1. Introduction
People spend about one-third of their lives sleeping [
1]. Complaints related to difficulty in initiating and maintaining sleep increase with age [
2,
3,
4]. Moreover, thermoregulation during exposure to heat or cold also deteriorates with aging [
5,
6,
7]. The sleep quality of older people is found to be influenced by the surrounding environment and the total sleep time is found to be shorter due to higher temperature in the summer than in other seasons due to longer wakefulness [
8,
9]. This finding is attributed to the fact that older people were unable to not control their surrounding environment during the period of nocturnal sleep in the summer season because they lived independently and sustained themselves in detached old houses in suburban areas. The proportion of older people is currently expanding at its highest rate in Japan [
10]. As a consequence, the necessity for nursing home care is increasing markedly. In urban areas there are many facilities built and run by non-governmental management. In contrast, low-cost social welfare facilities for the aged are managed by local government authorities. Nursing homes for older people are superintended by managers and their indoor environment is controlled by air-conditioning systems. However, not much is known about the thermal environments present around the occupants of these elderly facilities.
In Japan, general buildings must be controlled to comply with the Japanese Standard for Maintenance of Sanitation in Buildings [
11], which specifies that buildings with a gross floor area of more than 3000 m
2 must have an air conditioning facility or a mechanical centrally controlled ventilation system. The Standard for Maintenance of Sanitation in Buildings stipulates 17–28 °C for Ta, 40–70% for Rh, and less than 0.5 m/s for air velocity, irrespective of occupant age or gender, while recommending that adaptive comfort temperature is not dependent on outdoor temperature. The elder care facility is one of the special-purpose buildings which does not need to comply with the Japanese Standard for Maintenance of Sanitation in Buildings. The most-used general thermal comfort standards, ASHRAE Standard 55 [
12] and ISO 7730 [
13], are based on subject experiments in a climatic chamber. Furthermore, there are abundant field studies on the thermal environment and thermal comfort in offices, schools, and residential buildings all over the world [
14]. An adaptive approach to thermal comfort would be based on the findings of thermal comfort surveys conducted in the field [
15]. As a result, people evaluate the climate differently in buildings where they can open windows and influence the indoor thermal climate. Particularly in periods with higher outdoor temperatures, higher indoor temperatures in such buildings are more acceptable than Fanger’s model predicts [
16]. Although adaptive thermal comfort may promote energy savings and occupants’ sensations, the suitable and comfortable temperature for work performance, academic success, daily activities, and behaviors including sleep have not been investigated much. This is because adaptive thermal comfort is not confined to building use, occupant behavior, and other contexts for comfort temperature. Moreover, most respondents to questionnaire surveys are young healthy people in the field study of thermal comfort. Only a few thermal comfort studies have been conducted in nursing home environments [
17,
18,
19,
20,
21]. There appears to be a lack of consensus on how the indoor environment is perceived by elderly people.
This study aimed at investigating the temperature and humidity levels for four seasons around the older people residing in public elderly facilities, in addition to the occupants’ sleeping habits and thermal comfort among the four seasons.
4. Discussion
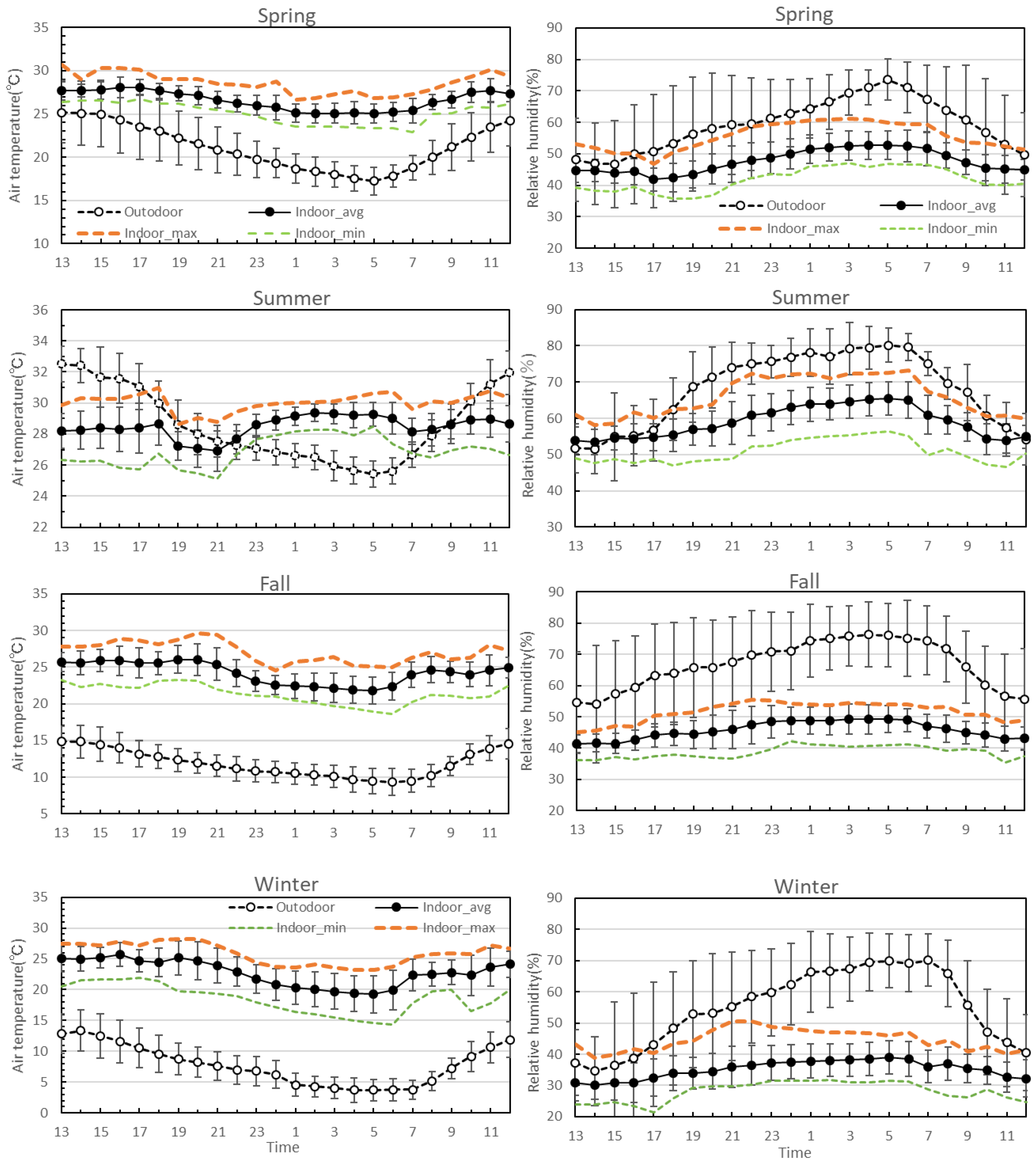
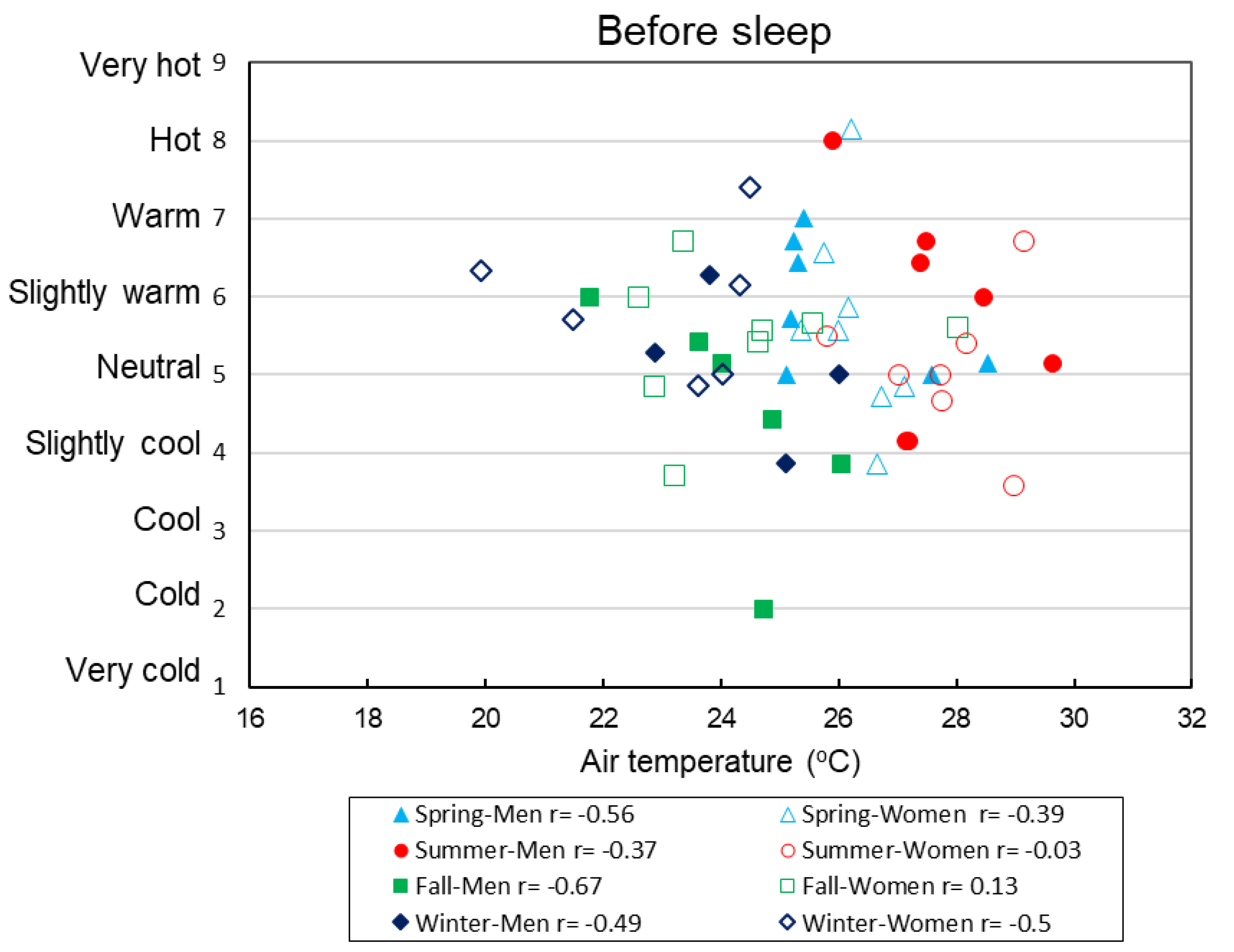
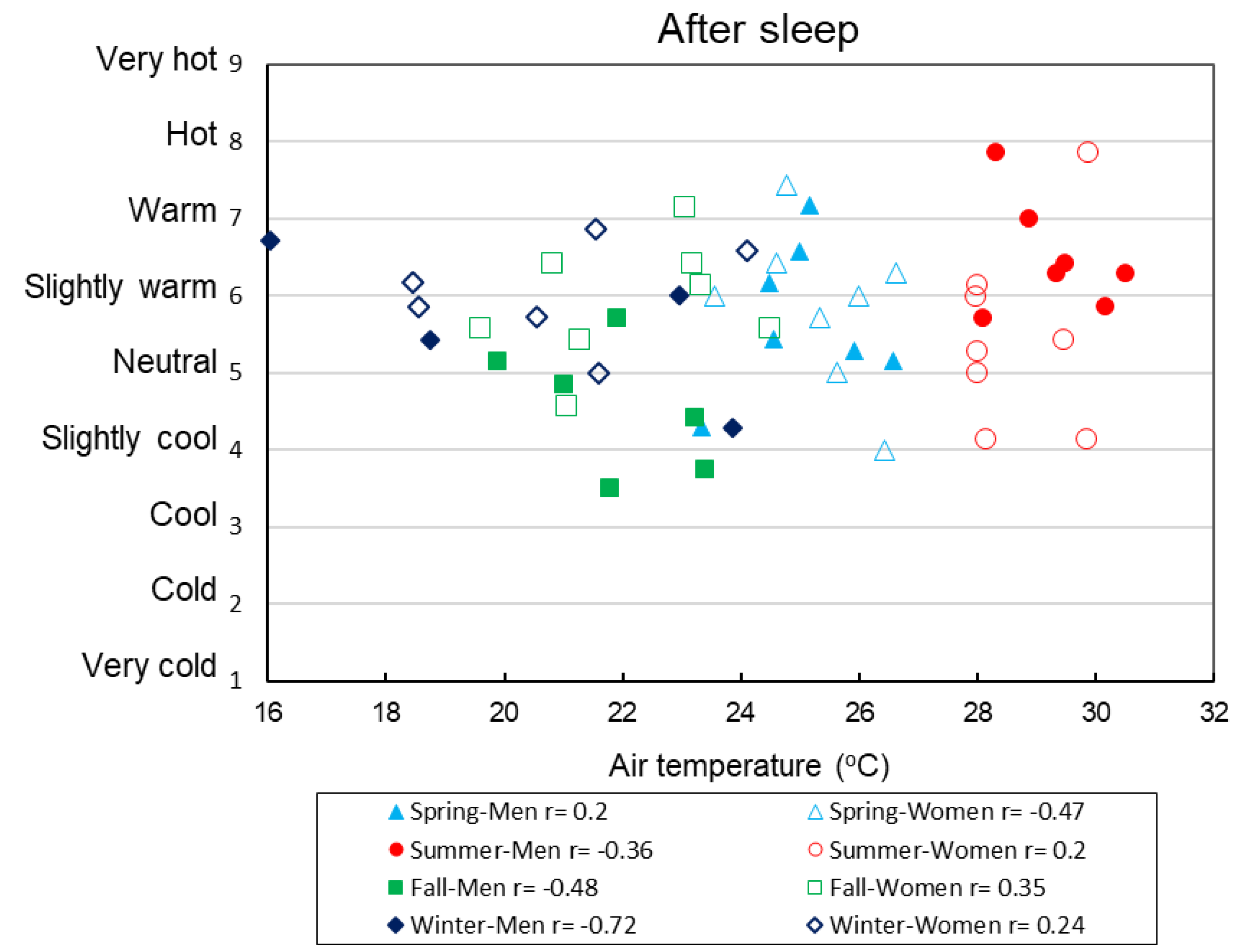
This study investigated the thermal environment, thermal comfort, and sleeping quality of residents living in elder care facilities in Japan, over the four seasons. The buildings operated in mixed-mode [
26], where the HVAC system was not in operation at night. The air conditioners were turned off while the caregivers were absent from the facilities during the night. Excluding summer, the average Ta was between 17 and 28 °C in the three seasons, which complies with the Japanese Standard for Maintenance of Sanitation in Buildings [
11]. Between 7 pm and 9 pm, before turning off the air conditioners, the Ta in the bedrooms was almost 27 °C in spring and in summer. After the air conditioners were turned off around 9 pm, the Ta gradually decreased in spring, however, the Ta gradually increased in summer and, exceeded 28 °C after 10 pm. Between 0 am and 6 am in summer, the average Ta was 29 °C. The buildings under study were constructed from reinforced concrete and were located in the center of the city. It is possible that the elevated indoor Ta at night in summer was due to the stored heat in their concrete structure from the daytime exposure to solar radiation. After turning off the air conditioners, the stored heat in the building structure may have transferred to the indoor environment where the elderly people slept, causing the increase in indoor Ta while the outdoor Ta remained around 26 °C. In this study, neutral sensations were found between 23 and 30 °C before sleep and 19–28 °C after sleep, depending on the season as the clothing differed. In previous studies on nursing homes for elderly people conducted in Australia [
20], the long-term monitoring of indoor temperature and humidity showed the neutral temperature in bedrooms in winter and summer was 21.2 °C and 22.9 °C, respectively, which meant the HVAC was operating day and night in both seasons. Hwang and Chen [
21] observed that the neutral temperature for the elderly was 25.2 °C, and Wong et al. [
19] estimated that the neutral temperature for residents who were living in Hong Kong nursing homes was 25.8 °C. These previous results support the results of the current study, even though the previous studies did not investigate thermal comfort at night or early morning.
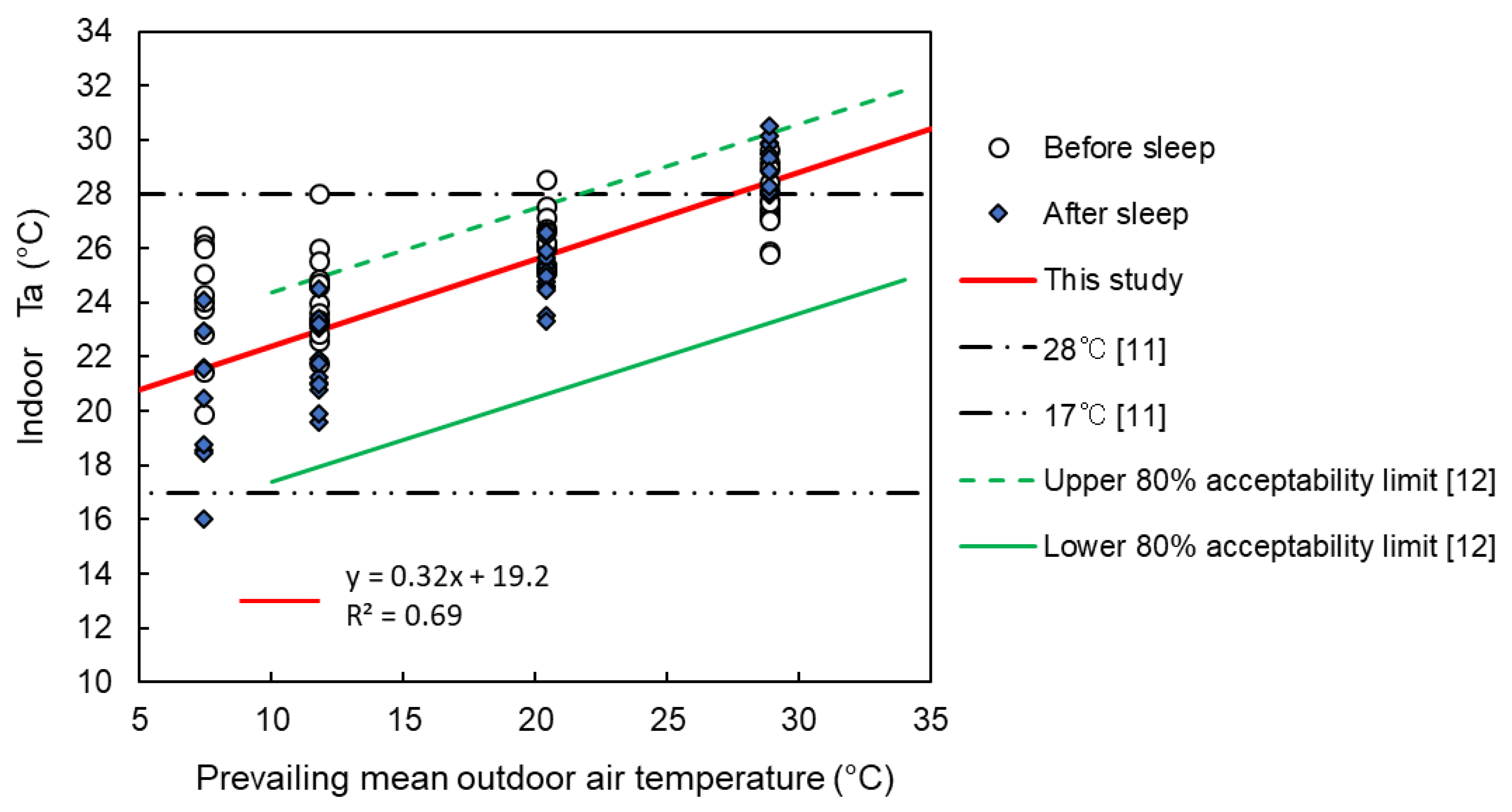
Figure 4 shows that the slope of the relationship between the prevailing mean outdoor Ta and indoor comfort temperature determined in this study was similar to that of the adaptive model. This regression line lies between the 80% acceptability limiting lines of ASHRAE [
12] and the adaptive model [
15]. The Ta in the summer did not comply with the Japanese Standard; however, it conformed to the adaptive model. Some residents used adaptive behavior to deal with the heat. Four of the seven male occupants used an electric fan and three of the eight female occupants tried to increase air velocity in the rooms by opening windows during summer nights. Thermal comfort is greatly influenced by air velocity. Although air velocity could not be continuously measured in this study, it can be assumed that air velocity was higher after opening windows and using fans, and this helped the occupants to reduce the heat load resulting from the higher temperatures.
Appendix B shows the average (SD) air velocity around people lying down. Airflow (1.7 m/s) has been reported to improve the sleep quality of young people by reducing the heat load in a hot humid environment (32 °C with 80% Rh) [
27]. However, the thermal comfort was not improved by the airflow. In this study, thermal comfort of the participants may not have been improved by the airflow during the sleeping period because the air velocity was not sufficiently high to reduce the heat load. Moreover, the sleep efficiency among men did not improve even with the use of a fan. The adaptive behavior of using a fan or opening a window was observed in more than 50 % of participants in summer. The other participants, however, did nothing. This suggests that adaptive behavior of the elderly themselves should not be expected. Monitoring Ta and using an air conditioner at night by the manager were necessary.
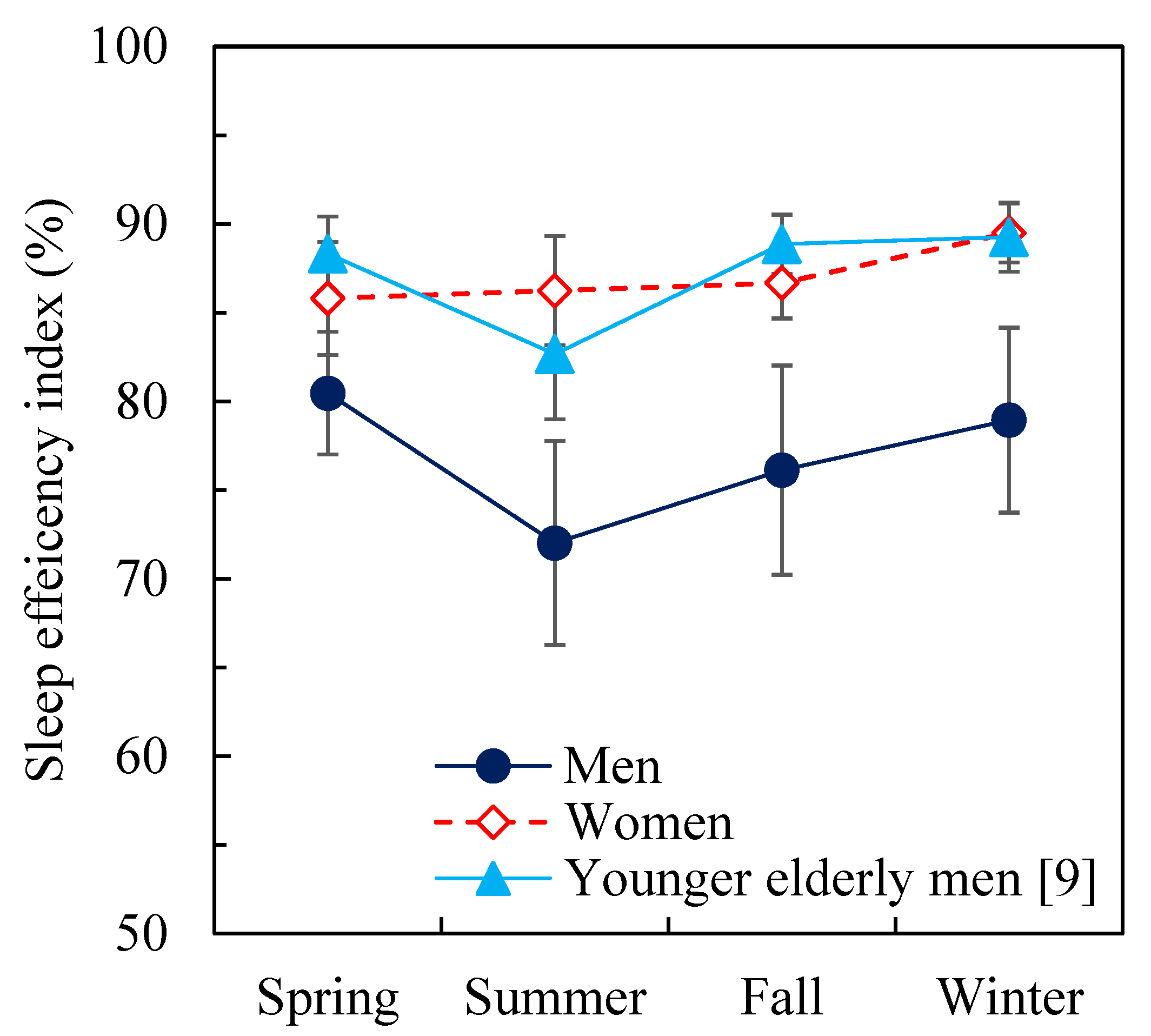
The interesting hypothesis that sleep quality of elderly people is worse in summer due to higher temperatures [
8,
9] was not supported by the case of women in this study. This study found no seasonal difference in the sleep parameters; however, significant differences were found in the total sleep time, wake time, sleep efficiency index, and sleep latency between women and men. The sleep efficiency index was significantly lower for men than for women, especially in summer. Neither the sleep efficiency index nor the length of wake time during the sleeping period were different for elderly women in the different seasons. These results mean that sleep quality was better for women than for men regardless of the season. Women were not poor sleepers, because their sleep efficiency was over 85%, which has been used as a cut-off value for poor sleepers [
28]. However, the men’s sleep efficiency was less than 80%, which is consistent with previous research indicating that sleep efficiency below 80% substantially increased mortality risk in elderly people [
29]. The sleep quality for elderly men was worse in summer; these results are supported by a study on younger elderly men [
9]. However, no statistically significant differences in subjective sleep evaluations were found between men and women in either season, although the women felt significantly more difficulty in falling asleep than the men. These results are supported by a population-based study [
30]. The difference in subjective sleep quality and objective sleep quality for elderly men and women presented by actigraphic sleep measurements showed poorer sleep for men than for women. However, elderly women reported shorter and poorer sleep than men in a diary or interview [
30]. Although women’s sleep onset latency and sleep period were longer, movement during sleep did not show differences between elderly men and women [
31]. Unfortunately, these studies did not consider the effects of the seasons, nor the ambient temperature or lighting. When thermal environment and thermal sensation were investigated in the elderly nursing home in August, the temperature and humidity were 25–26 °C and 45–70%Rh, respectively. In a questionnaire, these parameters were evaluated as good by the elderly occupants [
32]. Although the objective sleep parameters were not investigated and subjective sleep sensation did not show any difference relative to sex [
33], the seasonal effects on sleep parameters for the elderly, especially for those living in elderly care facilities or nursing homes, were not fully investigated, and the results are somewhat limited. Recent studies have focused on lighting or illumination levels during sleep [
34,
35] and on sleep–wake cycles [
36]. When objective measures of sleep patterns and subjective sleep quality for 16 senior people (aged 72–99 years) living in a care home were compared in summer and winter across a suite of blue light, illuminance levels, and health and well-being indicators [
37], seasonal differences were found relative to lighting. However, there was no significant difference in sleep parameters, although daytime physical activity level was higher in proportion to the lighting level. Seasonal effects on the sleep–wake cycle, the rest–activity rhythm, and quality of life for Japanese and Thai senior people were examined, and the data showed that both sets of participants had a shorter sleep time in summer. However, there was no significant difference in sleep efficiency during the four seasons in Japan or the three seasons in Thailand [
36], although lighting and physical activity were significantly higher in summer. A field study investigated the relation between sleep and lighting in both summer and winter seasons [
9]. Although the periods when participants were exposed to lighting over 1000 lx and 3000 lx were longer in summer, there was no significant difference observed in the sleep parameters relative to the season. Moreover, no seasonal effects were shown on sleep parameters even though the lighting and activity levels were higher in summer than in winter.
Thermoregulation during heat exposure changes with aging. Older male subjects who are awake exhibit lower heat tolerance than younger men [
5,
6,
7]. The ability to maintain a core body temperature and the sweating response during heat exposure appears to be reduced [
7]. In our previous study, thermoregulation and sleep for elderly men (average 69 years old) were compared in two cases—at 26 °C and at 32 °C, while the Rh in both cases was maintained at 50% [
34]. The results showed that a decrease in rectal temperature was suppressed and the sleep efficiency index was significantly lower due to increased wakefulness at 32 °C as compared to 26 °C when the elderly men wore short sleeve pajamas. In a previous experimental study, the duration of wakefulness was minimal at 29 and 34 °C in comparison to 21, 24, and 37 °C for young men during the sleeping period without clothing and bedding [
38]. This discrepancy may be due to the age of the subjects. In the current study, the Ta in the bedroom was maintained at 29 °C at night, which can be expected to present a heat load on the human body during sleep because the ability of thermoregulation deteriorated for the elderly men. It can be expected that elderly men would have worse sleep quality, although elderly women did not seem to be influenced by the temperature. Moreover, the adaptive behavior was limited for the elderly women. The adaptive approach assumes people change their behavior. The adaptive approach of turning on a fan or opening a window is difficult for sleeping people, although sleeping people can sometimes move or remove the bedding covers unconsciously. Although more than 50% of the male participants used a fan during the sleeping period, the male participants demonstrated a waking time that was twice that of the female participants in summer. The sleep efficiency index of the male participants was reduced by more than 10% when compared to the women and the younger elderly men in our previous study [
9], as shown in
Figure 4. This fact means that the adaptive approach is not enough to improve the sleep efficiency of sleeping elderly people even within the acceptable temperature range based on the thermal comfort, especially for elderly men. The adaptive approach should be limited to waking elderly people or during the daytime. The HVAC should continue to operate while elderly people occupy the facilities, regardless of whether the caregivers or managers are absent. We strongly recommend that indoor temperature is monitored by the caregivers, managers, or local government authorities.
No large-scale survey was approved by the facility. Although we recruited 20 people, only 16 people were able to complete the first spring experiment. This is also because the standard requirements for the health of the subjects were strict. Although the number of subjects was limited, not only the measurement of the thermal environment in the building, but also the questionnaire survey of thermal comfort and the sleep measurement using the actigraph, showed that indoor environment had an adverse effect on the elderly residents at night in summer. This study started with 16 elderly participants—8 men and 8 women—in two facilities. Two men passed away after the summer experiments, and one more was hospitalized after the fall experiment. The age of the participants in the present study was around 80 years old (70–87 years old) for both men and women. At the time when this field survey was undertaken in Japan, the average life expectancy was 79 and 85 years of age for men and women, respectively. The missing data of the three men may be due to life expectancy. The sleep quality was worse for the men in summer, and, was worse for the men than for the women in all four seasons. It is still unclear why the sleeping quality of elderly women in summer season did not deteriorate as it did for men. It is necessary to investigate thermoregulation and sleep quality of the elderly women during sleep. The co-existence of other factors—not yet disclosed in the present study—in addition to the thermal environment, may also influence the sleep quality of senior people.
There are certain limitations to the study as follows:
The air velocity and radiant temperature could not be measured continuously during the night because the researchers could not stay overnight. Moreover, other physiological parameters were also not measured because the ethical committee did not accept the procedure to measure physiological responses by means other than an actigraph. One of the largest limitations was the small sample size used to investigate the thermal comfort for elderly people. Moreover, the assessments of clothing and bed cover insulation levels are likely to introduce uncertainties.