Abstract
Quarantine policies during the coronavirus disease 2019 (COVID-19) pandemic prolonged time spent at home, leading to an unintended occurrence of sick building syndrome (SBS) symptoms. The aim of this study was to investigate the prevalence of SBS symptoms among residents in Suzhou, China, during the COVID-19 pandemic. A questionnaire survey was conducted online from February to May 2022. A total of 442 adults were included in this study. The prevalence of SBS symptoms was much higher during the COVID-19 pandemic, and the proportions of general, mucosal, and skin symptoms were 59.3%, 45.5% and 49.1%, respectively. The influences of building characteristics, occupant lifestyle, indoor environment and perception of indoor environment were analysed using a multivariate logistic regression model. Neighbourhood pollutant sources, older residences, non-ownership and humidity indicators were significant risk factors for SBS symptoms. Frequent use of air fresheners was significantly associated with general (adjusted odds ratio (AOR): 4.9, 95% confidence interval (CI: 2.4–10.0), mucosal (AOR: 5.3, 95% CI: 2.4–11.5), and skin symptoms (AOR: 4.6, 95% CI: 1.6–13.1), while the use of disinfectants was significantly correlated with skin symptoms (AOR: 4.0, 95% CI: 1.5–10.7). Residents’ perception of an uncomfortable indoor environment was a significant predictor of general (AOR: 2.2, 95% CI: 1.2–4.0) and mucosal symptoms (AOR: 3.1, 95% CI: 1.6–6.0). The use of air cleaners can reduce the prevalence of general symptoms. An important finding of this study is that the psychological impact of staying at home for a long time was associated with general symptoms (AOR: 1.3, 95% CI: 1.1–1.7), which means that attention should also be paid to the mental health of residents during the COVID-19 pandemic. Although the quarantine period has now ended, our results can still serve as a reference for the impact of the indoor environment on the health of people with SBS, especially for those who stay at home for a long time, such as the elderly.
1. Introduction
Sick building syndrome (SBS) was defined by the World Health Organization in 1983 as a set of symptoms experienced by occupants [1]. SBS is widespread and can occur in many indoor environments, especially in homes where people spend long periods of time indoors. SBS symptoms can be categorised into general symptoms (e.g., fatigue, dizziness and difficulty concentrating), mucosal irritation (e.g., eye irritation, nasal irritation and dry throat) and skin symptoms (e.g., flushed skin, itchy scalp and itchy hands). Although most of these symptoms are temporary, they can further affect occupants’ work performance and learning ability [2,3] and lead to economic losses due to sickness absence and healthcare costs [4].
As it is a complex and multifactorial problem, various factors contribute to the prevalence of SBS symptoms, which can be categorised into two general categories: individual and environmental factors [5]. Individual factors such as gender [6,7,8], age [3,9,10], history of asthma or allergy [11] and smoking status [7] have been widely reported as typical factors for SBS. Emerging evidence indicates that personal psychosocial status [12] and stress levels [9] are strongly associated with SBS symptoms. In addition to individual factors, the occurrence of SBS symptoms is probably related to environmental factors. Dampness in buildings and mould have often been identified as risk factors for SBS symptoms in previous studies [13]. Indoor particulate matters and ultrafine particles were identified as strong predictors of SBS symptoms [11,14,15]. When indoor air monitoring is not possible, occupants’ perception of air quality, odour, noise, etc., is usually utilized as indicators of SBS symptoms. Several studies have found a correlation between SBS and perceived indoor air quality [16,17,18]. In addition, occupant behaviour also plays an important role in indoor air pollution and influences the occurrence of SBS symptoms. For example, indoor smoking [19], cooking [20], burning incense [20], etc., can lead to increased concentrations of indoor air pollutants, which are often associated with an increased incidence of SBS. However, frequent ventilation [21], daily cleaning [10,18] and exposing bedding to sunshine [7,18] have been reported as protective factors.
SBS symptoms are often relieved when occupants leave the building or room but can also be aggravated with the extension of time spent indoors [4]. In December 2019, the outbreak of coronavirus disease (COVID-19) outbreak spread fear worldwide and changed people’s lives. To contain the spread of the disease, governments around the world adopted a series of “social distancing” measures, shutting down businesses and ordering people to stay at home to break the chain of transmission of the virus from person to person [22]. The “stay-at-home” policy resulted in residents spending significantly more time working and living at home [23]. Indoor activities include cooking, smoking and the use of various disinfectants [24,25]. As a result, the quality of the indoor environment and its potential health consequences, referred to as SBS symptoms, have attracted increasing attention [26]. A pilot study conducted in the US evaluated the frequency of SBS symptoms in six employees working from home during the pandemic and found a higher frequency of multiple symptoms [27]. Another study discussed the implications of quarantine measures on eye health associated with SBS and found that the COVID-19 pandemic period led to an increase in patients with dry eyes [28]. However, similar reports remain insufficient, which limits our understanding of people’s health during the COVID-19 pandemic. Furthermore, whether the factors influencing SBS symptoms during the pandemic differ from previous studies remains to be investigated, which could provide recommendations for interventions to reduce the health impact on people during certain periods. In addition, the results can also serve as a reference for measures to improve indoor air quality for people who usually stay at home for long periods of time such as the elderly and housewives.
In 2022, the city of Suzhou, China, experienced a severe epidemic from February to May. Under the quarantine policy, most residents stayed at home, worked or studied, which brought environmental risks from the outdoor environment into homes and may have led to an increase in SBS symptoms. The aim of this study was to determine the prevalence of SBS symptoms among Suzhou residents and to investigate the risk factors associated with SBS during the COVID-19 pandemic. In addition, residents’ behavioural intentions to reduce indoor air pollution and their association with SBS symptoms were investigated.
2. Materials and Methods
2.1. Study Area
Suzhou is a megacity in Jiangsu Province, located in eastern China. Suzhou has a total area of 8657.32 km2square kilometres and a permanent population of 12,748,300 [29]. Figure 1 shows the location of Suzhou city. In 2022, Suzhou experienced a severe COVID-19 pandemic from February to May. During the pandemic, the government imposed a series of measures to contain the virus, such as the “stay at home” order. As a result, most citizens worked or studied from home, which extended the time they spent at home. This study was conducted in Suzhou city from 28 April 28 to 9 May 2022 during the COVID-19 lockdown period.
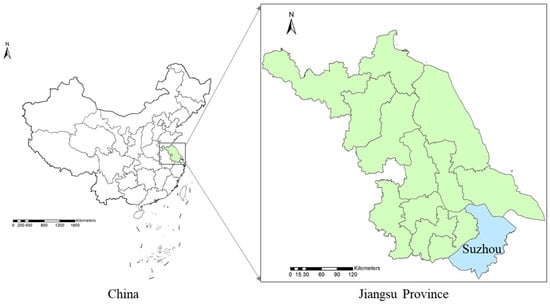
Figure 1.
The location of Suzhou city.
2.2. Questionnaire Survey
A self-administered questionnaire used in previous studies on SBS was modified and used in this study to better reflect the characteristics of Chinese residential buildings, the indoor environment and the lifestyle of residents during the pandemic [18,30,31]. The questionnaire consists of six parts, including information on SBS symptoms, personal characteristics, building characteristics, lifestyle, indoor environment, and behavioural intentions to reduce indoor air pollution. The details of the questionnaire can be found in the Appendix B.
The questions about SBS symptoms in the last three months focused on three groups: general symptoms (fatigue/heavy head, dizziness/nausea, difficulty concentrating, shortness of breath), mucosal (eye irritation, nose irritation, dry throat/cough) and skin symptoms (dry/flushed facial skin, itchy scalp/ears and itchy hands). There were four possible answers for each question: (1) often (every week), (2) sometimes (1–2 weeks), (3) rarely (>2 weeks) and (4) never. Participants were asked to indicate whether their symptoms were relieved when they left the house. Only the responses “often (every week)” and “yes, the symptom is relieved when leaving the house” were defined as the presence of SBS.
Personal demographic characteristics included gender, age, occupation, education, monthly household income and a history of respiratory disease such as diagnosed pneumonia, asthma, etc. Questions on building characteristics included nearby sources of pollution, residential floors, year of construction, dwelling area, and ownership. Occupants’ lifestyles, including the frequency of cleaning, use of disinfectants and air fresheners, pet keeping, exposure to sunlight on bedding and smoking indoors, were investigated. Questions about the indoor environment included the duration of indoor lighting, ventilation, the use of composite flooring, renovation within a year, mould stains, damp patches, water damage and condensation.
Occupants’ perceptions of indoor air pollution and health hazards were analysed using a five-point Likert scale, ranging from completely unpolluted (=1) to heavily polluted (=5) and completely harmless (=1) to very serious (=5). A score equal to or higher than “4” was finally defined as polluted or serious for the perception of indoor air pollution or health hazards, respectively. Indoor comfort was assessed using six questions (lighting, ventilation, noise, air quality, humidity and temperature). Each question was also answered using a five-point Likert scale, ranging from very comfortable to very uncomfortable (very comfortable = 1, very uncomfortable = 5). If one of the indicators was rated as “4” or “5”, indoor comfort was defined as “uncomfortable” and the others as “comfortable”.
One question was related to the psychological effects of prolonged indoor exposure (yes = 1 and no = 0) to find out whether the occupants feel anxious, restless, irritable, etc. The questionnaire contained five questions on occupants’ behavioural intentions to reduce indoor air pollution, including reducing indoor smoking, improving ventilation, using adsorption materials or green plants, detecting indoor air pollutants and treating indoor air pollution.
Considering that most people were working or studying at home during the COVID-19 pandemic, random sampling was conducted by online questionnaires via an online platform (www.wjx.cn). Informed consent was obtained from all participants prior to the survey. In order to avoid deliberately incorrect answers in the online surveys, a completion restriction was set, i.e., a device or IP address could only provide answers once. The IP addresses were also used to determine whether the interviewers were resident in Suzhou. In addition, a question about the district of residence was included and the option “not living in Suzhou” was added. If the responses to the questionnaire were complete and the residents of Suzhou were assessed according to their IP address and district of residence, the questionnaires were considered valid and used for the analysis.
2.3. Statistical Analysis
The collected data were analysed using the Statistical Product and Services Solutions software (SPSS 18.0). The internal consistency or reliability for each set of variables was measured, and the Cronbach’s alpha of each item was above 0.7 in this questionnaire. Chi-square tests were used to compare the prevalence of SBS symptoms in participants with different demographic characteristics. Univariate associations between SBS and building characteristics, lifestyle and indoor environment were analysed. Factors that were significantly associated with SBS symptoms (p < 0.05) were selected for the logistic regression model (forward selection with likelihood ratio statistics). The outcome variable was treated as binary, i.e., whether it had a particular symptom (0 or 1). Confounding factors such as age, gender and education were included in the model as independent variables, as were other factors. Results were presented as adjusted odds ratios (AORs) and 95% confidence intervals (CIs), with a p < 0.05 considered statistically significant. Differences in behavioural intentions to reduce indoor air pollution between residents with different SBS symptoms were analysed using a chi-square test.
3. Results
3.1. Demographic Information of the Participants
A total of 510 completed questionnaires were collected, of which 442 were included after excluding incorrect answers. The overall response rate was 86.67%. The sample size was consistent with the minimum sample size (Nn = 384) for random sampling calculated by Equation (1) [32]. Details of the participants’ demo-graphic characteristics are presented in Table 1. In total, 54.8 of the 442 participants were women, 61.2% were younger than 40 years old and 73.5% had completed an under-graduate degree. Most of the participants worked for private companies (32.1%) or as civil servants (27.6%), and 3.2% were housewives. Of the participants, 43.4% had a history of respiratory diseases and 60.4% had a monthly household income of CNY 5000–20,000 (Chinese Yuan, CNY).
N = Z2p(1 − p)/e2,

Table 1.
Characteristics of study participants and distribution of SBS symptom prevalence.
In the above equation, N is the minimum sample size; Z is the Z-value of the positive distribution corresponding to the 95 confidence level, Z = 1.96; p is the probability value, p = 0.5; e is the error value, e = 5%.
3.2. Prevalence of SBS Symptoms
The prevalence of SBS symptoms among Suzhou residents during the COVID-19 pandemic is shown in Figure 2. Of the participants, 59.3%, 45.5% and 49.1% reported general, mucosal and skin SBS symptoms, respectively. Dry throat/cough was the most common symptom (28.9%), followed by fatigue/heavy head (27.6%) and dizziness/nausea (27.4%).
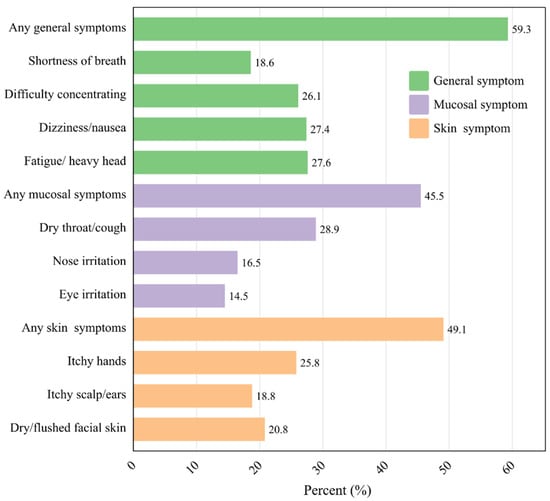
Figure 2.
Prevalence of SBS symptoms among residents.
The results of the chi-square test for the prevalence of SBS symptoms by demographic characteristics are shown in Table 1. There was no significant difference in the prevalence of SBS between men and women. A history of respiratory disease also had no significant effect on SBS symptoms. Other variables, such as age, occupation, education, and household income, were significantly associated with at least one SBS symptom.
3.3. Factors Associated with SBS
The associations between SBS symptoms and building characteristics, occupant lifestyle, indoor environment, perception of indoor environment and psychological effect in the univariate analysis are shown in Table A1. The results of the multivariate logistic regression analysis of the relationship between all influencing factors and the three SBS symptoms are shown in Table 2. It was found that residents living within 200 m of pollution sources had more general and mucosal symptoms. The association between the neighbourhood pollution source and SBS symptoms remained significant even when other factors were taken into account (Table 2). In this study, a significant association was found between the year of construction of the building, dwelling ownership, and the three SBS symptoms. However, in the multivariate logistic regression analysis only the correlations between the year of building construction and the mucosal symptoms and between the home ownership and the skin symptoms remained. Residents on higher floors reported more mucosal and skin symptoms than residents of lower floors. The floor area of the flats was significantly associated with general and skin symptoms. The effects of floor and floor area on SBS were not significant after adjustment for other variables, as shown in Table 2.

Table 2.
Multivariate logistic regression on the association between SBS symptoms and all variables.
Regarding the association between lifestyle and SBS symptoms, the use of air fresheners and disinfectants, keeping pets and smoking indoors were significantly associated with general, mucosal and skin symptoms. When other factors were taken into account, the correlations between the use of air fresheners and the three SBS symptoms remained significant (Table 2). However, the use of disinfectants was only associated with skin symptoms in the multivariate logistic regression model. In the univariate regression analysis, the use of extractor bonnets and air cleaner as well as frequent exposure to sunlight on bedding proved to be protective factors against SBS symptoms. However, this association did not persist when adjusted for other factors, except for the use of air cleaners (Table 2).
This study also found a correlation between the indoor environment and SBS symptoms (Table A1). A short duration of indoor lighting and reduced natural ventilation were significant risk factors for SBS symptoms among residents (p < 0.05). Home renovation within one year and the use of composite flooring were significantly associated with a higher prevalence of SBS. Indicators of dampness (damp stains and water damage) and the presence of rats and mosquitoes/flies were observed as risk factors for different types of SBS. Although the indoor environment had a significant effect on SBS symptoms, only damp stains and water damage were associated with mucosal symptoms in the multivariate logistic regression analysis (Table 2).
In addition, the occupants’ perception of the indoor environment and its relationship with SBS symptoms were analysed. As shown in Table A1, the perception of “indoor air pollution” and the feeling of being uncomfortable in the indoor environment were associated with all types of SBS. Occupants’ perceived indoor environmental comfort remained significantly associated with general and mucosal symptoms even when other variables were taken into account (Table 2).
Following the outbreak of COVID-19 in Suzhou, the government issued a “stay-at-home” order, which significantly increased the amount of time people spent at home. As shown in Figure 3, about 76.2% of participants spent more than 10 h a day at home. Considering the changes in residents’ mental state during the COVID-19 pandemic, the psychological impact of staying at home longer on residents’ SBS symptoms was also investigated. The results showed that residents who were psychologically impaired by staying at home for a longer period of time were more likely to suffer from general SBS symptoms (Table 2).
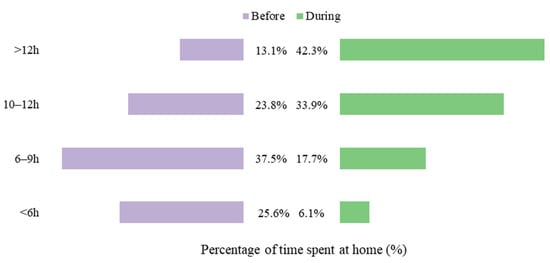
Figure 3.
Percentage of time spent at home before and during the COVID-19 outbreak.
3.4. Behavioural Intentions to Improve Indoor Environmental Quality
To reduce indoor air pollution, 94.6% of residents were willing to restrict smoking indoors, and 78.1% intended to use adsorbent materials (such as activated carbon) or green plants to remove air pollutants. More than half of the participants intended to hire professionals to detect indoor air pollutants (54.1%) and treat indoor air pollution (54.3%). The proportion of people who wanted to improve their indoor ventilation was the lowest (48.2%).
This study investigated the behavioural intentions of people with different SBS symptoms. As shown in Table 3, participants with general symptoms were more likely to improve indoor air quality by limiting indoor smoking, using adsorbent materials or green plants, detecting indoor air pollutants, and controlling indoor air pollution. Significant differences in indoor air pollution treatment behaviours were also found in this study among people with and without mucosal and skin symptoms. Skin symptoms were more likely to be associated with the use of adsorbent materials or green plants to reduce indoor air pollution. Compared to people with SBS symptoms, others were more likely to improve indoor ventilation.

Table 3.
Behavioural intentions related to SBS symptoms.
4. Discussion
This study investigated SBS symptoms in residents of Suzhou, China, during the COVID-19 epidemic. The results (Figure 1) showed that general symptoms were the most prevalent (59.3%), followed by skin (49.1%) and mucosal (45.5%) symptoms. The prevalence of SBS symptoms was much higher than that reported in our previous study conducted in Nanjing, China, in which the prevalence of general, mucosal, and skin symptoms was 14.4%, 9.5% and 5.1%, respectively [33]. During the COVID-19 pandemic, the government imposed a series of containment measures against the virus, such as “stay at home” order, which significantly extended the time people spent at home (Figure 2). These measures may have adverse effect on residents’ health. For example, Napoli et al. found that restrictive measures might act as predisposing factors for eye diseases related to SBS [28]. Roh et al. examined the frequency of six SBS symptoms in 6 employees before and during the pandemic and found that the frequency of several symptoms was higher while working at home [27]. In addition, the stay-at-home policy may also lead to an increase in indoor air pollution as more activities take place indoors (e.g., cooking, smoking indoors and use of disinfectants) [24,34]. Previous studies have shown the association between indoor air pollution and SBS [15,35,36]. Exposure to higher levels of indoor air pollution in homes than in offices during the pandemic may lead to a higher incidence of SBS symptoms [27], and measures to improve indoor air quality should be considered when staying at home for long periods of time.
The building characteristics of the dwellings were associated with the residents’ SBS symptoms. The most important risk factors in this study were living near pollutant sources, year of construction of the building, and dwelling ownership (Table 3). People living in buildings close to pollution sources were more likely to have SBS symptoms. Previous reports have found an association between neighbourhood pollution sources and SBS symptoms. A cross-sectional study conducted in northeast China found that higher exposure to outdoor pollution sources, such as gutters, rubbish stations and noise near homes, may be associated with a higher risk of SBS [20]. Another study compared the association between exposure to the home environment and SBS symptoms in 2010 and 2019. The results showed that living near busy roads was a risk factor for fatigue, skin and throat symptoms [7]. Traffic-related air pollutants such as nitrogen dioxide (NO2) can react with water to form nitrous acid, which has been linked to lung function and respiratory symptoms [37]. A correlation was also found between home ownership and skin symptoms. This finding is consistent with the results of some previous studies [7,38]. Renters often have a higher prevalence of SBS symptoms than homeowners [39]. Possible reasons for this include their social status or the economic value of the dwelling and differences in building maintenance [38], which may encourage residents to improve their living environment [7]. In addition, tenants often face greater psychological stress, which may lead to poorer health and more SBS symptoms [39]. McKee et al. found that instability and insecurity are common feelings among non-homeowners, which can lead to anxiety and discomfort [40]. This may partly explain why a higher prevalence of SBS symptoms was observed among non-homeowners. Older residence is often considered to be a risk factor for SBS [41]. Our study also found that people living in older buildings have a higher risk of SBS. However, other studies have found that newly built homes also contribute to SBS [33,39]. This may be related to other indoor factors, such as chemical residues [39].
An unexpected association was found between the use of air fresheners and SBS. Daily use of air fresheners was significantly associated with a higher risk of general, mucosal and skin symptoms. Several studies have reported an association between the use of fragrant products and symptoms of SBS. A cross-sectional survey of 2143 female students in Tianjin, China, found that the use of air fresheners had a significant dose–response pattern with fatigue, irritation and stuffiness or runny nose [17]. A nationwide study in Japan also found that daily use of deodorants and perfumes was a significant risk factor for SBS symptoms [10]. Another nationwide cross-sectional study of 3335 workers in Japan showed the risk effect of air freshener use on upper respiratory symptoms in occupants [42]. During the use of fragrant products, reactive terpenes can be released and react with ozone to produce secondary organic aerosols, which are harmful to health [17]. Our results are consistent with those of previous studies and confirm that the use of air fresheners is a risk factor for SBS symptoms. In addition, our study found a correlation between the use of disinfectants and skin symptoms. The use of disinfectants usually releases chemicals that can affect the health of residents. However, there are few studies on the negative effects of disinfectant use on residents’ SBS symptoms. This study provides evidence of the potential risk of using disinfectants. Given the widespread use of disinfectants, further studies are needed to investigate their negative effects on human health.
The use of air cleansers was significantly associated with general, mucosal and skin symptoms, although only the use of air purifiers was found to be associated with general symptoms when other influencing factors were taken into account. The use of an air cleaner is generally considered a protective factor against SBS, which is consistent with the results of this study. With the use of air cleansers, the concentrations of indoor air pollutants, such as fine particulate matter, decreased significantly [43]. In addition, some studies have shown that the use of air cleaners can contribute to a better perception of indoor air quality by occupants [44]. The use of air cleaners can therefore help to improve the health of residents.
Dampness-related problems such as damp stains and water damage have been found to be risk factors for mucosal symptoms. Dampness in homes can exacerbate SBS symptoms in residents [13]. A study conducted in Chongqing, China, investigated the perception of humidity and SBS symptoms in 4530 parents and found that water damage and damp stains were risk factors for the perception of humid air and reported mucosal and skin symptoms [18]. Another study investigated the indoor environment in a university dormitory in Sri Lanka and its association with SBS symptoms in students and found that damp stains were a major risk factor for increased fatigue, ocular, throat and skin symptoms [8]. In Japan, Motoko et al. found that condensation from window panes and moisture from the floor at home increased the risk of SBS symptoms in students [45]. In addition, indoor dampness is frequently reported, and moulds, fungi and bacteria are more likely to grow in damp buildings [46], which can have a negative impact on human health.
Occupants’ subjective perception of the indoor environment was a significant factor associated with SBS symptoms. This finding is supported by several previous studies. For example, Qiao et al. observed a strong association between perceived air quality complaints and increased symptom reports [17]. Wang et al. found that adults’ perceptions of odours were related to SBS symptoms [18], and the connection between perceived draught and odours in the workplace and SBS was also found in another study in Thailand [16]. The association between indoor air pollution and SBS symptoms has been confirmed in previous studies [35,36,47], and self-perception questionnaires have been shown to be valuable for investigating indoor air quality and SBS [16]. Our study showed a correlation between perceived uncomfortable indoor environments and general and mucosal symptoms after adjusting for other factors. The results could indicate potentially poor indoor air quality during the COVID-19 pandemic. The subjective perception of indoor air should be taken into account to investigate the effects of air pollution on the health of occupants when indoor air monitoring is not possible.
An important finding of this study is that the psychological effect of staying at home longer was associated with an increased incidence of general symptoms. During the COVID-19 pandemic, the psychological state of occupants may have been influenced by the pandemic response measures (e.g., staying at home). In more recent studies, psychological factors were found to be important for SBS. For example, Dhungana and Chalise found that workers who were under work pressure were more likely to report general and ocular SBS symptoms [9]. A cross-sectional study in Taiwan, China, also found an association between work-related psychosocial stress and SBS symptoms [12]. However, psychological factors were only considered in the study of workers’ SBS symptoms, and the mental status of residents was rarely included in the research of risk factors for SBS symptoms. Our study showed the influence of psychological effects on residents’ SBS symptoms during the epidemic. This suggests that in addition to indoor air quality, attention should also be paid to the mental health of residents, especially when they spend long periods of time at home.
This study investigated occupants’ intention to reduce indoor air pollution through their behaviour. Our results showed that SBS symptoms increased people’s intention to reduce indoor air pollution, especially by reducing indoor smoking and using adsorbent materials. The results of this study suggest that individuals with SBS symptoms may be exposed to indoor air pollution. The importance of occupant behaviour for indoor air quality has been noted previously [48], and indoor air pollution tends to contribute to the onset of SBS [35,36]. This may partly explain why occupants with SBS symptoms had greater behavioural intentions to control indoor air. However, there are few studies that have looked at the differences between the different types of SBS symptoms. Given the strong impact of occupant behaviour on the indoor environment and human health, further studies are needed to investigate occupant behaviour in relation to SBS symptoms.
Our study has some strengths. It examined the SBS symptoms of residents during the COVID-19 epidemic, which leads to a better understanding of public health during a long stay-at-home period. Another strength is that in addition to general individual and home environmental factors, the effect of residents’ psychological state on SBS symptoms was also examined. However, the study has some limitations. The study was only conducted in a single city. In addition, SBS symptoms and information about home environment, lifestyle and other factors were self-reported based on a questionnaire. Residents may overestimate or underestimate their SBS symptoms and the influencing factors. Since most of the residents lived or worked at home during the epidemic, the survey was conducted online, so it is difficult to accompany the completion of the questionnaire face-to-face, which may lead to some bias.
5. Conclusions
In conclusion, the prevalence of SBS symptoms was much higher among residents during the COVID-19 pandemic, especially the general symptoms. Due to the “stay at home” order during the pandemic, staying at home for extended periods of time may increase the risk of SBS symptoms. Therefore, more attention should be paid to people who normally stay at home for long periods of time, such as the elderly.
Neighbourhood pollutant sources, older residences and non-homeowners were significant risk factors for SBS symptoms. Indoor dampness-related problems can increase the risk of SBS symptoms. Thus, residents are encouraged to improve ventilation and cleaning to reduce damp stains, water damage and associated SBS symptoms. Frequent use of air fresheners and disinfectants may increase the risk of SBS symptoms, while the use of air cleaners was found to be a protective factor. The results suggest that maintaining a healthy lifestyle and improving the home environment are beneficial for human health. Future research needs to investigate how to help people change their lifestyle and improve the indoor environment.
Occupants’ perception of uncomfortable indoor environments correlated with general and mucosal symptoms. The psychological impact of prolonged exposure to indoor environments was found to be an emerging risk factor for general symptoms. This study showed the psychological impact on residents’ SBS symptoms during the COVID-19 pandemic. Therefore, more attention should be paid to people’s subjective perception and psychological state in addition to the indoor environment when investigating the factors for SBS symptoms.
Author Contributions
Conceptualization, Z.S.; Data curation, Z.S.; Funding acquisition, Z.S.; Investigation, Q.S., C.W. and J.Y.; Methodology, Z.S.; Software, Q.S.; Supervision, M.X.; Validation, Z.S.; Visualization, C.W.; Writing—original draft, Z.S.; Writing—review and editing, M.X. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the State Key Laboratory of Pollution Control and Resource Reuse Foundation (No. PCRRF22028).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Acknowledgments
We thank all the questionnaire investigators and residents who participated in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Univariate analysis of the association with SBS symptoms.
Table A1.
Univariate analysis of the association with SBS symptoms.
| Variables | Adjusted Odds Ratio (95% CI) | ||||
|---|---|---|---|---|---|
| General Symptoms | Mucosal Symptoms | Skin Symptoms | |||
| Building characteristic | Neighbourhood pollution source | Yes | 36.3 (8.6–154.2) *** | 41.1 (5.6–303.6) *** | 25.5 (6.0–107.9) |
| No | 1.0 | 1.0 | 1.0 | ||
| Residential floor | >18 | 2.4 (1.0–5.4) * | 2.6 (1.1–5.8) * | 2.4 (1.1–5.4) * | |
| 10–18 | 1.8 (0.9–3.4) | 2.7 (1.4–5.2) ** | 2.0 (1.0–3.8) * | ||
| 7–9 | 1.9 (1.0–3.5) | 3.0 (1.6–5.8) ** | 2.5 (1.34–4.66) ** | ||
| 4–6 | 1.42 (0.8–2.7) | 1.1 (0.6–2.1) | 1.83 (1.0–3. 5) | ||
| 1–3 | 1.0 | 1.0 | 1.0 | ||
| Construction year | Before 1980 | 7.9 (3.0–20.6) *** | 6.9 (2.9–16.3) *** | 2.8 (1.2–6.2) * | |
| 1980–1990 | 3.4 (1.7–6.6) *** | 6.74 (3.3–13.9) *** | 4.34 (2.2–8.6) *** | ||
| 1991–2000 | 3.9 (2.7–7.4) *** | 3.7 (1.9–7.2) *** | 2.61 (1.4–4.9) ** | ||
| 2001–2010 | 1.5 (0.8–2.7) | 1.5 (0.8–3.0) | 1.0 (0.6–1.9) | ||
| 2011–now | 1.0 | 1.0 | 1.0 | ||
| Dwelling area | <60 m2 | 2.2 (1.1–4.5) * | 1.6 (0.8–3.2) | 1.9 (1.0–3.8) | |
| 61–90 m2 | 1.6 (1.0–2.8) | 1.6 (1.0–2.7) | 2.1 (1.2–3.5) ** | ||
| 91–120 m2 | 1.1 (0.6–1.9) | 1.3 (0.8–2.3) | 1.5 (0.8–2.5) | ||
| >120 m2 | 1.0 | 1.0 | 1.0 | ||
| Ownership | Other | 2.6 (1.8–3.9) *** | 2.7 (1.8–4.0) *** | 2.9 (2.0–4.4) *** | |
| Owned | 1.0 | 1.0 | 1.0 | ||
| Lifestyles | Cleaning frequency | >1/week | 0.5 (0.2–1.2) | 0.9 (0.4–2.1) | 0.7 (0.3–1.6) |
| 1/week | 3.3 (0.6–2.9) | 1.5 (0.7–3.4) | 1.2 (0.6–2.7) | ||
| 1/2–4 days | 1.4 (0.60–3.3) | 2.0 (0.8–4.6) | 1.1 (0.5–2.4) | ||
| Everyday | 1.0 | 1.0 | 1.0 | ||
| Use of disinfectant | Everyday | 9.3 (5.1–19.2) *** | 7.9 (4.0–15.6) *** | 9.8 (4.8–19.8) *** | |
| 1/2–4 days | 9.0 (5.0–16.3) *** | 8.6 (4.5–16.4) *** | 13.1 (6.7–25.5) *** | ||
| 1/week | 8.0 (3.6–17.9) *** | 6.6 (2.9–14.9) *** | 17.0 (7.2–40.4) *** | ||
| >1/week | 1.0 | 1.0 | 1.0 | ||
| Use of air freshener | Everyday | 10.9 (5.7–21.0) *** | 11.3 (5.6–22.8) *** | 12.2 (5.8–25.4) *** | |
| 1/2–4 days | 8.6 (4.8–15.5) *** | 7.5 (3.9–14.6) *** | 16.0 (7.9–32.5) *** | ||
| 1/week | 5.6 (2.6–12.1) *** | 9.6 (4.2–21.9) *** | 18.5 (7.7–44.4) *** | ||
| >1/week | 1.0 | 1.0 | 1.0 | ||
| Use of kitchen hood | Yes | 0.4 (0.2–0.6) *** | 0.5 (0.3–0.7) *** | 0.6 (0.4–0.9) * | |
| No | 1.0 | 1.0 | 1.0 | ||
| Use of air cleaner | Yes | 0.4 (0.2–0.6) *** | 0.4 (0.3–0.7) *** | 0.4 (0.2–0.6) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Pet keeping | Yes | 2.2 (1.5–3.4) *** | 1.5 (1.0–2.2) * | 2.0 (1.3–2.9) ** | |
| No | 1.0 | 1.0 | 1.0 | ||
| Exposing bedding to the sun | Yes | 0.3 (0.2–0.5) *** | 0.5 (0.3–0.7) ** | 0.5 (0.3–0.7) *** | |
| No | 1.0 | 1.0 | 1.0 | ||
| Indoor smoking | Often | 3.1 (1.9–5.2) *** | 2.4 (1.5–3.9) *** | 1.5 (0.9–2.3) | |
| Occasionally | 2.8 (1.7–4.5) *** | 2.1 (1.3–3.3) ** | 1.7 (1.1–2.6) * | ||
| No | 1.0 | 1.0 | 1.0 | ||
| Indoor environment | Indoor light duration | <2 h | 2.8 (1.6–4.9) *** | 2.1 (1.3–3.5) ** | 3.6 (2.1–6.0) *** |
| 3–6 h | 1.6 (1.0–2.5) * | 1.5 (0.9–2.3) | 1.6 (1.0–2.5) * | ||
| >6 h | 1.0 | 1.0 | 1.0 | ||
| Ventilation | <6 h/day | 1.6 (1.1–2.4) * | 1.7 (1.1–2.5) * | 1.3 (0.9–2.0) | |
| ≥6 h/day | 1.0 | 1.0 | 1.0 | ||
| Composite floor board | Yes | 1.6 (1.1–2.4) * | 1.7 (1.2–2.6) ** | 1.5 (1.1–2.3) * | |
| No | 1.0 | 1.0 | 1.0 | ||
| Renovation within a year | Yes | 1.8 (1.2–2.7) ** | 1.4 (1.0–2.1) | 2.0 (1.3–2.9) ** | |
| No | 1.0 | 1.0 | 1.0 | ||
| Mould spots | Yes | 1.1 (0.8–1.7) | 0.8 (0.5–1.2) | 1.3 (0.9–1.9) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Damp stains | Yes | 1.3 (0.9–1.9) | 1.5 (1.0–2.2) * | 1.0 (0.7–1.5) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Water damage | Yes | 1.4 (0.9–2.0) | 1.8 (1.2–2.6) ** | 1.2 (0.8–1.7) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Condensation | Yes | 1.1 (0.7–1.6) | 1.1 (0.7–1.6) | 1.3 (0.9–1.9) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Cockroaches | Yes | 1.3 (0.9–1.9) | 1.2 (0.8–1.7) | 1.2 (0.8–1.8) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Rats | Yes | 3.0 (1.9–4.6) *** | 1.7 (1.2–2.6) ** | 2.1 (1.4–3.2) *** | |
| No | 1.0 | 1.0 | 1.0 | ||
| Mosquitoes /flies | Yes | 0.6 (0.4–0.9) ** | 0.6 (0.4–0.8) ** | 0.8 (0.5–1.2) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Perception of indoor environment | Indoor air pollution | Yes | 2.2 (1.3–3.6) ** | 1.9 (1.2–3.0) ** | 2.3 (1.4–3.6) ** |
| No | 1.0 | 1.0 | 1.0 | ||
| Health hazards of indoor air pollution | Yes | 1.1 (0.7–1.7) | 1.1 (0.8–1.8) | 1.1 (0.7–1.6) | |
| No | 1.0 | 1.0 | 1.0 | ||
| Indoor environmental comfort | No | 5.1 (3.1–8.4) *** | 6.4 (3.5–11.4) *** | 4.5 (2.7–7.6) *** | |
| Yes | 1.0 | 1.0 | 1.0 | ||
| Psychological effect | Yes | 2.2 (1.4–3.5) ** | 1.5 (0.9–2.2) | 1.4 (0.9–2.1) | |
| No | 1.0 | 1.0 | 1.0 | ||
* p < 0.05, ** p < 0.01, *** p < 0.001.
Appendix B
Questionnaire
PART 1. Building characteristics
- (1)
- Is there any pollution source within 200 m of your house?
□ Yes □ No
- (2)
- On which floor do you live?
□ 1–3 floor □ 4–6 floor □ 7–9 floor □ 10–18 floor □ >18 floor
- (3)
- The construction year of your residential building.
□ Before 1990 □ 1991–2000 □ 2001–2010 □ 2011–now
- (4)
- The dwelling area of your home.
□ <60 m2 □ 61–90 m2 □ 91–120 m2 □ >120 m2
- (5)
- Do you own your home?
□ Owned □ Other
PART 2. Occupants’ lifestyle
- (6)
- How often do you clean your home?
□ Everyday □ 1/2–4 days □ 1/week □ >1/week
- (7)
- How often do you use the disinfectant?
□ Everyday □ 1/2–4 days □ 1/week □ >1/week
- (8)
- How often do you use the air freshener?
□ Everyday □ 1/2–4 days □ 1/week □ >1/week
- (9)
- Do you use an extractor hood when cooking?
□ Yes □ No
- (10)
- Do you use an air cleaner?
□ Yes □ No
- (11)
- Do you have pets in your home?
□ Yes □ No
- (12)
- Do you often expose your bedding to the sun?
□ Yes □ No
- (13)
- Does anyone smoke in your home?
□ Often □ Occasionally □ No
PART 3. Indoor environment
- (14)
- How long does the light in your house last?
□ <2 h □ 3–6 h □ >6 h
- (15)
- How long do you ventilate every day?
□ <6 h □ ≥6 h
- (16)
- Do you use composite flooring?
□ Yes □ No
- (17)
- Have you carried out any renovation work in your home in the last year?
□ Yes □ No
- (18)
- Did you see any mould spot in your house before?
□ Yes □ No
- (19)
- Did you see any damp stain in your house before?
□ Yes □ No
- (20)
- Did you see condensation on the window panels in your home in winter before?
□ Yes □ No
- (21)
- Did you see any cockroaches in your home before?
□ Yes □ No
- (22)
- Did you see any rats in your house before?
□ Yes □ No
- (23)
- Did you see any mosquitos/flies in your house before?
□ Yes □ No
PART 4. Perception of indoor environment and psychological effects of staying at home for a long time.
- (24)
- In your opinion, how polluted is the air in your home?
□ Completely unpolluted □ Unpolluted □ Generally □ Polluted □ Heavily polluted
- (25)
- Do you think that indoor air pollution is harmful to humans?
□ Completely harmless □ Harmless □ Generally □ Serious □ Very serious
- (26)
- How do you feel about the comfort of the indoor environment? Please complete the following form.

Table A2.
Indoor environmental comfort.
Table A2.
Indoor environmental comfort.
| Indoor Environment | Very Comfortable | Comfortable | Generally | Uncomfortable | Very Uncomfortable | |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| 1. | Lighting condition | □ | □ | □ | □ | □ |
| 2. | Ventilation | □ | □ | □ | □ | □ |
| 3. | Noise level | □ | □ | □ | □ | □ |
| 4. | Indoor air quality | □ | □ | □ | □ | □ |
| 5. | Humidity | □ | □ | □ | □ | □ |
| 6. | Temperature | □ | □ | □ | □ | □ |
- (27)
- Is your psychological state affected by staying at home for a long time?
□ Yes □ No
PART 5. Behavioural intentions to reduce indoor air pollution
- (28)
- What will you do if indoor air is polluted? Please complete the following form.

Table A3.
Behavioural intentions to reduce indoor air pollution.
Table A3.
Behavioural intentions to reduce indoor air pollution.
| Behavioural Intentions | Yes | No | |
|---|---|---|---|
| 1. | Reducing indoor smoking | □ | □ |
| 2. | Improving ventilation | □ | □ |
| 3. | Using adsorption materials or green plants | □ | □ |
| 4. | Detecting indoor air pollutants | □ | □ |
| 5. | Treating indoor air pollution | □ | □ |
PART 6. SBS symptoms
Please fill in the following form according to your situation and tick the □.

Table A4.
Questions for SBS symptoms.
Table A4.
Questions for SBS symptoms.
| Have You Had Any of the Following Symptoms in the Last Three Months When You Were at Home? | Did the Symptoms Subside When You Left the House? | |||||
|---|---|---|---|---|---|---|
| Often (Every Week) | Sometimes (1–2 Weeks) | Rarely (>2 Weeks) | Never | Yes | No | |
| General symptoms | ||||||
| Fatigue/heavy head | □ | □ | □ | □ | □ | □ |
| Dizziness/nausea | □ | □ | □ | □ | □ | □ |
| Difficulty concentrating | □ | □ | □ | □ | □ | □ |
| Shortness of breath | □ | □ | □ | □ | □ | □ |
| Mucosal symptoms | ||||||
| Dry throat/cough | □ | □ | □ | □ | □ | □ |
| Nose irritation | □ | □ | □ | □ | □ | □ |
| Eye irritation | □ | □ | □ | □ | □ | □ |
| Skin symptoms | ||||||
| Itchy hands | □ | □ | □ | □ | □ | □ |
| Itchy scalp/ears | □ | □ | □ | □ | □ | □ |
| Dry/flushed facial skin | □ | □ | □ | □ | □ | □ |
PART 7. Personal information
- (29)
- Gender
□ Male □ Female
- (30)
- Age
□ 16–25 □ 26–40 □ 41–50 □ 51–60 □ ≥60
- (31)
- Occupation
□ Self-employed □ Housewife □ Employee in private company □ Civil servant
□ Student □ Retiree □ Other
- (32)
- Educational attainment
□ Primary school or less □ Junior high school □ Senior high school
□ University □ Postgraduate
- (33)
- Your household income per month (CNY)
□ ≤5000 □ 5001–10,000 □ 10,001–20,000 □ ≥20,001
- (34)
- Do you have a history of respiratory disease?
□ Yes □ No
References
- WHO. Indoor Air Pollutants: Exposure and Health Effects; EURO Reports and Studies 78; WHO: Copenhagen, Denmark, 1983. [Google Scholar]
- Dorizas, P.V.; Assimakopoulos, M.N.; Santamouris, M. A holistic approach for the assessment of the indoor environmental quality, student productivity, and energy consumption in primary schools. Environ. Monit. Assess. 2015, 187, 259. [Google Scholar] [CrossRef] [PubMed]
- Mansor, A.A.; Abdullah, S.; Ahmad, A.N.; Ahmed, A.N.; Zulkifli, M.F.R.; Jusoh, S.M.; Ismail, M. Indoor air quality and sick building syndrome symptoms in administrative office at public university. Dialogues Health 2024, 4, 100178. [Google Scholar] [CrossRef]
- Sarkhosh, M.; Najafpoor, A.A.; Alidadi, H.; Shamsara, J.; Amiri, H.; Andrea, T.; Kariminejad, F. Indoor Air Quality associations with sick building syndrome: An application of decision tree technology. Build. Environ. 2021, 188, 107446. [Google Scholar] [CrossRef]
- Ghaffarianhoseini, A.; Alwaer, H.; Omrany, H.; Ghaffarianhoseini, A.; Alalouch, C.; Clements-Croome, D.; Tookey, J. Sick building syndrome: Are we doing enough? Archit. Sci. Rev. 2018, 61, 99–121. [Google Scholar] [CrossRef]
- Huo, X.; Sun, Y.; Hou, J.; Wang, P.; Kong, X.; Zhang, Q.; Sundell, J. Sick building syndrome symptoms among young parents in Chinese homes. Build. Environ. 2020, 169, 106283. [Google Scholar] [CrossRef]
- Cheng, H.; Norback, D.; Zhang, H.; Yang, L.; Li, B.; Zhang, Y.; Zhao, Z.; Deng, Q.; Huang, C.; Yang, X.; et al. Home environment exposure and sick building syndrome (SBS) symptoms among adults in southern China: Health associations in 2010 and 2019. Build. Environ. 2024, 248, 111061. [Google Scholar] [CrossRef]
- Marasinghe, S.A.; Sun, Y.; Norback, D.; Adikari, A.M.P.; Mlambo, J. Indoor environment in Sri Lankan university dormitories: Associations with ocular, nasal, throat and dermal symptoms, headache, and fatigue among students. Build. Environ. 2024, 251, 111194. [Google Scholar] [CrossRef]
- Dhungana, P.; Chalise, M. Prevalence of sick building syndrome symptoms and its associated factors among bank employees in Pokhara Metropolitan, Nepal. Indoor Air 2020, 30, 244–250. [Google Scholar] [CrossRef]
- Nakayama, Y.; Nakaoka, H.; Suzuki, N.; Tsumura, K.; Hanazato, M.; Todaka, E.; Mori, C. Prevalence and risk factors of pre-sick building syndrome: Characteristics of indoor environmental and individual factors. Environ. Health Prev. Med. 2019, 24, 77. [Google Scholar] [CrossRef]
- Subri, M.S.M.; Arifin, K.; Sohaimin, M.F.A.M.; Abas, A. The parameter of the Sick Building Syndrome: A systematic literature review. Heliyon 2024, 10, e32431. [Google Scholar] [CrossRef]
- Lu, C.Y.; Tsai, M.C.; Muo, C.H.; Kuo, Y.H.; Sung, F.C.; Wu, C.C. Personal, psychosocial and environmental factors related to sick building syndrome in official employees of Taiwan. Int. J. Environ. Res. Public Health 2018, 15, 7. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Norback, D.; Cheng, H.; Li, B.; Zhang, Y.; Zhao, Z.; Deng, Q.; Huang, C.; Yang, X.; Lu, C.; et al. Dampness and mould in Chinese homes and sick building syndrome (SBS) symptoms—Associations with climate, family size, cleaning and ventilation. Build. Environ. 2023, 245, 1180878. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Yao, M.; He, M.; Shang, W.; Dong, X. Indoor air quality and sick-building syndrome at a metro station in Tianjin, China. Environ. Int. 2024, 187, 1008673. [Google Scholar] [CrossRef]
- Hosseini, M.R.; Godini, H.; Fouladi-Fard, R.; Ghanami, Z.; Ghafoory, N.; Balali, M.; Faridan, M. Comparing classic regression with credit scorecard model for predicting sick building syndrome risk: A machine learning perspective in environmental assessment. Build. Environ. 2024, 253, 111351. [Google Scholar] [CrossRef]
- Surawattanasakul, V.; Sirikul, W.; Sapbamrer, R.; Wangsan, K.; Assavanopakun, P.; Panumasvivat, J. Perceived draught and odors: The key to SBS and indoor environment in hospital administrative offices—The AIRMED project. Build. Environ. 2024, 258, 111592. [Google Scholar] [CrossRef]
- Qiao, R.; Lou, X.; Sun, Y.; Liu, Y. Effects of occupant behaviors on perceived dormitory air quality and sick building syndrome symptoms among female college students. Indoor Air 2022, 32, e13153. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, B.; Yang, Q.; Yu, W.; Wang, H.; Norback, D.; Sundell, J. Odors and sensations of humidity and dryness in relation to sick building syndrome and home environment in Chongqing, China. PLoS ONE 2013, 8, e72385. [Google Scholar] [CrossRef]
- Mizoue, T.; Reijula, K.; Andersson, K. Environmental tobacco smoke exposure and overtime work as risk factors for sick building syndrome in Japan. Am. J. Epidemiol. 2001, 154, 803–808. [Google Scholar] [CrossRef]
- He, Y.; Zhang, S.; Wei, X.; Shang, S.; Wang, Y.; Zhang, R.; Guo, J.; Sun, M.; Li, Y.; Ma, Y. A high environmental composite quality factor score was associated with the risk of sick building syndrome among adults in northeast China. J. Environ. Manag. 2022, 306, 114458. [Google Scholar] [CrossRef]
- Irga, P.J.; Torpy, F.R. Indoor air pollutants in occupational buildings in a sub-tropical climate: Comparison among ventilation types. Build. Environ. 2016, 100, 227. [Google Scholar] [CrossRef]
- Koren, M.; Peto, R. Business disruptions from social distancing. PLoS ONE 2020, 15, e0239113. [Google Scholar] [CrossRef] [PubMed]
- De Haas, M.; Faber, R.; Hamersma, M. How COVID-19 and the Dutch ‘intelligent lockdown’ change activities, work and travel behaviour: Evidence from longitudinal data in the Netherlands. Transp. Res. Perspect. 2020, 6, 100150. [Google Scholar] [CrossRef] [PubMed]
- Mahabee-Gittens, E.M.; Merianos, A.L.; Matt, G.E. Letter to the editor regarding: “An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19)”-Secondhand and Thirdhand Smoke As Potential Sources of COVID-19. Environ. Sci. Technol. 2020, 54, 5309–5310. [Google Scholar] [CrossRef]
- Hosseini, M.R.; Fouladi-Fard, R.; Aali, R. COVID-19 pandemic and sick building syndrome. Indoor Built Environ. 2020, 29, 1181–1183. [Google Scholar] [CrossRef]
- Awada, M.; Becerik-Gerber, B.; Hoque, S.; O’Neill, Z.; Pedrielli, G.; Wen, J.; Wu, T. Ten questions concerning occupant health in buildings during normal operations and extreme events including the COVID-19 pandemic. Build. Environ. 2021, 188, 107480. [Google Scholar] [CrossRef] [PubMed]
- Roh, T.; Moreno-Rangel, A.; Baek, J.; Obeng, A.; Hasan, N.T.; Carrillo, G. Indoor air quality and health outcomes in employees working from home during the COVID-19 pandemic: A pilot study. Atmosphere 2021, 12, 1665. [Google Scholar] [CrossRef]
- Napoli, P.E.; Nioi, M.; Fossarello, M. The “Quarantine Dry Eye”: The lockdown for coronavirus disease 2019 and its implications for ocular surface health. Risk Manag. Healthc. Policy 2021, 14, 1629–1636. [Google Scholar] [CrossRef]
- Suzhou Bureau of Statistics. Suzhou Statistical Yearbook; Suzhou Bureau of Statistics: Suzhou, China, 2023. [Google Scholar]
- Che, W.W.; Tso, C.Y.; Sun, L.; Ip, D.Y.K.; Lee, H.; Chao, C.Y.H.; Lau, A.K.H. Energy consumption, indoor thermal comfort and air quality in a commercial office with retrofitted heat, ventilation and air conditioning (HVAC) system. Energy Build. 2019, 201, 202–215. [Google Scholar] [CrossRef]
- Suzuki, N.; Nakayama, Y.; Nakaoka, H.; Takaguchi, K.; Tsumura, K.; Hanazato, M.; Hayashi, T.; Mori, C. Risk factors for the onset of sick building syndrome: A cross-sectional survey of housing and health in Japan. Build. Environ. 2021, 202, 107976. [Google Scholar] [CrossRef]
- Hao, D. Survey Methods in Social Research, 4th ed.; China Renmin University Press: Beijing, China, 2019. [Google Scholar]
- Shao, Z.; Bi, J.; Yang, J.; Ma, Z. Indoor PM2.5, home environmental factors and lifestyles are related to sick building syndrome among residents in Nanjing, China. Build. Environ. 2023, 235, 110204. [Google Scholar] [CrossRef]
- Dutheil, F.; Baker, J.S.; Navel, V. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020, 263, 114466. [Google Scholar] [CrossRef] [PubMed]
- Takigawa, T.; Wang, B.L.; Sakano, N.; Wang, D.H.; Ogino, K.; Kishi, R. A longitudinal study of environmental risk factors for subjective symptoms associated with sick building syndrome in new dwellings. Sci. Total Environ. 2009, 407, 5223–5228. [Google Scholar] [CrossRef] [PubMed]
- Colton, M.D.; MacNaughton, P.; Vallarino, J.; Kane, J.; Bennett-Fripp, M.; Spengler, J.D.; Adamkiewicz, G. Indoor air quality in green vs conventional multifamily low-income housing. Environ. Sci. Technol. 2014, 48, 7833–7841. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, D.L.; Leaderer, B.P.; Chinn, S.; Burney, P.G. Indoor nitrous acid and respiratory symptoms and lung function in adults. Thorax 2005, 60, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Engvall, K.; Norrby, C.; Bandel, J.; Hult, M.; Norback, D. Development of a multiple regression model to identify multi-family residential buildings with a high prevalence of sick building syndrome (SBS). Indoor Air 2000, 10, 101–110. [Google Scholar] [CrossRef]
- Fu, P.; Zhao, Z.; Norback, D.; Zhang, X.; Yung, K.K.L. Associations between indoor environment and lifestyles and sick building syndrome symptoms among adults in Taiyuan and Urumqi of China. Indoor Air 2022, 32, e13081. [Google Scholar] [CrossRef]
- Mckee, K.; Soaita, A.M.; Hoolachan, J. ‘Generation rent’ and the emotions of private renting: Self-worth, status and insecurity amongst low-income renters. Hous. Stud. 2020, 35, 1468–1487. [Google Scholar] [CrossRef]
- Yau, Y.H.; Phuah, K.S. Indoor air quality study in four Malaysian hospitals for centralized and non-centralized ACMV systems. Air Qual. Atmos. Health 2023, 16, 375–390. [Google Scholar] [CrossRef]
- Azuma, K.; Ikeda, K.; Kagi, N.; Yanagi, U.; Osawa, H. Prevalence and risk factors associated with nonspecific building-related symptoms in office employees in Japan: Relationships between work environment, Indoor Air Quality, and occupational stress. Indoor Air 2015, 25, 499–511. [Google Scholar] [CrossRef]
- Rice, J.L.; Brigham, E.; Dineen, R.; Muqueeth, S.; O’Keefe, G.; Regenold, S.; Koehler, K.; Rule, A.; McCormack, M.; Hansel, N.N.; et al. The feasibility of an air purifier and secondhand smoke education intervention in homes of inner city pregnant women and infants living with a smoker. Environ. Res. 2018, 160, 524–530. [Google Scholar] [CrossRef]
- Cooper, E.; Wang, Y.; Stamp, S.; Burman, E.; Mumovic, D. Use of portable air purifiers in homes: Operating behaviour, effect on indoor PM2.5 and perceived indoor air quality. Build. Environ. 2021, 191, 107621. [Google Scholar] [CrossRef]
- Takaoka, M.; Suzuki, K.; Norback, D. Sick building syndrome among junior high school students in Japan in relation to the home and school environment. Glob. J. Health Sci. 2015, 8, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Nevalainen, A.; Pasanen, A.L.; Niininen, M.; Reponen, T.; Kalliokoski, P.; Jantunen, M.J. The indoor air quality in finnish homes with mold problems. Environ. Int. 1991, 17, 299–302. [Google Scholar] [CrossRef]
- Zhang, X.; Li, F.; Zhang, L.; Zhao, Z.; Norback, D. A Longitudinal Study of Sick Building Syndrome (SBS) among Pupils in Relation to SO2, NO2, O-3 and PM10 in Schools in China. PLoS ONE 2014, 9, e112933. [Google Scholar] [CrossRef]
- Luo, N.; Weng, W.; Xu, X.; Hong, T.; Fu, M.; Sun, K. Assessment of occupant-behavior-based indoor air quality and its impacts on human exposure risk: A case study based on the wildfires in Northern California. Sci. Total Environ. 2019, 686, 1251–1261. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).