rRNA sequencing | Susceptible to aminoglycosides and ciprofloxacin. | Tigecycline and vancomycin | Improved |
| 2021 [10] | COPD | None | Brain lesion | MALDI-TOF MS | - | Levofloxacin | Improved |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiao, J.; Liu, L.; Qin, X.; Xu, Y. Early Detection and Identification of Methylobacterium radiotolerans Bacteremia in an Early T-Cell Precursor Acute Lymphoblastic Leukemia Patient: A Rare Infection and Literature Review. Pathogens 2025, 14, 1015. https://doi.org/10.3390/pathogens14101015
Xiao J, Liu L, Qin X, Xu Y. Early Detection and Identification of Methylobacterium radiotolerans Bacteremia in an Early T-Cell Precursor Acute Lymphoblastic Leukemia Patient: A Rare Infection and Literature Review. Pathogens. 2025; 14(10):1015. https://doi.org/10.3390/pathogens14101015
Chicago/Turabian StyleXiao, Jiayu, Lingli Liu, Xuzhen Qin, and Yingchun Xu. 2025. "Early Detection and Identification of Methylobacterium radiotolerans Bacteremia in an Early T-Cell Precursor Acute Lymphoblastic Leukemia Patient: A Rare Infection and Literature Review" Pathogens 14, no. 10: 1015. https://doi.org/10.3390/pathogens14101015
APA StyleXiao, J., Liu, L., Qin, X., & Xu, Y. (2025). Early Detection and Identification of Methylobacterium radiotolerans Bacteremia in an Early T-Cell Precursor Acute Lymphoblastic Leukemia Patient: A Rare Infection and Literature Review. Pathogens, 14(10), 1015. https://doi.org/10.3390/pathogens14101015






