Clostridium perfringens-Induced Host-Pathogen Transcriptional Changes in the Small Intestine of Broiler Chickens
Abstract
:1. Introduction
2. Materials and methods
2.1. Animals Used for This Study
2.2. Challenge Infection by C. perfringens and RNA Extraction
2.3. Library Construction and Sequencing Analysis
2.4. Statistical Analysis
3. Results
3.1. Growth Underperformance Post C. perfringens Infection
3.2. Identification of DEGs in the Small Intestines between C. perfringens-Infected and Control Groups
3.3. Identification of Highly Abundant Up-/Down-Regulated Genes in Response to C. perfringens Infection
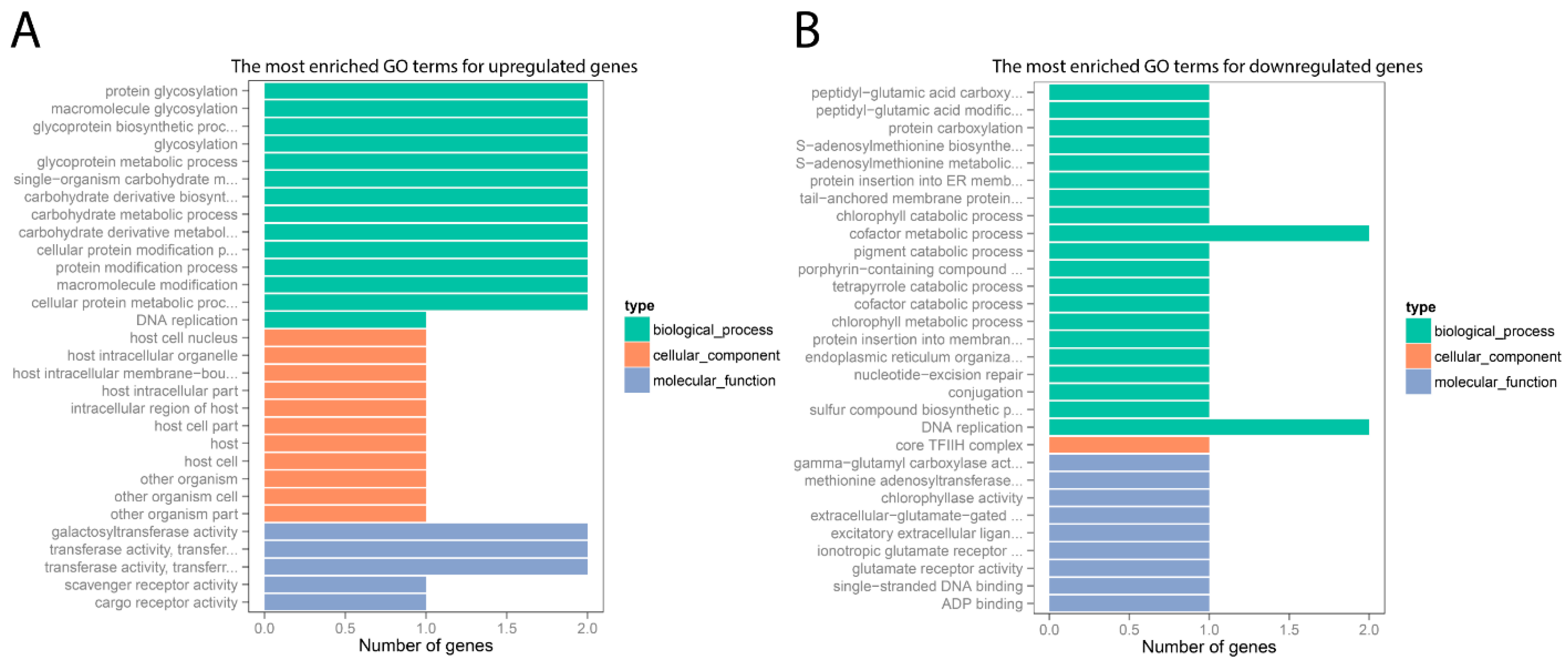
3.4. GO Annotation for DEGs
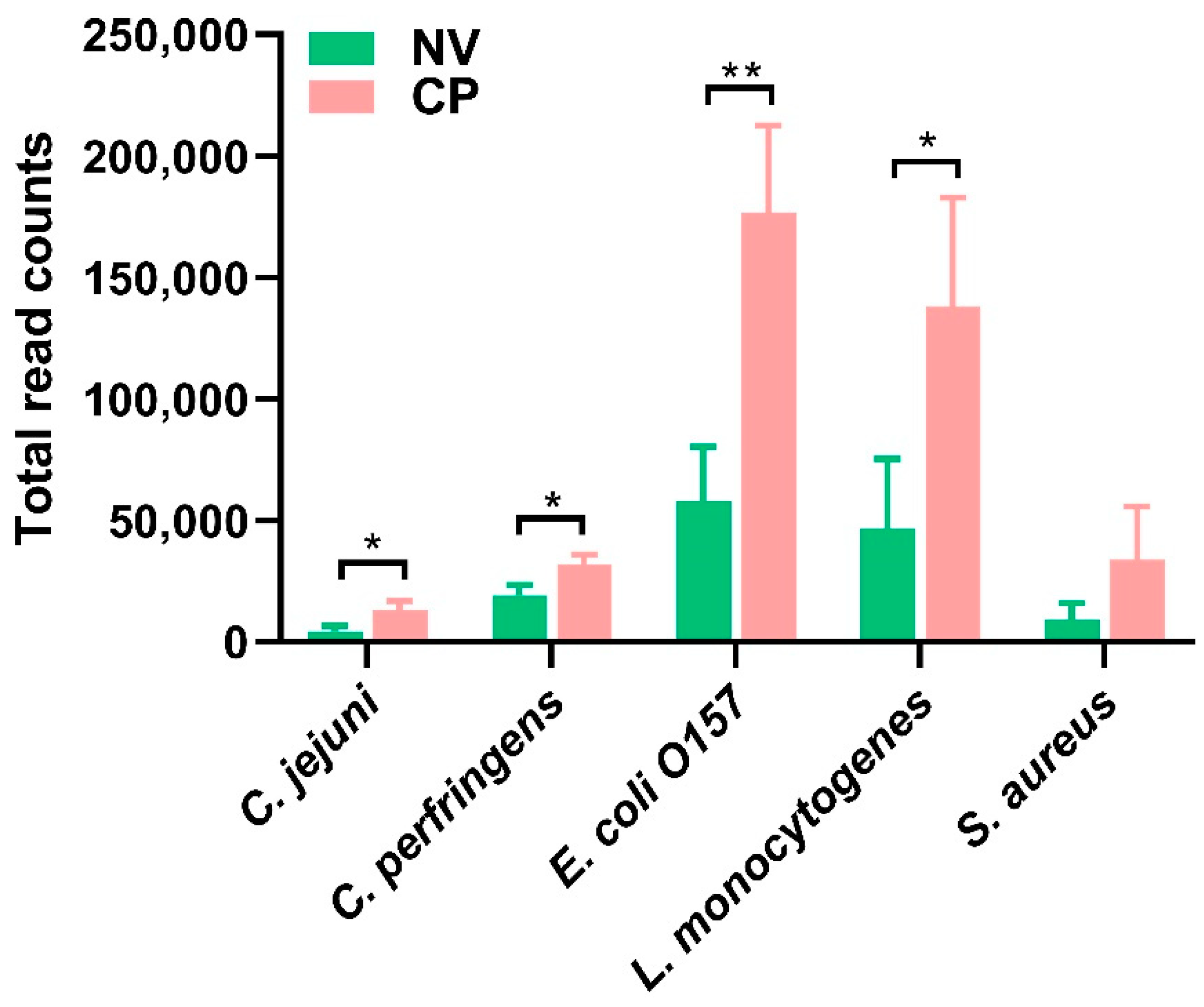
3.5. The Mapping of C. perfringens and Other Foodborne Pathogens
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NE | necrotic enteritis |
| RNA-seq | RNA sequencing |
| NV | uninfected sham control |
| RBWG% | relative body weight gain percentage |
| GO | Gene Ontology |
| DGE | Differential gene expression |
| DEG | Differentially expressed genes |
| FDR | False discovery rate |
References
- Hassan, K.A.; Elbourne, L.D.; Tetu, S.G.; Melville, S.B.; Rood, J.I.; Paulsen, I.T. Genomic analyses of Clostridium perfringens isolates from five toxinotypes. Res. Microbiol. 2015, 166, 255–263. [Google Scholar] [CrossRef]
- Uzal, F.A.; Freedman, J.C.; Shrestha, A.; Theoret, J.R.; Garcia, J.; Awad, M.M.; Adams, V.; Moore, R.J.; Rood, J.I.; McClane, B.A. Towards an understanding of the role of Clostridium perfringens toxins in human and animal disease. Future Microbiol. 2014, 9, 361–377. [Google Scholar] [CrossRef] [Green Version]
- Kiu, R.; Hall, L.J. An update on the human and animal enteric pathogen Clostridium perfringens. Emerg. Microbes Infect. 2018, 7, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Revitt-Mills, S.A.; Rood, J.I.; Adams, V. Clostridium perfringens extracellular toxins and enzymes: 20 and counting. Microbiol. Aust. 2015, 36, 114–117. [Google Scholar] [CrossRef]
- Rood, J.I.; Adams, V.; Lacey, J.; Lyras, D.; McClane, B.A.; Melville, S.B.; Moore, R.J.; Popoff, M.R.; Sarker, M.R.; Songer, J.G. Expansion of the Clostridium perfringens toxin-based typing scheme. Anaerobe 2018, 53, 5–10. [Google Scholar] [CrossRef]
- Scallan, E.; Hoekstra, R.M.; Angulo, F.J.; Tauxe, R.V.; Widdowson, M.-A.; Roy, S.L.; Jones, J.L.; Griffin, P.M. Foodborne illness acquired in the United States—major pathogens. Emerg. Infect. Dis. 2011, 17, 7. [Google Scholar] [CrossRef]
- Grass, J.E.; Gould, L.H.; Mahon, B.E. Epidemiology of foodborne disease outbreaks caused by Clostridium perfringens, United States, 1998–2010. Foodborne Pathog. Dis. 2013, 10, 131–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dewey-Mattia, D.; Manikonda, K.; Hall, A.J.; Wise, M.E.; Crowe, S.J. Surveillance for foodborne disease outbreaks—United States, 2009–2015. MMWR Surveill. Summ. 2018, 67, 1. [Google Scholar] [CrossRef]
- Zahoor, I.; Ghayas, A.; Basheer, A. Genetics and genomics of susceptibility and immune response to necrotic enteritis in chicken: A review. Mol. Biol. Rep. 2018, 45, 31–37. [Google Scholar] [CrossRef]
- Hofacre, C.L.; Smith, J.A.; Mathis, G.F. An optimist’s view on limiting necrotic enteritis and maintaining broiler gut health and performance in today’s marketing, food safety, and regulatory climate. Poul. Sci. 2018, 97, 1929–1933. [Google Scholar] [CrossRef] [PubMed]
- Coursodon, C.; Glock, R.; Moore, K.; Cooper, K.; Songer, J. TpeL-producing strains of Clostridium perfringens type A are highly virulent for broiler chicks. Anaerobe 2012, 18, 117–121. [Google Scholar] [CrossRef]
- Drew, M.; Syed, N.; Goldade, B.; Laarveld, B.; Van Kessel, A. Effects of dietary protein source and level on intestinal populations of Clostridium perfringens in broiler chickens. Poul. Sci. 2004, 83, 414–420. [Google Scholar] [CrossRef]
- Wu, S.-B.; Stanley, D.; Rodgers, N.; Swick, R.A.; Moore, R.J. Two necrotic enteritis predisposing factors, dietary fishmeal and Eimeria infection, induce large changes in the caecal microbiota of broiler chickens. Vet. Microbiol. 2014, 169, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, S.; Gadde, U.; Oh, S.; Lee, S.; Lillehoj, H. Allium hookeri supplementation improves intestinal immune response against necrotic enteritis in young broiler chickens. Poul. Sci. 2018, 97, 1899–1908. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Li, R.W.; Zhao, H.; Yan, X.; Lillehoj, H.S.; Sun, Z.; Oh, S.; Wang, Y.; Li, C. Effects of Eimeria maxima and Clostridium perfringens infections on cecal microbial composition and the possible correlation with body weight gain in broiler chickens. Res. Vet. Sci. 2020, 132, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Gadde, U.; Kim, W.H.; Oh, S.T.; Lillehoj, H.S. Alternatives to antibiotics for maximizing growth performance and feed efficiency in poultry: A review. Anim. Health Res. Rev. 2017, 18, 26–45. [Google Scholar] [CrossRef]
- Emami, N.K.; Dalloul, R.A. CENTENNIAL REVIEW: Recent Developments in Host-Pathogen Interactions during Necrotic Enteritis in Poultry. Poul. Sci. 2021, 100, 101330. [Google Scholar] [CrossRef]
- Caly, D.L.; D’Inca, R.; Auclair, E.; Drider, D. Alternatives to antibiotics to prevent necrotic enteritis in broiler chickens: A microbiologist’s perspective. Front. Microbiol. 2015, 6, 1336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh, S.T.; Lillehoj, H.S. The role of host genetic factors and host immunity in necrotic enteritis. Avian Pathol. 2016, 45, 313–316. [Google Scholar] [CrossRef]
- Paul, M.S.; Brisbin, J.T.; Abdul-Careem, M.F.; Sharif, S. Immunostimulatory properties of Toll-like receptor ligands in chickens. Vet. Immunol. Immunopathol. 2013, 152, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Criado-Mesas, L.; Abdelli, N.; Noce, A.; Farré, M.; Pérez, J.; Solà-Oriol, D.; Martin-Venegas, R.; Forouzandeh, A.; González-Solé, F.; Folch, J. Transversal gene expression panel to evaluate intestinal health in broiler chickens in different challenging conditions. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Fasina, Y.O.; Lillehoj, H.S. Characterization of intestinal immune response to Clostridium perfringens infection in broiler chickens. Poul. Sci. 2019, 98, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Rehman, H.U.; Vahjen, W.; Awad, W.A.; Zentek, J. Indigenous bacteria and bacterial metabolic products in the gastrointestinal tract of broiler chickens. Arch. Anim. Nutr. 2007, 61, 319–335. [Google Scholar] [CrossRef]
- Yang, W.-Y.; Lee, Y.; Lu, H.; Chou, C.-H.; Wang, C. Analysis of gut microbiota and the effect of lauric acid against necrotic enteritis in Clostridium perfringens and Eimeria side-by-side challenge model. PLoS ONE 2019, 14, e0205784. [Google Scholar] [CrossRef] [Green Version]
- Gu, C.; Lillehoj, H.S.; Sun, Z.; Lee, Y.; Zhao, H.; Xianyu, Z.; Yan, X.; Wang, Y.; Lin, S.; Liu, L.; et al. Characterization of Virulent netB(+)/tpeL(+) Clostridium perfringens Strains from Necrotic Enteritis-Affected Broiler Chicken Farms. Avian Dis. 2019, 63, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Shojadoost, B.; Vince, A.R.; Prescott, J.F. The successful experimental induction of necrotic enteritis in chickens by Clostridium perfringens: A critical review. Vet. Res. 2012, 43, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Yan, X.; Lillehoj, H.S.; Oh, S.; Liu, L.; Sun, Z.; Gu, C.; Lee, Y.; Xianyu, Z.; Zhao, H. Eimeria maxima-induced transcriptional changes in the cecal mucosa of broiler chickens. Parasit Vectors 2019, 12, 285. [Google Scholar] [CrossRef]
- Parreira, V.R.; Russell, K.; Athanasiadou, S.; Prescott, J.F. Comparative transcriptome analysis by RNAseq of necrotic enteritis Clostridium perfringens during in vivo colonization and in vitro conditions. BMC Microbiol. 2016, 16, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glass, C.K.; Olefsky, J.M. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab. 2012, 15, 635–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickard, J.M.; Zeng, M.Y.; Caruso, R.; Núñez, G. Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunol. Rev. 2017, 279, 70–89. [Google Scholar] [CrossRef]
- Fei, Z.; Li, S.; Wang, J.; Wang, Y.; Jiang, Z.; Huang, W.; Sun, H. Rhodotorula glutinis as a living cell liposome to deliver polypeptide drugs in vivo. Drug Deliv. 2019, 26, 51–62. [Google Scholar] [CrossRef] [Green Version]
- Brewer, J.W.; Solodushko, V.; Aragon, I.; Barrington, R.A. Phosphatidylcholine as a metabolic cue for determining B cell fate and function. Cell Immunol. 2016, 310, 78–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smallwood, A.; Hon, G.C.; Jin, F.; Henry, R.E.; Espinosa, J.M.; Ren, B. CBX3 regulates efficient RNA processing genome-wide. Genome Res. 2012, 22, 1426–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stossel, T.P.; Condeelis, J.; Cooley, L.; Hartwig, J.H.; Noegel, A.; Schleicher, M.; Shapiro, S.S. Filamins as integrators of cell mechanics and signalling. Nat. Rev. Mol. Cell Biol. 2001, 2, 138–145. [Google Scholar] [CrossRef]
- Lu, J.; Lian, G.; Lenkinski, R.; De Grand, A.; Vaid, R.R.; Bryce, T.; Stasenko, M.; Boskey, A.; Walsh, C.; Sheen, V. Filamin B mutations cause chondrocyte defects in skeletal development. Hum. Mol. Genet. 2007, 16, 1661–1675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krakow, D.; Robertson, S.P.; King, L.M.; Morgan, T.; Sebald, E.T.; Bertolotto, C.; Wachsmann-Hogiu, S.; Acuna, D.; Shapiro, S.S.; Takafuta, T.; et al. Mutations in the gene encoding filamin B disrupt vertebral segmentation, joint formation and skeletogenesis. Nat. Genet. 2004, 36, 405–410. [Google Scholar] [CrossRef]
- Agrawal, P.B.; Pierson, C.R.; Joshi, M.; Liu, X.; Ravenscroft, G.; Moghadaszadeh, B.; Talabere, T.; Viola, M.; Swanson, L.C.; Haliloglu, G.; et al. SPEG interacts with myotubularin, and its deficiency causes centronuclear myopathy with dilated cardiomyopathy. Am. J. Hum. Genet. 2014, 95, 218–226. [Google Scholar] [CrossRef] [Green Version]
- Nagahama, M.; Itohayashi, Y.; Hara, H.; Higashihara, M.; Fukatani, Y.; Takagishi, T.; Oda, M.; Kobayashi, K.; Nakagawa, I.; Sakurai, J. Cellular vacuolation induced by Clostridium perfringens epsilon-toxin. FEBS J. 2011, 278, 3395–3407. [Google Scholar] [CrossRef] [PubMed]
- Lahav-Ariel, L.; Caspi, M.; Nadar-Ponniah, P.T.; Zelikson, N.; Hofmann, I.; Hanson, K.K.; Franke, W.W.; Sklan, E.H.; Avraham, K.B.; Rosin-Arbesfeld, R. Striatin is a novel modulator of cell adhesion. FASEB J. 2019, 33, 4729–4740. [Google Scholar] [CrossRef]
- Roadcap, D.W.; Clemen, C.S.; Bear, J.E. The role of mammalian coronins in development and disease. Subcell. Biochem. 2008, 48, 124–135. [Google Scholar] [PubMed]
- Shao, J.; Zhang, H.; Wang, Z. Coronin 1c and F-actin Promote Metastasis of Breast Cancer. Med. Sci. Monit. 2018, 24, 5980–5987. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Peng, C.W.; Hou, J.X.; Zhang, Y.H.; Chen, C.; Chen, L.D.; Li, Y. Coronin-1C is a novel biomarker for hepatocellular carcinoma invasive progression identified by proteomics analysis and clinical validation. J. Exp. Clin. Cancer Res. 2010, 29, 17. [Google Scholar] [CrossRef] [Green Version]
- Chagnon, M.J.; Uetani, N.; Tremblay, M.L. Functional significance of the LAR receptor protein tyrosine phosphatase family in development and diseases. Biochem. Cell Biol. 2004, 82, 664–675. [Google Scholar] [CrossRef] [PubMed]
- Den Hertog, J.; Blanchetot, C.; Buist, A.; Overvoorde, J.; van der Sar, A.; Tertoolen, L.G. Receptor protein-tyrosine phosphatase signalling in development. Int. J. Dev. Biol. 1999, 43, 723–733. [Google Scholar] [PubMed]
- Nabeka, H. Prosaposin, a neurotrophic factor, protects neurons against kainic acid-induced neurotoxicity. Anat. Sci. Int. 2021, 96, 359–369. [Google Scholar] [CrossRef]
- Badura, M.; Braunstein, S.; Zavadil, J.; Schneider, R.J. DNA damage and eIF4G1 in breast cancer cells reprogram translation for survival and DNA repair mRNAs. Proc. Natl. Acad. Sci. USA 2012, 109, 18767–18772. [Google Scholar] [CrossRef] [Green Version]
- FitzGerald, L.M.; Zhang, X.; Kolb, S.; Kwon, E.M.; Liew, Y.C.; Hurtado-Coll, A.; Knudsen, B.S.; Ostrander, E.A.; Stanford, J.L. Investigation of the relationship between prostate cancer and MSMB and NCOA4 genetic variants and protein expression. Hum. Mutat. 2013, 34, 149–156. [Google Scholar] [CrossRef]
- Sakakura, I.; Tanabe, K.; Nouki, N.; Suzuki, M.; Satake, M.; Watanabe, T. The carboxy-terminal region of SMAP2 directs subcellular localization as well as Arf protein specificity. Biochem. Biophys. Res. Commun. 2011, 404, 661–666. [Google Scholar] [CrossRef]
- Skanseng, B.; Kaldhusdal, M.; Rudi, K. Comparison of chicken gut colonisation by the pathogens Campylobacter jejuni and Clostridium perfringens by real-time quantitative PCR. Mol. Cell. Probes 2006, 20, 269–279. [Google Scholar] [CrossRef]
- Shimizu, T.; Ohtani, K.; Hirakawa, H.; Ohshima, K.; Yamashita, A.; Shiba, T.; Ogasawara, N.; Hattori, M.; Kuhara, S.; Hayashi, H. Complete genome sequence of Clostridium perfringens, an anaerobic flesh-eater. Proc. Natl. Acad. Sci. USA 2002, 99, 996–1001. [Google Scholar] [CrossRef] [Green Version]


| Gene ID# | FDR | Chromosome | Gene Symbol | Description | Absolute Fold Change |
|---|---|---|---|---|---|
| ENSGALT00000099249 | 0.001 | 9 | PCYT1A | phosphate cytidylyltransferase 1, choline, alpha | 26.26 |
| ENSGALT00000065275 | 0 | 2 | CBX3 | chromobox 3 (CBX3) | 25.65 |
| ENSGALT00000102383 | 0.026 | 12 | FLNB | filamin B (FLNB) | 25.32 |
| ENSGALT00000080045 | 0 | 10 | VPS33B, | late endosome and lysosome associated | 24.22 |
| ENSGALT00000047160 | 0.012 | 7 | SPEG | complex locus [SourceNCBIgene; Acc429033] 0 | 20.46 |
| ENSGALT00000017218 | 0.013 | 3 | STRN | striatin [SourceHGNC Symbol;AccHGNC11424] 00 | 18.08 |
| ENSGALT00000103665 | 0.044 | 31 | NA | 16.51 | |
| ENSGALT00000065256 | 0.025 | 3 | DAAM2 | dishevelled associated activator of morphogenesis | 16.38 |
| ENSGALT00000101515 | 0.008 | 28 | TCF3 | transcription factor 3 | 12.86 |
| ENSGALT00000108349 | 0 | 17 | NACC2 | NACC family member | 12.76 |
| ENSGALT00000095627 | 0.005 | 33 | CCS | copper chaperone for superoxide dismutase | 12.64 |
| ENSGALT00000082640 | 0.013 | 33 | NACA | nascent polypeptide associated complex subunit | 12.29 |
| ENSGALT00000047943 | 0.001 | 15 | DEP | domain containing 5 [SourceNCBI gene; Acc416956] | 11.39 |
| ENSGALT00000087703 | 0 | 1 | NA | 11.32 | |
| ENSGALT00000094693 | 0.001 | 26 | NA | 10.12 | |
| ENSGALT00000026339 | 0.039 | 3 | GSTA2 | Glutathione S-Transferase 2 | 9.41 |
| ENSGALT00000012083 | 0.009 | 9 | PCYT1A | phosphate cytidylyltransferase 1, choline, alpha | 8.66 |
| ENSGALT00000090554 | 0.018 | NA | 7.86 | ||
| ENSGALT00000074687 | 0 | 20 | MYL9 | myosin, light chain 9, regulatory | 7.79 |
| ENSGALT00000014587 | 0.003 | 3 | EPCAM | epithelial cell adhesion | 6.86 |
| ENSGALT00000091530 | 0.012 | 6 | NA | 6.45 | |
| ENSGALT00000095666 | 0 | 2 | SLC4A7 | solute carrier family 4 member | 6.36 |
| ENSGALT00000018245 | 0.024 | 4 | NA | 6.08 | |
| ENSGALT00000050930 | 0.013 | 23 | PUM1 | pumilio RNA binding | 6.01 |
| ENSGALT00000081307 | 0.001 | 2 | STT3B | STT3B, catalytic subunit | 5.98 |
| ENSGALT00000067100 | 0.011 | 1 | ATP2B1 | ATese plasma membrane | 5.52 |
| ENSGALT00000063811 | 0.008 | Z | ribosomal | ribosomal protein S23 | 5.36 |
| ENSGALT00000107263 | 0.039 | 1 | FNDC3A | fibronectin type III | 5.30 |
| ENSGALT00000099291 | 0.029 | 28 | GATAD2A | GATA zinc finger domain containing | 5.13 |
| ENSGALT00000092961 | 0.019 | 25 | MTMR11 | myotubularin related protein 11 [SourceHGNC | 4.46 |
| ENSGALT00000092785 | 0.016 | NA | 4.29 | ||
| ENSGALT00000060227 | 0.005 | 14 | HBM | hemoglobin subunit mu | 4.26 |
| ENSGALT00000056811 | 0.012 | 30 | DNM2 | dynamin 2 [SourceHGNC Symbol;AccHGNC2974] 0 | 4.17 |
| ENSGALT00000057600 | 0.013 | 1 | IL17D | interleukin 17D [SourceHGNC Symbol;AccHGNC5984] 0 | 4.07 |
| ENSGALT00000070149 | 0.045 | 31 | DHDH | dihydrodiol dehydrogena | 4.04 |
| ENSGALT00000094063 | 0.045 | 16 | NA | 3.82 | |
| ENSGALT00000026767 | 0.026 | 3 | PBK | PDZ binding kinase | 3.82 |
| ENSGALT00000033333 | 0.012 | 8 | LMO4 | LIM domain only | 3.81 |
| ENSGALT00000098491 | 0.004 | 6 | NA | 3.50 | |
| ENSGALT00000053882 | 0.031 | 17 | NA | 3.36 | |
| ENSGALT00000089781 | 0.001 | 1 | DCN | decorin (DCN), mRNA | 3.31 |
| ENSGALT00000036373 | 0.04 | 1 | HBBA | hemoglobin beta, subunit A [SourceNCBI | 3.20 |
| ENSGALT00000038226 | 0.035 | 15 | SMTN | smoothelin [SourceNCBI gene; Acc100858894] 00 | 3.20 |
| ENSGALT00000104581 | 0.016 | 2 | 2.66 | ||
| ENSGALT00000043405 | 0.047 | 28 | TIMM13 | translocase of inner mitochondrial membrane | 2.59 |
| ENSGALT00000107499 | 0.047 | 18 | SRSF2 | serine/arginine-rich splicing factor | 2.55 |
| ENSGALT00000068151 | 0.023 | MT | ND6 | NADH dehydrogenase subunit 6 [SourceNCBI | 2.28 |
| ENSGALT00000045265 | 0.045 | 3 | Cystatin | SourceUniProtKB/Swiss-Prot; AccP01038]0000 | 2.11 |
| Gene ID# | FDR | Chromosome | Gene Symbol | Description | Absolute Fold Change |
|---|---|---|---|---|---|
| ENSGALT00000096799 | 0.045 | #N/A | #N/A | −45.54 | |
| ENSGALT00000087336 | 0.021 | 15 | CORO1C | coronin 1C (CORO1C) | −32.92 |
| ENSGALT00000077706 | 0.002 | 8 | PTPRF | protein tyrosine phosphatase, receptor type | −29.51 |
| ENSGALT00000081103 | 0 | 6 | PSAP | prosaposin | −27.67 |
| ENSGALT00000049779 | 0 | 9 | EIF4G1 | eukaryotic translation initiation factor 4 | −24.18 |
| ENSGALT00000087331 | 0.016 | 6 | microsemino protein beta | −22.96 | |
| ENSGALT00000078878 | 0.043 | #N/A | #N/A | −22.35 | |
| ENSGALT00000066511 | 0.023 | 2 | RPL7 | ribosomal protein L7 | −15.15 |
| ENSGALT00000064276 | 0.028 | 18 | TBCD | tubulin folding cofactor | −12.68 |
| ENSGALT00000018692 | 0 | 5 | EIF5 | eukaryotic translation initiation | −12.48 |
| ENSGALT00000096298 | 0.036 | 3 | SMAP1 | small ArfGAP 1 | −12.08 |
| ENSGALT00000021113 | 0 | 1 | DENND5B | DENN domain containing 5B | −10.93 |
| ENSGALT00000036292 | 0.005 | 12 | PRKCD | protein kinase C | −10.82 |
| ENSGALT00000098137 | 0 | 3 | SPTBN1 | spectrinbeta non-erythrocytic | −9.17 |
| ENSGALT00000101130 | 0 | 9 | PCYT1A | phosphate cytidylyltransferase 1, choline, alpha | −8.61 |
| ENSGALT00000047339 | 0.05 | 4 | SMAD1 | SMAD family member 1 | −8.45 |
| ENSGALT00000095523 | 0.007 | 4 | FAT1 | FAT atypical cadherin 1 | −8.33 |
| ENSGALT00000096470 | 0 | 2 | SLC4A7 | Solute carrier family4 member | −6.63 |
| ENSGALT00000107225 | 0 | 24 | APOA4 | apolipoprotein A4(APOA4) | −6.43 |
| ENSGALT00000055069 | 0.003 | 2 | SEMA5A | semaphorin 5A | −6.34 |
| ENSGALT00000007275 | 0.027 | 20 | NCOA3 | nuclear receptor coactivator 3 | −6.32 |
| ENSGALT00000090409 | 0.05 | 1 | TMCC3 | transmembrane and coiled-coil domain family | −5.76 |
| ENSGALT00000107684 | 0.001 | 6 | PDCD4 | programmed cell death 4 | −5.31 |
| ENSGALT00000015332 | 0.026 | 3 | BROX | BRO1 domain and CAAX motif | −4.73 |
| ENSGALT00000086950 | 0.023 | 2 | YWHAZ | tyrosine 3-monooxygenase/tryptophan 5-monooxygenase | −4.63 |
| ENSGALT00000017711 | 0.045 | 7 | ABCB11 | ATP binding cassette subfamily B | −4.50 |
| ENSGALT00000022319 | 0.003 | 3 | GTF2H5 | general transcription factor | −4.37 |
| ENSGALT00000104993 | 0.009 | 8 | LMO4 | LIM domain only | −4.26 |
| ENSGALT00000004104 | 0.027 | 21 | CLSTN1 | Cal syntenin 1 (CLSTN1) | −3.90 |
| ENSGALT00000007773 | 0.002 | 15 | ISCU | iron-sulfur cluster assembly enzyme | −3.78 |
| ENSGALT00000061711 | 0.004 | 23 | PTP4A2 | protein tyrosine phosphatase type IVA, | −3.53 |
| ENSGALT00000006691 | 0.012 | 8 | SOAT1 | sterol O-acyltransferase 1 | −3.32 |
| ENSGALT00000032201 | 0.025 | 4 | HPGD | 15-hydroxyprostaglandin dehydrogenase (HPGD) | −3.23 |
| ENSGALT00000039749 | 0.001 | 1 | CD36 | CD36 molecule (CD36) | −3.15 |
| ENSGALT00000025653 | 0 | 3 | EEF1A1 | eukaryotic translation elongation factor 1 | −3.12 |
| ENSGALT00000105502 | 0.017 | #N/A | #N/A | −2.90 | |
| ENSGALT00000008547 | 0.001 | 9 | RBP2 | retinol binding protein | −2.90 |
| ENSGALT00000066968 | 0 | #N/A | #N/A | −2.83 | |
| ENSGALT00000063525 | 0.045 | 6 | CYP2C18 | cytochrome | −2.79 |
| ENSGALT00000018393 | 0.025 | 2 | RAB5A | RAB5A, member RAS | −2.74 |
| ENSGALT00000024116 | 0.026 | 3 | SOT3A1L | sulfotransferase family 3A | −2.56 |
| ENSGALT00000052923 | 0.023 | 11 | CA7 | carbonic anhydrase 7 | −2.54 |
| ENSGALT00000089467 | 0.049 | 16 | BF1 | MHC BF1 | −2.47 |
| ENSGALT00000019554 | 0.043 | 4 | FABP2 | fatty acid binding protein 2 | −2.45 |
| ENSGALT00000083719 | 0.012 | 2 | MEP1B | meprin A subunit beta | −2.39 |
| ENSGALT00000086032 | 0.028 | 1 | GAPDH | glyceraldehyde-3-phosphate dehydrogenase | −2.33 |
| ENSGALT00000062517 | 0.035 | #N/A | #N/A | −2.21 | |
| ENSGALT00000004055 | 0.028 | 15 | RAN | RAN, member RAS | −2.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, M.; Yuan, B.; Yan, X.; Sun, Z.; Lillehoj, H.S.; Lee, Y.; Baldwin-Bott, C.; Li, C. Clostridium perfringens-Induced Host-Pathogen Transcriptional Changes in the Small Intestine of Broiler Chickens. Pathogens 2021, 10, 1607. https://doi.org/10.3390/pathogens10121607
Lu M, Yuan B, Yan X, Sun Z, Lillehoj HS, Lee Y, Baldwin-Bott C, Li C. Clostridium perfringens-Induced Host-Pathogen Transcriptional Changes in the Small Intestine of Broiler Chickens. Pathogens. 2021; 10(12):1607. https://doi.org/10.3390/pathogens10121607
Chicago/Turabian StyleLu, Mingmin, Baohong Yuan, Xianghe Yan, Zhifeng Sun, Hyun S. Lillehoj, Youngsub Lee, Calder Baldwin-Bott, and Charles Li. 2021. "Clostridium perfringens-Induced Host-Pathogen Transcriptional Changes in the Small Intestine of Broiler Chickens" Pathogens 10, no. 12: 1607. https://doi.org/10.3390/pathogens10121607
APA StyleLu, M., Yuan, B., Yan, X., Sun, Z., Lillehoj, H. S., Lee, Y., Baldwin-Bott, C., & Li, C. (2021). Clostridium perfringens-Induced Host-Pathogen Transcriptional Changes in the Small Intestine of Broiler Chickens. Pathogens, 10(12), 1607. https://doi.org/10.3390/pathogens10121607





