Abstract
Cases of amoebic keratitis involving species other than Acanthamoeba are hypothesised to be underdiagnosed and poorly understood. Amoebic keratitis is debilitating and associated with chronic visual impairment. Understanding associated symptoms of non-Acanthamoeba amoebic keratitis could facilitate new diagnostic procedures and enable prompt treatment, ultimately leading to improved patient outcomes. Thus, a review of the literature was undertaken surrounding non-Acanthamoeba amoebic keratitis. Cases were geographically widespread and mostly confined to contact lens wearers ≤ 30 years old exposed to contaminated water sources and/or demonstrating poor lens hygiene. Vermamoeba vermiformis (previously Hartmanella vermiformis) was the most common causative agent, and a moderate number of mixed keratitis cases were also reported. A crucial disease indicator was early onset stromal deterioration/ulcerations, reported in 10 of the studies, usually only occurring in advanced Acanthamoeba keratitis. Mixed infections were the most difficult to treat, often requiring keratoplasty after unsuccessful combination treatment regimens. New diagnostic measures for non-Acanthamoeba amoebic keratitis should consider early onset stromal disease as a key disease indicator. Deep corneal scrapes are also necessary for accurate amoebic identification. Moreover, a combination approach to diagnosis is advised and should involve culture, microscopy and PCR techniques. In vitro drug sensitivity tests should also be conducted to help develop patient-specific treatment regimes.
Keywords:
keratitis; amoeba; hartmannella; acanthamoeba; vannella; vahlkampfia; vermamoeba; diagnosis; pathogenesis 1. Introduction
Amoebic keratitis is of growing clinical concern given the recent rise in cases globally and the difficulties associated with accurate diagnosis and treatment [1]. A recent outbreak of amoebic keratitis has been described in the UK, with other developed countries following similar trends [1,2,3,4,5]. Acanthamoeba spp. are most commonly associated with amoebic keratitis, and most cases can be linked to contact lens wear and poor contact lens hygiene [6,7,8]. Although not the only risk pathways of infection, exposure of contact lenses to contaminated water, overwearing lenses and improper cleaning and storage of lenses and cases (e.g., using tap water for cleaning purposes) enable amoebic adhesion and growth on lens surfaces and subsequently increase the risk of corneal infection [7].
While Acanthamoeba keratitis is the most common form of amoebic keratitis and as such has been the subject of extensive research, there are other potential contributing organisms that are less considered [1]. Despite a lack of conclusive evidence demonstrating that amoebae, with the exception of Acanthamoeba, are capable of causing keratitis in isolation, there have been several reported cases of positively identified non-Acanthamoeba amoeba species during keratitis infections documented in the literature. For example, Vermamoeba vermiformis (previously Hartmannella vermiformis), Vannella and Vahlkampfia species have all been associated with amoebic keratitis, and a lack of knowledge surrounding their potential for infections may hinder effective diagnostic or treatment protocols [9].
Because of the poorly understood role of non-Acanthamoeba amoebic keratitis, we have conducted an extensive review of the literature to further detail its prevalence, diagnoses, disease symptoms and treatments. In doing this, we aim to further the accuracy of diagnostic procedures that might aid in the rapid diagnosis and treatment of these pathogens.
2. Results
A total of 18 articles satisfied the inclusion guidelines set for this review (Figure 1), and key information was extracted from each article (Table 1). Studies were conducted in various locations worldwide, and study participants were diverse with respect to gender, age and history of contact lens wear (Table 2). Of all the identified case studies, participant specifics were only detailed in the study conducted by Hajialilo et al. [10]; consequently, they are excluded from Table 2’s participant section. Cases were described more frequently in females with 61.5% (8 female to 5 male) and also more frequent in participants within the 30-and-under age category (69.2% of cases, 9 ≤ 30 y/o to 4 > 30 y/o). Cases were much more apparent in contact lens wearers than in non-contact lens wearers, with 92% of cases linked to contact lens wear (61 to 5).
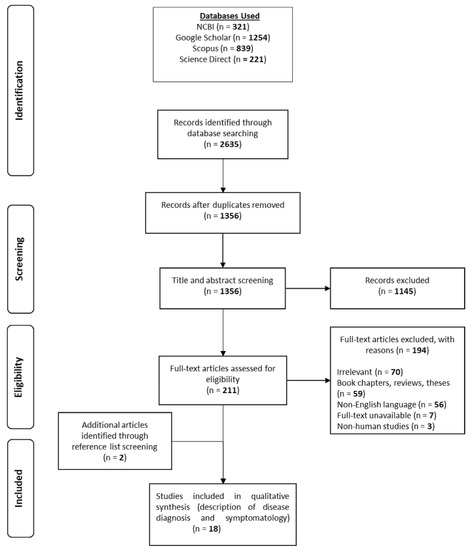
Figure 1.
PRISMA flow diagram.

Table 1.
Suspected or confirmed cases of non-Acanthamoeba amoebic keratitis (1995–2019).

Table 2.
Summary of study characteristics.
Of all infections, 21% were identified in conjunction with an additional amoebic infection, with half being a co-infection with an Acanthamoeba spp. Isolated infections with Vermamoeba vermiformis were most frequent, followed by isolated Vahlkampfia infections (53% and 23%, respectively). It should also be noted that in many cases, non-amoebic co-infective agents were identified during diagnoses, and in others, evidence of extensive screening to exclude the presence of additional microbial or viral pathogens was not provided. Thus, the role of these amoebae as causative agents of keratitis and not as vectors for the transmission of other microbial pathogens, as has been described in other free-living amoebae [27], remains inconclusive. Nonetheless, the most common clinical manifestations of non-Acanthamoeba amoebic keratitis included pain (61% of studies), inflammation and irritation (61%), stromal keratitis and ulcerations (56%), epithelial abnormalities (50%), ring infiltrates (50%), impaired vision (44%) and photophobia (44%) (Table 3).

Table 3.
Amoebic keratitis causative agents and symptoms described across all studies.
Diagnostic techniques vary between studies, with earlier studies relying primarily on culture and microscopy techniques to identify suspected pathogens. More recent diagnoses, however, have involved the use of 18s rRNA sequencing techniques to provide more accurate diagnoses with genus-specific primers (Figure 2). Additionally, temperature tolerance tests have been performed, as they are deemed to be good indicators of pathogenic virulence [26,28].
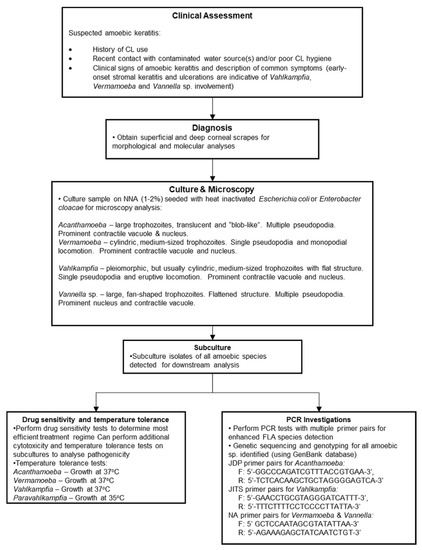
Figure 2.
Diagnostic flowchart for non-Acanthamoeba amoebic keratitis. Stromal involvement is a key disease indicator. Deep corneal scrapes can facilitate non-Acanthamoeba amoebic detection, and the use of multiple primer pairs can aid detection of multi-amoeba sp. in a sample.
Therapeutic approaches were broad and predominantly included drug combinations for all forms of amoebic keratitis (Table 1). This approach is similar to the approach taken with AK because no single anti-amoebic agent exists that can successfully eradicate all Acanthamoeba genotypes; hence, drug combinations are used [7,29]. Medical interventions included anti-amoebic agents (topical biguanides and aromatic diamidines), antibiotics, antifungals, antivirals and anti-inflammatory medications. Notably, several studies reported the need for keratoplasty due to poor treatment responses (Table 1) [12,13,14,17,18,22,24,26]. This emphasises the difficulty of finding an effective therapeutic agent to cure amoebic keratitis and highlights the possibility of drug resistance in other FLA besides Acanthamoeba.
3. Discussion
This review demonstrates that cases of non-Acanthamoeba amoebic keratitis are occurring and are geographically widespread; no single location showed a significantly higher incidence rate than any other (Table 2). Notably, however, disease incidence appears to be confined to developed countries, thus following a similar pattern to AK occurrences [7]. Although it is unclear, this might be the result of differences in diagnostic techniques between countries. In terms of patient demographics, Table 2 shows that the majority of individuals diagnosed with non-Acanthamoeba amoebic keratitis were ≤30 years old, and a significantly high proportion of positive cases were associated with contact lens wearers (61 cases vs. 5 non-CL wearers who had suffered ocular trauma). These findings also coincide with typical AK observations in which amoebic keratitis predominantly occurs in young, economically active adults who are most likely to wear contact lenses [2,7].
The similarities to AK infections complicate diagnoses. Generally, treatment outcomes of AK infections coincide with the speed by which accurate diagnoses can be made [7,30]; thus, a similar emphasis should be placed on rapid diagnosis in non-Acanthamoeba amoebic keratitis. Differentiation between amoebic infections is difficult; despite this, early onset stromal keratitis and ulcerations are indicative of Vahlkampfia, Vermamoeba and Vannella sp. involvement and could be useful during early observations (see Table 1) [9,11,13,14,15,17,19,20,22,24]. While microscopic and culture techniques can be applied during diagnostics, species identification using PCR tests remains the most accurate strategy for diagnosis and should be utilised at the earliest possible convenience [1]. We provide a more comprehensive diagnostic workflow for suspected amoebic keratitis in Figure 2. The presence of co-infectious agents in amoebic keratitis is common, and several non-amoebic species were also identified that can complicate treatment, diagnosis and the overall understanding of amoebic influence during infections [11,12,17,18]. For example, Kennedy et al. (1995) [11] reported growth of Staphylococcus aureus from corneal swabs, while Aitken et al. (1996) [12] noted the presence of yeast-like fungi on the corneal surface of the patient. Advances in molecular techniques allow more comprehensive screening for co-infectious agents and should be conducted in tandem with a traditional culture-based approach to assess the most appropriate course of action for the patient.
Despite the rarity of non-Acanthamoeba amoebic keratitis, the literature compiled within this review demonstrates that care must be applied during the initial diagnoses of amoebic keratitis to ensure the most suitable treatment method is applied. It is also worth noting the recent rise in AK infections globally [2,3,4,5] and that consideration must also be given as to whether non-Acanthamoeba causative agents of amoebic keratitis follow a similar trend. Overall, we demonstrate here that non-Acanthamoeba amoebic keratitis follows a similar pattern with regard to patient demographics and treatment regimens and that infections generally coincide with contact lens wear. We also highlight differences in disease presentation and methods of diagnoses. Despite its low prevalence, a broad-spectrum approach should be applied to the initial treatment of amoebic keratitis, which will necessitate further investigation into how AK therapies interact with other causative agents of amoebic keratitis. Furthermore, the role of non-Acanthamoeba amoebic species in keratitis infections has yet to be fully elucidated and, therefore, warrants additional research.
4. Materials and Methods
Four key databases were accessed: Scopus, Science Direct, Google Scholar and The National Center for Biotechnology Information (NCBI). The search criteria narrowly focused on Vahlkampfia, Vermamoeba (Hartmannella) and Vannella sp. and their involvement in keratitis. No date restrictions were applied due to the elusive nature of non-Acanthamoeba amoebic infections and the scarcity of relevant literature. Key words combined with Boolean operators and nested search strings were used to ensure results were confined to the topic of interest. Figure 1 details the flow path by which studies of non-Acanthamoeba amoebic keratitis infections were identified. All reported cases of keratitis associated with Vahlkampfia and Vermamoeba vermiformis (Hartmannella), coupled with descriptions of symptomatology and diagnostic measures, were included in this review. No restrictions to publication date, country, patient gender, race or age were applied. Studies selected for inclusion in this review were analysed against a Scottish Intercollegiate Guidelines Network flowchart [31], as recommended by the University of Strathclyde [32], to accurately determine study type. All studies were established to be case reports (CR) or case series (CS). Thereafter, each paper was quality-assessed against two critical appraisal tools provided by The Joanna Briggs Institute [33] and the Centre for Evidence-Based Management [34]. Data were presented as both total counts and percentages of overall data.
Author Contributions
R.M. designed the structure of the review article, critically reviewed and contributed to the manuscript; S.M. conducted the review of the literature and data analysis and contributed to the manuscript; F.L.H. conceived and designed the review article, critically reviewed the manuscript and coordinated the activities of co-authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lorenzo-Morales, J.; Khan, N.A.; Walochnik, J. An update on Acanthamoeba keratitis: Diagnosis, pathogenesis and treatment. Parasite 2015, 22, 10. [Google Scholar] [CrossRef] [PubMed]
- Carnt, N.; Hoffman, J.J.; Verma, S.; Hau, S.; Radford, C.F.; Minassian, D.C.; Dart, J.K.G. Acanthamoeba keratitis: Confirmation of the UK outbreak and a prospective case-control study identifying contributing risk factors. Br. J. Ophthalmol. 2018, 102, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- Randag, A.C.; Van Rooij, J.; Van Goor, A.T.; Verkerk, S.; Wisse, R.P.; Saelens, I.E.; Stoutenbeek, R.; van Dooren, B.T.; Cheng, Y.Y.; Eggink, C.A. The rising incidence of Acanthamoeba keratitis: A 7-year nationwide survey and clinical assessment of risk factors and functional outcomes. PLoS ONE 2019, 14, e0222092. [Google Scholar] [CrossRef]
- Höllhumer, R.; Keay, L.; Watson, S.L. Acanthamoeba keratitis in Australia: Demographics, associated factors, presentation and outcomes: A 15-year case review. Eye 2020, 34, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Scruggs, B.A.; Quist, T.S.; Salinas, J.L.; Greiner, M.A. Acanthamoeba keratitis cases—Iowa, 2002–2017. Morb. Mortal Wkly. Rep. 2019, 68, 448–449. [Google Scholar] [CrossRef]
- Rocha-Azevedo, B.D.; Tanowitz, H.B.; Marciano-Cabral, F. Diagnosis of Infections Caused by Pathogenic Free-Living Amoe-bae. Interdiscip. Perspect. Infect. Dis. 2009, 2009, 251406. [Google Scholar] [PubMed]
- de Lacerda, A.G.; Lira, M. Acanthamoeba keratitis: A review of biology, pathophysiology and epidemiology. Ophthalmic Physiol. Opt. 2020, 41, 116–129. [Google Scholar] [CrossRef]
- Fanselow, N.; Sirajuddin, N.; Yin, X.T.; Huang, A.J.; Stuart, P.M. Acanthamoeba Keratitis, Pathology, Diagnosis and Treatment. Pathology 2021, 10, 323. [Google Scholar] [CrossRef]
- Abedkhojasteh, H.; Niyyati, M.; Rahimi, F.; Heidari, M.; Farnia, S.; Rezaeian, M. First Report of Hartmannella keratitis in a Cosmetic Soft Contact Lens Wearer in Iran. Iran. J. Parasitol. 2013, 8, 481–485. [Google Scholar]
- Hajialilo, E.; Niyyati, M.; Solaymani, M.; Rezaeian, M. Pathogenic Free-Living Amoebae Isolated From Contact Lenses of Keratitis Patients. Iran. J. Parasitol. 2016, 10, 541–546. [Google Scholar]
- Kennedy, S.M.; Devine, P.; Hurley, C.; Ooi, Y.S.; Collum, L.M. Corneal infection associated with Hartmannella vermiformis in contact-lens wearer. Lancet 1995, 346, 637–638. [Google Scholar] [CrossRef]
- Aitken, D.; Hay, J.; Kinnear, F.B.; Kirkness, C.M.; Lee, W.R.; Seal, D.V. Amebic Keratitis in a Wearer of Disposable Contact Lenses due to a Mixed Vahlkampfia and Hartmannella Infection. Ophthalmology 1996, 103, 485–494. [Google Scholar] [CrossRef]
- Inoue, T.; Asari, S.; Tahara, K.; Hayashi, K.; Kiritoshi, A.; Shimomura, Y. Acanthamoeba keratitis with symbiosis of Hartmannella amoeba. Am. J. Oph-Thalmology 1998, 125, 721–723. [Google Scholar] [CrossRef]
- Aimard, L.; Brasseur, P.; Favennec, L.; Perrine, D.; Watt, L.; Brasseur, G. Amebic Keratitis Due to a Mixed Infection with Acanthamoeba and Hartmannella Species. Clin. Infect. Dis. 1998, 26, 187–188. [Google Scholar] [CrossRef][Green Version]
- Alexandrakis, G.; Miller, D.; Huang, A.J. Amebic keratitis due to Vahlkampfia infection following corneal trauma. Arch. Ophthalmol. 1998, 116, 950–951. [Google Scholar]
- Bennett, H.G.B.; Hay, J.; Kirkness, C.M.; Seal, D.V.; Devonshire, P. Antimicrobial management of presumed microbial keratitis: Guidelines for treatment of central and peripheral ulcers. Br. J. Ophthalmol. 1998, 82, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Michel, R.; Schmid, E.N.; Böker, T.; Hager, D.G.; Müller, K.-D.; Hoffmann, R.; Seitz, H.M. Vannella sp. harboring Microsporidia-like organisms isolated from the contact lens and inflamed eye of a female keratitis patient. Parasitol. Res. 2000, 86, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P. Mechanism of intrusion of a microsporidian-like organism into the nucleus of host amoebae (Vannella sp.) isolated from a keratitis patient. Parasitol. Res. 2007, 101, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Morales, J.; Martínez-Carretero, E.; Batista, N.; Álvarez-Marín, J.; Bahaya, Y.; Walochnik, J.; Valladares, B. Early diagnosis of amoebic keratitis due to a mixed infection with Acanthamoeba and Hartmannella. Parasitol. Res. 2007, 102, 167–169. [Google Scholar] [CrossRef]
- Yera, H.; Zamfir, O.; Bourcier, T.; Viscogliosi, E.; Noël, C.; Dupouy-Camet, J.; Chaumeil, C. The genotypic characterisation of Acanthamoeba isolates from human ocular sam-ples. Br. J. Ophthalmol. 2008, 92, 1139–1141. [Google Scholar] [CrossRef]
- Ozkoc, S.; Tuncay, S.; Delibas, S.B.; Akisu, C.; Ozbek, Z.; Durak, I.; Walochnik, J. Identification of Acanthamoeba genotype T4 and Paravahlkampfia sp. from two clinical samples. J. Med. Microbiol. 2008, 57, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Niyyati, M.; Lorenzo-Morales, J.; Rezaie, S.; Rahimi, F.; Martín-Navarro, C.M.; Mohebali, M.; Maghsood, A.H.; Farnia, S.; Valladares, B.; Rezaeian, M. First report of a mixed infection due to Acanthamoeba genotype T3 and Vahlkampfia in a cosmetic soft contact lens wearer in Iran. Exp. Parasitol. 2010, 126, 89–90. [Google Scholar] [CrossRef] [PubMed]
- Mattana, A.; Pinna, A.; Erre, G.; Fiori, P.L.; Cappuccinelli, P. Biological characterization of free-living amoebae isolated from cases of amoebic keratitis in Sassari. Mappe Parassitol. 2012, 18, 49. [Google Scholar]
- Arnalich-Montiel, F.; Lorenzo-Morales, J.; Irigoyen, C.; Morcillo-Laiz, R.; López-Vélez, R.; Muñoz-Negrete, F.; Piñero, J.E.; Valladares, B. Co-isolation of Vahlkampfia and Acanthamoeba in Acanthamoe-ba-Like Keratitis in a Spanish Population. Cornea 2013, 32, 608–614. [Google Scholar] [CrossRef]
- Tolba, M.E.M.; Huseein, E.A.M.; Farrag, H.M.M.; Mohamed, H.E.D.; Kobayashi, S.; Suzuki, J.; Ali, T.A.M.; Sugano, S. Allovahlkampfia spelaea Causing Keratitis in Humans. PLoS Negl. Trop. Dis. 2016, 10, e0004841. [Google Scholar] [CrossRef] [PubMed]
- Pinna, A.; Porcu, T.; Boscia, F.; Cano, A.; Erre, G.; Mattana, A. Free-Living Amoebae Keratitis. Cornea 2017, 36, 785–790. [Google Scholar] [CrossRef]
- Henriquez, F.L.; Mooney, R.; Bandel, T.; Giammarini, E.; Zeroual, M.; Fiori, P.L.; Margarita, V.; Rappelli, P.; Dessì, D. Paradigms of Protist/Bacteria Symbioses Affecting Human Health: Acanthamoeba species and Trichomonas vaginalis. Front. Microbiol. 2021, 11, 616213. [Google Scholar] [CrossRef]
- Griffin, J.L. Temperature Tolerance of Pathogenic and Nonpathogenic Free-Living Amoebas. Science 1972, 178, 869–870. [Google Scholar] [CrossRef]
- Rayamajhee, B.; Willcox, M.D.; Henriquez, F.L.; Petsoglou, C.; Carnt, N. Acanthamoeba keratitis: An increasingly common infectious disease of the cornea. Lancet Microbe 2021, 2, e345–e346. [Google Scholar] [CrossRef]
- Maycock, N.J.R.; Jayaswal, R. Update on Acanthamoeba Keratitis. Cornea 2016, 35, 713–720. [Google Scholar] [CrossRef]
- Scottish Intercollegiate Guidelines Network. Algorithm for Classifying Study Design for Questions of Effectiveness. 2021. Available online: https://www.sign.ac.uk/assets/study_design.pdf (accessed on 17 July 2021).
- University of Strathclyde. Systematic Review Steps. 2020. Available online: https://guides.lib.strath.ac.uk/systematic/steps (accessed on 10 July 2021).
- The Joanna Briggs Institute. Checklist for Case Control Studies. Available online: https://jbi.global/critical-appraisal-tools (accessed on 1 May 2021).
- Centre for Evidence Based Management. Critical Appraisal. 2019. Available online: https://cebma.org/resources-and-tools/what-is-critical-appraisal/ (accessed on 17 July 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).