Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework
Abstract
1. Introduction
1.1. Physical Environment Assessment and POE
1.2. Assessing Hospital Built Environment: Yesterday, Today, and Tomorrow
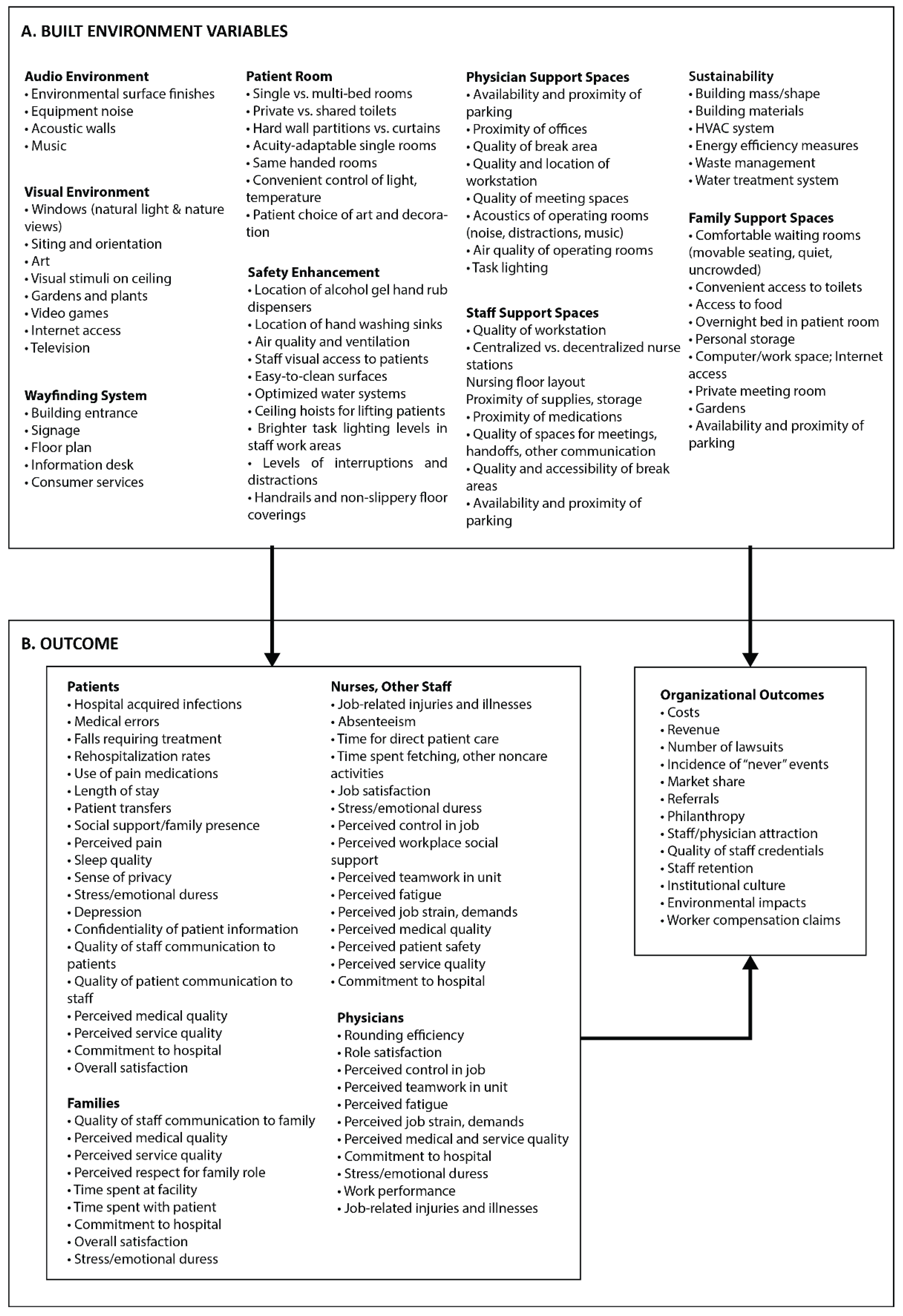
- It is important to note that within the hospital design and evaluation research field, a theoretical model is available to assess the impact of physical environment on user’s health outcomes based on evidence. Those topics, some of which are connected to Indoor Environmental Quality (IEQ) dimensions [9,15], have been stated after collecting several papers and reviews. The EBD theory developed by Ulrich [16,17,18] and its further applications in several healthcare settings (i.e., [19,20]) is able to support IEQ analysis and POE evaluations with a structured framework different empirical studies (Figure 2).
1.3. Hospitals as High-Performance Environments
1.4. Research Gap and the Paper’s Objective
- are there tools able to evaluate hospital physical environment through POE?
- which are the most used assessment criteria and with which terms do they measure health and/or sustainability?
- is it possible to frame trends or insights for future research on the topic?
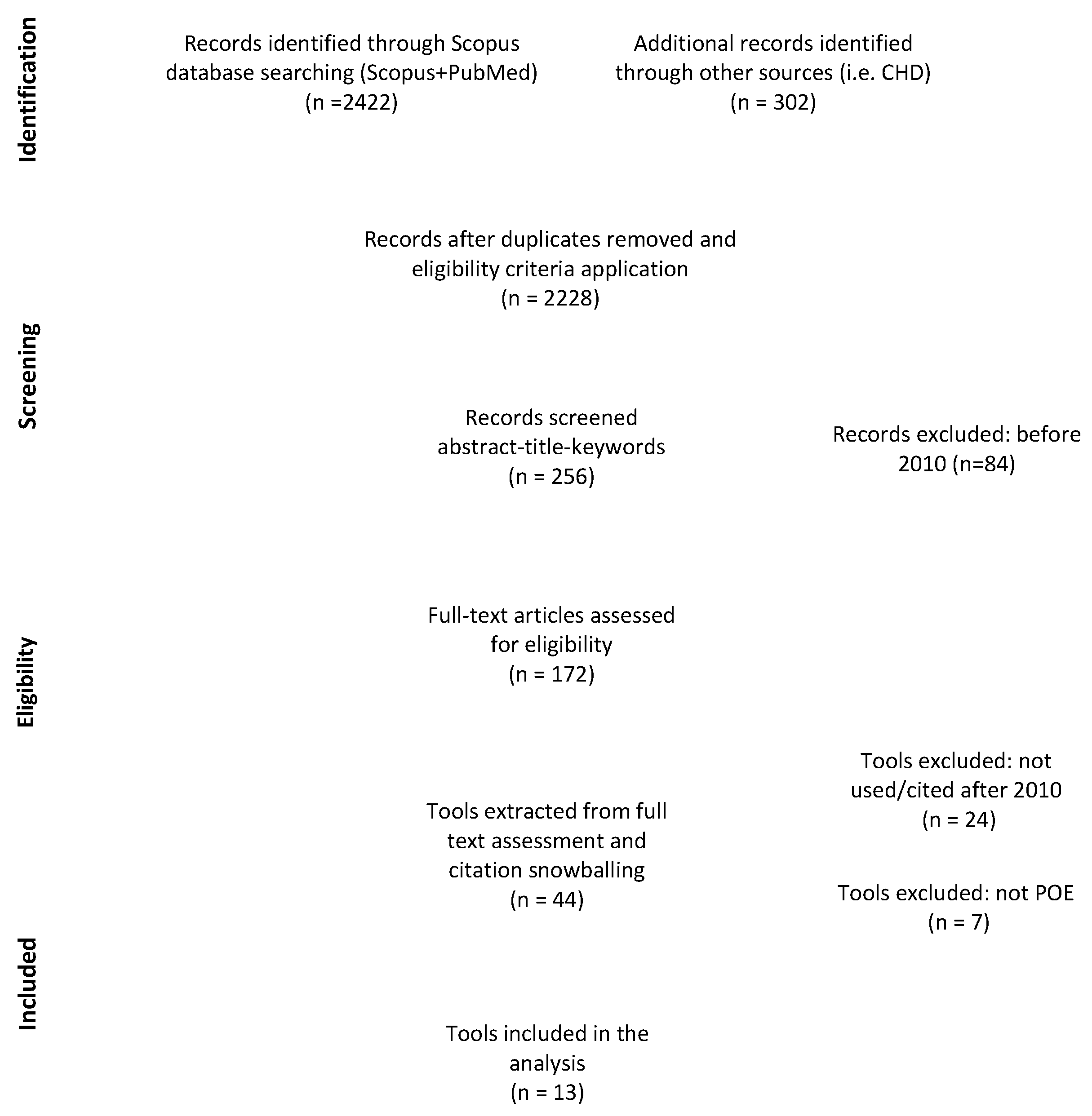
2. Methods
- Center of Health Design (CHD). Available online: https://www.healthdesign.org
- Health and Care Infrastructure Research and Innovation Centre (HaCiCR). Available online: http://www.haciric.org
- International Academy for Design & Health (IADH). Available online: https://www.designandhealth.org
3. Results
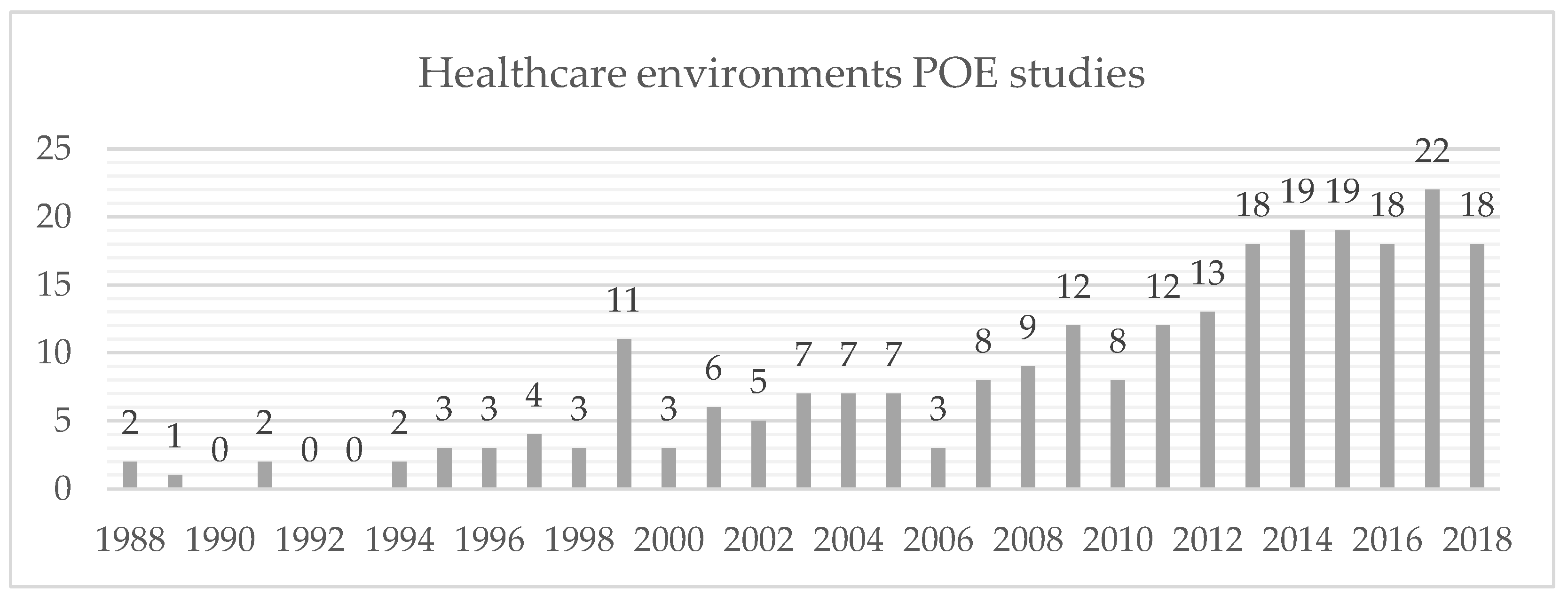
3.1. General Information
3.1.1. Tools’ Structure
3.1.2. Item Sources and Selection
3.1.3. Economic Purpose
3.1.4. Territorial Development
3.1.5. Recurrent Topics
3.2. EBD Health-Related Topics
3.2.1. Safety Enhancement
3.2.2. Visual Environment
3.2.3. Staff and Doctors’ Space Features
3.2.4. Patient Room Features
3.2.5. Wayfinding Features
3.2.6. Family/Visitors’ Space Features
3.2.7. Audio Environment
3.3. Sustainability Topics
3.4. Other Topics
4. Discussion
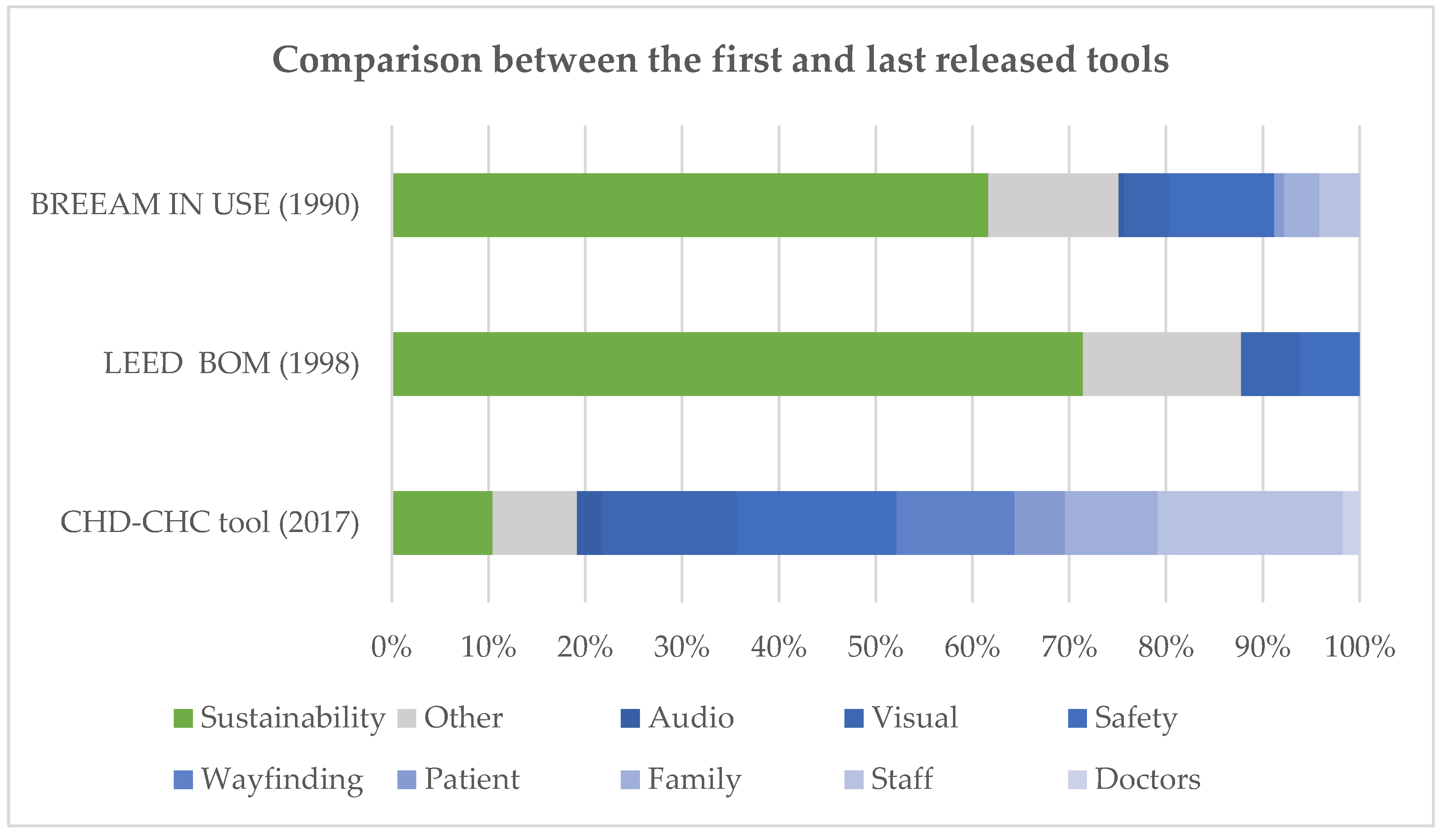
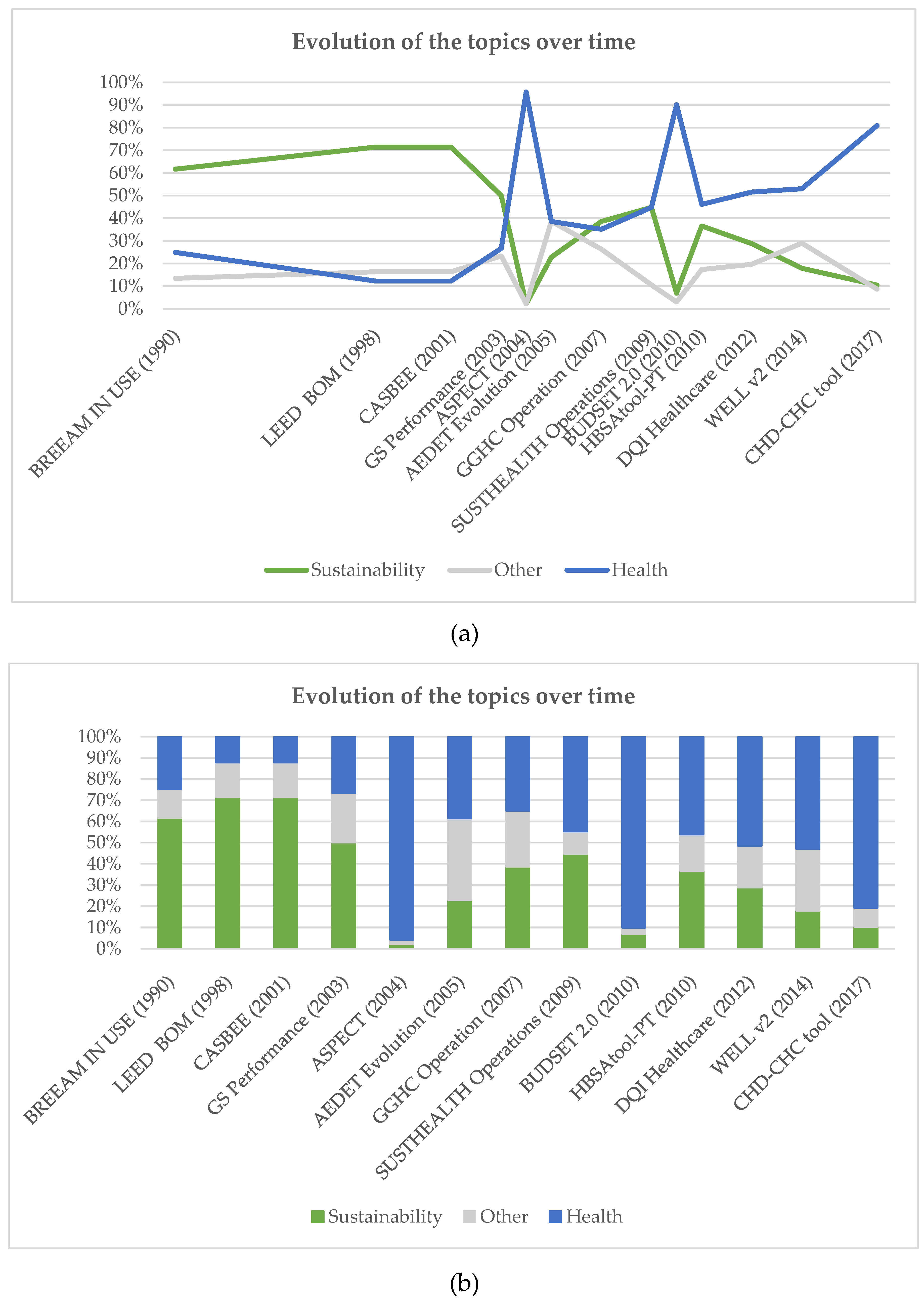
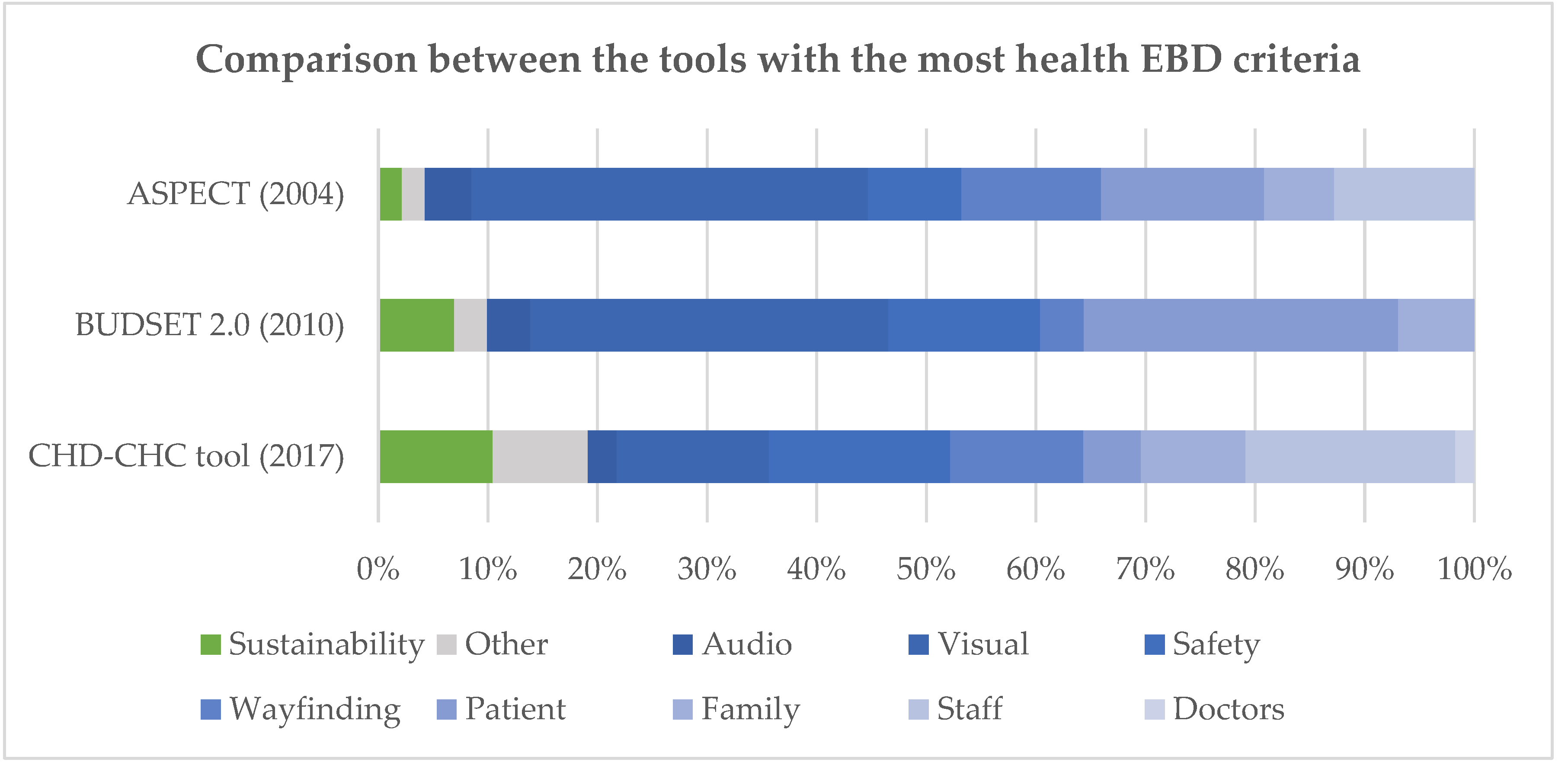
4.1. Evolution of POE Tools over Time
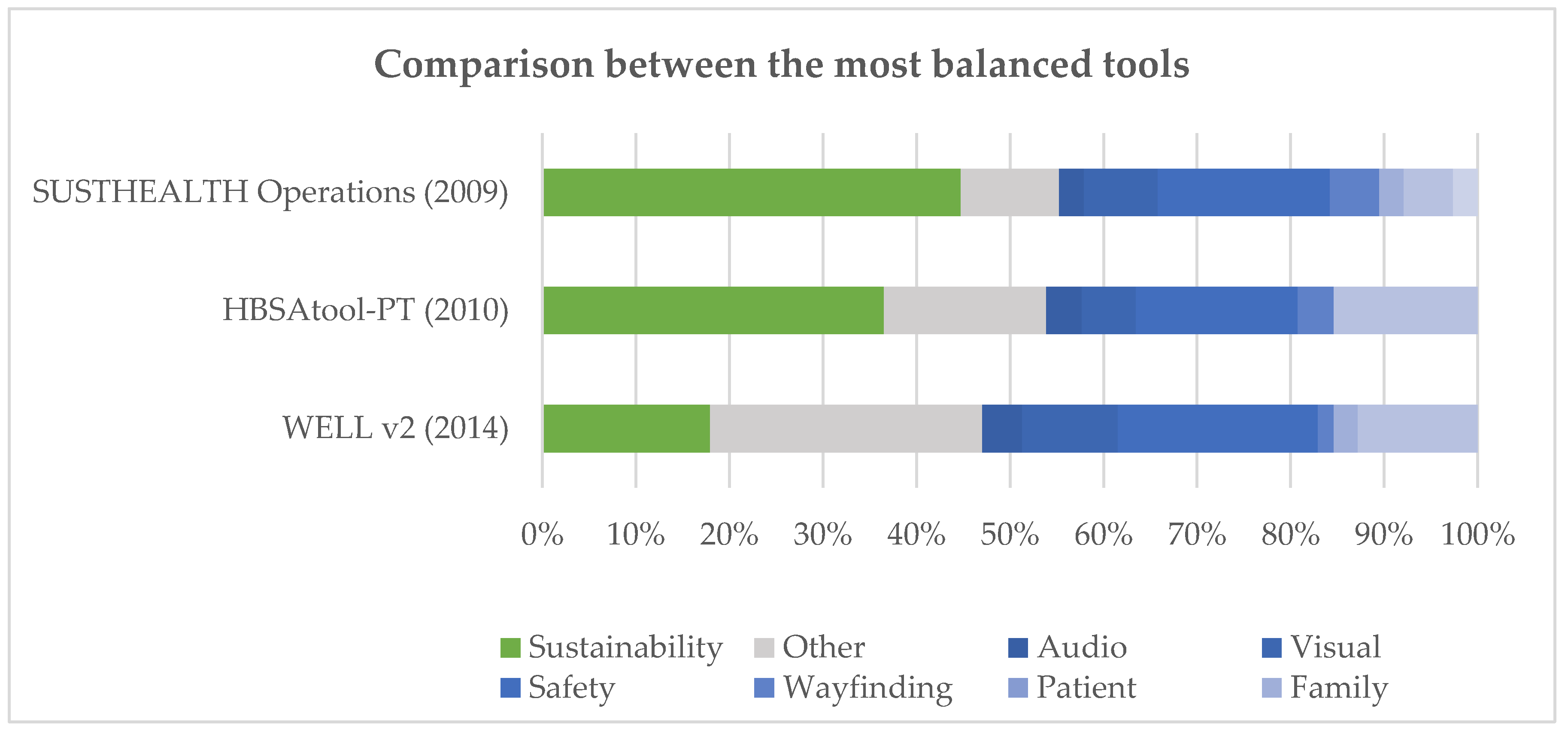
4.2. Health and Sustainability Balance
5. Conclusions
5.1. Innovation/Originality
5.2. Impacts for Research
5.3. Future Development
5.4. Limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Li, P.; Froese, T.M.; Brager, G. Post-occupancy evaluation: State-of-the- art analysis and state-of-the-practice review. Build. Environ. 2018, 133, 187–202. [Google Scholar] [CrossRef]
- Preiser, W.F.E.; Rabinowitz, H.Z.; White, E.T. Postoccupancy Evaluation; Van Nostrand Reinhold: New York, NY, USA, 1988. [Google Scholar]
- Connellan, K.; Gaardboe, M.; Riggs, D.; Due, C.; Reinschmidt, A.; Mustillo, L. Stressed spaces: Mental health and architecture. Health Environ. Res. Des. J. 2013, 6, 127–168. [Google Scholar] [CrossRef]
- Cooper, B.A.; Ahrentzen, S.; Hasselkus, B.R. Post-occupancy evaluation: An environment-behaviour technique for assessing the built environment. Can. J. Occup. Ther. 1991, 58, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Woon, N.B.; Mohammad, I.S.; Baba, M.; Mei, J.L.Y.; Zainol, N.N.; Nazir, A.O. Critical Success Factors for Post Occupancy Evaluation of Hospital Building Performance. J. Teknol. (Sci. Eng.) 2014, 71, 161–166. [Google Scholar]
- Costa, P. Valutare L’architettura. Ricerca Sociologica e Post-Occupancy Evaluation; Franco Angeli: Milano, Italy, 2014. [Google Scholar]
- Meir, I.A.; Garb, Y.; Jiao, D.; Cicelsky, A. Post-Occupancy Evaluation: An Inevitable Step Toward Sustainability. Adv. Build. Energy Res. 2009, 3, 189–219. [Google Scholar] [CrossRef]
- Preiser, W.F.E.; Vischer, J. (Eds.) Assessing Building Performance; Butterworth-Heinemann: Oxford, UK, 2005. [Google Scholar]
- Candido, C.; Kim, J.; De Dear, R.; Thomas, L. BOSSA: A multidimensional post-occupancy evaluation tool. Build. Res. Inf. 2016, 42, 214–228. [Google Scholar] [CrossRef]
- Preiser, W.F.E. Post-occupancy evaluation: How to make buildings work better’. Facilities 1995, 13, 19–28. [Google Scholar] [CrossRef]
- Zeisel, J. Towards a POE paradigm. In Building Evaluation; Preiser, W., Ed.; Plenum: New York, NY, USA, 1989; pp. 167–180. [Google Scholar]
- Simeone, D.; Fioravanti, A. An ontology-based system to support agent-based simulation of building use. J. Inf. Technol. Construct. (ITcon) 2012, 17, 258–270. [Google Scholar]
- Steinke, C.; Webster, L.; Fontaine, M. Evaluating Building Performance in Healthcare Facilities: An Organizational Perspective. Health Environ. Res. Des. J. 2010, 3, 63–83. [Google Scholar] [CrossRef]
- Paraskevopoulou, A.T.; Kamperi, E. Design of hospital healing gardens linked to pre-or post-occupancy research findings. Front. Archit. Res. 2018, 7, 395–414. [Google Scholar] [CrossRef]
- Heinzerling, D.; Schiavon, S.; Webster, T.; Arens, E. Indoor environmental quality assessment models: A literature review and a proposed weighting and classification scheme. Build. Environ. 2013, 70, 210–222. [Google Scholar] [CrossRef]
- Ulrich, R.S. View Through a Window May Influence Recovery from Surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.B.; Choi, Y.S.; Quan, X.; Joseph, A. A Review of the Research Literature on Evidence-Based Healthcare Design. Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Berry, L.L.; Quan, X.; Parish, J.T. A Conceptual Framework for the Domain of Evidence-Based Design. Health Environ. Res. Des. J. 2010, 4, 95–114. [Google Scholar] [CrossRef]
- Quan, X.; Anjali, J. Developing Evidence-based Tools for Designing and Evaluating Hospital Inpatient Rooms. J. Int. Des. 2017, 42, 19–38. [Google Scholar] [CrossRef]
- Ferrante, T. Design enhancing instruments: Post Occupancy Evaluation in Hospice Design. Teche 2013, 6, 125–132. [Google Scholar]
- Elf, M.; Nordin, S.; Wijk, H.; Mckee, K.J. A Systematic Review of the Psychometric Properties of Instruments for Assessing the Quality of the Physical Environment in Healthcare. J. Adv. Nurs. 2017, 73, 2796–2816. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.d.F.; Mateus, R.; Bragança, L. Healthcare Building Sustainability Assessment tool—Sustainable Effective Design criteria in the Portuguese context. Environ. Impact Assess. Rev. 2017, 67, 49–60. [Google Scholar] [CrossRef]
- Codinhoto, R.; Tzortzopoulos, P.; Kagioglou, M.; Aouad, G.; Cooper, R. The Effects of the Built Environment on Health Outcomes. Health and Care Infrastructure Research and Innovation Centre (HaCiCR) Research Report. 2008. Available online: http://www.haciric.org/static/pdf/publications/634202246063608588_The.pdf (accessed on 4 February 2019).
- Mills, G.R.W.; Phiri, M.; Erskine, J.; Price, D.F.A. Rethinking healthcare building design quality: An evidence-based strategy. Build. Res. Inf. 2015, 43, 499–515. [Google Scholar] [CrossRef]
- Latimer, H.S.; Gutknecht, H.; Hardesty, K. Analysis of Hospital Facility Growth: Are We Super-Sizing Healthcare? HERD 2008, 1, 70–88. [Google Scholar] [CrossRef] [PubMed]
- Capolongo, S. Social aspects and well-being for improving healing processes’ effectiveness. Ann. Ist Super Sanità 2016, 52, 11–14. [Google Scholar] [CrossRef][Green Version]
- D’Alessandro, D.; Tedesco, P.; Rebecchi, A.; Capolongo, S. Water use and water saving in Italian hospitals. A preliminary investigation. Ann. Ist Super Sanità 2016, 52, 56–62. [Google Scholar] [CrossRef]
- Day, J.K.; O’Brien, W. Oh behave! Survey stories and lessons learned from building occupants in high-performance buildings. Energy Res. Soc. Sci. 2017, 3, 111–120. [Google Scholar] [CrossRef]
- Donabedian, A. An Introduction to Quality Assurance in Health Care; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- JCI. Standard Joint Commission International per l’Accreditamento degli Ospedali. JCI, 2014. Available online: https://www.jcrinc.com/assets/1/14/EBJCIH14I_Sample_Pages.pdf (accessed on 4 February 2019).
- Malkin, J. The business case for creating a healing environment. Bus. Brief. Hosp. Eng. Facilit. Manag. 2003, 1, 32–36. [Google Scholar]
- Macmillan, S. Added value of good design. Build. Res. Inf. 2006, 34, 257–271. [Google Scholar] [CrossRef]
- Zhao, Y.; Mourshed, M. Design indicators for better accommodation environments in hospitals: inpatients’ perceptions. Intell. Build. Int. 2012, 4, 199–215. [Google Scholar] [CrossRef]
- Fink, A. Conducting Research Literature Reviews: From Paper to the Internet; SAGE: London, UK, 1998. [Google Scholar]
- Pati, D.; Lorusso, L.N. How to Write a Systematic Review of the Literature. HERD 2017, 11, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Hampt, A.; Harris, P.; Maxwell, M. The Health Impacts of the Design of Hospital Facilities on Patient Recovery and Wellbeing, and Staff Wellbeing: A Review of the Literature Centre for Primary Health Care and Equity; University of New South Wales: Sydney, Australia, 2008; Available online: https://www.swslhd.health.nsw.gov.au/populationhealth/PH_environments/pdf/Rpt_Liverpool_Redev_Design_Impact.pdf (accessed on 4 February 2019).
- Brambilla, A.; Rebecchi, A.; Capolongo, S. Evidence Based Hospital Design. A literature review of the recent publications about the EBD impact of built environment on hospital occupants’ and organizational outcomes. Ann Ig 2019, 31. [Google Scholar] [CrossRef]
- Xuan, X. Effectiveness of indoor environment quality in LEED-certified healthcare settings. Indoor Built Environ. 2015, 1–13. [Google Scholar] [CrossRef]
- Deuble, M.P.; De Dear, R.J. Green occupants for green buildings: The missing link? Build. Environ. 2012, 56, 21–27. [Google Scholar] [CrossRef]
- Capolongo, S.; Buffoli, M.; di Noia, M.; Gola, M.; Rostagno, M. Current scenario analysis. In Improving Sustainability During Hospital Design and Operation: A Multidisciplinary Evaluation Tool; Capolongo, S., Bottero, M.C., Buffoli, M., Lettieri, E., Eds.; Springer: Cham, Switzerland, 2015; pp. 11–22. [Google Scholar] [CrossRef]
- Keeney, R.L. Identifying, prioritizing, and using multiple objectives. Eur. J. Decis. Process 2013, 1, 45–67. [Google Scholar] [CrossRef]
- Podvezko, V. The comparative analysis of MCDA Methods SAW and COPRAS. Inzinerine Ekon.-Eng. Econ. 2011, 22, 134–146. [Google Scholar] [CrossRef]
- Saaty, T.L. Multicriteria Decision Making—The Analytic Hierarchy Process. Planning, Priority Setting, Resource Allocation; RWS Publishing: Pittsburgh, PA, USA, 1988. [Google Scholar]
- Harputlugil, T.; Gultekin, A.T.; Prins, M. Architectural design quality assessment based on analytic hierarchy process: A case study. Metu Jfa 2014, 2, 139–161. [Google Scholar] [CrossRef]
- Watson, K.J.; Whitley, T. Applying Social Return on Investment (SROI) to the built environment. Build. Res. Inf. 2017, 45, 875–891. [Google Scholar] [CrossRef]
- Gola, M.; Settimo, G.; Capolongo, S. Indoor air in healing environments: Monitoring chemical pollution in inpatient rooms. Facilities 2019. in pres. [Google Scholar] [CrossRef]
- Mosca, E.I.; Herssens, J.; Rebecchi, A.; Froyen, H.; Capolongo, S. “Design for All” Manual: From Users’ Needs to Inclusive Design Strategies. Adv. Intell. Syst. Comput. 2019, 824, 1724–1734. [Google Scholar]
- Wilson, E. Biophilia; Harvard University Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Nejati, A.; Shepley, M.; Rodiek, S.; Lee, C.; Varni, J. Restorative Design Features for Hospital Staff Break Areas: A Multi-Method Study. HERD 2016, 9, 16–35. [Google Scholar] [CrossRef] [PubMed]
- Minton, C.; Batten, L. Rethinking the intensive care environment: Considering nature in nursing practice. J. Clin. Nurs. 2016, 25, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Astley, P.; Capolongo, S.; Gola, M.; Tartaglia, A. Operative and design adaptability in healthcare facilities. Technè 2015, 9, 162–170. [Google Scholar] [CrossRef]
- Jiang, S.; Verderber, S. On the Planning and Design of Hospital Circulation Zones. HERD 2016, 10, 124–146. [Google Scholar] [CrossRef]
- Hurtley, C. (Ed.) Night Noise Guidelines for Europe; WHO Regional Office for Europe: Copenaghen, Denmark, 2009; ISBN 978 92 890 4173 7. [Google Scholar]
- Jayakaran, T.G.; Rekha, C.V.; Annamalai, S.; Baghkomeh, P.N.; Sharmin, D.D. Preferences and choices of a child concerning the environment in a pediatric dental operatory. Dent. Res. J. 2017, 14, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Oppio, A.; Buffoli, M.; Dell’Ovo, M.; Capolongo, S. Addressing decisions about new hospitals’ siting: A multidimensional evaluation approach. Ann Ist Super Sanità 2016, 52, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Medical Architecture, Edge Lane, Liverpool Design 4 Future Climate Project, Final Report, 2012. Available online: https://www.arcc-network.org.uk/wp-content/D4FC/D4FC25-Edge-Lane-full-report.pdf (accessed on 10 March 2019).
- BRE, BREEAM In-Use International Technical Manual SD221, Version: 2, 2016. Available online: https://www.breeam.com/discover/technical-standards/breeam-in-use/ (accessed on 4 February 2019).
- Bernardi, E.; Carlucci, S.; Bohne, R.A. An Analysis of the Most Adopted Rating Systems for Assessing the Environmental Impact of Buildings. Sustainability 2017, 9, 1226. [Google Scholar] [CrossRef]
- Phiri, M.; Chen, B. Sustainability and Evidence-Based Design in the Healthcare Estate; SpringerBrief in Applied Sciences and Technologies: London, UK, 2014. [Google Scholar] [CrossRef]
- USGBC, LEED v4 for Building Operations and Maintenance, 2018. Available online: https://www.usgbc.org/resources/leed-v4-building-operations-and-maintenance-current-version (accessed on 4 February 2019).
- Buffoli, M.; Gola, M.; Rostagno, M.; Capolongo, S.; Nachiero, D. Making hospitals healthier: How to improve sustainability in healthcare facilities. Ann Ig. 2014, 26, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Japan Sustainable Building Consortium (JSBC) and Institute for Building Environment and Energy Conservation (IBEC), CASBEE for Building. Available online: http://www.ibec.or.jp/CASBEE/english/toolsE_building.htm (accessed on 4 February 2019).
- Center for Maximum Potential Building Systems and Practice Greenhealth, Green Guide for Healthcare—Best Practices for Creating High Performance Healing Environment. Version 2.2 Operations Sections, 2008. Available online: httpp://www.gghc.org (accessed on 4 February 2019).
- Green Building Council of Australia (GBCA), Green Star—Performance v1.2, 2017. Available online: https://new.gbca.org.au/green-star/rating-system/ (accessed on 4 February 2019).
- Center Health Design (CHD), Community Health Center Facility Evaluation Tool, 2017. Available online: https://www.healthdesign.org/community-health-center-facility-evaluation-tool-pdf-version (accessed on 4 February 2019).
- Candido, C.; Thomas, L.; Haddad, S.; Zhang, F.; Mackey, M.; Ye, W. Designing activity-based workspaces: Satisfaction, productivity and physical activity. Build. Res. Inf. 2019, 47, 275–289. [Google Scholar] [CrossRef]
- Gann, D.M.; Salter, A.J.; Whyte, J.K. Design Quality Indicator as a tool for thinking. Build. Res. Inf. 2003, 31, 318–333. [Google Scholar] [CrossRef]
- Edward Williams Architects, Company Report and Selected Projects, 2016. Available online: https://cdn.edwardwilliamsarchitects.com/files/EWA_WEBBRO_sept16.pdf?mtime=20160921164413 (accessed on 10 March 2019).
- Phiri, M. Design Tools for Evidence-Based Healthcare Design; Routledge: New York, NY, USA, 2015. [Google Scholar]
- Ghazali, R.; Abbas, M.Y. Assessment of Healing Environment in Paediatric Wards. Procedia Soc. Behav. Sci. 2012, 38, 149–159. [Google Scholar] [CrossRef]
- Department of Health, Achieving Excellence Design Evaluation Toolkit (AEDET Evolution) and A Staff and Patient Environment Calibration Tool (ASPECT), 2008. Available online: https://webarchive.nationalarchives.gov.uk (accessed on 4 February 2019).
- Foureur, M.J.; Sheehy, A.; Forbes, I.F.W.; Davis, D.L.; Pandolfo, B.; Fenwick, J.; Verghese, G.; Leap, N.; Homer, C.S.E. The BUDSet Tool: Birthing Unit Design Spatial Evaluation Tool (Version 2); Centre for Midwifery Child and Family Health, University of Technology Sydney: Sydney, Australia, 2010. [Google Scholar]
- Buffoli, M.; Capolongo, S.; Di Noia, M.; Gherardi, G.; Gola, M. Healthcare sustainability evaluation systems. In Improving Sustainability During Hospital Design and Operation: A Multidisciplinary Evaluation Tool; Capolongo, S., Bottero, M.C., Buffoli, M., Lettieri, E., Eds.; Springer: Cham, Switzerland, 2015; pp. 23–30. [Google Scholar] [CrossRef]
- Anthes, E. The Office Experiment: Can Science Build the Perfect Workspace? Nature 2016, 537, 294–296. [Google Scholar] [CrossRef]
- International Well Building Institute (IWBI). Available online: https://www.wellcertified.com (accessed on 4 February 2019).
- Constitution of the World Health Organization; World Health Organization: Geneva, Switzerland, 1948; Available online: http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?ua=1 (accessed on 4 February 2019).
- Miller, N.; Spivey, J.; Florance, A. Does Green Pay Off? J. Real Estate Portf. Manag. 2008, 14, 385–400. [Google Scholar] [CrossRef]
- Weisz, U.; Haas, W.; Pelikan, J.M.; Schmied, H. Sustainable Hospitals: A Socio-Ecological Approach. GAIA 2011, 20, 191–198. [Google Scholar] [CrossRef]
- Gou, Z. Editorial Human Factors in Green Building: Building Types and Users’ Needs. Buildings 2019, 9, 17. [Google Scholar] [CrossRef]
- Huisman, E.R.C.M.; Morales, E.; van Hoof, J.; Kort, H.S.M. Healing environment: A review of the impact of physical environmental factors on users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef]
- Alvaro, C.; Wilkinson, A.J.; Gallant, S.N.; Kostovski, D.; Gardner, P. Evaluating Intention and Effect: The Impact of Healthcare Facility Design on Patient and Staff Well-Being. HERD 2016, 9, 82–104. [Google Scholar] [CrossRef] [PubMed]
- Faroldi, E.; Fabi, V.; Vettori, M.P.; Gola, M.; Brambilla, A.; Capolongo, S. Health tourism and thermal heritage. Assessing Italian Spas with innovative multidisciplinary tools. Tour. Anal. 2019, in press. [Google Scholar] [CrossRef]
- Crawley, D.; Aho, I. Building environmental assessment methods: Applications and development trends. Build. Res. Inf. 1999, 27, 300–308. [Google Scholar] [CrossRef]
| Keywords search string: | “HOSPITAL” or “HEALTHCARE ENVIRONMENT” or “HEALTHCARE BUILDING” or “HEALTHCARE FACILITIES” and “QUALITY” and “DESIGN” or “ARCHITECTURE or “BUILT ENVIRONMENT” or “PHYSICAL SPACE” |
| Eligibility criteria: | Exclusion of fields where the search terms have a different meaning, i.e., Computer Science (software architecture) and Biology (bone architecture, cells design) fields for risk of biases |
| n | Name | Acronym |
|---|---|---|
| 1 | Building Research Establishment Environmental Assessment Method | BREEAM |
| 2 | Leadership in Energy and Environmental Design | LEED |
| 3 | Comprehensive Assessment System for Building Environment Efficiency | CASBEE |
| 4 | Green Star | GS |
| 5 | A Staff and Patient Environment Calibration Toolkit (plug-in of AEDET) | ASPECT |
| 6 | Achieving Excellence Design Evaluation Toolkit | AEDET |
| 7 | Green Guide for Healthcare | GGHC |
| 8 | Sustainable High Quality Healthcare | SUSTHEALTH |
| 9 | Birthing Unit Design Spatial Evaluation Tool 2.0 | BUDSET |
| 10 | Healthcare Building Sustainability Assessment tool | HBSA |
| 11 | Design Quality Indicator | DQI |
| 12 | Well Building Standard | WELL |
| 13 | Community Health Center Facility Evaluation Tool | CHD-CHC |
| USA (n = 4; 30%) | UK (n = 4; 30%) | Australia (n = 2; 15%) | Others (n = 3; 23%) |
|---|---|---|---|
| - LEED - GGHC - WELL - CHD-CHC | - BREEAM - ASPECT - AEDET - DQI | - GS - BUDSET | - CASBEE (Japan) - SUSTHEALTH (Italy) - HBSA (Portugal) |
| Safety Enhancement Topics | n (/131) | % |
|---|---|---|
| Pollution risks | 19 | 15% |
| Risk Management | 16 | 12% |
| Accessibility | 14 | 11% |
| Cleaning | 14 | 11% |
| Indoor Air Quality (IAQ) | 14 | 11% |
| Security | 12 | 9% |
| Education | 10 | 8% |
| Water risks | 8 | 6% |
| Management of emergencies | 6 | 5% |
| Materials | 6 | 5% |
| Layout features | 5 | 4% |
| Smoke | 3 | 2% |
| Technologies | 3 | 2% |
| Outdoor risks | 1 | 1% |
| Visual Environment Topics | n (/119) | % |
|---|---|---|
| Interior design appearance | 30 | 25% |
| Outdoor views | 21 | 18% |
| Lighting control | 15 | 13% |
| Outdoor design appearance | 15 | 13% |
| Artificial light | 12 | 10% |
| Natural light | 10 | 8% |
| Outdoor access | 8 | 7% |
| Light pollution | 5 | 4% |
| Privacy | 3 | 3% |
| Staff and Doctors’ Space Features | n(/76) | % |
|---|---|---|
| Dedicated services | 25 | 34% |
| Flexibility of space | 16 | 22% |
| Dedicated space (work, rest, change) | 15 | 21% |
| Furniture quality | 8 | 11% |
| Transportation management | 8 | 11% |
| Dedicated space for Medical Doctors | 3 | 3% |
| Storage space | 1 | 1% |
| Patient Room Features | n (/46) | % |
|---|---|---|
| Toilets | 12 | 26% |
| Privacy | 9 | 20% |
| Furniture quality | 8 | 17% |
| Nutrition | 7 | 15% |
| Wide space | 6 | 13% |
| Medical utilities | 2 | 4% |
| Overall satisfaction | 2 | 4% |
| Wayfinding Features | n (/47) | % |
|---|---|---|
| Layout legibility | 11 | 23% |
| Indoor signage | 9 | 19% |
| Entrance clarity | 9 | 19% |
| Architectural composition | 4 | 9% |
| Interior finishing/art | 3 | 6% |
| Outdoor signage | 3 | 6% |
| Path distance | 3 | 6% |
| Logistics | 2 | 4% |
| Family/Visitors Space Features | n (/38) | % |
|---|---|---|
| Socialization space | 7 | 18% |
| Community enhancement | 6 | 16% |
| Parking space | 5 | 13% |
| Public transportation accessibility | 4 | 11% |
| Physical activities promotion | 3 | 8% |
| Service proximity | 3 | 8% |
| Furniture qualities | 2 | 5% |
| Landscape qualities | 2 | 5% |
| Night space area | 2 | 5% |
| Nutrition services | 2 | 5% |
| Bike accessibility | 1 | 3% |
| Playground areas | 1 | 3% |
| Audio Environment | n (/21) | % |
|---|---|---|
| Noise level (DbA) | 10 | 48% |
| Materials and layout features | 7 | 33% |
| Music features | 2 | 10% |
| Noise pollution | 1 | 5% |
| Privacy | 1 | 5% |
| Sustainability | n (/313) | % |
|---|---|---|
| Energy consumption | 63 | 20% |
| Water use | 39 | 12% |
| Material sustainability | 28 | 9% |
| Environmental pollution | 24 | 8% |
| Thermal comfort | 24 | 8% |
| Waste management | 23 | 7% |
| Construction choices | 21 | 7% |
| Energy sources | 20 | 6% |
| Site management | 20 | 6% |
| HVAC efficiency | 17 | 5% |
| Management of environmental policies | 16 | 5% |
| Heat island effect reduction | 4 | 1% |
| Passive environmental strategies | 4 | 1% |
| Sustainability education | 3 | 1% |
| Green rating tools | 3 | 1% |
| Transportation sustainability | 2 | 1% |
| Life Cycle Assessment (LCA) | 1 | <1% |
| Lighting efficiency | 1 | <1% |
| Other Topics | n (/154) | % |
|---|---|---|
| Occupants education & services | 27 | 18% |
| Organizational quality | 25 | 16% |
| Maintenance and Facility Management (FM) | 14 | 9% |
| Urban and social integration | 13 | 8% |
| Food services | 9 | 6% |
| Building survey/commissioning | 8 | 5% |
| Design process | 8 | 5% |
| Building appearance | 7 | 5% |
| Innovation/research | 7 | 5% |
| Satisfaction surveys | 6 | 4% |
| Construction process | 5 | 3% |
| Cultural issues | 5 | 3% |
| Materials data & certification | 5 | 3% |
| Transportations | 4 | 3% |
| Costs and budgeting | 3 | 2% |
| Professionals involvement | 3 | 2% |
| Space ratio | 3 | 2% |
| Bonus points | 1 | 1% |
| Regional priority | 1 | 1% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brambilla, A.; Capolongo, S. Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework. Buildings 2019, 9, 76. https://doi.org/10.3390/buildings9040076
Brambilla A, Capolongo S. Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework. Buildings. 2019; 9(4):76. https://doi.org/10.3390/buildings9040076
Chicago/Turabian StyleBrambilla, Andrea, and Stefano Capolongo. 2019. "Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework" Buildings 9, no. 4: 76. https://doi.org/10.3390/buildings9040076
APA StyleBrambilla, A., & Capolongo, S. (2019). Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework. Buildings, 9(4), 76. https://doi.org/10.3390/buildings9040076