High Prevalence of Epilepsy in an Onchocerciasis-Endemic Area in Mvolo County, South Sudan: A Door-To-Door Survey
Abstract
1. Introduction
2. Methodology
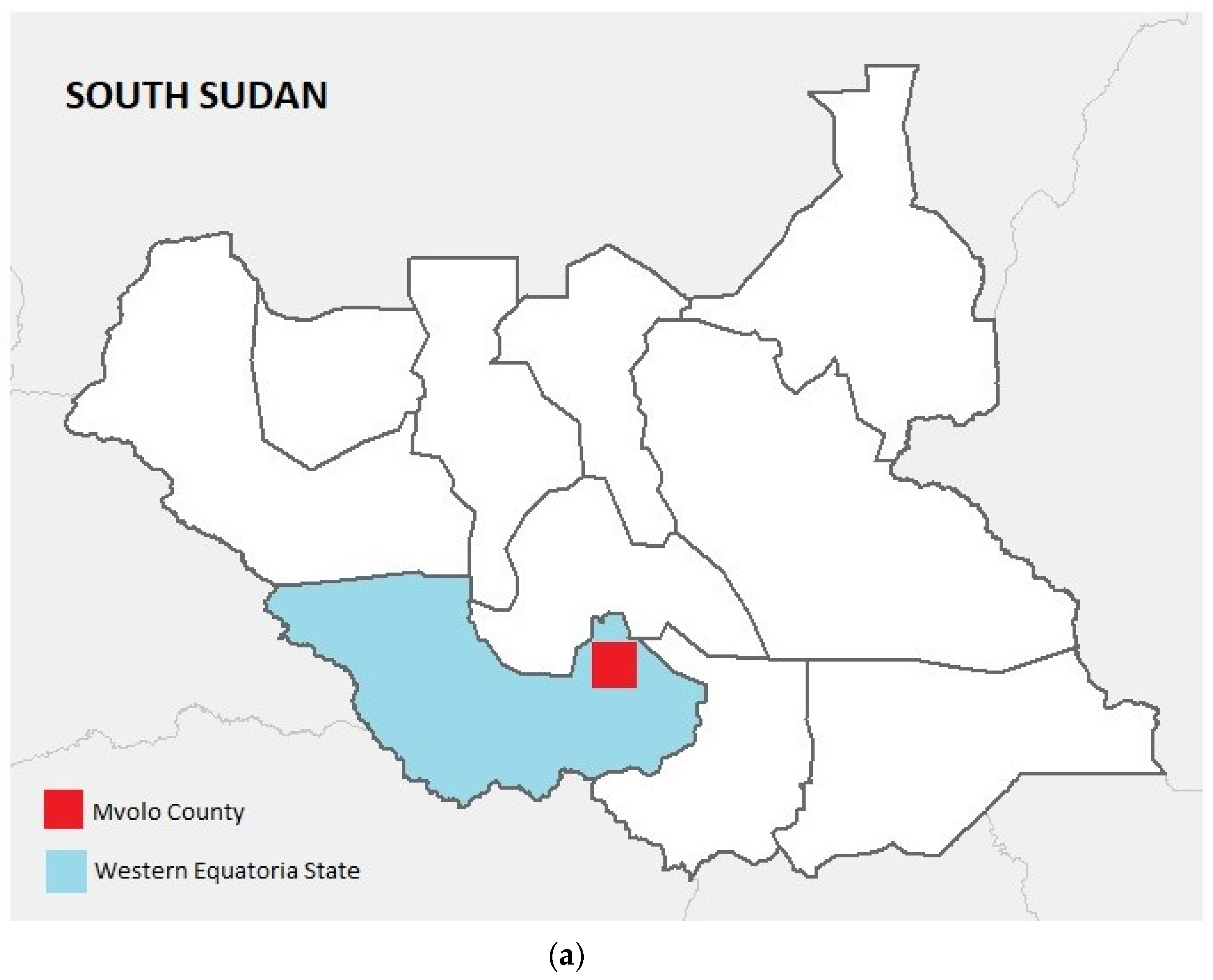
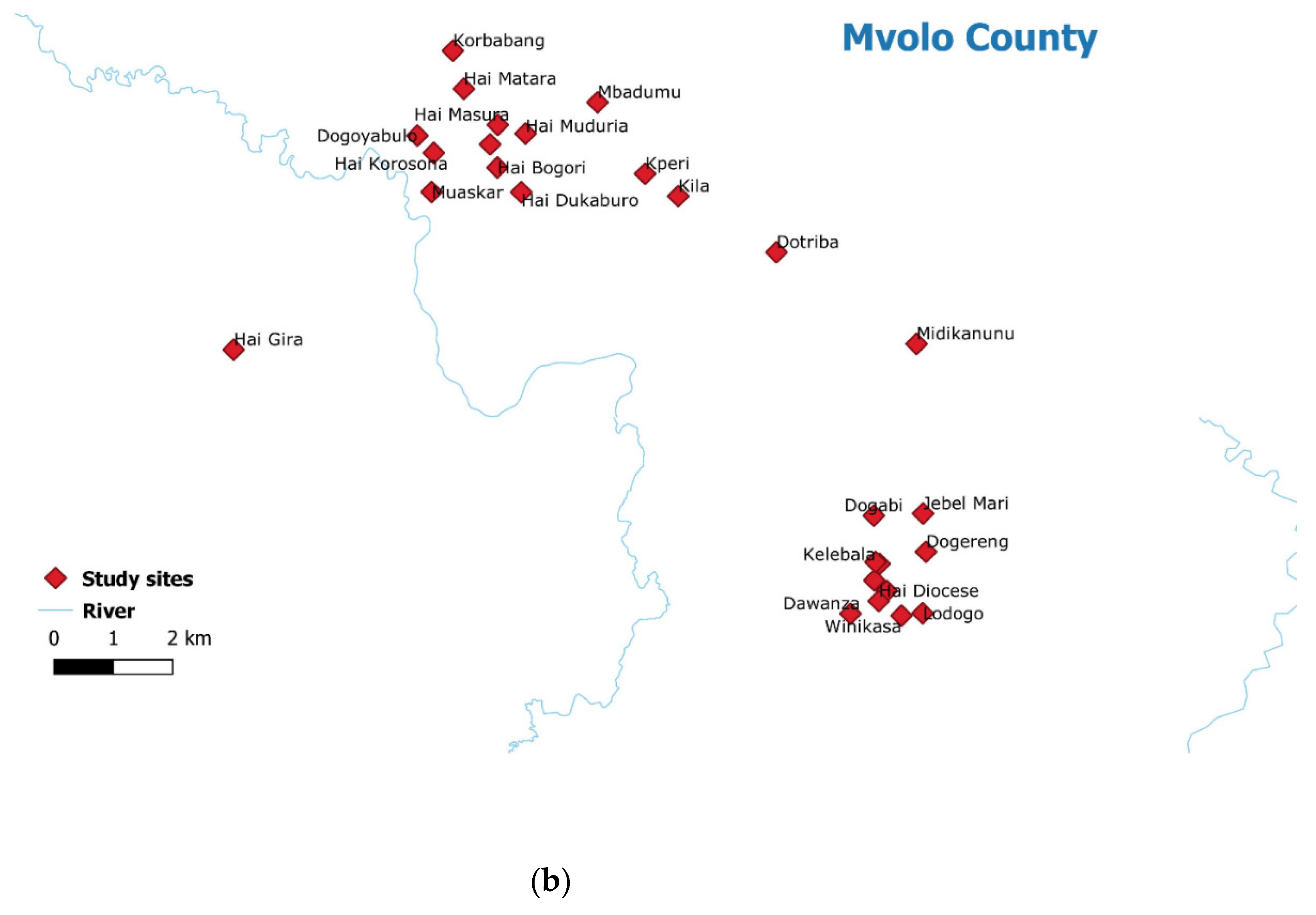
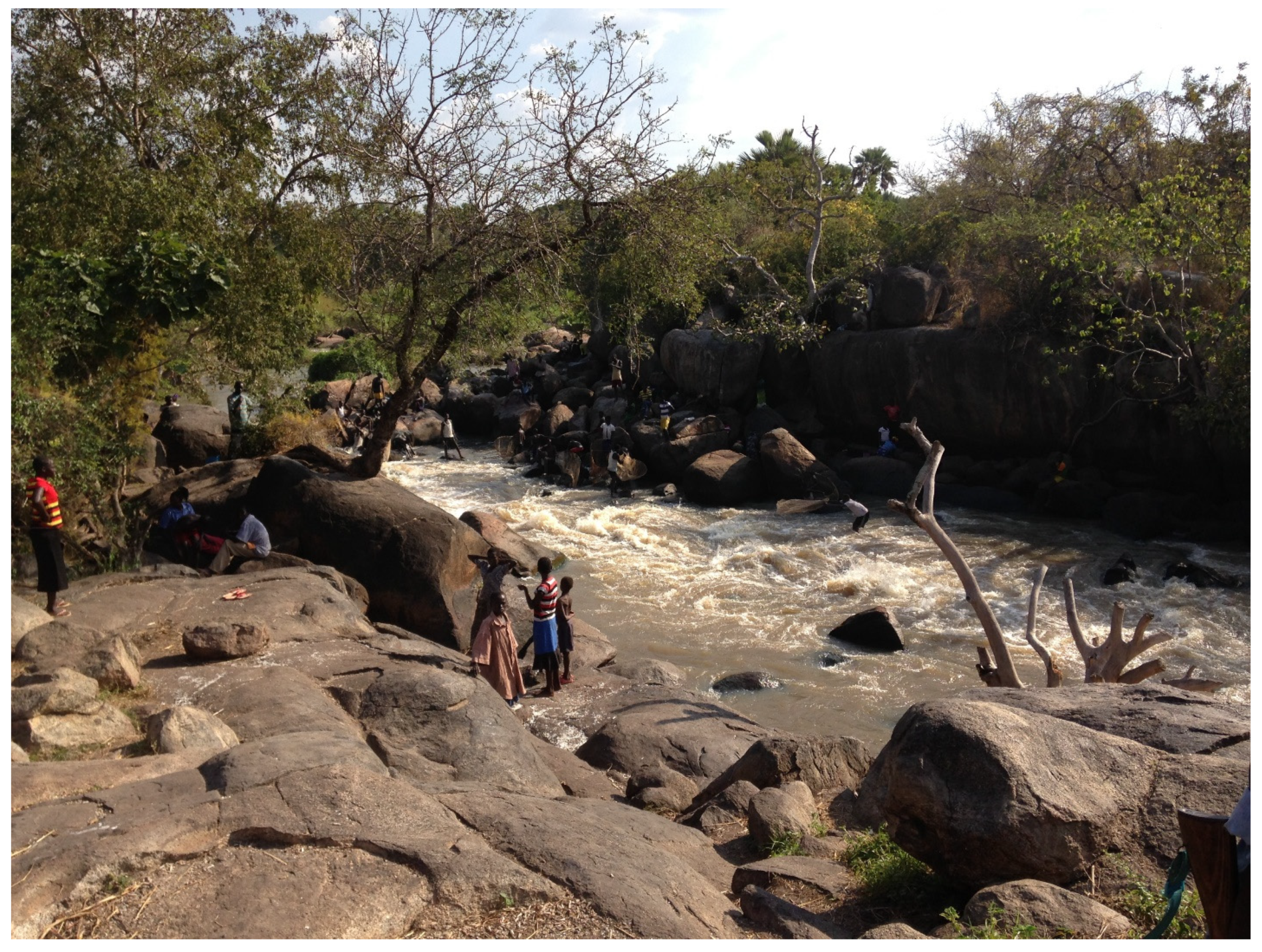
2.1. Study Setting
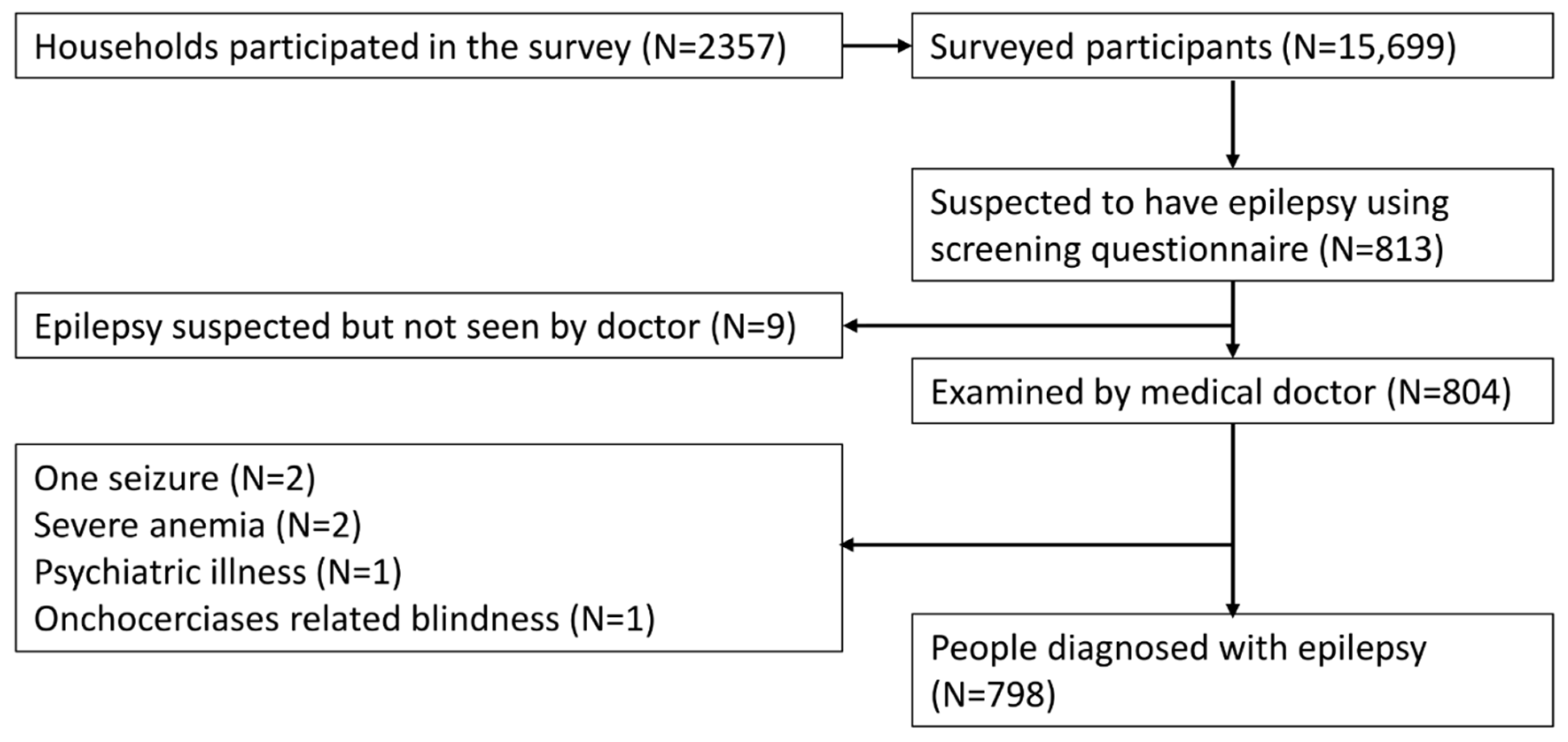
2.2. Study Design
2.2.1. Definitions
2.2.2. Data Collection and Management
2.2.3. Onchocerciasis Antibody Testing
2.3. Data Analysis
3. Results
3.1. Prevalence of Potential Onchocerciasis Associated Co-Morbidities
3.2. Prevalence of Epilepsy
3.3. Incidence of Epilepsy
3.4. Characteristics of Epilepsy
3.5. Risk Factors for Epilepsy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tumwine, J.K.; Vandemaele, K.; Chungong, S.; Richer, M.; Anker, M.; Ayana, Y.; Opoka, M.L.; Klaucke, D.N.; Quarello, A.; Spencer, P.S. Clinical and epidemiologic characteristics of nodding syndrome in Mundri County, southern Sudan. Afr. Health Sci. 2012, 12, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Nodding Syndrome—South Sudan, 2011. Morb. Mortal. Wkly. Rep. 2012, 61, 52–54. [Google Scholar]
- Colebunders, R.; Hendy, A.; Mokili, J.L.; Wamala, J.F.; Kaducu, J.; Kur, L.; Tepage, F.; Mandro, M.; Mucinya, G.; Mambandu, G.; et al. Nodding syndrome and epilepsy in onchocerciasis endemic regions: Comparing preliminary observations from South Sudan and the Democratic Republic of the Congo with data from Uganda. BMC Res. Notes 2016, 9, 182. [Google Scholar] [CrossRef]
- Colebunders, R.; Carter, J.Y.; Olore, P.C.; Puok, K.; Bhattacharyya, S.; Menon, S.; Abd-Elfarag, G.; Ojok, M.; Ensoy-Musoro, C.; Lako, R.; et al. High prevalence of onchocerciasis-associated epilepsy in villages in Maridi County, Republic of South Sudan: A community-based survey. Seizure 2018, 63, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.J. Simulium Damnosum and its relation to onchocerciasis in the Anglo-Egyptian Sudan. Bull. Entomol. Res. 1953, 43, 597–644. [Google Scholar] [CrossRef]
- Gumisiriza, N.; Mubiru, F.; Siewe Fodjo, J.N.; Mbonye Kayitale, M.; Hotterbeekx, A.; Idro, R.; Makumbi, I.; Lakwo, T.; Opar, B.; Kaducu, J.; et al. Prevalence and incidence of nodding syndrome and other forms of epilepsy in onchocerciasis-endemic areas in northern Uganda after the implementation of onchocerciasis control measures. Infect. Dis. Poverty 2020, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Gumisiriza, N.; Kaiser, C.; Asaba, G.; Onen, H.; Mubiru, F.; Kisembo, D.; Siewe Fodjo, J.N.; Colebunders, R. Changes in epilepsy burden after onchocerciasis elimination in a hyperendemic focus of western Uganda: A comparison of two population-based, cross-sectional studies. Lancet Infect. Dis. 2020, 20, 1315–1323. [Google Scholar] [CrossRef]
- Siewe Fodjo, J.N.; Tatah, G.; Tabah, E.N.; Ngarka, L.; Nfor, L.N.; Chokote, S.E.; Mengnjo, M.K.; Dema, F.; Sitouok, A.T.; Nkoro, G.; et al. Epidemiology of onchocerciasis-associated epilepsy in the Mbam and Sanaga river valleys of Cameroon: Impact of more than 13 years of ivermectin. Infect. Dis. Poverty 2018, 7, 114. [Google Scholar] [CrossRef]
- Abd-Elfarag, G.; Logora, M.Y.; Carter, J.Y.; Ojok, M.; Songok, J.; Menon, S.; Wit, F.; Lako, R.; Colebunders, R. The effect of bi-annual community-directed treatment with ivermectin on the incidence of epilepsy in onchocerciasis endemic villages in South Sudan: A study protocol. Infect. Dis. Poverty 2018, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Diagana, M.; Preux, P.M.; Tuillas, M.; Ould Hamady, A.; Druet-Cabanac, M. Depistage de l’epilepsie en zones tropicales: Validation d’un questionnaire en Mauritanie. Bull. Soc. Pathol. Exot. 2006, 99, 103–107. [Google Scholar] [PubMed]
- Fisher, R.S.; Acevedo, C.; Arzimanoglou, A.; Bogacz, A.; Cross, J.H.; Elger, C.E.; Engel, J., Jr.; Forsgren, L.; French, J.A.; Glynn, M.; et al. ILAE official report: A practical clinical definition of epilepsy. Epilepsia 2014, 55, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Colebunders, R.; Abd-Elfarag, G.; Carter, J.Y.; Olore, P.C.; Puok, K.; Menon, S.; Fodjo Siewe, J.N.; Bhattacharyya, S.; Ojok, M.; Lako, R.; et al. Clinical characteristics of onchocerciasis-associated epilepsy in villages in Maridi County, Republic of South Sudan. Seizure 2018, 62, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Dusabimana, A.; Bhwana, D.; Raimon, S.; Mmbando, B.P.; Hotterbeekx, A.; Tepage, F.; Mandro, M.; Siewe Fodjo, J.N.; Abrams, S.; Colebunders, R. Ivermectin Treatment Response in Onchocerca Volvulus Infected Persons with Epilepsy: A Three-Country Short Cohort Study. Pathogens 2020, 9, 617. [Google Scholar] [CrossRef] [PubMed]
- Wahl, G.; Enyong, P.; Ngosso, A.; Schibel, J.M.; Moyou, R.; Tubbesing, H.; Ekale, D.; Renz, A. Onchocerca ochengi: Epidemiological evidence of cross-protection against Onchocerca volvulus in man. Parasitology 1998, 116 Pt 4, 349–362. [Google Scholar] [CrossRef]
- Boussinesq, M.; Pion, S.D.; Demanga, N.; Kamgno, J. Relationship between onchocerciasis and epilepsy: A matched case-control study in the Mbam Valley, Republic of Cameroon. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 537–541. [Google Scholar] [CrossRef]
- Dusabimana, A.; Bhwana, D.; Mandro, M.; Mmbando, B.P.; Siewe Fodjo, J.N.; Colebunders, R. OV16 Seroprevalence among Persons with Epilepsy in Onchocerciasis Endemic Regions: A Multi-Country Study. Pathogens 2020, 9, 847. [Google Scholar] [CrossRef] [PubMed]
- Chesnais, C.B.; Nana-Djeunga, H.C.; Njamnshi, A.K.; Lenou-Nanga, C.G.; Boulle, C.; Bissek, A.Z.; Kamgno, J.; Colebunders, R.; Boussinesq, M. The temporal relationship between onchocerciasis and epilepsy: A population-based cohort study. Lancet Infect. Dis. 2018, 18, 1278–1286. [Google Scholar] [CrossRef]
- Chesnais, C.B.; Bizet, C.; Campillo, J.T.; Njamnshi, W.Y.; Bopda, J.; Nwane, P.; Pion, S.D.; Njamnshi, A.K.; Boussinesq, M. A Second Population-Based Cohort Study in Cameroon Confirms the Temporal Relationship Between Onchocerciasis and Epilepsy. Open Forum Infect. Dis. 2020, 7, ofaa206. [Google Scholar] [CrossRef] [PubMed]
- Colebunders, R.; Njamnshi, A.K.; Menon, S.; Newton, C.R.; Hotterbeekx, A.; Preux, P.M.; Hopkins, A.; Vaillant, M.; Siewe Fodjo, J.N. Onchocerca volvulus and epilepsy: A comprehensive review using the Bradford Hill criteria for causation. PLoS Negl. Trop. Dis. 2021, 15, e0008965. [Google Scholar] [CrossRef] [PubMed]
- Colebunders, R.; Siewe Fodjo, J.N.; Hopkins, A.; Hotterbeekx, A.; Lakwo, T.L.; Kalinga, A.; Logora, M.Y.; Basanez, M.G. From river blindness to river epilepsy: Implications for onchocerciasis elimination programmes. PLoS Negl. Trop. Dis. 2019, 13, e0007407. [Google Scholar] [CrossRef] [PubMed]
| Village | Distance to the Naam River (in km) | Participants in Survey | Persons with Epilepsy, n (%) | Itching, n (%) | Blind, n (%) |
|---|---|---|---|---|---|
| Dogoyabulo * | 0.7 | 377 | 20 (5.3) | 111 (29.4) | 6 (1.6) |
| Dokaburo * | 2.3 | 93 | 3 (3.2) | 17 (18.3) | 9 (9.7) |
| Hai Bogori * | 1.9 | 677 | 70 (10.3) | 210 (31.0) | 32 (4.6) |
| Hai Dileb * | 1.8 | 194 | 6 (3.1) | 26 (13.4) | 19 (9.8) |
| Hai-Gira * | 4.3 | 1181 | 93 (7.9) | 467 (39.5) | 38 (3.2) |
| Hai Korosona * | 0.9 | 674 | 59 (8.8) | 172 (25.5) | 21 (3.1) |
| Hai Matara * | 1.9 | 1205 | 62 (5.1) | 341 (28.3) | 23 (1.9) |
| Hai Masura * | 2.0 | 230 | 16 (7.0) | 61 (26.5) | 6 (2.6) |
| Mbadumu * | 3.7 | 551 | 33 (6.0) | 123 (22.3) | 26 (4.7) |
| Muaskar * | 0.9 | 17 | 2 (11.8) | 4 (23.5) | 0 (0.0) |
| Muduria * | 0.9 | 484 | 24 (5.0) | 105 (21.7) | 9 (1.9) |
| Hai Diocese | 35.6 | 551 | 30 (5.4) | 175 (31.8) | 19 (3.4) |
| Hai Malakia | 33.7 | 363 | 20 (5.5) | 107 (29.5) | 5 (1.4) |
| Hai Zira | 34.4 | 572 | 26 (4.5) | 145 (25.3) | 21 (3.7) |
| Dawanza | 35.4 | 89 | 3 (3.4) | 36 (40.4) | 3 (3.4) |
| Dogabi | 31.2 | 217 | 8 (3.7) | 54 (24.9) | 5 (2.3) |
| Dogereng | 34.7 | 689 | 34 (4.9) | 279 (40.5) | 18 (2.6) |
| Dokati Ngobo | 6.1 | 379 | 11 (2.9) | 118 (31.1) | 8 (2.1) |
| Dolo | 24.3 | 216 | 3 (1.4) | 20 (9.3) | 2 (0.9) |
| Domeri | 13.4 | 565 | 48 (8.5) | 264 (46.7) | 13 (2.3) |
| Dotriba | 6.7 | 866 | 21 (2.4) | 435 (50.2) | 28 (3.2) |
| Jebel Mira | 32.0 | 107 | 8 (7.5) | 39 (36.4) | 0 (0.0) |
| Kelibala | 33.5 | 347 | 11 (3.2) | 84 (24.2) | 3 (0.9) |
| Korbabang | 30.0 | 712 | 15 (2.1) | 244 (34.3) | 7 (1.0) |
| Kperi | 4.4 | 938 | 44 (4.7) | 159 (17.0) | 39 (4.2) |
| Kulu | 5.0 | 621 | 25 (4.0) | 138 (22.2) | 33 (5.3) |
| Lamu | 26.0 | 364 | 5 (1.4) | 124 (34.1) | 7 (1.9) |
| Lodogo | 37.6 | 80 | 3 (3.8) | 24 (30.0) | 4 (5.0) |
| Medikanunu | 9.4 | 321 | 15 (4.7) | 135 (42.1) | 5 (1.6) |
| Minikolome | 7.7 | 1026 | 39 (3.8) | 332 (32.4) | 17 (1.7) |
| Tiboro | 22.1 | 281 | 22 (7.8) | 118 (42.0) | 7 (2.5) |
| Winikasa | 37.0 | 261 | 5 (1.9) | 90 (34.5) | 11 (4.2) |
| Winikelo | 5.3 | 107 | 6 (5.6) | 67 (62.6) | 0 (0.0) |
| Yeri Centre | 35.4 | 344 | 8 (2.3) | 222 (64.5) | 1 (0.3) |
| Overall | 15,699 | 798 (5.1) | 5046 (32.1) | 445 (2.8) |
| Total Number of Participants | Persons with Epilepsy, n ‰ (95%CI) | Nodding Syndrome, n ‰ (95%CI) | |
|---|---|---|---|
| Sex | |||
| Female | 7847 | 378 (48.2, 43.7–53.1) | 168 (21.9, 18.8–25.5) |
| Male | 7845 | 419 (53.4, 49.7–58.6) | 184 (23.5, 20.3–27.0) |
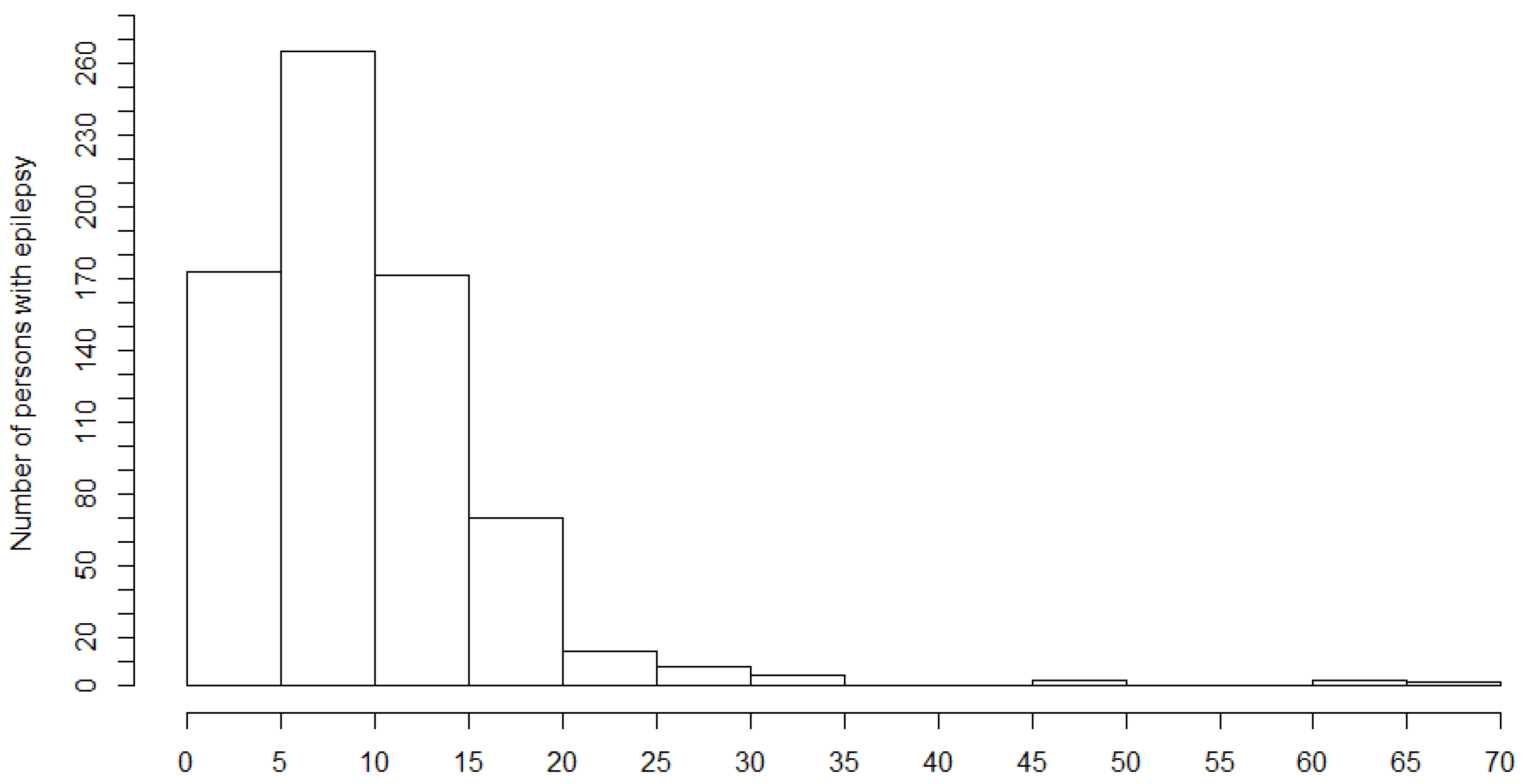
| Age groups in years | |||
| 0−4 | 1919 | 6 (3.1, 1.4–6.8) | 3 (1.6, 0.5–4.6) |
| 5−10 | 2928 | 31 (10.6, 7.5–15.0) | 20 (6.8, 4.4–10.5) |
| 11−15 | 2105 | 122 (58.0, 48.8–68.8) | 67 (31.8, 25.1–40.2) |
| 16−20 | 2459 | 277 (112.3, 100.8–125.8) | 138 (56.1, 47.7–65.9) |
| 21−25 | 1244 | 175 (140.7, 122.5–161.1) | 73 (58.7, 46.9–73.2) |
| 26−30 | 1447 | 109 (75.3, 62.8–90.1) | 34 (23.5, 16.9–32.7) |
| 31−35 | 754 | 35 (46.4, 33.6–63.9) | 10 (13.3, 7.2–24.2) |
| 36−40 | 1079 | 24 (22.1, 15.0–32.9) | 4 (3.7, 1.4–9.5) |
| 41−45 | 492 | 6 (12.2, 5.6–16.3) | 1 (2.0, 0.4–11.4) |
| >45 | 1272 | 13 (10.2, 6.0–17.7) | 2 (1.6, 0.4–5.7) |
| Overall | 15,699 | 798 (50.8, 47.6–54.4) | 352 (22.4, 20.1–24.7) |
| Characteristics | |
| Female, n (%) | 378 (47.4) |
| Age (years), median (IQR) | 20 (17.0–25.0) |
| Born in the village, n (%) | 731 (91.6) |
| Period (years) of residing in the survey area, median (IQR) | 20 (15.0–25.0) |
| Epilepsy Symptoms | |
| Age onset of the first seizure in all PWE, median (IQR)d | 10.0 (6.0–15.0) |
| Age onset of the first nodding seizure, median (IQR) | 7.0 (5.0–10.0) |
| Onset of the first seizure last year, n (%) | 13 (1.6) |
| Seizures in the last year, n (%) | 729 (91.8) |
| Sudden loss of consciousness, n (%) | 738 (92.5) |
| Loss of bladder control #, n (%) | 458 (62.1) |
| Foaming at the mouth #, n (%) | 654 (88.6) |
| Biting of the tongue #, n (%) | 499 (67.6) |
| Most Frequent Seizure Types | |
| Generalized convulsive seizures, n (%) | 614 (80.3) |
| Atonic seizures (drop attacks), n (%) | 79 (9.9) |
| Absences, n (%) | 79 (9.9) |
| Nodding seizures, n (%) | 317 (39.7) |
| Focal motor seizures with decreased consciousness | 4 (0.5) |
| Focal motor seizures without loss of consciousness, n (%) | 1 (0.1) |
| Frequency of Seizures | |
| Daily seizures, n (%) | 210 (26.8) |
| Weekly seizures, n (%) | 191 (24.4) |
| Monthly seizures, n (%) | 342 (43.7) |
| Yearly seizures | 39 (5.0) |
| Experienced seizure in the last 12 months, n (%) | 729 (91.8) |
| Family Members with Epilepsy | |
| Family history of seizures, n (%) | 483 (60.8) |
| Siblings (brother/sister) *, n (%) | 366 (75.6) |
| Father *, n (%) | 8 (1.6) |
| Mother *, n (%) | 1 (0.2) |
| Grandparent *, n (%) | 49 (10.1) |
| Seizures/Head Nodding Triggers | |
| Spontaneous (no obvious trigger), n (%) | 666 (83.7) |
| Sight of food, n (%) | 134 (16.8) |
| Cold weather, n (%) | 114 (14.3) |
| New moon appearance, n (%) | 29 (3.6) |
| Sunlight/sunset, n (%) | 10 (1.2) |
| Psychomotor Development during Childhood | |
| Normal growth prior to the seizure onset, n (%) | 722 (90.8) |
| Normal psycho-motoric development prior to the seizure onset, n (%) | 715 (89.9) |
| Intellectual disability prior to seizure onset, n (%) | 63 (7.9) |
| Severe Disease Preceding the Onset of Epileptic Seizures | |
| Measles, n (%) | 39 (4.9) |
| Malaria, n (%) | 110 (14.2) |
| Encephalitis/meningitis, n (%) | 19 (2.4) |
| Head injury with loss of consciousness, (%) | 16 (2.0) |
| Prolonged post-traumatic coma, n (%) | 6 (0.7) |
| Tuberculosis, n (%) | 2 (0.2) |
| Persistent headache, n (%) | 3 (0.2) |
| Diarrhoea, n (%) | 4 (0.5) |
| Physical Examination | |
| Blind, n (%) | 32 (4.0) |
| Facial abnormalities, n (%) | 18 (2.2) |
| Cervical lymph nodes, n (%) | 12 (1.5) |
| Nakalanga features, n (%) | 51 (6.4) |
| Itching, n (%) | 302 (37.8) |
| Burn lesions, n (%) | 115 (14.4) |
| Papular/nodular pruritic skin, n (%) | 63 (7.9) |
| Leopard skin, n (%) | 15 (1.9) |
| Dry, thickened, or wrinkled skin, n (%) | 30 (3.8) |
| Neurological Examination ** | |
| Disoriented in place/time/person, n (%) | 86 (10.8) |
| Paresis, n (%) | 27 (4.6) |
| Behavioural problem, n (%) | 51 (8.7) |
| Epilepsy Classification | |
| Epilepsy without head nodding, n (%) | 446 (55.9) |
| Head nodding, n (%) | 82 (10.3) |
| Head nodding plus other seizure types, n (%) | 270 (33.8) |
| Current Seizure Medication | |
| Never used anti-seizure medication, n (%) | 112 (14.0) |
| Traditional treatment, n (%) | 1 (0.1) |
| Ever used anti-seizure medication, n (%) | 15 (1.9) |
| Currently use anti-seizure medication, n (%) | 644 (80.7) |
| Anti-Seizure Medication | |
| Phenobarbital, n (%) | 89 (11.1) |
| Phenytoin, n (%) | 32 (4.0) |
| Carbamazepine, n (%) | 545 (68.3) |
| Sodium valproate, n (%) | 5 (0.6) |
| Ivermectin Use | |
| Ever taken ivermectin, n (%) | 661 (82.8) |
| Never received ivermectin, n (%) | 95 (11.9) |
| Ivermectin Intake the Year before the Survey | |
| No ivermectin, n (%) | 119 (14.9) |
| Ivermectin intake, n (%) | 645 (80.8) |
| Ivermectin intake not known, n (%) | 34 (4.3) |
| Meeting the OAE criteria, n (%) *** | 556 (78.4) |
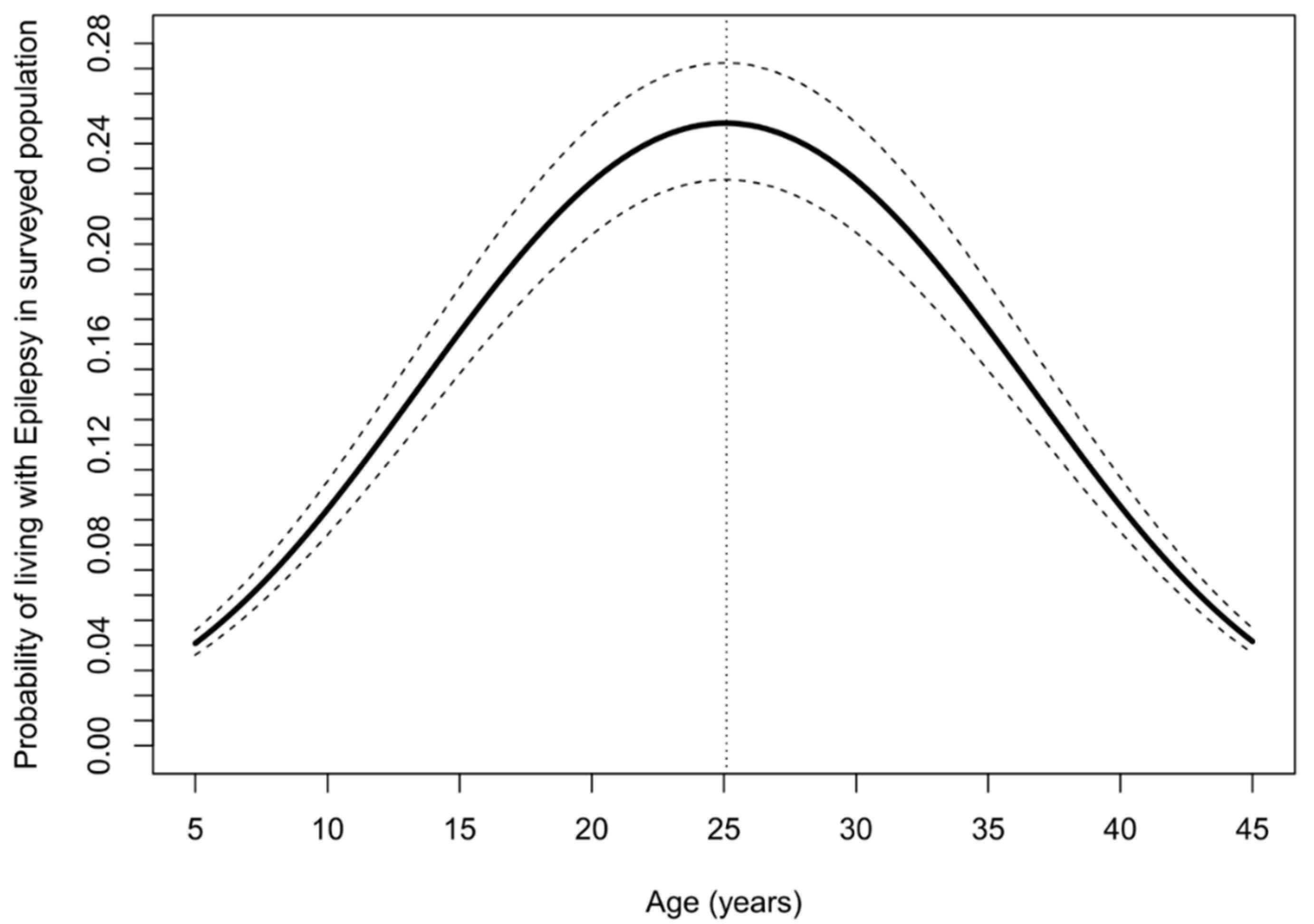
| Parameter | Estimate | 95% CI | p-Value | |
|---|---|---|---|---|
| Intercept | 0.006 | 0.002 | 0.018 | <0.001 |
| Age (years) | 1.291 | 1.194 | 1.397 | <0.001 |
| Age × age (years) | 0.995 | 0.993 | 0.997 | <0.001 |
| Male vs. female | 1.239 | 1.065 | 1.441 | 0.006 |
| Farming vs. no farming | 0.996 | 0.832 | 1.192 | 0.963 |
| Fishing vs. no fishing | 0.409 | 0.079 | 2.112 | 0.286 |
| Employee vs. non-employee | 1.212 | 0.377 | 3.893 | 0.747 |
| Cattle keeping vs. no cattle in the households | 0.744 | 0.297 | 1.863 | 0.528 |
| Skin itching vs. no itching | 1.308 | 1.102 | 1.552 | 0.002 |
| Blindness | 2.031 | 1.280 | 3.222 | 0.003 |
| Recent ivermectin vs. no ivermectin intake | 1.112 | 0.916 | 1.349 | 0.283 |
| Distance to the river (kilometer) | 0.986 | 0.978 | 0.993 | 0.001 |
| Age (Years) | Ov16 Positive, n (%, 95% CI) | Ivermectin Use, n (%, 95% CI) |
|---|---|---|
| 3 (n = 26) | 3 (11.5, 4.0–28.9) | |
| 4 (n = 24) | 5 (20.8, 9.2–40.5) | |
| 5 (n = 25) | 8 (32.0, 17.2–51.6) | 6 (24.0, 11.5–43.4) |
| 6 (n = 22) | 7 (31.8, 14.3–47.6) | 7 (31.8, 14.3–47.6) |
| 7 (n = 15) | 7 (46.7, 24.8–68.9) | 7 (46.7, 24.8–68.9) |
| 8 (n = 20) | 4 (20.0, 8.1–41.6) | 6 (30.0, 14.5–51.9) |
| 9 (n = 18) | 7 (38.8, 20.3–61.4) | 9 (50.0, 29.0–70.9) |
| Overall (n = 150) | 41 (27.3, 20.8–34.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raimon, S.; Dusabimana, A.; Abd-Elfarag, G.; Okaro, S.; Carter, J.Y.; Newton, C.R.; Logora, M.Y.; Colebunders, R. High Prevalence of Epilepsy in an Onchocerciasis-Endemic Area in Mvolo County, South Sudan: A Door-To-Door Survey. Pathogens 2021, 10, 599. https://doi.org/10.3390/pathogens10050599
Raimon S, Dusabimana A, Abd-Elfarag G, Okaro S, Carter JY, Newton CR, Logora MY, Colebunders R. High Prevalence of Epilepsy in an Onchocerciasis-Endemic Area in Mvolo County, South Sudan: A Door-To-Door Survey. Pathogens. 2021; 10(5):599. https://doi.org/10.3390/pathogens10050599
Chicago/Turabian StyleRaimon, Stephen, Alfred Dusabimana, Gasim Abd-Elfarag, Samuel Okaro, Jane Y. Carter, Charles R. Newton, Makoy Yibi Logora, and Robert Colebunders. 2021. "High Prevalence of Epilepsy in an Onchocerciasis-Endemic Area in Mvolo County, South Sudan: A Door-To-Door Survey" Pathogens 10, no. 5: 599. https://doi.org/10.3390/pathogens10050599
APA StyleRaimon, S., Dusabimana, A., Abd-Elfarag, G., Okaro, S., Carter, J. Y., Newton, C. R., Logora, M. Y., & Colebunders, R. (2021). High Prevalence of Epilepsy in an Onchocerciasis-Endemic Area in Mvolo County, South Sudan: A Door-To-Door Survey. Pathogens, 10(5), 599. https://doi.org/10.3390/pathogens10050599







