Abstract
According to the Dutch colonizers in Suriname, leprosy (or Hansen’s disease) was highly contagious and transmitted from human-to-human. A “cordon sanitaire” was constructed around the patients, mainly African slaves and Asian indentured laborers and their descendants. They were tracked down and incarcerated in remote leprosy settlements located in the rainforest. Some patients obeyed the authorities while others resisted and rebelled. Their narratives, revealing conceptual entanglement of the disease with their culture and the Surinamese natural environment, contain important information for understanding their world and their life inside and outside of leprosy settlements. They combined traditional health practices and medicinal plants from their natural habitat with biomedical treatments (practicing medical pluralism). They believed in a diversity of disease explanations, predominantly the taboo concepts treef, tyina, and totem animals associated with their natural habitat (the Surinamese biome). Some of their imaginary explanations (e.g., “leprosy is carried and/or transmitted through soil and certain animals”) show a surprising analogy with recent findings from leprosy scientists. Our research shows that nature contributes to shaping the world of Hansen’s disease patients. An ecological approach can make a valuable contribution to understanding their world. Comparative historical and anthropological research needs to be conducted to map the influence of different biomes on local explanatory models. The now deserted Hansen’s disease settlements and their natural environments are interesting research sites and important places of cultural heritage.
1. Introduction
1.1. Hansen’s Disease and the Natural Environment
Leprosy or Hansen’s disease is a chronic infectious disease of the skin and peripheral nerves, characterized by deformities and disabilities [1] and by severe stigmatization1 [2]. It is caused by Mycobacterium leprae [3] and by Mycobacterium lepromatosis [4], but the way this bacterium is transmitted is not well understood. It is spread from person-to-person via nasal droplets [5] and by skin-to-skin contact [6]. The idea that humans are the only reservoir of the disease appears problematic. Several studies suggest that soil might be an additional reservoir of leprosy bacteria [7,8]. Furthermore, in 1975 in Louisiana (USA), it was discovered that nine banded armadillos (Dasypus novemcinctus) are natural carriers of the leprosy bacterium [9]. In the Southern states of the USA, leprosy spreads from armadillos to humans [10]. In 2016, it appeared that red squirrels (Sciurus vulgaris) in Great Britain are naturally infected with leprosy, but there is no evidence that these animals infect humans [11].
1.2. Suriname
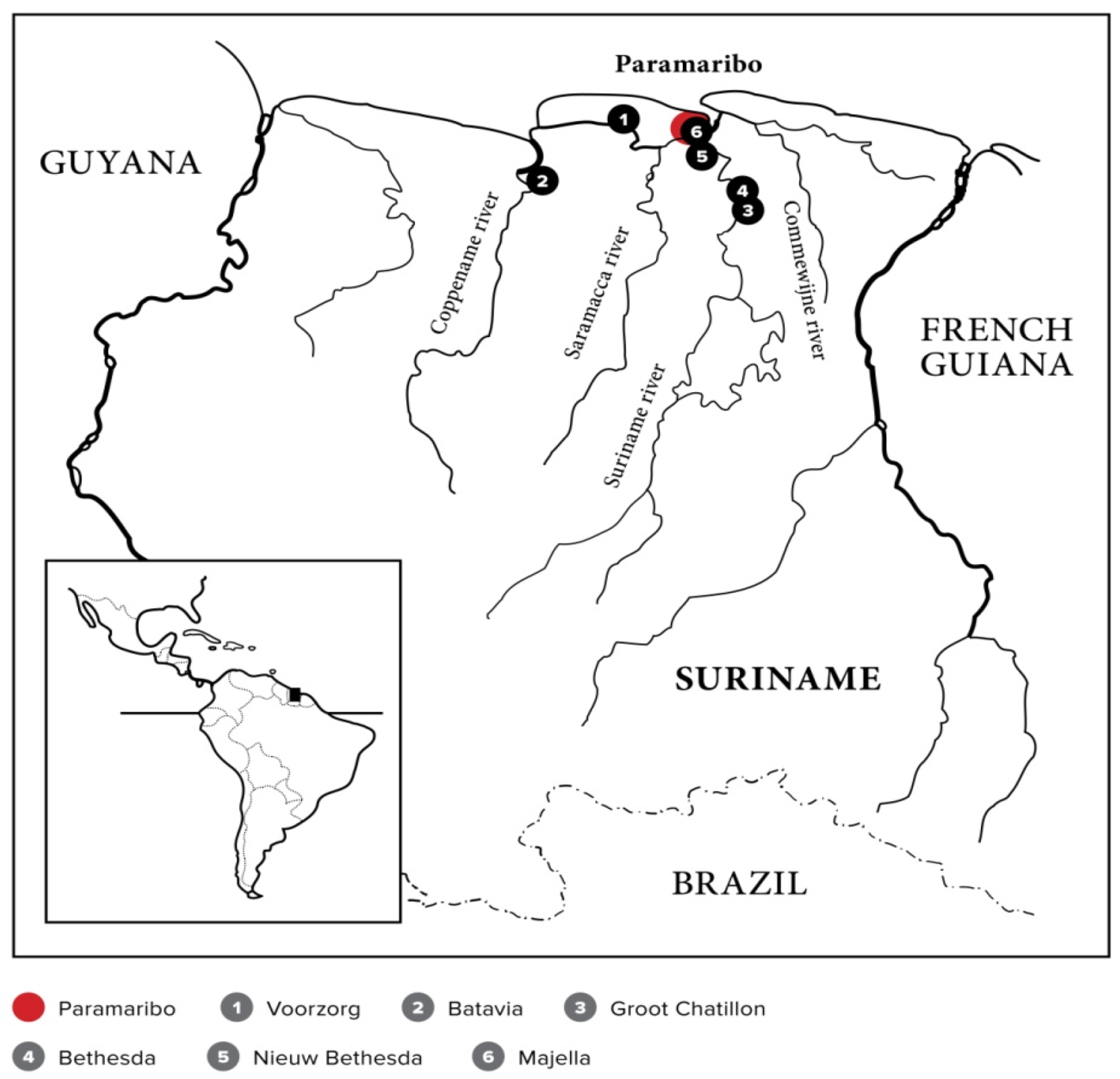
Suriname, situated in the north eastern part of South America (Figure 1), is included in the larger Guiana Shield and the Amazon biome. It is part of the largest pristine continuous tract of tropical forest in the world [12] (pp. 8–9). The Guiana shield, sandwiched between the Amazon and Orinoco rivers, is a geographical region sometimes referred to as “the land of the many rivers” [13] (pp. 26–38). The Surinamese rainforest includes an estimated number of almost 5000 different plant species [14] (p. 7), [15] (p. 2). It is also the habitat of an enormous diversity of insects, fishes, amphibians, reptiles, birds, and mammals [16]. It was in this biosphere that the Surinamese leprosy (or Hansen’s disease) narrative unfolded in colonial times.
Figure 1.
The six leprosy settlements in Suriname. This map is an adapted version of the original by Hendrik Rypkema, Naturalis Biodiversity Center, Leiden, the Netherlands.
In pre-Columbian times, the country was inhabited by indigenous people. From the early 17th century onward, small groups of Europeans, mainly British and Dutch, established plantations in the coastal region along the Suriname and Commewijne rivers. In 1667, Suriname officially became a Dutch colony, with Paramaribo as its capital [17] (pp. 9–20). The plantation economy expanded in the 18th century, with the number of plantations increasing to 406 around the year 1770, but hit an economic downturn in the 19th century [18] (pp. 33–37). The key products were sugar and coffee, but other commodity crops were also produced for export to Europe. To allow the cash-crop economy to function effectively, the plantations needed cheap labor. The workforce consisted of enslaved Africans procured by the Dutch West Indian Company (WIC), who were notoriously ill-treated in Suriname. Many fled from the plantations to the hinterland, establishing Maroon communities [19] (pp. 1–38). Slavery was abolished in 1863. To prevent further deterioration of the plantation economy, indentured workers from China, British India (now India), and the Dutch East Indies (now Indonesia), were recruited from the mid-19th century onward to replace the formerly enslaved Africans who had abandoned the plantations in large numbers after abolition [20] (pp. 181–186), [21] (pp. 2–3). Suriname, a multi-ethnic society, became an independent republic in 1975.
1.3. Leprosy in Suriname
Leprosy raged in Suriname in colonial times [22] (pp. 17–61). People with this disease were hunted down and incarcerated in one of the six leprosy settlements that had been established in the country from 1790 onward (Figure 1).
The control strategy, designed and implemented by the colonizers, was regarded as a hard line approach [23] (p. 55) that further stigmatized and dehumanized the already heavily oppressed colonized people. The colonized people had an obvious power disadvantage compared to the Europeans [24]. The latter affected their dominance through three institutions: political institutions (government supported, using military and police forces); economic institutions (the profit-oriented enterprises that used slaves and cheap labor); and religious institutions (which worked as soft power but were also active in the colonial health forces regarding leprosy control). Tropical medicine, the aggregate activity of imperial doctors and medical systems, was not a neutral, altruistic enterprise but an instrument of imperialism that facilitated the presence of Europeans in the tropics [25] (pp. 79–80), [26,27]. These institutions designed, constructed, and implemented the leprosy control system. However, the harsh health control regime was not naturally accepted by Surinamese patients and their families, who—whether incarcerated or not—played their own decisive role in the Surinamese leprosy narrative, with a central role for the tropical ecology.
1.4. Ecology and Surinamese Leprosy Narratives, an Unexplored Area
This study is about leprosy control in colonial times in Suriname and, more particularly, the establishment of leprosy settlements (also called leprosy colonies or leprosaria). The colonizers were convinced of the contagiousness of leprosy, hence their strategy of isolating patients in leprosy settlements generally located in remote places in the rainforest [28]. We noticed that the daily life of the patients was strongly linked with the natural environment and that they used natural products (plants and animals) in their culturally determined treatment practices. Their explanation of the origin of the disease was also linked to nature—many saw leprosy as a punishment for violating taboos against certain things in nature around them, such as animals or soil [29] (pp. 73–134), [30] (pp. 162–163). It is clear that there was a wide gap between the colonizers’ explanations of leprosy and those of the people with Hansen’s disease. This is a rather unexplored area in Surinamese leprosy historiography. The present conceptual paper aims to draw attention to the role of Surinamese ecology in the disease narratives of Hansen’s disease patients. We argue that adopting an ecological approach to the social history of health and disease contributes to a better understanding both of the disease histories of Surinamese Hansen’s patients and their coping behavior and of the transmission mechanisms and patterns of Hansen’s disease.
2. Objective and Methods
For a long time, descriptions of Surinamese leprosy colonies reflected the vision and activities of colonial rulers, including church representatives [31] (pp. 61–72) and physicians [32]. Only recently has attention been paid to the opinions and practices of patients [33] (pp 78–92), [29] (pp 71–134). The natural environment (more precisely, the rainforest) has always been neglected in publications about leprosy in Suriname. We believe however, as we shall demonstrate in this paper, that nature remarkably contributed to shaping life in these settlements. This contribution is reflected in 1) daily life, 2) the explanatory models of the disease, and 3) treatment practices using plants and animals from the natural environment.
The objective of this conceptual paper is to describe and explain how control strategies for containing leprosy were designed and executed by the colonizer—culminating in a “cordon sanitaire” [34] (pp. 52–53), [35] (pp. 1–4), a barrier around the patients to prevent the spread of infectious disease. Furthermore, this paper describes and explains how patients and their families adhered to alternative disease explanations, treatments, and practices originating from their own culture, thus protesting and revolting against the system (both openly and privately). Finally, quintessential to our message is our description of how the ideas and practices of patients and their families appear to have been closely related to the Surinamese tropical ecology.
This paper is based on information from relevant publications and archival documents, with the aim of reconstructing the colonizer’s view. The reconstruction of patients’ views is based on in-depth, semi-structured interviews (oral history) with 30 Surinamese ex-Hansen’s patients. Sixteen of them had experienced isolation in a leprosy asylum, and 14 were diagnosed with leprosy in the post-segregation period (after 1972). The interviews were conducted between 2011 and 2013 and aimed to learn the patients’ experiences, ideas, and feelings. A report of these interviews, including nine full life stories, has been published in Dutch [29] (pp. 73–134), [30] (pp. 135–164) and constitutes the basis of this paper.2 Historian Selma Leydesdorff explains that narratives based on daily experiences may give insight into the emotions, behavior, family and community relations, and responses of subordinated groups to the dominant discourse of those in power [36] (pp. 23–42). The narratives of these ex-Hansen’s patients discussed in this paper are important for understanding how leprosy settlements and the natural environment influenced their life and experiences. This study is furthermore based on our published observations and laboratory findings during ecologically and archaeologically oriented expeditions to the site of the (now deserted) leprosy colonies [37,38]. Finally, we also undertook an expedition to the hinterland of Suriname to study the explanatory concepts of leprosy of the Maroon people so as to better understand the contextualized views of leprosy patients [30] (164–167). Thus, in our multidisciplinary (historical, anthropological, biological) analysis, we focus on the perspectives of both the colonizing and colonized people while paying special attention to the interaction of the leprosy patients with the natural environment.
3. Results and Discussion
3.1. The Colonizers’ Views and Strategies
3.1.1. Contagion
In the middle of the 18th century, a new and devastating disease emerged, especially affecting the enslaved, who called it boasie [39] (pp. 432–433). Philippe Fermin, a German-born physician who worked in Suriname from 1754 until 1762, identified the disease as originating from Africa, as identical to medieval leprosy, and as both highly infectious and incurable [40] (p. 127). Godfried Schilling, a Dutch physician who worked in Suriname in the second half of the 18th century, proposed a comprehensive, multi-factorial explanatory hypothesis: boasie was caused by a “poison” that one could contract through close contact with a leprosy sufferer, and, more particularly, through contact with wound exudate or through sexual intercourse with an African women suffering from the disease [41] (pp. 4–40). He furthermore claimed that the hot climate and the bad food of the enslaved weakened their bodies and thus could be considered to be contributing factors. Schilling’s concept is explained as contingent or malleable leprosy contagionism [28] (p. 175). Thus, boasie or leprosy was essentially considered a contagious disease of Africans, but Europeans could contract it. This definition, including a racialized and sexualized view of the disease [39] (pp. 446–447), was adopted by Dutch physicians until the 1860s [42,43]. In 1869, a Suriname-born physician of Dutch-Huguenot ancestry, Charles Louis Drognat Landré, launched his contagion theory in a French monograph [44]. He narrowed down Schilling’s contingent contagionism to a monocausal contagionism concept and, at the same time, rejected the hereditary theory (supported by influential Norwegian and British researchers) that had emerged in the middle of the 19th century as the dominant explanatory hypothesis [45,46]. In 1873, the Norwegian Gerhard Henrik Armauer Hansen discovered leprosy bacterium as the cause of leprosy [3]. His research was in part based on the contagion theory of Drognat Landré [47,48].
3.1.2. The Construction of a “Cordon Sanitaire”
Snelders et al. explain that there was much fear of contracting boasie among white settlers. The authors furthermore suggest that forced labor, leprosy, and compulsory segregation were connected through a “colonial gaze,”3 legitimizing compulsory segregation of leprosy sufferers who had become useless to the plantation economy and might threaten the health of white inhabitants [49]. Fear and the “colonial gaze” may explain the rather stringent leprosy containment policy. This strategy can, however, also be understood as a result of the system of colonial rule. According to the medical historian Erwin Ackerknecht, there is a close connection between a country’s political system and its approach toward epidemic diseases: an autocratic system (as opposed to a more liberal system) favors a view of epidemic diseases as contagious and consequently applies tactics of isolation. The slave colony Suriname had an authoritarian system of government that did not care much about the rights of the non-white residents, something that should be considered to be a precondition for the severe leprosy control measures that were taken [28,50] (p. 173).
The control system was based on legal rules (called “plakaten”) issued by the governor of the colony. According to the rule of 1761, enslaved people with boasie were required to avoid public roads under penalty of a fine to be paid by their owner [51] (pp. 707–708). This measure failed to have the desired effect: the number of leprosy patients only increased. As a result, a much tougher policy was propagated in a set of rules issued in 1790: all leprosy patients, except whites, were to be incarcerated at Voorzorg, the first leprosy settlement in Suriname, located on the Saramacca river [51] (pp. 1144–1147). Whites were allowed to isolate themselves in their own houses. Furthermore, according to the last article of this rule (article 8) every citizen of the colony was called upon to report to the officie fiscaal (a bureau of the colonial government) anyone they thought might suffer from boasie, who would then be examined by two members of the Collegium medicum (the colonial medical board). In fact, with this 1790 rule, the citizens of the colony were legally involved in the fight against leprosy. The tone was set for severe leprosy policies that can be summed up as “chasing and jailing” people with boasie, a strategy that was to be continued until the middle of the 20th century. In 1823, Voorzorg was abandoned, and the inmates were relocated to Batavia, the new leprosy colony situated further away from the capital city on the Coppename river [52] (p. 63). However, the system, and, more particularly, the tracking down of new leprosy patients, failed again. The colonial regime responded in 1830 with another new set of rules,4 which can be considered to be the most comprehensive leprosy laws ever launched in Suriname. The hunt for leprosy patients was intensified in several ways—for example, by carrying out a house-to-house search to discover new leprosy cases, conducted by the police, the city physician, and the surgeon-general every three years in all houses in Paramaribo and on the plantations. Additionally, a commission named “Commissie tot onderzoek naar de ziekte der Melaatschheid en besmettelijke Elephantiasis” (Commission for Examination of People in Order to Detect Leprosy and Contagious Elephantiasis) was established to determine whether a person who was brought in suffered from leprosy or not. For a period of 130 years, this so-called “leprosy commission” played a decisive role in Surinamese leprosy control. The members acted as judges who decided whether someone suffered from leprosy and would hence be sentenced to a leprosy colony. Illustrative of this process is the narrative of Hendrik, an 84-year-old leprosy patient, who lived in the Bethesda leprosy colony for 22 years. He was examined by the “leprosy commission” in 1936, and explained how this commission functioned, sometimes in collaboration with anonymous informers or bounty hunters. He also criticized the racialized colonial system [29] (pp. 99–100).
When I was seven years old, white spots were detected on my buttocks during a medical examination at school. I was brought before the leprosy commission, six physicians, all of them had a light skin: whites, Jews, basradyu (bastard Jews), and mulattos. In those days you could not study [to become a doctor] when you were black, even if you were intelligent. The commission decided [about your future]. If four of the six said that you had to be turned in, then you had to go to a leprosy colony. The commission decided that [for the time being] I had to stay at home. There was no verification [of my home isolation]. But [they counted on] “dalaskowtu,” anonymous informers, receiving one dollar, when bringing in “sick children” walking on public roads. Incidentally, [dalaskowtu] did not only betray sick children but everyone who violated the law. They were a sort of policemen or spies for the colonial government. They were Surinamese who were used to oppress other Surinamese.
The 1830 rule remained in effect for about 100 years. In 1929, a new set of rules was launched, which in fact were nothing more than the 1830 rules in a modern guise, with hunting down and jailing leprosy sufferers and with the “leprosy commission” continuing its work. In a way, the rules were even tighter. This is not really surprising since, after the infectious nature of leprosy had been accepted worldwide at the first international leprosy conference held in Berlin in 1897, stringent isolation was advised as the only way to contain the disease. For example, according to article 3 of the 1929 rules, letters and other objects might only leave the leprosarium after they were properly disinfected, and lijfsgoederen (underwear) should be burnt when no longer in use by a patient. Hendrik explains the emotional pain he had to endure because of this confinement regime [19] (p. 103).
If you wanted to surprise a family member with something you had made yourself, for instance a beautiful frame, it had to be disinfected, with [methylated] spirit, I think. [The object] was kept in a special cabinet [for a while]. When you brought it [to the nurse] to be disinfected, you felt the pain, it’s a strange feeling. Even if you wanted to send a letter it had to be disinfected. Those were the rules in Bethesda.
According to article 15 (of the 1929 rule), children born of parents with leprosy were immediately separated from their parents. Nadia, an 82-year-old leprosy patient of Javanese origin who was isolated in Groot Chatillon (generally known as Chatillon) from 1950–1956, tells of her experience [29] (p. 96).
In Chatillon, my four children were born. They were taken away from me at once after birth, to prevent them from contracting leprosy. Those were the rules. I handed them over to my mother-in-law, but when I was released from the asylum, I took them back to raise them myself.
With the rules of 1960, the leprosy control system finally loosened: the legal obligation to isolate leprosy patients and the feared leprosy commission were both abandoned.5 The last Surinamese leprosarium (Chatillon) was closed in 1972. In conclusion, with the consecutive series of increasingly stringent rules over a period of 200 years, the colonial government attempted to maintain a cordon sanitaire around leprosy or Hansen’s patients. However, as stated above, patients had their own explanations and treatment practices, and many resisted the system in some way.
3.1.3. The Leprosaria
Anatomy of Leprosaria
Like plantations, the Surinamese leprosy asylums (Table 1 and Figure 1) were situated on a river or creek.

Table 1.
Leprosaria of Suriname.
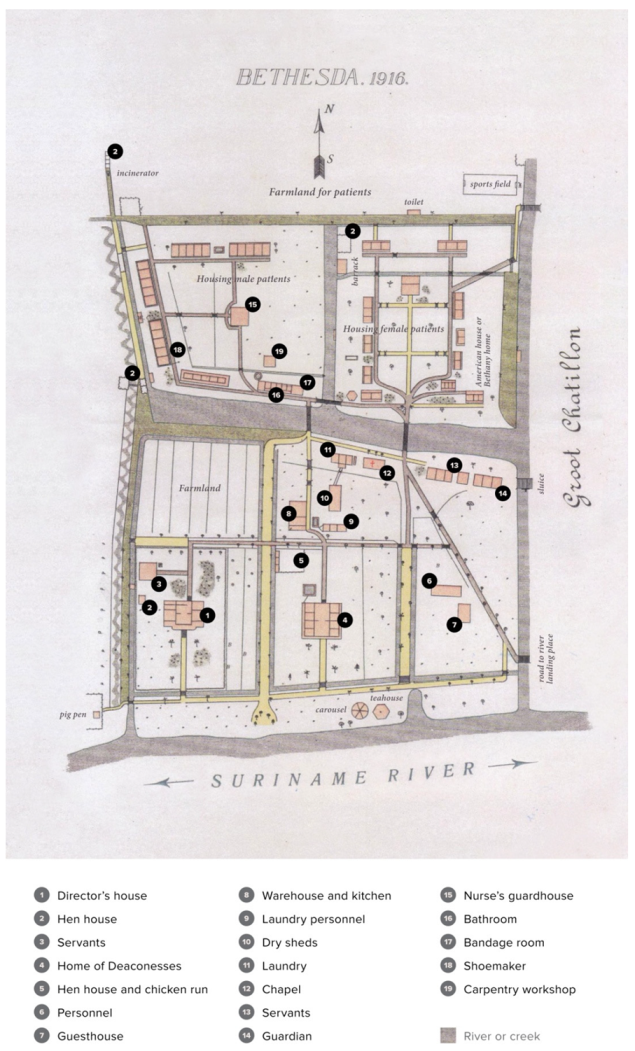
The asylums of Voorzorg, Chatillon, and Bethesda (the latter two having been located next to one another) were situated on peninsulas formed by strong bends in a river. The water and jungle around the leprosy settlements constituted natural barriers between incarcerated patients and the general population, acting as the envisaged cordon sanitaire and, furthermore, discouraging patients from running away. The building plan of the asylums demonstrated a basically hierarchical arrangement reminiscent of plantations [53] (p. 38) and probably reflecting comparable power relations. Illustrative is the plan of Bethesda (Figure 2), with the director’s house/office situated prominently in the front, close to the river and clearly visible when arriving by boat. The management buildings (e.g., nurses’ housing) were located next to this house and behind these buildings, at the back of the leprosy village, one would find the dwellings of the inmates. The asylum constituted a microcosm of society with its own customs and rules.
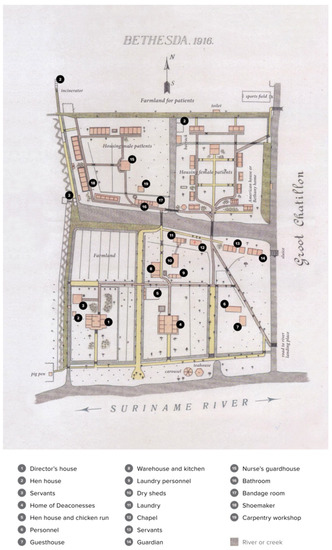
Figure 2.
Plan of the leprosy settlement Bethesda (1916), by J.H. de Bussy, Amsterdam, slightly adapted (legends in English) by the authors. Source: het Utrechts archief, nr. 895 (Utrecht, the Netherlands).
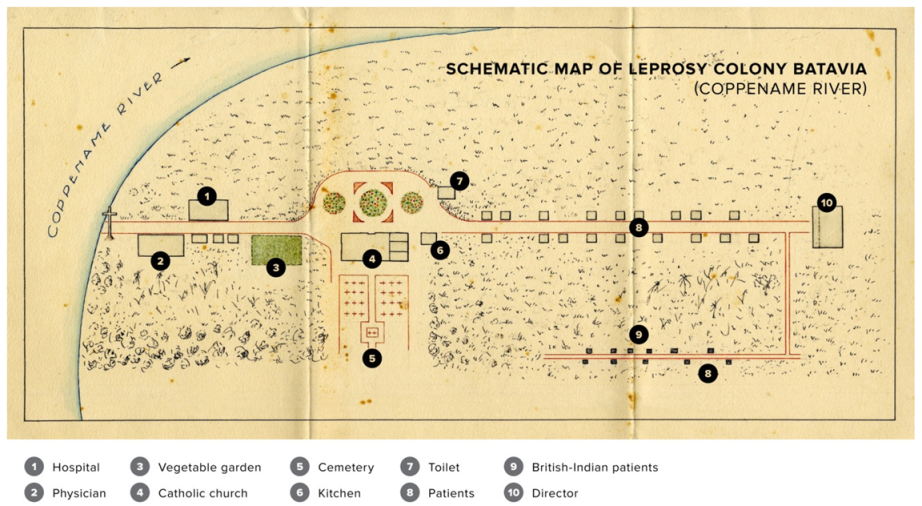
Figure 3 shows the Batavia settlement, with the director’s house at the back of the colony and the house of the medical doctor, another authoritative person, near the river.
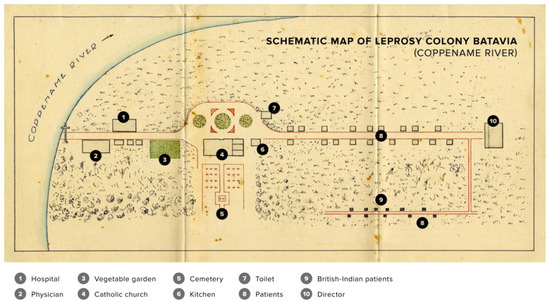
Figure 3.
Plan of leprosy settlement Batavia (from approximately 1880–1890). Slightly adapted (legends in English) by the authors. Source: Archief Kloosterleven St Agatha, inventaris nr. 9301 (the Netherlands).
In the more modern asylums (contrary to Batavia and, probably, to Voorzorg) a physical barrier in the form of a small canal or creek prevented contact between inmates and personnel. This feature points to a tightening of the cordon sanitaire in the modern settlements, with less freedom of movement (and actions) for the inmates, which probably related to the fact that the rather complex and elusive idea of contingent contagionism had (in the second half of the 18th century) given way to a comprehensible, almost tangible, monocausal contagionism (at the end of the 19th century) with Hansen’s bacterium viewed as a transmissible germ.
The Old Leprosaria
Voorzorg was established on the eastern bank of the Saramacca river in a pristine rainforest. With just a few eyewitness reports available, little is known about this settlement. Medical and religious supervision were absent [33] (pp. 28–29). The patients were kept under control by soldiers stationed in Groningen on the left bank of the same river just opposite the asylum [54] (p. 171). Voorzorg was abandoned in 1823 because of a mosquito plague and because it was considered too close to Paramaribo and thus a threat to public health [52] (p. 63).
The new leprosy settlement, Batavia, was established further away from Paramaribo on the right bank of the Coppename river—the premises of a former military post [55] (p. 168). The inmates of Voorzorg resisted transport to Batavia. To ensure their compliance, Abraham de Veer, Governor of Suriname, forged an alliance with the Roman Catholics, a religious group that existed outside the social and political establishment of the protestant colony [33] (pp. 95–96). Batavia subsequently became the domain of the Roman Catholics. In the meantime, the continuous hunt for leprosy patients was fueled by the rigorous rules of 1830. In the period between 1830–1860, exclusion from society of leprosy patients resembled a “Great Confinement” [33] (pp. 43–77), [56] (pp. 38–40), with close to one in every 100 inhabitants of the country confined to Batavia or isolated at home. Batavia was rather chaotic and unruly. Snelders designates the settlement as a “battleground in the jungle” [33] (p. 94). He refers to conflicts between Protestants and Catholics and to the struggles between inmates and (religious and secular) supervisors. The following two events exemplify the continuously rather tense relationship between inmates and the Catholic Church. A large tree that stood on the riverbank (Surinamese name: kankantrie; scientific name: Ceiba pentandra) [14] (pp. 304–306) was considered sacred in Afro-Surinamese religious practices. The priest, Martinus Van der Weijden, had the tree felled in September 1826 and put a large wooden cross in its place. He did not long survive the felling. After his return to Paramaribo in October 1826, he came down with a severe fever and died after a week [33] (pp. 97–99). The second event refers to Gerardus Johannes Heinink, priest at Batavia from 1844 onward. A slave named Andreia, a rum smuggler who delivered alcohol to the inmates of the asylum in defiance of Catholic supervision, was caught in the act by Heinink in October 1849. Heinink took drastic action by sinking Andreia’s boat in the river. That same evening, the priest fell ill after supper, and by the next day, he was dead. Heinink’s milk had been poisoned by the priest’s Afro-Surinamese housemaid [33] (p. 107).
The cordon sanitaire around Batavia was far from watertight. The Dutch physician Andries van Hasselaar, who visited the settlement in 1827 as a member of a medical committee, complained that quite a number of inmates were not present at Batavia for the intended visitation. The director, who apparently was aware of the fact that these inmates had left the establishment, immediately ordered other inmates to pick them up by boat. Peter Lens, a medical officer stationed at the Dutch West Indian island Curacao, visited Batavia almost 60 years later. He was shocked to see the “reckless” interactions between healthy people and people with leprosy; indigenous people from a nearby village wandered between the houses and interacted amicably with leprosy patients [57] (p. 504). From 1856 until his death in 1887, Priest Peerke Donders was stationed at Batavia. Upon his arrival, he found the moral standards to be extremely low, with drunkenness and sexual debaucheries as the norm. He managed to restore order through, on the one hand, being strict with the inmates and, on the other hand, often taking their side in conflicts with the Protestant director. He also ensured improvement of the housing conditions of inmates [33] (pp. 109–110).6 The number of leprosy patients segregated at Batavia declined in the years just prior to the abolition of slavery in 1863, pointing to a weakening of leprosy control. An explanation might be found in the fact that slave owners were unwilling to report leprosy among their slaves, as slaves suspected of having leprosy were excluded from financial compensation for their owners [49] (p. 11).
Establishing Modern Leprosaria in a Pillarized Society
Mgr. Wilhelmus Wulfingh, head of the Roman Catholic church in Suriname from 1889–1906, proposed to the governor to move the leprosy settlement Batavia to Groot Chatillon (a plantation at the Suriname river that had been bought by the Roman Catholic Church) [57] (pp. 544–552). He furthermore suggested that the Catholics would take care of all inmates with leprosy, irrespective of their religion. The Protestant church objected to this proposal because freedom of religious expression was, in their opinion, not guaranteed. They looked for support in the Netherlands and, backed by the Dutch minister of colonial affairs, Wulfingh’s proposal was dismissed. He then sold Chatillon to the government and bought lands on the northern edge of Paramaribo. Wulfingh got permission from the colonial government to start a Roman Catholic leprosarium named Gerardus Majella (generally known as Majella) at this location [33] (p. 154). The government decided to build a new state leprosarium at Chatillon to replace Batavia. The Protestants (a combination of the Calvinist, Lutheran, and Moravian congregations) got permission to build their own leprosy colony Bethesda next to Chatillon [58] (pp. 69–71). In 1933, Bethesda was replaced by New Bethesda, because the leprosarium was endangered by erosion of the riverbank from the river’s strong current and because the protestants preferred a location closer to the capital [33] (p. 232).
The new settlements were relatively comfortable—tiny villages with many facilities, such as bandage rooms, a laundry, and workshops for the inmates (Figure 2). Care, including inmate discipline, was maintained by a staff of trained nurses and other personnel. Majella was staffed by Dutch nuns from the Sisters of Charity congregation in Tilburg, the Netherlands [52] (p. 66) and Bethesda and New Bethesda by German deaconesses of the Moravian church [59] (pp.18–19). Chatillon was largely run by Surinamese staff [48], sometimes with managers from the Netherlands such as, for example, from the Dutch Salvation Army between 1955 to 1960 [60] (pp. 203–209). A civilizing mission was added to the other primary tasks of the settlements (segregation and medical care), particularly in the two religious leprosy colonies. In interviews, many inmates indeed praised the religious leprosy colonies for their educational zeal. For example, Eddy Jharap, an ex-Hansen’s patient and co-founder and former director of one of Suriname’s main industries (state oil), said that his successful career is inseparably associated with his confinement in Bethesda [61] (pp. 46–65). However, from interviews with ex-leprosy patients, we have concluded that the general feelings and attitudes of the inmates were more ambiguous—leaning towards compliance, on the one hand, and disobedience and resistance, on the other. The latter included running away, romantic and sexual relations, refusing food, and refusing medication.
Running away was common. Inmate Hendrik from New Bethesda explains [29] (pp. 103–104):
[We] ran away in the evening, some [of us] visited a “working girl.” Yes, a young man needs a woman. So, we went to the Maagden street, Jodenbree street… the well-known streets where one can find “working girls” … I was a young [man], I could not resist it … We secretly ran away, to town.
Between three and 15 people escaped annually from Chatillon between 1902 and 1924 [33] (p. 226). In 1951, no less than 151 escapes from Chatillon were counted. Eight patients never returned to the asylum. Salomon John Bueno de Mesquita, head of the leprosy service, complained that the spread of leprosy was facilitated by these runaways, who stayed with their family or friends for days, weeks, or even months.7 Intimate relations between patients, while strictly forbidden in the religious leprosaria, were not uncommon. Inmate Nadia, a Javanese woman who was isolated at Bethesda from 1938 till 1950, explains [29] (pp. 94–95):
I was 19 years old and fell in love with another inmate. I became pregnant, but a pregnant woman was not allowed at Bethesda. We were transported to Chatillon [where relations between men and women were permitted].
The lives of the inmates were intertwined with the natural habitat. This is not surprising, if we take into account that the settlements were surrounded by jungle and river. The food supply was supplemented with hunting and fishing in Voorzorg [62] (p. 13) and Batavia [57] (p. 544). Nadia, who was first incarcerated at Bethesda (1938–1950) and later at Chatillon (1950–1956) describes [29] (pp. 93–94):
… the river was full of fish … I like fishing. The river [also] separated us from the rest of the world. Some of the inmates were looking for freedom. They escaped in a dugout canoe. Water entered the little boat, but they had no fear.
Eddie Jharap says that he and other inmates at New Bethesda secretly swam in the river, though this was forbidden by those in charge [22] (p. 50). Deaths by drowning sometimes occurred. For example, 17-year-old Paul Stelligt went swimming in the river at Chatillon with two other inmates and drowned.8 In addition to its role in supplying food and leisure activities, the natural environment also played an important role in the inmates’ efforts to treat, cope with, and explain their disease.
3.2. The Patients’ View: Entanglement of Culture and Nature
3.2.1. The Explanation of Leprosy by Patients
The following three narratives demonstrate the world of the Surinamese ex-Hansen’s patients: the entanglement of their culture and nature, their explanations and treatment practices, and the co-existence of traditional and modern ideas. These are clear examples of a view that is completely different from the view of the European colonizers (medical staff, religious caretakers, and colonial administration).
The Narrative of Diana (Animal Totemism, Treef, and Medical Pluralism)
Diana is a female creole Christian ex-Hansen patient from Paramaribo, born in 1937, who was segregated in the leprosarium Majella from 1941 until 1953. She reveals her story, in which an iguana plays an important role in explaining the origin of her leprosy [29] (pp. 78–85):
My illness is not something of God. My mother did not feel well, she lay down and fell asleep. In a dream, an old woman appeared to her and said, “What you’ve done with my child will also happen to your child.” When my mother woke up, she called my dad, “Eddy, come on, did you do anything?” He replied, “That rotten iguana creeping around here, I have nothing to do with that animal. I threw stones at her, I hit her.” With a stone, my father mutilated the toes of the unborn baby iguana in the belly of mother iguana. The iguana was pregnant, just like my mother, who was at the time pregnant with me. When my fingers were crooked in my 13th year, my mom knew immediately: “Indeed, it was not good what my husband did then, throwing stones … those stones damaged the toes of the baby iguana, that’s why my child’s fingers became crooked.”
Diana’s narrative contains a traditional explanation in which the iguana is a tyina,9 a totem animal. However, she combines this easily with another explanation—treef or food taboo:
My mother said that I had a treef: pork and unscaled fish. I was lucky that these things were not prepared in Majella. They did eat salted fish there, but that is scaled fish. Maybe the nuns had spoken with the “bigi sma” (elder wise women)10, and on their advice the meals for the patients were adapted. There was a time that I did believe that you could get leprosy through treef, but later on I understood that this was a wrong idea and now I eat everything.
In her narrative, Diana also presents a modern, Western concept to explain her leprosy:
I know that leprosy is simply caused by a bacillus that comes into your body, yet I do not believe that this story of infectivity of leprosy is entirely true. The doctors who came into contact with the patients did not get leprosy anyway?
Finally, Diana’s narrative also illustrates how modern and traditional treatment practices may have coexisted:
In 1948, when I was 11 years old, Doctor Gehr and Doctor Bueno de Mesquita brought the [new] medicine to Majella. And that’s why people could be dismissed in the 1950s. We were cured by the drug from America. [Originally] I was not treated with oso-dresi (traditional medication), my mother did not know those things. But after being dismissed from Majella she gave me Neem drink once a week. She said, “It’s something to purify blood.”
There are three remarkable points in Diana’s narrative on the genesis and healing of leprosy. First, the coexistence of traditional and modern explanations. Second, the co-existence of two traditional explanations—the food taboo and the curse of the totem animal (the iguana). Third, the co-existence of traditional and modern healing practices: although Diana believed in the effectiveness of modern medicine, traditional healing was still practiced after someone was dismissed from the leprosarium. Diana’s narrative is an example of explanatory and medical pluralism.
The Narrative of Kromo and Pawiro (Animal Totemism and Medical Pluralism)
Animal totemism is also demonstrated in the narratives of two Javanese patients originating from the Commewijne district in Suriname, Kromo and Pawiro, who links leprosy to a supernatural event. In the narratives, a snake is associated with the place and space of the leprosy colony Chatillon, as well as with the community of Javanese people in Commewijne [29] (pp. 86–92), [30] (pp. 150–151).
Kromo, a Javanese male patient (1936) who was segregated in Chatillon from the 1960s, explains,
The Javanese people in Commewijne were afraid to go to Chatillon because they believed that a snake was living under the bridge or under the director’s house. It was told that this snake would eat them. I’ve looked around, but never saw that snake. I think it was nonsense. I was not afraid at Chatillon.
Pawiro, a Javanese male ex-Hansen’s patient (1947) who had successfully resisted segregation in a leprosarium, also links leprosy with a snake at Chatillon. He was diagnosed with leprosy when he was eight years old. His mother had consulted a Javanese traditional healer, who advised that the boy should never enter Chatillon. Pawiro reveals,
My mother had taken me to a traditional healer to protect me so that they would not send me to Chatillon. In the past, many parents were afraid to lose their children and many died in Chatillon,
where a man-eating snake lived and that’s why many Javanese went to a traditional healer … Yes, that snake eats people, living people. They say when someone wants to go home, they jail that person in a guardhouse rather than taking the person home. Then the snake comes to eat that person in the night.
The snake in the patient narratives could be considered a totem of the Javanese community in the Commewijne district. The Javanese patients raised in this district associate leprosy with a snake that is related to Chatillon as a place and space of horror. Totemism is a system of belief in which humans are said to have kinship or a mystical relationship with a spirit-being, such as an animal or plant. The entity, or totem, is thought to interact with a given kin group or an individual and to serve as their emblem or symbol. Often, the animal or plant represents a particular taboo, which implies that it is forbidden to kill or eat the sacred animal or plant [63]. In his narrative, the Javanese patient Kromo killed a snake when he was fishing in Commewijne; his wife was six months pregnant at the time. This killing of the snake can be considered a violation of a taboo. Kromo says that his daughter was born with a serious disorder, though not leprosy. The story of the snake, called “Bajul bèbèk,” is probably not an original Javanese story but seems to be based on a tale from slavery times [64] (pp. 178–179). Kromo is furthermore another example of people using both modern, Western medicine and traditional healing practices. In addition to taking modern medicines in the leprosarium, in particular DDS, he took different alternative treatments: a drink of boiled neem leaves and mokko, aloe vera, and grated bitter cassava for local application on leprosy wounds.
The Narrative of Losita (Sand is the Tyina, the Taboo)
Losita is a sixty-year-old Maroon woman from the upper Suriname, the residential area of the Saramaccans, a Marroon people. She has Hansen’s disease and says that her leprosy bumps were caused by sand [29] (pp.119–123):
My sister fought with another woman—it was an argument related to my sister’s husband. That woman took sand and threw it on my sister. The sand also hit me. My sister got bumps, so did I. Sand is my sister’s tyina. It’s my tyina too, because we have the same father.
This is a remarkable story because, in this case not an animal or something edible is the patient’s tyina (taboo)—it is sand (soil) (i.e., dead or apparently dead matter, but it is still a natural product). According to Losita, sand in her case caused Hansen’s disease. We will discuss in a subsequent paragraph that the tyina concept is a broad taboo concept, certainly not limited to just edible things.
Discussion of the Patients’ Explanations
The above narratives indicate that the explanations (treef, tyina, and totem animals) are linked with nature. The iguana and snake are the totem animals in these narratives, but in interviews with other leprosy patients, tortoises [29] (pp. 124–128) and armadillos [30] (pp. 166–167) are mentioned as totem animals. In Table 2, the ideas of 30 ex-Hansen’s patients interviewed about the origin of their leprosy are shown. Not only the older persons who have been incarcerated but also young patients adhere to these (super-)natural explanations. So, it is clear that the patients adhered to their own ideas, different from the explanations by those who designed and implemented leprosy control.

Table 2.
Ideas of 30 ex-Hansen’s patients about the cause of their leprosy (some people mention more than one cause).
Treef and Tyina
Some physicians emphasized already in the 19th and early-20th centuries that common people basically believed in treef or trefu,12 a food taboo, as the cause of their leprosy which could hamper control strategy and treatment [65,66]. Treef is a personalized food taboo. The current significance of this taboo is confirmed by our interviews: 10 of the 16 patients (63%) who had been segregated and nine of the 14 (64%) who had not been segregated (Table 2) believed that their leprosy was caused by violating their treef. If we look closer at ethnicity, we see that all seven patients of Afro-Surinamese descent (100%) mentioned treef as the cause, versus two of the four Hindustanis (50%) and one of the five Javanese (20%). This is not surprising because, as we shall explain, treef has African roots, though, due to interculturalism in Suriname, it now occurs across ethnicities. Table 3 shows the wide variety of food products indicated by people of African descent as their treef.

Table 3.
Food mentioned as their treef (food taboo) by nine ex-Hansen’s patients of Afro-Surinamese descent.
According to Peter Lampe [66] (pp. 555–560), there are several types of treef, including father treef (inherited from the father), dream treef (the forbidden food is revealed in a dream, for example to the grandmother), treef based on experience, etc. But what is the origin of treef? It is a Surinamese hybrid concept with Jewish and West African roots. It has probably been adopted by the Africans enslaved by Jewish masters [66] (pp. 564–566). The word treef is derived from the Hebrew word tereifa, which, according to Jewish dietary laws, refers to food that is unsuited for human consumption (though the fact that treef is inherited through the paternal line points to an African origin) [67] (p. 191). To endorse the African origin, Benjamins refers to Willem Bosman, a merchant of the Dutch West Indian Company, who wrote in his account on West Africa (present day Ghana down to Angola) that each of the Africans had their own prohibited food: one did not eat sheep, another did not eat goats, etc. [67] (p. 191). During the interviews with Surinamese leprosy patients, the tyina notion was mentioned by patients of African origin, referring to food taboo. Saamaka Maroons from the upper Suriname river were interviewed [30] (pp. 164–165) to better understand this concept. Tyina appears to be a key concept in the Maroon culture. It is an umbrella concept with a much broader meaning than treef. In addition to taboo foods, the tyina concept includes several other forms of taboo. A tyina can be something someone is not allowed to eat, a place someone is not allowed to go, or an action someone is not allowed to do. Violating such a taboo can be punished by, for example, getting leprosy. Hence, the Maroons use the concept tyina siki (meaning tyina disease) to indicate leprosy. One may acquire a tyina in different ways. First, it can be heredity through the paternal line, the so-called tata tyina. Thus, if a man is not allowed to eat something, his children inherit this tyina. A second way to get a tyina is through reincarnation, the so-called neseki tyina. Saamaka people believe that the traits of a deceased person can return to the body of a newborn child. Third, a tyina can be linked to a tapa (or tapu). A tapa offers protection against something (for example against snake bites) but at the same time it is linked to a tyina. If you break the rules associated with your tapa, the protection is lost. There is a fourth way to achieve a tyina. If a person become ill after eating something, that person may have a tyina for that specific food. The same is true if someone experiences always being injured in a certain place. That particular place is a tyina for the person concerned. For the Saamaka people, violating a tyina can cause leprosy; thus (for example), violating a tyina associated with a turtle may cause leprosy. But Maroons think that although tyina is an important cause of leprosy, this disease may also have other causes, such as heredity, physical transferability (through sweat and sperm), infection, contact with certain trees, and, finally, through supernatural, magical phenomena. In short, this is explanatory pluralism: according to the Saamaka people, leprosy has a diversity of natural and supernatural causes.
3.2.2. Use of Plants for the Treatment of Leprosy
The above narratives indicate that the patients highly value their own traditional treatment with nature-based methods (plant extracts) and rituals of traditional religions like winti. Twelve of the 16 interviewed leprosy patients (75%) who had been incarcerated used these traditional medical practices. The plants they used are listed in Table 4.

Table 4.
Plants used by Surinamese ex-Hansen’s patients to treat their leprosy.
Most of these plants were indigenous, but some were brought to Suriname by enslaved or indentured laborers from their countries of origin. In addition to the plants mentioned by the interviewed leprosy patients (Table 4), Tinde van Andel describes four more indigenous Surinamese plants (present in the Surinamese jungle) that are used against leprosy by the Surinamese people (Table 5) [14] (pp. 39, 260, 313–314, 493). She explains that, with regard to Afro-Surinamers and related West African groups, although most plants used by these groups are neo-tropical, the preparation methods and applications are still very African. This illustrates durability and persistence of household medicine despite the disruption during the Middle Passage.

Table 5.
Herbal cures for leprosy in Surinamese folk medicine using plants present in the Surinamese jungle.
Afro-Surinamers reinvented their household medicines by using familiar Old-World plants, selecting New-World plants that were related to African ones, incorporating knowledge from other ethnic groups, and deploying trial and error [68]. Virtually all patients interviewed by us who used these alternative medications combined these methods with treatments provided by Western biomedicine, thus practicing medical pluralism.
3.2.3. Neighboring Countries
While this study about Hansen’s disease in Suriname is not designed as a comparative study, some remarks about the neighboring countries should be added (based on the limited information available). Suriname, located on the northern edge of South America, has, on the one hand, ecological characteristics of the Amazon rainforest. On the other hand, it shares demographic and cultural features of the Caribbean region, which reaches from territories on the northeastern part of South America to the islands in the Caribbean Sea [69]. On the Caribbean islands, St Kitts and Nevis people believe that you can get cocobay (a local name for Hansen’s disease) from a small lizard (also called cocobay) through the actions of an Obeah witchcraft doctor [70] (pp. 93–126). The (former) leprosy settlements in Guyana [71] (623–648), French Guiana [72] (pp. 583–598), and the northern states of Brazil13 were or are located in the rainforest, a natural habitat similar to Suriname. Creoles (people of African descent) in French Guiana believe that leprosy can be transmitted to humans by animals in the wild, such as armadillos, turtles, and deer.14
Cassandra White interviewed people with Hansen’s disease in Rio de Janeiro [73]. Some mentioned “the wind” as a source of their disease, an idea that overlaps with the biomedical model of leprosy being transmitted by air droplets emitted by a patient. One of the most common beliefs in Rio and throughout Brazil is that leprosy comes from dogs. White explains that, in Brazil, the word “lepra” is used both for Hansen’s disease and for dog mange. Another belief that exists in Brazil is that leprosy can be contracted by eating certain foods, e.g., pork and fish. Cassandra explains that there are no dietary taboos or constructions of pigs and fish as unclean animals. She suggests that these ideas may have diffused into the popular imagination from Europe, Africa, and Asia, where foods were linked to Hansen’s disease in both folk belief and in early bio-medical theory.
The above information is limited but still has some value for our analysis. The narratives from St Kitts and Nevis and from French Guiana suggest that wild animals may cause leprosy in a supernatural way, in accordance with the Surinamese explanation. The narratives of patients from urbanized Rio de Janeiro are partly consistent with those from the rainforest, but on the other hand, they tend more toward a biological rather than supernatural explanation. We believe that a comparative study based on interviews of leprosy patients living in different biomes might significantly add to our concept that ambient ecology contributes to explanatory models.
3.3. Natural Environment: the Presence of Leprosy Bacterium DNA in the Soil of the Deserted Settlements
From the narratives (Section 3.2.1), it is apparent that the lives of Surinamese leprosy patients were closely linked with the natural environment. This was again evident during our expeditions to abandoned leprosy settlements:
We pass the ruins of the housing of staff and inmates on the former leprosy colony Chatillon. They are overgrown with low vegetation and high trees, including palms with perilous thorns. The terrain is uneven, dotted with shallow puddles. Trunks of fallen trees litter the forest floor and as we walk through, we suffer an aerial attack by a swarm of bees and run for our lives. “Those were the deadly Brazilian bees, for sure,” our guide tells us. As he is speaking, his sharp eyes pick out a tortoise, its shell damaged with cracks running through the hard surface. Still alive, he picks it up. “The poor creature probably survived a swipe by a jaguar,” he says, “we’ll take it back to camp.” [22] (pp. 44–45).
This quote illustrates how the once bustling leprosy colony Chatillon was located in the jungle and has been altogether swallowed up again in the wilderness, much like other Surinamese leprosy asylums. These places are once again the habitat of wildlife. As discussed above, many leprosy patients believe that animals play a role in the origin of their leprosy. Their ideas, described as totemism by anthropologists, are generally ignored by biomedical researchers. During our expeditions to the (deserted) leprosy colonies of Chatillon and Batavia, we encountered armadillo burrows in the vicinity of the cemeteries of these settlements [22] (pp.36, 45). DNA type 1 and/or 2 of Mycobacterium leprae, the microorganism that causes leprosy, was identified in three of the seven samples of soil taken by us from these burrows [37] (p. 3). The findings suggest that armadillos living in those regions are infected with the bacterium that causes leprosy. This is in accordance with findings in the southern USA [9] [10] and in Brazil [74]. The preliminary indication that leprosy bacterium has nestled in the Surinamese ecology in and around former leprosy colonies needs further substantiation.
4. Concluding Remarks: A Call for an Ecological Approach
Our findings show that, from a patient perspective, nature plays an essential role in the Surinamese world of Hansen’s disease. This is evident from the combination of the patient’s believes and interactions with nature, as reflected in everyday life. A case in point is the treatments that they (secretly) applied with products from nature, supported by their own explanatory models. We note that these issues have received little attention in research publications and other documents related to the Surinamese history of Hansen’s disease. But biomedical researchers worldwide have also ignored ecology as an integral part of leprosy research. The neglect of the topic of ecology by researchers from the humanities, social sciences, and biomedicine may be due to the strong dominance of the concept of leprosy contagionism or Hansen’s paradigm. According to this conceptual framework, leprosy is an infectious disease caused by a bacterium that can only be passed from human to human, with humans as the only reservoir. From a biomedical point of view, much can be understood and explained with this paradigm, but not everything. For example, why is there no decrease worldwide in the number of new leprosy patients per year, despite vigorous treatment with effective antimicrobials? [75] With the discovery of the occurrence of leprosy in the armadillo in the Americas and in squirrels in the British Isles, and also the finding that the leprosy bacteria can survive in the soil for some time, things are starting to change. Our research points to a remarkable analogy between the (supernatural) ideas of Surinamese leprosy patients and the findings of the biomedical leprosy researchers. In the narratives of patients, sand (soil) and animals are considered “carriers” of the disease. Meanwhile, modern scientific research has shown that leprosy bacteria can actually survive in the soil and furthermore occur in certain animals in nature [76]. It should come as no surprise that the limited information on this matter from neighboring countries also points in the same direction. In view of our findings, we advocate changing or modifying Hansen’s disease research in the field of the humanities and social sciences towards a one-health approach. We believe that an ecological perspective may contribute to a better understanding of the world of Hansen’s disease patients. Comparative historical and anthropological research needs to be conducted to map the influence of different biomes on local explanatory models. In addition, we advocate for a multidisciplinary approach in which humanities, social sciences, and biomedical science join forces. This multidisciplinary, ecological approach could, from a patient’s perspective, result in new insights in the what and how of Hansen’s disease. The stigma and anxiety patients experience after a diagnosis of leprosy is often exacerbated by their lack of knowledge about how or from where they may have acquired this infection. Understanding that leprosy has clear environmental or biological origins can be quite beneficial in ameliorating the social and psychological impacts of leprosy.
5. Epilogue: The Future of Former Surinamese Hansen’s Disease Settlements
The last Surinamese leprosy asylum was closed in 1972. The current state of the places and spaces of the six former asylums are different, due to various developments after their closure. We visited all settlements in the period of 2016–2018, except for Voorzorg. This place is now overgrown by jungle and difficult to access [77] (p. 30). Batavia has been restored by the Roman Catholic church and is a modest place of pilgrimage, dedicated to the beatified Peerke Donders [22] (pp. 35–36). The buildings of Chatillon and Bethesda have fallen into ruin and are overgrown by jungle [22] (pp. 44–45). New Bethesda has made way for urbanization and industrialization resulting from the southward expansion of Paramaribo [22] (pp. 49–50). Majella is now practically located in the heart of the capital due to the northward expansion of Paramaribo. Parts of this former leprosarium, including some buildings, have been kept up or restored to their original state [22] (p. 41).
The remains of the settlements, including the neighboring biome, represent a wealth of tangible and intangible heritage to be used as public places of memory (lieux de memoires) and as places of historical, archaeological, paleontological, and medical–biological research. An important and first policy action for sustaining Suriname’s leprosy heritage is to pursue “salvage” archaeology. This refers to the collection of archaeological data and materials from a site that is in danger of damage or imminent destruction. As stated above, the Roman Catholic church has already made valuable steps in the preservation of Batavia and Majella. Furthermore, we have recently (in collaboration with others) started up research on the settlements, in particular paleontological investigations and genomics [37,38] (p. 3). A national policy for achieving sustainability of leprosy sites in Suriname should be based on international, regional, and national partnerships, as well as exchange programs with countries and institutions that are familiar with the conservation and development of leprosy sites and with establishment and maintenance of lieux de memoires and (virtual) museums.
Author Contributions
Conceptualization, H.M., T.P., and J.M.; methodology, J.M.; writing H.M.; review and editing T.P. and J.M. All authors have read the manuscript and agreed to the submitted version.
Funding
This research received no external funding.
Acknowledgments
We would like to acknowledge Frank-Jan van Lunteren MA, for the adaptation of the original figures and both Kathryn Burns and Nathalie Kuijpers for the English corrections. We are also very grateful for the support, input, and advice over the course of the project given to us by the following colleagues: William Faber, Frank Huisman, Maurits Hassankhan, Samunda Jabini, Sahiensha Ramdas, Melinda Reyme, Karin Sewpersad, Stephen Snelders, and Henry de Vries.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhang, G.; Li, W.; Yan, L.; Yang, Z.; Chen, X.; Zheng, T.; Ye, G. An epidemiological survey of deformities and disabilities among 14,257 cases of leprosy in 11 counties. Lepr. Rev. 1993, 64, 143–149. [Google Scholar]
- Deps, P.; Cruz, A. Why we should stop using the word leprosy. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Vogelsang, T.M. Gerhard Henrik Armauer Hansen 1841–1912. The discoverer of the leprosy bacillus. His life and his work. Int. J. Lepr. Other Mycobact. Dis. 1978, 46, 257–332. [Google Scholar] [PubMed]
- Han, X.Y.; Seo, Y.H.; Sizer, K.C.; Schoberle, T.; May, G.S.; Spencer, J.S.; Li, W.; Nair, R.G. A new Mycobacterium species causing diffuse lepromatous leprosy. Am. J. Clin. Pathol. 2008, 130, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Hatta, M.; van Beers, S.M.; Madjid, B.; Djumadi, A.; de Wit, M.Y.; Klatser, P.R. Distribution and persistence of Mycobacterium leprae nasal carriage among a population in which leprosy is endemic in Indonesia. Trans. R. Soc. Trop. Med. Hyg. 1995, 89, 381–385. [Google Scholar] [CrossRef]
- Job, C.K.; Jayakumar, J.; Kearney, M.; Gillis, T.P. Transmission of leprosy: A study of skin and nasal secretions of household contacts of leprosy patients using PCR. Am. J. Trop. Med. Hyg. 2008, 78, 518–521. [Google Scholar] [CrossRef]
- Turankar, R.P.; Lavania, M.; Singh, M.; Sengupta, U.; Siva Sai, K.; Jadhav, R.S. Presence of viable Mycobacterium leprae in environmental specimens around houses of leprosy patients. Indian J. Med. Microbiol. 2016, 34, 315–321. [Google Scholar]
- Mohanty, P.S.; Naaz, F.; Katara, D.; Misba, L.; Kumar, D.; Dwivedi, D.K.; Tiwari, A.K.; Chauhan, D.S.; Bansal, A.K.; Tripathy, S.P.; et al. Viability of Mycobacterium leprae in the environment and its role in leprosy dissemination. Indian J. Dermatol. Venereol. Leprol. 2016, 82, 23–27. [Google Scholar] [CrossRef]
- Walsh, G.P.; Storrs, E.E.; Burchfield, H.P.; Cotrell, E.H.; Vidrine, M.F.; Binford, C.H. Leprosy-like disease occurring naturally in armadillos. J. Reticuloendothel. Soc. 1975, 18, 347–351. [Google Scholar]
- Truman, R.W.; Singh, P.; Sharma, R.; Busso, P.; Rougemont, J.; Paniz-Mondolfi, A.; Kapopoulou, A.; Brisse, S.; Scollard, D.M.; Gillis, T.P.; et al. Probable zoonotic leprosy in the southern United States. N. Engl. J. Med. 2011, 364, 1626–1633. [Google Scholar] [CrossRef]
- Avanzi, C.; Del-Pozo, J.; Benjak, A.; Stevenson, K.; Simpson, V.R.; Busso, P.; McLuckie, J.; Loiseau, C.; Lawton, C.; Schoening, J.; et al. Red squirrels in the British Isles are infected with leprosy bacilli. Science 2016, 354, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Plouvier, D.; Gomes, L.; Verweij, P.; Verlinden, N. Living Guianas; WWF: Gland, Switzerland, 2012; pp. 8–9. Available online: https://wwf.panda.org/?306012/The-Living-Guianas-Report (accessed on 10 December 2019).
- Helman, A. Kroniek van Eldorado. Boek I Folteraars over en Weer; Globe Pocket, In de Knipscheer: Amsterdam, The Netherlands, 1995; pp. 26–38. [Google Scholar]
- Van Andel, T.; Ruysschaert, S. Medicinale en Rituele Planten van Suriname; KIT Publishers: Amsterdam, The Netherlands, 2011; p. 7. [Google Scholar]
- Funk, V.; Hollowell, T.; Berry, P.; Kelloff, C.; Alexander, S.N. Checklist of the Plants of the Guiana Shield (Venezuela: Amazonas, Bolivar, Delta Amacuro; Guyana, Surinam, French Guiana); Contributions from the United States National Herbarium 55:1-584 (2007); Department of Botany National Museum of Natural History: Washington, DC, USA, 2007; p. 2. [Google Scholar]
- De Dijn, B. Natural History and Ecology of Suriname; LM publishers: Volendam, The Netherlands, 2018; pp. 4–480. [Google Scholar]
- Buddingh’, H. Geschiedenis van Suriname; Het Spectrum BV: Utrecht, the Netherlands, 1995; pp. 9–20. [Google Scholar]
- Van Stipriaan, A. Surinaams Contrast; KITLV Uitgeverij: Leiden, the Netherlands, 1995; pp. 33–37. [Google Scholar]
- Hoogbergen, W. ‘De Bosnegers zijn Gekomen’! Prometheus: Amsterdam, The Netherlands, 1992; pp. 1–38. [Google Scholar]
- Ankum-Houwink, J.C. Chinese kontraktarbeiders in de 19e eeuw. OSO Tijdschr. voor Surinamistiek 1985, 4, 181–186. [Google Scholar]
- Hoefte, R. Control and Resistance: Indentured Labor in Suriname. New West Indian Guide 1997, 61, 1–22. [Google Scholar] [CrossRef]
- Menke, H.; Pieters, T. Deel 1 Historische ontdekkingsreis; over kolonialisme, slavernij, een raadselachtige ziekte en een ongrijpbare bacterie. In De tenen van de Leguaan, Verhalen uit de Wereld van Surinaamse Leprapatiënten; Menke, H., Pieters, T., Reyme, M., Menke, J., Eds.; LM Publishers: Volendam, The Netherlands, 2019; pp. 11–72. [Google Scholar]
- Edmond, R. Leprosy and Empire A Medical and Cultural History; Cambridge University Press: Cambridge, UK, 2006; p. 55. [Google Scholar]
- Abernethy, D.B. The Dynamics of Global Dominance: European O zxverseas Empires. 1415–1980; Yale University Press: New Haven, CT, USA, 2001. [Google Scholar]
- Mertens, M. Van ‘Triomfalisme’ naar ‘Postkolonialisme’: Trends in de Geschiedschrijving van de Tropische Geneeskunde. Studium 2009, 2, 78–91. [Google Scholar] [CrossRef]
- Arnold, D. Introduction: Disease, Medicine and Empire. In Imperial Medicine and Indigenous Society; Arnold, D., Ed.; Manchester University Press: Manchester, UK, 1998. [Google Scholar]
- MacLeod, R. Preface. In Disease, Medicine and Empire: Perspectives on Western Medicine and the Experience of European Expansion; MacLeod, R., Lewis, M., Eds.; Routledge: London, UK, 1988. [Google Scholar]
- Menke, H.E.; Snelders, S.; Pieters, T. Leprosy Control and Contagionism in Suriname. Acad. J. Sur. 2011, 2, 168–175. [Google Scholar]
- Reyme, M.; Menke, J. Deel 2 De wereld van de Surinaamse leprapatiënt I Verhalen over liefde en haat, geloof en vloek, medeleven en uitsluiting. In De Tenen van de Leguaan Verhalen uit de Wereld van Surinaamse Leprapatiënten; Menke, H., Pieters, T., Reyme, M., Menke, J., Eds.; LM Publishers: Volendam, The Netherlands, 2019; pp. 73–134. [Google Scholar]
- Ramdas, S.; Menke, H.; Pieters, T.; Menke, J. Deel 3 De wereld van de Surinaamse leprapatiënt II Analyse: Over stigma, pluralisme, treef en tyina. In De Tenen van de Leguaan Verhalen uit de Wereld van Surinaamse Leprapatiënten; Menke, H., Pieters, T., Reyme, M., Menke, J., Eds.; LM Publishers: Volendam, The Netherlands, 2019; pp. 162–163. [Google Scholar]
- Weiss, H. Vier maanden in Suriname; G. F. Callenbach: Nijkerk, The Netherlands, 1915; pp. 61–72. [Google Scholar]
- Schuitemaker, E.P. De Lepra en de Gouvernementsleproserie in Suriname met Kaart en elf Platen; J.H. de Bussy: Amsterdam, The Netherlands, 1915. [Google Scholar]
- Snelders, S. Leprosy and Colonialism. Suriname under Dutch rule, 1750–1950; Manchester University Press: Manchester, UK, 2017. [Google Scholar]
- Proust, A. Essai sur L’hygiène Internationale, Ses Applications Contre la Peste, la Fièvre Jaune et le Choléra Asiatique (Avec une Carte Indiquant la Marche des Epidémies de Choléra); G. Masson: Paris, France, 1873; pp. 52–53. [Google Scholar]
- Weismann, G. Ebola, dynamin, and the cordon sanitaire of Dr. Adrien Proust. FASEB J. 2015, 29, 1–4. [Google Scholar] [CrossRef][Green Version]
- Leydesdorff, S. De Mensen en de Woorden; J.M. Meulenhoff: Amsterdam, The Netherlands, 2004; pp. 23–42. [Google Scholar]
- Tió-Coma, M.; Wijnands, T.; Pierneef, L.; Schilling, A.K.; Alam, K.; Roy, J.C.; Faber, W.R.; Menke, H.; Pieters, T.; Stevenson, K.; et al. Detection of Mycobacterium leprae DNA in soil: Multiple needles in the haystack. Sci. Rep. 2019, 9, 3165. [Google Scholar] [CrossRef]
- Van Dissel, J.T.; Pieters, T.; Geluk, A.; Maat, G.; Menke, H.E.; Tió-Coma, M.; Altena, E.; Laros, J.F.J.; Adhin, M.R. Archival, paleopathological and aDNA-based techniques in leprosy research and the case of Father Petrus Donders at the Leprosarium ‘Batavia’, Suriname. Int. J. Paleopathol. 2019, 27, 1–8. [Google Scholar] [CrossRef]
- Snelders, S. Leprosy and Slavery in Suriname: Godfried Schilling and the Framing of a Racial Pathology in the Eighteenth Century. Soc. Hist. Med. 2013, 26, 432–450. [Google Scholar] [CrossRef]
- Fermin, P. Traité des Maladies Fréquentes á Surinam et des Remèdes le plus Propres à les Guérir. Jacques Lekens: Maastricht, The Netherlands, 1764; p. 127. [Google Scholar]
- Schilling, G.W. Verhandeling over de Melaatschheid. Ph.D. Thesis, Utrecht University, Utrecht, The Netherlands, 1769. [Google Scholar]
- Van Hasselaar, A. Beschrijving der in de Kolonie Suriname Voorkomende Elephantiasis en Lepra (Melaatschheid). Ph.D. Thesis, Amsterdam University, Amsterdam, The Netherlands, 1835. [Google Scholar]
- Ter Beek, J.P. Dissertatio Inauguralis de Elephantiasis Surinamensis. Ph.D. Thesis, Leiden University, Leiden, The Netherlands, 1841. [Google Scholar]
- Drognat Landré, C.L. De la Contagion, Seule Cause de la Propagation de la Lèpre; Baillière: Paris, France, 1869. [Google Scholar]
- Danielssen, D.C.; Boeck, C.W. Traité de la Spédalskhed ou Elephantiasis des Grecs. Traduit du Norwégien sous les Yeux de Mr Danielssen par L. A. Cosson (de Nogaret) avec un Atlas de 24 Planches Colorées; Baillière: Paris, France, 1848. [Google Scholar]
- Report on Leprosy by the Royal College of Physicians. Prepared for, and Published by Her Majesty ´s Secretary of State for the Colonies; with an Appendix; Eyre and Spottiswoode: London, UK, 1867.
- Irgens, L.M. Leprosy in Norway: An interplay of research and public health work. Int. J. Lepr. Other Mycobact. Dis. 1973, 41, 189–198. [Google Scholar]
- Menke, H.E.; Faber, W.R.; Pieters, T. Charles Louis Drognat Landré and Gerhard Henrik Armauer Hansen. Contribution from a Dutch colony to the discovery of the leprosy bacterium. Lepr. Rev. 2010, 81, 82–86. [Google Scholar] [PubMed]
- Snelders, S.; van Bergen, L.; Huisman, M. Leprosy and the Colonial Gaze: Comparing the Dutch West and East Indies, 1750–1950. Soc. Hist. Med. 2020. Available online: https://academic.oup.com/shm/advance-article/doi/10.1093/shm/hkz079/5681883?guestAccessKey=554dd703-2e1e-4253-9328-68d6e9d1efaf (accessed on 6 January 2020).
- Ackerknecht, E.H.; Fielding, H. Garrison lecture: Anticontagionism between 1821 and 1867. Bull Hist. Med. 1948, 22, 562–593. [Google Scholar]
- Schiltkamp, J.A.; de Smidt, J.T. West Indisch Plakaatboek. Plakaten, Ordonnantiën en Andere Wetten Uitgevaardigd in Suriname II, 1761–1816; S. Emmering: Amsterdam, The Netherlands, 1973. [Google Scholar]
- Vernooij, J. Een opvallende relatie. De Rooms Katholieke kerk en lepra in Suriname. OSO Tijdschr. voor Surinamistiek 2003, 22, 62–68. [Google Scholar]
- Kapper, A. Plantages langs de Commewijnerivier, de goudkust van Suriname. Vitruvius 2011, 4, 36–42. [Google Scholar]
- Bosser, A. Beknopte Geschiedenis der Katholieke Missie in Suriname; M. Alberts: Gulpen, The Netherlands, 1884; p. 171. [Google Scholar]
- van der Aa, A.J. Aardrijkskundig Woordenboek der Nederlanden, Tweede deel B; Jacobus Noorduyn: Gorinchem, The Netherlands, 1840; p. 168. [Google Scholar]
- Foucault, M. Madness and civilization: A History of Insanity in the Age of Reason; Routledge: London, UK, 2001; pp. 38–40. [Google Scholar]
- Lens, T. Lepra in Suriname. Elsevier’s Geïllustreerd Maandschr. 1895, 5, 521–552. [Google Scholar]
- Postma, J. De leprozerie Bethesda tussen 1897 en 1928. OSO Tijdschr. voor Surinamistiek 2003, 22, 69–82. [Google Scholar]
- Zaalberg, H.H. De Melaatschen in Suriname en hun Verpleging; G.C.Visser: Den Haag, The Netherlands, 1904; pp. 18–19. [Google Scholar]
- Merritt, J.G.; Satterlee, A. Historical Dictionary of the Salvation Army; Rowman and Littlefield: London, UK, 2017; pp. 203–209. [Google Scholar]
- Hira, S. Eddy Jharap Geloof in Eigen Kunnen; Amrit Consultancy: Den Haag, The Netherlands, 2011; pp. 45–65. [Google Scholar]
- Van Hinte-Rustwijk, D.; van Steenderen-Rustwijk, G. Van bedrijfsschade tot verzuilde paria naar ex-Hansen cliënt. OSO Tijdschr. voor Surinamistiek 2003, 22, 10–20. [Google Scholar]
- Haekel, J. Totemism. in Encyclopaedia Britannica. Available online: https://www.britannica.com/topic/totemism-religion (accessed on 6 January 2020).
- Vruggink, H. Javaanse volksverhalen: Een eerste kennismaking. Oso Tijdschr. voor Surinamistiek 1989, 8, 170–183. [Google Scholar]
- Landré, C. Over de OORZAKEN der verbreiding van de lepra. Een Waarschuwend Woord Hoofdzakelijk Gericht tot de Bewoners van Suriname; Martinus Nijhoff: Den Haag, The Netherlands, 1889. [Google Scholar]
- Lampe, P.H.J. ‘Het Surinaams treefgeloof’ Een volksgeloof betreffende het ontstaan van de melaatschheid. De West-Indische Gids 1929, 10, 545–568. [Google Scholar] [CrossRef]
- Benjamins, H.D. Treef en lepra in Suriname. De West-Indische Gids 1930, 11, 187–218. [Google Scholar] [CrossRef]
- Van Andel, T. The reinvention of household medicine by enslaved Africans in Suriname. Soc. Hist. Med. 2016, 29, 676–694. [Google Scholar] [CrossRef]
- Girvan, N. Reinterpreting the Caribbean. In New Caribbean Thought; Meeks, B., Lindahl, F., Eds.; University of the West Indies Press: Kingston, Jamaica, 2001. [Google Scholar]
- Anderson, N.R. “It’s Not Catching”: Hansen Home and the Local Knowledge of Leprosy in the Federation of St. Kitts and Nevis, West Indies. Master’s Thesis, University of Tennessee, Knoxville, Tennessee, 2005. Available online: http://trace.tennessee.edu/utk_gradthes/580 (accessed on 24 March 2020).
- Gampat, R. Guyana from Slavery to the Present. Volume 2. Major Diseases; Xlibris: Bloomington, Indiana, 2015; pp. 623–648. [Google Scholar]
- De Souza-Araujo, H.C. A la lepra na Guiana Francêsa in: O problema da lepra na America do Sul. Memórias do Inst. Oswaldo Cruz 1945, 43, 583–598. [Google Scholar] [CrossRef]
- White, C. Explaining a Complex Disease Process: Talking to Patients about Hansen’s Disease (Leprosy) in Brazil. Med Anthropol. Q. 2008, 19, 310–330. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, M.B.; Portela, J.M.; Li, W.; Jackson, M.; Gonzalez-Juarrero, M.; Hidalgo, A.S.; Belisle, J.T.; Bouth, R.C.; Gobbo, A.R.; Barreto, J.G.; et al. Evidence of zoonotic leprosy in Pará, Brazilian Amazon, and risks associated with human contact or consumption of armadillos. PLoS. Negl. Trop. Dis. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- WHO Weekly Epidemiological Record 2019, 94, 389–412. Available online: https://zeroleprosy.org/wp-content/uploads/2020/02/WHO-August-2019-Leprosy-Report.pdf (accessed on 24 March 2020).
- Ploemacher, T.; Faber, W.R.; Menke, H.; Rutten, V.; Pieters, T. Reservoirs and Transmission Routes of Leprosy; A Systematic Review. PLoS. Negl. Trop. Dis. Under review.
- Sitalsing, K. Boeroes een Familiegeschiedenis van Witte Surinamers; Uitgeverij Atlas Contact: Amsterdam, The Netherlands, 2016; p. 30. [Google Scholar]
| 1 | We are fully aware of the disadvantages of the word leprosy, as explained by Deps and Cruz (2020, see reference [2]), but we have deliberately chosen to use the word in this historical article when necessary, in addition to ‘Hansen’s disease.’ |
| 2 | The transcribed interviews are kept in the National Archive of Suriname (www.nationaalarchief.sr). |
| 3 | In their paper, Snelders, et al. use the term ‘colonial gaze’ to refer to the ways in which plantation owners, colonial administrators, doctors, and surgeons legitimised compulsory segregation of leprosy sufferers who were no longer of use on the plantation or as labourers in general.). |
| 4 | Publicatie van 15 september 1830. Gouvernements Blad van Suriname No 13. |
| 5 | Landsverordening van 23 maart 1960 houdende bepalingen ter wering en bestrijding van lepra. Gouvernementsblad van Suriname no 37, 1960. |
| 6 | Peerke (Petrus) Donders became an icon of Roman Catholic missionary work and was beatified by the Pope in 1982. |
| 7 | Bueno de Mesquita, S.J. Leprosy Annual report of the year 1952. Van der Kuyp files, National Archive of Suriname (www.nationaalarchief.sr). |
| 8 | Surinamese newspaper ‘de West: nieuwsblad uit en voor Suriname’, 23-02-1948. Available online: https://www.delpher.nl/nl/kranten. |
| 9 | Tyina is the Surinamese spelling of this word. It can be found in the literature as tchina and kina. |
| 10 | These are elder female leprosy inmates (generally of African-Surinamese descent) who assisted, informed, and advised the European caretakers in the leprosaria on matters related to life in Suriname. |
| 11 | Winti is a traditional African-Surinamese religion. |
| 12 | Treef is the Dutch spelling and trefu is the Surinamese spelling of this word. |
| 13 | |
| 14 | Personal information (received on 28 October 2019) from Roxane Schaub, leprosy researcher in French Guyana. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).