Primary Stability of Temporary Screws after Dentary and Orthopedic Forces under Static and Dynamic Load Cycles
Abstract
:1. Introduction
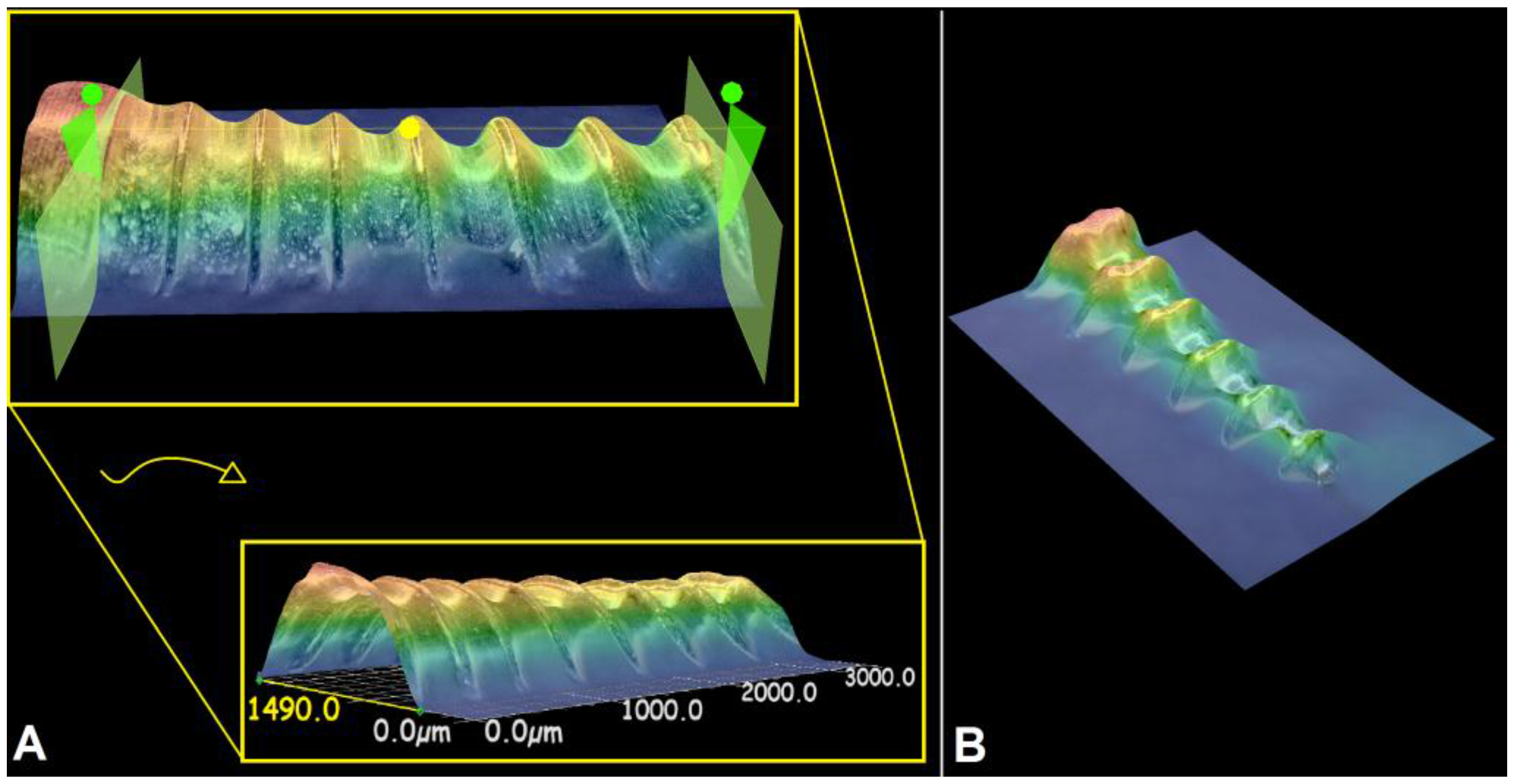
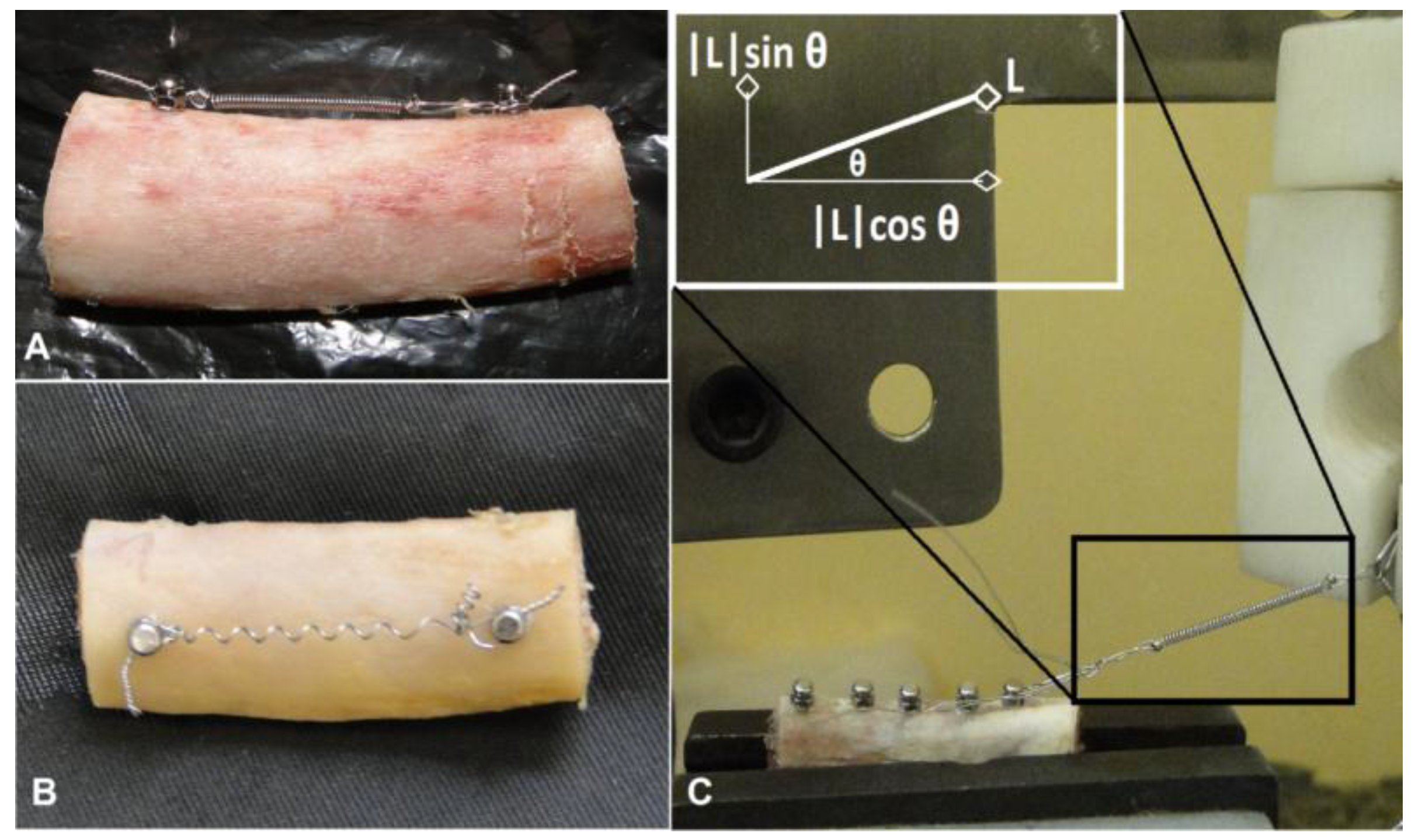
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- Limited influence in screws primary stability were identified by static loads applied by 2 N forces (dentary forces), although 5 N loads (orthopedic forces) had produced significant influence in stability loss;
- Dynamic loads applied under 56,000 cycles showed relevant influence in screw stability loss after paired comparisons;
- The magnitude of dynamic loads had limited impact into torque peak values, being the type of load significant in primary stability changes. Intermittent forces (dynamic cycles) had relevant effects onto stability loss of temporary screws.
Acknowledgments
Authors Contributions
Conflicts of Interest
References
- Mihara, H.; Cheng, B.C.; David, S.M.; Ohnari, K.; Zdeblick, T.A. Biomechanical comparison of posterior cervical fixation. Spine 2001, 26, 1662–1667. [Google Scholar] [CrossRef] [PubMed]
- Calvert, G.C.; Lawrence, B.D.; Abtahi, A.M.; Bachus, K.N.; Brodke, D.S. Cortical screws used to rescue failed lumbar pedicle screw construct: A biomechanical analysis. J. Neurosurg. Spine 2015, 22, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Ruellas, A.C.O.; Fernandes, D.J. Orthodontic implants: Concepts for the orthodontic practitioner. Int. J. Dent. 2012, 2012, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Z.; Chen, Y.; Tung, Y.; Chiang, Y.; Lai, E.H.; Chen, W.; Lin, C. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Tabuchi, M. ; Ikeda, T; Nakagawa, K.; Hirota, M.; Park, W.; Miyazawa, K.; Goto, S.; Ogawa, T. Ultraviolet photofunctionalization increases removal torque values and horizontal stability of orthodontic miniscrews. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Zarb, G.A. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry, 1st ed.; Zarb, G.A., Albrektsson, T., Branemark, P.I., Eds.; Quintessence: Chicago, IL, USA, 1985; pp. 199–209. [Google Scholar]
- Alrbata, R.H.; Yu, W.; Kyung, H. Biomechanical effectiveness of cortical bone thickness on orthodontic microimplant stability: An evaluation based on the load share between cortical and cancellous bone. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Cunha, A.C.; Marquezan, M.; Lima, I.; Lopes, R.T.; Nojima, L.I.; Sant’Anna, E.F. Influence of bone architecture on the primary stability of different mini-implant designs. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, D.J.; Elias, C.N.; Ruellas, A.C.O. Influence of screw length and bone thickness on the stability of temporary implants. Materials 2015, 8, 6558–6569. [Google Scholar] [CrossRef]
- Farnsworth, D.; Rossouw, P.E.; Ceen, R.F.; Buschang, P.H. Cortical bone thickness at common miniscrew implant placement sites. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Migliorati, M.; Signori, A.; Biavati, S. Temporary anchorage device stability: An evaluation of thread shape factor. Eur. J. Orthod. 2012, 34, 582–586. [Google Scholar] [CrossRef] [PubMed]
- Brettin, B.T.; Grosland, N.M.; Qian, F.; Southard, K.A.; Stuntz, T.D.; Morgan, T.A.; Marshall, S.D.; Southard, T.E. Bicortical vs monocortical orthodontic skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, F.; Tozlu, M.; Germec-Cakan, D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.; Park, Y.; Hwang, C.; Kim, J.; Choi, E.; Cha, J. A comparison of tapered and cylindrical miniscrew stability. Eur. J. Orthod. 2014, 36, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E.Y.; Suzuki, B. Placement and removal torque values of orthodontic miniscrew implants. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.; Hwang, C.; Kwon, S.H.; Jung, H.; Kim, K.; Yu, H.S. Strain of bone-implant interface and insertion torque regarding different miniscrew thread designs using an artificial bone model. Eur. J. Orthod. 2015, 37, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.; Choi, Y.; Evans, C.A.; Hwang, H.S. Predictors of initial stability of orthodontic miniscrew implants. Eur. J. Orthod. 2011, 33, 528–532. [Google Scholar] [CrossRef] [PubMed]
- McManus, M.M.; Qian, F.; Grosland, N.M.; Marshall, S.D.; Southard, T.E. Effect of miniscrew placement torque on resistance to miniscrew movement under load. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e93–e98. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, F.A.; Barboza, A.; Fernandes, D.J.; Elias, C.N. Stability of temporary orthodontic implants after dynamic load cycles. Int. J. Oral Dent. Health 2016, 2, 35–39. [Google Scholar] [CrossRef]
- Reynders, R.; Ronchi, L.; Bipat, S. Mini-implants in orthodontics: A systematic review of the literature. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 564.e1–564.e9. [Google Scholar] [CrossRef]
- Camey, L.O.; Campbell, P.M.; Spears, R.; Ceen, R.F.; Melo, A.C.; Buschang, P.H. Effects of pilot holes on longitudinal miniscrew stability and bony adaptation. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 554–564. [Google Scholar]
- Suzuki, M.; Deguchi, T.; Watanabe, H.; Seiryu, M.; Likubo, M.; Sasano, T.; Fujiyama, K.; Takano-Yamamoto, T. Evaluation of optimal length and insertion torque for miniscrews. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Inonue, M.; Kuroda, S.; Yasue, A.; Horiuchi, S.; Kyung, H.; Tanaka, E. Torque ratio as a predictable factor on primary stability of orthodontic miniscrew implants. Implant Dent. 2014, 23, 576–581. [Google Scholar]
- Santos, R.F.; Ruellas, A.C.O.; Fernandes, D.J.; Elias, C.N. Insertion torque versus mechanical resistance of mini-implants inserted in different cortical thickness. Dent. Press J. Orthod. 2014, 19, 90–94. [Google Scholar] [CrossRef]
- Vilani, G.N.L.; Ruellas, A.C.O.; Mattos, C.T.; Fernandes, D.J.; Elias, C.N. Influence of cortical thickness on the stability of mini-implants with microthreads. Braz. Oral. Res. 2015, 29, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- El-Dawlatly, M.M.; Abou-EL-Ezz, A.M.; El-Sharaby, F.A.; Mostafa, Y.A. Zygomatic mini-implant for Class II correction in growing patients. J. Orofac. Orthop. 2014, 75, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.T.; Kim, S.H.; Choi, Y.S.; Park, Y.J.; Chung, K.R.; Suk, K.E.; Choo, H.; Huang, J.C. Cone-beam computed tomography evaluation of orthodontic miniplate anchoring screws in the posterior maxilla. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 628.e1–628.e10. [Google Scholar] [CrossRef]
- Woodall, N.; Tadepalli, S.C.; Qian, F.; Grosland, N.M.; Marshall, S.D.; Southard, T.E. Effect of miniscrew angulation on anchorage resistance. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e147–e152. [Google Scholar] [CrossRef] [PubMed]
- Motoyoshi, M.; Yoshida, T.; Ono, A.; Shimizu, N. Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implants. Int. J. Oral. Maxillofac. Implants 2007, 22, 779–784. [Google Scholar] [PubMed]
- Oliscovicz, N.F.; Shimano, A.C.; Marcantonio Junior, É.; Lepri, C.P.; Dos Reis, A.C. Analysis of primary stability of dental implants inserted in different substrates using the pullout test and insertion torque. Int. J. Dent. 2013, 2013, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Uemera, M.; Motoyoshi, M.; Yano, S.; Sakaguchi, M.; Igarashi, Y.; Shimizu, N. Orthodontic mini-implant stability and the ratio of pilot hole implant diameter. Eur. J. Orthod. 2012, 34, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.C.; Baek, S.H. Effects of predrilling depth and implant shape on the mechanical properties of orthodontic mini-implants during the insertion procedure. Angle Orthod. 2012, 82, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Son, S.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Comparative study of the primary stability of self-drilling and self-tapping orthodontic miniscrews. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Ahn, H.; Park, Y.; Kim, S.; Chung, K.; Cho, I.; Nelson, G. Effects of predrilling on the osseointegration potential of mini-implants. Angle Orthod. 2012, 82, 1008–1013. [Google Scholar] [CrossRef] [PubMed]
- Esenlik, E.; Aglarci, C.; Albayrak, G.E.; Findik, Y. Maxillary protraction using skeletal anchorage and intermaxillary elastics in Skeletal Class III patients. Korean J. Orthod. 2015. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.M. Coiled Wire Spring Appliances for Use in Orthodontics. U.S. Patent 3,618,214 A, 4 May 1970. [Google Scholar]
- Lewis-Klapper, R.G. Orthodontic device for correcting overbite and underbite. U.S. Patent 5,846,074 A, 8 December 1998. [Google Scholar]
- Brown, R.N.; Sexton, B.E.; Chu, T.G.; Katona, T.R.; Stewart, K.T.; Kyung, H.; Liu, S.S. Comparison of stainless steel and titanium alloy orthodontic miniscrew implants: A mechanical and histologic analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Catharino, P.C.C.; Dominguez, G.C.; Pinto, D.S., Jr.; Morea, C. Histologic, histomorphometric, and radiographic monitoring of bone healing around in-office-sterilized orthodontic mini-implants with or without immediate load: Study in rabbit tibiae. Int. J. Oral. Maxillofac. Implants 2014, 29, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Shin, H.; Kyung, H. Biomechanical and histological comparison of self-drilling and self-tapping orthodontic microimplants in dogs. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Çehreli, S.; Arman-Ozçirpici, A. Primary stability and histomorphometric bone-implant contact of self-drilling and self-tapping orthodontic microimplants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Largura, L.Z.; Argenta, M.A.; Sakima, M.T.; Camargo, E.S.; Guariza-Filho, O.; Tanaka, O.M. Bone stress and strain after use of a miniplate for molar protraction and uprighting: A 3-dimensional finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, L.A.; Ryken, T.C. Screw Pullout Testing. In Mechanical Testing of Bone and the Bone-Implant Interface, 1st ed.; Draughn, R.A., An, Y.H., Eds.; CRC Press: Boca Raton, FL, USA, 2000; pp. 551–566. [Google Scholar]
- Wu, J.H.; Wang, H.C.; Chen, C.M.; Lu, P.C.; Lai, S.T.; Lee, K.T.; Du, J.K. Pullout strengths of orthodontic palatal mini-implants tested in vitro. J. Dent. Sci. 2011, 6, 200–204. [Google Scholar] [CrossRef]
- Crum, M.S.; Young, F.A.; An, Y.H. Screw pullout test for evaluating mechanical properties of bone. In Mechanical Testing of Bone and the Bone-Implant Interface, 1st ed.; Draughn, R.A., An, Y.H., Eds.; CRC Press: Boca Raton, FL, USA, 2000; pp. 321–328. [Google Scholar]
- Huja, S.S.; Litsky, A.S.; Beck, F.M.; Johnson, K.A.; Larsen, P.E. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Wu, Y.; Zhao, L.; Zhou, Y.; Wei, X.; Tang, N.; Feng, X.; Tang, T.; Zhao, Z. Effect of placement angle on the stability of loaded titanium microscrews in beagle jaws. Angle Orthod. 2013, 83, 659–666. [Google Scholar] [CrossRef] [PubMed]
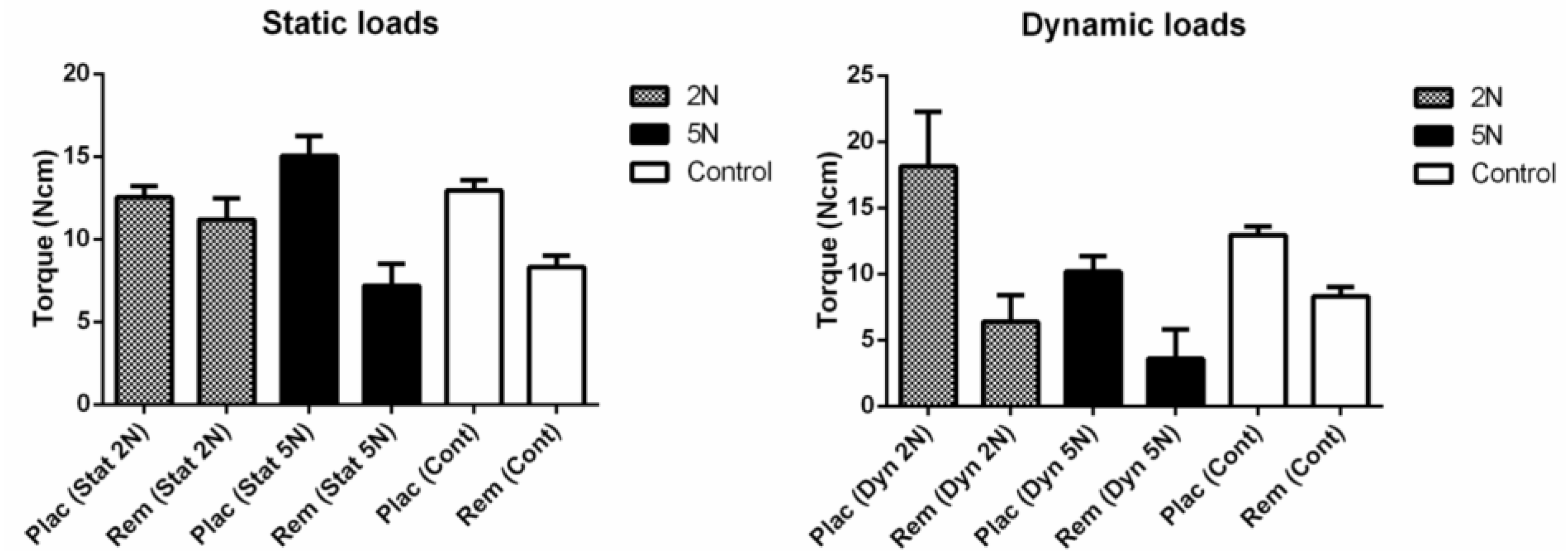
| Load | Control | 2 N | 5 N | ||
|---|---|---|---|---|---|
| Torque | Static | Dynamic | Static | Dynamic | |
| Placement | 12.95 (1.55) | 12.54 (1.75) | 18.14 (4.14) | 15.03 (2.96) | 10.18 (1.17) |
| Removal | 8.3 (1.76) | 11.2 (3.37) | 6.38 (2.01) | 7.18 (3.23) | 3.6 (2.22) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, D.J.; Barbosa, F.A.; Ferreira, L.M.; Elias, C.N. Primary Stability of Temporary Screws after Dentary and Orthopedic Forces under Static and Dynamic Load Cycles. Metals 2017, 7, 80. https://doi.org/10.3390/met7030080
Fernandes DJ, Barbosa FA, Ferreira LM, Elias CN. Primary Stability of Temporary Screws after Dentary and Orthopedic Forces under Static and Dynamic Load Cycles. Metals. 2017; 7(3):80. https://doi.org/10.3390/met7030080
Chicago/Turabian StyleFernandes, Daniel J., Flavia A. Barbosa, Ligia M. Ferreira, and Carlos N. Elias. 2017. "Primary Stability of Temporary Screws after Dentary and Orthopedic Forces under Static and Dynamic Load Cycles" Metals 7, no. 3: 80. https://doi.org/10.3390/met7030080
APA StyleFernandes, D. J., Barbosa, F. A., Ferreira, L. M., & Elias, C. N. (2017). Primary Stability of Temporary Screws after Dentary and Orthopedic Forces under Static and Dynamic Load Cycles. Metals, 7(3), 80. https://doi.org/10.3390/met7030080






