Gender, Shame, and Social Support in LGBTQI+ Exposed to Discrimination: A Model for Understanding the Impact on Mental Health
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Participants’ Sociodemographic Characteristics
3.2. Independent and Interaction Impact of Sexual Orientation and Gender on Exposure to Discrimination, Mental Health, Shame, and Social Support
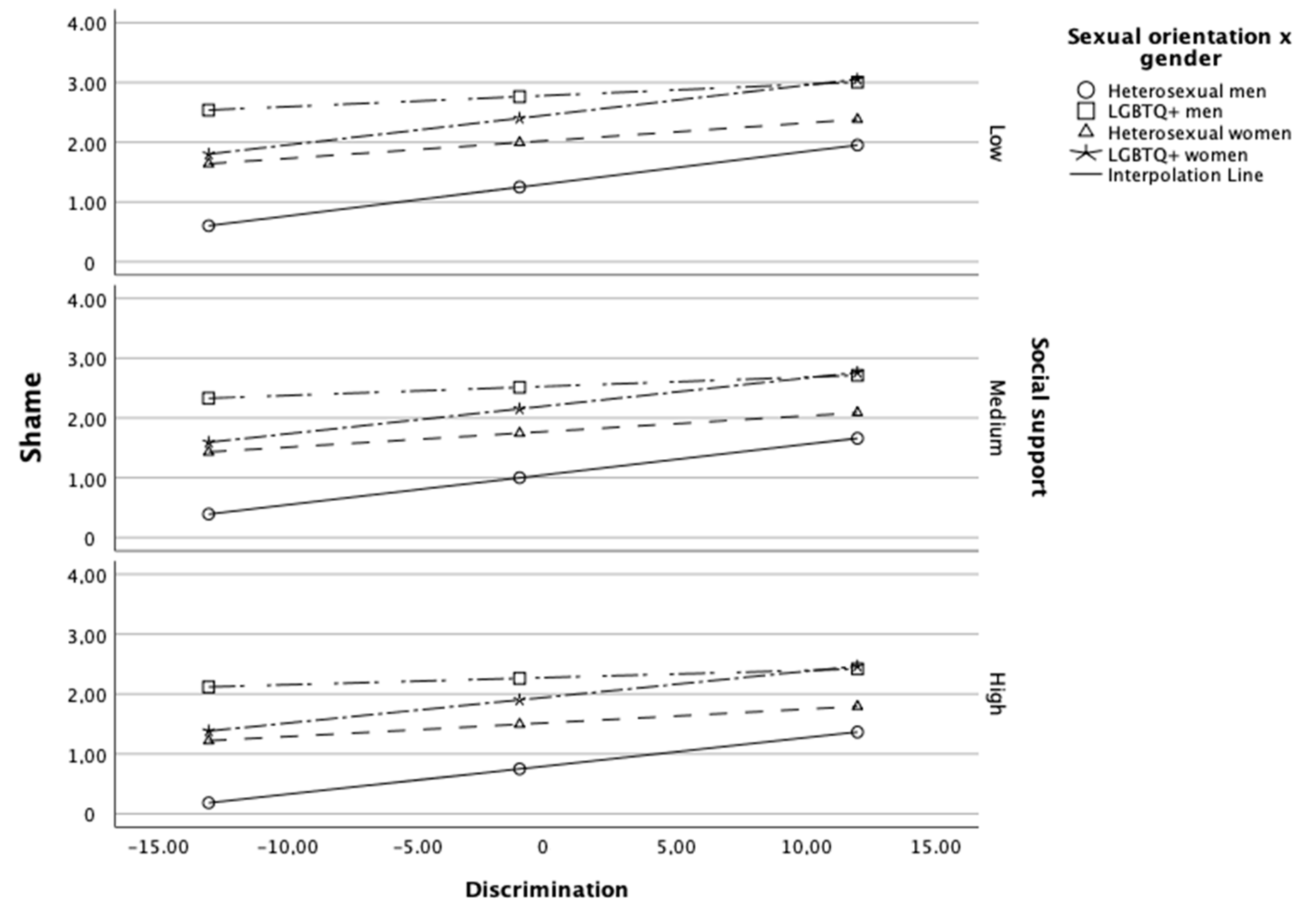
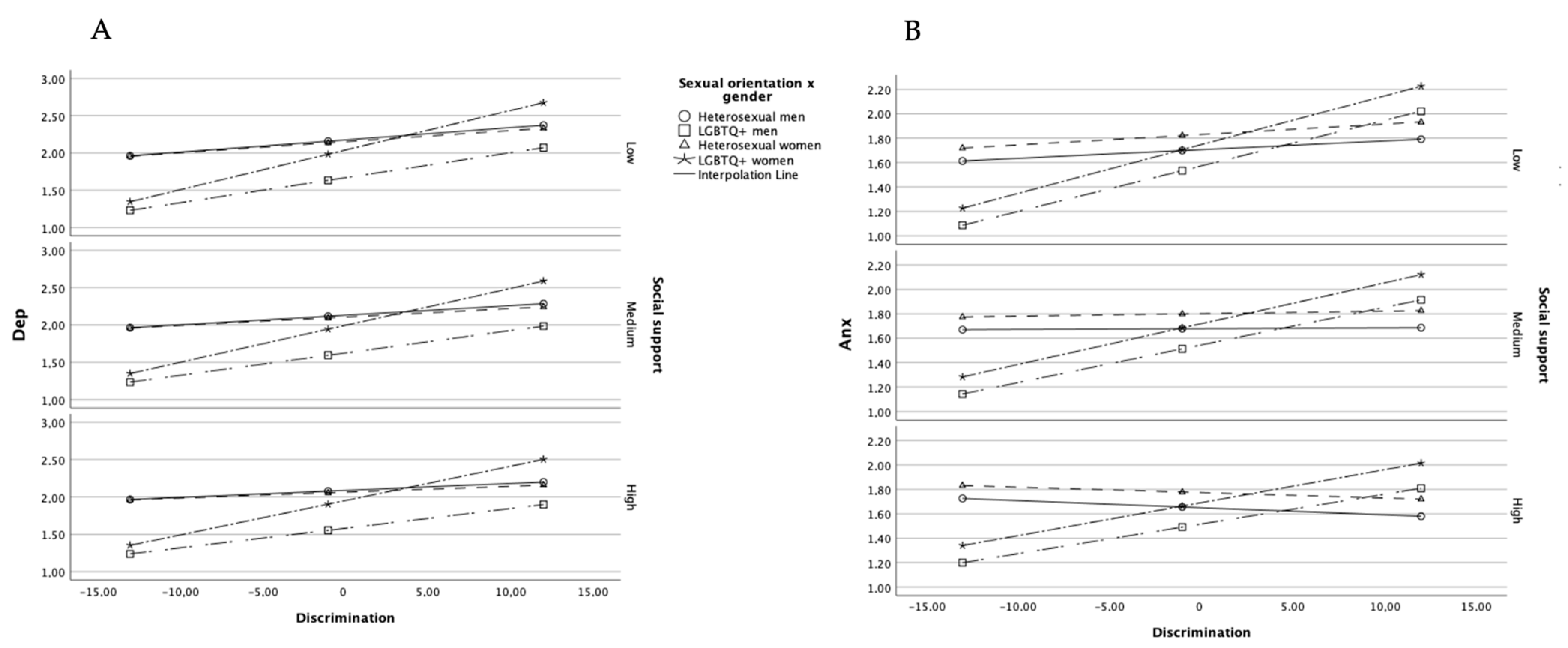
3.3. Impact of Exposure to Discrimination on Mental Health: The Mediating Role of Shame and the Moderating Role of Social Support
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ballard, Mary E., John Paul Jameson, and Denise M. Martz. 2017. Sexual Identity and Risk Behaviors among Adolescents in Rural Appalachia. Rural Mental Health 41: 17–29. [Google Scholar] [CrossRef]
- Benetti-McQuoid, Jessica, and Krisanne Bursik. 2005. Individual differences in experiences of and responses to guilt and shame: Examining the lenses of gender and gender role. Sex Roles 53: 133–42. [Google Scholar] [CrossRef]
- Bostwick, Wendy B., Carol J. Boyd, Tonda L. Hughes, Brady T. West, and Sean Esteban McCabe. 2014. Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry 84: 35. [Google Scholar] [CrossRef]
- Breakwell, Glynis. 2020. In the Age of Societal Uncertainty, the Era of Threat. In Societies under Threat: A Pluri-Disciplinary Approach. Edited by Denise Jodelet, Jorge Vala and Ewa Drozda-Senkowska. New York: Springer-Nature, pp. 55–74. [Google Scholar]
- Breakwell, Glynis M., and Rusi Jaspal. 2022. Coming out, Distress and Identity Threat in Gay Men in the UK. Sexuality Research & Social Policy 19: 1166–77. [Google Scholar] [CrossRef]
- Brown, Adrienne, Simon M. Rice, Debra J. Rickwood, and Alexandra G. Parker. 2016. Systematic Review of Barriers and Facilitators to Accessing and Engaging with Mental Health Care among At-Risk Young People: Barriers and Facilitators to Youth Mental Health Care. Asia-Pacific Psychiatry 8: 3–22. [Google Scholar] [CrossRef]
- Canavarro, M. Cristina. 1999. Inventário de Sintomas Psicopatológicos BSI. In Testes e Provas Psicológicas em Portugal. Edited by Mário Simões, Miguel Gonçalves and Leandro Almeida. Braga: SHO/APPORT, vol. 2, pp. 95–109. [Google Scholar]
- Canavarro, M. Cristina, Adriano Vaz Serra, Mário R. Simões, Marco Pereira, Sofia Gameiro, Manuel J. Quartilho, Daniel Rijo, Carlos Carona, and Tiago Paredes. 2007. Avaliação psicológica: Instrumentos validados para a população portuguesa. Edited by Mário Simões, Carla Machado, Miguel Gonçalves and Leandro Almeida. Coimbra: Quarteto Editora, vol. III, pp. 77–100. [Google Scholar]
- Connell, Robert W., and James W. Messerschmidt. 2005. Hegemonic masculinity: Rethinking the concept. Gender & Society 19: 829–59. [Google Scholar] [CrossRef]
- Cook, David R. 1996. Empirical studies of shame and guilt: The Internalized Shame Scale. In Knowing Feeling: Affect, Script, and Psychotherapy. Edited by Donald L. Nathanson. New York: W. W. Norton & Company, pp. 132–65. [Google Scholar]
- Corliss, Heather L., Marvin Belzer, Catherine Forbes, and Erin C. Wilson. 2007. An Evaluation of Service Utilization among Male to Female Transgender Youth: Qualitative Study of a Clinic-Based Sample. Journal of LGBT Health Research 3: 49–61. [Google Scholar] [CrossRef]
- Dahlhamer, James M., Adena M. Galinsky, Sarah S. Joestl, and Brian W. Ward. 2016. Barriers to Health Care among Adults Identifying as Sexual Minorities: A US National Study. American Journal of Public Health 106: 1116–22. [Google Scholar] [CrossRef]
- Derogatis, Leonard R. 1993. Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual, 3rd ed. Minneapolis: National Computer Systems. [Google Scholar]
- Everly, Benjamin A., Miguel M. Unzueta, and Margaret J. Shih. 2016. Can Being Gay Provide a Boost in the Hiring Process? Maybe If the Boss Is Female. Journal of Business and Psychology 31: 293–306. [Google Scholar] [CrossRef]
- Faul, Franz, Edgar Erdfelder, Albert-Georg Lang, and Axel Buchner. 2007. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39: 175–91. [Google Scholar] [CrossRef]
- Faul, Franz, Edgar Erdfelder, Axel Buchner, and Albert-Georg Lang. 2009. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods 41: 1149–60. [Google Scholar] [CrossRef] [PubMed]
- Feinstein, Brian A., Marvin R. Goldfried, and Joanne Davila. 2012. The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of Consulting and Clinical Psychology 80: 917. [Google Scholar] [CrossRef] [PubMed]
- Felner, Jennifer K., Jennifer P. Wisdom, Tenneill Williams, Laura Katuska, Sean J. Haley, Hee-Jin Jun, and Heather L. Corliss. 2020. Stress, Coping, and Context: Examining Substance Use among LGBTQ Young Adults with Probable Substance Use Disorders. Psychiatric Services 71: 112–20. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, Federico, Chiara Imperato, and Tiziana Mancini. 2021. Heteronormativity and the Justification of Gender Hierarchy: Investigating the Archival Data from 16 European Countries. Frontiers in Psychology 12: 686974. [Google Scholar] [CrossRef]
- Fontanella, Cynthia A., Danielle L. Hiance-Steelesmith, Gary S. Phillips, Jeffrey A. Bridge, Natalie Lester, Helen Anne Sweeney, and John V. Campo. 2015. Widening Rural-Urban Disparities in Youth Suicides, United States, 1996–2010. JAMA Pediatrics 169: 466–73. [Google Scholar] [CrossRef] [PubMed]
- Gato, Jorge, Jaime Barrientos, Fiona Tasker, Marina Miscioscia, Elder Cerqueira-Santos, Anna Malmquist, Daniel Seabra, Daniela Leal, Marie Houghton, Mikael Poli, and et al. 2021. Psychosocial Effects of the COVID-19 Pandemic and Mental Health among LGBTQ+ Young Adults: A Cross-Cultural Comparison across Six Nations. Journal of Homosexuality 68: 612–30. [Google Scholar] [CrossRef] [PubMed]
- Gebhard, Kris T., Lauren B. Cattaneo, June P. Tangney, Stephanie Hargrove, and Rachel Shor. 2019. Threatened-masculinity shame-related responses among straight men: Measurement and relationship to aggression. Psychology of Men & Masculinities 20: 429. [Google Scholar] [CrossRef]
- Gilbert, Paul. 2022. Shame, humiliation, guilt, and social status: The distress and harms of social disconnection. In Compassion Focused Therapy. Abingdon: Routledge, pp. 122–63. [Google Scholar]
- Gilligan, Carol, and Naomi Snider. 2018. Why Does Patriarchy Persist? Hoboken: John Wiley & Sons. [Google Scholar]
- Greytak, Emily A., Joseph G. Kosciw, and Madelyn J. Boesen. 2013. Putting the ‘T’ in ‘Resource’: The Benefits of LGBT-Related School Resources for Transgender Youth. Journal of LGBT Youth 10: 45–63. [Google Scholar] [CrossRef]
- Gross, James J. 2015. Emotion regulation: Current status and future prospects. Psychological Inquiry 26: 1–26. [Google Scholar] [CrossRef]
- Hafeez, Hudaisa, Muhammad Zeshan, Muhammad A. Tahir, Nusrat Jahan, and Sadiq Naveed. 2017. Health Care Disparities among Lesbian, Gay, Bisexual, and Transgender Youth: A Literature Review. Cureus 9: e1184. [Google Scholar] [CrossRef]
- Hall, William J. 2018. Psychosocial risk and protective factors for depression among lesbian, gay, bisexual, and queer youth: A systematic review. Journal of Homosexuality 65: 263–316. [Google Scholar] [CrossRef] [PubMed]
- Han, Benjamin H., Dustin T. Duncan, Mauricio Arcila-Mesa, and Joseph J. Palamar. 2020. Co-Occurring Mental Illness, Drug Use, and Medical Multimorbidity among Lesbian, Gay, and Bisexual Middle-Aged and Older Adults in the United States: A Nationally Representative Study. BMC Public Health 20: 1123. [Google Scholar] [CrossRef] [PubMed]
- Haynes, Tonya, and Halimah A. F. DeShong. 2017. Queering Feminist Approaches to Gender-Based Violence in the Anglophone Caribbean. Social and Economic Studies 66: 105–31. [Google Scholar]
- Henry, Richard S., Cosima Hoetger, Annie E. Rabinovitch, Adriana Aguayo Arelis, Brenda Viridiana Rabago Barajas, and Paul B. Perrin. 2021. Discrimination, Mental Health, and Suicidal Ideation among Sexual Minority Adults in Latin America: Considering the Roles of Social Support and Religiosity. Trauma Care 1: 143–61. [Google Scholar] [CrossRef]
- Herek, Gregory M., and Linda D. Garnets. 2007. Sexual Orientation and Mental Health. Annual Review of Clinical Psychology 3: 353–75. [Google Scholar] [CrossRef]
- Herek, Gregory M., J. Roy Gillis, and Jeanine C. Cogan. 2015. Internalized Stigma among Sexual Minority Adults: Insights from a Social Psychological Perspective. Stigma and Health 1: 18–34. [Google Scholar] [CrossRef]
- Hubbard, Luke. 2020. Online Hate Crime Report: Challenging Online Homophobia, Biphobia and Transphobia. London: Galop, the LGBT+ Anti-Violence Charity. Available online: https://galop.org.uk/wp-content/uploads/2021/06/Galop-Hate-Crime-Report-2021-1.pdf (accessed on 22 October 2022).
- Igartua, Juan-José, and Andrew F. Hayes. 2021. Mediation, Moderation, and Conditional Process Analysis: Concepts, Computations, and Some Common Confusions. The Spanish Journal of Psychology 24: e49. [Google Scholar] [CrossRef]
- ILGA. 2020. Relatório Anual 2019: Discriminação contra pessoas LGBTQIA+ [Discrimination against LGBTQIA+ People]. Available online: https://ilga-portugal.pt/ficheiros/pdfs/observatorio/ILGA_Relatorio_Discriminacao_2019.pdf (accessed on 22 October 2022).
- Jablonski, Kate. 2020. Minority Stress, Social Support, and Mental Health Among LGBQP+ Religious Disaffiliates. Doctoral dissertation, The University of San Francisco, San Francisco, CA, USA. Available online: https://repository.usfca.edu/cgi/viewcontent.cgi?article=1537&context=diss (accessed on 22 October 2022).
- James, Sandy, Jody Herman, Susan Rankin, Mara Keisling, Lisa Mottet, and Ma’ayan Anafi. 2016. The Report of the 2015 US Transgender Survey. Available online: https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf (accessed on 22 October 2022).
- Jaspal, Rusi, Barbara Lopes, and Glynis M. Breakwell. 2022. Minority Stressors, Protective Factors and Mental Health Outcomes in Lesbian, Gay and Bisexual People in the UK. Current Psychology. [Google Scholar] [CrossRef]
- Johns, Michelle Marie, Oscar Beltran, Heather L. Armstrong, Paula E. Jayne, and Lisa C. Barrios. 2018. Protective Factors among Transgender and Gender Variant Youth: A Systematic Review by Socioecological Level. The Journal of Primary Prevention 39: 263–301. [Google Scholar] [CrossRef]
- Kaniuka, Andrea, Kelley C. Pugh, Megan Jordan, Byron Brooks, Julia Dodd, Abbey K. Mann, Stacey L. Williams, and Jameson K. Hirsch. 2019. Stigma and Suicide Risk among the LGBTQ Population: Are Anxiety and Depression to Blame and Can Connectedness to the LGBTQ Community Help? Journal of Gay & Lesbian Mental Health 23: 205–20. [Google Scholar] [CrossRef]
- Lisboa, Manuel (coord.), Zélia Barroso, Joana Patrício, and Alexandra Leandro. 2009. Violência e Género—Inquérito Nacional sobre a Violência Contra as Mulheres e Homens [Violence and Gender—National Survey on Violence Against Women and Men]. Comissão para a Cidadania e Igualdade de Género [Commission for Citizenship and Gender Equality]. Available online: https://run.unl.pt/bitstream/10362/56714/1/Viol_ncia_e_G_nero.pdf (accessed on 22 October 2022).
- Lozano-Verduzco, Ignacio, Julián Alfredo Fernández-Niño, and Ricardo Baruch-Domínguez. 2017. Association between Internalized Homophobia and Mental Health Indicators in LGBT Individuals in Mexico City. Salud Mental 40: 219–26. [Google Scholar] [CrossRef]
- Luiggi-Hernández, José Giovanni, Gabriel E. Laborde Torres, Joyce González Domínguez, Glorián M. Carrasquillo Sánchez, Marieli Piñero Meléndez, Dánae M. Castro Medina, and Camil D. González Rentas. 2015. Outing the discrimination towards LGBT people during the hiring process: What about their well-being? Revista Puertorriqueña de Psicología 26: 194–213. [Google Scholar]
- Luthar, Suniya S., Elizabeth J. Crossman, and Phillip J. Small. 2015. Resilience and adversity. In Handbook of Child Psychology and Developmental Science. Edited by Richard M. Lerner, Michael E. Lamb and Marc H. Bornstein. Hoboken: John Wiley & Sons, Inc., vol. 3, pp. 247–86. [Google Scholar] [CrossRef]
- Marchia, Joseph, and Jamie M. Sommer. 2019. (Re)Defining Heteronormativity. Sexualities 22: 267–95. [Google Scholar] [CrossRef]
- Matos, Marcela, and José Pinto-Gouveia. 2014. Shamed by a parent or by others: The role of attachment in shame memories relation to depression. International Journal of Psychology and Psychological Therapy 14: 217–44. [Google Scholar]
- Matos, Marcela, Sérgio A. Carvalho, Marina Cunha, Ana Galhardo, and Carlos Sepodes. 2017. Psychological flexibility and self-compassion in gay and heterosexual men: How they relate to childhood memories, shame, and depressive symptoms. Journal of LGBT Issues in Counseling 11: 88–105. [Google Scholar] [CrossRef]
- Matos, Marcela, José Pinto-Gouveia, and Cristiana Duarte. 2012. When I don’t like myself: Portuguese version of the internalized shame scale. The Spanish Journal of Psychology 15: 1411–23. [Google Scholar] [CrossRef]
- McDermott, Elizabeth, Katrina Roen, and Anna Piela. 2015. Explaining Self-Harm: Youth Cybertalk and Marginalized Sexualities and Genders. Youth & Society 47: 873–89. [Google Scholar] [CrossRef]
- McGuire, Jenifer K., Charles R. Anderson, Russell B. Toomey, and Stephen T. Russell. 2010. School Climate for Transgender Youth: A Mixed Method Investigation of Student Experiences and School Responses. Journal of Youth and Adolescence 39: 1175–88. [Google Scholar] [CrossRef]
- Meyer, Ilan H. 2013. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychology of Sexual Orientation and Gender Diversity 1: 3–26. [Google Scholar] [CrossRef]
- Mishel, Emma. 2016. Discrimination against Queer Women in the U.S. Workforce: A Résumé Audit Study. Socius 2: 1–13. [Google Scholar] [CrossRef]
- Newcomb, Michael E., and Brian Mustanski. 2010. Internalized Homophobia and Internalizing Mental Health Problems: A Meta-Analytic Review. Clinical Psychology Review 30: 1019–29. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, Michael E., Michael C. LaSala, Alida Bouris, Brian Mustanski, Guillermo Prado, Sheree M. Schrager, and David M. Huebner. 2019. The Influence of Families on LGBTQ Youth Health: A Call to Action for Innovation in Research and Intervention Development. LGBT Health 6: 139–45. [Google Scholar] [CrossRef] [PubMed]
- Norton, Michael I., and Samuel R. Sommers. 2011. Whites See Racism as a Zero-Sum Game That They Are Now Losing. Perspectives on Psychological Science 6: 215–18. [Google Scholar] [CrossRef]
- Oginni, Olakunle A., Kolawole S. Mosaku, Boladale M. Mapayi, Adesanmi Akinsulore, and Temitope O. Afolabi. 2018. Depression and Associated Factors among Gay and Heterosexual Male University Students in Nigeria. Archives of Sexual Behavior 47: 1119–32. [Google Scholar] [CrossRef] [PubMed]
- Ozeren, Emir. 2014. Sexual Orientation Discrimination in the Workplace: A Systematic Review of Literature. Procedia, Social and Behavioral Sciences 109: 1203–15. [Google Scholar] [CrossRef]
- Parra, Luis A., Timothy S. Bell, Michael Benibgui, Jonathan L. Helm, and Paul D. Hastings. 2018. The Buffering Effect of Peer Support on the Links between Family Rejection and Psychosocial Adjustment in LGB Emerging Adults. Journal of Social and Personal Relationships 35: 854–71. [Google Scholar] [CrossRef]
- Pereira, Henrique, and Patrícia Silva. 2021. The Importance of Social Support, Positive Identity, and Resilience in the Successful Aging of Older Sexual Minority Men. Geriatrics 6: 98. [Google Scholar] [CrossRef]
- Pflum, Samantha R., Rylan J. Testa, Kimberly F. Balsam, Peter B. Goldblum, and Bruce Bongar. 2015. Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychology of Sexual Orientation and Gender Diversity 2: 281. [Google Scholar] [CrossRef]
- Pizmony-Levy, Oren, and Joseph G. Kosciw. 2016. School Climate and the Experience of LGBT Students: A Comparison of the United States and Israel. Journal of LGBT Youth 13: 46–66. [Google Scholar] [CrossRef]
- Reck, Jen. 2009. Homeless Gay and Transgender Youth of Color in San Francisco: ‘No One Likes Street Kids’—Even in the Castro. Journal of LGBT Youth 6: 223–42. [Google Scholar] [CrossRef]
- Reilly, Erin D., Aaron B. Rochlen, and Germine H. Awad. 2014. Men’s self-compassion and self-esteem: The moderating roles of shame and masculine norm adherence. Psychology of Men & Masculinity 15: 22. [Google Scholar] [CrossRef]
- Rice, Simon M., Helen M. Aucote, Anne Maria Möller-Leimkühler, Alexandra G. Parker, Ryan A. Kaplan, Zac E. Seidler, Haryana M. Dhillon, and G. Amminger. 2016. Conformity to Masculine Norms and the Mediating Role of Internalised Shame on Men’s Depression: Findings from an Australian Community Sample. International Journal of Men’s Health 15: 157–64. [Google Scholar]
- Rizzuto, Ana-María. 2014. Shame in Psychoanalysis: The Function of Unconscious Fantasies. In Shame and Sexuality: Psychoanalysis and Visual Culture. Edited by Claire Pajaczkowska and Ivan Ward. Abingdon: Routledge, pp. 65–86. [Google Scholar]
- Rothman, Emily F., Deinera Exner, and Allyson L. Baughman. 2011. The prevalence of sexual assault against people who identify as gay, lesbian, or bisexual in the United States: A systematic review. Trauma, Violence, & Abuse 12: 55–66. [Google Scholar] [CrossRef]
- Russell, Stephen T., and Jessica N. Fish. 2016. Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annual Review of Clinical Psychology 12: 465–87. [Google Scholar] [CrossRef] [PubMed]
- Ryan, Caitlin, Stephen T. Russell, David Huebner, Rafael Diaz, and Jorge Sanchez. 2010. Family Acceptance in Adolescence and the Health of LGBT Young Adults. Journal of Child and Adolescent Psychiatric Nursing 23: 205–13. [Google Scholar] [CrossRef] [PubMed]
- Sandfort, Theo G. M., Ron de Graaf, Margreet Ten Have, Yusuf Ransome, and Paul Schnabel. 2014. Same-Sex Sexuality and Psychiatric Disorders in the Second Netherlands Mental Health Survey and Incidence Study (NEMESIS-2). LGBT Health 1: 292–301. [Google Scholar] [CrossRef]
- Sattler, Frank A., Ulrich Wagner, and Hanna Christiansen. 2016. Effects of Minority Stress, Group-Level Coping, and Social Support on Mental Health of German Gay Men. PLoS ONE 11: e0150562. [Google Scholar] [CrossRef]
- Scheer, Jillian R., Patricia Harney, Jessica Esposito, and Julie M. Woulfe. 2020. Self-Reported Mental and Physical Health Symptoms and Potentially Traumatic Events among Lesbian, Gay, Bisexual, Transgender, and Queer Individuals: The Role of Shame. Psychology of Violence 10: 131–42. [Google Scholar] [CrossRef]
- Schmitz, Rachel M., Brandon Andrew Robinson, Jennifer Tabler, Brett Welch, and Sidra Rafaqut. 2020. LGBTQ+ Latino/a Young People’s Interpretations of Stigma and Mental Health: An Intersectional Minority Stress Perspective. Society and Mental Health 10: 163–79. [Google Scholar] [CrossRef]
- Seabra, Daniel, Jorge Gato, Nicola Petrocchi, and Maria do Céu Salvador. 2021. Minority Stress Model and Shame: The Moderating Role of Social Support. Paper presented at EABCT: Annual Congress 2021, Belfast, Ireland, September 8–11; Available online: https://www.researchgate.net/publication/355184660_Minority_Stress_Model_and_Shame_The_moderating_role_of_social_support (accessed on 22 October 2022).
- Singh, Anneliese A., Sarah Meng, and Anthony Hansen. 2013. “It’s Already Hard Enough Being a Student”: Developing Affirming College Environments for Trans Youth. Journal of LGBT Youth 10: 208–23. [Google Scholar] [CrossRef]
- Smart, Benjamin D., Lilli Mann-Jackson, Jorge Alonzo, Amanda E. Tanner, Manuel Garcia, Lucero Refugio Aviles, and Scott D. Rhodes. 2022. Transgender women of color in the U.S. South: A qualitative study of social determinants of health and healthcare perspectives. International Journal of Transgender Health 23: 164–77. [Google Scholar] [CrossRef]
- Stotzer, Rebecca L., Lana Sue I. Ka’opua, and Tressa P. Diaz. 2014. Is Healthcare Caring in Hawaii? Preliminary Results from a Health Assessment of Lesbian, Gay, Bisexual, Transgender, Questioning, and Intersex People in Four Counties. Hawaii Journal of Medicine & Public Health 73: 175–80. [Google Scholar]
- Straub, Kelsey T., Amy A. McConnell, and Terri L. Messman-Moore. 2018. Internalized Heterosexism and Posttraumatic Stress Disorder Symptoms: The Mediating Role of Shame Proneness among Trauma-Exposed Sexual Minority Women. Psychology of Sexual Orientation and Gender Diversity 5: 99–108. [Google Scholar] [CrossRef]
- Tangney, June Price, Jeff Stuewig, and Debra J. Mashek. 2007. Moral emotions and moral behavior. Annual Review of Psychology 58: 345–72. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Shelley E. 2012. Social support: A review. In The Oxford Handbook of Health Psychology. Oxford: Oxford University Press, vol. 1, pp. 189–214. [Google Scholar] [CrossRef]
- Timmins, Liadh, Katharine A. Rimes, and Qazi Rahman. 2020. Minority Stressors, Rumination, and Psychological Distress in Lesbian, Gay, and Bisexual Individuals. Archives of Sexual Behavior 49: 661–80. [Google Scholar] [CrossRef] [PubMed]
- Van Beusekom, Gabriël, Henny Mw Bos, Lisette Kuyper, Geertjan Overbeek, and Theo Gm Sandfort. 2018. Gender Nonconformity and Mental Health among Lesbian, Gay, and Bisexual Adults: Homophobic Stigmatization and Internalized Homophobia as Mediators. Journal of Health Psychology 23: 1211–22. [Google Scholar] [CrossRef]
- Vandello, Joseph A., and Jennifer K. Bosson. 2013. Hard won and easily lost: A review and synthesis of theory and research on precarious manhood. Psychology of Men & Masculinity 14: 101. [Google Scholar] [CrossRef]
- Veale, Jaimie F., Elizabeth M. Saewyc, Hélène Frohard-Dourlent, Sarah Dobson, and Beth Clark. 2015. Being Safe, Being Me: Results of the Canadian Trans Youth Health Survey Stigma and Resilience among Vulnerable Youth Centre. Available online: http://apscsaravyc.sites.olt.ubc.ca/files/2018/03/SARAVYC_Trans-Youth-Health-Report_EN_Final_Web2.pdf (accessed on 22 October 2022).
- Veale, Jaimie F., Ryan J. Watson, Tracey Peter, and Elizabeth M. Saewyc. 2017. Mental Health Disparities among Canadian Transgender Youth. The Journal of Adolescent Health 60: 44–49. [Google Scholar] [CrossRef] [PubMed]
- Walters, Mark A., Jennifer Paterson, Rupert Brown, and Liz McDonnell. 2020. Hate Crimes against Trans People: Assessing Emotions, Behaviors, and Attitudes toward Criminal Justice Agencies. Journal of Interpersonal Violence 35: 4583–613. [Google Scholar] [CrossRef]
- Watson, Ryan J., Arnold H. Grossman, and Stephen T. Russell. 2019a. Sources of Social Support and Mental Health among LGB Youth. Youth & Society 51: 30–48. [Google Scholar] [CrossRef]
- Watson, Ryan J., Jaimie F. Veale, Allegra R. Gordon, Beth A. Clark, and Elizabeth M. Saewyc. 2019b. Risk and Protective Factors for Transgender Youths’ Substance Use. Preventive Medicine Reports 15: 100905. [Google Scholar] [CrossRef] [PubMed]
- West, James. 2013. Rethinking Representations of Sexual and Gender-Based Violence: A Case Study of the Liberian Truth and Reconciliation Commission. Journal of International Women’s Studies 14: 109–23. Available online: https://vc.bridgew.edu/jiws/vol14/iss4/9 (accessed on 22 October 2022).
- Williams, A. Jess, Christopher Jones, Jon Arcelus, Ellen Townsend, Aikaterini Lazaridou, and Maria Michail. 2021. A Systematic Review and Meta-Analysis of Victimisation and Mental Health Prevalence among LGBTQ+ Young People with Experiences of Self-Harm and Suicide. PLoS ONE 16: e0245268. [Google Scholar] [CrossRef] [PubMed]
| % (N = 114) | ||
|---|---|---|
| Sexual orientation | LGBTQI+ | 48.2 |
| Heterosexual | 51.8 | |
| Gender | Female | 62.4 |
| Male | 34.9 | |
| Trans or non-binary | 2.7 | |
| Years of schooling | 6–9 | 13.3 |
| 10–12 | 32.5 | |
| >12 | 53.5 | |
| Monthly income | 250 €–500 € | 0.9 |
| 501 €–1000 € | 22.8 | |
| 1001 €–2000 € | 36.8 | |
| >2000 € | 24.6 | |
| Socioeconomic level | Low | 30.7 |
| Medium | 35.1 | |
| High | 0.9 | |
| Marital status | Single | 55.3 |
| Married/cohabiting/with partner | 40.3 | |
| Divorced | 4.4 | |
| Sexual Orientation | Gender | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LGBTQI+ (n = 48) | Heterosexual (n = 59) | Women (n = 68) | Men (n = 39) | ||||||||
| M | SD | M | SD | F | M | SD | M | SD | F | df | |
| Discrimination | 30.48 | 11.43 | 25.98 | 11.32 | 5.04 * | 27.43 | 10.22 | 29.00 | 13.61 | 0.56 | 3,103 |
| Depressive symptoms | 2.13 | 0.91 | 1.95 | 0.70 | 1.39 | 2.10 | 0.81 | 1.91 | 0.78 | 1.36 | 3,103 |
| Anxiety symptoms | 1.84 | 0.68 | 1.71 | 0.47 | 1.86 | 1.81 | 0.57 | 1.70 | 0.58 | 0.89 | 3,103 |
| Shame | 2.47 | 0.93 | 1.53 | 0.98 | 34.68 *** | 2.01 | 0.93 | 1.85 | 1.27 | 0.53 | 3,103 |
| Social support | 3.67 | 0.93 | 3.70 | 1.15 | 0.00 | 3.81 | 1.01 | 3.46 | 1.10 | 2.55 | 3,103 |
| (1) LGBTQI+ Women (n = 30) | (2) LGBTQI+ Men (n = 18) | (3) Heterosexual Women (n = 38) | (4) Heterosexual Men (n = 21) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | F | df | ||
| Discrimination | 28.87 | 10.51 | 33.17 | 12.67 | 26.29 | 9.98 | 25.43 | 13.66 | 0.26 | 3,103 | 1 = 2 = 3 = 4 |
| Depressive symptoms | 2.17 | 1.01 | 2.04 | 0.73 | 2.04 | 0.60 | 1.79 | 0.83 | 0.15 | 3,103 | 1 = 2 = 3 = 4 |
| Anxiety symptoms | 1.84 | 0.72 | 1.84 | 0.64 | 1.79 | 0.43 | 1.57 | 0.51 | 0.95 | 3,103 | 1 = 2 = 3 = 4 |
| Shame | 2.32 | 0.96 | 2.74 | 0.85 | 1.78 | 0.84 | 1.08 | 1.06 | 8.98 ** | 3,103 | 1, 2, 3 > 4; 2 < 3 > 4 |
| Social support | 3.77 | 0.93 | 3.50 | 0.93 | 3.84 | 1.08 | 3.42 | 1.26 | 0.13 | 3,103 | 1 = 2 = 3 = 4 |
| R (R2) | F | β | p | CI 95% | |
|---|---|---|---|---|---|
| Outcome variable—shame | 0.77 (0.59) | 15.19 *** | <0.001 | ||
| Discrimination | 0.25 *** | <0.001 | 0.02–0.08 | ||
| All (1) vs. heterosexual men (0) | 1.48 *** | <0.001 | 0.97–1.98 | ||
| Women (1) vs. men (0) | 0.76 *** | <0.001 | 0.32–1.19 | ||
| LGBTQI+ women (1) vs. all others (0) | 0.43 * | 0.017 | 0.08–0.78 | ||
| Social support | −0.25 ** | 0.001 | −0.40–−0.10 | ||
| Discrimination × all but heterosexual men | −0.04 † | 0.077 | −0.07–0.00 | ||
| Discrimination × women | 0.01 | 0.551 | −0.03–0.05 | ||
| Discrimination × LGBTQI+ women | 0.02 | 0.240 | −0.01–0.05 | ||
| Discrimination × social support | −0.00 | 0.562 | −0.01–0.01 | ||
| Discrimination × GxSO × social support | 1.52 | 0.203 | |||
| Outcome variable—depressive symptoms | 0.74 (0.54) | 11.07 *** | <0.001 | ||
| Discrimination | 0.01 | 0.241 | −0.01–0.04 | ||
| Shame | 0.31 *** | <0.001 | 0.15–0.48 | ||
| All (1) vs. heterosexual men (0) | −0.51 * | 0.035 | 0.04–0.97 | ||
| Women (1) vs. men (0) | 0.48 * | 0.010 | 0.12–0.85 | ||
| LGBTQI+ women (1) vs. all others (0) | −0.11 | 0.441 | −0.40–0.17 | ||
| Social support | −0.04 | 0.493 | −0.17–0.08 | ||
| Discrimination × all but heterosexual men | 0.02 | 0.284 | −0.01–0.05 | ||
| Discrimination × women | −0.02 | 0.205 | −0.05–0.01 | ||
| Discrimination × LGBTQI+ women | 0.04 ** | 0.006 | 0.01–0.07 | ||
| Discrimination × social support | −0.00 | 0.445 | −0.01–0.01 | ||
| Discrimination × GxSO × social support | 2.39 † | 0.056 | |||
| Outcome variable—anxiety symptoms | 0.65 (0.43) | 7.10 *** | <0.001 | ||
| Discrimination | 0.00 | 0.779 | −0.02–0.02 | ||
| Shame | 0.15 ** | 0.002 | 0.02–0.28 | ||
| All (1) vs. heterosexual men (0) | −0.13 | 0.490 | −0.51–0.25 | ||
| Women (1) vs. men (0) | 0.26 † | 0.088 | −0.04–0.55 | ||
| LGBTQI+ women (1) vs. all others (0) | −0.08 | 0.482 | −0.31–0.15 | ||
| Social support | −0.03 | 0.581 | −0.13–0.07 | ||
| Discrimination × all but heterosexual men | 0.03 * | 0.021 | 0.00–0.06 | ||
| Discrimination × women | −0.03 * | 0.016 | −0.05–−0.01 | ||
| Discrimination × LGBTQI+ women | 0.03 ** | 0.006 | 0.01–0.05 | ||
| Discrimination × social support | −0.01 † | 0.083 | −0.01–0.01 | ||
| Discrimination × GxSO × social support | 3.73 ** | 0.007 |
| Social Support | Effect | p | CI 95% | |
|---|---|---|---|---|
| Internal Shame | ||||
| Sexual orientation × gender | ||||
| Heterosexual men (1) | −0.69 | 0.054 *** | 0.0001 | 0.029–079 |
| Heterosexual men (1) | 0.31 | 0.051 ** | 0.001 | 0.021–0.080 |
| Heterosexual men (1) | 1.31 | 0.047 * | 0.013 | 0.010–0.084 |
| LGBTQI+ men (2) | −0.69 | 0.018 | 0.194 | −0.010–0.047 |
| LGBTQI+ men (2) | 0.31 | 0.015 | 0.268 | −0.012–0.043 |
| LGBTQI+ men (2) | 1.31 | 0.012 | 0.443 | −0.019–0.043 |
| Heterosexual women (3) | −0.69 | 0.030 * | 0.023 | 0.004–0.055 |
| Heterosexual women (3) | 0.31 | 0.026 * | 0.033 | 0.002–0.050 |
| Heterosexual women (3) | 1.31 | 0.023 | 0.106 | −0.005–0.051 |
| LGBTQI+ women (4) | −0.69 | 0.050 * | 0.001 | 0.023–0.078 |
| LGBTQI+ women (4) | 0.31 | 0.047 * | 0.001 | 0.021–0.073 |
| LGBTQI+ women (4) | 1.31 | 0.043 * | 0.004 | 0.014–0.073 |
| Depressive symptoms | ||||
| Sexual orientation × gender | ||||
| Heterosexual men (1) | −0.69 | 0.016 | 0.140 | −0.006–0.038 |
| Heterosexual men (1) | 0.31 | 0.013 | 0.306 | −0.012–0.038 |
| Heterosexual men (1) | 1.31 | 0.009 | 0.542 | −0.021–0.040 |
| LGBTQI+ men (2) | −0.69 | 0.034 * | 0.004 | 0.011–0.056 |
| LGBTQI+ men (2) | 0.31 | 0.030 * | 0.008 | 0.008–0.051 |
| LGBTQI+ men (2) | 1.31 | 0.026 * | 0.035 | 0.002–0.051 |
| Heterosexual women (3) | −0.69 | 0.015 | 0.158 | −0.006–0.036 |
| Heterosexual women (3) | 0.31 | 0.011 | 0.259 | −0.008–0.031 |
| Heterosexual women (3) | 1.31 | 0.008 | 0.488 | −0.015–0.030 |
| LGBTQI+ women (4) | −0.69 | 0.053 *** | <0.001 | 0.030–0.076 |
| LGBTQI+ women (4) | 0.31 | 0.050 *** | <0.001 | 0.028–0.071 |
| LGBTQI+ women (4) | 1.31 | 0.046 *** | <0.001 | 0.021–0.070 |
| Anxiety symptoms | ||||
| Sexual orientation × gender | ||||
| Heterosexual men (1) | −0.69 | 0.007 | 0.423 | −0.011–0.025 |
| Heterosexual men (1) | 0.31 | 0.001 | 0.949 | −0.019–0.021 |
| Heterosexual men (1) | 1.31 | −0.006 | 0.636 | −0.030–0.019 |
| LGBTQI+ men (2) | −0.69 | 0.037 *** | <0.001 | 0.019–0.056 |
| LGBTQI+ men (2) | 0.31 | 0.031 ** | 0.001 | 0.013–0.048 |
| LGBTQI+ men (2) | 1.31 | 0.024 * | 0.017 | 0.005–0.044 |
| Heterosexual women (3) | −0.69 | 0.009 | 0.314 | −0.008–0.025 |
| Heterosexual women (3) | 0.31 | 0.002 | 0.796 | −0.014–0.018 |
| Heterosexual women (3) | 1.31 | −0.004 | 0.628 | −0.023–0.014 |
| LGBTQI+ women (4) | −0.69 | 0.040 *** | <0.001 | 0.021–0.059 |
| LGBTQI+ women (4) | 0.31 | 0.034 *** | <0.001 | 0.016–0.051 |
| LGBTQI+ women (4) | 1.31 | 0.027 ** | 0.008 | 0.007–0.047 |
| Social Support | Effect | CI 95% | |
|---|---|---|---|
| Depressive symptoms | |||
| Sexual orientation × gender | |||
| Heterosexual men (1) | −0.69 | 0.02 | 0.01–0.03 |
| Heterosexual men (1) | 0.31 | 0.02 | 0.00–0.03 |
| Heterosexual men (1) | 1.31 | 0.01 | 0.00–0.03 |
| LGBTQI+ men (2) | −0.69 | 0.01 | −0.00–0.02 |
| LGBTQI+ men (2) | 0.31 | 0.01 | −0.00–0.02 |
| LGBTQI+ men (2) | 1.31 | 0.00 | −0.01–0.02 |
| Heterosexual women (3) | −0.69 | 0.01 | −0.00–0.02 |
| Heterosexual women (3) | 0.31 | 0.01 | −0.00–0.02 |
| Heterosexual women (3) | 1.31 | 0.01 | −0.00–0.02 |
| LGBTQI+ women (4) | −0.69 | 0.02 | 0.00–0.03 |
| LGBTQI+ women (4) | 0.31 | 0.01 | 0.00–0.03 |
| LGBTQI+ women (4) | 1.31 | 0.01 | 0.00–0.03 |
| Anxiety symptoms | |||
| Sexual orientation × gender | |||
| Heterosexual men (1) | −0.69 | 0.01 | 0.00–0.02 |
| Heterosexual men (1) | 0.31 | 0.01 | 0.00–0.02 |
| Heterosexual men (1) | 1.31 | 0.01 | 0.00–0.02 |
| LGBTQI+ men (2) | −0.69 | 0.00 | −0.00–0.01 |
| LGBTQI+ men (2) | 0.31 | 0.00 | −0.00–0.01 |
| LGBTQI+ men (2) | 1.31 | 0.00 | −0.00–0.01 |
| Heterosexual women (3) | −0.69 | 0.00 | −0.00–0.01 |
| Heterosexual women (3) | 0.31 | 0.00 | −0.00–0.01 |
| Heterosexual women (3) | 1.31 | 0.00 | −0.00–0.01 |
| LGBTQI+ women (4) | −0.69 | 0.01 | 0.00–0.02 |
| LGBTQI+ women (4) | 0.31 | 0.01 | 0.00–0.02 |
| LGBTQI+ women (4) | 1.31 | 0.01 | 0.00–0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabral, J.; Pinto, T.M. Gender, Shame, and Social Support in LGBTQI+ Exposed to Discrimination: A Model for Understanding the Impact on Mental Health. Soc. Sci. 2023, 12, 454. https://doi.org/10.3390/socsci12080454
Cabral J, Pinto TM. Gender, Shame, and Social Support in LGBTQI+ Exposed to Discrimination: A Model for Understanding the Impact on Mental Health. Social Sciences. 2023; 12(8):454. https://doi.org/10.3390/socsci12080454
Chicago/Turabian StyleCabral, Joana, and Tiago Miguel Pinto. 2023. "Gender, Shame, and Social Support in LGBTQI+ Exposed to Discrimination: A Model for Understanding the Impact on Mental Health" Social Sciences 12, no. 8: 454. https://doi.org/10.3390/socsci12080454
APA StyleCabral, J., & Pinto, T. M. (2023). Gender, Shame, and Social Support in LGBTQI+ Exposed to Discrimination: A Model for Understanding the Impact on Mental Health. Social Sciences, 12(8), 454. https://doi.org/10.3390/socsci12080454








