Digital Marketing: A Unique Multidisciplinary Approach towards the Elimination of Viral Hepatitis
Abstract
1. Introduction
Digital Marketing and Its Tools
2. Health and Digital Technologies
2.1. Social Media’s Impact on Health Care System
2.2. Current Pandemic and Digital Revolution
2.3. Engagement of Influencers in Public Health Issues
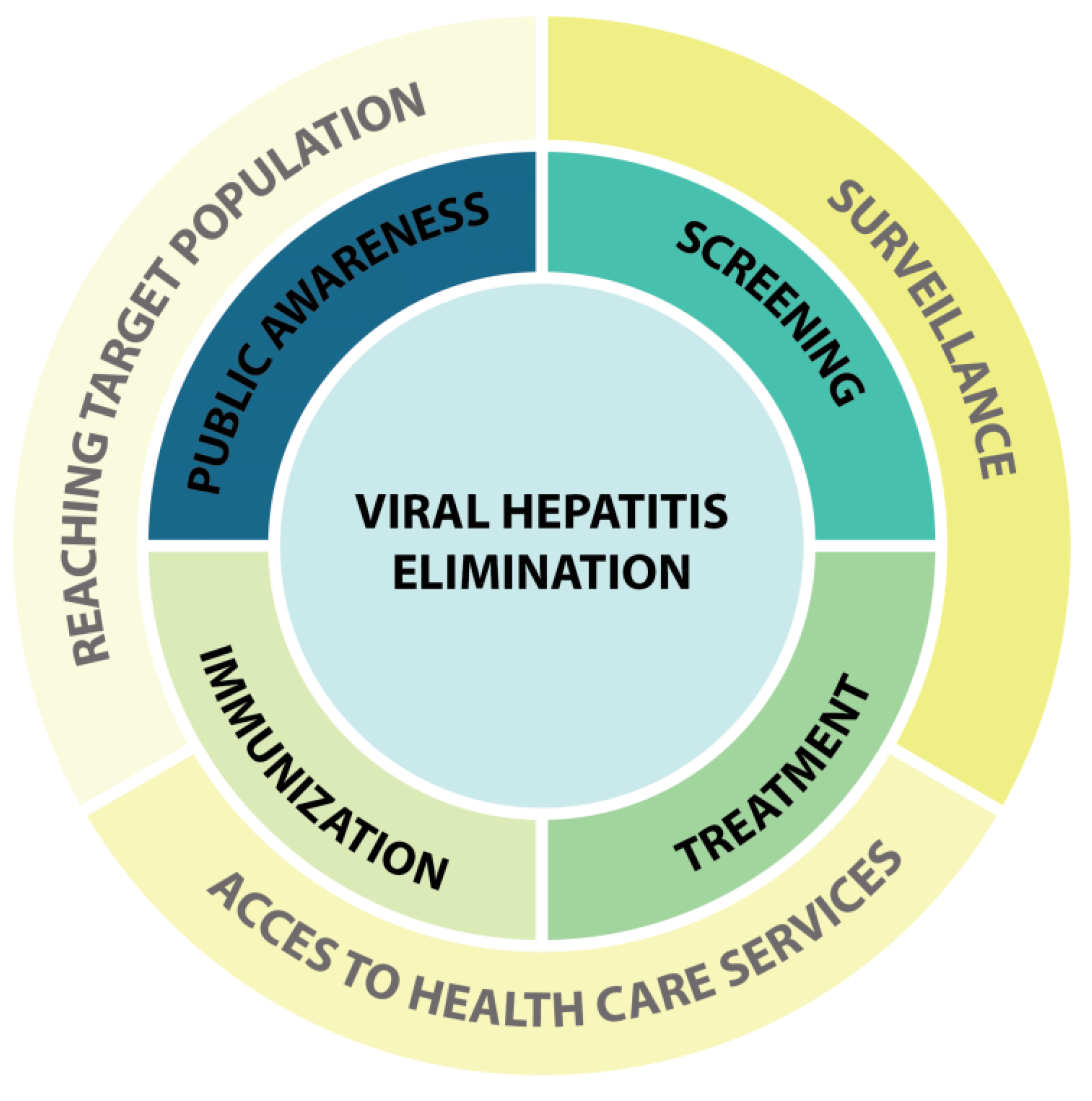
3. Viral Hepatitis Elimination and Applicable Digital Marketing
3.1. Burden of Viral Hepatitis
3.2. Current Status of Viral Hepatitis and Digital Technologies
3.3. Social Media and Data Mining in Viral Hepatitis Elimination
3.4. Merging Strategies
Author Contributions
Funding
Conflicts of Interest
References
- Ghezzi, A.; Dramitinos, M. Towards a Future Internet infrastructure: Analyzing the multidimensional impacts of assured quality Internet interconnection. Telemat. Inform. 2016, 33, 613–630. [Google Scholar] [CrossRef]
- Serval, T. Transformation digitale: Quand les problématiques industrielles refont surface. J. L’école Paris Manag. 2018, 4, 15–22. [Google Scholar] [CrossRef]
- Kannan, P. Digital marketing: A framework, review and research agenda. Int. J. Res. Mark. 2017, 34, 22–45. [Google Scholar] [CrossRef]
- Brandt, D.; Henning, K. Information and communication technologies: Perspectives and their impact on society. AI Soc. 2002, 16, 210–223. [Google Scholar] [CrossRef]
- Heinze, A.; Fletcher, G.; Rashid, T.; Cruz, A. Digital and Social Media Marketing: A Results-Driven Approach; Routledge: London, UK, 2020. [Google Scholar]
- Holloway, I.W.; Dunlap, S.; Del Pino, H.E.; Hermanstyne, K.; Pulsipher, C.; Landovitz, R.J. Online social networking, sexual risk and protective behaviors: Considerations for clinicians and researchers. Curr. Addict. Rep. 2014, 1, 220–228. [Google Scholar] [CrossRef]
- Madden, M.; Lenhart, A.; Cortesi, S.; Gasser, U.; Duggan, M.; Smith, A.; Beaton, M. Teens, social media, and privacy. Pew Res. Cent. 2013, 21, 2–86. [Google Scholar]
- Barreto, A.M. Do users look at banner ads on Facebook? J. Res. Interact. Mark. 2013, 7, 119–139. [Google Scholar] [CrossRef]
- Duffett, R.G. Influence of social media marketing communications on young consumers’ attitudes. Young Consum. 2017, 18, 19–39. [Google Scholar] [CrossRef]
- Chu, S.-C.; Kim, Y. Determinants of consumer engagement in electronic word-of-mouth (eWOM) in social networking sites. Int. J. Advert. 2011, 30, 47–75. [Google Scholar] [CrossRef]
- Floreddu, P.B.; Cabiddu, F. Social media communication strategies. J. Serv. Mark. 2016, 30, 490–503. [Google Scholar] [CrossRef]
- Gvili, Y.; Levy, S. Consumer engagement with eWOM on social media: The role of social capital. Online Inf. Rev. 2018, 42, 482–505. [Google Scholar] [CrossRef]
- Jernigan, D.H.; Rushman, A.E. Measuring youth exposure to alcohol marketing on social networking sites: Challenges and prospects. J. Public Health Policy 2014, 35, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Glazyrin, Y.E.; Veprintsev, D.V.; Ler, I.A.; Rossovskaya, M.L.; Varygina, S.A.; Glizer, S.L.; Zamay, T.N.; Petrova, M.M.; Minic, Z.; Berezovski, M.V. Proteomics-Based Machine Learning Approach as an Alternative to Conventional Biomarkers for Differential Diagnosis of Chronic Kidney Diseases. Int. J. Mol. Sci. 2020, 21, 4802. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; An, J.; Bruno, A.; Cai, X.; Fan, J.; Fujimoto, J.; Golfieri, R.; Hao, X.; Jiang, H.; Jiao, L.R. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatol. Int. 2020, 14, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Utunen, H.; Attias, M.; George, R.; Ndiaye, N.; Piroux, C.; Farzi, M.R.; Sy, A.; Gamhewage, G. Global Access to OpenWHO’s Online Learning Resources for COVID-19. Stud. Health Technol. Inform. 2020, 272, 304–305. [Google Scholar]
- Moorhead, S.A.; Hazlett, D.E.; Harrison, L.; Carroll, J.K.; Irwin, A.; Hoving, C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Internet Res. 2013, 15, e85. [Google Scholar] [CrossRef]
- Tang, L.; Bie, B.; Park, S.-E.; Zhi, D. Social media and outbreaks of emerging infectious diseases: A systematic review of literature. Am. J. Infect. Control. 2018, 46, 962–972. [Google Scholar] [CrossRef]
- Truth, A.U. No health without a workforce. In World Health Organisation (WHO) Report; WHO: Geneva, Switzerland, 2013; pp. 1–104. [Google Scholar]
- Dhingra, D.; Dabas, A. Global Strategy on Digital Health. Indian Pediatrics 2020, 57, 356–358. [Google Scholar] [CrossRef]
- Improta, G.; De Luca, V.; Illario, M.; Triassi, M. Digital innovation in healthcare: A device with a method for monitoring, managing and preventing the risk of chronic polypathological patients. Transl. Med. UniSa 2020, 21, 61. [Google Scholar]
- Simpson, S.; Reid, C. Telepsychology in A ustralia: 2020 vision. Aust. J. Rural. Health 2014, 22, 306–309. [Google Scholar] [CrossRef]
- Fox, S. Online Health Search 2006. Pew Internet and American Life Project. 29 October 2006. Available online: http://www.pewinternet.org/pdfs/PIP_Online_Health_2006.pdf (accessed on 29 October 2006).
- Nielsen, R.C.; Luengo-Oroz, M.; Mello, M.B.; Paz, J.; Pantin, C.; Erkkola, T. Social media monitoring of discrimination and HIV testing in Brazil, 2014–2015. AIDS Behav. 2017, 21, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Polgreen, P.M.; Chen, Y.; Pennock, D.M.; Nelson, F.D.; Weinstein, R.A. Using internet searches for influenza surveillance. Clin. Infect. Dis. 2008, 47, 1443–1448. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, J.; Mohebbi, M.H.; Patel, R.S.; Brammer, L.; Smolinski, M.S.; Brilliant, L. Detecting influenza epidemics using search engine query data. Nature 2009, 457, 1012–1014. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.H.; Sahai, V.; Conrad, C.; Brownstein, J.S. Using web search query data to monitor dengue epidemics: A new model for neglected tropical disease surveillance. PLoS Negl. Trop. Dis. 2011, 5, e1206. [Google Scholar] [CrossRef]
- Chan, E.; Sahai, V.; Conrad, C.; Brownstein, J. Web search query data to monitor dengue epidemics: A new model for dengue surveillance. In Proceedings of the International Society for Disease Surveillance 10th Annual Conference 2011 Building the Future of Public Health Surveillance, Atlanta, GA, USA; 2011. [Google Scholar]
- Smith, C.; Sokhey, L.; Tijamo, C.F.E.; McLaren, M.; Free, C.; Watkins, J.; Amra, O.; Masuda, C.; Oreglia, E. Development of an intervention to support reproductive health of garment factory workers in Cambodia: A qualitative study. BMJ Open 2021, 11, e049254. [Google Scholar] [CrossRef]
- Yousef, H.; Al-Sheyab, N.; Al Nsour, M.; Khader, Y.; Al Kattan, M.; Bardus, M.; Alyahya, M.; Taha, H.; Amiri, M. Perceptions Toward the Use of Digital Technology for Enhancing Family Planning Services: Focus Group Discussion with Beneficiaries and Key Informative Interview with Midwives. J. Med. Internet Res. 2021, 23, e25947. [Google Scholar] [CrossRef]
- Hempler, N.F.; Joensen, L.E.; Willaing, I. Relationship between social network, social support and health behaviour in people with type 1 and type 2 diabetes: Cross-sectional studies. BMC Public Health 2016, 16, 198. [Google Scholar] [CrossRef]
- Ashrafi, S.; Taylor, D.; Tang, T.S. Moving beyond ‘don’t ask, don’t tell’: Mental health needs of adults with type 1 diabetes in rural and remote regions of British Columbia. Diabet. Med. 2021, 38, e14534. [Google Scholar] [CrossRef]
- Li, C.; Ademiluyi, A.; Ge, Y.; Park, A. Using Social Media to Understand Web-Based Social Factors Concerning Obesity: Systematic Review. JMIR Public Health Surveill. 2022, 8, e25552. [Google Scholar] [CrossRef]
- Yan, Q.; Jensen, K.J.; Thomas, R.; Field, A.R.; Jiang, Z.; Goei, C.; Davies, M.G. Digital Footprint of Academic Vascular Surgeons in the Southern United States on Physician Rating Websites: Cross-sectional Evaluation Study. JMIR Cardio 2021, 5, e22975. [Google Scholar] [CrossRef]
- Fung, I.C.-H.; Tse, Z.T.H.; Cheung, C.-N.; Miu, A.S.; Fu, K.-W. Ebola and the social media. Lancet 2014, 384, 2207. [Google Scholar] [CrossRef]
- Young, S.D.; Rivers, C.; Lewis, B. Methods of using real-time social media technologies for detection and remote monitoring of HIV outcomes. Prev. Med. 2014, 63, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Stoové, M.A.; Pedrana, A.E. Making the most of a brave new world: Opportunities and considerations for using Twitter as a public health monitoring tool. Prev. Med. 2014, 63, 109–111. [Google Scholar] [CrossRef] [PubMed]
- van der Worp, H.; Brandenbarg, D.; Boek, P.A.; Braams, J.H.; Brink, L.J.; Keupers, J.; Blanker, M.H. Identifying women’s preferences for treatment of urinary tract infection: A discrete choice experiment. BMJ Open 2021, 11, e049916. [Google Scholar] [CrossRef] [PubMed]
- Muflih, S.M.; Al-Azzam, S.; Karasneh, R.A.; Conway, B.R.; Aldeyab, M.A. Public Health Literacy, Knowledge, and Awareness Regarding Antibiotic Use and Antimicrobial Resistance during the COVID-19 Pandemic: A Cross-Sectional Study. Antibiotics 2021, 10, 1107. [Google Scholar] [CrossRef]
- Stevens, R.; Gilliard-Matthews, S.; Dunaev, J.; Todhunter-Reid, A.; Brawner, B.; Stewart, J. Social media use and sexual risk reduction behavior among minority youth: Seeking safe sex information. Nurs. Res. 2017, 66, 368. [Google Scholar] [CrossRef]
- Phillips, G.; Magnus, M.; Kuo, I.; Rawls, A.; Peterson, J.; Jia, Y.; Opoku, J.; Greenberg, A.E. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behav. 2014, 18, 1630–1637. [Google Scholar] [CrossRef]
- Rendina, H.J.; Jimenez, R.H.; Grov, C.; Ventuneac, A.; Parsons, J.T. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS Behav. 2014, 18, 41–49. [Google Scholar] [CrossRef]
- Holloway, I.W.; Rice, E.; Gibbs, J.; Winetrobe, H.; Dunlap, S.; Rhoades, H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav. 2014, 18, 285–296. [Google Scholar] [CrossRef]
- Acharya, K.P.; Subedi, D. Use of Social Media as a Tool to Reduce Antibiotic Usage: A Neglected Approach to Combat Antimicrobial Resistance in Low and Middle Income Countries. Front. Public Health 2020, 8, 671. [Google Scholar] [CrossRef]
- Mazińska, B.; Strużycka, I.; Hryniewicz, W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: Did the European Antibiotic Awareness Day campaigns change attitudes? PLoS ONE 2017, 12, e0172146. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.; Lam, K.; Ho, P.; Yung, W. Knowledge, attitude, and behaviour toward antibiotics among Hong Kong people: Local-born versus immigrants. Hong Kong Med. J. 2015, 21, S41–S47. [Google Scholar] [PubMed]
- Or, P.-L.; Ching, T.-Y. The effectiveness of raising Hong Kong parents’ awareness of antimicrobial resistance through an education program with peer support on social media: A randomized, controlled pilot study. BMC Public Health 2022, 22, 315. [Google Scholar] [CrossRef] [PubMed]
- Alumran, A.; Hou, X.-Y.; Hurst, C. Assessing the overuse of antibiotics in children in Saudi Arabia: Validation of the parental perception on antibiotics scale (PAPA scale). Health Qual. Life Outcomes 2013, 11, 39. [Google Scholar] [CrossRef]
- Hutinel, M.; Larsson, D.J.; Flach, C.-F. Antibiotic resistance genes of emerging concern in municipal and hospital wastewater from a major Swedish city. Sci. Total Environ. 2022, 812, 151433. [Google Scholar] [CrossRef]
- Ellis, J.; Vassilev, I.; Kennedy, A.; Moore, M.; Rogers, A. Help seeking for antibiotics; is the influence of a personal social network relevant? BMC Fam. Pract. 2019, 20, 63. [Google Scholar] [CrossRef]
- Djerf-Pierre, M.; Lindgren, M. Making sense of “superbugs” on YouTube: A storytelling approach. Public Underst. Sci. 2021, 30, 535–551. [Google Scholar] [CrossRef]
- Pisano, J.; Pettit, N.; Bartlett, A.; Bhagat, P.; Han, Z.; Liao, C.; Landon, E. Social media as a tool for antimicrobial stewardship. Am. J. Infect. Control. 2016, 44, 1231–1236. [Google Scholar] [CrossRef]
- Hale, A.R.; Young, V.L.; Grand, A.; McNulty, C.A.M. Can gaming increase antibiotic awareness in children? A mixed-methods approach. JMIR Serious Games 2017, 5, e6420. [Google Scholar] [CrossRef]
- Patel, M.K.; Dumolard, L.; Nedelec, Y.; Sodha, S.V.; Steulet, C.; Gacic-Dobo, M.; Kretsinger, K.; McFarland, J.; Rota, P.A.; Goodson, J.L. Progress toward regional measles elimination—worldwide, 2000–2018. Morb. Mortal. Wkly. Rep. 2019, 68, 1105. [Google Scholar] [CrossRef]
- Wawrzuta, D.; Jaworski, M.; Gotlib, J.; Panczyk, M. Characteristics of antivaccine messages on social media: Systematic review. J. Med. Internet Res. 2021, 23, e24564. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.L.; Zollo, F.; Scala, A.; Betsch, C.; Quattrociocchi, W. Polarization of the vaccination debate on Facebook. Vaccine 2018, 36, 3606–3612. [Google Scholar] [CrossRef] [PubMed]
- Bozzola, E.; Spina, G.; Tozzi, A.E.; Villani, A. Global measles epidemic risk: Current perspectives on the growing need for implementing digital communication strategies. Risk Manag. Healthc. Policy 2020, 13, 2819. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, K.; Coomes, E.A.; Haghbayan, H. Temporal trends in anti-vaccine discourse on Twitter. Vaccine 2019, 37, 4867–4871. [Google Scholar] [CrossRef] [PubMed]
- Broniatowski, D.A.; Hilyard, K.M.; Dredze, M. Effective vaccine communication during the disneyland measles outbreak. Vaccine 2016, 34, 3225–3228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kang, G.J.; Culp, R.K.; Abbas, K.M. Facilitators and barriers of parental attitudes and beliefs toward school-located influenza vaccination in the United States: Systematic review. Vaccine 2017, 35, 1987–1995. [Google Scholar] [CrossRef] [PubMed]
- Bodson, J.; Wilson, A.; Warner, E.L.; Kepka, D. Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in Utah. PLoS ONE 2017, 12, e0183725. [Google Scholar] [CrossRef]
- Massey, P.M.; Kearney, M.D.; Hauer, M.K.; Selvan, P.; Koku, E.; Leader, A.E. Dimensions of misinformation about the HPV vaccine on Instagram: Content and network analysis of social media characteristics. J. Med. Internet Res. 2020, 22, e21451. [Google Scholar] [CrossRef]
- Zhong, B.; Liu, Q. Medical Insights from Posts About Irritable Bowel Syndrome by Adolescent Patients and Their Parents: Topic Modeling and Social Network Analysis. J. Med. Internet Res. 2021, 23, e26867. [Google Scholar] [CrossRef]
- Lammert, C.; Comerford, M.; Love, J.; Bailey, J.R. Investigation gone viral: Application of the social mediasphere in research. Gastroenterology 2015, 149, 839–843. [Google Scholar] [CrossRef][Green Version]
- Sheppard, M.K. mHealth Apps: Disruptive Innovation, Regulation, and Trust—A Need for Balance. Med. Law Rev. 2020, 28, 549–572. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.A.; Lunney, M.; Chong, C.; Tonelli, M. Identifying Mobile Applications Aimed at Self-Management in People with Chronic Kidney Disease. Can. J. Kidney Health Dis. 2019, 6, 2054358119834283. [Google Scholar] [CrossRef] [PubMed]
- Falkenhain, K.; Locke, S.R.; Lowe, D.A.; Lee, T.; Singer, J.; Weiss, E.J.; Little, J.P. Use of an mHealth Ketogenic Diet App Intervention and User Behaviors Associated with Weight Loss in Adults with Overweight or Obesity: Secondary Analysis of a Randomized Clinical Trial. JMIR mHealth uHealth 2022, 10, e33940. [Google Scholar] [CrossRef] [PubMed]
- Turesson, C.; Liedberg, G.; Björk, M. Development of a Digital Support Application with Evidence-Based Content for Sustainable Return to Work for Persons with Chronic Pain and Their Employers: User-Centered Agile Design Approach. JMIR Hum. Factors 2022, 9, e33571. [Google Scholar] [CrossRef]
- Rochat, J.; Ehrler, F.; Siebert, J.N.; Ricci, A.; Ruiz, V.G.; Lovis, C. Usability Testing of a Patient-Centered Mobile Health App for Supporting and Guiding the Pediatric Emergency Department Patient Journey: Mixed Methods Study. JMIR Pediatrics Parent. 2022, 5, e25540. [Google Scholar] [CrossRef]
- Denecke, K.; Schmid, N.; Nüssli, S. Implementation of Cognitive Behavioral Therapy in e–Mental Health Apps: Literature Review. J. Med. Internet Res. 2022, 24, e27791. [Google Scholar] [CrossRef]
- Anastasiadou, D.; Lupiañez-Villanueva, F.; Faulí, C.; Cunillera, J.A.; Serrano-Troncoso, E. Cost-effectiveness of the mobile application TCApp combined with face-to-face CBT treatment compared to face-to-face CBT treatment alone for patients with an eating disorder: Study protocol of a multi-centre randomised controlled trial. BMC Psychiatry 2018, 18, 118. [Google Scholar] [CrossRef]
- Oladeru, O.T.; Eber, G.; McClelland, S., III. Should patients who are incarcerated on death row receive palliative cancer care? Lancet Oncol. 2020, 21, 337–338. [Google Scholar] [CrossRef]
- Lwin, M.O.; Lu, J.; Sheldenkar, A.; Schulz, P.J.; Shin, W.; Gupta, R.; Yang, Y. Global sentiments surrounding the COVID-19 pandemic on Twitter: Analysis of Twitter trends. JMIR Public Health Surveill. 2020, 6, e19447. [Google Scholar] [CrossRef]
- Seltzer, E.K.; Jean, N.; Kramer-Golinkoff, E.; Asch, D.A.; Merchant, R. The content of social media’s shared images about Ebola: A retrospective study. Public Health 2015, 129, 1273–1277. [Google Scholar] [CrossRef]
- Gui, X.; Wang, Y.; Kou, Y.; Reynolds, T.L.; Chen, Y.; Mei, Q.; Zheng, K. Understanding the patterns of health information dissemination on social media during the Zika outbreak. AMIA Annu. Symp. Proc. 2017, 2017, 820–829. [Google Scholar] [PubMed]
- Gu, H.; Chen, B.; Zhu, H.; Jiang, T.; Wang, X.; Chen, L.; Jiang, Z.; Zheng, D.; Jiang, J. Importance of Internet surveillance in public health emergency control and prevention: Evidence from a digital epidemiologic study during avian influenza A H7N9 outbreaks. J. Med. Internet Res. 2014, 16, e2911. [Google Scholar] [CrossRef] [PubMed]
- Lwin, M.O.; Jayasundar, K.; Sheldenkar, A.; Wijayamuni, R.; Wimalaratne, P.; Ernst, K.C.; Foo, S. Lessons from the implementation of Mo-Buzz, a mobile pandemic surveillance system for dengue. JMIR Public Health Surveill. 2017, 3, e7376. [Google Scholar] [CrossRef] [PubMed]
- Fung, I.C.-H.; Fu, K.-W.; Ying, Y.; Schaible, B.; Hao, Y.; Chan, C.-H.; Tse, Z.T.-H. Chinese social media reaction to the MERS-CoV and avian influenza A (H7N9) outbreaks. Infect. Dis. Poverty 2013, 2, 31. [Google Scholar] [CrossRef] [PubMed]
- Ginossar, T.; Cruickshank, I.J.; Zheleva, E.; Sulskis, J.; Berger-Wolf, T. Cross-platform spread: Vaccine-related content, sources, and conspiracy theories in YouTube videos shared in early Twitter COVID-19 conversations. Hum. Vaccines Immunother. 2022, 18, 1–13. [Google Scholar] [CrossRef]
- Thijssen, M.; Devos, T.; Ejtahed, H.-S.; Amini-Bavil-Olyaee, S.; Pourfathollah, A.A.; Pourkarim, M.R. Convalescent plasma against COVID-19: A broad-spectrum therapeutic approach for emerging infectious diseases. Microorganisms 2020, 8, 1733. [Google Scholar]
- Halim, D.A.; Kurniawan, A.; Agung, F.H.; Angelina, S.; Jodhinata, C.; Winata, S.; Wijovi, F.; Agatha, C.M. Understanding of Young People About COVID-19 During Early Outbreak in Indonesia. Asia-Pac. J. Public Health 2020, 32, 363–365. [Google Scholar] [CrossRef]
- Yousuf, H.; Corbin, J.; Sweep, G.; Hofstra, M.; Scherder, E.; Van Gorp, E.; Zwetsloot, P.P.; Zhao, J.; Van Rossum, B.; Jiang, T. Association of a public health campaign about coronavirus disease 2019 promoted by news media and a social influencer with self-reported personal hygiene and physical distancing in the Netherlands. JAMA Netw. Open 2020, 3, e2014323. [Google Scholar] [CrossRef]
- Stechemesser, A.; Wenz, L.; Levermann, A. Corona crisis fuels racially profiled hate in social media networks. EClinicalMedicine 2020, 23, 100372. [Google Scholar] [CrossRef]
- Yadav, S.K.; Yadav, N. Continuity of cancer care in the era of COVID-19 pandemic: Role of social media in low-and middle-income countries. World J. Clin. Cases 2021, 9, 291. [Google Scholar] [CrossRef]
- Li, H.; Zheng, S.; Da Li, D.J.; Liu, F.; Guo, W.; Zhao, Z.; Zhou, Y.; Liu, J.; Zhao, R. The Establishment and Practice of Pharmacy Care Service Based on Internet Social Media: Telemedicine in Response to the COVID-19 Pandemic. Front. Pharmacol. 2021, 12, 707442. [Google Scholar] [CrossRef] [PubMed]
- Pulido, C.M.; Ruiz-Eugenio, L.; Redondo-Sama, G.; Villarejo-Carballido, B. A New Application of Social Impact in Social Media for Overcoming Fake News in Health. Int. J. Environ. Res. Public Health 2020, 17, 2430. [Google Scholar] [CrossRef] [PubMed]
- Constantinou, M.; Kagialis, A.; Karekla, M. COVID-19 scientific facts vs. Conspiracy theories: Is science failing to pass its message? Int. J. Environ. Res. Public Health 2021, 18, 6343. [Google Scholar] [CrossRef] [PubMed]
- Shahsavari, S.; Holur, P.; Wang, T.; Tangherlini, T.R.; Roychowdhury, V. Conspiracy in the time of corona: Automatic detection of emerging COVID-19 conspiracy theories in social media and the news. J. Comput. Soc. Sci. 2020, 3, 279–317. [Google Scholar] [CrossRef]
- Siegler, A.J.; Luisi, N.; Hall, E.W.; Bradley, H.; Sanchez, T.; Lopman, B.A.; Sullivan, P.S. Trajectory of COVID-19 Vaccine Hesitancy Over Time and Association of Initial Vaccine Hesitancy with Subsequent Vaccination. JAMA Netw. Open 2021, 4, e2126882. [Google Scholar] [CrossRef]
- Clark, S.E.; Bledsoe, M.C.; Harrison, C.J. The role of social media in promoting vaccine hesitancy. Curr. Opin. Pediatrics 2022, 34, 156–162. [Google Scholar] [CrossRef]
- Blane, J.T.; Bellutta, D.; Carley, K.M. Social-Cyber Maneuvers During the COVID-19 Vaccine Initial Rollout: Content Analysis of Tweets. J. Med. Internet Res. 2022, 24, e34040. [Google Scholar] [CrossRef]
- Keelan, J.; Pavri-Garcia, V.; Tomlinson, G.; Wilson, K. YouTube as a source of information on immunization: A content analysis. Jama 2007, 298, 2482–2484. [Google Scholar] [CrossRef]
- Bonnevie, E.; Goldbarg, J.; Gallegos-Jeffrey, A.K.; Rosenberg, S.D.; Wartella, E.; Smyser, J. Content themes and influential voices within vaccine opposition on Twitter, 2019. Am. J. Public Health 2020, 110, S326–S330. [Google Scholar] [CrossRef]
- Hoffman, B.L.; Felter, E.M.; Chu, K.-H.; Shensa, A.; Hermann, C.; Wolynn, T.; Williams, D.; Primack, B.A. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook. Vaccine 2019, 37, 2216–2223. [Google Scholar] [CrossRef]
- Bonnevie, E.; Smith, S.M.; Kummeth, C.; Goldbarg, J.; Smyser, J. Social media influencers can be used to deliver positive information about the flu vaccine: Findings from a multi-year study. Health Educ. Res. 2021, 36, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, S.C.; Eaton, L.A.; Earnshaw, V.A.; Brousseau, N. Faster than warp speed: Early attention to COVD-19 by anti-vaccine groups on Facebook. J. Public Health 2022, 44, e96–e105. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Tong, Y.; Du, F.; Lu, L.; Zhao, S.; Yu, K.; Piatek, S.J.; Larson, H.J.; Lin, L. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: A global social listening study. J. Med. Internet Res. 2021, 23, e27632. [Google Scholar] [CrossRef] [PubMed]
- Jamison, A.M.; Broniatowski, D.A.; Dredze, M.; Sangraula, A.; Smith, M.C.; Quinn, S.C. Not just conspiracy theories: Vaccine opponents and proponents add to the COVID-19 ‘infodemic’on Twitter. Harv. Kennedy Sch. Misinform. Rev. 2020, 1. [Google Scholar] [CrossRef]
- Donzelli, G.; Palomba, G.; Federigi, I.; Aquino, F.; Cioni, L.; Verani, M.; Carducci, A.; Lopalco, P. Misinformation on vaccination: A quantitative analysis of YouTube videos. Hum. Vaccines Immunother. 2018, 14, 1654–1659. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, L.; Wijermans, A.; Orchard, F.; Höhle, M.; Czernichow, T.; Coletti, P.; Hermans, L.; Faes, C.; Kissling, E.; Mollet, T. Epitweetr: Early warning of public health threats using Twitter data. SSRN 2021, 397, 3811673. [Google Scholar] [CrossRef]
- Leonard, N.R.; Casarjian, B.; Fletcher, R.R.; Prata, C.; Sherpa, D.; Kelemen, A.; Rajan, S.; Salaam, R.; Cleland, C.M.; Gwadz, M.V. Theoretically-based emotion regulation strategies using a mobile app and wearable sensor among homeless adolescent mothers: Acceptability and feasibility study. JMIR Pediatrics Parent. 2018, 1, e9037. [Google Scholar] [CrossRef]
- Ming, L.C.; Untong, N.; Aliudin, N.A.; Osili, N.; Kifli, N.; Tan, C.S.; Goh, K.W.; Ng, P.W.; Al-Worafi, Y.M.; Lee, K.S. Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. JMIR mHealth uHealth 2020, 8, e19796. [Google Scholar] [CrossRef]
- Lattie, E.G.; Cohen, K.A.; Hersch, E.; Williams, K.D.; Kruzan, K.P.; MacIver, C.; Hermes, J.; Maddi, K.; Kwasny, M.; Mohr, D.C. Uptake and effectiveness of a self-guided mobile app platform for college student mental health. Internet Interv. 2022, 27, 100493. [Google Scholar] [CrossRef]
- Davalbhakta, S.; Advani, S.; Kumar, S.; Agarwal, V.; Bhoyar, S.; Fedirko, E.; Misra, D.; Goel, A.; Gupta, L.; Agarwal, V. A systematic review of the smartphone applications available for coronavirus disease 2019 (COVID19) and their assessment using the mobile app rating scale (MARS). medRxiv 2020. [Google Scholar] [CrossRef]
- Huang, Z.; Guo, H.; Lim, H.Y.-F.; Chow, A. Determinants of the acceptance and adoption of a digital contact tracing tool during the COVID-19 pandemic in Singapore. Epidemiol. Infect. 2022, 150, e54. [Google Scholar] [CrossRef] [PubMed]
- Tsvyatkova, D.; Buckley, J.; Beecham, S.; Chochlov, M.; O’Keeffe, I.R.; Razzaq, A.; Rekanar, K.; Richardson, I.; Welsh, T.; Storni, C. Digital Contact Tracing Apps for COVID-19: Development of a Citizen-Centered Evaluation Framework. JMIR mHealth uHealth 2022, 10, e30691. [Google Scholar] [CrossRef] [PubMed]
- Majeed, M.T.; Khan, F.N. Do information and communication technologies (ICTs) contribute to health outcomes? An empirical analysis. Qual. Quant. 2019, 53, 183–206. [Google Scholar] [CrossRef]
- Becker, E.R.; Shegog, R.; Savas, L.S.; Frost, E.L.; Coan, S.P.; Healy, C.M.; Spinner, S.W.; Vernon, S.W. Parents’ Experience with a Mobile Health Intervention to Influence Human Papillomavirus Vaccination Decision Making: Mixed Methods Study. JMIR Pediatrics Parent. 2022, 5, e30340. [Google Scholar] [CrossRef]
- Muñoz-Ramírez, S.; Escribano-López, B.; Rodrigo-Casares, V.; Vergara-Hernández, C.; Gil-Mary, D.; Sorribes-Monrabal, I.; Garcés-Sánchez, M.; Muñoz-Del-Barrio, M.-J.; Albors-Fernández, A.-M.; Úbeda-Sansano, M.-I. Feasibility of a hybrid clinical trial for respiratory virus detection in toddlers during the influenza season. BMC Med. Res. Methodol. 2021, 21, 273. [Google Scholar] [CrossRef]
- Antonelli, M.; Penfold, R.S.; Merino, J.; Sudre, C.H.; Molteni, E.; Berry, S.; Canas, L.S.; Graham, M.S.; Klaser, K.; Modat, M. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: A prospective, community-based, nested, case-control study. Lancet Infect. Dis. 2022, 22, 43–55. [Google Scholar] [CrossRef]
- Fahy, N.; Williams, G.A. Use of Digital Health Tools in Europe: Before, during and after COVID-19; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2021. [Google Scholar]
- Arias-Oliva, M.; Pelegrín-Borondo, J.; Almahameed, A.A.; Andrés-Sánchez, J.d. Ethical Attitudes toward COVID-19 Passports: Evidences from Spain. Int. J. Environ. Res. Public Health 2021, 18, 13098. [Google Scholar] [CrossRef]
- Morley, J.; Cowls, J.; Taddeo, M.; Floridi, L. Ethical Guidelines for COVID-19 Tracing Apps; Nature Publishing Group: Berlin, Germany, 2020. [Google Scholar]
- Bengio, Y.; Ippolito, D.; Janda, R.; Jarvie, M.; Prud’homme, B.; Rousseau, J.-F.; Sharma, A.; Yu, Y.W. Inherent privacy limitations of decentralized contact tracing apps. J. Am. Med. Inform. Assoc. 2020, 28, 193–195. [Google Scholar] [CrossRef]
- Vandamme, A.-M.; Nguyen, T. Belgium--concerns about coronavirus contact-tracing apps. Nature 2020, 581, 384–385. [Google Scholar] [CrossRef]
- Godinho, M.A.; Martins, H.; Al-Shorbaji, N.; Quintana, Y.; Liaw, S.-T. “Digital Health Diplomacy” in Global Digital Health? A call for critique and discourse. J. Am. Med. Inform. Assoc. 2021, 29, 1019–1024. [Google Scholar] [CrossRef]
- Zeng, K.; Bernardo, S.N.; Havins, W.E. The use of digital tools to mitigate the COVID-19 pandemic: Comparative retrospective study of six countries. JMIR Public Health Surveill. 2020, 6, e24598. [Google Scholar] [CrossRef] [PubMed]
- Grande, D.; Mitra, N.; Marti, X.L.; Merchant, R.; Asch, D.; Dolan, A.; Sharma, M.; Cannuscio, C. Consumer views on using digital data for COVID-19 control in the United States. JAMA Netw. Open 2021, 4, e2110918. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.L.; Malik, A.; Ruhi, U.; Al-Busaidi, A. Conflicting attitudes: Analyzing social media data to understand the early discourse on COVID-19 passports. Technol. Soc. 2022, 68, 101830. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Hudders, L.; De Jans, S.; De Veirman, M. The value of influencer marketing for business: A bibliometric analysis and managerial implications. J. Advert. 2021, 50, 160–178. [Google Scholar] [CrossRef]
- Childers, C.C.; Lemon, L.L.; Hoy, M.G. #Sponsored# Ad: Agency perspective on influencer marketing campaigns. J. Curr. Issues Res. Advert. 2019, 40, 258–274. [Google Scholar]
- Glucksman, M. The rise of social media influencer marketing on lifestyle branding: A case study of Lucie Fink. Elon J. Undergrad. Res. Commun. 2017, 8, 77–87. [Google Scholar]
- Lou, C.; Yuan, S. Influencer marketing: How message value and credibility affect consumer trust of branded content on social media. J. Interact. Advert. 2019, 19, 58–73. [Google Scholar] [CrossRef]
- Gough, A.; Hunter, R.F.; Ajao, O.; Jurek, A.; McKeown, G.; Hong, J.; Barrett, E.; Ferguson, M.; McElwee, G.; McCarthy, M. Tweet for behavior change: Using social media for the dissemination of public health messages. JMIR Public Health Surveill. 2017, 3, e6313. [Google Scholar] [CrossRef]
- Byrne, E.; Kearney, J.; MacEvilly, C. The role of influencer marketing and social influencers in public health. Proc. Nutr. Soc. 2017, 76, E103. [Google Scholar] [CrossRef]
- Navarro, M.A.; O’Brien, E.K.; Ganz, O.; Hoffman, L. Influencer prevalence and role on cigar brand Instagram pages. Tob. Control. 2021, 30, e33–e36. [Google Scholar] [CrossRef]
- La Fauci, V.; Mondello, S.; Squeri, R.; Alessi, V.; Genovese, C.; Laudani, N.; Cattaruzza, M. Family, lifestyles and new and old type of smoking in young adults: Insights from an italian multiple-center study. Ann Ig 2021, 33, 131–140. [Google Scholar] [PubMed]
- Ortiz, R.R.; Smith, A.; Coyne-Beasley, T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccines Immunother. 2019, 15, 1465–1475. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Stevens, R. Applying lessons from behavioral economics to increase flu vaccination rates. Health Promot. Int. 2017, 32, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Priebe Rocha, L.; Soares, C.; McGregor, A.; Chen, S.; Kaplan, A.; Rose, R.R.; Galvão, H.; Siqueira, C.E.; Allen, J.D. Understanding health priorities, behaviors, and service utilization among Brazilian immigrant women: Implications for designing community-based interventions. J. Racial Ethn. Health Disparities 2022, 9, 135–145. [Google Scholar] [CrossRef]
- Hong, Y.A.; Yee, S.; Bagchi, P.; Juon, H.-S.; Kim, S.C.; Le, D. Social media-based intervention to promote HBV screening and liver cancer prevention among Korean Americans: Results of a pilot study. Digit. Health 2022, 8, 20552076221076257. [Google Scholar] [CrossRef]
- Massaro, M.; Tamburro, P.; La Torre, M.; Dal Mas, F.; Thomas, R.; Cobianchi, L.; Barach, P. Non-pharmaceutical interventions and the infodemic on Twitter: Lessons learned from Italy during the COVID-19 Pandemic. J. Med. Syst. 2021, 45, 50. [Google Scholar] [CrossRef]
- Arora, S.; Bø, B.; Tjoflåt, I.; Eslen-Ziya, H. Immigrants in Norway: Resilience, challenges and vulnerabilities in times of COVID-19. J. Migr. Health 2022, 5, 100089. [Google Scholar] [CrossRef]
- Xu, L.; Tang, F.; Chen, Y.; Dong, X. Acculturation and depressive symptoms among older Chinese immigrants in the United States: The roles of positive and negative social interactions. Aging Ment. Health 2022, 26, 1–8. [Google Scholar] [CrossRef]
- Zhou, X.; Yap, P.; Tanner, M.; Bergquist, R.; Utzinger, J.; Zhou, X.-N. Surveillance and response systems for elimination of tropical diseases: Summary of a thematic series in infectious diseases of poverty. Infect. Dis. Poverty 2016, 5, 9–15. [Google Scholar] [CrossRef]
- Henderson, D.A. The eradication of smallpox–an overview of the past, present, and future. Vaccine 2011, 29, D7–D9. [Google Scholar] [CrossRef]
- Hasso-Agopsowicz, M.; Crowcroft, N.; Biellik, R.; Gregory, C.J.; Menozzi-Arnaud, M.; Amorij, J.-P.; Gilbert, P.-A.; Earle, K.; Frivold, C.; Jarrahian, C. Accelerating the Development of Measles and Rubella Microarray Patches to Eliminate Measles and Rubella: Recent Progress, Remaining Challenges. Front. Public Health 2022, 10, 809675. [Google Scholar] [CrossRef] [PubMed]
- De La Santé, O.M.; World Health Organization. Malaria vaccine: WHO position paper–March 2022–Rapport mensuel des cas de dracunculose, janvier 2022. Wkly. Epidemiol. Rec. Relev. Épidémiol. Hebd. 2022, 97, 60–78. [Google Scholar]
- Vorsters, A.; Bosch, F.X.; Poljak, M.; Stanley, M.; Garland, S.M.; HPV Prevention and Control Board and the International Papillomavirus Society. HPV prevention and control–The way forward (1490 words, 1500 limit). Prev. Med. 2022, 156, 106960. [Google Scholar] [CrossRef] [PubMed]
- Malik, G.F.; Zakaria, N.; Majeed, M.I.; Ismail, F.W. Viral Hepatitis-The Road Traveled and the Journey Remaining. Hepatic Med. Evid. Res. 2022, 14, 13. [Google Scholar]
- Pourkarim, M.R.; Amini-Bavil-Olyaee, S.; Kurbanov, F.; Van Ranst, M.; Tacke, F. Molecular identification of hepatitis B virus genotypes/subgenotypes: Revised classification hurdles and updated resolutions. World J. Gastroenterol. WJG 2014, 20, 7152. [Google Scholar] [CrossRef] [PubMed]
- Rezaee-Zavareh, M.S.; Hesamizadeh, K.; Behnava, B.; Alavian, S.M.; Gholami-Fesharaki, M.; Sharafi, H. Combination of ledipasvir and sofosbuvir for treatment of hepatitis C virus genotype 1 infection: Systematic review and meta-analysis. Ann. Hepatol. 2017, 16, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Sharafi, H.; Alavian, S.M. The rising threat of hepatocellular carcinoma in the Middle East and North Africa region: Results from Global Burden of Disease Study 2017. Clin. Liver Dis. 2019, 14, 219. [Google Scholar] [CrossRef]
- Sonderup, M.W.; Spearman, C.W. Global Disparities in Hepatitis B Elimination—A Focus on Africa. Viruses 2022, 14, 82. [Google Scholar] [CrossRef]
- Pourkarim, M.R.; Thijssen, M.; Alavian, S.M.; Van Ranst, M. Natural disasters pose a challenge for hepatitis elimination in Iran. Lancet Gastroenterol. Hepatol. 2019, 4, 581–582. [Google Scholar] [CrossRef]
- Zangiabadian, M.; Zamani, A.; Nasiri, M.J.; Behzadi, E.; Fooladi, A.A.I. Diagnostic Accuracy and Validity of Serological and Molecular Tests for Hepatitis B and C. Curr. Pharm. Biotechnol. 2022, 23, 803–817. [Google Scholar] [CrossRef]
- Cuypers, L.; Thijssen, M.; Shakibzadeh, A.; Sabahi, F.; Ravanshad, M.; Pourkarim, M.R. Next-generation sequencing for the clinical management of hepatitis C virus infections: Does one test fits all purposes? Crit. Rev. Clin. Lab. Sci. 2019, 56, 420–434. [Google Scholar] [CrossRef] [PubMed]
- Cuypers, L.; Thijssen, M.; Shakibzadeh, A.; Deboutte, W.; Sarvari, J.; Sabahi, F.; Ravanshad, M.; Pourkarim, M.R. Signature of natural resistance in NS3 protease revealed by deep sequencing of HCV strains circulating in Iran. Infect. Genet. Evol. 2019, 75, 103966. [Google Scholar] [CrossRef] [PubMed]
- Pourkarim, M.R.; Vergote, V.; Amini-Bavil-Olyaee, S.; Sharifi, Z.; Sijmons, S.; Lemey, P.; Maes, P.; Alavian, S.M.; Van Ranst, M. Molecular characterization of hepatitis B virus (HBV) strains circulating in the northern coast of the Persian Gulf and its comparison with worldwide distribution of HBV subgenotype D1. J. Med. Virol. 2014, 86, 745–757. [Google Scholar] [CrossRef] [PubMed]
- Fakhr, A.E.; Pourkarim, M.R.; Maes, P.; Atta, A.H.; Marei, A.; Azab, M.; Van Ranst, M. Hepatitis C virus NS5B sequence-based genotyping analysis of patients from the Sharkia Governorate, Egypt. Hepat. Mon. 2013, 13, e12706. [Google Scholar]
- Trovão, N.S.; Thijssen, M.; Vrancken, B.; Pineda-Peña, A.-C.; Mina, T.; Amini-Bavil-Olyaee, S.; Lemey, P.; Baele, G.; Pourkarim, M.R. Reconstruction of the Origin and Dispersal of the Worldwide Dominant Hepatitis B Virus Subgenotype D1. Virus Evol. 2022, 8, veac028. [Google Scholar] [CrossRef]
- Mina, T.; Amini-Bavil-Olyaee, S.; Shirvani-Dastgerdi, E.; Trovao, N.S.; Van Ranst, M.; Pourkarim, M.R. 15year fulminant hepatitis B follow-up in Belgium: Viral evolution and signature of demographic change. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2017, 49, 221–225. [Google Scholar] [CrossRef]
- Mina, T.; Amini Bavil Olyaee, S.; Tacke, F.; Maes, P.; Van Ranst, M.; Pourkarim, M.R. Genomic Diversity of Hepatitis B Virus Infection Associated with Fulminant Hepatitis B Development. Hepat. Mon. 2015, 15, e29477. [Google Scholar] [CrossRef]
- Amini-Bavil-Olyaee, S.; Pourkarim, M.; Schaefer, S.; Mahboudi, F.; Van Ranst, M.; Adeli, A.; Trautwein, C.; Tacke, F. Single-step real-time PCR to quantify hepatitis B virus and distinguish genotype D from non-D genotypes. J. Viral Hepat. 2011, 18, 300–304. [Google Scholar] [CrossRef]
- Zhang, M.; Li, G.; Shang, J.; Pan, C.; Zhang, M.; Yin, Z.; Xie, Q.; Peng, Y.; Mao, Q.; Xiao, X. Rapidly decreased HBV RNA predicts responses of pegylated interferons in HBeAg-positive patients: A longitudinal cohort study. Hepatol. Int. 2020, 14, 212–224. [Google Scholar] [CrossRef]
- Pourkarim, M.R.; Ranst, M.V. Guidelines for the detection of a common source of hepatitis B virus infections. Hepat. Mon. 2011, 11, 783–785. [Google Scholar]
- Amini-Bavil-Olyaee, S.; Maes, P.; Van Ranst, M.; Pourkarim, M.R. Providing strong evidence of nosocomial outbreak of hepatitis B virus infection. J. Hosp. Infect. 2012, 80, 269–270. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Sector Strategy on Viral Hepatitis 2016–2021. Towards Ending Viral Hepatitis; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Combating hepatitis B and C to reach elimination by 2030. 2016; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Thijssen, M.; Lemey, P.; Amini-Bavil-Olyaee, S.; Dellicour, S.; Alavian, S.M.; Tacke, F.; Verslype, C.; Nevens, F.; Pourkarim, M.R. Mass migration to Europe: An opportunity for elimination of hepatitis B virus? Lancet Gastroenterol. Hepatol. 2019, 4, 315–323. [Google Scholar] [CrossRef]
- Pourkarim, M.R.; Razavi, H.; Lemey, P.; Van Ranst, M. Iran’s hepatitis elimination programme is under threat. Lancet 2018, 392, 1009. [Google Scholar] [CrossRef]
- Collaborators, P.O.; Razavi, H.; Blach, S.; Razavi-Shearer, D.; Abaalkhail, F.; Abbas, Z.; Abdallah, A.; Abrao Ferreira, P.; Abu Raddad, L.J.; Adda, D. The case for simplifying and using absolute targets for viral hepatitis elimination goals. J. Viral Hepat. 2021, 28, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Haering, C.; McMahon, B.; Harris, A.; Weis, N.; Lundberg Ederth, J.; Axelsson, M.; Olafsson, S.; Osiowy, C.; Tomas, K.; Bollerup, S. Hepatitis B virus elimination status and strategies in circumpolar countries, 2020. Int. J. Circumpolar Health 2021, 80, 1986975. [Google Scholar] [CrossRef] [PubMed]
- De Villiers, M.J.; Nayagam, S.; Hallett, T.B. The impact of the timely birth dose vaccine on the global elimination of hepatitis B. Nat. Commun. 2021, 12, 6223. [Google Scholar] [CrossRef]
- Artenie, A.; Luhmann, N.; Lim, A.G.; Fraser, H.; Ward, Z.; Stone, J.; MacGregor, L.; Walker, J.G.; Trickey, A.; Marquez, L.K. Methods and indicators to validate country reductions in incidence of hepatitis C virus infection to elimination levels set by WHO. Lancet Gastroenterol. Hepatol. 2022, 7, 353–366. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wiktor, S.; Colombo, M.; Thursz, M. Micro-elimination–A path to global elimination of hepatitis C. J. Hepatol. 2017, 67, 665–666. [Google Scholar] [CrossRef]
- Ólafsson, S.; Tyrfingsson, T.; Rúnarsdóttir, V.; Bergmann, O.; Hansdóttir, I.; Björnsson, E.S.; Johannsson, B.; Sigurdardottir, B.; Fridriksdottir, R.; Löve, A. Treatment as Prevention for Hepatitis C (TraP Hep C)–a nationwide elimination programme in Iceland using direct-acting antiviral agents. J. Intern. Med. 2018, 283, 500–507. [Google Scholar] [CrossRef]
- Whitelaw, S.; Mamas, M.A.; Topol, E.; Van Spall, H.G. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit. Health 2020, 2, e435–e440. [Google Scholar] [CrossRef]
- Thijssen, M.; Van Ranst, M.; Pourkarim, M.R. Elimination of Viral Hepatitis and an Update on Blood Safety Technology; Kowsar: Heerlen, The Netherlands, 2018; Volume 18. [Google Scholar]
- Harjai, K.J.; Agarwal, S.; Bauch, T.; Bernardi, M.; Casale, A.S.; Green, S.; Harostock, M.; Ierovante, N.; Mascarenhas, V.; Matsumura, M. Coronary and structural heart disease interventions during COVID-19 pandemic: A road map for clinicians and health care delivery systems. Cardiovasc. Revascularization Med. 2020, 21, 939–945. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Shaw, R. Identifying research trends and gaps in the context of COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3370. [Google Scholar] [CrossRef] [PubMed]
- Chuaypen, N.; Khlaiphuengsin, A.; Prasoppokakorn, T.; Susantitaphong, P.; Prasithsirikul, W.; Avihingsanon, A.; Tangkijvanich, P.; Praditpornsilpa, K. Prevalence and genotype distribution of hepatitis C virus within hemodialysis units in Thailand: Role of HCV core antigen in the assessment of viremia. BMC Infect. Dis. 2022, 22, 79. [Google Scholar] [CrossRef] [PubMed]
- Ehelepola, N.; Wijewardana, B. An episode of transmission of COVID-19 from a vaccinated healthcare worker to co-workers. Infect. Dis. 2021, 54, 297–302. [Google Scholar] [CrossRef]
- Ai, J.; Zhang, H.; Zhang, Y.; Lin, K.; Zhang, Y.; Wu, J.; Wan, Y.; Huang, Y.; Song, J.; Fu, Z. Omicron variant showed lower neutralizing sensitivity than other SARS-CoV-2 variants to immune sera elicited by vaccines after boost. Emerg. Microbes Infect. 2021, 11, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chemaitelly, H.; Tang, P.; Hasan, M.R.; AlMukdad, S.; Yassine, H.M.; Benslimane, F.M.; Al Khatib, H.A.; Coyle, P.; Ayoub, H.H.; Al Kanaani, Z. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N. Engl. J. Med. 2021, 385, e83. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Safreed-Harmon, K.; Thursz, M.R.; Dillon, J.F.; El-Sayed, M.H.; Elsharkawy, A.M.; Hatzakis, A.; Jadoul, M.; Prestileo, T.; Razavi, H. The micro-elimination approach to eliminating hepatitis C: Strategic and operational considerations. Semin. Liver Dis. 2018, 38, 181–192. [Google Scholar]
- Schwartz, P.; Sedillo, J.L.; Sapp, J.L. Hepatitis a Vaccine Promotion Using Facebook Ads to Reach At-Risk Groups. Am. J. Health Promot. 2021, 35, 08901171211044594. [Google Scholar] [CrossRef]
- Bentouhami, M.; Chakib, A.; El Fane, M. Hepatitis B knowledge, attitudes and practices among Moroccan college students. Rev. D’épidémiologie St. Publique 2019, 67, 397–402. [Google Scholar] [CrossRef]
- Wong, W.C.; Yang, N.S.; Li, J.; Li, H.; Wan, E.Y.; Fitzpatrick, T.; Xiong, Y.; Seto, W.-K.; Chan, P.; Liu, R. Crowdsourcing to promote hepatitis C testing and linkage-to-care in China: A randomized controlled trial protocol. BMC Public Health 2020, 20, 1048. [Google Scholar] [CrossRef]
- World Health Organization. Action Plan for the Health Sector Response to Viral Hepatitis in the WHO European Region; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Momin, B.; Nielsen, D.; Schaff, S.; Mezzo, J.L.; Cariou, C. Promising Interventions to Prevent Liver Cancer in Idaho. Health Promot. Pract. 2021, 22, 15248399211057154. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Zhang, X.; Wu, A.; Miser, J.S.; Liu, Y.-L.; Hsu, J.C.; Shia, B.-C.; Ye, L. Association between Social Media Use and Cancer Screening Awareness and Behavior for People without a Cancer Diagnosis: Matched Cohort Study. J. Med. Internet Res. 2021, 23, e26395. [Google Scholar] [CrossRef] [PubMed]
- Alber, J.M.; Cohen, C.; Nguyen, G.T.; Ghazvini, S.F.; Tolentino, B.T. Exploring communication strategies for promoting hepatitis B prevention among young Asian American adults. J. Health Commun. 2018, 23, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Nicolay, N.; Bourhis-Zaimi, L.; Lesourd, A.; Martel, M.; Roque-Afonso, A.-M.; Erouart, S.; Etienne, M.; Ndeikoundam Ngangro, N. A description of a hepatitis A outbreak in men who have sex with men and public health measures implemented in Seine-Maritime department, Normandy, France, 2017. BMC Public Health 2020, 20, 1441. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, H.; Benusic, M.; Ota, S.; Stuart, R.; Maclachlan, J.; Dubey, V.; Andonov, A. Open Science/Open Data: Community outbreak of hepatitis A disproportionately affecting men who have sex with men in Toronto, Canada, January 2017–November 2018. Can. Commun. Dis. Rep. 2019, 45, 262. [Google Scholar] [CrossRef]
- Roy, A.; King, C.; Gilson, R.; Richardson, D.; Burns, F.; Rodger, A.; Clark, L.; Miners, A.; Pollard, A.; Desai, S. Healthcare provider and service user perspectives on STI risk reduction interventions for young people and MSM in the UK. Sex. Transm. Infect. 2020, 96, 26–32. [Google Scholar] [CrossRef]
- Cavazos-Rehg, P.; Grucza, R.; Krauss, M.J.; Smarsh, A.; Anako, N.; Kasson, E.; Kaiser, N.; Sansone, S.; Winograd, R.; Bierut, L.J. Utilizing social media to explore overdose and HIV/HCV risk behaviors among current opioid misusers. Drug Alcohol Depend. 2019, 205, 107690. [Google Scholar] [CrossRef]
- Baker, L.S.; Smith, W.; Gulley, T.; Tomann, M.M. Community perceptions of comprehensive harm reduction programs and stigma towards people who inject drugs in rural Virginia. J. Community Health 2020, 45, 239–244. [Google Scholar] [CrossRef]
- Seehusen, D.A.; Bowman, M.A.; Neale, A.V. New tools and approaches for family physicians. Am. Board Fam. Med. 2015, 28, 689–692. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; Castellanos-Mateus, S.; Rojas-Moreno, H.; Suárez-Molina, J. YouTube videos as a source of Hepatitis C-related information: A cross-sectional study. Travel Med. Infect. Dis. 2020, 37, 101708. [Google Scholar] [CrossRef]
- Islam, J.Y.; Spees, L.; Camacho-Rivera, M.; Vidot, D.C.; Yarosh, R.; Wheldon, C.W. Disparities in awareness of hepatitis C virus among US adults: An analysis of the 2019 Health Information National Trends Survey. Sex. Transm. Dis. 2021, 48, 981–985. [Google Scholar] [CrossRef] [PubMed]
- Robotin, M.C.; Wallace, J.; Gallego, G.; George, J. Hepatitis B and Liver Cancer: Community Awareness, Knowledge and Beliefs of Middle Eastern Migrants in Sydney, Australia. Int. J. Environ. Res. Public Health 2021, 18, 8534. [Google Scholar] [CrossRef] [PubMed]
- Plant, A.; Snow, E.G.; Montoya, J.A.; Young, S.; Javanbakht, M.; Klausner, J.D. Test4HepC: Promoting hepatitis C testing to baby boomers using social media. Health Promot. Pract. 2020, 21, 780–790. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.L.; Wiysonge, C. Social media and vaccine hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef]
- Bar-Lev, S.; Reichman, S.; Barnett-Itzhaki, Z. Prediction of vaccine hesitancy based on social media traffic among Israeli parents using machine learning strategies. Isr. J. Health Policy Res. 2021, 10, 49. [Google Scholar] [CrossRef]
- Becker, B.F.; Larson, H.J.; Bonhoeffer, J.; Van Mulligen, E.M.; Kors, J.A.; Sturkenboom, M.C. Evaluation of a multinational, multilingual vaccine debate on Twitter. Vaccine 2016, 34, 6166–6171. [Google Scholar] [CrossRef]
- Sharpe, J.D.; Hopkins, R.S.; Cook, R.L.; Striley, C.W. Evaluating Google, Twitter, and Wikipedia as tools for influenza surveillance using Bayesian change point analysis: A comparative analysis. JMIR Public Health Surveill. 2016, 2, e5901. [Google Scholar] [CrossRef]
- Qiu, R.; Hadzikadic, M.; Yu, S.; Yao, L. Estimating disease burden using Internet data. Health Inform. J. 2019, 25, 1863–1877. [Google Scholar] [CrossRef]
- Da, B.L.; Surana, P.; Schueler, S.A.; Jalaly, N.Y.; Kamal, N.; Taneja, S.; Vittal, A.; Gilman, C.L.; Heller, T.; Koh, C. Twitter As a Noninvasive Bio-Marker for Trends in Liver Disease. Hepatol. Commun. 2019, 3, 1271–1280. [Google Scholar] [CrossRef]
- Sommaggio, P.; Marchiori, S. Health data ethics in the time of covid-19: A legal perspective. Humanid. Tecnol. 2020, 25, 95–101. [Google Scholar]
- Rashti, R.; Sharafi, H.; Alavian, S.M.; Moradi, Y.; Mohamadi Bolbanabad, A.; Moradi, G. Systematic Review and Meta-Analysis of Global Prevalence of HBsAg and HIV and HCV Antibodies among People Who Inject Drugs and Female Sex Workers. Pathogens 2020, 9, 432. [Google Scholar] [CrossRef]
- Thijssen, M.; Trovão, N.S.; Mina, T.; Maes, P.; Pourkarim, M.R. Novel hepatitis B virus subgenotype A8 and quasi-subgenotype D12 in African–Belgian chronic carriers. Int. J. Infect. Dis. 2020, 93, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Cooke, G.S.; Andrieux-Meyer, I.; Applegate, T.L.; Atun, R.; Burry, J.R.; Cheinquer, H.; Dusheiko, G.; Feld, J.J.; Gore, C.; Griswold, M.G. Accelerating the elimination of viral hepatitis: A Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol. Hepatol. 2019, 4, 135–184. [Google Scholar] [PubMed]
- Rogers, E.M.; Storey, J.D. Communication Campaigns; Sage: London, UK, 1987. [Google Scholar]
- Snyder, L.B. Health communication campaigns and their impact on behavior. J. Nutr. Educ. Behav. 2007, 39, S32–S40. [Google Scholar] [CrossRef] [PubMed]
- Kraak, V.I.; Consavage Stanley, K.; Harrigan, P.B.; Zhou, M. How have media campaigns been used to promote and discourage healthy and unhealthy beverages in the United States? A systematic scoping review to inform future research to reduce sugary beverage health risks. Obes. Rev. 2022, 23, e13425. [Google Scholar] [CrossRef]
- Kraak, V.I.; Consavage Stanley, K. A Systematic Scoping Review of Media Campaigns to Develop a Typology to Evaluate Their Collective Impact on Promoting Healthy Hydration Behaviors and Reducing Sugary Beverage Health Risks. Int. J. Environ. Res. Public Health 2021, 18, 1040. [Google Scholar] [CrossRef]
- Perler, B. Thrombolytic therapies: The current state of affairs. J. Endovasc. Ther. 2005, 12, 224–232. [Google Scholar] [CrossRef]
- Bonnevie, E.; Morales, O.; Rosenberg, S.D.; Goldbarg, J.; Silver, M.; Wartella, E.; Smyser, J. Evaluation of a campaign to reduce consumption of sugar-sweetened beverages in New Jersey. Prev. Med. 2020, 136, 106062. [Google Scholar] [CrossRef]
- Farley, T.A.; Halper, H.S.; Carlin, A.M.; Emmerson, K.M.; Foster, K.N.; Fertig, A.R. Mass media campaign to reduce consumption of sugar-sweetened beverages in a rural area of the United States. Am. J. Public Health 2017, 107, 989–995. [Google Scholar] [CrossRef]
- Alemany-Pagès, M.; Azul, A.M.; Ramalho-Santos, J. The use of comics to promote health awareness: A template using nonalcoholic fatty liver disease. Eur. J. Clin. Investig. 2022, 52, e13642. [Google Scholar] [CrossRef]
- Wogu, J.O.; Chukwu, C.O.; Orekyeh, E.S.S.; Anorue, L.I.; Nwokedi, O.; Chukwu, L.C. Communicating health risk in Southeast Nigeria: The case of media campaign against viral hepatitis and its implication for health communication. Medicine 2019, 98, e15847. [Google Scholar] [CrossRef] [PubMed]
- Moffat, R.; Sayer, A.; DeCook, K.; Cornia, A.; Linehan, M.; Torres, S.; Mulokozi, G.; Crookston, B.; Hall, C.; West, J. A National Communications Campaign to decrease childhood stunting in Tanzania: An analysis of the factors associated with exposure. BMC Public Health 2022, 22, 531. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-J.; Pena-y-Lillo, M. A communication inequalities approach to disparities in fruit and vegetable consumption: Findings from a national survey with US adults. Patient Educ. Couns. 2022, 105, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, K.; Yamamoto, K.; Leppold, C.; Tanimoto, T.; Kusumi, E.; Komatsu, T.; Kami, M. Trends of media coverage on human papillomavirus vaccination in Japanese newspapers. Clin. Infect. Dis. 2016, 63, ciw647. [Google Scholar]
- de Vries, M.; Claassen, L.; Te Wierik, M.J.; Timmermans, D.R.; Timmermans, A. Dynamics in public perceptions and media coverage during an ongoing outbreak of meningococcal W disease in the Netherlands. BMC Public Health 2022, 22, 9. [Google Scholar] [CrossRef]
- Neiger, B.L.; Thackeray, R.; Van Wagenen, S.A.; Hanson, C.L.; West, J.H.; Barnes, M.D.; Fagen, M.C. Use of social media in health promotion: Purposes, key performance indicators, and evaluation metrics. Health Promot. Pract. 2012, 13, 159–164. [Google Scholar] [CrossRef]
- Silva, T.M.; Estrela, M.; Roque, V.; Gomes, E.R.; Figueiras, A.; Roque, F.; Herdeiro, M.T. Perceptions, knowledge and attitudes about COVID-19 vaccine hesitancy in older Portuguese adults. Age Ageing 2022, 51, afac013. [Google Scholar] [CrossRef]
- Ford, K.; Bellis, M.A.; Hill, R.; Hughes, K. An evaluation of a short film promoting kindness in Wales during COVID-19 restrictions# TimeToBeKind. BMC Public Health 2022, 22, 583. [Google Scholar]
- Colston, D.C.; Xie, Y.; Thrasher, J.F.; Patrick, M.E.; Titus, A.R.; Emery, S.; McLeod, M.C.; Elliott, M.R.; Fleischer, N.L. Examining Truth and State-Sponsored Media Campaigns as a Means of Decreasing Youth Smoking and Related Disparities in the United States. Nicotine Tob. Res. 2022, 24, 469–477. [Google Scholar] [CrossRef]
- Vallone, D.; Cantrell, J.; Bennett, M.; Smith, A.; Rath, J.M.; Xiao, H.; Greenberg, M.; Hair, E.C. Evidence of the impact of the truth FinishIt campaign. Nicotine Tob. Res. 2018, 20, 543–551. [Google Scholar] [CrossRef]
- Kandra, K.; McCullough, A.; Summerlin-Long, S.; Agans, R.; Ranney, L.; Goldstein, A. The evaluation of North Carolina’s state-sponsored youth tobacco prevention media campaign. Health Educ. Res. 2013, 28, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Pandya, R.K.; Hussain, J.S.; Lau, R.J.; Chambers, E.A.B.; Geng, A.; Jin, B.X.; Zhou, O.; Wu, T.; Barr, L. Perceptions of using infographics for scientific communication on social media for COVID-19 topics: A survey study. J. Vis. Commun. Med. 2022, 45, 105–133. [Google Scholar] [CrossRef] [PubMed]
- Niederdeppe, J.; Kellogg, M.; Skurka, C.; Avery, R.J. Market-level exposure to state antismoking media campaigns and public support for tobacco control policy in the United States, 2001–2002. Tob. Control. 2018, 27, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Halkjelsvik, T. Do disgusting and fearful anti-smoking advertisements increase or decrease support for tobacco control policies? Int. J. Drug Policy 2014, 25, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Durkin, S.J.; Brennan, E.; Wakefield, M.A. Optimising Tobacco Control Campaigns within a Changing Media Landscape and among Priority Populations; BMJ Publishing Group Ltd.: London, UK, 2022. [Google Scholar]
- Hamill, S.; Turk, T.; Murukutla, N.; Ghamrawy, M.; Mullin, S. I ‘like’MPOWER: Using Facebook, online ads and new media to mobilise tobacco control communities in low-income and middle-income countries. Tob. Control. 2015, 24, 306–312. [Google Scholar] [CrossRef]
- Sims, M.; Langley, T.; Lewis, S.; Richardson, S.; Szatkowski, L.; McNeill, A.; Gilmore, A.B. Effectiveness of tobacco control television advertisements with different types of emotional content on tobacco use in England, 2004–2010. Tob. Control. 2016, 25, 21–26. [Google Scholar] [CrossRef]
- Murphy-Hoefer, R.; Davis, K.C.; Beistle, D.; King, B.A.; Duke, J.; Rodes, R.; Graffunder, C. Peer Reviewed: Impact of the Tips From Former Smokers Campaign on Population-Level Smoking Cessation, 2012–2015. Prev. Chronic Dis. 2018, 15, E71. [Google Scholar] [CrossRef]
- Stefanone, M.; Anker, A.E.; Evans, M.; Feeley, T.H. Click to “like” organ donation: The use of online media to promote organ donor registration. Prog. Transplant. 2012, 22, 168–174. [Google Scholar] [CrossRef]
- Carter, O.B.; Donovan, R.; Jalleh, G. Using viral e-mails to distribute tobacco control advertisements: An experimental investigation. J. Health Commun. 2011, 16, 698–707. [Google Scholar] [CrossRef]
- Quinn, S.C.; Hilyard, K.M.; Jamison, A.M.; An, J.; Hancock, G.R.; Musa, D.; Freimuth, V.S. The influence of social norms on flu vaccination among African American and White adults. Health Educ. Res. 2017, 32, 473–486. [Google Scholar] [CrossRef]
- Al-Marshoudi, S.; Al-Balushi, H.; Al-Wahaibi, A.; Al-Khalili, S.; Al-Maani, A.; Al-Farsi, N.; Al-Jahwari, A.; Al-Habsi, Z.; Al-Shaibi, M.; Al-Msharfi, M. Knowledge, Attitudes, and Practices (KAP) toward the COVID-19 vaccine in Oman: A pre-campaign cross-sectional study. Vaccines 2021, 9, 602. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, S.; Cotter, T.; Perez, D.; Wakefield, M. Televised antismoking advertising: Effects of level and duration of exposure. Am. J. Public Health 2013, 103, e66–e73. [Google Scholar] [CrossRef] [PubMed]
- Biener, L.; Wakefield, M.; Shiner, C.M.; Siegel, M. How broadcast volume and emotional content affect youth recall of anti-tobacco advertising. Am. J. Prev. Med. 2008, 35, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Okada, M.; Oeda, S.; Katsuki, N.; Iwane, S.; Kawaguchi, Y.; Kawamoto, S.; Tomine, Y.; Fukuyoshi, J.; Maeyama, K.; Tanaka, H. Recommendations from primary care physicians, family, friends and work colleagues influence patients’ decisions related to hepatitis screening, medical examinations and antiviral treatment. Exp. Ther. Med. 2020, 19, 2973–2982. [Google Scholar] [CrossRef]
- Signorelli, C.; Odone, A. Four Italian experiences on vaccination policies: Results and lessons. Ann Ig 2019, 31, 36–44. [Google Scholar]
- Jones, J.; Salazar, L.F. A review of HIV prevention studies that use social networking sites: Implications for recruitment, health promotion campaigns, and efficacy trials. AIDS Behav. 2016, 20, 2772–2781. [Google Scholar] [CrossRef]
- Brinn, M.P.; Carson, K.V.; Esterman, A.J.; Chang, A.B.; Smith, B.J. Cochrane review: Mass media interventions for preventing smoking in young people. Evid. Based Child Health A Cochrane Rev. J. 2012, 7, 86–144. [Google Scholar] [CrossRef]
- Allen, J.A.; Duke, J.C.; Davis, K.C.; Kim, A.E.; Nonnemaker, J.M.; Farrelly, M.C. Using mass media campaigns to reduce youth tobacco use: A review. Am. J. Health Promot. 2015, 30, e71–e82. [Google Scholar] [CrossRef]
- Bala, M.M.; Strzeszynski, L.; Topor-Madry, R. Mass media interventions for smoking cessation in adults. Cochrane Database Syst. Rev. 2017, 11, CD004704. [Google Scholar] [CrossRef]
- Mosdøl, A.; Lidal, I.B.; Straumann, G.H.; Vist, G.E. Targeted mass media interventions promoting healthy behaviours to reduce risk of non-communicable diseases in adult, ethnic minorities. Cochrane Database Syst. Rev. 2017, 2, CD011683. [Google Scholar] [CrossRef]
- Wakefield, M.A.; Loken, B.; Hornik, R.C. Use of mass media campaigns to change health behaviour. Lancet 2010, 376, 1261–1271. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pourkarim, M.; Nayebzadeh, S.; Alavian, S.M.; Hataminasab, S.H. Digital Marketing: A Unique Multidisciplinary Approach towards the Elimination of Viral Hepatitis. Pathogens 2022, 11, 626. https://doi.org/10.3390/pathogens11060626
Pourkarim M, Nayebzadeh S, Alavian SM, Hataminasab SH. Digital Marketing: A Unique Multidisciplinary Approach towards the Elimination of Viral Hepatitis. Pathogens. 2022; 11(6):626. https://doi.org/10.3390/pathogens11060626
Chicago/Turabian StylePourkarim, Mohammadreza, Shahnaz Nayebzadeh, Seyed Moayed Alavian, and Seyyed Hassan Hataminasab. 2022. "Digital Marketing: A Unique Multidisciplinary Approach towards the Elimination of Viral Hepatitis" Pathogens 11, no. 6: 626. https://doi.org/10.3390/pathogens11060626
APA StylePourkarim, M., Nayebzadeh, S., Alavian, S. M., & Hataminasab, S. H. (2022). Digital Marketing: A Unique Multidisciplinary Approach towards the Elimination of Viral Hepatitis. Pathogens, 11(6), 626. https://doi.org/10.3390/pathogens11060626






