Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Registration and Reporting
2.2. Search Strategy and Databases
2.3. Study Selection and Data Extraction
2.4. Risk of Bias and Publication Bias
2.5. Data Synthesis
3. Results
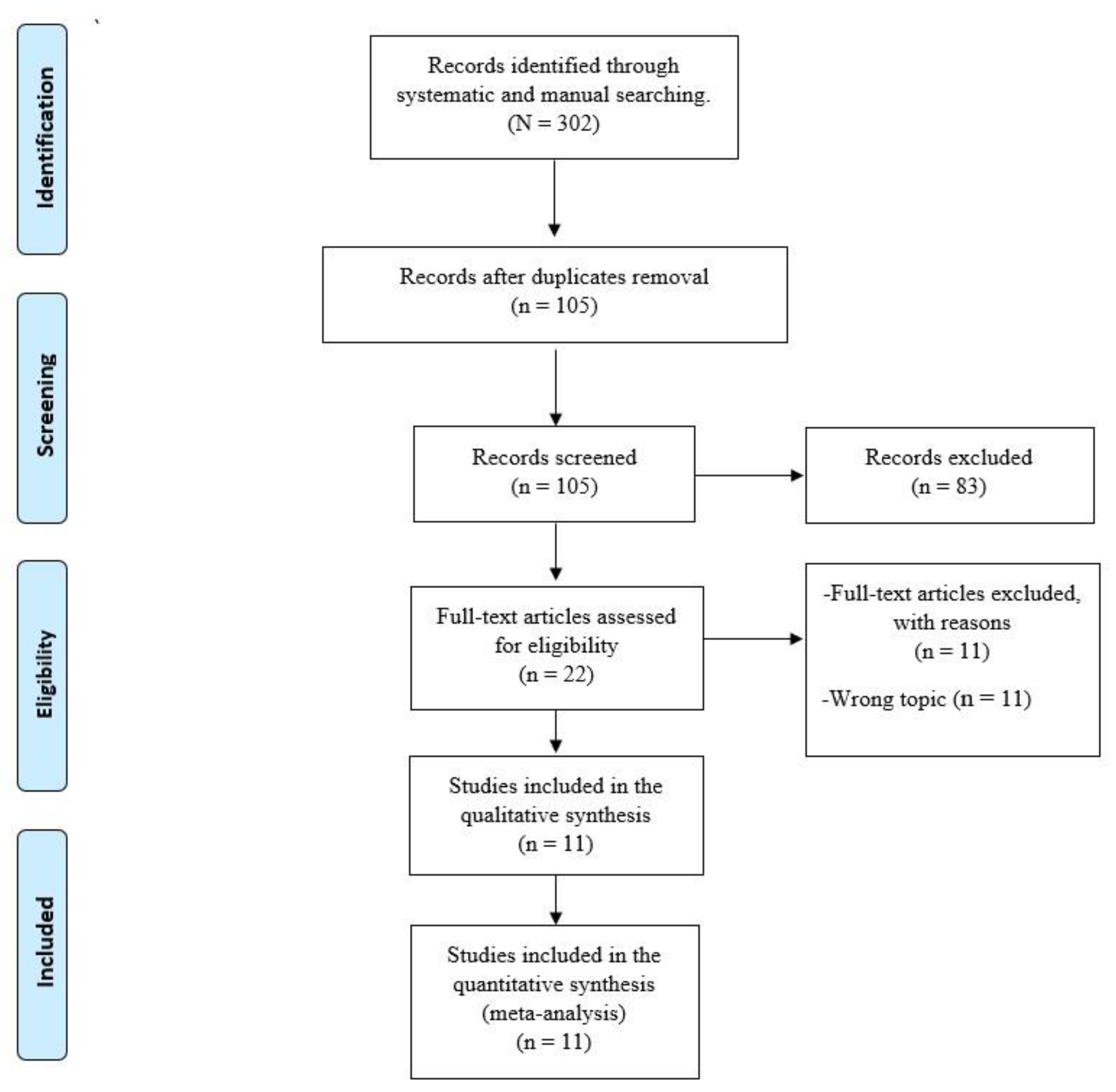
3.1. Study Selection
3.2. Study Characteristics
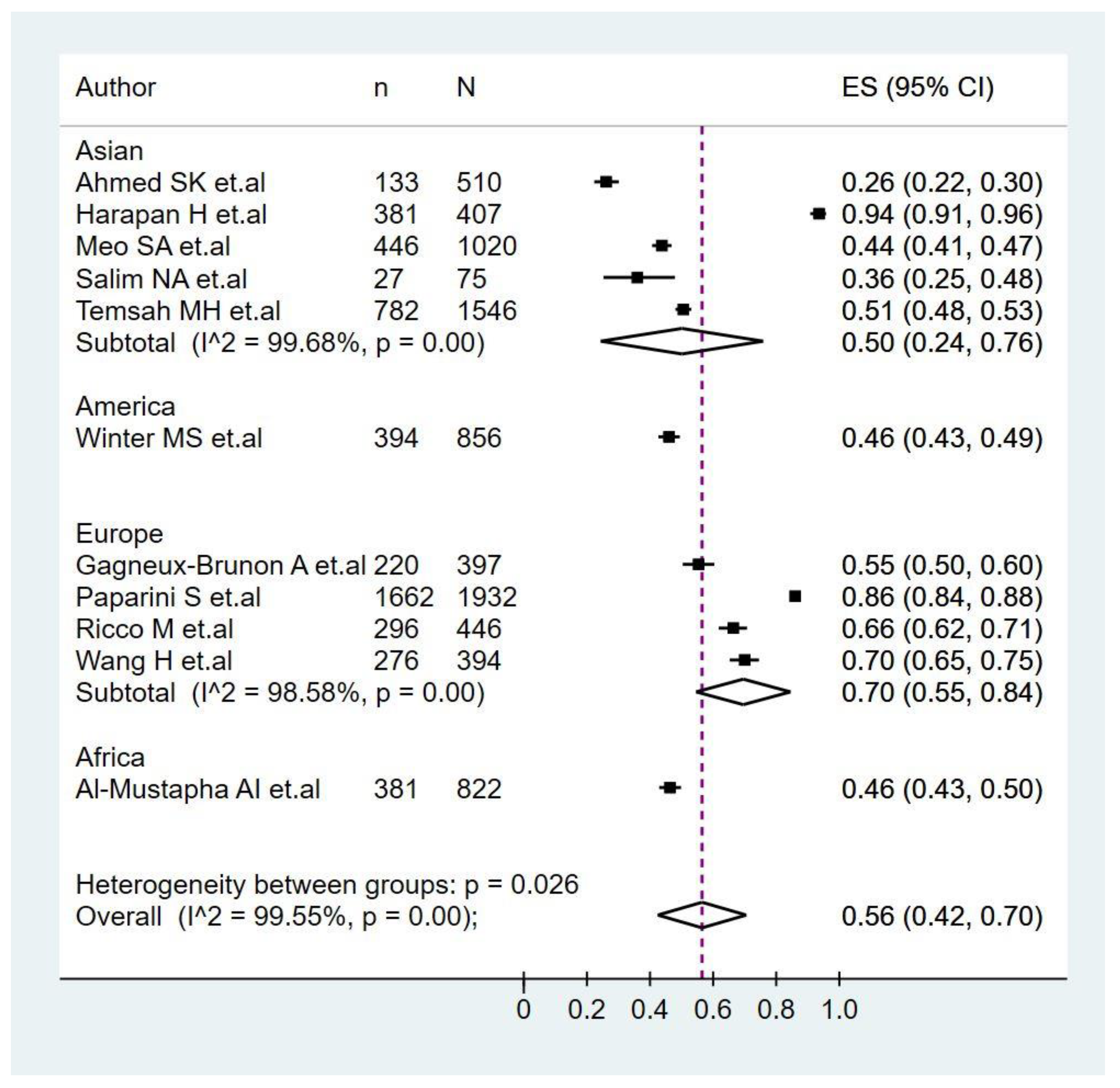
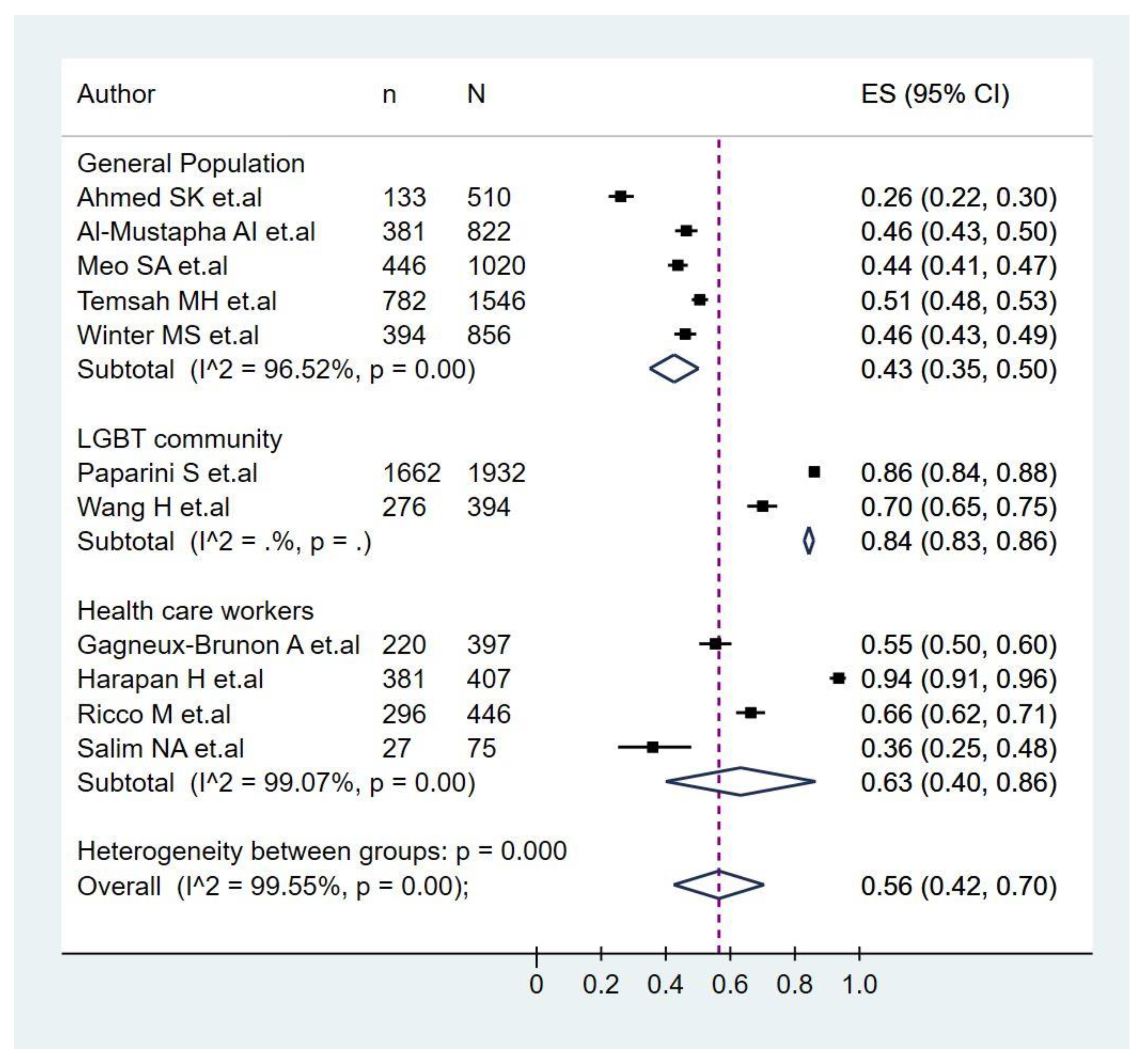
3.3. Prevalence of Monkeypox Vaccination Acceptance
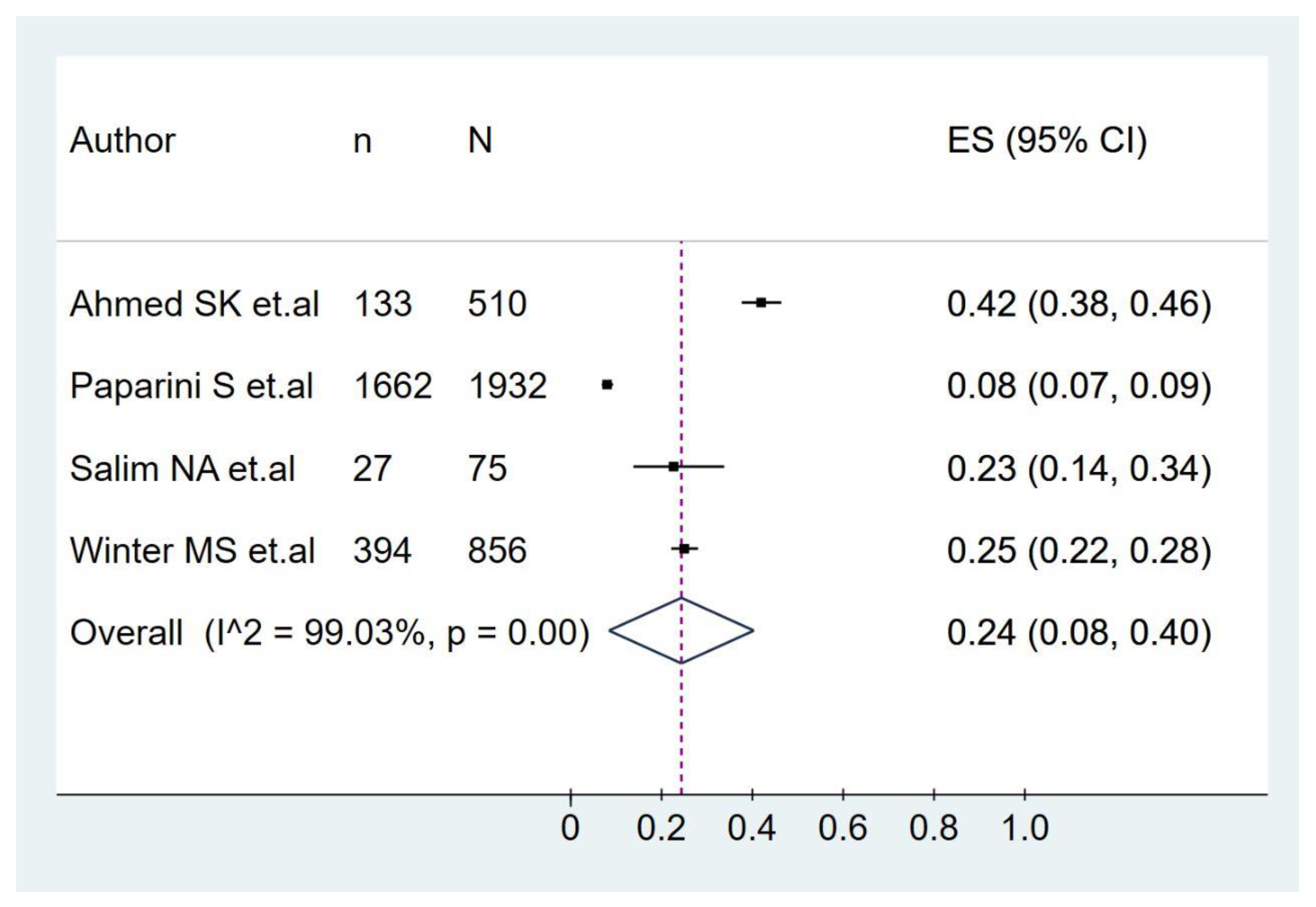
3.4. Prevalence of Monkeypox Vaccination Hesitancy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- León-Figueroa, D.A.; Bonilla-Aldana, D.K.; Pachar, M.; Romaní, L.; Saldaña-Cumpa, H.M.; Anchay-Zuloeta, C.; Diaz-Torres, M.; Franco-Paredes, C.; Suárez, J.A.; Ramirez, J.D.; et al. The never ending global emergence of viral zoonoses after COVID-19? The rising concern of monkeypox in Europe, North America and beyond. Travel Med. Infect. Dis. 2022, 49, 102362. [Google Scholar] [CrossRef] [PubMed]
- Sah, R.; Reda, A.; Lashin, B.I.; Mohanty, A.; Abdelaal, A.; Rodriguez-Morales, A.J. Public health emergencies of international concernin the 21st century. Ann. Med. Surg. 2022, 81, 104417. [Google Scholar] [CrossRef] [PubMed]
- Benites-Zapata, V.A.; Ulloque-Badaracco, J.R.; Alarcon-Braga, E.A.; Hernandez-Bustamante, E.A.; Mosquera-Rojas, M.D.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Clinical features, hospitalisation and deaths associated with monkeypox: A systematic review and meta-analysis. Ann. Clin. Microbiol. Antimicrob. 2022, 21, 36. [Google Scholar] [CrossRef]
- Farahat, R.A.; Abdelaal, A.; Shah, J.; Ghozy, S.; Sah, R.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J.; McHugh, T.D.; Leblebicioglu, H. Monkeypox outbreaks during COVID-19 pandemic: Are we looking at an independent phenomenon or an overlapping pandemic? Ann. Clin. Microbiol. Antimicrob. 2022, 21, 26. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Lopardo, G.; Verbanaz, S.; Orduna, T.; Lloveras, S.; Azeñas-Burgoa, J.M.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Barbosa, A.N.; Diaz-Quijano, F.; et al. Latin America: Situation and preparedness facing the multi-country human monkeypox outbreak. Lancet Reg. Health Am. 2022, 13, 100318. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; Rodríguez-Morales, A.J.; Franco-Paredes, C.; Chastain, D.B.; Gharamti, A.A.; Vargas Barahona, L.; Henao-Martínez, A.F. Monkeypox—A description of the clinical progression of skin lesions: A case report from Colorado, USA. Ther. Adv. Infect Dis. 2022, 9, 20499361221117726. [Google Scholar] [CrossRef]
- Farahat, R.A.; Sah, R.; El-Sakka, A.A.; Benmelouka, A.Y.; Kundu, M.; Labieb, F.; Shaheen, R.S.; Abdelaal, A.; Abdelazeem, B.; Bonilla-Aldana, D.K.; et al. Human monkeypox disease (MPX). Infez. Med. 2022, 30, 372–391. [Google Scholar] [CrossRef]
- Sah, R.; Mohanty, A.; Abdelaal, A.; Reda, A.; Rodriguez-Morales, A.J.; Henao-Martinez, A.F. First Monkeypox deaths outside Africa: No room for complacency. Adv. Infect Dis. 2022, 9, 20499361221124027. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; Sarmiento, J.; Bonilla-Aldana, D.K.; Rodríguez-Morales, A.J. Monkeypox goes viral: Measuring the misinformation outbreak on Twitter. J. Infect. Dev. Ctries. 2022, 16, 1218–1220. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; Galvis-Cataño, L.M.; Arias-Rodríguez, D.; Romero-Dager, C.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. YouTube and 2022 Monkeypox outbreak: Opportunities for awareness and infection control. J. Hosp. Infect. 2022. [Google Scholar] [CrossRef]
- Sah, R.; Abdelaal, A.; Asija, A.; Basnyat, S.; Sedhai, Y.R.; Ghimire, S.; Sah, S.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Monkeypox virus containment: The application of ring vaccination and possible challenges. J. Travel Med. 2022, 29, taac085. [Google Scholar] [CrossRef]
- Abdelaal, A.; Reda, A.; Lashin, B.I.; Katamesh, B.E.; Brakat, A.M.; Al-Manaseer, B.M.; Kaur, S.; Asija, A.; Patel, N.K.; Basnyat, S.; et al. Preventing the Next Pandemic: Is Live Vaccine Efficacious against Monkeypox, or Is There a Need for Killed Virus and mRNA Vaccines? Vaccines 2022, 10, 1419. [Google Scholar] [CrossRef]
- Alarcón-Braga, E.A.; Hernandez-Bustamante, E.A.; Salazar-Valdivia, F.E.; Valdez-Cornejo, V.A.; Mosquera-Rojas, M.D.; Ulloque-Badaracco, J.R.; Rondon-Saldaña, J.C.; Zafra-Tanaka, J.H. Acceptance towards COVID-19 vaccination in Latin America and the Caribbean: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2022, 49, 102369. [Google Scholar] [CrossRef]
- Benites-Zapata, V.A.; Herrera-Añazco, P.; Benites-Meza, J.K.; Bonilla-Aguilar, K.; Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Hernandez, A.V. Prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19: A comparative analysis in Colombia and Peru. Vaccine X 2022, 12, 100198. [Google Scholar] [CrossRef]
- Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Toro-Huamanchumo, C.J.; Rodriguez-Morales, A.J.; Hernandez, A.V.; Benites-Zapata, V.A. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med. Infect. Dis. 2021, 41, 102059. [Google Scholar] [CrossRef]
- Mezones-Holguin, E.; Al-kassab-Córdova, A.; Maguiña, J.L.; Rodriguez-Morales, A.J. Vaccination coverage and preventable diseases in Peru: Reflections on the first diphtheria case in two decades during the midst of COVID-19 pandemic. Travel Med. Infect. Dis. 2021, 40, 101956. [Google Scholar] [CrossRef]
- Russo, A.T.; Berhanu, A.; Bigger, C.B.; Prigge, J.; Silvera, P.M.; Grosenbach, D.W.; Hruby, D. Co-administration of tecovirimat and ACAM2000™ in non-human primates: Effect of tecovirimat treatment on ACAM2000 immunogenicity and efficacy versus lethal monkeypox virus challenge. Vaccine 2020, 38, 644–654. [Google Scholar] [CrossRef]
- Bendezu-Quispe, G.; Benites-Meza, J.K.; Urrunaga-Pastor, D.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Toro-Huamanchumo, C.J.; Hernandez, A.V.; Benites-Zapata, V.A. Mass Media Use to Learn About COVID-19 and the Non-intention to Be Vaccinated Against COVID-19 in Latin America and Caribbean Countries. Front. Med. 2022, 9, 877764. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Franco, O.H. Public trust, misinformation and COVID-19 vaccination willingness in Latin America and the Caribbean: Today’s key challenges. Lancet Reg. Health Am. 2021, 3, 100073. [Google Scholar] [CrossRef]
- Mangla, S.; Zohra Makkia, F.T.; Pathak, A.K.; Robinson, R.; Sultana, N.; Koonisetty, K.S.; Karamehic-Muratovic, A.; Nguyen, U.D.T.; Rodriguez-Morales, A.J.; Sanchez-Duque, J.A.; et al. COVID-19 Vaccine Hesitancy and Emerging Variants: Evidence from Six Countries. Behav. Sci. 2021, 11, 148. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; López-López, M.; Ruiz-González, C.E.; Turbay-Caballero, V.; Sacoto, D.H.; Caldera-Caballero, M.; Bravo, H.; Sarmiento, J.; Rodriguez-Morales, A.J. Willingness to receive COVID-19 vaccination in people living with HIV/AIDS from Latin America. Int. J. STD AIDS 2022, 33, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Setiawan, A.M.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; et al. Acceptance and willingness to pay for a hypothetical vaccine against monkeypox viral infection among frontline physicians: A cross-sectional study in Indonesia. Vaccine 2020, 38, 6800–6806. [Google Scholar] [CrossRef] [PubMed]
- Ajman, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Alhaboob, A.; Altawil, E.S.; Alshahrani, F.; Alrabiaah, A.; Alaraj, A.; Alkriadees, K.; et al. Healthcare Workers’ Worries and Monkeypox Vaccine Advocacy during the First Month of the WHO Monkeypox Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines 2022, 10, 1408. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, N.Z.; Alzahrani, F.; Alarifi, A.M.; Algethami, M.R.; Alhumam, M.N.; Ayied, H.A.M.; Awan, A.Z.; Almutairi, A.F.; Bamakhrama, S.A.; Almushari, B.S.; et al. Assessment of Knowledge of Monkeypox Viral Infection among the General Population in Saudi Arabia. Pathogens 2022, 11, 904. [Google Scholar] [CrossRef] [PubMed]
- Ansari, Z.; Ramzan, H.; Shakeel, R. Is there a need of monkeypox vaccine amidst the hesitancy of COVID-19 immunization in Pakistan? Ann. Med. Surg. 2022, 81, 104391. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.J.; Marshall, G.S. Navigating parental vaccine hesitancy. Pediatr. Ann. 2010, 39, 476–482. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Barker, T.H.; Migliavaca, C.B.; Stein, C.; Colpani, V.; Falavigna, M.; Aromataris, E.; Munn, Z. Conducting proportional meta-analysis in different types of systematic reviews: A guide for synthesisers of evidence. BMC Med. Res. Methodol. 2021, 21, 189. [Google Scholar] [CrossRef]
- Hunter, J.P.; Saratzis, A.; Sutton, A.J.; Boucher, R.H.; Sayers, R.D.; Bown, M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014, 67, 897–903. [Google Scholar] [CrossRef]
- Ahmed, S.K.; Abdulqadirb, S.O.; Omar, R.M.; Hussein, S.H.; M-Amin, H.I.; Chandran, D.; Sharma, A.K.; Dhama, K.; Ahmed, Z.K.; Essa, R.A.; et al. Study of knowledge, attitude and anxiety in Kurdistan-region of Iraqi population during the monkeypox outbreak in 2022: An online cross-sectional study. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Malik, A.A.; Winters, M.S.; Omer, S.B. Attitudes of the US general public towards Monkeypox. medRxiv 2022. [Google Scholar] [CrossRef]
- Wang, H.; D’Abreu De Paulo, K.J.I.; Gültzow, T.; Zimmermann, H.M.L.; Jonas, K.J. Monkeypox self-diagnosis abilities, determinants of vaccination and self-isolation intention after diagnosis among MSM, the Netherlands, July 2022. Eurosurveillance 2022, 27, 2200603. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Dauby, N.; Launay, O.; Botelho-Nevers, E. Intentions to get vaccinated against Monkeypox in Healthcare workers in France and Belgium correlates with attitudes toward COVID-19 vaccination. medRxiv 2022. [Google Scholar] [CrossRef]
- Riccò, M.; Ferraro, P.; Camisa, V.; Satta, E.; Zaniboni, A.; Ranzieri, S.; Baldassarre, A.; Zaffina, S.; Marchesi, F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop. Med. Int. Health 2022, 7, 135. [Google Scholar] [CrossRef]
- Meo, S.A.; Al-Khlaiwi, T.; Aljofan, Z.F.; Alanazi, A.I.; Meo, A.S. Public Perceptions of the Emerging Human Monkeypox Disease and Vaccination in Riyadh, Saudi Arabia: A Cross-Sectional Study. Vaccines 2022, 10, 1534. [Google Scholar] [CrossRef]
- Temsah, M.H.; Aljamaan, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Al-Barag, A.; Alhaboob, A.; Bahabri, N.; Alshahrani, F.; Alrabiaah, A.; et al. Monkeypox caused less worry than COVID-19 among the general population during the first month of the WHO Monkeypox alert: Experience from Saudi Arabia. Travel Med. Infect. Dis. 2022, 49, 102426. [Google Scholar] [CrossRef]
- Paparini, S.; Whitacre, R.; Smuk, M.; Thornhill, J.; Mwendera, C.; Strachan, S.; Nutland, W.; Orkin, C. Public understanding, awareness, and response to monkeypox virus outbreak: A cross-sectional survey of the most affected communities in the United Kingdom during the 2022 public health emergency. medRxiv 2022. [Google Scholar] [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S.; et al. Physicians’ willingness to be vaccinated with a smallpox vaccine to prevent monkeypox viral infection: A cross-sectional study in Indonesia. Clin. Epidemiol. Glob. Health 2020, 8, 1259–1263. [Google Scholar] [CrossRef] [PubMed]
- Al-Mustapha, A.I.; Sikiru, N.A.; Kolawole, B.; Oyewo, M.; Ahmed, H.; Odukoya, A.; Ogundijo, O.A.; Asiegbu, E.C.; Nanven, M.B.; Lawal-Atolagbe, T.; et al. A Cross-sectional Survey of Public Knowledge of the Monkeypox Disease in Nigeria. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Salim, N.A.; Septadina, I.S.; Permata, M.; Hudari, H. Knowledge, attitude, and perception of anticipating 2022 global human monkeypox infection among internal medicine residents at Palembang Indonesia: An online survey. J. Ilmu Kedokt Kesehat J. Med. Health Sci. 2022, 9, 253–262. [Google Scholar] [CrossRef]
- Gates, B. How to Prevent the Next Pandemic; Knopf: Seatle, WA, USA, 2022. [Google Scholar]
- Sah, R.; Mohanty, A.; Reda, A.; Lashin, B.I.; Abdelaal, A.; Rath, R.S.; Rodriguez-Morales, A.J. Monkeypox: A potential pandemic at door of Asia. Ann. Med. Surg. 2022, 81, 104509. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Morales, A.J.; Ortiz-Martínez, Y.; Bonilla-Aldana, D.K. What has been researched about monkeypox? a bibliometric analysis of an old zoonotic virus causing global concern. New Microbes New Infect. 2022, 47, 100993. [Google Scholar] [CrossRef]
- Haider, N.; Guitian, J.; Simons, D.; Asogun, D.; Ansumana, R.; Honeyborne, I.; Velavan, T.P.; Ntoumi, F.; Valdoleiros, S.R.; Petersen, E.; et al. Increased outbreaks of monkeypox highlight gaps in actual disease burden in Sub-Saharan Africa and in animal reservoirs. Int. J. Infect. Dis. IJID 2022, 122, 107–111. [Google Scholar] [CrossRef]
- Al-Musa, A.; Chou, J.; LaBere, B. The resurgence of a neglected orthopoxvirus: Immunologic and clinical aspects of monkeypox virus infections over the past six decades. Clin. Immunol. 2022, 243, 109108. [Google Scholar] [CrossRef]
- World Health Organization. Multi-Country Monkeypox Outbreak: Situation Update. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON390 (accessed on 14 October 2022).
- Guagliardo, S.A.J.; Monroe, B.; Moundjoa, C.; Athanase, A.; Okpu, G.; Burgado, J.; Townsend, M.B.; Satheshkumar, P.S.; Epperson, S.; Doty, J.B.; et al. Asymptomatic Orthopoxvirus Circulation in Humans in the Wake of a Monkeypox Outbreak among Chimpanzees in Cameroon. Am. J. Trop. Med. Hyg. 2020, 102, 206–212. [Google Scholar] [CrossRef] [Green Version]
- De Albuquerque, T.R.; Macedo, L.F.R.; de Oliveira, E.G.; Neto, M.L.R.; de Menezes, I.R.A. Vaccination for COVID-19 in children: Denialism or misinformation? J. Pediatr. Nurs. 2022, 64, 141–142. [Google Scholar] [CrossRef]
- De Saint Laurent, C.; Murphy, G.; Hegarty, K.; Greene, C.M. Measuring the effects of misinformation exposure and beliefs on behavioural intentions: A COVID-19 vaccination study. Cogn. Res. Princ. Implic. 2022, 7, 87. [Google Scholar] [CrossRef]
- Ganie, A.U.R.; Mukhter, I. Misinformation induced anxieties and fear affecting vaccination programs: Challenge for COVID-19 vaccination program. J. Fam. Med. Prim. Care 2022, 11, 405–406. [Google Scholar] [CrossRef] [PubMed]
- Kalayou, M.H.; Awol, S.M. Myth and Misinformation on COVID-19 Vaccine: The Possible Impact on Vaccination Refusal Among People of Northeast Ethiopia: A Community-Based Research. Risk Manag. Health Policy 2022, 15, 1859–1868. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Lee, C.J.; Ihm, J.; Kim, Y. A comprehensive examination of association between belief in vaccine misinformation and vaccination intention in the COVID-19 context. J. Health Commun. 2022, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Li, H.O.; Pastukhova, E.; Brandts-Longtin, O.; Tan, M.G.; Kirchhof, M.G. YouTube as a source of misinformation on COVID-19 vaccination: A systematic analysis. BMJ Glob. Health 2022, 7. [Google Scholar] [CrossRef]
- Pierri, F.; Perry, B.L.; DeVerna, M.R.; Yang, K.C.; Flammini, A.; Menczer, F.; Bryden, J. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci. Rep. 2022, 12, 5966. [Google Scholar] [CrossRef]
- Sah, R.; Mohanty, A.; Reda, A.; Padhi, B.K.; Rodriguez-Morales, A.J. Stigma during monkeypox outbreak. Front. Public Health 2022, 10, 1023519. [Google Scholar] [CrossRef]
- Narain, K.; Mkhize, N. Monkeypox in South Africa: The need for responsible messaging to avoid stigmatising the LGBTI community. South Afr. Med. J. Suid-Afrik. Tydskr. Geneeskd. 2022, 112, 741. [Google Scholar] [CrossRef]
- Gandrakota, N.; Lee, H.; Nwosu, O.; Kulshreshtha, A. Monkeypox coinfection with Neurosyphilis in a transgender with HIV in Atlanta, USA. Travel Med. Infect. Dis. 2022, 50, 102454. [Google Scholar] [CrossRef]
- Hubach, R.D.; Owens, C. Findings on the Monkeypox Exposure Mitigation Strategies Employed by Men Who Have Sex with Men and Transgender Women in the United States. Arch. Sex. Behav. 2022, 1–6. [Google Scholar] [CrossRef]
- Reda, A.; Abdelaal, A.; Brakat, A.M.; Lashin, B.I.; Abouelkheir, M.; Abdelazeem, B.; Rodriguez-Morales, A.J.; Sah, R. Monkeypox Viral Detection In Semen Specimens of Confirmed Cases: A Systematic Review and Meta-Analysis. J. Med. Virol. 2022. [Google Scholar] [CrossRef]
- Ortiz-Martínez, Y.; Saul, Z.; Hutchinson, K.A.; Miljkovic, G.; Rodríguez-Morales, A.J. Not Just Differential Diagnoses… Importance of Sexually Transmitted Infections as Coinfections with Monkeypox Amidst the Outbreak. Int. J. STD AIDS 2022, 9564624221127746. [Google Scholar] [CrossRef]
- Alvarado-Socarras, J.L.; Vesga-Varela, A.L.; Quintero-Lesmes, D.C.; Fama-Pereira, M.M.; Serrano-Diaz, N.C.; Vasco, M.; Carballo-Zarate, V.; Zambrano, L.I.; Paniz-Mondolfi, A.; Rodriguez-Morales, A.J. Perception of COVID-19 Vaccination Amongst Physicians in Colombia. Vaccines 2021, 9, 287. [Google Scholar] [CrossRef]
- Ubale, M.R.; Bagle, T.R.; Gaikwad, S.; Baviskar, P.A.; Nanoty, V.A. Attitude and perception of COVID-19 vaccines in healthcare workers. J. Fam. Med. Prim. Care 2022, 11, 2448–2455. [Google Scholar] [CrossRef]
- Reyes-Urueña, J.; D’Ambrosio, A.; Croci, R.; Bluemel, B.; Cenciarelli, O.; Pharris, A.; Dukers-Muijrers, N.; Nutland, W.; Niaupari, S.; Badran, J.; et al. High monkeypox vaccine acceptance among male users of smartphone-based online gay-dating apps in Europe, 30 July to 12 August 2022. Euro Surveill. 2022, 27, 2200757. [Google Scholar] [CrossRef] [PubMed]
- Zaeck, L.M.; Lamers, M.M.; Verstrepen, B.E.; Bestebroer, T.M.; van Royen, M.E.; Götz, H.; Shamier, M.C.; van Leeuwen, L.P.M.; Schmitz, K.S.; Alblas, K.; et al. Low levels of monkeypox virus neutralizing antibodies after MVA-BN vaccination in healthy individuals. Nat. Med. 2022. [Google Scholar] [CrossRef] [PubMed]

| Author | Year of Publication | Country | Target Population | Participants (Male/Female/Nonbinary) | Age (Mean ± SD or Age Ranges) | Survey Type | Data Collection Date | Response Recorded as Vaccine Acceptance | Prevalence of Vaccination Acceptance | Prevalence of Monkeypox Vaccination Hesitancy |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmed SK, et al. [33] | 2022 | Iraq | General population | 510 (277/233) | 18–57 | Online survey | 27 July 2022–30 July 2022 | Yes | 26% | 42% |
| Winter MS, et al. [34] | 2022 | United States | General population | 856 (419/437) | NR | Online survey | June 2022 | Yes | 46% | 25% |
| Wang H, et al. [35] | 2022 | Netherlands | LGBTI community | 394 (394/0) | NR | Online survey | July 2022 | High/very high vaccination intention (scale 4 and 5) | 70% | NR |
| Gagneux-Brunon A, et al. [36] | 2022 | France and Belgium | Healthcare workers | 397 (101/296) | 43.3(12) | Online survey | 15 June 2022–8 August 2022 | Intention to get vaccinated | 55.4% | NR |
| Salim NA, et al. [43] | 2022 | Indonesia | Healthcare workers | 75 (49/26) | 26–38 | Online survey | 2 August 2022–5 August 2022 | Yes | 36% | 22.70% |
| Ricco M, et al. [37] | 2022 | Italy | Healthcare workers | 446 (149) | 42.9 (10) | Online survey | 4 May 2022–31 May 2022 | Totally Agree/Agree | 66.36% | NR |
| Meo SA et al. [38] | 2022 | Saudi Arabia | General population | 1020 (466/554) | NR | Online survey | 15 May 2022–15 July 2022 | Yes | 43.7% | NR |
| Temsah MH, et al. [39] | 2022 | Saudi Arabia | General population | 1546 (650/896) | NR | Online survey | 27 May 2022–5 June 2022 | Yes | 50.6% | NR |
| Paparini S, et al. [40] | 2022 | United Kingdom | LGBTI community | 1932 (1750/88/94) | NR | Online survey | 15 June 2022–27 July 2022 | Yes | 86% | 8% |
| Harapan H, et al. [41] | 2020 | Indonesia | Healthcare workers | 407 (128/279) | NR | Online survey | 25 May 2019–25 July 2019 | Yes | 93.6% | NR |
| Al-Mustapha AI, et al. [42] | 2022 | Nigeria | General population | 822 (472/342/8) | NR | Online survey | 16 August 2022–29 August 2022 | NR | 46.37% | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulloque-Badaracco, J.R.; Alarcón-Braga, E.A.; Hernandez-Bustamante, E.A.; Al-kassab-Córdova, A.; Benites-Zapata, V.A.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis. Pathogens 2022, 11, 1248. https://doi.org/10.3390/pathogens11111248
Ulloque-Badaracco JR, Alarcón-Braga EA, Hernandez-Bustamante EA, Al-kassab-Córdova A, Benites-Zapata VA, Bonilla-Aldana DK, Rodriguez-Morales AJ. Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis. Pathogens. 2022; 11(11):1248. https://doi.org/10.3390/pathogens11111248
Chicago/Turabian StyleUlloque-Badaracco, Juan R., Esteban A. Alarcón-Braga, Enrique A. Hernandez-Bustamante, Ali Al-kassab-Córdova, Vicente A. Benites-Zapata, D. Katterine Bonilla-Aldana, and Alfonso J. Rodriguez-Morales. 2022. "Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis" Pathogens 11, no. 11: 1248. https://doi.org/10.3390/pathogens11111248
APA StyleUlloque-Badaracco, J. R., Alarcón-Braga, E. A., Hernandez-Bustamante, E. A., Al-kassab-Córdova, A., Benites-Zapata, V. A., Bonilla-Aldana, D. K., & Rodriguez-Morales, A. J. (2022). Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis. Pathogens, 11(11), 1248. https://doi.org/10.3390/pathogens11111248