Childhood Adversity Moderates Change in Latent Patterns of Psychological Adjustment during the COVID-19 Pandemic: Results of a Survey of U.S. Adults
Abstract
1. Introduction
1.1. Stress Sensitization and Mental Health
1.2. The COVID-19 Pandemic as a Stressor
1.3. Person-Centered Approaches
1.4. Current Study
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Indicators of Mental Health
2.2.2. Childhood Adversity
2.2.3. Covariates
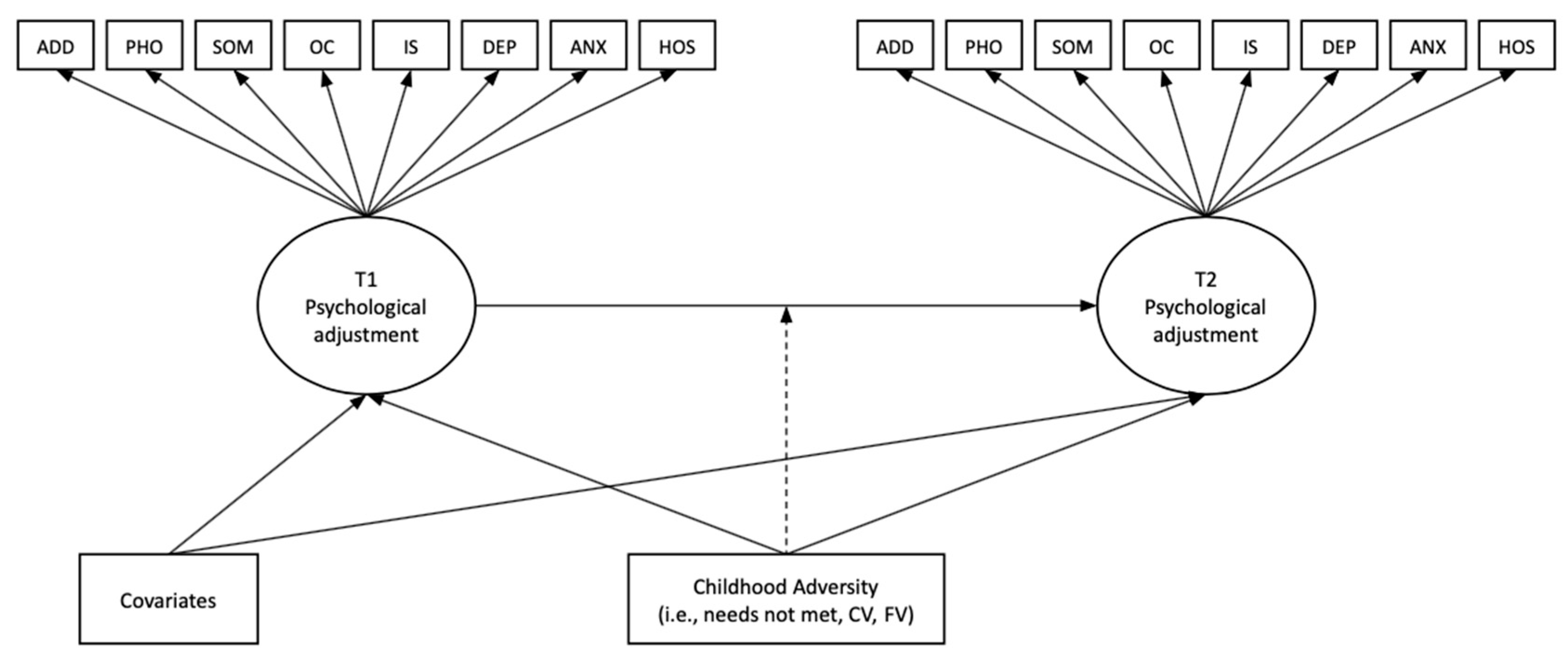
2.3. Analytic Plan
Latent Transition Analysis
3. Results
3.1. Descriptive Statistics
3.2. Latent Profile Analyses
3.3. Latent Transition Analysis
4. Discussion
4.1. Sociodemographic Characteristics and Adjustment
4.2. Childhood Adversity and Adjustment
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albott, C. Sophia, Miriam K. Forbes, and Justin J. Anker. 2018. Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Network Open 1: e185354. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, Jennifer W., Chuck W. Peek, and Barbara A. Zsembik. 2020. Examining U.S. pet ownership using the General Social Survey. The Social Science Journal 60: 1–10. [Google Scholar] [CrossRef]
- Bradley, Robert H., and Robert F. Corwyn. 2002. Socioeconomic status and child development. Annual Review of Psychology 53: 371–99. [Google Scholar] [CrossRef]
- Bridgland, Victoria M. E., Ella K. Moeck, Deanne M. Green, Tay;or L. Swain, Diane M. Nayda, Lucy A. Matson, Nadine P. Hutchison, and Melanie K. T. Takarangi. 2021. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 16: e0240146. [Google Scholar] [CrossRef] [PubMed]
- Busse, Heide, Christoph Buck, Christiane Stock, Hajo Zeeb, Claudia R. Pischke, Paula M. M. Fialho, Claus Wendt, and Stefanie M. Helmer. 2021. Engagement in health risk behaviours before and during the COVID-19 pandemic in German university students: Results of a cross-national study. International Journal of Environmental Research and Public Health 18: 1410. [Google Scholar] [CrossRef]
- Carvalho, Poliana, Marcial M. Moreira, Matheus N. A. de Oliveira, José M. M. Landim, and Modesto L. R. Neto. 2020. The psychiatric impact of the novel coronavirus outbreak. Psychiatry Research 286: 112902. [Google Scholar] [CrossRef] [PubMed]
- Chapman, Daniel P., Charles L. Whitfield, Vincent J. Felitti, Shanta R. Dube, Valerie J. Edwards, and Robert F. Anda. 2004. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders 82: 217–25. [Google Scholar] [CrossRef] [PubMed]
- Community Marketing & Insights. 2019. 13th Annual LGBTQ Community Survey: USA Summary Report. July. Available online: https://www.communitymarketinginc.com/documents/temp/CMI-13th_LGBTQ_Community_Survey_US_Profile.pdf (accessed on 12 June 2022).
- Crouch, Elizabeth, Janice C. Probst, Elizabeth Radcliff, Kevin J. Bennett, and Selina H. McKinney. 2019. Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse & Neglect 92: 209–18. [Google Scholar] [CrossRef]
- Derogatis, Leonard R., and Kathryn L. Savitz. 2000. The SCL-90-R and Brief Symptom Inventory (BSI) in primary care. In Handbook of Psychological Assessment in Primary Care Settings. Edited by Mark E. Maruish. Mahwah: Lawrence Erlbaum Associates Publishers, pp. 297–334. [Google Scholar]
- Donnelly, Robert, and Katherine Holzer. 2018. The moderating effect of parental support: Internalizing symptoms of emerging adults exposed to community violence. Journal of Evidence-Informed Social Work 15: 564–78. [Google Scholar] [CrossRef]
- Dumas, Tara M., Wendy Elllis, and Dana M. Litt. 2020. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. Journal of Adolescent Health 67: 354–61. [Google Scholar] [CrossRef]
- Farrell, Albert D., Erin L. Thompson, Patrick J. Curran, and Terri N. Sullivan. 2020. Bidirectional relations between witnessing violence, victimization, life events, and physical aggression among adolescents in urban schools. Journal of Youth and Adolescence 49: 1309–27. [Google Scholar] [CrossRef] [PubMed]
- Felitti, Vincent J., Robert F. Anda, Dale Nordenberg, David F. Williamson, Alison M. Spitz, Valerie Edwards, Mary P. Koss, and James S. Marks. 1998. Relationship of child abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14: 245–58. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, Rodrigo S., Lucia Crivelli, Nahuel M. Guimet, Ricardo F. Allegri, and Maria E. Pedreira. 2020. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. Journal of Affective Disorders 277: 75–84. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, David, Heather A. Turner, Anne Shattuck, and Sherry L. Hamby. 2015. Prevalence of childhood exposure to violence, crime, and abuse: Results from the National Survey of Children’s Exposure to Violence. JAMA Pediatrics 169: 746–54. [Google Scholar] [CrossRef]
- Fritz, Catherine O., Peter E. Morris, and Jennifer J. Richler. 2012. Effect size estimates: Current use, calculations, and interpretation. Journal of Experimental Psychology: General 141: 2–18. [Google Scholar] [CrossRef]
- Galea, Sandro, Jennifer Ahern, Heidi Resnick, Dean Kilpatrick, Michael Bucuvalas, Joel Gold, and David Vlahov. 2002. Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine 346: 982–87. [Google Scholar] [CrossRef]
- Garfin, Dana R., E. Aalison Holman, and Roxane C. Silver. 2020. Exposure to prior negative life events and responses to the Boston marathon bombings. Psychological Trauma: Theory, Research, Practice, and Policy 12: 320–29. [Google Scholar] [CrossRef]
- Green, Jennifer G., Katie A. McLaughlin, Patricia A. Berglund, Michael J. Gruber, Nancy A. Sampson, Alan M. Zaslavsky, and Ronald C. Kessler. 2010. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry 67: 113–23. [Google Scholar] [CrossRef]
- Griffin, Gene. 2020. Defining trauma and a trauma-informed COVID-19 response. Psychological Trauma: Theory, Research, Practice, and Policy 12: S279–80. [Google Scholar] [CrossRef]
- Gustavson, Kristin, Ann K. Knudsen, Ragnar Nesvåg, Gun P. Knudsen, Stein E. Vollset, and Ted Reichborn-Kiennerun. 2018. Prevalence and stability of mental disorders among young adults: Findings from a longitudinal study. BMC Psychiatry 18: 65. [Google Scholar] [CrossRef]
- Hammen, Constance, Risha Henry, and Shannon E. Daley. 2000. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology 68: 782–87. [Google Scholar] [CrossRef]
- Hanscom, David, David R. Clawson, Stephen W. Porges, Ray Bunnage, Les Aria, Steve Lederman, James Taylor, and Sue C. Carter. 2020. Polyvagal and global cytokine theory of safety and COVID-19–Plan B. SciMedicine Journal 2: 9–27. [Google Scholar] [CrossRef]
- Harkness, Kate L., Alanna E. Bruce, and Margaret N. Lumley. 2006. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology 115: 730–41. [Google Scholar] [CrossRef] [PubMed]
- Harris Interactive. 2010. The Lesbian, Gay, Bisexual and Transgender (LGBT) Population At-a-Glance. Available online: https://www.witeck.com/wp-content/uploads/2013/03/HI_LGBT_SHEET_WCC_AtAGlance.pdf (accessed on 12 June 2022).
- Hart, Betty, and Todd R. Risley. 1995. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore: Paul H. Brookes Publishing. [Google Scholar]
- Hatem, Cherine, Che Y. Lee, Xue Zhao, Reesor-Layton Oyer, Tabbetha Lopez, and Daphne C. Hernandez. 2020. Food insecurity and housing instability during early childhood as predictors of adolescent mental health. Journal of Family Psychology 34: 721–30. [Google Scholar] [CrossRef]
- Hayes, Andrew F., and Jacob J. Coutts. 2020. Use omega rather than Cronbach’s alpha for estimating reliability. But…. Communication Methods and Measures 14: 1–24. [Google Scholar] [CrossRef]
- Heleniak, Charlotte, Kevin M. King, Kathryn C. Monahan, and Katie A. McLaughlin. 2018. Disruptions in emotion regulation as a mechanism linking community violence exposure to adolescent internalizing problems. Journal of Research on Adolescence 28: 229–44. [Google Scholar] [CrossRef] [PubMed]
- Ho, Jolie T. K., and David A. Moscovitch. 2022. The moderating effects of reported pre-pandemic social anxiety, symptom impairment, and current stressors on mental health and affiliative adjustment during the first wave of the COVID-19 pandemic. Anxiety, Stress & Coping 35: 86–100. [Google Scholar] [CrossRef]
- Holman, E. Alison, Rebecca R. Thompson, Dana Rose Garfin, and Roxane Cohen Silver. 2020. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances 6: 42. [Google Scholar] [CrossRef]
- Hong, Jun Sung, Benjamin W. Fisher, and Dorothy L. Espelage. 2021. An introduction to the special issue: Family violence and youth violence–Examining the connections from interdisciplinary perspectives (an extension of Anna Costanza Baldry’s legacy. Journal of Family Violence 36: 1–4. [Google Scholar] [CrossRef]
- John-Henderson, Neha A., Cory J. Counts, and Annie T. Ginty. 2021. Associations between childhood abuse and COVID-19 hyperarousal in adulthood: The role of social environment. Frontiers in Psychology 12: 565610. [Google Scholar] [CrossRef]
- Kalia, Vrinda, Katherine Knauft, and Niki Hayatbini. 2020. Cognitive flexibility and perceived threat from COVID-19 mediate the relationship between childhood maltreatment and state anxiety. PLoS ONE 15: e0243881. [Google Scholar] [CrossRef] [PubMed]
- Kendler, Kenneth S., Jonathan W. Kuhn, and Carol A. Prescott. 2004. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychological Medicine 34: 1475–82. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, Traci M., and Rosario Ceballo. 2014. Who, what, when, and where? Toward a dimensional conceptualization of community violence exposure. Review of General Psychology 18: 69–81. [Google Scholar] [CrossRef]
- Kessler, Ronald C., Christopher G. Davis, and Kenneth S. Kendler. 1997. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine 27: 1101–19. [Google Scholar] [CrossRef] [PubMed]
- Keyes, Corey L. M. 2007. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. American Psychologist 62: 95–108. [Google Scholar] [CrossRef]
- Keyes, Corey L. M., Satvinder S. Dhingra, and Eduardo J. Simoes. 2010. Change in level of positive mental health as a predictor of future risk of mental illness. American Journal of Public Health 100: 2366–71. [Google Scholar] [CrossRef]
- Killgore, William D. S., Emily C. Taylor, Sara A. Cloonan, and Natalie S. Dailey. 2020. Psychological resilience during the COVID-19 lockdown. Psychiatry Research 291: 113216. [Google Scholar] [CrossRef]
- Kim, Hyunsik, and Nicholas R. Eaton. 2017. A hierarchical integration of person-centered comorbidity models: Structure, stability, and transition over time. Clinical Psychological Science 5: 595–612. [Google Scholar] [CrossRef]
- Kolacz, Jacek, Lourdes P. Dale, Evan J. Nix, Olivia K. Roath, Gregory F. Lewis, and Stephen W. Porges. 2020. Adversity history predicts self-reported autonomic reactivity and mental health in US residents during the COVID-19 pandemic. Frontiers in Psychiatry 11: 577728. [Google Scholar] [CrossRef]
- La Rocque, Cherie L., Kate L. Harkness, and R. Michael Bagby. 2014. The differential relation of childhood maltreatment to stress sensitization in adolescent and young adult depression. Journal of Adolescence 37: 871–82. [Google Scholar] [CrossRef]
- Lambert, Hilary K., Kevin M. King, Kathryn C. Monahan, and Katie A. McLaughlin. 2017. Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Development and Psychopathology 29: 929–40. [Google Scholar] [CrossRef] [PubMed]
- Lambert, Sharon F., Rhonda C. Boyd, Nicole L. Cammack, and Nicholas S. Ialongo. 2012. Relationship proximity to victims of witnessed community violence: Associations with adolescent internalizing and externalizing behaviors. American Journal of Orthopsychiatry 82: 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lanza, Stephanie T., and Brittany L. Rhoades. 2013. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prevention Science: The Official Journal of the Society for Prevention Research 14: 157–68. [Google Scholar] [CrossRef] [PubMed]
- Lanza, Stephanie T., and Brittany R. Cooper. 2016. Latent class analysis for developmental research. Child Development Perspectives 10: 59–64. [Google Scholar] [CrossRef] [PubMed]
- Lanza, Stephanie T., Bethany C. Bray, and Linda M. Collins. 2013. An introduction to latent class and latent transition analysis. In Handbook of Psychology: Research Methods in Psychology, 2nd ed. Edited by John A. Schinka, Wayne F. Velicer and Irving B. Weiner. Hoboken: John Wiley & Sons Inc., vol. 2, pp. 691–716. [Google Scholar] [CrossRef]
- Lee, Haenim, Youngmi Kim, and Jasmine Terry. 2020. Adverse childhood experiences (ACEs) on mental disorders in young adulthood: Latent classes and community violence exposure. Preventive Medicine 134: 106039. [Google Scholar] [CrossRef]
- Liu, Sabrina R., and Sheila Modir. 2020. The outbreak that was always here: Racial trauma in the context of COVID-19 and implications for mental health providers. Psychological Trauma: Theory, Research, Practice, and Policy 12: 439. [Google Scholar] [CrossRef]
- Masyn, Katherine E. 2013. Latent class analysis and finite mixture modeling. In The Oxford Handbook of Quantitative Methods: Statistical Analysis. Edited by Todd D. Little. Oxford: Oxford University Press, vol. 2, pp. 551–611. [Google Scholar]
- McCrory, Eamon, Stephane A. De Brito, and Essi Viding. 2011. The impact of childhood maltreatment: A review of neurobiological and genetic factors. Frontiers in Psychiatry 2: 48. [Google Scholar] [CrossRef]
- McDonald, Shelby E., Kelly E. O’connor, Angela Matijczak, Camie A. Tomlinson, Jennifer W. Applebaum, Jennifer L. Murphy, and Barbara A. Zsembik. 2021. Attachment to pets moderates transitions in latent patterns of mental health following the onset of the COVID-19 pandemic: Results of a survey of U.S. adults. Animals 11: 895. [Google Scholar] [CrossRef]
- McDowell, Caitlin, and Ellie Fossey. 2014. Workplace accommodations for people with mental illness: A scoping review. Journal of Occupational Rehabilitation 25: 197–206. [Google Scholar] [CrossRef]
- McGinty, Emma E., Rachel Presskreischer, Hahrie Han, and Colleen L. Barry. 2020. Psychological distress and loneliness reported by US adults in. 2018 and April. JAMA 324: 93–94. [Google Scholar] [CrossRef]
- McKnight-Eily, Lela R., Catherine A. Okoro, Tara W. Strine, Jorge Verlenden, NaTasha D. Hollis, Rashid Njai, Elizabeth W. Mitchell, Amy Board, Richard Puddy, and Craig Thomas. 2021. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. Morbidity and Mortality Weekly Report 70: 162–66. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, Katie A., and Margaret Sheridan. 2016. Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science 25: 239–45. [Google Scholar] [CrossRef]
- McLaughlin, Katie A., David Weissman, and Debbie Bitrán. 2019. Childhood adversity and neural development: A systematic review. Annual Review of Developmental Psychology 1: 277–312. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, Katie A., Jennifer Greif Green, Michael J. Gruber, Nancy A. Sampson, Alan M. Zaslavsky, and Ronald C. Kessler. 2012. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry 69: 1151–60. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, Katie A., Karestan C. Koenen, Evelyn J. Bromet, Elie G. Karam, Howard Liu, Maria Petukhova, Ayelet Meron Ruscio, Nancy A. Sampson, Dan J. Stein, Sergio Aguilar-Gaxiola, and et al. 2017. Childhood adversities and post-traumatic stress disorder: Evidence for stress sensitisation in the World Mental Health Surveys. The British Journal of Psychiatry 211: 280–88. [Google Scholar] [CrossRef]
- McLaughlin, Katie A., Kerith J. Conron, Karestan C. Koenen, and Stephen E. Gilman. 2010. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine 40: 1647–58. [Google Scholar] [CrossRef]
- McLaughlin, Katie A., Margaret A. Sheridan, Sonia Alves, and Wendy Berry Mendes. 2014. Child maltreatment and autonomic nervous system reactivity: Identifying dysregulated stress reactivity patterns using the biopsychosocial model of challenge and threat. Psychosomatic Medicine 76: 538–46. [Google Scholar] [CrossRef]
- Merrick, Melissa T., Katie A. Ports, Derek C. Ford, Tracie O. Afifi, Elizabeth T. Gershoff, and Andrew Grogan-Kaylor. 2017. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect 69: 10–19. [Google Scholar] [CrossRef]
- Mersky, J. P., J. Topitzes, and A. J. Reynolds. 2013. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect 37: 917–25. [Google Scholar] [CrossRef]
- Meyer, Ilan H. 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin 129: 674–97. [Google Scholar] [CrossRef]
- Meyers, Jacquelyn L., Sarah R. Lowe, Nicholas R. Eaton, Robert Krueger, Bridget F. Grant, and Deborah Hasin. 2015. Childhood maltreatment, 9/11 exposure, and latent dimensions of psychopathology: A test of stress sensitization. Journal of Psychiatric Research 68: 337–45. [Google Scholar] [CrossRef] [PubMed]
- Moreno, Carmen, Til Wykes, Silvana Galderisi, Merete Nordentoft, Nicolas Crossley, Nev Jones, Mary Cannon, Christoph U. Correll, Louise Byrne, Sarah Carr, and et al. 2020. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry 7: 813–24. [Google Scholar] [CrossRef] [PubMed]
- Norman, Rosana E., Munkhtsetseg Byambaa, Rumna De, Alexander Butchart, James Scott, and Theo Vos. 2012. The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine 9: e1001349. [Google Scholar] [CrossRef] [PubMed]
- Nurius, Paula S., Sara Green, Patricia Logan-Greene, and Sharon Borja. 2015. Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse & Neglect 45: 143–53. [Google Scholar] [CrossRef]
- Nylund-Gibson, Karen, and Shelley R. Hart. 2014. Latent class analysis in prevention science. In Defining Prevention Science. Edited by Zili Sloboda and Hanno Petras. Berlin and Heidelberg: Springer US, pp. 493–511. [Google Scholar] [CrossRef]
- Panchal, Nirmita, Rabah Kamal, Cynthia Cox, and Rachel Garfield. 2021. The Implications of COVID-19 for Mental Health and Substance Use [Issue Brief]. San Francisco: Kaiser Family Foundation. Available online: https://www.kff.org/Coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ (accessed on 12 June 2022).
- Penninx, Brenda WJH, Michael E. Benros, Robyn S. Klein, and Christiaan H. Vinkers. 2022. How COVID-19 shaped mental health: From infection to pandemic effects. Nature Medicine 28: 2027–37. [Google Scholar] [CrossRef] [PubMed]
- Perry, Kristin J., Jamie M. Ostrov, Shannon Shisler, Rina D. Eiden, Amanda B. Nickerson, Stephanie A. Godleski, and Pamela Schuetze. 2021. Pathways from early family violence to adolescent reactive aggression and violence victimization. Journal of Family Violence 36: 75–86. [Google Scholar] [CrossRef] [PubMed]
- Peterson, Zoë D., Ellen L. Vaughan, and Dasha N. Carver. 2020. Sexual identity and psychological reactions to COVID-19. Traumatology 27: 6. [Google Scholar] [CrossRef]
- Poole-Di Salvo, Elizabeth, Ellen J. Silver, and Ruth EK Stein. 2016. Household food insecurity and mental health problems among adolescents: What do parents report? Academic Pediatrics 16: 90–96. [Google Scholar] [CrossRef]
- Porges, Stephen W. 1993. Body Perception Questionnaire. College Park: Laboratory of Developmental Assessment, University of Maryland. Available online: https://www.stephenporges.com/body-scales (accessed on 12 June 2022).
- Porges, Stephen W. 1995. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology 32: 301–18. [Google Scholar] [CrossRef]
- Porges, Stephen W. 2007. The polyvagal perspective. Biological Psychology 74: 116–43. [Google Scholar] [CrossRef]
- Porges, Stephen W. 2020. Challenge to our nervous system: A polyvagal perspective. Clinical Neuropsychiatry 17: 135–38. [Google Scholar] [CrossRef]
- Robillard, Rebecca, Mysa Saad, Jodi Edwards, Elizaveta Solomonova, Marie-Hélène Pennestri, Alexander Daros, Samuel Paul Louis Veissière, Lena Quilty, Karianne Dion, Ashley Nixon, and et al. 2020. Social, financial and psychological stress during an emerging pandemic: Observations from a population survey in the acute phase of COVID-19. BMJ Open 10: e043805. [Google Scholar] [CrossRef] [PubMed]
- Salerno, John P., Natasha D. Williams, and Karina A. Gattamorta. 2020. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy 12: S239. [Google Scholar] [CrossRef] [PubMed]
- Scandurra, Cristiano, Agostino Carbone, Roberto Baiocco, Selene Mezzalira, Nelson Mauro Maldonato, and Vincenzo Bochicchio. 2021. Gender identity milestones, minority stress and mental health in three generational cohorts of Italian binary and nonbinary transgender people. International Journal of Environmental Research and Public Health 18: 9057. [Google Scholar] [CrossRef]
- Shackman, Jessica E., Alexander J. Shackman, and Seth D. Pollakk. 2007. Physical abuse amplifies attention to threat and increases anxiety in children. Emotion 7: 838–52. [Google Scholar] [CrossRef]
- Shanahan, Lilly, Annekatrin Steinhoff, Laura Bechtiger, Aja L. Murray, Amy Nivette, Urs Hepp, Denis Ribeaud, and Manuel Eisner. 2022. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine 52: 824–33. [Google Scholar] [CrossRef] [PubMed]
- Shin, Sunny H., Shelby Elaine McDonald, and David Conley. 2018. Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addictive Behaviors 78: 187–92. [Google Scholar] [CrossRef]
- Shreffler, Karina M., Christine N. Joachims, Stacy Tiemeyer, W. Kyle Simmons, T. Kent Teague, and Jennifer Hays-Grudo. 2021. Childhood adversity and perceived distress from the COVID-19 pandemic. Adversity and Resilience Science 2: 1–4. [Google Scholar] [CrossRef]
- Stein, Bradley D., Lisa H. Jaycox, Sheryl Kataoka, Hilary J. Rhodes, and Katherine D. Vestal. 2003. Prevalence of child and adolescent exposure to community violence. Clinical Child and Family Psychology Review 6: 247–64. [Google Scholar] [CrossRef]
- Taylor, Jeremy J., Kathryn E. Grant, Courtney A. Zulauf, Patrick J. Fowler, David A. Meyerson, and Sireen Irsheid. 2018. Exposure to community violence and the trajectory of internalizing and externalizing symptoms in a sample of low-income urban youth. Journal of Clinical Child & Adolescent Psychology 47: 421–35. [Google Scholar] [CrossRef]
- Vaidyanathan, Uma, Christopher J. Patrick, and William G. Iacono. 2011. Patterns of comorbidity among mental disorders: A person-centered approach. Comprehensive Psychiatry 52: 527–35. [Google Scholar] [CrossRef]
- Wakeel, Fathima, and Anuli Njoku. 2021. Application of the weathering framework: Intersection of racism, stigma, and COVID-19 as a stressful life event among African Americans. Healthcare 9: 145. [Google Scholar] [CrossRef] [PubMed]
- Wingo, Aliza P., Glenda Wrenn, Tiffany Pelletier, Alisa R. Gutman, Bekh Bradley, and Kerry J. Ressler. 2010. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of Affective Disorders 126: 411–14. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Jiaqi, Orly Lipsitz, Flora Nasri, Leanna M. W. Lui, Hartej Gill, Lee Phan, David Chen-Li, Michelle Iacobucci, Roger Ho, Amna Majeed, and et al. 2020. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders 277: 55–64. [Google Scholar] [CrossRef] [PubMed]
- Zinzow, Heidi M., Kenneth J. Ruggiero, Heidi Resnick, Rochelle Hanson, Daniel Smith, Benjamin Saunders, and Dean Kilpatrick. 2009. Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal of Child Psychology and Psychiatry 50: 441–50. [Google Scholar] [CrossRef]
| Variable | Variable Categories | N | % |
|---|---|---|---|
| Race/ethnicity | Arab/Arab American | 2 | 0.1 |
| Asian/Asian American | 42 | 2.2 | |
| Black/African American | 15 | 0.8 | |
| First Nations/Indigenous | 3 | 0.2 | |
| Latino/Latina/Latinx | 50 | 2.6 | |
| South Asian/Pacific Islander | 7 | 0.4 | |
| White | 1702 | 87.6 | |
| Multiracial/Mixed Race | 111 | 5.7 | |
| Prefer to self-describe | 10 | 0.5 | |
| Gender identity | Cisgender female/woman | 1743 | 89.8 |
| Cisgender male/man | 135 | 7.0 | |
| Genderqueer/gender non-conforming | 21 | 1.1 | |
| Transgender female/woman | 2 | 0.1 | |
| Transgender male/man | 7 | 0.4 | |
| Multiple identities | 29 | 1.5 | |
| Missing | 5 | 0.3 | |
| Sexual orientation | Asexual | 25 | 1.3 |
| Bisexual | 157 | 8.1 | |
| Demisexual | 11 | 0.6 | |
| Gay | 21 | 1.1 | |
| Heterosexual/straight | 1510 | 77.8 | |
| Lesbian | 50 | 2.6 | |
| Pansexual | 27 | 1.4 | |
| Queer | 29 | 1.5 | |
| Two-Spirit | 1 | 0.1 | |
| Multiple identities | 83 | 4.3 | |
| Not sure/questioning | 22 | 1.1 | |
| Prefer to self-describe | 6 | 0.3 | |
| Relationship status | Divorced | 132 | 6.8 |
| Married/permanently partnered | 1209 | 62.3 | |
| Single/never married | 522 | 26.9 | |
| Separated | 27 | 1.4 | |
| Widowed | 20 | 1.0 | |
| Prefer to self-describe | 32 | 1.6 | |
| Employment status change due to COVID-19 a,b | None | 836 | 43.0 |
| Work from home | 909 | 46.8 | |
| Laid off/Fired | 151 | 7.8 | |
| New job | 25 | 1.3 | |
| Other | 273 | 14.1 | |
| Missing | 1 | 0.1 | |
| Childhood adversity exposure b | Family violence | 538 | 27.7 |
| Community violence | 408 | 21.0 | |
| Basic needs not met | 260 | 13.4 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Somatization a | - | |||||||||||||||||||||||
| 2. Obsessive-compulsive a | 0.47 Δ | - | ||||||||||||||||||||||
| 3. Interpersonal sensitivity a | 0.40 Δ | 0.62 Δ | - | |||||||||||||||||||||
| 4. Depressed mood a | 0.43 Δ | 0.64 Δ | 0.68 Δ | - | ||||||||||||||||||||
| 5. Anxiety a | 0.46 Δ | 0.62 Δ | 0.61 Δ | 0.62 Δ | - | |||||||||||||||||||
| 6. Hostility a | 0.37 Δ | 0.52 Δ | 0.52 Δ | 0.52 Δ | 0.51 Δ | - | ||||||||||||||||||
| 7. Phobic anxiety a | 0.35 Δ | 0.47 Δ | 0.50 Δ | 0.46 Δ | 0.50 Δ | 0.37 Δ | - | |||||||||||||||||
| 8. Additional items a | 0.43 Δ | 0.54 Δ | 0.47 Δ | 0.53 Δ | 0.50 Δ | 0.36 Δ | 0.38 Δ | - | ||||||||||||||||
| 9. Somatization b | 0.68 Δ | 0.37 Δ | 0.34 Δ | 0.37 Δ | 0.38 Δ | 0.29 Δ | 0.30 Δ | 0.33 Δ | - | |||||||||||||||
| 10. Obsessive–compulsive b | 0.36 Δ | 0.69 Δ | 0.50 Δ | 0.53 Δ | 0.53 Δ | 0.40 Δ | 0.39 Δ | 0.45 Δ | 0.44 Δ | - | ||||||||||||||
| 11. Interpersonal sensitivity b | 0.34 Δ | 0.49 Δ | 0.73 Δ | 0.55 Δ | 0.47 Δ | 0.40 Δ | 0.42 Δ | 0.38 Δ | 0.39 Δ | 0.55 Δ | - | |||||||||||||
| 12. Depressed mood b | 0.34 Δ | 0.47 Δ | 0.54 Δ | 0.68 Δ | 0.50 Δ | 0.38 Δ | 0.38 Δ | 0.41 Δ | 0.46 Δ | 0.65 Δ | 0.63 Δ | - | ||||||||||||
| 13. Anxiety b | 0.34 Δ | 0.43 Δ | 0.45 Δ | 0.46 Δ | 0.62 Δ | 0.34 Δ | 0.39 Δ | 0.37 Δ | 0.48 Δ | 0.60 Δ | 0.52 Δ | 0.66 Δ | - | |||||||||||
| 14. Hostility b | 0.26 Δ | 0.38 Δ | 0.40 Δ | 0.41 Δ | 0.41 Δ | 0.56 Δ | 0.29 Δ | 0.29 Δ | 0.34 Δ | 0.41 Δ | 0.49 Δ | 0.53 Δ | 0.52 Δ | - | ||||||||||
| 15. Phobic anxiety b | 0.20 Δ | 0.28 Δ | 0.31 Δ | 0.28 Δ | 0.34 Δ | 0.23 Δ | 0.42 Δ | 0.26 Δ | 0.31 Δ | 0.41 Δ | 0.36 Δ | 0.46 Δ | 0.55 Δ | 0.30 Δ | - | |||||||||
| 16. Additional items b | 0.33 Δ | 0.44 Δ | 0.41 Δ | 0.45 Δ | 0.44 Δ | 0.30 Δ | 0.34 Δ | 0.64 Δ | 0.42 Δ | 0.57 Δ | 0.46 Δ | 0.60 Δ | 0.57 Δ | 0.43 Δ | 0.41 Δ | - | ||||||||
| 17. Age | −0.08 Ψ | −0.26 Δ | −0.30 Δ | −0.24 Δ | −0.26 Δ | −0.22 Δ | −0.21 Δ | −0.10 Δ | −0.08 Δ | −0.31 Δ | −0.28 Δ | −0.30 Δ | −0.24 Δ | −0.27 Δ | −0.12 Δ | −0.18 Δ | - | |||||||
| 18. Race/ethnicity c | −0.01 | −0.05 * | −0.03 | −0.06 Ψ | −0.04 | −0.08 Δ | −0.03 | −0.04 | −0.02 | −0.04 | −0.04 | −0.02 | −0.03 | −0.06 Ψ | −0.02 | −0.04 | 0.11 Δ | - | ||||||
| 19. SGM d | 0.14 Δ | 0.18 Δ | 0.17 Δ | 0.21 Δ | 0.19 Δ | 0.12 Δ | 0.18 Δ | 0.12 Δ | 0.13 Δ | 0.21 Δ | 0.17 Δ | 0.22 Δ | 0.19 Δ | 0.10 Δ | 0.10 Δ | 0.16 Δ | −0.23 Δ | −0.03 | - | |||||
| 20. Relationship status e | −0.02 | −0.11 Δ | −0.10 Δ | −0.19 Δ | −0.09 Δ | −0.04 | −0.04 | −0.06 | −0.06 * | −0.13 Δ | −0.08 Δ | −0.18 Δ | −0.07 Ψ | −0.04 | −0.01 | −0.08 Ψ | 0.10 Δ | 0.04 | −0.14 Δ | - | ||||
| 21. Employment change due to COVID f | 0.04 | 0.11 Δ | 0.09 Δ | 0.08 Δ | 0.13 Δ | 0.08 Δ | 0.06 Ψ | 0.03 | 0.05 * | 0.15 Δ | 0.07 Ψ | 0.10 Δ | 0.12 Δ | 0.07 Ψ | 0.07 Ψ | 0.07 Ψ | −0.25 Δ | −0.02 | 0.10 Δ | −0.02 | - | |||
| 22. Family violence g | 0.13 Δ | 0.13 Δ | 0.13 Δ | 0.16 Δ | 0.17 Δ | 0.13 Δ | 0.16 Δ | 0.14 Δ | 0.13 Δ | 0.11 Δ | 0.12 Δ | 0.11 Δ | 0.15 Δ | 0.07 Ψ | 0.08 Δ | 0.13 Δ | 0.07 Ψ | −0.05 * | 0.13 Δ | −0.02 | 0.01 | - | ||
| 23. Community violence g | 0.15 Δ | 0.17 Δ | 0.12 Δ | 0.17 Δ | 0.19 Δ | 0.09 Δ | 0.14 Δ | 0.17 Δ | 0.14 Δ | 0.15 Δ | 0.14 Δ | 0.12 Δ | 0.14 Δ | 0.11 Δ | 0.09 Δ | 0.16 Δ | −0.06 * | −0.13 Δ | 0.11 Δ | −0.07 Ψ | 0.01 | 0.27 Δ | - | |
| 24. Needs not met g | 0.11 Δ | 0.12 Δ | 0.13 Δ | 0.15 Δ | 0.15 Δ | 0.10 Δ | 0.15 Δ | 0.11 Δ | 0.10 | 0.13 Δ | 0.10 Δ | 0.12 Δ | 0.14 Δ | 0.06 * | 0.08 Ψ | 0.12 Δ | 0.002 | −0.03 | 0.13 Δ | −0.001 | 0.03 | 0.50 Δ | 0.23 Δ | - |
| N | 1938 | 1938 | 1938 | 1939 | 1934 | 1934 | 1936 | 1933 | 1921 | 1921 | 1923 | 1923 | 1921 | 1921 | 1921 | 1921 | 1942 | 1942 | 1942 | 1942 | 1942 | 1918 | 1937 | 1941 |
| M/n | 0.96 | 1.42 | 1.32 | 1.29 | 1.24 | 1.26 | 0.89 | 1.38 | 1.01 | 1.64 | 1.11 | 1.58 | 1.46 | 1.31 | 1.73 | 1.67 | 39.68 | 1702 | 446 | 1233 | 1262 | 538 | 408 | 260 |
| SD/% | 0.80 | 0.77 | 0.92 | 0.87 | 0.77 | 0.76 | 0.92 | 0.87 | 0.88 | 0.90 | 0.99 | 0.95 | 0.88 | 0.88 | 1.21 | 0.91 | 13.61 | 87.6 | 23.0 | 63.5 | 65.0 | 27.7 | 21.0 | 13.4 |
| k | Par | LL | AIC | BIC | aBIC | VLMR-LRT | LMR-LRT | BLRT | Entropy | Smallest Class | Condition Number | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | p-Value | p-Value | n | % | |||||||||
| Pre-COVID | 1 | 16 | −20,027.8 | 40,087.5 | 40,177.3 | 40,126.5 | NA | NA | NA | NA | 2021 | 100% | 3.63 × 10−2 |
| 2 | 25 | −17,758.9 | 35,567.8 | 35,708.0 | 35,628.6 | 0.000 | 0.000 | 0.000 | 0.888 | 482 | 24% | 1.92 × 10−2 | |
| 3 | 34 | −16,789.1 | 33,646.2 | 33,837.0 | 33,728.9 | 0.000 | 0.000 | 0.000 | 0.855 | 286 | 14% | 5.04 × 10−3 | |
| 4 | 43 | −16,438.3 | 32,962.7 | 33,204.0 | 33,067.3 | 0.021 | 0.022 | 0.000 | 0.846 | 150 | 7% | 1.33 × 10−3 | |
| 5 | 52 | −16,277.8 | 32,659.5 | 32,951.3 | 32,786.1 | 0.000 | 0.000 | 0.000 | 0.809 | 91 | 5% | 5.41 × 10−4 | |
| 6 | 61 | −16,221.7 | 32,565.3 | 32,907.6 | 32,713.8 | 0.318 | 0.325 | 0.000 | 0.826 | 95 | 5% | 2.77 × 10−6 | |
| Post-COVID | 1 | 16 | −21,822.8 | 43,677.6 | 43,767.2 | 43,716.4 | NA | NA | NA | NA | 2000 | 100% | 1.73 × 10−2 |
| 2 | 25 | −19,516.7 | 39,083.4 | 39,223.5 | 39,144.0 | 0.000 | 0.000 | 0.000 | 0.860 | 672 | 34% | 3.46 × 10−2 | |
| 3 | 34 | −18,651.1 | 37,370.3 | 37,560.7 | 37,452.7 | 0.000 | 0.000 | 0.000 | 0.844 | 267 | 13% | 9.08 × 10−3 | |
| 4 | 43 | −18,309.1 | 36,704.3 | 36,945.1 | 36,808.5 | 0.000 | 0.000 | 0.000 | 0.833 | 198 | 10% | 2.62 × 10−3 | |
| 5 | 52 | −18,203.7 | 36,511.5 | 36,802.7 | 36,637.5 | 0.036 | 0.037 | 0.000 | 0.823 | 80 | 4% | 6.78 × 10−4 | |
| 6 | 61 | −18,122.4 | 36,366.9 | 36,708.5 | 36,514.7 | 0.002 | 0.002 | 0.000 | 0.796 | 77 | 4% | 5.03 × 10−4 | |
| 7 | 70 | −18,034.2 | 36,208.5 | 36,600.5 | 36,378.1 | 0.412 | 0.418 | 0.000 | 0.861 | 92 | 4.6% | 2.77 × 10−6 | |
| Pre-Pandemic | During Pandemic | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | X2 | df | p | OR | X2 | df | p | |
| Employment | 31.12 | 4 | 0.000 | 25.63 | 4 | 0.000 | ||
| Severe | 0.94 *** | 0.65 ** | ||||||
| High | 0.80 *** | 1.13 *** | ||||||
| Moderate | 1.43 *** | 1.62 *** | ||||||
| Mild | 1.24 *** | 1.25 *** | ||||||
| Low | 0.48 *** | 0.56 *** | ||||||
| Age | 83.30 | 4 | 0.000 | 103.45 | 4 | 0.000 | ||
| Severe | 0.79 *** | 0.86 *** | ||||||
| High | 0.71 *** | 0.73 *** | ||||||
| Moderate | 1.21 *** | 1.08 *** | ||||||
| Mild | 1.56 *** | 1.57 *** | ||||||
| Low | 1.71 *** | 1.65 *** | ||||||
| Race/Ethnicity | 11.66 | 4 | 0.020 | 30.66 | 4 | 0.000 | ||
| Severe | 0.48 ** | 0.32 ** | ||||||
| High | 1.21 *** | 1.75 ** | ||||||
| Moderate | 1.53 *** | 1.89 *** | ||||||
| Mild | 0.99 *** | 1.56 *** | ||||||
| Low | 0.69 *** | 0.59 ** | ||||||
| In a Relationship | 15.77 | 4 | 0.003 | 15.13 | 4 | 0.004 | ||
| Severe | 0.86 *** | 0.53 *** | ||||||
| High | 0.73 *** | 1.44 *** | ||||||
| Moderate | 1.08 *** | 1.08 *** | ||||||
| Mild | 1.57 *** | 1.36 *** | ||||||
| Low | 1.65 *** | 2.17 *** | ||||||
| Sexual/Gender Minority | 43.60 | 4 | 0.000 | 50.75 | 4 | 0.000 | ||
| Severe | 1.12 *** | 1.04 *** | ||||||
| High | 1.51 *** | 1.46 *** | ||||||
| Moderate | 0.85 *** | 0.99 *** | ||||||
| Mild | 0.44 *** | 0.45 *** | ||||||
| Low | 0.28 ** | 0.24 ** | ||||||
| Post-COVID | ||||||
|---|---|---|---|---|---|---|
| Low Symptoms (12%) | Mild Symptoms (42%) | Moderate Symptoms (32%) | High Symptoms (11%) | Severe Symptoms (4%) | ||
| Pre-COVID | Transition probabilities | |||||
| Low symptoms (12%) | 0.67 | 0.23 | 0.08 | 0.03 | 0.00 | |
| Mild symptoms (39%) | 0.02 | 0.81 | 0.14 | 0.03 | 0.00 | |
| Moderate symptoms (33%) | 0.00 | 0.09 | 0.79 | 0.12 | 0.01 | |
| High symptoms (11%) | 0.00 | 0.04 | 0.23 | 0.70 | 0.03 | |
| Severe symptoms (5%) | 0.01 | 0.06 | 0.20 | 0.34 | 0.39 | |
| Transition proportions (%) | ||||||
| Low symptoms (12%) | 10.14% | 1.34% | 0.36% | 0.05% | 0.00% | |
| Mild symptoms (39%) | 1.85% | 33.52% | 3.50% | 0.77% | 0.26% | |
| Moderate symptoms (33%) | 0.26% | 3.50% | 25.49% | 3.30% | 0.36% | |
| High symptoms (11%) | 0.00% | 0.46% | 2.21% | 7.11% | 0.82% | |
| Severe symptoms (5%) | 0.05% | 0.21% | 0.57% | 0.88% | 2.99% | |
| Childhood exposure to FV (X2)—n = 1918 | ||||||
| Low symptoms (12%) | a | 0.41 | −21.03 *** | −22.93 *** | 1.41 b | |
| Mild symptoms (39%) | a | −0.35 | 0.02 | −1.63 | 0.58 | |
| Moderate symptoms (33%) | a | −0.40 | −0.66 | −0.46 | 1.43 | |
| High symptoms (11%) | a | −0.26 | −1.32 | −1.54 | −1.10 | |
| Severe symptoms (5%) | a | 23.46 b | 23.39 *** | 24.74 *** | 23.59 *** | |
| Childhood exposure to CV (X2)—n = 1937 | ||||||
| Low symptoms (12%) | a | 0.28 | −4.08 | −22.29 *** | −0.36 b | |
| Mild symptoms (39%) | a | −1.04 | −1.40 | −0.58 | −19.19 *** | |
| Moderate symptoms (33%) | a | 23.62 *** | 23.86 *** | 24.61 *** | 28.01 *** | |
| High symptoms (11%) | a | 12.12 b | 10.69 *** | 10.26 *** | 10.06 *** | |
| Severe symptoms (5%) | a | 46.16 *** | 21.77 *** | 22.19 *** | 22.35 *** | |
| Childhood needs not met (X2)—n = 1941 | ||||||
| Low symptoms (12%) | a | 0.19 | 1.27 | 8.77 ** | 0.05 b | |
| Mild symptoms (39%) | a | 0.21 | 1.25 | −23.77 *** | −21.80 *** | |
| Moderate symptoms (33%) | a | −1.63 | −2.08 * | −1.29 | 1.01 | |
| High symptoms (11%) | a | 8.72 b | 7.52 *** | 6.87 *** | 7.66 *** | |
| Severe symptoms (5%) | a | 22.19 *** | 22.44 *** | 22.74 *** | 22.13 *** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Connor, K.E.; Tomlinson, C.A.; McDonald, S.E.; Brown, S.; Applebaum, J.W.; Murphy, J.L.; Matijczak, A.; Zsembik, B.A.; Porges, S.W. Childhood Adversity Moderates Change in Latent Patterns of Psychological Adjustment during the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Soc. Sci. 2023, 12, 185. https://doi.org/10.3390/socsci12030185
O’Connor KE, Tomlinson CA, McDonald SE, Brown S, Applebaum JW, Murphy JL, Matijczak A, Zsembik BA, Porges SW. Childhood Adversity Moderates Change in Latent Patterns of Psychological Adjustment during the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Social Sciences. 2023; 12(3):185. https://doi.org/10.3390/socsci12030185
Chicago/Turabian StyleO’Connor, Kelly E., Camie A. Tomlinson, Shelby E. McDonald, Samantha Brown, Jennifer W. Applebaum, Jennifer L. Murphy, Angela Matijczak, Barbara A. Zsembik, and Stephen W. Porges. 2023. "Childhood Adversity Moderates Change in Latent Patterns of Psychological Adjustment during the COVID-19 Pandemic: Results of a Survey of U.S. Adults" Social Sciences 12, no. 3: 185. https://doi.org/10.3390/socsci12030185
APA StyleO’Connor, K. E., Tomlinson, C. A., McDonald, S. E., Brown, S., Applebaum, J. W., Murphy, J. L., Matijczak, A., Zsembik, B. A., & Porges, S. W. (2023). Childhood Adversity Moderates Change in Latent Patterns of Psychological Adjustment during the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Social Sciences, 12(3), 185. https://doi.org/10.3390/socsci12030185







