Covid-19 Infection in India: A Comparative Analysis of the Second Wave with the First Wave
Abstract
:1. Introduction
2. Results
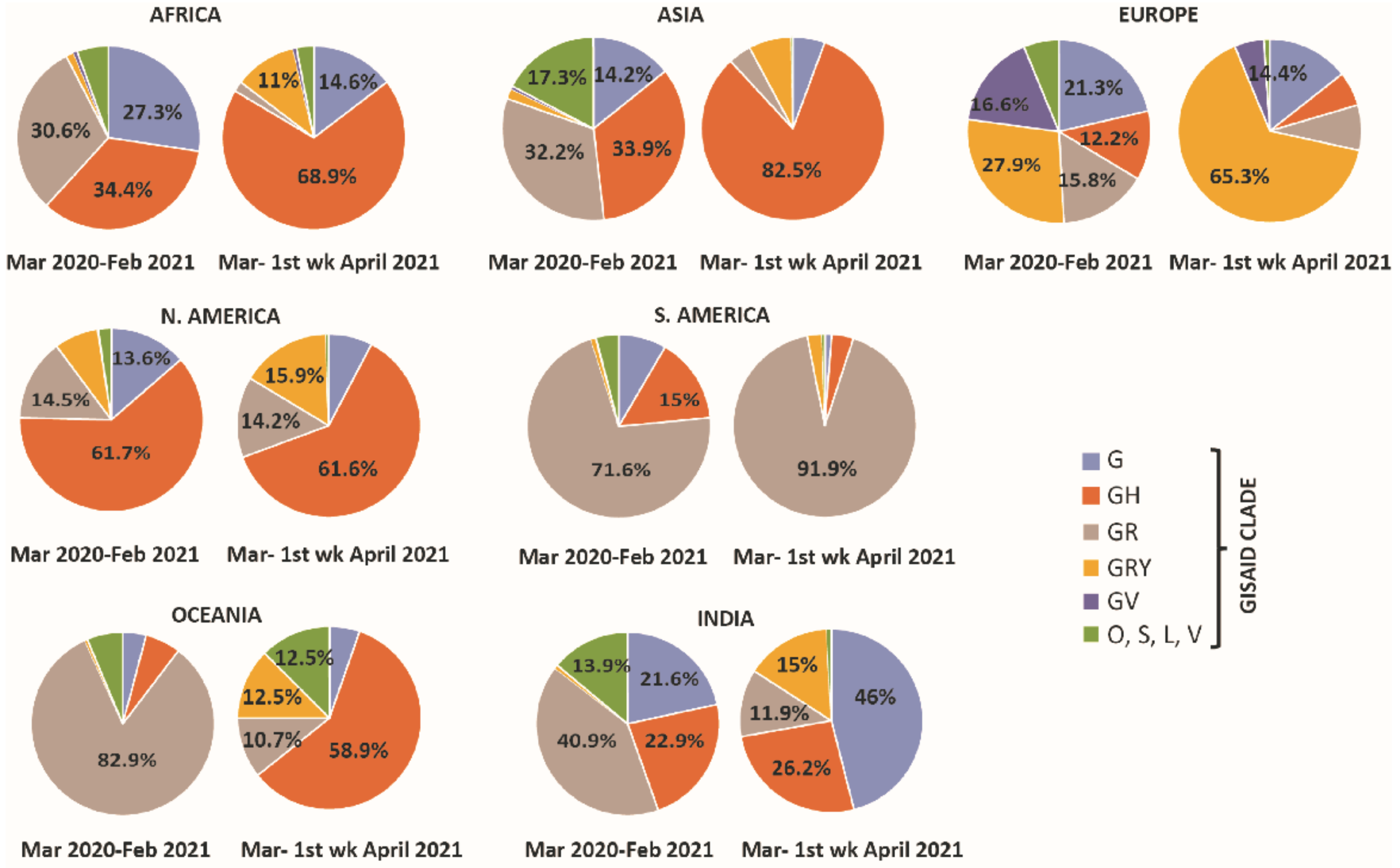
2.1. Global Distribution of Clade Variations in March 2020–February 2021 (Period I) and March 2021–First Week of April 2021 (Period II)
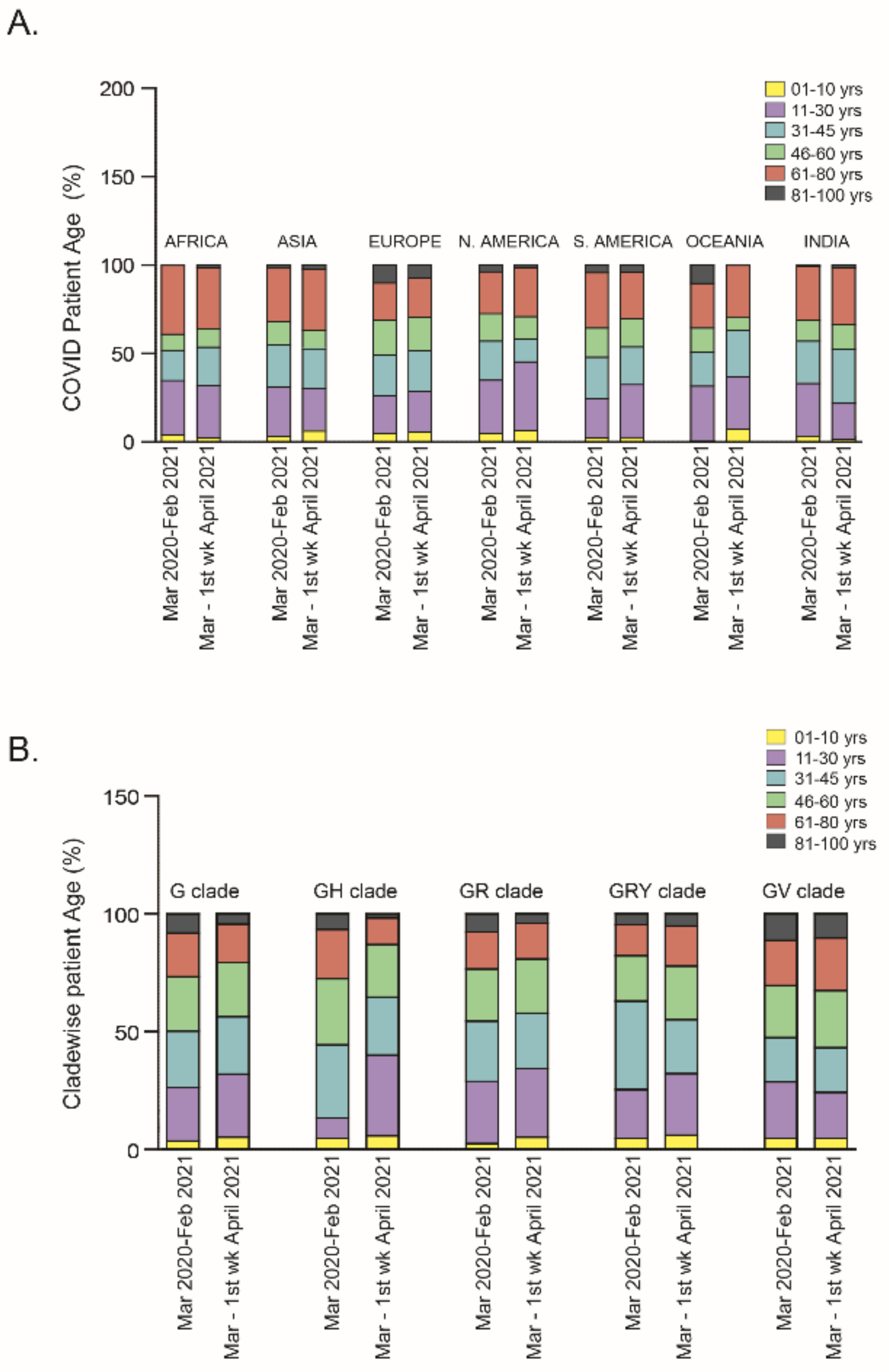
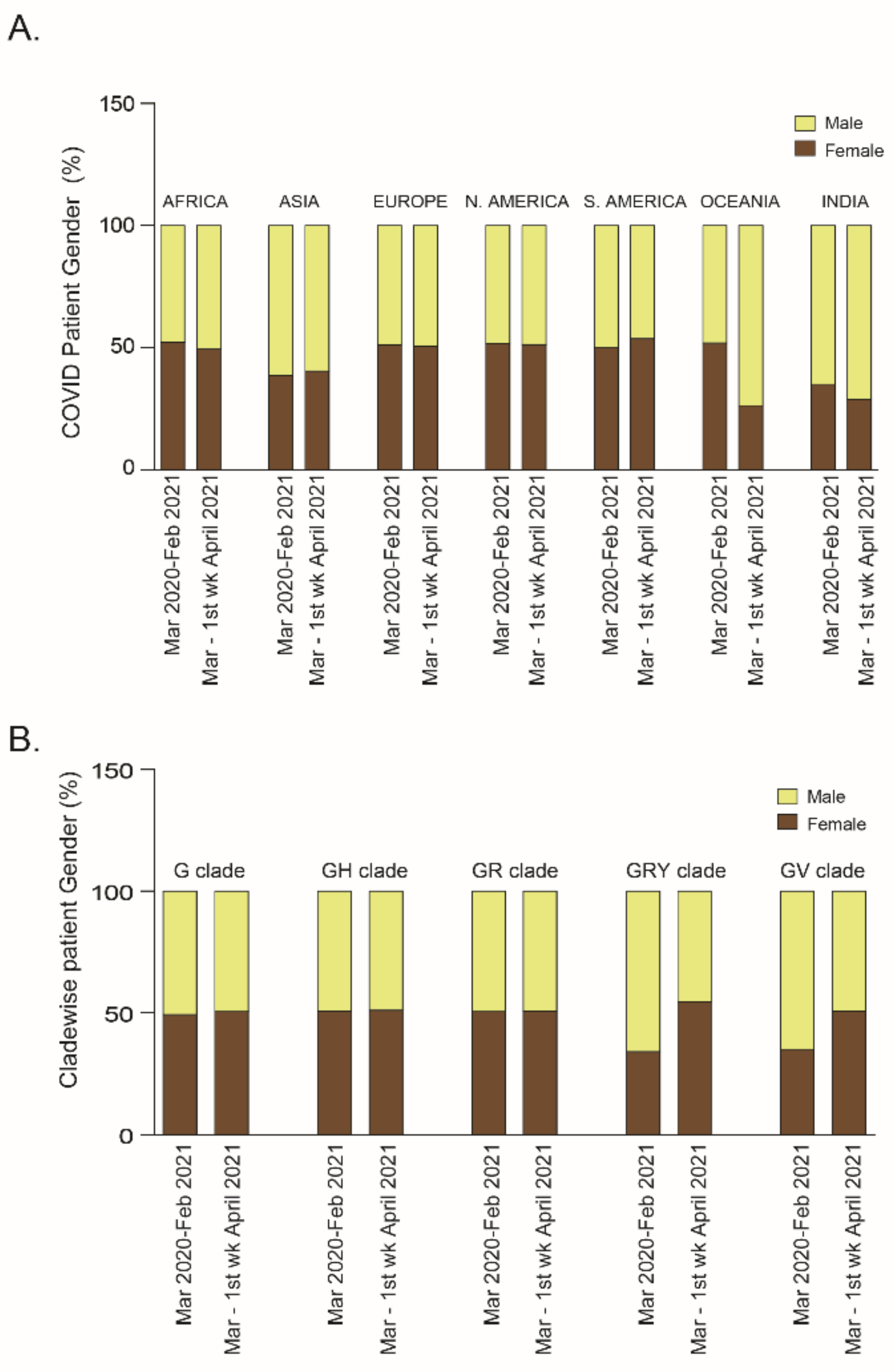
2.2. Relationship of Patient Age or Gender with SARS-CoV-2 Clade Variations: A Global Analysis
2.2.1. Patient Age
2.2.2. Patient Gender
2.3. Phylogenetic Analysis of the First and Second Waves of COVID-19 Infection in India
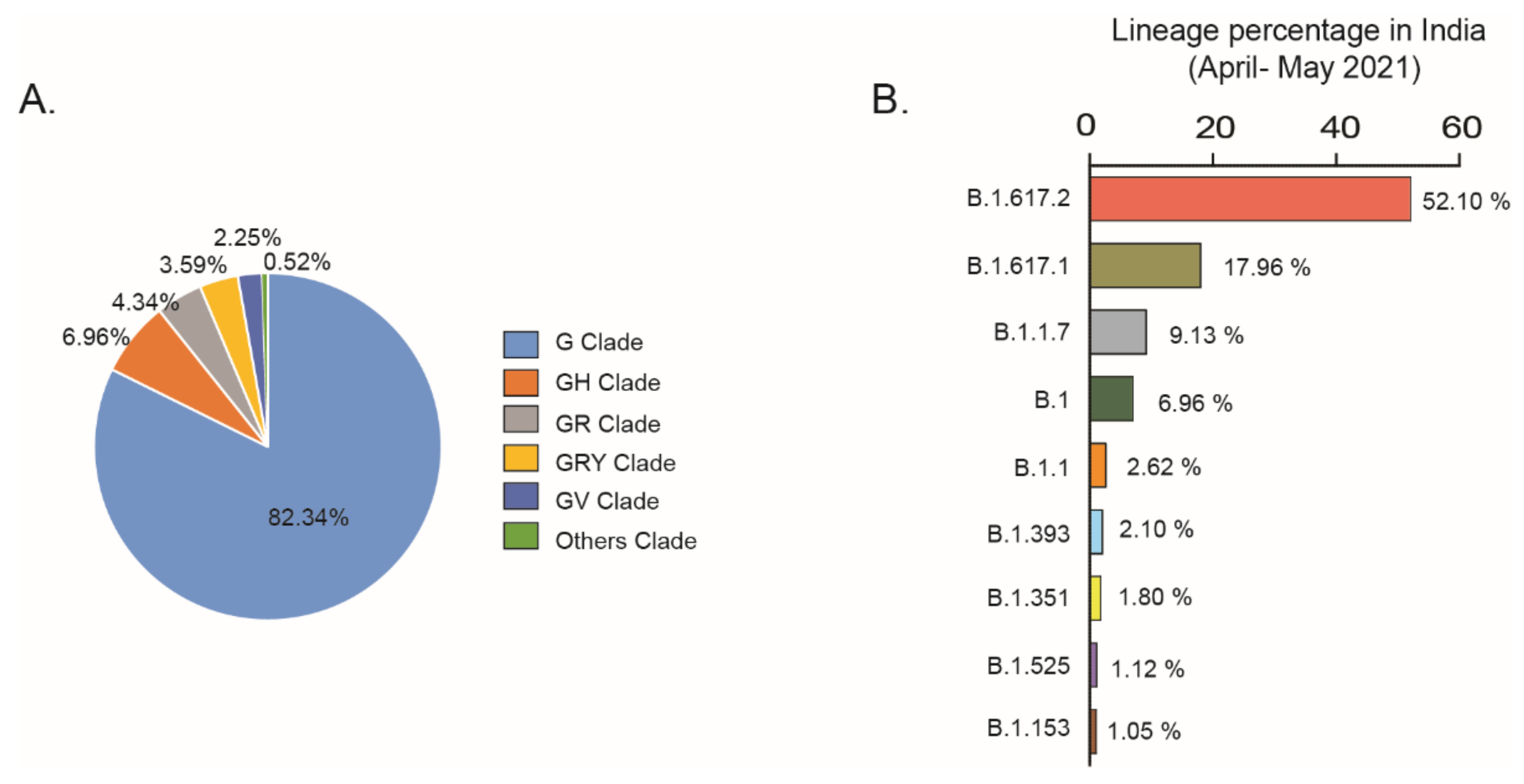
2.4. Current Scenario (April 2021–May 2021) in India
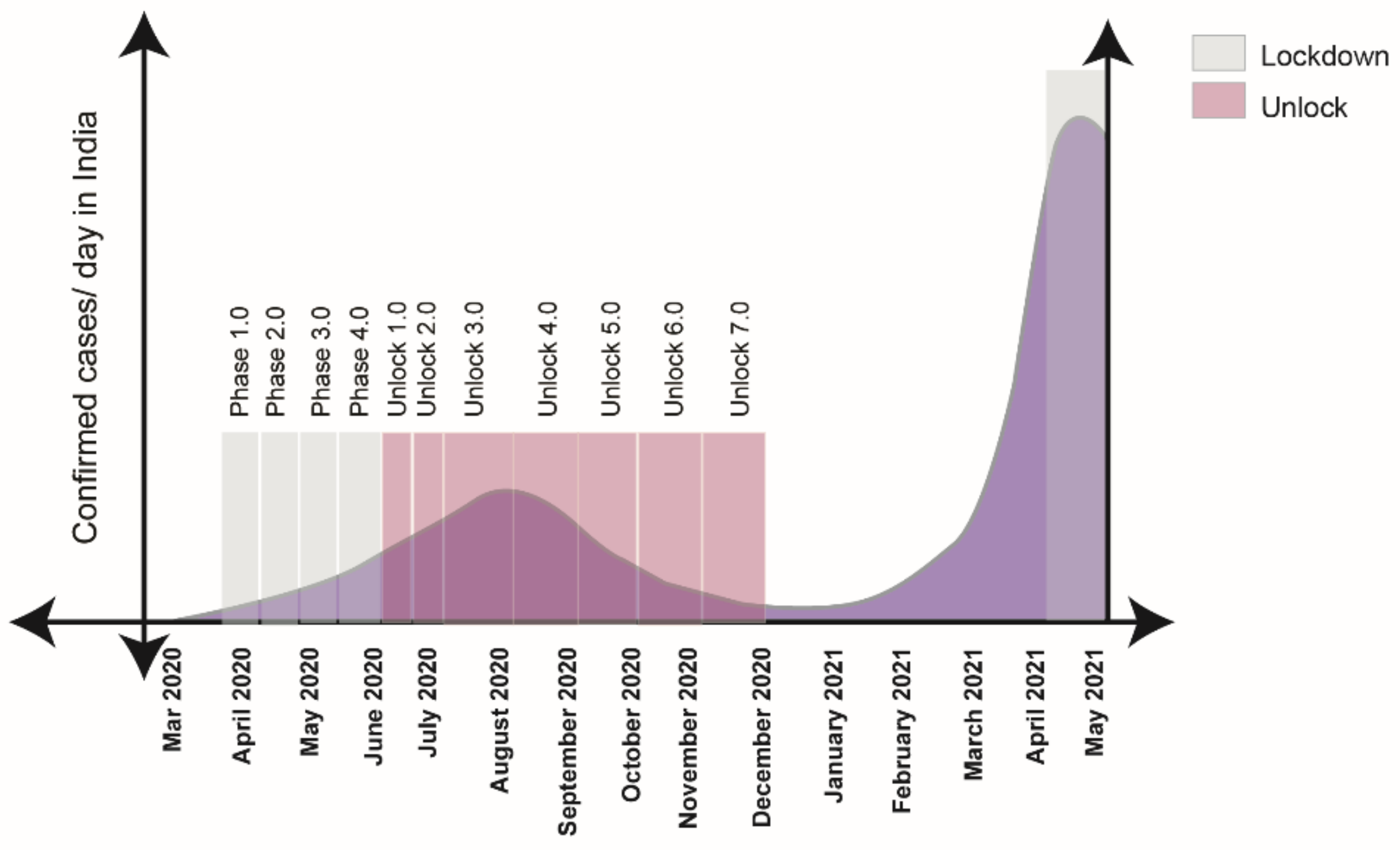
2.5. Government Stringent Policies
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. SARS-CoV-2 Metadata Analysis
5.2. Case Study of Clades and Lineages in April–May 2021 in India
5.3. Mutation Status of SARS-CoV-2 Variants in India
5.4. Vaccination Data Sources
5.5. Phylogenetic Analysis
5.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biswas, A.; Bhattacharjee, U.; Chakrabarti, A.K.; Tewari, D.N.; Banu, H.; Dutta, S. Emergence of Novel Coronavirus and COVID-19: Whether to Stay or Die Out? Crit. Rev. Microbiol. 2020, 46, 182–193. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.-Z.; Holmes, E.C. A Genomic Perspective on the Origin and Emergence of SARS-CoV-2. Cell 2020, 181, 223–227. [Google Scholar] [CrossRef]
- Zhu, Z.; Lian, X.; Su, X.; Wu, W.; Marraro, G.A.; Zeng, Y. From SARS and MERS to COVID-19: A Brief Summary and Comparison of Severe Acute Respiratory Infections Caused by Three Highly Pathogenic Human Coronaviruses. Respir. Res. 2020, 21, 224. [Google Scholar] [CrossRef]
- Forni, D.; Cagliani, R.; Clerici, M.; Sironi, M. Molecular Evolution of Human Coronavirus Genomes. Trends Microbiol. 2017, 25, 35–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, A.; Peng, Y.; Huang, B.; Ding, X.; Wang, X.; Niu, P.; Meng, J.; Zhu, Z.; Zhang, Z.; Wang, J.; et al. Genome Composition and Divergence of the Novel Coronavirus (2019-NCoV) Originating in China. Cell Host Microbe 2020, 27, 325–328. [Google Scholar] [CrossRef] [Green Version]
- Gordon, D.E.; Jang, G.M.; Bouhaddou, M.; Xu, J.; Obernier, K.; White, K.M.; O’Meara, M.J.; Rezelj, V.V.; Guo, J.Z.; Swaney, D.L.; et al. A SARS-CoV-2 Protein Interaction Map Reveals Targets for Drug Repurposing. Nature 2020, 583, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yang, C.; Xu, X.; Xu, W.; Liu, S. Structural and Functional Properties of SARS-CoV-2 Spike Protein: Potential Antivirus Drug Development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef]
- Sasaki, M.; Uemura, K.; Sato, A.; Toba, S.; Sanaki, T.; Maenaka, K.; Hall, W.W.; Orba, Y.; Sawa, H. SARS-CoV-2 Variants with Mutations at the S1/S2 Cleavage Site Are Generated in Vitro during Propagation in TMPRSS2-Deficient Cells. PLoS Pathog. 2021, 17, e1009233. [Google Scholar] [CrossRef]
- Shu, Y.; McCauley, J. GISAID: Global Initiative on Sharing All Influenza Data—From Vision to Reality. Eurosurveillance 2017, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rambaut, A.; Holmes, E.C.; O’Toole, Á.; Hill, V.; McCrone, J.T.; Ruis, C.; du Plessis, L.; Pybus, O.G. A Dynamic Nomenclature Proposal for SARS-CoV-2 Lineages to Assist Genomic Epidemiology. Nat. Microbiol. 2020, 5, 1403–1407. [Google Scholar] [CrossRef]
- Magro, G. SARS-CoV-2 and COVID-19: Is Interleukin-6 (IL-6) the ‘Culprit Lesion’ of ARDS Onset? What Is There besides Tocilizumab? SGP130Fc. Cytokine X 2020, 2, 100029. [Google Scholar] [CrossRef]
- Mokhtari, T.; Hassani, F.; Ghaffari, N.; Ebrahimi, B.; Yarahmadi, A.; Hassanzadeh, G. COVID-19 and Multiorgan Failure: A Narrative Review on Potential Mechanisms. J. Mol. Hist. 2020, 51, 613–628. [Google Scholar] [CrossRef] [PubMed]
- Wańkowicz, P.; Szylińska, A.; Rotter, I. Evaluation of Mental Health Factors among People with Systemic Lupus Erythematosus during the SARS-CoV-2 Pandemic. JCM 2020, 9, 2872. [Google Scholar] [CrossRef]
- Wańkowicz, P.; Szylińska, A.; Rotter, I. The Impact of the COVID-19 Pandemic on Psychological Health and Insomnia among People with Chronic Diseases. JCM 2021, 10, 1206. [Google Scholar] [CrossRef] [PubMed]
- Andrews, M.; Areekal, B.; Rajesh, K.; Krishnan, J.; Suryakala, R.; Krishnan, B.; Muraly, C.; Santhosh, P. First Confirmed Case of COVID-19 Infection in India: A Case Report. Indian J. Med. Res. 2020, 151, 490. [Google Scholar] [CrossRef] [PubMed]
- Seong, H.; Hyun, H.J.; Yun, J.G.; Noh, J.Y.; Cheong, H.J.; Kim, W.J.; Song, J.Y. Comparison of the Second and Third Waves of the COVID-19 Pandemic in South Korea: Importance of Early Public Health Intervention. Int. J. Infect. Dis. 2021, 104, 742–745. [Google Scholar] [CrossRef] [PubMed]
- Taboada, M.; González, M.; Alvarez, A.; Eiras, M.; Costa, J.; Álvarez, J.; Seoane-Pillado, T. First, Second and Third Wave of COVID-19. What Have We Changed in the ICU Management of These Patients? J. Infect. 2021, 82, e14–e15. [Google Scholar] [CrossRef] [PubMed]
- Gili, T.; Benelli, G.; Buscarini, E.; Canetta, C.; La Piana, G.; Merli, G.; Scartabellati, A.; Viganò, G.; Sfogliarini, R.; Melilli, G.; et al. SARS-COV-2 Comorbidity Network and Outcome in Hospitalized Patients in Crema, Italy. PLoS ONE 2021, 16, e0248498. [Google Scholar] [CrossRef]
- Cunningham, J.W.; Vaduganathan, M.; Claggett, B.L.; Jering, K.S.; Bhatt, A.S.; Rosenthal, N.; Solomon, S.D. Clinical Outcomes in Young US Adults Hospitalized With COVID-19. JAMA Intern. Med. 2021, 181, 379. [Google Scholar] [CrossRef]
- Goldstein, E.; Lipsitch, M.; Cevik, M. On the Effect of Age on the Transmission of SARS-CoV-2 in Households, Schools, and the Community. J. Infect. Dis. 2021, 223, 362–369. [Google Scholar] [CrossRef]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; Eggo, R.M.; CMMID COVID-19 Working Group. Age-Dependent Effects in the Transmission and Control of COVID-19 Epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Jin, J.-M.; Bai, P.; He, W.; Wu, F.; Liu, X.-F.; Han, D.-M.; Liu, S.; Yang, J.-K. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front. Public Health 2020, 8, 152. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Mukherjee, S.; Pahan, K. Is COVID-19 Gender-Sensitive? J. Neuroimmune Pharmacol. 2021, 16, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Lakbar, I.; Luque-Paz, D.; Mege, J.-L.; Einav, S.; Leone, M. COVID-19 Gender Susceptibility and Outcomes: A Systematic Review. PLoS ONE 2020, 15, e0241827. [Google Scholar] [CrossRef]
- Elbe, S.; Buckland-Merrett, G. Data, Disease and Diplomacy: GISAID’s Innovative Contribution to Global Health: Data, Disease and Diplomacy. Glob. Chall. 2017, 1, 33–46. [Google Scholar] [CrossRef] [Green Version]
- Thompson, R.N.; Stockwin, J.E.; van Gaalen, R.D.; Polonsky, J.A.; Kamvar, Z.N.; Demarsh, P.A.; Dahlqwist, E.; Li, S.; Miguel, E.; Jombart, T.; et al. Improved Inference of Time-Varying Reproduction Numbers during Infectious Disease Outbreaks. Epidemics 2019, 29, 100356. [Google Scholar] [CrossRef]
- Madewell, Z.J.; Yang, Y.; Longini, I.M.; Halloran, M.E.; Dean, N.E. Household Transmission of SARS-CoV-2: A Systematic Review and Meta-Analysis. JAMA Netw. Open. 2020, 3, e2031756. [Google Scholar] [CrossRef]
- Comunian, S.; Dongo, D.; Milani, C.; Palestini, P. Air Pollution and COVID-19: The Role of Particulate Matter in the Spread and Increase of COVID-19’s Morbidity and Mortality. IJERPH 2020, 17, 4487. [Google Scholar] [CrossRef] [PubMed]
- Zoran, M.A.; Savastru, R.S.; Savastru, D.M.; Tautan, M.N. Assessing the Relationship between Ground Levels of Ozone (O3) and Nitrogen Dioxide (NO2) with Coronavirus (COVID-19) in Milan, Italy. Sci. Total Environ. 2020, 740, 140005. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Vaccine Key to Reaching ‘Herd Immunity’. Available online: https://www.muhealth.org/our-stories/covid-19-vaccine-key-reaching-herd-immunity (accessed on 21 September 2020).
- Young, B.E.; Wei, W.E.; Fong, S.-W.; Mak, T.-M.; Anderson, D.E.; Chan, Y.-H.; Pung, R.; Heng, C.S.; Ang, L.W.; Zheng, A.K.E.; et al. Association of SARS-CoV-2 Clades with Clinical, Inflammatory and Virologic Outcomes: An Observational Study. EBioMedicine 2021, 66, 103319. [Google Scholar] [CrossRef]
- Liu, J.; Li, S.; Liu, J.; Liang, B.; Wang, X.; Wang, H.; Li, W.; Tong, Q.; Yi, J.; Zhao, L.; et al. Longitudinal Characteristics of Lymphocyte Responses and Cytokine Profiles in the Peripheral Blood of SARS-CoV-2 Infected Patients. EBioMedicine 2020, 55, 102763. [Google Scholar] [CrossRef]
- He, L.; Ding, Y.; Zhang, Q.; Che, X.; He, Y.; Shen, H.; Wang, H.; Li, Z.; Zhao, L.; Geng, J.; et al. Expression of Elevated Levels of Pro-Inflammatory Cytokines in SARS-CoV-Infected ACE2 + Cells in SARS Patients: Relation to the Acute Lung Injury and Pathogenesis of SARS. J. Pathol. 2006, 210, 288–297. [Google Scholar] [CrossRef]
- Esper, F.P.; Cheng, Y.-W.; Adhikari, T.M.; Tu, Z.J.; Li, D.; Li, E.A.; Farkas, D.H.; Procop, G.W.; Ko, J.S.; Chan, T.A.; et al. Genomic Epidemiology of SARS-CoV-2 Infection During the Initial Pandemic Wave and Association With Disease Severity. JAMA Netw. Open 2021, 4, e217746. [Google Scholar] [CrossRef]
- Pandit, B.; Bhattacharjee, S.; Bhattacharjee, B. Association of Clade-G SARS-CoV-2 Viruses and Age with Increased Mortality Rates across 57 Countries and India. Infect. Genet. Evol. 2021, 90, 104734. [Google Scholar] [CrossRef]
- Nakamichi, K.; Shen, J.Z.; Lee, C.S.; Lee, A.; Roberts, E.A.; Simonson, P.D.; Roychoudhury, P.; Andriesen, J.; Randhawa, A.K.; Mathias, P.C.; et al. Hospitalization and Mortality Associated with SARS-CoV-2 Viral Clades in COVID-19. Sci. Rep. 2021, 11, 4802. [Google Scholar] [CrossRef]
- Hamed, S.M.; Elkhatib, W.F.; Khairalla, A.S.; Noreddin, A.M. Global Dynamics of SARS-CoV-2 Clades and Their Relation to COVID-19 Epidemiology. Sci. Rep. 2021, 11, 8435. [Google Scholar] [CrossRef]
- Takahashi, T.; Ellingson, M.K.; Wong, P.; Israelow, B.; Lucas, C.; Klein, J.; Silva, J.; Mao, T.; Oh, J.E.; Yale IMPACT Research Team; et al. Sex Differences in Immune Responses That Underlie COVID-19 Disease Outcomes. Nature 2020, 588, 315–320. [Google Scholar] [CrossRef]
- Marimuthu, S.; Joy, M.; Malavika, B.; Nadaraj, A.; Asirvatham, E.S.; Jeyaseelan, L. Modelling of Reproduction Number for COVID-19 in India and High Incidence States. Clin. Epidemiol. Glob. Health 2021, 9, 57–61. [Google Scholar] [CrossRef]
- Ranjan, R.; Sharma, A.; Verma, M.K. Characterization of the Second Wave of COVID-19 in India. medRxiv 2021. [Google Scholar] [CrossRef]

| Lineage | Clade | ORF1a | ORF1b | S | ORF3a | ORF6 | ORF7a | ORF8 | M | E | N | Location Percentage |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B.1.617.2 | G | ----- | P314L, G662S, P1000L | T19R, del157/158, L452R, T478K, D614G, P681R, D950N | S26L | ----- | V82A T12OI | Del119/120 | I82T | ----- | D63G, R203M, D377Y | India (14%), Worldwide (1%) |
| B.1.617.1 | G | ----- | T1567I, T3646A, P314L, M1352I, K2310R | L452R, E484Q, D614G, P681R, Q1071H | S26L | ----- | V82A | ----- | ----- | ----- | R203M, D377Y | India (19%), Worldwide (0.5%) |
| B.1.1.7 | GRY | T1001I, A17O8D, I2230T, del3675/ 3677 | P314L | Del69/70, del144/145, N501Y, A570D, D614G, P681H, T716I, S982A, D1118H | ----- | ----- | ----- | Q27, R25I, Y73C | ----- | ----- | D3L, R203K, G204R, S235F | India (10%), Worldwide (42%) |
| B.1 | G/GH | ----- | P314L | D614G | ----- | ----- | ----- | ----- | ----- | ----- | ----- | India (11%), Worldwide (5%) |
| B.1.1 | GR | ----- | P314L | D614G | ----- | ----- | ----- | ----- | ----- | ----- | R203K, G204R, | India (7%), Worldwide (3%) |
| B.1.393 | unknown | ----- | P314L | D614G | ----- | ----- | ----- | ----- | ----- | ----- | ----- | India (1%), Worldwide (0.5%) |
| B.1.351 | GH | T265I, K1655N, K3353R, del3675/3677 | P314L | D80A, D215G, del241/243, K417, E484K,N501Y, D614G, A701V | Q57H, S171L | ----- | ----- | ----- | ----- | P71L | T205I | India (2%), Worldwide (1%) |
| B.1.525 | G | T2007I, del 3675/3677 | P314L | Q52R, A67V, del69/70, del144/145, E484K, D614G, Q677H,F888L | ----- | Del2/3 | ----- | ----- | I82T | L21F | T205I, del3, A12G | India (1%), Worldwide (0.5%) |
| B.1.153 | G | ----- | ----- | D614G | ----- | ----- | ----- | ----- | ----- | ----- | ----- | India (1%), Worldwide (0.5%) |
| Month, 2021 | Average Vaccination/Day | Average Full Vaccination/Day |
|---|---|---|
| January | 2,50,589 | 0 |
| February | 2,88,794 | 87,721 |
| March | 14,17,358 | 2,21,887 |
| April | 23,19,791 | 5,76,215 |
| Up to 25 May | 11,25,377 | 6,14,969 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarkar, A.; Chakrabarti, A.K.; Dutta, S. Covid-19 Infection in India: A Comparative Analysis of the Second Wave with the First Wave. Pathogens 2021, 10, 1222. https://doi.org/10.3390/pathogens10091222
Sarkar A, Chakrabarti AK, Dutta S. Covid-19 Infection in India: A Comparative Analysis of the Second Wave with the First Wave. Pathogens. 2021; 10(9):1222. https://doi.org/10.3390/pathogens10091222
Chicago/Turabian StyleSarkar, Arnab, Alok Kumar Chakrabarti, and Shanta Dutta. 2021. "Covid-19 Infection in India: A Comparative Analysis of the Second Wave with the First Wave" Pathogens 10, no. 9: 1222. https://doi.org/10.3390/pathogens10091222
APA StyleSarkar, A., Chakrabarti, A. K., & Dutta, S. (2021). Covid-19 Infection in India: A Comparative Analysis of the Second Wave with the First Wave. Pathogens, 10(9), 1222. https://doi.org/10.3390/pathogens10091222






