Contextualizing Maternal Education and Child Health in Sub-Saharan Africa: The Role of Intimate Partner Violence
Abstract
1. Introduction
1.1. Bronfenbrenner’s Person-Process-Context-Time Model
1.2. Maternal Education and Child Health
1.3. Intimate Partner Violence and Child Well-Being
1.4. Community-Level IPV and Child Well-Being
1.5. Importance of the Question
1.6. Current Study
2. Materials and Methods
2.1. Data
2.2. Variables
2.3. Analytic Strategy
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
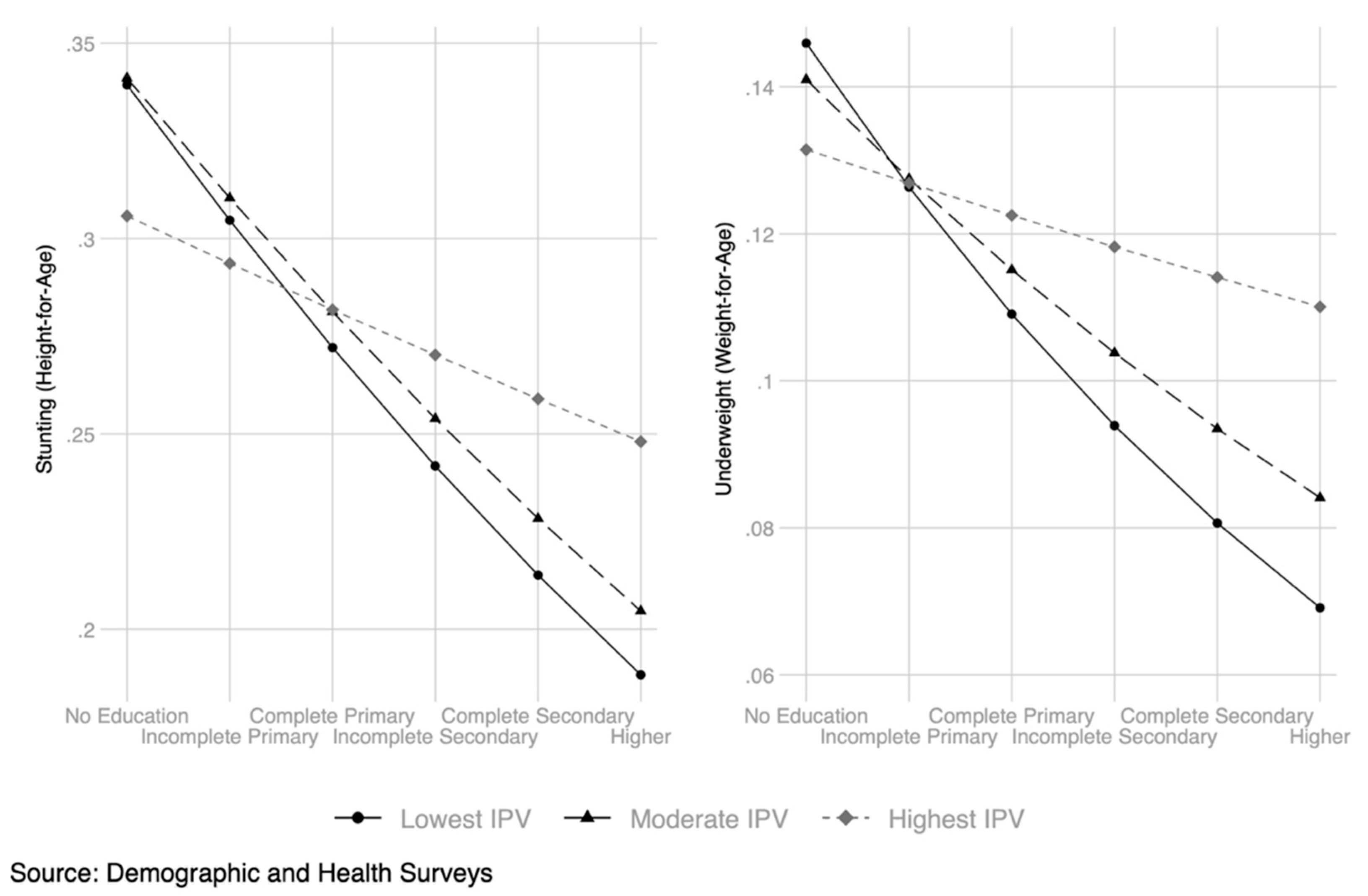
| 1 | Note that it is equally valid to say that Figure 2 shows how maternal education attenuates the link between IPV and child stunting and child underweight, respectively. |
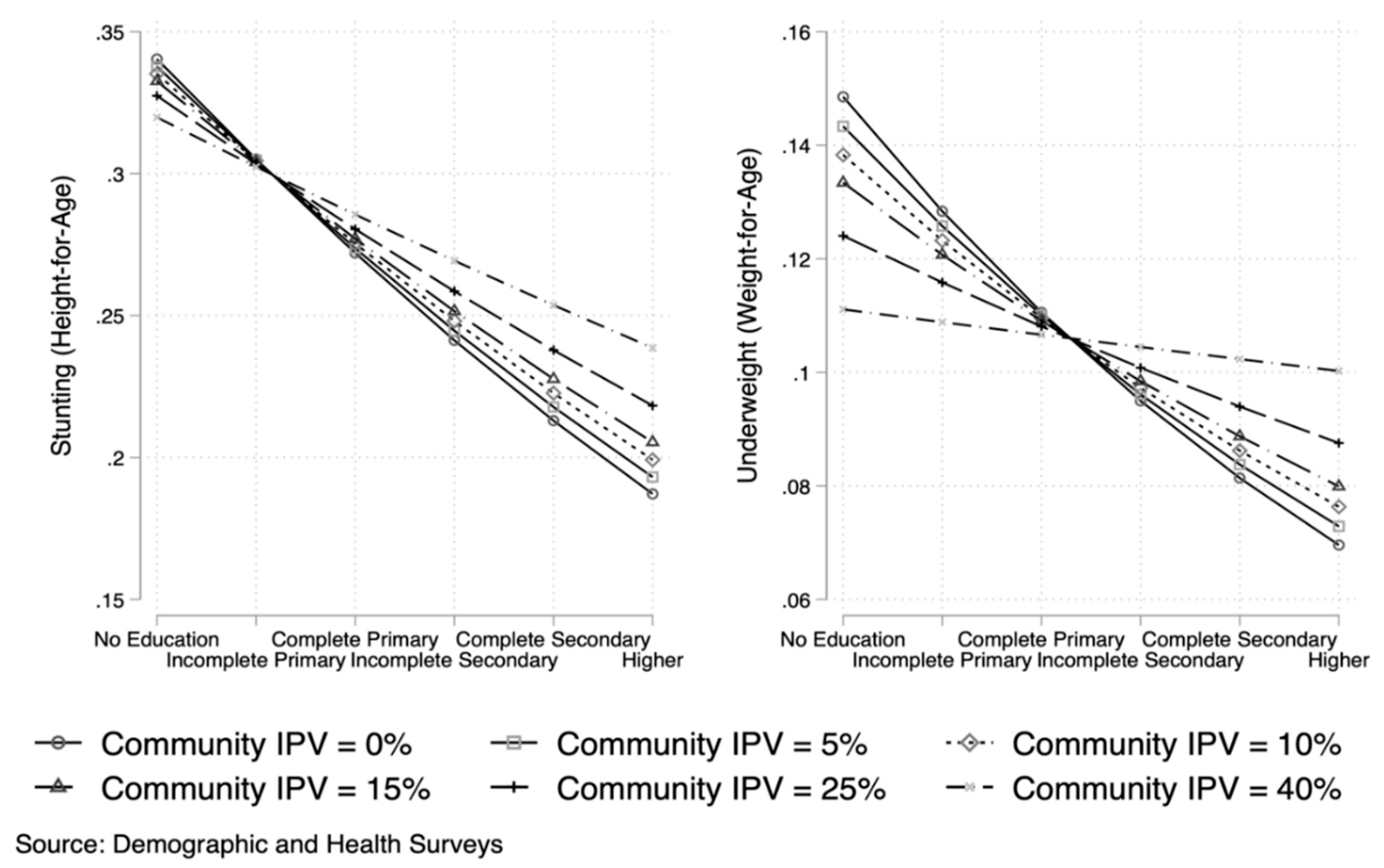
| 2 | These numbers correspond approximately to the 70th (70 percent of clusters had no women in the High IPV group), 75th, 80th, 90th, 95th, and 99th percentile of community IPV. |
References
- Acock, Alan C. 2005. Working With Missing Values. Journal of Marriage and Family 67: 1012–28. [Google Scholar] [CrossRef]
- Akombi, Blessing J., Kingsley E. Agho, John J. Hall, Nidhi Wali, Andre M. N. Renzaho, and Dafna Merom. 2017. Stunting, wasting and underweight in sub-Saharan Africa: A systematic review. International Journal of Environmental Research and Public Health 14: 863. [Google Scholar] [CrossRef]
- Anderson, Kristin L. 2005. Theorizing Gender in Intimate Partner Violence Research. Sex Roles 52: 853–65. [Google Scholar] [CrossRef]
- Bacchini, Dario, Maria Concetta Miranda, and Gaetana Affuso. 2011. Effects of Parental Monitoring and Exposure to Community Violence on Antisocial Behavior and Anxiety/Depression among Adolescents. Journal of Interpersonal Violence 26: 269–92. [Google Scholar] [CrossRef] [PubMed]
- Bacchus, Loraine J., Manuela Colombini, Manuel Contreras Urbina, Emma Howarth, Frances Gardner, Jeannie Annan, Kim Ashburn, Bernadette Madrid, Ruti Levtov, and Charlotte Watts. 2017. Exploring Opportunities for Coordinated Responses to Intimate Partner Violence and Child Maltreatment in Low and Middle Income Countries: A Scoping Review. Psychology, Health & Medicine 22: 135–65. [Google Scholar] [CrossRef]
- Barbarin, Oscar A., Linda Richter, and Thea DeWet. 2001. Exposure to violence, coping resources, and psychological adjustment of South African children. American Journal of Orthopsychiatry 71: 16–25. [Google Scholar] [CrossRef] [PubMed]
- Bedi, Gillinder, and Chris Goddard. 2007. Intimate partner violence: What are the impacts on children? Australian Psychologist 42: 66–77. [Google Scholar] [CrossRef]
- Bintabara, Deogratius, and Stephen M. Kibusi. 2018. Intimate Partner Violence Victimization Increases the Risk of Under-Five Morbidity: A Stratified Multilevel Analysis of Pooled Tanzania Demographic Health Surveys, 2010–2016. PLoS ONE 13: e0201814. [Google Scholar] [CrossRef]
- Bonomi, Amy E., Robert S. Thompson, Melissa Anderson, Robert J. Reid, David Carrell, Jane A. Dimer, and Frederick P. Rivara. 2006. Intimate partner violence and women’s physical, mental, and social functioning. American Journal of Preventive Medicine 30: 458–66. [Google Scholar] [CrossRef]
- Boynton-Jarrett, Renée, Jessica Fargnoli, Shakira Franco Suglia, Barry Zuckerman, and Rosalind J. Wright. 2010. Association between maternal intimate partner violence and incident obesity in preschool-aged children: Results from the Fragile Families and Child Well-being Study. Archives of Pediatrics & Adolescent Medicine 164: 540–46. [Google Scholar]
- Brody, Gene H., and Douglas L. Flor. 1998. Maternal resources, parenting practices, and child competence in rural, single-parent African American families. Child Development 69: 803–16. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, Urie. 1986a. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology 22: 723. [Google Scholar] [CrossRef]
- Bronfenbrenner, Urie. 1986b. Recent advances in research on the ecology of human development. Development as Action in Context, Springer International, 287–309. [Google Scholar]
- Bronfenbrenner, Urie, and Ann C. Crouter. 1983. Evolution of environmental models in developmental research. In Handbook of Child Psychology: Formerly Carmichael’s Manual of Child Psychology. Edited by Paul H. Mussen. New York: Wiley. [Google Scholar]
- Carlson, Karen Townsend. 2006. Poverty and youth violence exposure: Experiences in rural communities. Children & Schools 28: 87–96. [Google Scholar]
- Costanza, Robert, Lorenzo Fioramonti, and Ida Kubiszewski. 2016. The UN Sustainable Development Goals and the Dynamics of Well-Being. Frontiers in Ecology and the Environment 14: 59. [Google Scholar] [CrossRef]
- Cutts, Diana Becker, Alan F. Meyers, Maureen M. Black, Patrick H. Casey, Mariana Chilton, John T. Cook, Joni Geppert, Stephanie Ettinger de Cuba, Timothy Heeren, Sharon Coleman, and et al. 2011. US housing insecurity and the health of very young children. American Journal of Public Health 101: 1508–14. [Google Scholar] [CrossRef]
- Daelmans, Bernadette, Gary L. Darmstadt, Joan Lombardi, Maureen M. Black, Pia R. Britto, Stephen Lye, Tarun Dua, Zulfiqar A. Bhutta, and Linda M. Richter. 2017. Early Childhood Development: The Foundation of Sustainable Development. The Lancet 389: 9–11. [Google Scholar] [CrossRef]
- Desai, Sonalde, and Soumya Alva. 1998. Maternal Education and Child Health: Is There a Strong Causal Relationship? Demography 35: 71. [Google Scholar] [CrossRef]
- Dilnot, Julia, Lorna Hamilton, Barbara Maughan, and Margaret J. Snowling. 2017. Child and Environmental Risk Factors Predicting Readiness for Learning in Children at High Risk of Dyslexia. Development and Psychopathology 29: 235–44. [Google Scholar] [CrossRef]
- Dursun, Bahadir, Resul Cesur, and Inas Rashad Kelly. 2017. The Value of Mandating Maternal Education in A Developing Country. NBER Working Paper Series; Cambridge: National Bureau of Economic Research. [Google Scholar]
- Ellsberg, Mary, Henrica A. F. M. Jansen, Lori Heise, Charlotte H. Watts, and Claudia Garcia-Moreno. 2008. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: An observational study. The Lancet 371: 1165–72. [Google Scholar] [CrossRef] [PubMed]
- Emina, Jacques Be-Ofuriyua, Ngianga-Bakwin Kandala, Joseph Inungu, and Y. Yazoume. 2011. Maternal Education and Child Nutritional Status in the Democratic Republic of Congo. Journal of Public Health and Epidemiology 3: 576–92. [Google Scholar] [CrossRef]
- Ettinger, Adrienne S. 2004. Children’s Health, the Nation’s Wealth: Assessing and Improving Child Health. Washington, DC: The National Academis Press. [Google Scholar] [CrossRef]
- Ewerling, Fernanda, John W. Lynch, Cesar G. Victora, Anouka van Eerdewijk, Marcelo Tyszler, and Aluisio J.D. Barros. 2017. The SWPER Index for Women’s Empowerment in Africa: Development and Validation of an Index Based on Survey Data. The Lancet Global Health 5: e916–23. [Google Scholar] [CrossRef] [PubMed]
- Fagan, Abigail A., and Emily M. Wright. 2011. Gender differences in the effects of exposure to intimate partner violence on adolescent violence and drug use. Child Abuse & Neglect 35: 543–50. [Google Scholar]
- Fang, Xiangming, and Phaedra S. Corso. 2008. Gender differences in the connections between violence experienced as a child and perpetration of intimate partner violence in young adulthood. Journal of Family Violence 23: 303–13. [Google Scholar] [CrossRef]
- Gakidou, Emmanuela, Krycia Cowling, Rafael Lozano, and Christopher Jl Murray. 2010. Increased Educational Attainment and Its Effect on Child Mortality in 175 Countries between 1970 and 2009: A Systematic Analysis. The Lancet 376: 959–74. [Google Scholar] [CrossRef]
- Gass, Jesse D., Dan J. Stein, David R. Williams, and Soraya Seedat. 2011. Gender differences in risk for intimate partner violence among South African adults. Journal of Interpersonal Violence 26: 2764–89. [Google Scholar] [CrossRef]
- Gibson-Davis, Christina, and Heather Rackin. 2014. Marriage or Carriage? Trends in Union Context and Birth Type by Education. Journal of Marriage and Family 76: 506–19. [Google Scholar] [CrossRef]
- Glinski, Allison, Chloe Schwenke, Lila O’Brien-Milne, and Kathryn Farley. 2018. Gender Equity and Male Engagement: It Only Works When Everyone Plays. Washington, DC: ICRW. [Google Scholar]
- Graham-Bermann, Sandra A., Kathryn H. Howell, Laura E. Miller, Jean Kwek, and Michelle M. Lilly. 2010. Traumatic Events and Maternal Education as Predictors of Verbal Ability for Preschool Children Exposed to Intimate Partner Violence (IPV). Journal of Family Violence 25: 383–92. [Google Scholar] [CrossRef]
- Gratz, Kim L., Autumn Paulson, Matthew Jakupcak, and Matthew T. Tull. 2009. Exploring the relationship between childhood maltreatment and intimate partner abuse: Gender differences in the mediating role of emotion dysregulation. Violence and Victims 24: 68–82. [Google Scholar] [CrossRef]
- Grépin, Karen A., and Prashant Bharadwaj. 2015. Maternal Education and Child Mortality in Zimbabwe. Journal of Health Economics 44: 97–117. [Google Scholar] [CrossRef]
- Guerrero, Natalie, Kevin M. Wagner, Ronald Gangnon, Carmen R. Valdez, Marah A. Curtis, Deborah B. Ehrenthal, and Elizabeth A. Jacobs. 2020. Food insecurity and housing instability partially mediate the association between maternal depression and child problem behavior. The Journal of Primary Prevention 41: 245–59. [Google Scholar] [CrossRef] [PubMed]
- Güneş, Pinar Mine. 2015. The Role of Maternal Education in Child Health: Evidence from a Compulsory Schooling Law. Economics of Education Review 47: 1–16. [Google Scholar] [CrossRef]
- James, Spencer L. 2015. Variation in Trajectories of Women’s Marital Quality. Social Science Research 49: 16–30. [Google Scholar] [CrossRef]
- Johnson, David R., and Rebekah Young. 2011. Toward Best Practices in Analyzing Datasets with Missing Data: Comparisons and Recommendations. Journal of Marriage and Family 73: 926–45. [Google Scholar] [CrossRef]
- Kan, Janice M., Caitlin S.M. Cowan, Chee Y. Ooi, and Nadine A. Kasparian. 2019. What Can the Gut Microbiome Teach Us about the Connections between Child Physical and Mental Health? A Systematic Review. Developmental Psychobiology 61: 700–713. [Google Scholar] [CrossRef] [PubMed]
- Keeley, Brian, Céline Little, Juliano Diniz de Oliveira, Eric Zuehlke, Gregory Sclama, Kasper Vrolijk, Upasana Young, Dawit Ghebremichael, and David Anthony. 2019. The State of the World’s Children: Children, Food, and Nutrition. Available online: https://www.unicef.org/media/63016/file/SOWC-2019.pdf (accessed on 8 June 2022).
- Kelly, Joan B., and Michael E. Lamb. 2003. Developmental issues in relocation cases involving young children: When, whether, and how? Journal of Family Psychology 17: 193. [Google Scholar] [CrossRef]
- Lamers-Winkelman, Francien, J. Clasien De Schipper, and Mirjam Oosterman. 2012. Children’s physical health complaints after exposure to intimate partner violence. British Journal of Health Psychology 17: 771–84. [Google Scholar] [CrossRef]
- Le Blanc, David. 2015. Towards Integration at Last? The Sustainable Development Goals as a Network of Targets. Sustainable Development 23: 176–87. [Google Scholar] [CrossRef]
- Martorell, Reynaldo. 2017. Improved Nutrition in the First 1000 Days and Adult Human Capital and Health. American Journal of Human Biology 29: 1–12. [Google Scholar] [CrossRef]
- Matysiak, Anna, Marta Styrc, and Daniele Vignoli. 2014. The educational gradient in marital disruption: A meta-analysis of European research findings. Population Studies 68: 197–215. [Google Scholar] [CrossRef] [PubMed]
- McGowan, Philip J. K., Gavin B. Stewart, Graham Long, and Matthew J. Grainger. 2019. An Imperfect Vision of Indivisibility in the Sustainable Development Goals. Nature Sustainability 2: 43–45. [Google Scholar] [CrossRef]
- Miranda, Jenniffer K., Nuria de la Osa, Roser Granero, and Lourdes Ezpeleta. 2013. Maternal childhood abuse, intimate partner violence, and child psychopathology: The mediator role of mothers’ mental health. Violence against Women 19: 50–68. [Google Scholar] [CrossRef] [PubMed]
- Mondal, Dinabandhu, and Pintu Paul. 2020. Association between intimate partner violence and child nutrition in India: Findings from recent National Family Health Survey. Children and Youth Services Review 119: 105493. [Google Scholar] [CrossRef]
- Muluneh, Muluken Dessalegn, Virginia Stulz, Lyn Francis, and Kingsley Agho. 2020. Gender Based Violence against Women in Sub-Saharan Africa: A Systematic Review and Meta-Analysis of Cross-Sectional Studies. International Journal of Environmental Research and Public Health 17: 903. [Google Scholar] [CrossRef]
- Nagin, Daniel S., and Richard E. Tremblay. 2005. The ANNALS of the American Academy of Political and Social Science Modeling and Analyzing Developmental A Response to Maughan and Raudenbush. The Annals of the American Academy of Political and Social Science 602: 145–54. [Google Scholar] [CrossRef]
- Njue, Jane Rose, Dorothy Rombo, Laura S. Smart, Anne N. Lutomia, and Lucy Wandiri Mbirianjau. 2014. Domestic Violence in Kenya: Strengths-Based Research. In Family Violence from a Global Perspective: A Strengths-Based Approach. New York: SAGE Publications, pp. 29–50. [Google Scholar] [CrossRef]
- Noonan, Clare Bridget, and Pamela Doreen Pilkington. 2020. Intimate partner violence and child attachment: A systematic review and meta-analysis. Child Abuse & Neglect 109: 104765. [Google Scholar]
- Nylund, Karen L., Tihomir Asparouhov, and Bengt O. Muthén. 2007. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling 14: 535–69. [Google Scholar] [CrossRef]
- Nylund-Gibson, Karen, and Andrew Young Choi. 2018. Ten Frequently Asked Questions about Latent Class Analysis. Translational Issues in Psychological Science 4: 440–61. [Google Scholar] [CrossRef]
- Ononokpono, Dorothy Ngozi, and Ezinwanne Christiana Azfredrick. 2014. Intimate partner violence and the utilization of maternal health care services in Nigeria. Health Care for Women International 35: 973–89. [Google Scholar] [CrossRef]
- Organization for African Unity. 1990. African Charter on the Rights and Welfare of the Child. Addis Ababa: Organization for African Unity. [Google Scholar]
- Owen, Ashley E., Martie P. Thompson, Anne Shaffer, Emily B. Jackson, and Nadine J. Kaslow. 2009. Family variables that mediate the relation between intimate partner violence (IPV) and child adjustment. Journal of Family Violence 24: 433–45. [Google Scholar] [CrossRef]
- Pamuk, Elsie R., Regina Fuchs, and Wolfgang Lutz. 2011. Comparing Relative Effects of Education and Economic Resources on Infant Mortality in Developing Countries. Population and Development Review 37: 637–64. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, Martin, and Yuhui Shen. 2011. Behavior Problems in Children and Adolescents with Chronic Physical Illness: A Meta-Analysis. Journal of Pediatric Psychology 36: 1003–16. [Google Scholar] [CrossRef] [PubMed]
- Prickett, Kate C., and Jennifer March Augustine. 2016. Maternal Education and Investments in Children’s Health. Journal of Marriage and Family 78: 7–25. [Google Scholar] [CrossRef] [PubMed]
- Proctor, Laura J. 2006. Children Growing up in a Violent Community: The Role of the Family. Aggression and Violent Behavior 11: 558–76. [Google Scholar] [CrossRef]
- Protano, Carmela, Federica Valeriani, Alessandro Macedonio, Flavia Cammarota, Vincenzo Romano Spica, Giovanni Battista Orsi, and Matteo Vitali. 2017. Family-based social determinants and child health: Cross-sectional study. Pediatrics International 59: 201–8. [Google Scholar] [CrossRef]
- Rico, Emily, Bridget Fenn, Tanya Abramsky, and Charlotte Watts. 2011. Associations between maternal experiences of intimate partner violence and child nutrition and mortality: Findings from Demographic and Health Surveys in Egypt, Honduras, Kenya, Malawi and Rwanda. Journal of Epidemiology & Community Health 65: 360–67. [Google Scholar]
- Sampson, Robert J. 2003. The Neighborhood Context of Well-Being. Perspectives in Biology and Medicine 46: S53–S64. [Google Scholar] [CrossRef]
- Sanville, Julie, Annie Gjelsvik, and Patrick Vivier. 2019. Assessing the Association Between Maternal Education and Access to Pediatric Specialty Care. Clinical Pediatrics 58: 1478–83. [Google Scholar] [CrossRef]
- Sardinha, Lynn Marie, and Héctor E. Nájera Catalán. 2018. Attitudes towards Domestic Violence in 49 Low- and Middle-Income Countries: A Gendered Analysis of Prevalence and Countrylevel Correlates. PLoS ONE 13: e0206101. [Google Scholar] [CrossRef]
- Sardinha, Lynnmarie, Mathieu Maheu-Giroux, Heidi Stöckl, Sarah Rachel Meyer, and Claudia García-Moreno. 2022. Global, regional, and national prevalence estimates of physical or sexual, or both, intimate partner violence against women in 2018. The Lancet 399: 803–13. [Google Scholar] [CrossRef] [PubMed]
- Shay-Zapien, Gina, and Linda Bullock. 2010. Impact of intimate partner violence on maternal child health. MCN: The American Journal of Maternal/Child Nursing 35: 206–12. [Google Scholar] [CrossRef] [PubMed]
- Smith-Greenaway, Emily. 2017. Community context and child health: A human capital perspective. Journal of Health and Social Behavior 58: 307–21. [Google Scholar] [CrossRef]
- Smith-Greenaway, Emily. 2020. Does Parents’ Union Instability Disrupt Intergenerational Advantage? An Analysis of Sub-Saharan Africa. Demography 57: 445–73. [Google Scholar] [CrossRef]
- Thurstans, Susan, Charles Opondo, Andrew Seal, Jonathan Wells, Tanya Khara, Carmel Dolan, André Briend, Mark Myatt, Michel Garenne, Rebecca Sear, and et al. 2020. Boys are more likely to be undernourished than girls: A systematic review and meta-analysis of sex differences in undernutrition. BMJ Global Health 5: e004030. [Google Scholar] [CrossRef] [PubMed]
- UN General Assembly. 1989. Convention on the Rights of a Child. United Nations, Treaty Series 1577: 1–15. [Google Scholar] [CrossRef]
- United Nations. 2016. The Sustainable Development Goals Report 2016. Available online: https://doi.org/10.29171/azu_acku_pamphlet_k3240_s878_2016 (accessed on 13 June 2022).
- United Nations Department of Economic and Social Affairs. 2020. World Fertility and Family Planning 2020: Highlights. Available online: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2020_worldfertilityfamilyplanning_highlights.pdf (accessed on 15 October 2020).
- Uthman, Olalekan A., Evanson Z. Sambala, Abdu A. Adamu, Duduzile Ndwandwe, Alison B. Wiyeh, Tawa Olukade, Ghose Bishwajit, Sanni Yaya, Jean-Marie Okwo-Bele, and Charles S. Wiysonge. 2018. Does it really matter where you live? A multilevel analysis of factors associated with missed opportunities for vaccination in sub-Saharan Africa. Human Vaccines & Immunotherapeutics 14: 2397–404. [Google Scholar]
- VanderEnde, Kristin E., Kathryn M. Yount, Michelle M. Dynes, and Lynn M. Sibley. 2012. Community-level correlates of intimate partner violence against women globally: A systematic review. Social Science and Medicine 75: 1143–55. [Google Scholar] [CrossRef] [PubMed]
- Wamani, Henry, Thorkild Tylleskär, Anne Nordrehaug Åstrøm, James K. Tumwine, and Stefan Peterson. 2004. Mothers’ education but not fathers’ education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. International Journal for Equity in Health 3: 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wolde, Mekides, Yifru Berhan, and Alemzewed Chala. 2015. Determinants of underweight, stunting and wasting among schoolchildren. BMC Public Health 15: 1–9. [Google Scholar] [CrossRef]
- Wood, Samantha L., and Marilyn S. Sommers. 2011. Consequences of intimate partner violence on child witnesses: A systematic review of the literature. Journal of Child and Adolescent Psychiatric Nursing 24: 223–36. [Google Scholar] [CrossRef] [PubMed]
- Woszidlo, Alesia, and Chris Segrin. 2013. Negative affectivity and educational attainment as predictors of newlyweds’ problem solving communication and marital quality. The Journal of Psychology 147: 49–73. [Google Scholar] [CrossRef]
- Wu, Hanbo. 2022. The Effect of Maternal Education on Child Mortality in Bangladesh. Population and Development Review 8: 475–503. [Google Scholar] [CrossRef]
- Zhang, Saijun, and Steven G. Anderson. 2010. Low-Income Single Mothers’ Community Violence Exposure and Aggressive Parenting Practices. Children and Youth Services Review 32: 889–95. [Google Scholar] [CrossRef]
- Ziaei, Shirin, Ruchira Tabassum Naved, and Eva Charlotte Ekström. 2014. Women’s Exposure to Intimate Partner Violence and Child Malnutrition: Findings from Demographic and Health Surveys in Bangladesh. Maternal and Child Nutrition 10: 347–59. [Google Scholar] [CrossRef]

| # Sample Size | Stunting | Wasting (0–1) | Underweight | |
|---|---|---|---|---|
| (0–1) | (0–1) | |||
| Angola 7 | 8236 | 0.18 | 0.03 | 0.09 |
| Burkina Faso 6 | 9715 | 0.17 | 0.08 | 0.13 |
| Benin 7 | 4498 | 0.29 | 0.05 | 0.16 |
| Burundi 7 | 7771 | 0.20 | 0.02 | 0.10 |
| Cote d’Ivoire 6 | 4240 | 0.14 | 0.04 | 0.07 |
| Cameroon 7 | 4064 | 0.20 | 0.03 | 0.08 |
| Ethiopia 7 | 3996 | 0.37 | 0.10 | 0.23 |
| Gabon 6 | 2905 | 0.10 | 0.02 | 0.04 |
| Ghana 5 | 1364 | 0.23 | 0.08 | 0.12 |
| The Gambia 6 | 3490 | 0.09 | 0.04 | 0.06 |
| Kenya 6 | 3539 | 0.25 | 0.04 | 0.11 |
| Comoros 6 | 2171 | 0.25 | 0.09 | 0.13 |
| Liberia 5 | 3114 | 0.34 | 0.06 | 0.16 |
| Mali 7 | 3531 | 0.25 | 0.09 | 0.17 |
| Malawi 7 | 4073 | 0.35 | 0.03 | 0.11 |
| Mozambique 6 | 4693 | 0.41 | 0.06 | 0.15 |
| Nigeria 7 | 8872 | 0.36 | 0.07 | 0.22 |
| Senegal 7 | 2349 | 0.16 | 0.09 | 0.14 |
| Sao Tome and | 1362 | 0.21 | 0.08 | 0.10 |
| Principe 5 | ||||
| Togo 6 | 4708 | 0.13 | 0.03 | 0.08 |
| Tanzania 7 | 6458 | 0.33 | 0.05 | 0.13 |
| South Africa 7 | 865 | 0.08 | 0.01 | 0.01 |
| Zambia 7 | 6060 | 0.33 | 0.05 | 0.11 |
| Zimbabwe 7 | 3846 | 0.25 | 0.03 | 0.07 |
| Total | 105,920 | 0.25 | 0.05 | 0.12 |
| Maternal | Low IPV | Moderate IPV | High IPV | |
| Education (0–5) | (0–1) | (0–1) | (0–1) | |
| Angola 7 | 1.43 | 0.82 | 0.13 | 0.05 |
| Burkina Faso 6 | 0.28 | 0.95 | 0.04 | 0.01 |
| Benin 7 | 0.67 | 0.88 | 0.09 | 0.03 |
| Burundi 7 | 0.91 | 0.76 | 0.19 | 0.05 |
| Cote d’Ivoire 6 | 0.59 | 0.84 | 0.12 | 0.04 |
| Cameroon 7 | 1.71 | 0.78 | 0.17 | 0.05 |
| Ethiopia 7 | 0.56 | 0.86 | 0.10 | 0.04 |
| Gabon 6 | 2.40 | 0.69 | 0.22 | 0.10 |
| Ghana 5 | 1.69 | 0.89 | 0.10 | 0.02 |
| The Gambia 6 | 1.00 | 0.90 | 0.09 | 0.01 |
| Kenya 6 | 1.98 | 0.77 | 0.18 | 0.05 |
| Comoros 6 | 1.32 | 0.97 | 0.02 | 0.01 |
| Liberia 5 | 0.80 | 0.75 | 0.19 | 0.06 |
| Mali 7 | 0.61 | 0.80 | 0.17 | 0.03 |
| Malawi 7 | 1.45 | 0.86 | 0.11 | 0.03 |
| Mozambique 6 | 0.90 | 0.81 | 0.16 | 0.03 |
| Nigeria 7 | 2.00 | 0.90 | 0.08 | 0.02 |
| Senegal 7 | 0.65 | 0.91 | 0.07 | 0.02 |
| Sao Tome and | 1.60 | 0.81 | 0.12 | 0.06 |
| Principe 5 | ||||
| Togo 6 | 1.15 | 0.86 | 0.12 | 0.02 |
| Tanzania 7 | 1.65 | 0.76 | 0.19 | 0.06 |
| South Africa 7 | 3.41 | 0.88 | 0.10 | 0.02 |
| Zambia 7 | 1.95 | 0.79 | 0.16 | 0.05 |
| Zimbabwe 7 | 2.67 | 0.86 | 0.12 | 0.03 |
| Total | 1.27 | 0.84 | 0.13 | 0.03 |
| Log Likelihood | AIC | BIC | Adjusted BIC | Entropy | VLMR LRT | LMR adj. LRT | Small Classes? | |
|---|---|---|---|---|---|---|---|---|
| 2-class | −593,124.67 | 1,186,287.34 | 1,186,489.75 | 1,186,429.37 | 0.899 | 0 | 0 | N |
| 3-class | −578,766.93 | 1,157,591.86 | 1,157,900.80 | 1,157,808.64 | 0.852 | 0 | 0 | N |
| 4-class | −574,483.98 | 1,149,045.95 | 1,149,461.42 | 1,149,337.48 | 0.867 | 0 | 0 | Y |
| 5-class | −572,719.05 | 1,145,536.11 | 1,146,058.11 | 1,145,902.38 | 0.864 | 0 | 0 | Y |
| 6-class | −571,608.52 | 1,143,335.03 | 1,143,963.56 | 1,143,776.06 | 0.858 | 0 | 0 | Y |
| 7-class | −571,163.88 | 1,142,465.76 | 1,143,200.82 | 1,142,981.54 | 0.855 | 0 | 0 | Y |
| Stunting | Wasting | Underweight | ||||
|---|---|---|---|---|---|---|
| Individual | Community | Individual | Community | Individual | Community | |
| Maternal Education | −0.16 *** (0.01) | −0.16 *** (0.01) | −0.10 *** (0.03) | −0.10 *** (0.03) | −0.17 *** (0.02) | −0.17 *** (0.02) |
| Lowest IPV | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) |
| Moderate IPV | 0.01 (0.04) | 0.03 (0.03) | −0.09 (0.08) | −0.04 (0.06) | −0.04 (0.05) | 0.02 (0.04) |
| Highest IPV | −0.15 * (0.08) | −0.04 (0.06) | −0.18 (0.15) | −0.08 (0.12) | −0.12 (0.10) | 0.08 (0.07) |
| Lowest IPV * Maternal Education | 0.00 (.) | 0.00 (.) | 0.00 (.) | |||
| Moderate IPV * Maternal Education | 0.02 (0.02) | 0.04 (0.05) | 0.05 (0.03) | |||
| Highest IPV * Maternal Education | 0.10 * (0.04) | 0.01 (0.11) | 0.13 * (0.06) | |||
| Community IPV | −0.23 (0.19) | −0.78 * (0.37) | −0.83 *** (0.24) | |||
| Maternal Education * Community IPV | 0.20 * (0.09) | 0.24 (0.18) | 0.37 ** (0.12) | |||
| Child Age | 1.40 *** (0.06) | 1.40 *** (0.06) | 0.29 ** (0.10) | 0.28 ** (0.10) | 0.69 *** (0.07) | 0.69 *** (0.07) |
| Child Age * Child Age | −0.53 *** (0.04) | −0.53 *** (0.04) | −0.46 *** (0.07) | −0.45 *** (0.07) | −0.34 *** (0.04) | −0.34 *** (0.04) |
| Child Age * Child Age * Child Age | 0.06 *** (0.01) | 0.06 *** (0.01) | 0.08 *** (0.01) | 0.08 *** (0.01) | 0.05 *** (0.01) | 0.04 *** (0.01) |
| Child is Male | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) |
| Child is Female | −0.21 *** (0.02) | −0.21 *** (0.02) | −0.21 *** (0.04) | −0.21 *** (0.04) | −0.19 *** (0.03) | −0.19 *** (0.03) |
| Household Wealth Index | −0.17 *** (0.01) | −0.17 *** (0.01) | −0.10 *** (0.02) | −0.11 *** (0.02) | −0.19 *** (0.01) | −0.19 *** (0.01) |
| Urban | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) |
| Rural | 0.10 ** (0.03) | 0.10 ** (0.03) | −0.10 (0.06) | −0.11 (0.06) | 0.04 (0.04) | 0.03 (0.04) |
| Living with Partner | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) | 0.00 (.) |
| Married | 0.02 (0.03) | 0.02 (0.03) | 0.07 (0.07) | 0.07 (0.07) | −0.04 (0.04) | −0.04 (0.04) |
| Maternal Age @1st Union | −0.01 * (0.01) | −0.01 * (0.01) | −0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) | 0.00 (0.01) |
| Year | 0.02 (0.04) | 0.02 (0.04) | −0.02 (0.08) | −0.02 (0.08) | 0.04 (0.05) | 0.04 (0.05) |
| Maternal Age | −0.01 *** (0.00) | −0.01 *** (0.00) | 0.00 (0.00) | 0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Std autonomy SWPER score | −0.00 (0.03) | −0.00 (0.03) | 0.08 (0.05) | 0.08 (0.05) | −0.00 (0.04) | −0.00 (0.04) |
| Std attitude to violence SWPER score | −0.02 (0.01) | −0.02 (0.01) | −0.02 (0.02) | −0.02 (0.02) | −0.04 * (0.02) | −0.04 * (0.02) |
| Std decision making SWPER score | −0.02 (0.01) | −0.02 (0.01) | −0.04 (0.02) | −0.04 (0.02) | −0.04 * (0.02) | −0.04 * (0.02) |
| Child Immunizations | 0.01 (0.01) | 0.01 (0.01) | −0.03 ** (0.01) | −0.03 ** (0.01) | −0.01 * (0.01) | −0.01 * (0.01) |
| Child Had Diarrhea Past 2 Weeks | 0.16 *** (0.03) | 0.16 *** (0.03) | 0.30 *** (0.05) | 0.30 *** (0.05) | 0.29 *** (0.03) | 0.29 *** (0.03) |
| Child Had Acute Respiratory Infection Past 2 Weeks | 0.01 (0.02) | 0.01 (0.02) | −0.03 (0.03) | −0.03 (0.03) | 0.03 (0.02) | 0.03 (0.02) |
| Constant | −45.38 (82.56) | −45.72 (82.55) | 31.19 (156.78) | 38.47 (156.43) | −87.48 (110.57) | −81.31 (110.15) |
| Observations | 105,692 | 105,692 | 105,692 | 105,692 | 105,692 | 105,692 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
James, S.L.; Jorgensen Wells, M.A.; Larsen Gibby, A.; Njue, J.R.; Rarick, T.M.; Vogrinec, W.; Rautenbach, J.V. Contextualizing Maternal Education and Child Health in Sub-Saharan Africa: The Role of Intimate Partner Violence. Soc. Sci. 2023, 12, 324. https://doi.org/10.3390/socsci12060324
James SL, Jorgensen Wells MA, Larsen Gibby A, Njue JR, Rarick TM, Vogrinec W, Rautenbach JV. Contextualizing Maternal Education and Child Health in Sub-Saharan Africa: The Role of Intimate Partner Violence. Social Sciences. 2023; 12(6):324. https://doi.org/10.3390/socsci12060324
Chicago/Turabian StyleJames, Spencer L., Mckell A. Jorgensen Wells, Ashley Larsen Gibby, Jane Rose Njue, Timothy M. Rarick, Whitney Vogrinec, and John V. Rautenbach. 2023. "Contextualizing Maternal Education and Child Health in Sub-Saharan Africa: The Role of Intimate Partner Violence" Social Sciences 12, no. 6: 324. https://doi.org/10.3390/socsci12060324
APA StyleJames, S. L., Jorgensen Wells, M. A., Larsen Gibby, A., Njue, J. R., Rarick, T. M., Vogrinec, W., & Rautenbach, J. V. (2023). Contextualizing Maternal Education and Child Health in Sub-Saharan Africa: The Role of Intimate Partner Violence. Social Sciences, 12(6), 324. https://doi.org/10.3390/socsci12060324








