The Role of Microorganisms in the Development of Breast Implant-Associated Anaplastic Large Cell Lymphoma
Abstract
1. Introduction
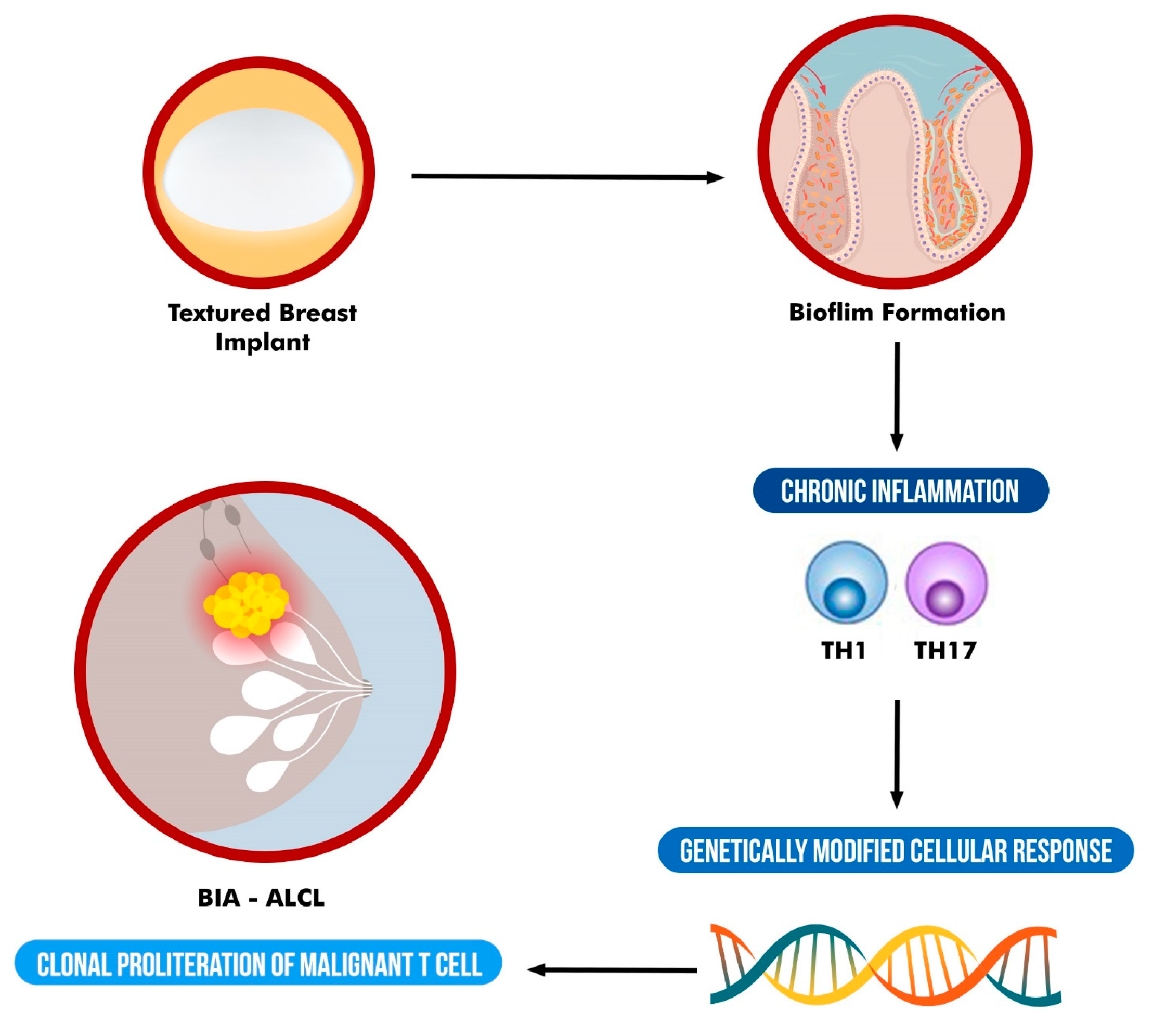
2. Textured Surface Implants and BIA-ALCL
3. Role of Bacterial Biofilm and Chronic Inflammation in BIA-ALCL
4. Genetics and BIA-ALCL
5. Implications for Clinical Practice
5.1. Clinical Presentation
5.2. Investigation
5.3. Treatment
5.4. Outcomes in BIA-ALCL
5.5. The Role of Antiseptic Solutions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DeCoster, R.C.; Clemens, M.W.; Di Napoli, A.; Lynch, E.B.; Bonaroti, A.R.; Rinker, B.D.; Butterfield, T.A.; Vasconez, H.C. Cellular and Molecular Mechanisms of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2021, 147, 30e–41e. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Q.; Tan, Y.; Lv, W.; Zhao, C.; Xiong, M.; Hou, K.; Wu, M.; Ren, Y.; Zeng, N.; et al. Current Progress in Breast Implant-Associated Anaplastic Large Cell Lymphoma. Front. Oncol. 2021, 11, 785887. [Google Scholar] [CrossRef]
- Leberfinger, A.N.; Behar, B.J.; Williams, N.C.; Rakszawski, K.L.; Potochny, J.D.; Mackay, D.R.; Ravnic, D.J. Breast Implant-Associated Anaplastic Large Cell Lymphoma: A Systematic Review. JAMA Surg. 2017, 152, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Srinivasa, D.R.; Miranda, R.N.; Kaura, A.; Francis, A.M.; Campanale, A.; Boldrini, R.; Alexander, J.; Deva, A.K.; Gravina, P.R.; Medeiros, L.J.; et al. Global Adverse Event Reports of Breast Implant-Associated ALCL: An International Review of 40 Government Authority Databases. Plast Reconstr. Surg. 2017, 139, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, P.; Riordan, E.; Moon, D.; Deva, A.K. Theories of Etiopathogenesis of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2019, 143, 23S–29S. [Google Scholar] [CrossRef]
- Clemens, M.W.; Medeiros, L.J.; Butler, C.E.; Hunt, K.K.; Fanale, M.A.; Horwitz, S.; Weisenburger, D.D.; Liu, J.; Morgan, E.A.; Kanagal-Shamanna, R.; et al. Complete Surgical Excision Is Essential for the Management of Patients With Breast Implant-Associated Anaplastic Large-Cell Lymphoma. J. Clin. Oncol. 2016, 34, 160–168. [Google Scholar] [CrossRef]
- Clemens, M.W.; Brody, G.S.; Mahabir, R.C.; Miranda, R.N. How to Diagnose and Treat Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2018, 141, 586e–599e. [Google Scholar] [CrossRef] [PubMed]
- Keech, J.A.; Creech, B.J. Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant. Plast. Reconstr. Surg. 1997, 100, 554–555. [Google Scholar] [CrossRef]
- Available online: https://www.fda.gov/news-events/press-announcements/fda-updates-analysis-medical-device-reports-breast-implant-illness-and-breast-implant-associated (accessed on 10 November 2022).
- Doren, E.L.; Miranda, R.N.; Selber, J.C.; Garvey, P.B.; Liu, J.; Medeiros, L.J.; Butler, C.E.; Clemens, M.W. U.S. Epidemiology of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2017, 139, 1042–1050. [Google Scholar] [CrossRef]
- Cordeiro, P.G.; Ghione, P.; Ni, A.; Hu, Q.; Ganesan, N.; Galasso, N.; Dogan, A.; Horwitz, S.M. Risk of breast implant associated anaplastic large cell lymphoma (BIA-ALCL) in a cohort of 3546 women prospectively followed long term after reconstruction with textured breast implants. J. Plast. Reconstr. Aesthet. Surg. 2020, 73, 841–846. [Google Scholar] [CrossRef]
- Collett, D.J.; Rakhorst, H.; Lennox, P.; Magnusson, M.; Cooter, R.; Deva, A.K. Current Risk Estimate of Breast Implant-Associated Anaplastic Large Cell Lymphoma in Textured Breast Implants. Plast. Reconstr. Surg. 2019, 143, 30S–40S. [Google Scholar] [CrossRef]
- de Boer, M.; van Leeuwen, F.E.; Hauptmann, M.; Overbeek, L.I.; de Boer, J.P.; Hijmering, N.J.; Sernee, A.; Klazen, C.A.; Lobbes, M.B.; van der Hulst, R.R.; et al. Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast. JAMA Oncol. 2018, 4, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Health C for D and R. Questions and Answers about Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). Available online: https://www.fda.gov/medical-devices/breast-implants/questions-and-answers-about-breast-implant-associated-anaplastic-large-cell-lymphoma-bia-alcl (accessed on 10 November 2022).
- Azzi, A.J.; Almadani, Y.; Davison, P. A National Survey to Assess the Population’s Perception of Breast Implant-Associated Anaplastic Large Cell Lymphoma and Breast Implant Illness. Plast. Reconstr. Surg. 2021, 147, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Santanelli di Pompeo, F.; Clemens, M.W.; Atlan, M.; Botti, G.; Cordeiro, P.G.; De Jong, D.; Di Napoli, A.; Hammond, D.; Haymaker, C.L.; Horwitz, S.M.; et al. 2022 Practice Recommendation Updates from the World Consensus Conference on BIA-ALCL. Aesthet. Surg. J. 2022, 42, 1262–1278. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.N.; Hanson, B.M.; Pinkner, C.L.; Simar, S.R.; Pinkner, J.S.; Parikh, R.; Clemens, M.W.; Hultgren, S.J.; Myckatyn, T.M. Insights into the Microbiome of Breast Implants and Periprosthetic Tissue in Breast Implant-Associated Anaplastic Large Cell Lymphoma. Sci. Rep. 2019, 9, 10393. [Google Scholar] [CrossRef]
- Laurent, C.; Haioun, C.; Brousset, P.; Gaulard, P. New insights into breast implant-associated anaplastic large cell lymphoma. Curr. Opin. Oncol. 2018, 30, 292–300. [Google Scholar] [CrossRef]
- Kadin, M.E.; Morgan, J.; Xu, H.; Epstein, A.L.; Sieber, D.; Hubbard, B.A.; Adams, W.P., Jr.; Bacchi, C.E.; Goes, J.C.; Clemens, M.W.; et al. IL-13 is produced by tumor cells in breast implant-associated anaplastic large cell lymphoma: Implications for pathogenesis. Hum. Pathol. 2018, 78, 54–62. [Google Scholar] [CrossRef]
- Hu, H.; Johani, K.; Almatroudi, A.; Vickery, K.; Van Natta, B.; Kadin, M.E.; Brody, G.; Clemens, M.; Cheah, C.Y.; Lade, S.; et al. Bacterial Biofilm Infection Detected in Breast Implant-Associated Anaplastic Large-Cell Lymphoma. Plast. Reconstr. Surg. 2016, 137, 1659–1669. [Google Scholar] [CrossRef]
- Ashley, F.L. Further studies on the natural-Y breast prosthesis. Plast. Reconstr. Surg. 1972, 49, 414–419. [Google Scholar] [CrossRef]
- Kaoutzanis, C.; Winocour, J.; Unger, J.; Gabriel, A.; Maxwell, G.P. The Evolution of Breast Implants. Semin. Plast. Surg. 2019, 33, 217–223. [Google Scholar] [CrossRef]
- Liu, X.; Zhou, L.; Pan, F.; Gao, Y.; Yuan, X.; Fan, D. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: A cumulative meta-analysis. PLoS ONE 2015, 10, e0116071. [Google Scholar] [CrossRef] [PubMed]
- Lista, F.; Austin, R.E.; Saheb-Al-Zamani, M.; Ahmad, J. Does Implant Surface Texture Affect the Risk of Capsular Contracture in Subglandular Breast Augmentation and Breast Augmentation-Mastopexy? Aesthet. Surg. J. 2020, 40, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Safran, T.; Nepon, H.; Chu, C.K.; Winocour, S.; Murphy, A.M.; Davison, P.G.; Dionisopolos, T.; Vorstenbosch, J. Current Concepts in Capsular Contracture: Pathophysiology, Prevention, and Management. Semin. Plast. Surg. 2021, 35, 189–197. [Google Scholar] [CrossRef]
- Ajdic, D.; Zoghbi, Y.; Gerth, D.; Panthaki, Z.J.; Thaller, S. The Relationship of Bacterial Biofilms and Capsular Contracture in Breast Implants. Aesthet. Surg. J. 2016, 36, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Lajevardi, S.S.; Rastogi, P.; Isacson, D.; Deva, A.K. What are the likely causes of breast implant associated anaplastic large cell lymphoma (BIA-ALCL)? JPRAS Open 2022, 32, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Pajkos, A.; Deva, A.K.; Vickery, K.; Cope, C.; Chang, L.; Cossart, Y.E. Detection of subclinical infection in significant breast implant capsules. Plast. Reconstr. Surg. 2003, 111, 1605–1611. [Google Scholar] [CrossRef] [PubMed]
- Rieger, U.M.; Mesina, J.; Kalbermatten, D.F.; Haug, M.; Frey, H.P.; Pico, R.; Frei, R.; Pierer, G.; Lüscher, N.J.; Trampuz, A. Bacterial biofilms and capsular contracture in patients with breast implants. Br. J. Surg. 2013, 100, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.N.; Heiman, A.J.; Patel, A. Implants and Breast Pocket Irrigation: Outcomes of Antibiotic, Antiseptic, and Saline Irrigation. Aesthet. Surg. J. 2022, 42, NP102–NP111. [Google Scholar] [CrossRef] [PubMed]
- Yalanis, G.C.; Liu, E.W.; Cheng, H.T. Efficacy and Safety of Povidone-Iodine Irrigation in Reducing the Risk of Capsular Contracture in Aesthetic Breast Augmentation: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2015, 136, 687–698. [Google Scholar] [CrossRef] [PubMed]
- De Jong, W.H.; Panagiotakos, D.; Proykova, A.; Samaras, T.; Clemens, M.W.; De Jong, D.; Hopper, I.; Rakhorst, H.A.; di Pompeo, F.S.; Turner, S.D.; et al. Final opinion on the safety of breast implants in relation to anaplastic large cell lymphoma: Report of the scientific committee on health, emerging and environmental risks (SCHEER). Regul. Toxicol. Pharmacol. 2021, 125, 104982. [Google Scholar] [CrossRef] [PubMed]
- Naga, H.I.; Mellia, J.A.; Basta, M.N.; Morris, M.P.; Christopher, A.N.; Campbell, F.M.; Sommers, K.; Levinson, H.; Nelson, J.A.; Fischer, J.P. Breast Implant-Associated Anaplastic Large-Cell Lymphoma: Updated Systematic Review and Analysis of Treatment Strategies. Plast. Reconstr. Surg. 2022, 150, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Asaad, M.; Offodile, A.C.; Di Pompeo, F.S.; Bevers, T.B.; Stelly, S.; Carew, L.A.; Barnea, Y.; Miranda, R.N.; Butler, C.E.; Clemens, M.W. Management of Symptomatic Patients with Textured Implants. Plast. Reconstr. Surg. 2021, 147, 58S–68S. [Google Scholar] [CrossRef]
- Munhoz, A.M.; Clemens, M.W.; Nahabedian, M.Y. Breast Implant Surfaces and Their Impact on Current Practices: Where We Are Now and Where Are We Going? Plast. Reconstr. Surg. Glob. Open 2019, 7, e2466. [Google Scholar] [CrossRef] [PubMed]
- Loch-Wilkinson, A.; Beath, K.J.; Knight, R.J.W.; Wessels, W.L.F.; Magnusson, M.; Papadopoulos, T.; Connell, T.; Lofts, J.; Locke, M.; Hopper, I.; et al. Breast Implant-Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk. Plast. Reconstr. Surg. 2017, 140, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Valencia-Lazcano, A.A.; Alonso-Rasgado, T.; Bayat, A. Characterisation of breast implant surfaces and correlation with fibroblast adhesion. J. Mech. Behav. Biomed. Mater. 2013, 21, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.A.; Dabic, S.; Mehrara, B.J.; Cordeiro, P.G.; Disa, J.J.; Pusic, A.L.; Matros, E.; Dayan, J.H.; Allen, R.J., Jr.; Coriddi, M.; et al. Breast Implant-associated Anaplastic Large Cell Lymphoma Incidence: Determining an Accurate Risk. Ann. Surg. 2020, 272, 403–409. [Google Scholar] [CrossRef]
- Nelson, J.A.; McCarthy, C.; Dabic, S.; Polanco, T.; Chilov, M.; Mehrara, B.J.; Disa, J.J. BIA-ALCL and Textured Breast Implants: A Systematic Review of Evidence Supporting Surgical Risk Management Strategies. Plast. Reconstr. Surg. 2021, 147, 7S–13S. [Google Scholar] [CrossRef]
- Doloff, J.C.; Veiseh, O.; de Mezerville, R.; Sforza, M.; Perry, T.A.; Haupt, J.; Jamiel, M.; Chambers, C.; Nash, A.; Aghlara-Fotovat, S.; et al. The surface topography of silicone breast implants mediates the foreign body response in mice, rabbits and humans. Nat. Biomed. Eng. 2021, 5, 1115–1130. [Google Scholar] [CrossRef]
- Caldara, M.; Belgiovine, C.; Secchi, E.; Rusconi, R. Environmental, Microbiological, and Immunological Features of Bacterial Biofilms Associated with Implanted Medical Devices. Clin. Microbiol. Rev. 2022, 35, e0022120. [Google Scholar] [CrossRef] [PubMed]
- Le, K.Y.; Park, M.D.; Otto, M. Immune Evasion Mechanisms of Staphylococcus epidermidis Biofilm Infection. Front. Microbiol. 2018, 9, 359. [Google Scholar] [CrossRef]
- Jacombs, A.; Tahir, S.; Hu, H.; Deva, A.K.; Almatroudi, A.; Wessels, W.L.F.; Bradshaw, D.A.; Vickery, K. In vitro and in vivo investigation of the influence of implant surface on the formation of bacterial biofilm in mammary implants. Plast. Reconstr. Surg. 2014, 133, 471e–480e. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Ryu, J.Y.; Lee, J.S.; Choi, K.Y.; Chung, H.Y.; Cho, B.C.; Kim, K.; Lee, Y.J.; Jin, H.K.; Bae, J.S.; et al. Effect of Breast Silicone Implant Topography on Bacterial Attachment and Growth: An In Vitro Study. In Vivo 2022, 36, 1703–1709. [Google Scholar] [CrossRef] [PubMed]
- James, G.A.; Boegli, L.; Hancock, J.; Bowersock, L.; Parker, A.; Kinney, B.M. Bacterial Adhesion and Biofilm Formation on Textured Breast Implant Shell Materials. Aesthet. Plast. Surg. 2019, 43, 490–497. [Google Scholar] [CrossRef]
- Jones, P.; Mempin, M.; Hu, H.; Chowdhury, D.; Foley, M.; Cooter, R.; Adams, W.P., Jr.; Vickery, K.; Deva, A.K. The Functional Influence of Breast Implant Outer Shell Morphology on Bacterial Attachment and Growth. Plast. Reconstr. Surg. 2018, 142, 837–849. [Google Scholar] [CrossRef]
- Bartsich, S.; Ascherman, J.A.; Whittier, S.; Yao, C.A.; Rohde, C. The breast: A clean-contaminated surgical site. Aesthet. Surg. J. 2011, 31, 802–806. [Google Scholar] [CrossRef]
- Clinton, A.; Carter, T. Chronic Wound Biofilms: Pathogenesis and Potential Therapies. Lab. Med. 2015, 46, 277–284. [Google Scholar] [CrossRef]
- Burg, G.; Kempf, W.; Haeffner, A.; Döbbeling, U.; Nestle, F.O.; Böni, R.; Kadin, M.; Dummer, R. From inflammation to neoplasia: New concepts in the pathogenesis of cutaneous lymphomas. Recent Results Cancer Res. 2002, 160, 271–280. [Google Scholar] [CrossRef]
- Hardy, M.Y.; Tye-Din, J.A. Coeliac disease: A unique model for investigating broken tolerance in autoimmunity. Clin. Transl. Immunol. 2016, 5, e112. [Google Scholar] [CrossRef]
- de Souza Gonçalves, V.L.; Santos, M.L.C.; Luz, M.S.; Marques, H.S.; de Brito, B.B.; da Silva, F.A.F.; Souza, C.L.; Oliveira, M.V.; de Melo, F.F. From Helicobacter pylori infection to gastric cancer: Current evidence on the immune response. World J. Clin. Oncol. 2022, 13, 186–199. [Google Scholar] [CrossRef]
- Lechner, M.G.; Megiel, C.; Church, C.H.; Angell, T.E.; Russell, S.M.; Sevell, R.B.; Jang, J.K.; Brody, G.S.; Epstein, A.L. Survival signals and targets for therapy in breast implant-associated ALK--anaplastic large cell lymphoma. Clin. Cancer Res. 2012, 18, 4549–4559. [Google Scholar] [CrossRef]
- Wolfram, D.; Rabensteiner, E.; Grundtman, C.; Böck, G.; Mayerl, C.; Parson, W.; Almanzar, G.; Hasenöhrl, C.; Piza-Katzer, H.; Wick, G. T regulatory cells and TH17 cells in peri-silicone implant capsular fibrosis. Plast. Reconstr. Surg. 2012, 129, 327e–337e. [Google Scholar] [CrossRef]
- Hu, H.; Jacombs, A.; Vickery, K.; Merten, S.L.; Pennington, D.G.; Deva, A.K. Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: Implications for breast implant-associated lymphoma. Plast. Reconstr. Surg. 2015, 135, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Mempin, M.; Hu, H.; Vickery, K.; Kadin, M.E.; Prince, H.M.; Kouttab, N.; Morgan, J.W.; Adams, W.P., Jr.; Deva, A.K. Gram-Negative Bacterial Lipopolysaccharide Promotes Tumor Cell Proliferation in Breast Implant-Associated Anaplastic Large-Cell Lymphoma. Cancers 2021, 13, 5298. [Google Scholar] [CrossRef] [PubMed]
- Salter, S.J.; Cox, M.J.; Turek, E.M.; Calus, S.T.; Cookson, W.O.; Moffatt, M.F.; Turner, P.; Parkhill, J.; Loman, N.J.; Walker, A.W. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014, 12, 87. [Google Scholar] [CrossRef]
- Mohammadi, T.; Reesink, H.W.; Vandenbroucke-Grauls, C.M.J.E.; Savelkoul, P.H.M. Removal of contaminating DNA from commercial nucleic acid extraction kit reagents. J. Microbiol. Methods 2005, 61, 285–288. [Google Scholar] [CrossRef]
- Kulakov, L.A.; McAlister, M.B.; Ogden, K.L.; Larkin, M.J.; O’Hanlon, J.F. Analysis of bacteria contaminating ultrapure water in industrial systems. Appl. Environ. Microbiol. 2002, 68, 1548–1555. [Google Scholar] [CrossRef]
- Tevis, S.E.; Hunt, K.K.; Miranda, R.N.; Lange, C.; Butler, C.E.; Clemens, M.W. Differences in Human Leukocyte Antigen Expression Between Breast Implant-Associated Anaplastic Large Cell Lymphoma Patients and the General Population. Aesthet. Surg. J. 2019, 39, 1065–1070. [Google Scholar] [CrossRef]
- Ionescu, P.; Vibert, F.; Amé, S.; Mathelin, C. New Data on the Epidemiology of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Eur. J. Breast Health 2021, 17, 302–307. [Google Scholar] [CrossRef]
- Adlard, J.; Burton, C.; Turton, P. Increasing Evidence for the Association of Breast Implant-Associated Anaplastic Large Cell Lymphoma and Li Fraumeni Syndrome. Case Rep. Genet. 2019, 2019, 5647940. [Google Scholar] [CrossRef]
- Oishi, N.; Miranda, R.N.; Feldman, A.L. Genetics of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). Aesthet. Surg. J. 2019, 39 (Suppl. 1), S14–S20. [Google Scholar] [CrossRef]
- Laurent, C.; Nicolae, A.; Laurent, C.; Le Bras, F.; Haioun, C.; Fataccioli, V.; Amara, N.; Adélaïde, J.; Guille, A.; Schiano, J.M.; et al. Gene alterations in epigenetic modifiers and JAK-STAT signaling are frequent in breast implant-associated ALCL. Blood 2020, 135, 360–370. [Google Scholar] [CrossRef]
- Di Napoli, A.; Jain, P.; Duranti, E.; Margolskee, E.; Arancio, W.; Facchetti, F.; Alobeid, B.; Santanelli di Pompeo, F.; Mansukhani, M.; Bhagat, G. Targeted next generation sequencing of breast implant-associated anaplastic large cell lymphoma reveals mutations in JAK/STAT signalling pathway genes, TP53 and DNMT3A. Br. J. Haematol. 2018, 180, 741–744. [Google Scholar] [CrossRef]
- Letourneau, A.; Maerevoet, M.; Milowich, D.; Dewind, R.; Bisig, B.; Missiaglia, E.; de Leval, L. Dual JAK1 and STAT3 mutations in a breast implant-associated anaplastic large cell lymphoma. Virchows Arch. 2018, 473, 505–511. [Google Scholar] [CrossRef]
- Sansone, P.; Bromberg, J. Targeting the interleukin-6/Jak/stat pathway in human malignancies. J. Clin. Oncol. 2012, 30, 1005–1014. [Google Scholar] [CrossRef]
- Blombery, P.; Thompson, E.; Ryland, G.L.; Joyce, R.; Byrne, D.J.; Khoo, C.; Lade, S.; Hertzberg, M.; Hapgood, G.; Marlton, P.; et al. Frequent activating STAT3 mutations and novel recurrent genomic abnormalities detected in breast implant-associated anaplastic large cell lymphoma. Oncotarget 2018, 9, 36126–36136. [Google Scholar] [CrossRef] [PubMed]
- Tevis, S.E.; Hunt, K.K.; Miranda, R.N.; Lange, C.; Pinnix, C.C.; Iyer, S.; Butler, C.E.; Clemens, M.W. Breast Implant-associated Anaplastic Large Cell Lymphoma: A Prospective Series of 52 Patients. Ann. Surg. 2022, 275, e245–e249. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K.; Gilmour, A.; Jones, G.; O’Donoghue, J.M.; Clemens, M.W. A Systematic Review of Outcomes Following Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). JPRAS Open 2022, 34, 178–188. [Google Scholar] [CrossRef] [PubMed]
- Clemens, M.W.; Jacobsen, E.D.; Horwitz, S.M. 2019 NCCN Consensus Guidelines on the Diagnosis and Treatment of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). Aesthet. Surg. J. 2019, 39, S3–S13. [Google Scholar] [CrossRef]
- Available online: https://www.nccn.org/professionals/physician_gls/pdf/t-cell.pdf (accessed on 29 November 2022).
- Jones, J.L.; Hanby, A.M.; Wells, C.; Calaminici, M.; Johnson, L.; Turton, P.; Deb, R.; Provenzano, E.; Shaaban, A.; Ellis, I.O.; et al. Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL): An overview of presentation and pathogenesis and guidelines for pathological diagnosis and management. Histopathology 2019, 75, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Lamaris, G.A.; Butler, C.E.; Deva, A.K.; Miranda, R.N.; Hunt, K.K.; Connell, T.; Lipa, J.E.; Clemens, M.W. Breast Reconstruction Following Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2019, 143, 51S–58S. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; O’donoghue, J.M.; McLean, N.; Turton, P.; Khan, A.A.; Turner, S.D.; Lennard, A.; Collis, N.; Butterworth, M.; Gui, G.; et al. Breast implant associated anaplastic large cell lymphoma: The UK experience. Recommendations on its management and implications for informed consent. Eur. J. Surg. Oncol. 2017, 43, 1393–1401. [Google Scholar] [CrossRef]
- Adams, W.P.; Culbertson, E.J.; Deva, A.K.; RMagnusson, M.; Layt, C.; Jewell, M.L.; Mallucci, P.; Hedén, P. Macrotextured Breast Implants with Defined Steps to Minimize Bacterial Contamination around the Device: Experience in 42,000 Implants. Plast. Reconstr. Surg. 2017, 140, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Epps, M.T.; Langsdon, S.; Pels, T.K.; Noyes, V.; Levine, D.; Thurston, T.E.; Spratt, H.G.; Brzezienski, M.A. Pocket Irrigation and Technique During Reconstructive Surgery: An American Society of Plastic Surgery Survey of Current Practice. Ann. Plast. Surg. 2019, 82, S427–S432. [Google Scholar] [CrossRef] [PubMed]
- Jewell, M.L.; Adams, W.P. Betadine and Breast Implants. Aesthet. Surg. J. 2018, 38, 623–626. [Google Scholar] [CrossRef]
- Jewell, M.L.; Bionda, N.; Moran, A.V.; Bevels, E.J.; Jewell, H.L.; Hariri, S.; Leung, B.K. In Vitro Evaluation of Common Antimicrobial Solutions Used for Breast Implant Soaking and Breast Pocket Irrigation-Part 2: Efficacy Against Biofilm-Associated Bacteria. Aesthet. Surg. J. 2021, 41, 1252–1262. [Google Scholar] [CrossRef]
- Ngaage, L.M.; Elegbede, A.; Brao, K.; Chopra, K.; Gowda, A.U.; Nam, A.J.; Ernst, R.K.; Shirtliff, M.E.; Harro, J.; Rasko, Y.M. The Efficacy of Breast Implant Irrigant Solutions: A Comparative Analysis Using an In Vitro Model. Plast. Reconstr. Surg. 2020, 146, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Culbertson, E.J.; Felder-Scott, C.; Deva, A.K.; Greenberg, D.E.; Adams, W.P. Optimizing Breast Pocket Irrigation: The Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) Era. Aesthet. Surg. J. 2020, 40, 619–625. [Google Scholar] [CrossRef]
- Swanson, E. The Case Against Betadine Irrigation of Breast Implant Pockets. Aesthet. Plast. Surg. 2022, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Dang, T.; Yim, N.; Tummala, S.; Parsa, A.A.; Parsa, F.D. Povidone-Iodine versus antibiotic irrigation in breast implant surgery: Revival of the ideal solution. J. Plast. Reconstr. Aesthet. Surg. 2020, 73, 391–407. [Google Scholar] [CrossRef]
- Venkataram, A.; Lahar, N.; Adams, W.P. Enhancing Patient Outcomes in Aesthetic Breast Implant Procedures Using Proven Antimicrobial Breast Pocket Irrigations: A 20 Year Follow-up. Aesthet. Surg. J. 2022, 43, 66–73. [Google Scholar] [CrossRef]
- Dawson, S.E.; Bamba, R.; Tran, P.C.; Mailey, B.; Lin, J.; Lester, M.; Sinha, M.; Hassanein, A.H. Implant-Based Breast Reconstruction Outcomes Using Oxychlorosene for Pocket Irrigation. Plast. Reconstr. Surg. 2021, 148, 518e–520e. [Google Scholar] [CrossRef]
- Baker, N.F.; Hart, A.M.; Carlson, G.W.; Losken, A. A Systematic Review of Breast Irrigation in Implant-Based Breast Surgery. Ann. Plast. Surg. 2021, 86, 359–364. [Google Scholar] [CrossRef]
| PROS | CONS | |
|---|---|---|
| Micro-organisms | ||
| Lipopolysaccharide (LPS) |
| |
| Silicone |
| |
| Lymphocytes | ||
| Interleukins |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alessandri-Bonetti, M.; Jeong, T.; Vaienti, L.; De La Cruz, C.; Gimbel, M.L.; Nguyen, V.T.; Egro, F.M. The Role of Microorganisms in the Development of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Pathogens 2023, 12, 313. https://doi.org/10.3390/pathogens12020313
Alessandri-Bonetti M, Jeong T, Vaienti L, De La Cruz C, Gimbel ML, Nguyen VT, Egro FM. The Role of Microorganisms in the Development of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Pathogens. 2023; 12(2):313. https://doi.org/10.3390/pathogens12020313
Chicago/Turabian StyleAlessandri-Bonetti, Mario, Tiffany Jeong, Luca Vaienti, Carolyn De La Cruz, Michael L. Gimbel, Vu T. Nguyen, and Francesco M. Egro. 2023. "The Role of Microorganisms in the Development of Breast Implant-Associated Anaplastic Large Cell Lymphoma" Pathogens 12, no. 2: 313. https://doi.org/10.3390/pathogens12020313
APA StyleAlessandri-Bonetti, M., Jeong, T., Vaienti, L., De La Cruz, C., Gimbel, M. L., Nguyen, V. T., & Egro, F. M. (2023). The Role of Microorganisms in the Development of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Pathogens, 12(2), 313. https://doi.org/10.3390/pathogens12020313







