Abstract
Mycoplasma pneumoniae is a major causative agent of community-acquired pneumonia which can lead to both acute upper and lower respiratory tract inflammation, and extrapulmonary syndromes. Refractory pneumonia caused by M. pneumonia can be life-threatening, especially in infants and the elderly. Here, based on a comprehensive review of the scientific literature related to the respective area, we summarize the virulence factors of M. pneumoniae and the major pathogenic mechanisms mediated by the pathogen: adhesion to host cells, direct cytotoxicity against host cells, inflammatory response-induced immune injury, and immune evasion. The increasing rate of macrolide-resistant strains and the harmful side effects of other sensitive antibiotics (e.g., respiratory quinolones and tetracyclines) in young children make it difficult to treat, and increase the health risk or re-infections. Hence, there is an urgent need for development of an effective vaccine to prevent M. pneumoniae infections in children. Various types of M. pneumoniae vaccines have been reported, including whole-cell vaccines (inactivated and live-attenuated vaccines), subunit vaccines (involving M. pneumoniae protein P1, protein P30, protein P116 and CARDS toxin) and DNA vaccines. This narrative review summarizes the key pathogenic mechanisms underlying M. pneumoniae infection and highlights the relevant vaccines that have been developed and their reported effectiveness.
1. Introduction
Community-acquired pneumonia (CAP) is associated with high morbidity and mortality, and the disease is also a major threat to public health worldwide [1]. About 8–40% of CAP in children admitted to hospitals were caused by Mycoplasma pneumoniae [2,3,4]. Based on the reported cases in China, M. pneumoniae infections accounted for 19.2% of all CAP cases in adults, and the prevalence of CAP in children and teenagers, ranged from 10% to 30% [1,5]. In the USA, a recent study of 2254 hospitalized children with CAP showed that 8% children with median age of 7 years were positive for M. pneumoniae by polymerase chain reaction (PCR) [6].
Airborne droplets containing M. pneumoniae can be transmitted and spread among people through coughing and sneezing. M. pneumoniae causes both upper and lower respiratory tract infections, and in most cases the clinical symptoms are non-specific [7]. Tracheobronchitis is the most common type of lower respiratory infection, the incidence of which is about 20 times that of pneumonia, and 10–40% of respiratory tract infections caused by M. pneumoniae will eventually develop into pneumonia [8]. While most pneumonia caused by M. pneumoniae (MPP) cases are benign, some cases may develop into severe pneumonia and refractory pneumonia with pleural effusion, multi-organ dysfunction, and serious long-term sequelae, including bronchiolitis obliterans and bronchiectasis [9]. Although CAP is the most significant disease caused by M. pneumoniae, the pathogen is known to cause upper respiratory tract infections. Pharyngitis is commonly reported while rhinosinusitis and otitis media are less frequently encountered in upper respiratory tract infections caused by M. pneumoniae [7].
M. pneumoniae respiratory infections are associated with asthma exacerbation during which patients will suffer from a combination of symptoms including sudden or progressive coughing, respiratory distress, wheezing or chest pain [10,11]. The onset of asthma is due to the release of Mycoplasma-mediated cytokine in infected patients [12]. Respiratory infections caused by M. pneumoniae are also associated with a wide array of extrapulmonary manifestations such as meningoencephalitis, myocarditis, nephritis, atherosclerosis and mucocutaneous eruptions, etc. [13,14,15,16,17]. More importantly, M. pneumoniae induces mucocutaneous diseases include Stevens-Johnson syndrome and M. pneumoniae-associated mucositis. These mucocutaneous diseases are frequently associated with systemic inflammation and higher risk of the occurrence of long-term sequelae [18,19,20,21].
Due to the atypical symptoms produced during M. pneumoniae infection, pneumonia can be underestimated during the early stage of infection. There are no distinctive clinical or radiographic features in patients with M. pneumoniae infections, so laboratory diagnosis mainly based on rapid culture of throat swab specimens, PCR and serological assays. Furthermore, enzyme-linked immunosorbent assays (ELISA) detecting the N-terminal fragment of P116 protein and the C-terminal region of P1 protein both hold promise for serodiagnosis [22,23]. The IgM ELISA assays based on the short recombinant P116 and P1 proteins were shown to improve the specificity of the immunodiagnostic assay [22].
Although M. pneumoniae infection is generally self-limiting and does not require antibiotic treatment, patients of all age groups can develop severe, life-threatening or extrapulmonary diseases [24]. Antibiotics such as tetracycline and fluoroquinolone have been reported to be effective in eliminating M. pneumoniae infections [25] but tetracyclines cause discoloration of bones and teeth in young children. Fluoroquinolones can also affect the muscle, joint and tendon. Instead, macrolides, which have fewer side effects, have been the drug of choice for treating M. pneumoniae infection in past years [26]. More worrisome is that the extensive use of macrolides in China has led to a particularly high rate of macrolide resistance in this organism (69%~95%) [27]. The emergence of antibiotic resistance represents another challenge regarding the treatment of M. pneumoniae infections. Failure in antibiotic treatment has caused an increase in mortality rate during recent years [28]. Although the clinical outcomes of infections caused by macrolide-susceptible and -resistant M. pneumoniae isolates are not significantly different, patients infected with macrolide-resistant isolates had a longer febrile period (1.71 days), length of hospital stay (1.61 day), antibiotic drug courses (2.93 days), and defervescence time after macrolide treatment (2.04 days) compared to patients infected with macrolide-sensitive isolates [29]. Furthermore, macrolide-resistant strains may be associated with more extrapulmonary complications, and severe clinical and radiological features [24,30]. Hence, the development of vaccines against M. pneumoniae infections is a potential solution for the prevention of infections caused by the pathogen.
2. Virulence and Pathogenesis of M. pneumoniae
M. pneumoniae encodes a variety of virulence factors, which include adhesins, glycolipids, toxic metabolites, community-acquired respiratory distress syndrome (CARDS) toxin, and capsular polysaccharides. Table 1 summarizes the key virulence factors associated with M. pneumoniae.

Table 1.
Key virulence factors of M. pneumoniae.
2.1. Adhesins
M. pneumoniae attaches to epithelial cell surfaces with a high affinity for human respiratory epithelial cells. The pathogen has no cell wall and colonizes the respiratory tract via its specific attachment organelle, which is a protrusion at one end of the Mycoplasma pneumoniae cell (Figure 1). The attachment organelle consists of internal and surface structures [58]. The internal structure is made up of a dumbbell-shaped terminal button consisting of three protein molecules (HMW2, HMW3, and P65), paired plates (HMW1, HMW2, CpsG, and HMW3), and a bowl complex (Lon, P24, TopJ, P200, P41, MPN387, and HMW2). The Nap structure in the surface adhesion complex consists of the main adhesins (P1 and P30) and accessory proteins (P40 and P90) surrounding the cell membrane (Figure 1). During gliding, the force generated at the bowl complexes is transmitted through the paired plates and reaches the P1 adhesin complex [58]. P30 adhesin is a membrane protein at the distal end of the attachment organelle, required for cytoadherence, gliding motility and stabilization of the accessory protein P65 [33]. Interaction of the M. pneumoniae attachment organelle with the host’s respiratory epithelium induces cytoskeleton rearrangement in the host cell, which promotes intracellular delivery of the pathogen [59,60].
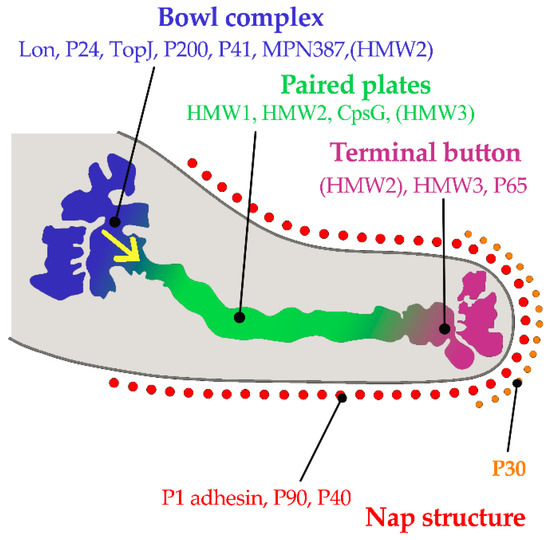
Figure 1.
Component proteins of the internal structure of attachment organelle and proposed mechanism of movements for gliding in M. pneumoniae. HMW1, HMW2, and HMW3 refer to three high molecular weight (HMW) proteins. The force is generated at the bowl complexes, transmitted through the paired plates, and reaches the P1 adhesin complex in the direction of the yellow arrow. (Based on ideas from Nakane, et al. [58]). Copyright: ©2015. Public Library of Science. Creative Commons Attribution License and disclaimer available from: http://creativecommons.org/licenses/by/4.0/.
The host receptors for M. pneumoniae are sialylated glycoproteins on the respiratory epithelium. The nature and density of host receptor moieties affect the attachment and gliding mobility of the pathogen. P1 adhesin binds to both α-2,3 and α-2,6 linkages, but only the latter type of linkage supports gliding of M. pneumoniae [61].
Attachment and invasion of M. pneumoniae produces direct damage to the host’s respiratory epithelium [59,62]. Disturbance of carbohydrate metabolism, amino acid intake and protein synthesis of the host cell results in nutrient depletion [46] Furthermore, the oxygen radicals generated by the pathogen in the host cell can lead to cilia destruction and host cell damage [63,64].
2.2. Inflammation Injury
Bacterial cellular components, metabolites and toxins released from M. pneumoniae are able to induce damage in the host tissues. These include cytotoxicity, oxidative damage, apoptosis and immune-pathological damage.
2.2.1. Enzymes and Metabolites
The enzyme, HapE, of M. pneumoniae is a virulence factor that can produce H2S by the desulfurization of cysteine [47,48] which can lead to erythrocyte lysis. This enzyme mediates inflammatory reactions via adenosine triphosphate (ATP)-sensitive K+ channels [65]. Oxidation of glycerol by the pathogen produces toxic metabolites [66] including hydrogen peroxide [67,68] which injures cells by causing inflammation. In addition, the Ca2+-dependent cytotoxic nuclease (encoded by MPN133) produced by M. pneumoniae can lead to apoptotic-like programmed cell death in the host.
2.2.2. Lipoproteins
More than 50 different lipoproteins have been identified in M. pneumoniae, many of them involved in inflammatory reactions [69]. The transcription of M. pneumoniae lipoprotein genes are regulated in response to changes in environmental conditions (e.g., oxidative and acidic stress) [70,71]. The N-terminal region of all the lipoproteins contains a lipid-cysteine structure and these lipoproteins induce inflammation [69]. M. pneumoniae lipoproteins can be recognized by toll-like receptor (TLR)1, TLR2 and TLR6, which stimulate the release of proinflammatory cytokines including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6 and other inflammatory mediators via the nuclear factor κB (NF-κB) pathway [72,73].
2.2.3. Community-Acquired Respiratory Distress Syndrome (CARDS) Toxin
The CARDS toxin encoded by MPN372 is a unique bacterial adenosine diphosphate (ADP)-ribosylating and vacuolating toxin produced by M. pneumoniae [74,75]. The structure of CARDS toxin comprises a triangular molecule in which N-terminal mono-ADP ribosyl-transferase (mART) and C-terminal tandem β-trefoil domains associate to form a unique overall architecture different from other well-recognized ADP-ribosylating bacterial toxins [53]. CARDS toxin demonstrates high binding affinity to human surfactant protein A and annexin A2 when present in the airway epithelia and exhibits specific biological activities including mono-ADP ribosylation and vacuolization [53,74]. CARDS toxin binds to mammalian cell surface receptors and is internalized rapidly in a dose and time-dependent manner. The internalization process is mediated by clathrin molecules, which form a molecular scaffold for uptake of CARDS toxin [76]. The toxin is cytotoxic to mammalian cells by activation of the NLRP3-associated inflammasome and further promotes the release of IL-1β and IL-18 [77,78,79]. CARDS toxin increases the expression of the proinflammatory cytokines IL-1β, IL-6 and TNF-α in a dose- and activity-dependent manner [80]. CARDS toxin is capable of inducing an allergic-type inflammation in animals [81,82], but there is no convincing evidence that CARDS toxin is a causal factor of M. pneumoniae-associated asthma.
2.2.4. Lipids
The cell membrane of M. pneumoniae has a high lipid content (comprising primarily of the acidic glycerophospholipids phospholipids and cholesterol), which can infiltrate the host epithelial cells, disrupt the lipid bilayer of the cell membrane and cause leakage of ionic metabolites [54,55]. Furthermore, some scholars speculate that these lipids may act as potential TLR4 ligands for binding to TLR4 and elicit macrophage autophagy, eventually leading to the secretion of proinflammatory cytokines [50,83] and triggering typical host cell inflammatory responses [50,84].
2.2.5. Capsules
M. pneumoniae has a capsular structure made up of polysaccharides [52] which may be potential virulence factors and are immunogenic, but its functional role in pathogenesis remains unclear and needs to be further explored [85,86,87].
2.3. Immune Evasion
M. pneumoniae has multiple strategies to escape host immune responses in order to ensure survival of the pathogen. Its survival includes immune evasion which may play an important role in pathogenesis. Inadequate immune responses against the invading pathogen results in uncontrolled proliferation and host tissue damage [88].
2.3.1. Molecular Mimicry
The term molecular mimicry can be described simply as “pathogens sharing a structural relationship with the host are tolerated as self, just like constituents of the host” [2,88,89]. The immune response targets the pathogen-peptide mimicking the host’s self-antigen, leading to the activation of naive, autoreactive T-cells specific to the corresponding self-antigen [89]. M. pneumoniae antigen mimics host cell components, thus the host immune response induced by the pathogen causes auto-immune responses and injuries to multiple organs [2,90].
The C-terminal region of the P1 and P30 proteins in M. pneumoniae show high levels of homology to troponin, cytoskeletal proteins, keratin and fibrinogen of the host [46,91]. Antibodies produced in response to M. pneumoniae infections will target various host tissues and form immune complexes, which aggravates the autoimmune response, leading to inflammatory injuries in the extrapulmonary tissues [13,46].
2.3.2. IbpM
Immunoglobin binding protein (IbpM) is a surface protein encoded by MPN400 that binds strongly to various immunoglobulins (IgM, IgG, and IgA) produced by the host [45]. Blötz et al. demonstrated that IbpM was required by M. pneumoniae to produce cytotoxic effects in host cells and is thus regarded as a virulent factor [45].
2.3.3. Antigen Variation
It has been observed that the surface adhesins P1, P40, and P90 of Mycoplasma pneumoniae display sequence variation [92,93]. Sluijter et al. demonstrated that the RecA protein homolog encoded by MPN490 promoted gene exchange between homologous DNA sequences (RepMP) in M. pneumoniae [94]. The RepMP are repetitive sequences present within genes encoding surface proteins such as the adhesins. Homologous recombination between these RepMP sequences generates sequence changes within the adhesin genes, which results in variations of surface adhesins and facilitates evasion of host immune surveillance [94,95,96].
The role of post-translational modifications of M. pneumoniae-specific proteins (e.g., P1, P40, P90) is a relatively new aspect of bacterial epigenetics [34]. The posttranslational modification of cytoadherence proteins by the protein kinase PrkC is essential for the development and function of the M. pneumoniae terminal organelle [97]. P1 adhesin of M. pneumoniae M129 is subject to extensive post-translational processing forming 22 proteo-forms, which are specific molecular forms of a protein product arising from a specific gene. Each of the proteo-forms retain the ability to bind to host molecules or their structural mimics and are surface accessible [31]. There are many issues that require further study, such as whether the antigen variations caused by post-translational modifications can affect the pathogenicity of M. pneumoniae.
2.3.4. Intracellular Survival
M. pneumoniae can survive for a long time in the human lung carcinoma cell (A549) [98], but the pathways related to intracellular survival remain to be elucidated. Intracellular M. pneumoniae has mechanisms to protect the pathogen against phagocytosis and antibiotics. This may explain why M. pneumoniae infection can develop into chronic lung disease, such as refractory pneumonia caused by macrolide-resistant M. pneumoniae due to the lack of timely and effective antibiotic treatment.
2.3.5. Others
Moreover, M. pneumoniae has an antioxidant mechanism to protect against oxidative reactions such as reactive oxygen species (ROS) damage [46,99]; A nuclease encoded by MPN491 can degrade neutrophil extracellular traps (NETs), which helps the pathogen to escape from the immune attack of host cells [44].
In summary, the pathogenesis of M. pneumoniae involves mainly the following four factors: immune evasion, adhesion, inflammatory injury and cytotoxicity. Figure 2 shows these four key pathogenic mechanisms of M. pneumoniae infection.
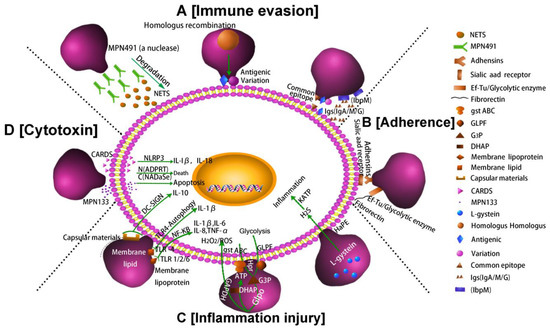
Figure 2.
Pathogenic mechanisms of M. pneumoniae. (A) Nuclease and IbpM in M. pneumoniae enable immune evasion, and homologous DNA recombination leads to antigen variation; (B) M. pneumoniae adhesion causes cell damage. Additionally, the P1 adhesin protein binds to the sialic acid receptor on the host cell surface contributing to M. pneumoniae adherence and gliding. Furthermore, elongation factor Tu (EF-Tu) can bind strongly to a diverse range of host molecules (such as fibronectin), contributing to adhesion; (C) Inflammation-inducing factors (HapE enzyme, oxidase GlpO, membrane lipids, lipoproteins, and capsular materials) activate host cell inflammatory pathways; (D) M. pneumoniae secretes cytotoxic nuclease (catalytic protein encoded by MPN133) and CARDS toxin.
3. Development of Vaccines against M. pneumoniae Infections
M. pneumoniae is a significant bacterial pathogen causing CAP. The lack of cell wall in M. pneumoniae greatly reduces the choice of current antibiotics. Furthermore, the increased number of refractory infections caused by macrolide-resistant M. pneumoniae makes clinical treatment extremely difficult, especially for children. Although the mortality and disability rates caused by M. pneumoniae infection are low, complications, and even fatal pneumonia, can occur in susceptible individuals (children of 5–15 years, adolescents, and the elderly of >60 years) in an epidemic area. At present, no vaccine is available for protection against M. pneumoniae infections. In view of the increasing importance of M. pneumoniae infection, there is an urgent need for an effective vaccine.
The types of vaccines that are most studied in M. pneumoniae include inactivated, live-attenuated, protein subunit and recombinant DNA vaccines. The vaccines are mainly developed to be administered via the nasal or parental route. It has been reported that nasal administration of inactivated vaccine elicited low levels of protection resulting in a high reinfection rate [100]. For vaccinated individuals who did not produce protective antibodies, M. pneumoniae reinfection could lead to an early hyper-accentuated histopathological response [100,101].
3.1. Whole-Cell Vaccines
Various M. pneumoniae vaccines developed from whole-cell antigen, including both inactivated and live-attenuated vaccines, have been reported since 1964. The protective effects of these vaccines were tested on military personnel [102,103,104,105,106], a small number of volunteers [107,108,109,110] and animal models [111,112]. These vaccines have been reported to have low efficiencies in reducing the incidence and disease severity [113,114,115]. A meta-analysis suggested that inactivated vaccines reduced the incidence of both M. pneumoniae (MPP) and respiratory infections by ~40% only [100]. Inactivated M. pneumoniae vaccines supplemented with alum adjuvant and increased dosage of vaccines were found to improve the immunogenicity and protective efficiency [116]. However, the improvement in vaccine efficiencies was observed in animal models, but still less effective in humans [113,114,115]. After inoculating with inactivated vaccines, most of recruited subjects showed no significant adverse reactions (including autoimmune responses) and vaccination did not exacerbate disease upon subsequent homologous challenge [117,118,119]. However, disease was more severe in human subjects who lacked an antibody response following vaccination [110].
In comparison, there were less studies of live-attenuated vaccines against M. pneumoniae. Live-attenuated vaccines were often prepared by continuous passage in vitro [107,111,120] and/or produced by temperature-sensitive mutants [121,122]. Live-attenuated vaccines were found to induce protective effect in hamsters. Clinical trials for efficiency evaluation of live-attenuated vaccine were never performed in humans because of the significant health risk involved [107,109,110].
3.2. Recombinant Protein Subunit Vaccines
As a group of important adhesion factors in M. pneumoniae, P1, P30 and other adhesion-associated protein have immunogenicity and immunoreactivity and are able to induce specific neutralizing antibodies. Currently, the strategies involved in the preparation of recombinant protein subunit vaccines include the employment of cell or cell-free protein synthesis system. So far, a number antigen targets for vaccine development were identified (Table 1). Among these virulence factors, cytoadherence proteins (including P1, P30, P116, CARDS toxin), polysaccharides, lipids and lipoproteins have immunogenicity and are likely to be potential candidates for vaccines antigens.
3.2.1. P1 Adhesin Protein Vaccine
P1 plays an important role in the pathogenesis of M. pneumoniae infection by mediating the attachment of the pathogen to host cells [123], and the p1 gene is used as target to detect M. pneumoniae by qRT-PCR, as well as to perform genotyping [124,125]. Although it is unclear whether genotype-specific antibodies have an influence on re-infections due to different genotypes of M. pneumoniae, genotyping is also crucial for the molecular epidemiological studies and the development of an effective vaccine [126]. Protein P1 is a transmembrane adhesin, and it has high immunogenicity and antigenic specificity [127,128] which means its epitopes were not or rarely found in other bacterial species. Intramuscular or intranasal inoculation of BALB/c mice with a DNA vaccine encoding amino acid 1125–1359 of the M. pneumoniae P1 protein C-terminal region (P1C) led to detectable protection against M. pneumoniae infection. The levels of IgG (IgG1, IgG2a, and IgG2b isotypes) and cytokines (IFN-γ and IL-4) were significantly elevated [129]. However, the effect of P1C DNA vaccine in humans remains unknown and requires further research.
3.2.2. P30 Vaccine
P30 is a transmembrane protein and is required for host receptor binding [58]. Similar to P1, P30 is also an important immunogenic factor [130]. Mutant M. pneumoniae without the gene encoding P30 is noninfectious and unable to adhere to host cells [45], which suggests that P30 could potentially be an ideal candidate target for a clinical vaccine. Szczepanek et al. created an avirulent P30 adhesin mutant for assessing its efficacy as a live-attenuated vaccine candidate in mice [112]. However, the live-attenuated vaccine caused severe complications in BALB/c mice, which appears to be driven by responses of the T helper type 17 (Th17) cells. In the recent years, a large number of studies have reported that Th17 cells play an important role in antimicrobial immune responses and causing autoimmune diseases in mouse models [131,132].
On the other hand, vaccine produced from recombinant P30 adhesin was found to elicit immune protection. Hausner et al. (2013) created a recombinant protein by combining protein P30 (amino acids 17 to 274) with the C-terminal of P1 adhesin (amino acids 1287–1518 of P1) [133]. When this recombinant vaccine was injected into guinea pigs, protective IgA were secreted in the respiratory tracts of the animals. These results provide insights into vaccine development for effective protection against M. pneumoniae infection in humans.
3.2.3. P116 Vaccine
P116 protein is another major antigen of M. pneumoniae and an important cellular adhesion factor [36,134]. It is a 116kDA protein consisting of 1030 amino acids. Svenstrup et al. has purified the P116 protein and found that polyclonal antibodies raised against this protein prevented M. pneumoniae adhesion to Hep-2 cells [135]. Additionally, the serum obtained from M. pneumoniae-infected patients contained antibodies that specifically reacted with P116 [136].
3.2.4. CARDS Toxin Vaccine
As mentioned elsewhere in this review, CARDS toxin is a specific virulence factor associated with M. pneumoniae pathogenesis. The amount of toxin produced is positively correlated with the severity of pulmonary disease [46,76]. In a BALB/cJ mouse model, CARD toxin dosage was correlated with inflammatory responses characterized by airway restriction and decreases in lung compliance [81]. Antibody against CARDS toxin was identified in the serum of M. pneumoniae-infected patients during both the acute infection and recovery periods, with higher levels in the recovery period. Analysis of serum antibodies on day 28 after the onset of M. pneumoniae infection showed that antibody against CARDS toxin was positive, while low levels of CARDS toxin-reactive antibodies were identified in the serum of healthy controls [75]. There was study showing that, the C-terminal region of CARDS toxin triggered an antibody response upon M. pneumoniae infection [137], this provides insights into the development of vaccine using attenuated CARDS toxin.
3.2.5. Recombinant Combined Vaccines
As described earlier, some apical organelle-localized proteins (P1, P30, P116, etc.) had immunogenicity [22,130]. Hence genetically engineered recombinant proteins by screening antigen dominant epitopes to stimulate the humoral immune response are promising vaccine candidates for preventing M. pneumoniae infection. Chen et al. designed a chimeric protein (P116N-P1C-P30), designated MP559, which contained various antigen epitopes of three antigens [138]. Vaccination with MP559 stimulated the same humoral immune response as the three antigens alone. The study showed that chimeric protein MP559 has the potential to replace the three individual protein subunit vaccine candidates.
3.2.6. Other Vaccines
In addition, the success of capsular polysaccharide vaccines against Streptococcus pneumoniae and Neisseria meningitidis provides enlightenment for the use of purified specific polysaccharides to develop a M. pneumoniae vaccine. But a recent study has revealed that antibodies to protein but not glycolipid structures are important for host defense against M. pneumoniae [139]. So, vaccines using other virulence factors as antigens (such as polysaccharides, lipids, glycolipid) may be unable to induce persistent protective immunity and the molecular mimicry-induced cross-reactive immunity may cause injury to multiple organs.
3.3. DNA Vaccines
DNA vaccines are emerging biotechnology products that involve novel approach to induce immune responses against the target immunogens. The immunogen is expressed in vivo from a DNA vector carrying the gene encoding the immunogen [140]. Compared with traditional vaccines, DNA vaccines have certain obvious advantages. First, they can be easily constructed and pose no infection risk. Second, they trigger immune responses corresponding to those produced against natural antigens. Third, the cost of producing, storing, and transporting DNA vaccines is lower than the cost associated with protein vaccines. DNA vaccines for preventing M. pneumoniae infection was shown induce both strong humoral and cell-mediated immunity (Th1 and Th2 responses), although antibody production by B-cells has been shown to be lower than that associated with traditional vaccines [141,142,143]. In addition to the P1C DNA vaccine [129], another DNA vaccine produced by fusing P1C with the E. coli heat-labile toxin B subunit (LTB) gene has been studied [144]. The LTB-P1C fusion DNA vaccine was shown to stimulate immune protection against M. pneumoniae infection in a BALB/c mouse model, with less pathological inflammation [144]. Besides, the study also demonstrated that production of M. pneumoniae-specific IgA and IgG2a/IgG1 ratios in the bronchoalveolar lavage fluid and sera were significantly higher in mice vaccinated with the LTB-P1C fusion DNA vaccine than in mice vaccinated with the P1C DNA vaccine [144]. Of course, there are also multiple obstacles that need to be overcome before DNA vaccines can be used in humans. These hurdles include target gene selection, fate of the injected DNA, immune tolerance, potential integration of the injected DNA material with human chromosomes and uncontrolled expression in vivo.
3.4. Live Vector Vaccines
In 1980, a Swiss scholar first reported DNA (SV40 DNA) can be transferred from bacteria to higher organisms (e.g., CV-1 cells), which also laid the foundation for research of live vector vaccines (LVVs) [145]. LVVs are produced by introducing a specific antigen gene into known bacteria using plasmid vector or by integrating into the bacterial chromosome. When the live bacteria are being taken orally by the vaccine recipient, the antigen gene is being expressed by the bacteria inside the recipient’s body to produce an antigen and then stimulate a specific immune response. The bacterial strains used in LVVs are avirulent organism (e.g., Bacillus subitilis), probiotics (Lactobacillus) or attenuated strains (e.g., attenuated Listeria monocytogenes strains) [146]. LVVs are associated with several advantages, including safety, stimulation of long-term humoral and mucosal immunity, and multivalent vaccines, making LVV promising candidates for successful vaccination. There are also certain issues, including unstable expression of foreign genes and reversion of the live-attenuated vector to a virulent form.
In the recent years, there are more LVVs that have been studied and some of them exhibited the potential for infection prevention, which makes the idea of developing an LVV to prevent M. pneumoniae infection more promising. Currently, there is no LVVs for preventing M. pneumoniae infection, but there is one for preventing infection of pigs with Mycoplasma hyopneumoniae [147]. Vectors for constructing LVVs mainly involve symbiotic bacteria, probiotics (e.g., Lactobacillus spp.), normally harmless bacteria and attenuated microorganisms [148,149,150,151]. Examples of harmless bacteria include Bacillus subtilis [152,153] and Saccharomycetes [154,155]. Examples of live-attenuated microorganisms that have been widely used as live vaccine vehicles include Salmonella [156,157], Listeria [158,159], poxvirus [160] and influenza virus [161]. Li et al. constructed a recombinant Lactobacillus-derived vaccine that displayed influenza epitopes (sM2 and HA2) [162]. Ferreira et al. also explored the immune efficiency of a recombinant Lactobacillus casei-derived vaccine that expressed a fusion protein involving pneumococcal PspA and PspC [163]. Based on the findings of these studies, LVV is a promising strategy for development of multiple epitopes-vaccine for M. pneumoniae using probiotics as vehicles.
4. Summary and Future Prospects
M. pneumoniae is the most common pathogen leading to atypical CAP, occasionally with extrapulmonary manifestations. Worse still, chronic refractory MPP can lead to serious complications. Refractory M. pneumoniae infections caused by macrolide-resistant M. pneumoniae have become more common in China, especially in children, which makes treatment more difficult. Owing to these reasons, there is an urgent need for development of effective vaccines for preventing M. pneumoniae infections.
There are various types of M. pneumoniae vaccines including inactivated, live-attenuated, and subunit vaccines. These vaccines are mainly administered via the nasal route or hypodermic needle. Whole-cell vaccines can be either inactivated or live-attenuated vaccines. Inactivated vaccines were found to elicit weak immune responses, and some individuals who did not produce antibodies after vaccination experienced severe immune responses on reinfection with M. pneumoniae. Vaccines based on M. pneumoniae adhesion proteins (P1, P30 and P116) have been considered as promising options. Hypodermic inoculation with a protein subunit vaccine results in effective immune protection [164]. However, the generation of a protein subunit vaccine can be challenging because they are accompanied by several inevitable shortcomings and technical difficulties. (1) The protein expression level in vitro is usually very low. Besides, purification of recombinant proteins is a complicated process [165,166]. (2) Protein subunit vaccines do not have a self-replicating ability compared with live attenuated vaccines or DNA vaccines, so multiple immunization is usually required [167]; (3) The protein subunit may lose its natural conformation when being expressed in heterologous systems [168]. DNA vaccines trigger both cell-mediated and humoral immunity, but the injected DNA cannot be consistently replicated in mammalian cells. These challenges need to be overcome in the future to develop effective vaccines.
M. pneumoniae infections in immunocompetent patients induce antibody responses that mainly direct against the terminal organelle-associated proteins in M. pneumoniae [169]. Thus, vaccine based on this adhesin can induce specific immunoglobulins that inhibit the adherence of M. pneumoniae to the respiratory epithelium of the host [169]. However, due to their weak humoral immunogenicity when used alone without aluminum adjuvant, a fusion protein with an adjuvant, such as hepatitis B virus capsid HN-144 fragment, is a preferred immunization strategy. Although LVVs using probiotics as expression vectors are still in its exploratory stage, it is believed that LVV could be a promising vaccine strategy against M. pneumoniae infections in the near future. The use of living probiotics as expression vector of LVVs enables vaccine delivery through pulmonary atomization and/or oral ingestion. We regard protein vaccines (usually manufactured by means of genetic engineering) are the most promising vaccines for the prevention of M. pneumoniae infections. Single-antigen protein formulated with vaccine adjuvant and multi-epitope fusion protein are promising vaccine candidates. Regardless of the vaccine type, the immunogenicity, safety, effectiveness, and functional mechanisms of vaccines used in humans need to be thoroughly researched before further clinical trials can be commenced.
At present, Coronavirus disease 2019 (COVID-19) has spread to almost every part of the world. COVID-19 co-infection with other common respiratory pathogens such as M. pneumoniae is not unexpected [170,171]. COVID-19 co-infection with M. pneumoniae may exacerbate clinical symptoms, delay recovery time, and increase morbidity and mortality [172,173], while vaccines for COVID-19 is on the way. There is no knowledge so far about whether co-infection of COVID-19 and M. pneumoniae will affect the outcome of vaccination. Although viral infection and bacterial infection are essentially different in terms of pathogenesis, some clinical manifestations of COVID-19 are similar to MPP, such as fever, dry cough, fatigue, ache all over, chest tightness, etc. [174,175]. Clinical practice indicates that reactive lymphocytes are frequently seen in COVID-19 infection, while in M. pneumoniae infection cold agglutination is common [172,174]. There are only subtle differences in radiographic features (chest X-ray and CT imaging) between these two diseases [171,174,176]. Genetic and serologic tests (e.g., serum IgM/IgG antibody rapid test) have definitely helped clinicians to diagnose and manage COVID-19 patients during the COVID-19 pandemic [173]. There are some questions as to whether COVID-19 or COVID-19 co-infection with M. pneumoniae will be in existence in humans for a long time. What is the mechanism via which COVID-19 co-infection with M. pneumoniae increases morbidity and mortality? We can speculate from our research experience: human cellular immunity may be suppressed by one pathogen with an immune escape mechanism, which causes a declining antigen reactivity to another pathogen. Is this true? Are there other mechanisms? These topics may be research hotspots in the future.
Author Contributions
Z.J. and S.L. wrote the first draft. S.L., C.Z., R.Z. and P.H.M.L. edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (81401512, 31970177), the Natural Science Foundation of Hunan Province (2019JJ40253), the Key Fund Project of Hunan Provincial Department of Education (18A234), and the Clinical Research Project of the University of South China (USCKF201902K01).
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Zhu, Y.G.; Tang, X.D.; Lu, Y.T.; Zhang, J.; Qu, J. Contemporary situation of community-acquired pneumonia in China: A systematic review. J. Transl. Int. Med. 2018, 6, 26–31. [Google Scholar] [CrossRef]
- Meyer Sauteur, P.M.; Jacobs, B.C.; Spuesens, E.B.M.; Jacobs, E.; Nadal, D.; Vink, C.; Rossum, A.M.C. Antibody responses to Mycoplasma pneumoniae: Role in pathogenesis and diagnosis of encephalitis? PLoS Pathog. 2014, 10, e1003983. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson1, E.J.; Courtney, D.M.; et al. Community-acquired pneumonia requiring Hospitalization among US adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef] [PubMed]
- Xiao, L.; Ptacek, T.; Osborne, J.D.; Crabb, D.M.; Simmons, W.L.; Lefkowitz, E.J.; Waites, K.B.; Atkinson, T.P.; Dybvig, K. Comparative genome analysis of Mycoplasma pneumoniae. BMC Genom. 2015, 16, 610. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Guo, L.; Dong, X.; Li, X.; Zhou, P.; Ni, Q.; Zhou, X.Y.; Wagner, B.L.; Li, L. Detection of viruses and Mycoplasma pneumoniae in hospitalized patients with severe acute respiratory infection in northern China, 2015–2016. Jpn. J. Infect. Dis. 2018, 71, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Kutty, P.K.; Jain, S.; Taylor, T.H.; Bramley, A.M.; Diaz, M.H.; Ampofo, K.; Arnold, S.R.; Williams, D.J.; Edwards, K.M.; McCullers, J.A.; et al. Mycoplasma pneumoniae among children hospitalized with community-acquired pneumonia. Clin. Infect. Dis. 2019, 68, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Li, X.; Liu, Y.; Balish, M.F.; Atkinson, T.P. Mycoplasma pneumoniae from the respiratory tract and beyond. Clin. Microbiol. Rev. 2017, 30, 747–809. [Google Scholar] [CrossRef]
- Søndergaard, M.J.; Friis, M.B.; Hansen, D.S.; Jørgensen, I.M. Clinical manifestations in infants and children with Mycoplasma pneumoniae infection. PLoS ONE 2018, 13, e0195288. [Google Scholar] [CrossRef]
- Gao, L.W.; Yin, J.; Hu, Y.H.; Liu, X.Y.; Feng, X.L.; He, J.X.; Liu, J.; Guo, Y.; Xu, B.P.; Shen, K.L. The epidemiology of paediatric Mycoplasma pneumoniae pneumonia in North China: 2006 to 2016. Epidemiol. Infect. 2019, 147, e192. [Google Scholar] [CrossRef]
- Kumar, S.; Roy, R.D.; Sethi, G.R.; Saigal, S.R. Mycoplasma pneumoniae infection and asthma in children. Trop. Dr. 2019, 49, 117–119. [Google Scholar] [CrossRef]
- Kassisse, E.; García, H.; Prada, L.; Salazar, I.; Kassisse, J. Prevalence of Mycoplasma pneumoniae infection in pediatric patients with acute asthma exacerbation. Arch. Argent. Pediatr. 2018, 116, 179–185. [Google Scholar] [PubMed]
- Esposito, S.; Droghetti, R.; Bosis, S.; Claut, L.; Marchisio, P.; Principi, N. Cytokine secretion in children with acute Mycoplasma pneumoniae infection and wheeze. Pediatr. Pulmonol. 2002, 34, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Narita, M. Pathogenesis of extrapulmonary manifestations of Mycoplasma pneumoniae infection with special reference to pneumonia. J. Infect. Chemother. 2010, 16, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Narita, M. Classification of extrapulmonary manifestations due to Mycoplasma pneumoniae infection on the basis of possible pathogenesis. Front. Microbiol. 2016, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Giavina-Bianchi, P.; Kalil, J. Mycoplasma pneumoniae infection induces asthma onset. J. Allergy Clin. Immunol. 2016, 137, 1024–1025. [Google Scholar] [CrossRef]
- Wang, K.; Chalker, V.; Bermingham, A.; Harrison, T.; Mant, D.; Harnden, A. Mycoplasma pneumoniae and respiratory virus infections in children with persistent cough in England: A retrospective analysis. Pediatr. Infect. Dis. J. 2011, 30, 1047–1051. [Google Scholar] [CrossRef]
- Takahashi, N.; Shinohara, T.; Oi, R.; Ota, M.; Toriumi, S.; Ogushi, F. Acute respiratory distress syndrome caused by Mycoplasma pneumoniae without elevated pulmonary vascular permeability: A case report. J. Thorac. Dis. 2016, 8, E319–E324. [Google Scholar] [CrossRef]
- Meyer Sauteur, P.M.; Theiler, M.; Buettcher, M.; Seiler, M.; Weibel, L.; Berger, C. Frequency and clinical presentation of mucocutaneous disease due to Mycoplasma pneumoniae infection in children with community-acquired pneumonia. JAMA Dermatol. 2019, 156, 144–150. [Google Scholar] [CrossRef]
- Meyer Sauteur, P.M.; Goetschel, P.; Lautenschlager, S. Mycoplasma pneumoniae and mucositis--part of the Stevens-Johnson syndrome spectrum. J. Dtsch. Dermatol. Ges. 2012, 10, 740–746. [Google Scholar]
- Harr, T.; French, L.E. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet. J. Rare. Dis. 2010, 5, 39. [Google Scholar] [CrossRef]
- Prindaville, B.; Newell, B.D.; Nopper, A.J.; Horii, K.A. Mycoplasma pneumonia—Associated mucocutaneous disease in children: Dilemmas in classification. Pediatr. dermatol. 2014, 31, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Tabassum, I.; Chaudhry, R.; Chourasia, B.K.; Malhotra, P. Identification of an N-terminal 27 kDa fragment of Mycoplasma pneumoniae P116 protein as specific immunogen in M. pneumoniae infections. BMC Infect. Dis. 2010, 10, 350. [Google Scholar] [CrossRef]
- Drasbek, M.; Nielsen, P.K.; Persson, K.; Birkelund, S.; Christiansen, G. Immune response to Mycoplasma pneumoniae P1 and P116 in patients with atypical pneumonia analyzed by ELISA. BMC Microbiol. 2004, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Meyer Sauteur, P.M.; Unger, W.W.; Nadal, D.; Berger, C.; Vink, C.; van Rossum, A.M. Infection with and carriage of Mycoplasma pneumoniae in children. Front. Microbiol. 2016, 7, 329. [Google Scholar] [CrossRef] [PubMed]
- De Groot, R.C.A.; Meyer Sauteur, P.M.; Unger, W.W.J.; van Rossum, A.M.C. Things that could be Mycoplasma pneumoniae. J. Infect. 2017, 74, S95–S100. [Google Scholar] [CrossRef]
- Spuesens, E.B.M.; Meyer Sauteur, P.M.; Vink, C.; van Rossum, A.M.C. Mycoplasma pneumoniae infections-does treatment help? J. Infect. 2014, 69, S42–S46. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Qu, J.; Yin, Y.; Eldere, J.V. Overview of antimicrobial options for Mycoplasma pneumoniae pneumonia, focus on macrolide resistance. Clin. Respir. J. 2017, 11, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Khoury, T.; Sviri, S.; Rmeileh, A.A.; Nubani, A.; Abutbul, A.; Hoss, S.; van Heerden, P.V.; Bayya, A.E.; Hidalgo-Grass, C.; Moses, A.E.; et al. Increased rates of intensive care unit admission in patients with Mycoplasma pneumoniae: A retrospective study. Clin. Microbiol. Infect. 2016, 22, 711–714. [Google Scholar] [CrossRef]
- Chen, Y.C.; Hsu, W.Y.; Chang, T.H. Macrolide-resistant Mycoplasma pneumoniae infections in pediatric community-acquired pneumonia. Emerg. Infect. Dis. 2020, 26, 1382–1391. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, Y.; Sheng, Y.; Zhang, L.; Shen, Z.; Chen, Z. More complications occur in macrolide-resistant than in macrolide-sensitive Mycoplasma pneumoniae pneumonia. Antimicrob. Agents Chemother. 2014, 58, 1034–1038. [Google Scholar] [CrossRef]
- Widjaja, M.; Berry, I.J.; Jarocki, V.M.; Padula, M.P.; Dumke, R.; Djordjevic, S.P. Cell surface processing of the P1 adhesin of Mycoplasma pneumoniae identifies novel domains that bind host molecules. Sci. Rep. 2020, 10, 6384. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Prince, O.A.; Sheppard, E.S.; Krause, D.C. Processing is required for a fully functional protein P30 in Mycoplasma pneumoniae gliding and cytadherence. J. Bacteriol. 2011, 193, 5841–5846. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Jordan, J.L.; Kraus, D.C. Domain analysis of protein P30 in Mycoplasma pneumoniae cytadherence and gliding motility. J. Bacteriol. 2011, 193, 1726–1733. [Google Scholar] [CrossRef] [PubMed]
- Widjaja, M.; Berry, I.J.; Pont, E.J.; Padula, M.P.; Djordjevic, S. P40 and P90 from Mpn142 are targets of multiple processing events on the surface of Mycoplasma pneumoniae. Proteomes 2015, 3, 512–537. [Google Scholar] [CrossRef]
- Jordan, J.L.; Chang, H.Y.; Balish, M.F.; Holt, L.S.; Bose, S.R.; Hasselbring, B.M.; Waldo, R.H.; Krunkosky, T.M.; Krause, D.C. Protein P200 is dispensable for Mycoplasma pneumoniae hemadsorption but not gliding motility or colonization of differentiated bronchial epithelium. Infect. Immun. 2007, 75, 518–522. [Google Scholar] [CrossRef]
- Chaudhry, R.; Varshney, A.K.; Malhotra, P. Adhesion proteins of Mycoplasma pneumoniae. Front. Biosci. 2007, 12, 690–699. [Google Scholar] [CrossRef]
- Hasselbring, B.M.; Sheppard, E.S.; Krause, D.C. P65 truncation impacts P30 dynamics during Mycoplasma pneumoniae gliding. J. Bacteriol. 2012, 194, 3000–3007. [Google Scholar] [CrossRef]
- Widjaja, M.; Harvey, K.L.; Hagemann, L.; Berry, I.J.; Jarocki, V.M.; Raymond, B.B.A.; Tacchi, J.L.; Gründe, A.; Steele1, J.R.; Padula, M.P.; et al. Elongation factor Tu is a multifunctional and processed moonlighting protein. Sci. Rep. 2017, 7, 11227. [Google Scholar] [CrossRef]
- Balasubramanian, S.; Kannan, T.R.; Baseman, J.B. The surface-exposed carboxyl region of Mycoplasma pneumoniae elongation factor Tu interacts with fibronectin. Infect. Immun. 2008, 76, 3116–3123. [Google Scholar] [CrossRef]
- Yu, Y.; Wang, H.; Wang, J.; Feng, Z.; Wu, M.; Liu, B.; Xin, J.; Xiong, Q.; Liu, M.; Shao, G. Elongation factor thermo unstable (EF-Tu) moonlights as an adhesin on the surface of Mycoplasma hyopneumoniae by binding to fibronectin. Front. Microbiol. 2018, 9, 974. [Google Scholar] [CrossRef]
- Thomas, C.; Jacobs, E.; Dumke, R. Characterization of pyruvate dehydrogenase subunit B and enolase as plasminogen-binding proteins in Mycoplasma pneumoniae. Microbiology 2013, 159, 352–365. [Google Scholar] [CrossRef] [PubMed]
- Dumke, R.; Hausner, M.; Jacobs, E. Role of Mycoplasma pneumoniae glyceraldehyde-3-phosphate dehydrogenase (GAPDH) in mediating interactions with the human extracellular matrix. Microbiology 2011, 157, 2328–2338. [Google Scholar] [CrossRef]
- Cloward, J.M.; Krause, D.C. Loss of co-chaperone TopJ impacts adhesin P1 presentation and terminal organelle maturation in Mycoplasma pneumoniae. Mol. Microbiol. J. 2011, 81, 528–539. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Kida, Y.; Sakamoto, Y.; Kuwano, K. Mpn491, a secreted nuclease of Mycoplasma pneumoniae, plays a critical role in evading killing by neutrophil extracellular traps. Cell Microbiol. 2017, 19, e12666. [Google Scholar] [CrossRef] [PubMed]
- Blötz, C.; Singh, N.; Dumke, R.; Stülke, J. Characterization of an immunoglobulin binding protein (IbpM) from Mycoplasma pneumoniae. Front. Microbiol. 2020, 11, 685. [Google Scholar] [CrossRef]
- He, J.; Liu, M.; Ye, Z.; Tan, T.; Liu, X.; You, X.; Zeng, Y.H.; Wu, Y.M. Insights into the pathogenesis of Mycoplasma pneumoniae. Mol. Med. Rep. 2016, 14, 4030–4036. [Google Scholar] [CrossRef]
- Großhennig, S.; Ischebeck, T.; Gibhardt, J.; Busse, J.; Feussner, I.; Stülke, J. Hydrogen sulfide is a novel potential virulence factor of Mycoplasma pneumoniae: Characterization of the unusual cysteine desulfurase/desulfhydrase HapE. Mol. Microbiol. 2016, 100, 42–54. [Google Scholar] [CrossRef]
- Li, S.; Xue, G.; Zhao, H.; Feng, Y.; Yan, C.; Cui, J.; Sun, H.M. The Mycoplasma pneumoniae HapE alters the cytokine profile and growth of human bronchial epithelial cells. Biosci. Rep. 2019, 39, BSR20182201. [Google Scholar] [CrossRef]
- Maenpuen, S.; Watthaisong, P.; Supon, P.; Sucharitakul, J.; Parsonage, D.; Karplus, P.A.; Claiborne, A.; Chaiyen, P. Kinetic mechanism of L-α-glycerophosphate oxidase from Mycoplasma pneumoniae. FEBS J. 2015, 282, 3043–3059. [Google Scholar] [CrossRef]
- Shimizu, T.; Kimura, Y.; Kida, Y.; Kuwano, K.; Achibana, M.; Hashino, M.; Watarai, M. Cytadherence of Mycoplasma pneumoniae induces inflammatory responses through autophagy and Toll-like receptor 4. Infect. Immun. 2014, 82, 3076–3086. [Google Scholar] [CrossRef]
- Choi, S.Y.; Lim, J.W.; Shimizu, T. Reactive oxygen species mediate Jak2/Stat3 activation and IL-8 expression in pulmonary epithelial cells stimulated with lipid-associated membrane proteins from Mycoplasma pneumoniae. Inflamm. Res. 2012, 61, 493–501. [Google Scholar] [CrossRef]
- Wilson, M.H.; Collier, A.M. Ultrastructural study of Mycoplasma pneumoniae in organ culture. J. Bacteriol. 1976, 125, 332–339. [Google Scholar] [CrossRef]
- Becker, A.; Kannan, T.R.; Taylor, A.B.; Pakhomova, O.N.; Zhang, Y.; Somarajan, S.R.; Galaleldeen, A.; Holloway, S.P.; Baseman, J.B.; Hart, P.J. Structure of CARDS toxin, a unique ADP-ribosylating and vacuolating cytotoxin from Mycoplasma pneumoniae. Proc. Natl. Acad. Sci. USA 2015, 112, 5165–5170. [Google Scholar] [CrossRef] [PubMed]
- Kannan, T.R.; Krishnan, M.; Ramasamy, M.; Becker, M.; Pakhomova, O.M.; Hart, P.H.; Baseman, J.B. Functional mapping of community-acquired respiratory distress syndrome (CARDS) toxin of Mycoplasma pneumoniae defines regions with ADP-ribosyltransferase, vacuolating and receptor-binding activities. Mol. Microbiol. 2014, 93, 568–581. [Google Scholar] [CrossRef] [PubMed]
- Somarajan, S.R.; Kannan, T.R.; Baseman, J.B. Mycoplasma pneumoniae Mpn133 is a cytotoxic nuclease with a glutamic acid-, lysine- and serine-rich region essential for binding and internalization but not enzymatic activity. Cell. Microbiol. 2010, 12, 1821–1831. [Google Scholar] [CrossRef] [PubMed]
- Kawakita, Y.; Kinoshita, M.; Furukawa, Y.; Tulum, I.; Tahara, Y.O.; Katayama, E.; Namba, K.; Miyata, M. Structural study of MPN387, an essential protein for gliding motility of a human-pathogenic bacterium, Mycoplasma pneumoniae. J. Bacteriol. 2016, 198, 2352–2359. [Google Scholar] [CrossRef]
- Hasselbring, B.M.; Krause, D.C. Proteins P24 and P41 function in the regulation of terminal-organelle development and gliding motility in Mycoplasma pneumoniae. J. Bacteriol. 2007, 189, 7442–7449. [Google Scholar] [CrossRef]
- Nakane, D.; Kenri, T.; Matsuo, L.; Miyata, M. Systematic structural analyses of attachment organelle in Mycoplasma pneumoniae. PLoS Pathog. 2015, 11, e1005299. [Google Scholar] [CrossRef]
- Miyata, M.; Hamaguchi, T. Integrated information and prospects for gliding mechanism of the pathogenic bacterium Mycoplasma pneumoniae. Front. Microbiol. 2016, 7, 960–976. [Google Scholar] [CrossRef]
- Miyata, M.; Ogaki, H. Cytoskeleton of mollicutes. J. Mol. Microbiol. Biotechnol. 2006, 11, 256–264. [Google Scholar] [CrossRef]
- Williams, C.R.; Chen, L.; Driver, A.D.; Arnold, E.A.; Sheppard, E.S.; Locklin, J.; Krause, D.C. Sialylated receptor setting influences Mycoplasma pneumoniae attachment and gliding motility. Mol. Microbiol. 2018, 109, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.C.; Balish, M.F. Structure, function, and assembly of the terminal organelle of Mycoplasma pneumoniae. FEMS Microbiol. Lett. 2001, 198, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, R.; Ghosh, A.; Chandolia, A. Pathogenesis of Mycoplasma pneumoniae: An update. Indian J. Med. Microbiol. 2016, 34, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Balish, M.F. Mycoplasma pneumoniae, an underutilized model for bacterial cell biology. J. Bacteriol. 2014, 196, 3675–3682. [Google Scholar] [CrossRef]
- Kang, M.; Hashimoto, A.; Gade, A.; Akbarali, H.I. Interaction between hydrogen sulfide-induced sulfhydration and tyrosine nitration in the KATP channel complex. Am. J. Physiol. Gastrointest. Liver. Physiol. 2015, 308, G532–G539. [Google Scholar] [CrossRef]
- Großhennig, S.; Schmidl, S.R.; Schmeisky, G.; Busse, J.; Stülke, J. Implication of glycerol and phospholipid transporters in Mycoplasma pneumoniae growth and virulence. Infect. Immun. 2013, 81, 896–904. [Google Scholar] [CrossRef]
- Merzbacher, M.; Detsch, C.; Hillen, W.; Stülke, J. Mycoplasma pneumoniae HPr kinase/phosphorylase. Eur. J. Biochem. 2004, 271, 367–374. [Google Scholar] [CrossRef]
- Halbedel, S.; Hames, C.; Stülke, J. Regulation of carbon metabolism in the Mollicutes and its relation to virulence. J. Mol. Microb. Biotech. 2007, 12, 147–154. [Google Scholar] [CrossRef]
- Into, T.; Dohkan, J.; Inomata, M.; Nakashima, M.; Shibata, K.I.; Matsushita, K. Synthesis and characterization of a dipalmitoylated lipopeptide derived from paralogous lipoproteins of Mycoplasma pneumoniae. Infect. Immun. 2007, 75, 2253–2259. [Google Scholar] [CrossRef]
- Hallamaa, K.M.; Browning, G.F.; Tang, S.L. Lipoprotein multigene families in Mycoplasma pneumoniae. J. Bacteriol. 2006, 188, 5393–5399. [Google Scholar] [CrossRef]
- Hallamaa, K.M.; Tang, S.L.; Ficorilli, N.; Browning, G.F. Differential expression of lipoprotein genes in Mycoplasma pneumoniae after contact with human lung epithelial cells, and under oxidative and acidic stress. BMC Microbiol. 2008, 8, 124. [Google Scholar] [CrossRef] [PubMed]
- Into, T.; Kiura, K.; Yasuda, M.; Kataoka, H.; Inoue, N.; Hasebe, A.; Takeda, K.; Akira, S.; Shibata, K. Stimulation of human Toll-like receptor (TLR) 2 and TLR6 with membrane lipoproteins of Mycoplasma fermentans induces apoptotic cell death after NF-kappa B activation. Cell Microbiol. 2004, 6, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Zhao, Y.; Wang, Z.; Hou, Y.; Bi, D.; Sun, J.; Peng, X. Chicken gga-miR-19a targets ZMYND11 and plays an important role in host defense against Mycoplasma gallisepticum (HS strain) infection. Front. Cell. Infect. Microbiol. 2016, 6, 102. [Google Scholar] [CrossRef] [PubMed]
- Kannan, T.R.; Provenzano, D.; Wright, J.R.; Baseman, J.B. Identification and characterization of human surfactant protein A binding protein of Mycoplasma pneumoniae. Infect. Immun. 2005, 73, 2828–2834. [Google Scholar] [CrossRef] [PubMed]
- Kannan, T.R.; Baseman, J.B. ADP-ribosylating and vacuolating cytotoxin of Mycoplasma pneumoniae represents unique virulence determinant among bacterial pathogens. Proc. Natl. Acad. Sci. USA 2006, 103, 6724–6729. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, M.; Kannan, T.R.; Baseman, J.B. Mycoplasma pneumoniae CARDS toxin is internalized via clathrin-mediated endocytosis. PLoS ONE 2013, 8, e62706. [Google Scholar] [CrossRef]
- Saber, S.; Ghanim, A.M.H.; El-Ahwany, E.; El-Kader, E.M.A. Novel complementary antitumour effects of celastrol and metformin by targeting IκBκB, apoptosis and NLRP3 inflammasome activation in diethylnitrosamine-induced hepatocarcinogenesis. Cancer Chemother. Pharmacol. 2020, 85, 331–343. [Google Scholar] [CrossRef]
- Bose, S.; Segovia, J.A.; Somarajan, S.R.; Chang, T.H.; Kannan, T.R.; Baseman, J.B. ADP-ribosylation of NLRP3 by Mycoplasma pneumoniae CARDS toxin regulates inflammasome activity. mBio 2014, 5, e02186-14. [Google Scholar] [CrossRef]
- Yin, H.; Guo, Q.; Li, X.; Tang, T.; Li, C.; Wang, H.; Sun, Y.; Feng, Q.; Ma, C.; Gao, C. Curcumin suppresses IL-1β secretion an prevents inflammation through inhibition of the NLRP3 Inflammasome. J. Immunol. 2018, 200, 2835–2846. [Google Scholar] [CrossRef]
- Hardy, R.D.; Coalson, J.J.; Peters, J.; Chaparro, A.; Techasaensiri, C.; Cantwell, A.M.; Kannan, T.R.; Baseman, J.B.; Dube, P.H. Analysis of pulmonary inflammation and function in the mouse and baboon after exposure to Mycoplasma pneumoniae CARDS toxin. PLoS ONE 2009, 4, e7562. [Google Scholar] [CrossRef]
- Medina, J.L.; Coalson, J.J.; Brooks, E.G.; Winter, V.T.; Chaparro, A.; Principe, M.F.; Kannan, T.R.; Baseman, J.B.; Dube, P.H. Mycoplasma pneumoniae CARDS toxin induces pulmonary eosinophilic and lymphocytic inflammation. Am. J. Respir. Cell. Mol. Biol. 2012, 46, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Maselli, D.J.; Medina, J.L.; Brooks, E.G.; Coalson, J.J.; Kannan, T.R.; Winter, V.T.; Principe, M.; Cagle, M.P.; Baseman, J.B.; Dube, P.H.; et al. The immunopathologic effects of Mycoplasma pneumoniae and community-acquired respiratory distress syndrome toxin: A primate model. Am. J. Respir. Cell. Mol. Biol. 2018, 58, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Kida, Y.; Kuwano, K. Cytoadherence-dependent induction of inflammatory responses by Mycoplasma pneumoniae. Immunology 2011, 133, 51–61. [Google Scholar] [CrossRef]
- Fang, X.; Liu, X.; Meng, C.; Fu, Y.; Wang, X.; Li, B.; Tu, F.; Zhao, F.; Ren, S. Breed-linked polymorphisms of porcine toll-like receptor 2 (TLR2) and TLR4 and the primary investigation on their relationship with prevention against Mycoplasma pneumoniae and bacterial LPS challenge. Immunogenetics 2013, 65, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.Z.; Prescott, B. Immunochemical studies on a Mycoplasma pneumoniae polysaccharide fraction: Cross-reactions with type 23 and 32 antipneumococcal rabbit sera. Infect. Immun. 1978, 20, 421–429. [Google Scholar] [CrossRef]
- Brunner, H. Protective efficacy of Mycoplasma pneumoniae polysaccharides. Isr. J. Med. Sci. 1981, 17, 678–681. [Google Scholar]
- Simmons, W.L.; Daubenspeck, J.M.; Osborne, J.D.; Balish, M.F.; Waites, K.B.; Dybvig, K. Type 1 and type 2 strains of Mycoplasma pneumoniae form different biofilms. Microbiology 2013, 159, 737–747. [Google Scholar] [CrossRef]
- Root-Bernstein, R.; Fairweather, D. Complexities in the relationship between infection and autoimmunity. Current allergy and asthma reports. Curr. Allergy. Asthma. Rep. 2014, 14, 407. [Google Scholar] [CrossRef]
- Sfriso, P.; Ghirardello, A.; Botsios, C.; Tonon, M.; Zen, M.; Bassi, N.; Bassetto, F.; Doria, A. Infections and autoimmunity: The multifaceted relationship. J. Leukoc. Biol. 2010, 87, 385–395. [Google Scholar] [CrossRef]
- Saraya, T.; Kurai, D.; Nakagaki, K.; Sasaki, Y.; Niwa, S.; Tsukagoshi, H.; Nunokawa, H.; Ohkuma, K.; Tsujimoto, N.; Hirao, S.; et al. Novel aspects on the pathogenesis of Mycoplasma pneumoniae pneumonia and therapeutic implications. Front. Microbiol. 2014, 5, 410. [Google Scholar] [CrossRef]
- Dallo, S.F.; Chavoya, A.; Baseman, J.B. Characterization of the gene for a 30-kilodalton adhesion-related protein of Mycoplasma pneumoniae. Infect. Immun. 1990, 58, 4163–4165. [Google Scholar] [CrossRef] [PubMed]
- Kenri, T.; Taniguchi, R.; Sasaki, Y.; Okazaki, N.; Narita, M.; Izumikawa, K.; Umetsu, M.; Sasaki, T. Identification of a new variable sequence in the P1 cytadhesin gene of Mycoplasma pneumoniae: Evidence for the generation of antigenic variation by DNA recombination between repetitive sequences. Infect. Immun. 1999, 67, 4557–4562. [Google Scholar] [CrossRef] [PubMed]
- Spuesens, E.B.M.; Hartwig, N.G.; van Rossum, A.M.C.; Vink, C. Sequence variation within the P1 gene of Mycoplasma pneumoniae. J. Clin. Microbiol. 2011, 49, 3723–3724. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sluijter, M.; Spuesens, E.B.M.; Hartwig, N.G.; van Rossum, A.M.C.; Vink, C. The Mycoplasma pneumoniae MPN490 and Mycoplasma genitalium MG339 genes encode recA homologs that promote homologous DNA strand exchange. Infect. Immun. 2009, 77, 4905–4911. [Google Scholar] [CrossRef]
- Zhao, F.; Cao, B.; Li, J.; Song, S.; Tao, X.; Yi, Y.; He, L.; Zhang, J. Sequence analysis of the P1 adhesin gene of Mycoplasma pneumoniae in clinical isolates collected in Beijing in 2008 to 2009. J. Clin. Microbiol. 2011, 49, 3000–3003. [Google Scholar] [CrossRef]
- Nakane, D.; Adan-Kubo, J.; Kenri, T.; Miyata, M. Isolation and characterization of P1 adhesin, a leg protein of the gliding bacterium Mycoplasma pneumoniae. J. Bacteriol. 2011, 193, 715–722. [Google Scholar] [CrossRef]
- Schmidl, S.R.; Gronau, K.; Hames, C.; Busse, J.; Becher, D.; Hecker, M.; Stülke, J. The stability of cytadherence proteins in Mycoplasma pneumoniae requires activity of the protein kinase PrkC. Infect. Immun. 2010, 78, 184–192. [Google Scholar] [CrossRef]
- Yavlovich, A.; Tarshis, M.; Rottem, S. Internalization and intracellular survival of Mycoplasma pneumoniae by non-phagocytic cells. FEMS Microbiol. Lett. 2004, 233, 241–246. [Google Scholar] [CrossRef]
- Lu, J.; Holmgren, A. The thioredoxin antioxidant system. Free Radic. Bio. Med. 2014, 66, 75–87. [Google Scholar] [CrossRef]
- Linchevski, I.; Klement, E.; Nir-Paz, R. Mycoplasma pneumoniae vaccine protective efficacy and adverse reactions--systematic review and meta-analysis. Vaccine 2009, 27, 2437–2446. [Google Scholar] [CrossRef]
- Cimolai, N.; Cheong, A.C.; Morrison, B.J.; Taylor, G.P. Mycoplasma pneumoniae reinfection and vaccination: Protective oral vaccination and harmful immunoreactivity after re-infection and parenteral immunization. Vaccine 1996, 14, 1479–1483. [Google Scholar] [CrossRef]
- Mogabgab, W.J. Protective effects of inactive Mycoplasma pneumoniae vaccine in military personnel, 1964–1966. Am. Rev. Respir. Dis. 1968, 97, 359–365. [Google Scholar] [PubMed]
- Brown, R.C.; Hendley, J.O.; Gwaltney, J.M., Jr. Mycoplasma pneumoniae vaccine: Antigenicity of buffered antigens in volunteers. Infect. Immun. 1972, 5, 657–661. [Google Scholar] [CrossRef]
- Mogabgab, W.J. Protective efficacy of killed Mycoplasma pneumoniae vaccine measured in large-scale studies in a military population. Am. Rev. Respir. Dis. 1973, 108, 899–908. [Google Scholar]
- Wenzel, R.P.; Craven, R.B.; Davies, J.A.; Hendley, J.O.; Hamory, B.H.; Gwaltney, J.M., Jr. Field trial of an inactivated Mycoplasma pneumoniae vaccine. I. vaccine efficacy. J. Infect. Dis. 1976, 134, 571–576. [Google Scholar] [CrossRef]
- Wenzel, R.P.; Craven, R.B.; Davies, J.A.; Hendley, J.O.; Hamory, B.H.; Gwaltney, J.M., Jr. Protective efficacy of an inactivated Mycoplasma pneumoniae vaccine. J. Infect. Dis. 1977, 136, S204–S207. [Google Scholar] [CrossRef] [PubMed]
- Couch, R.B.; Cate, T.R.; Chanock, R.M. Infection with artificially propagated Eaton agent (Mycoplasma pneumoniae) Implications for development of attenuated vaccine for cold agglutinin-positive pneumonia. JAMA 1964, 187, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.E.; Senterfit, L.B.; Chanock, R.M.; Smith, C.B.; Purcell, R.H. An inactivated Mycoplasma pneumoniae vaccine. JAMA 1965, 194, 248–252. [Google Scholar] [CrossRef]
- Smith, C.B.; Chanock, R.M.; Friedewald, W.T.; Alford, R.H. Mycoplasma pneumoniae infections in volunteers. Ann. N. Y. Acad. Sci. 1967, 143, 471–483. [Google Scholar] [CrossRef]
- Smith, C.B.; Friedewald, W.T.; Chanock, R.M. Inactivated Mycoplasma pneumoniae vaccine. Evaluation in volunteers. JAMA 1967, 199, 353–358. [Google Scholar] [CrossRef]
- Fernald, G.W.; Clyde, W.A. Protective effect of vaccines in experimental Mycoplasma pneumoniae disease. Infect. Immun. 1970, 1, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Szczepanek, S.M.; Majumder, S.; Sheppard, E.S.; Liao, X.; Rood, D.; Tulman, E.R.; Wyand, S.; Krause, D.C.; Silbart, L.K.; Geary, S.J. Vaccination of BALB/c mice with an avirulent Mycoplasma pneumoniae P30 mutant results in disease exacerbation upon challenge with a virulent strain. Infect. Immun. 2012, 80, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Barile, M.F.; Chandler, D.K.; Yoshida, H.; Grabowski, M.W.; Harasawa, R.; Ahmed, O.A. Hamster challenge potency assay for evaluation of Mycoplasma pneumoniae vaccines. Isr. J. Med. Sci. 1981, 17, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Barile, M.F. Immunization against Mycoplasma pneumoniae disease: A review. Isr. J. Med. Sci. 1984, 20, 912–915. [Google Scholar] [PubMed]
- Barile, M.F.; Bove, J.M.; Bradbury, J.M. Current status on control of mycoplasmal diseases of man, animals, plants and insects. Bull. Inst. Pasteur 1985, 83, 339–373. [Google Scholar]
- Metzgar, D.P.; Woodhour, A.F.; Vella, P.P.; Weibel, R.E.; Stokes, J., Jr.; Drake, M.E.; Tytell, A.A.; Hilleman, M.R. Respiratory virus vaccines II Mycoplasma pneumoniae (Eaton agent) vaccines. Am. Rev. Respir. Dis. 1966, 94, 1–9. [Google Scholar]
- Tamiya, S.; Yoshikawa, E.; Ogura, M.; Kuroda, E.; Suzuki, K.; Yoshioka, Y. Vaccination using inactivated Mycoplasma pneumoniae induces detrimental infiltration of neutrophils after subsequent infection in mice. Vaccine 2020, 38, 4979–4987. [Google Scholar] [CrossRef]
- Cimolai, N.; Mah, D.G.; Taylor, G.P.; Morrison, B.J. Bases for the early immune response after rechallenge or component vaccination in an animal model of acute Mycoplasma pneumoniae pneumonitis. Vaccine 1995, 13, 305–309. [Google Scholar] [CrossRef]
- Chu, H.W.; Breed, R.; Rino, J.G.; Harbeck, R.J.; Sills, M.R.; Martin, R.J. Repeated respiratory Mycoplasma pneumoniae infections in mice: Effect of host genetic background. Microbes Infect. 2008, 8, 1764–1772. [Google Scholar] [CrossRef]
- Yayoshi, M.; Araake, M.; Hayatsu, E.; Takezawa, T.; Yoshioka, M. Immunogenicity and protective effect of hemolysis mutants of Mycoplasma pneumoniae. Microbiol. Immunol. 1985, 29, 1029–1037. [Google Scholar] [CrossRef]
- Greenberg, H.; Helms, C.M.; Brunner, H.; Chanock, R.M. Asymptomatic infection of adult volunteers with a temperature sensitive mutant of Mycoplasma pneumoniae. Proc. Natl. Acad. Sci. USA 1974, 51, 4015–4019. [Google Scholar] [CrossRef] [PubMed]
- Brunner, H.; Greenberg, H.; James, W.D.; Horswood, R.L.; Chanock, R.M. Decreased virulence and protective effect of genetically stable temperature-sensitive mutants of Mycoplasma pneumoniae. Ann. N. Y. Acad. Sci. 2010, 225, 436–452. [Google Scholar] [CrossRef]
- Qiu, L.; Wang, L.; Tan, L.; Li, M.; Wu, C.; Li, L.; Zheng, Z.; Jiang, H.; Sun, Q.; Zhang, T. Molecular characterization of genomic DNA in Mycoplasma pneumoniae strains isolated from serious Mycoplasma pneumonia cases in 2016, Yunnan, China. Infect. Genet. Evol. 2018, 58, 125–134. [Google Scholar] [CrossRef]
- Fan, L.; Li, D.; Zhang, L.; Hao, C.; Sun, H.; Shao, X.; Xu, J.; Chen, Z. Pediatric clinical features of Mycoplasma pneumoniae infection are associated with bacterial P1 genotype. Exp. Ther. Med. 2017, 14, 1892–1898. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Xue, G.; Yan, C.; Li, S.; Zhao, H.; Feng, Y.; Wang, L. Changes in molecular characteristics of Mycoplasma pneumoniae in clinical specimens from children in Beijing between 2003 and 2015. PLoS ONE 2017, 12, e0170253. [Google Scholar] [CrossRef] [PubMed]
- Xue, G.; Cao, L.; Wang, L.; Zhao, H.; Feng, Y.; Ma, L.; Sun, H. Evaluation of P1 adhesin epitopes for the serodiagnosis of Mycoplasma pneumoniae infections. FEMS Microbiol. Lett. 2013, 340, 86–92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meng, Y.; Wang, W.; Lv, D.D.; An, Q.; Lu, W.; Wang, X.; Tang, G. The effect of platycodin D on the expression of cytoadherence proteins P1 and P30 in Mycoplasma pneumoniae models. Environ. Toxicol. Pharmacol. 2017, 49, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Rodman, J.B.; Krivec, U.; Praprotnik, M.; Mrvič, T.; Kogoj, R.; Keše, D. Clinical characteristics of infections caused by Mycoplasma pneumoniae P1 genotypes in children. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Wu, Y.; Chen, S.; Yu, M.; Zeng, Y.; You, X. Protective immune responses in mice induced by intramuscular and intranasal immunization with a Mycoplasma pneumoniae P1C DNA vaccine. Can. J. Microbiol. 2012, 58, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Varshney, A.K.; Chaudhry, R.; Kabra, S.K.; Malhotra, P. Cloning, expression, and immunological characterization of the P30 protein of Mycoplasma pneumoniae. Clin. Vaccine Immunol. 2008, 15, 215–220. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rathore, J.S.; Wang, Y. Protective role of Th17 cells in pulmonary infection. Vaccine 2016, 34, 1504–1514. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Sundrud, M.S.; Skepner, J.; Yamagata, T. Targeting Th17 cells in autoimmune diseases. Trends Pharmacol. Sci. 2014, 35, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Hausner, M.; Schamberger, A.; Naumann, W.; Jacobs, E.; Dumke, R. Development of protective anti-Mycoplasma pneumoniae antibodies after immunization of guinea pigs with the combination of a P1-P30 chimeric recombinant protein and chitosan. Microb. Pathog. 2013, 64, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Seymour, L.M.; Deutscher, A.T.; Jenkins, C.; Kuit, T.A.; Falconer, L.; Minion, F.C.; Crossett, B.; Padula, M.; Dixon, N.E.; Djordijevic, S.P.; et al. A processed multidomain Mycoplasma hyopneumoniae adhesin binds fibronectin, plasminogen, and swine respiratory cilia. J. Biol. Chem. 2010, 285, 33971–33978. [Google Scholar] [CrossRef]
- Svenstrup, H.F.; Nielsen, P.K.; Drasbek, M.; Birkelund, S.; Christiansen, G. Adhesion and inhibition assay of Mycoplasma genitalium and M. pneumoniae by immunofluorescence microscopy. J. Med. Microbiol. 2002, 51, 361–373. [Google Scholar] [CrossRef][Green Version]
- Duffy, M.F.; Walker, I.D.; Browning, G.F. The immunoreactive 116 kDa surface protein of Mycoplasma pneumoniae is encoded in an operon. Microbiology 1997, 143, 3391–3402. [Google Scholar] [CrossRef][Green Version]
- Medina, J.L.; Brooks, E.G.; Chaparro, A.; Dube, P.H. Mycoplasma pneumoniae CARDS toxin elicits a functional IgE response in Balb/c mice. PLoS ONE 2017, 12, e0172447. [Google Scholar] [CrossRef]
- Chen, C.; Qi, Y.; Gao, J.; Pan, Y.; Li, S.; Li, J.; Chen, H.; Li, S.; Li, Y.; Wang, M. Designing, expression and immunological characterization of a chimeric protein of Mycoplasma pneumonia. Protein Pept. Lett. 2016, 23, 592–596. [Google Scholar] [CrossRef]
- Meyer Sauteur, P.M.; de Bruijn, A.C.J.M.; Graça, C.; Tio-Gillen, A.P.; Estevão, S.C.; Hoogenboezem, T.; Hendriks, R.W.; Berger, C.; Jacobs, B.C.; van Rossum, A.; et al. Antibodies to protein but not glycolipid structures are important for host defense against Mycoplasma pneumoniae. Infect. Immun. 2019, 87, e00663-18. [Google Scholar] [CrossRef]
- Prugnaud, J.L. DNA vaccines. Ann. Pharm. Fr. 2003, 61, 219–233. [Google Scholar]
- Abdulhaqq, S.A.; Weiner, D.B. DNA vaccines: Developing new strategies to enhance immune responses. Immunol. Res. 2008, 42, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Galli, V.; Simionatto, S.; Marchioro, S.B.; Fisch, A.; Gomes, C.K.; Conceição, F.R. Immunisation of mice with Mycoplasma hyopneumoniae antigens P37, P42, P46 and P95 delivered as recombinant subunit or DNA vaccines. Vaccine 2008, 31, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Ghaffarifar, F. Plasmid DNA vaccines: Where are we now? Drugs Today 2018, 54, 315–333. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Wang, S.; Hu, S.; Yu, M.J.; Zeng, Y.H.; You, X.; Xiao, J.; Wu, Y. Protective efficacy of a Mycoplasma pneumoniae P1C DNA vaccine fused with the B subunit of Escherichia coli heat-labile enterotoxin. Can. J. Microbiol. 2012, 58, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Schaffner, W. Direct transfer of cloned genes from bacteria to mammalian cells. Proc. Natl. Acad. Sci. USA 1980, 77, 2163–2167. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.; Ma, J.; Dong, Q.; Liu, Q. Live bacterial vaccine vector and delivery strategies of heterologous antigen: A review. Immunol. Lett. 2018, 197, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Shimoji, Y.; Oishi, E.; Muneta, Y.; Nosaka, H.; Mori, Y. Vaccine efficacy of the attenuated Erysipelothrix rhusiopathiae YS-19 expressing a recombinant protein of Mycoplasma hyopneumoniae P97 adhesin against mycoplasmal pneumonia of swine. Vaccine 2003, 21, 532–537. [Google Scholar] [CrossRef]
- Tan, T.S.; Syed Hassan, S.; Yap, W.B. Expression of surface-bound nonstructural 1 (NS1) protein of influenza virus A H5N1 on Lactobacillus casei strain C1. Lett. Appl. Microbiol. 2017, 64, 446–451. [Google Scholar] [CrossRef]
- Gorain, C.; Singh, A.; Bhattacharyya, S.; Kundu, A.; Lahiri, A.; Gupta, S.; Mallick, A. Mucosal delivery of live Lactococcus lactis expressing functionally active JlpA antigen induces potent local immune response and prevent enteric colonization of Campylobacter jejuni in chickens. Vaccine 2020, 38, 1630–1642. [Google Scholar] [CrossRef]
- Hwang, I.Y.; Koh, E.; Wong, A.; March, H.C.; Bentley, W.E.; Lee, Y.S.; Chang, M.W. Engineered probiotic Escherichia coli can eliminate and prevent Pseudomonas aeruginosa gut infection in animal models. Nat. Commun. 2017, 8, 5028. [Google Scholar] [CrossRef]
- Harms, J.S.; Durward, M.A.; Magnani, D.M.; Splitter, G.A. Evaluation of recombinant invasive, non-pathogenic Escherichia coli as a vaccine vector against the intracellular pathogen. J. Immune Based Ther. Vaccines 2009, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Chen, D.; Cui, Z.; Zhang, X.; Zhou, Y.; Guo, X.; Li, H.; Zhang, Y. Oral vaccination of tilapia against Streptococcus agalactiae using Bacillus subtilis spores expressing Sip. Fish Shellfish Immun. 2019, 86, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.G.; Hao, Y.; Wang, L. A Bacillus-based Coxsackie virus A16 mucosal vaccine induces strong neutralizing antibody responses. Cent. Eur. J. Immunol. 2019, 44, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.K.; Kang, M.L.; Jung, M.H.; Cha, S.B.; Lee, W.J.; Kim, J.M.; Kim, G.H.; Yoo, H.S. Induction of protective immune responses against challenge of Actinobacillus pleuropneumoniae by oral administration with Saccharomyces cerevisiae expressing Apx toxins in pigs. Vet. Immunol. Immunopathol. 2013, 151, 132–139. [Google Scholar] [CrossRef]
- Bolhassani, A.; Muller, M.; Roohvand, F.; Motevalli, F.; Agi, E.; Shokri, M.; Rad, M.M.; Hosseinzadeh, S. Whole recombinant Pichia pastoris expressing HPV16 L1 antigen is superior in inducing protection against tumor growth as compared to killed transgenic. Leishmania. Hum. Vaccin. Immunother. 2014, 10, 3499–3508. [Google Scholar] [CrossRef]
- Senevirathne, A.; Hewawaduge, C.; Lee, J.H. Live vaccine consisting of attenuated Salmonella secreting and delivering Brucella ribosomal protein L7/L12 induces humoral and cellular immune responses and protects mice against virulent Brucella abortus 544 challenge. Vet. Res. 2020, 51, 6. [Google Scholar] [CrossRef]
- Ding, K.; Shang, K.; Yu, Z.H.; Yu, C.; Jia, Y.Y.; He, L.; Liao, C.S.; Li, J.; Zhang, C.J.; Li, Y.J.; et al. Recombinant-attenuated Salmonella pullorum strain expressing the hemagglutinin-neuraminidase protein of Newcastle disease virus (NDV) protects chickens against NDV and Salmonella pullorum challenge. J. Vet. Sci. 2018, 19, 232–241. [Google Scholar] [CrossRef]
- Jiang, M.; Liu, S.; Su, L.; Zhang, X.; Li, Y.; Tang, T.; Wang, C. Intranasal vaccination with Listeria ivanovii as vector of Mycobacterium tuberculosis antigens promotes specific lung-localized cellular and humoral immune responses. Sci. Rep. 2020, 10, 302. [Google Scholar] [CrossRef]
- Mahdy, S.E.; Sijing, L.; Lin, S.; Zhang, X.; Chen, H.; Pei, X.; Wang, C. Development of a recombinant vaccine against foot and mouth disease utilizing mutant attenuated Listeria ivanovii strain as a live vector. J. Virol. Methods 2019, 273, 113722. [Google Scholar] [CrossRef]
- Pérez, P.; Marín, M.Q.; Lázaro-Frías, A.; Oya, N.J.D.; Blázquez, A.B.; Romero, E.E.; Sorzano, C.O.; Ortego, J.; Saiz, J.C.; Esteban, M.; et al. A vaccine based on a modified vaccinia virus ankara vector expressing Zika virus structural proteins controls Zika virus replication in mice. Sci. Rep. 2018, 8, 17385. [Google Scholar] [CrossRef]
- Gerlach, T.; Elbahesh, H.; Saletti, G.; Rimmelzwaan, G. Recombinant influenza A viruses as vaccine vectors. Expert Rev. Vaccines 2019, 18, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Chowdhury, M.Y.; Kim, J.H.; Kim, T.H.; Pathinayake, P.; Koo, W.S.; Park, M.E.; Yoon, J.E.; Roh, J.B.; Hong, S.P.; et al. Mucosally administered Lactobacillus-displayed influenza antigens (sM2 and HA2) with cholera toxin subunit A1 (CTA1) induce broadly protective immune responses against divergent influenza subtypes. Vet. Microbiol. 2015, 179, 250–263. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, D.M.; Darrieux, M.; Silva, D.A.; Leite, L.C.C.; Ferreira, J.M.C., Jr.; Ho, P.L.; Miyaji, E.N.; Oliveira, M.L.S. Characterization of protective mucosal and systemic immune responses elicited by pneumococcal surface protein PspA and PspC nasal vaccines against a respiratory pneumococcal challenge in mice. Clin. Vaccine Immunol. 2009, 16, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Guo, Z.; MacDonald, N.E. Vaccine preventable community-acquired pneumonia in hospitalized children in northwest China. Pediatr. Infect. Dis. J. 2011, 30, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Lahiry, A.; Fan, Y.; Stimple, S.D.; Raith, M.; Wood, D.W. Inteins as tools for tagless and traceless protein purification. J. Chem. Technol. Biotechnol. 2018, 93, 1827–1835. [Google Scholar] [CrossRef]
- Yu, H.; Karunakaran, K.P.; Jiang, X.; Brunham, R.C. Subunit vaccines for the prevention of mucosal infection with Chlamydia trachomatis. Expert Rev. Vaccines. 2016, 15, 977–988. [Google Scholar] [CrossRef] [PubMed]
- Fitch, W.M.; Peterson, E.M.; de la Maza, L.M. Phylogenetic analysis of the outer-membrane-protein genes of Chlamydiae, and its implication for vaccine development. Mol. Biol. Evol. 1993, 10, 892–913. [Google Scholar]
- Pal, S.; Theodor, I.; Peterson, E.M.; de la Maza, L.M. Immunization with the Chlamydia trachomatis mouse pneumonitis major outer membrane protein can elicit a protective immune response against a genital challenge. Infect. Immun. 2001, 69, 6240–6247. [Google Scholar] [CrossRef]
- Dumke, R.; Jacobs, E. Antibody response to Mycoplasma pneumoniae: Protection of host and influence on outbreaks? Front. Microbiol. 2016, 7, 39. [Google Scholar] [CrossRef]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA 2020, 323, 2085–2086. [Google Scholar] [CrossRef]
- Wu, Q.; Xing, Y.; Shi, L.; Li, W.; Gao, Y.; Pan, S.; Wang, Y.; Wang, W.; Xing, Q. Coinfection and other clinical characteristics of COVID-19 in children. Pediatrics 2020, 146, e20200961. [Google Scholar] [CrossRef] [PubMed]
- Fan, B.E.; Lim, K.G.E.; Chong, V.C.L.; Chan, S.S.W.; Ong, K.H.; Kuperan, P. COVID-19 and Mycoplasma pneumoniae coinfection. Am. J. Hematol. 2020, 95, 723–724. [Google Scholar] [CrossRef] [PubMed]
- Amin, D.; McKitish, K.; Shah, P.S. Association of mortality and recent Mycoplasma pneumoniae infection in COVID-19 patients. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.C.; Huang, C.G.; Yang, C.T.; Hu, H.C. Concomitant infection with COVID-19 and Mycoplasma pneumoniae. Biomed. J. 2020, 43, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Zha, L.; Shen, J.; Tefsen, B.; Wang, Y.; Lu, W.; Xu, Q. Clinical features and outcomes of adult COVID-19 patients co-infected with Mycoplasma pneumoniae. J. Infect. 2020, 81, e12–e15. [Google Scholar] [CrossRef]
- Gayam, V.; Konala, V.M.; Naramala, S.; Garlapati, P.R.; Merghani, M.A.; Regmi, N.; Balla, M.; Adapa, S. Presenting characteristics, comorbidities, and outcomes of patients coinfected with COVID-19 and Mycoplasma pneumoniae in the USA. J. Med. Virol. 2020, 92, 2181–2187. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).