Gastrointestinal Complaints and Correlations with Self-Reported Macronutrient Intake in Independent Groups of (Ultra)Marathon Runners Competing at Different Distances
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Procedures
2.3.1. Screening Questionnaire
2.3.2. Food and Fluid Exercise Questionnaire (FFEQ)
2.3.3. Post-Race Complaints Questionnaire
2.4. Data Analysis
3. Results
3.1. Characteristics
3.2. Gastrointestinal and Other Exercise Related Complaints during Exercise
3.3. Gastrointestinal and Other Exercise Related Complaints after Exercise
3.4. Relationship between Gastrointestinal Complaints during and after Exercise
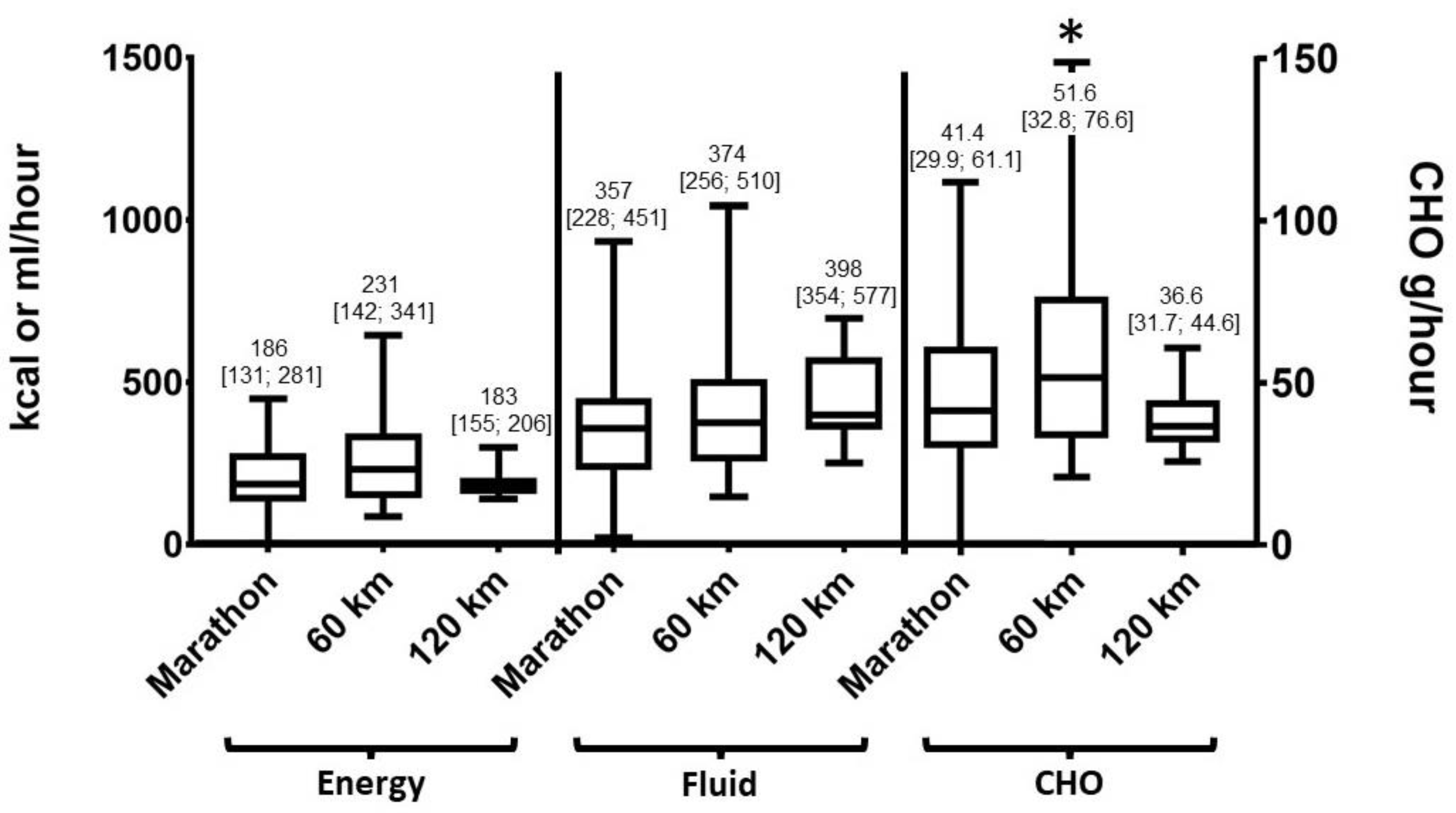
3.5. Macronutrient Intake
3.6. Correlations between GI Complaints and Macronutrient Intake
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Pfeiffer, B.; Stellingwerff, T.; Hodgson, A.B.; Randell, R.; Pöttgen, K.; Res, P.; Jeukendrup, A.E. Nutritional intake and gastrointestinal problems during competitive endurance events. Med. Sci. Sports Exerc. 2012, 44, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Stuempfle, K.J.; Hoffman, M.D.; Hew-Butler, T. Association of gastrointestinal distress in ultramarathoners with race diet. Int. J. Sport Nutr. Exerc. Metab. 2013, 23, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Wardenaar, F.C.; Dijkhuizen, R.; Ceelen, I.J.M.; Jonk, E.; De Vries, J.H.M.; Witkamp, R.F.; Mensink, M. Nutrient intake by ultramarathon runners: Can they meet recommendations? Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Wardenaar, F.C.; Hoogervorst, D.; Versteegen, J.J.; van der Burg, N.; Lambrechtse, K.J.; Bongers, C.C.W.G. Real-Time Observations of Food and Fluid Timing During a 120 km Ultramarathon. Front. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Karhu, E.; Forsgård, R.A.; Alanko, L.; Alfthan, H.; Pussinen, P.; Hämäläinen, E.; Korpela, R. Exercise and gastrointestinal symptoms: Running-induced changes in intestinal permeability and markers of gastrointestinal function in asymptomatic and symptomatic runners. Eur. J. Appl. Physiol. 2017, 117, 2519–2526. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, E.P.; Burini, R.C.; Jeukendrup, A. Gastrointestinal complaints during exercise: Prevalence, etiology, and nutritional recommendations. Sports Med. 2014, 44, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.J.S.; Snipe, R.M.J.; Kitic, C.M.; Gibson, P.R. Systematic review: Exercise-induced gastrointestinal syndrome-implications for health and intestinal disease. Aliment. Pharmacol. Ther. 2017, 46, 246–265. [Google Scholar] [CrossRef]
- Peters, H.P.; van Schelven, F.W.; Verstappen, P.A.; de Boer, R.W.; Bol, E.; Erich, W.B.; van der, T.C.R.; de Vries, W.R. Gastrointestinal problems as a function of carbohydrate supplements and mode of exercise. Med. Sci. Sports Exerc. 1993, 25, 1211–1224. [Google Scholar] [CrossRef]
- Ter Steege, R.W.F.; Van Der Palen, J.; Kolkman, J.J. Prevalence of gastrointestinal complaints in runners competing in a long-distance run: An internet-based observational study in 1281 subjects. Scand. J. Gastroenterol. 2008, 43, 1477–1482. [Google Scholar] [CrossRef]
- Stuempfle, K.J.; Hoffman, M.D.; Weschler, L.B.; Rogers, I.R.; Hew-Butler, T. Race diet of finishers and non-finishers in a 100 mile (161 km) mountain footrace. J. Am. Coll. Nutr. 2011, 30, 529–535. [Google Scholar] [CrossRef]
- Jeukendrup, A.E. Training the Gut for Athletes. Sports Med. 2017, 47, 101–110. [Google Scholar] [CrossRef]
- Rehrer, N.J.; van Kemenade, M.; Meester, W.; Brouns, F.; Saris, W.H.M. Gastrointestinal Complaints in Relation to Dietary Intake in Triathletes. Int. J. Sport Nutr. 1992, 2, 48–59. [Google Scholar] [CrossRef]
- Burke, L.M.; Jones, A.M.; Mooses, M. Contemporary Nutrition Strategies to Optimize Performance in Distance Runners and Race Walkers. Bioenergetic and Physiological Support for the Periodized Training Programs of Distance Athletes. Hum. Kinet. J. 2019, 29, 117–129. [Google Scholar]
- Ørtenblad, N.; Westerblad, H.; Nielsen, J. Muscle glycogen stores and fatigue. J. Physiol. 2013. [Google Scholar] [CrossRef]
- Jeukendrup, A. A step towards personalized sports nutrition: Carbohydrate intake during exercise. Sports Med. 2014, 44, 25–33. [Google Scholar] [CrossRef]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J. Acad. Nutr. Diet. 2016, 116, 501–528. [Google Scholar] [CrossRef]
- Stellingwerff, T. Competition Nutrition Practices of Elite Ultramarathon Runners. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 93–99. [Google Scholar] [CrossRef]
- Hew-Butler, T.; Rosner, M.H.; Fowkes-Godek, S.; Dugas, J.P.; Hoffman, M.D.; Lewis, D.P.; Maughan, R.J.; Miller, K.C.; Montain, S.J.; Rehrer, N.J. Statement of the 3rd International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Br. J. Sports Med. 2015, 49, 1432–1446. [Google Scholar] [CrossRef]
- Hoffman, M.D.; Stellingwerff, T.; Costa, R.J.S. Considerations for ultra-endurance activities: Part 2—hydration. Res. Sport Med. 2019, 27, 182–194. [Google Scholar] [CrossRef]
- Costa, R.J.S.; Tarnopolsky, M.; Hoffman, M.D. Nutrition for Ultramarathon Running: Trail, Track, and Road. Hum. Kinet. J. 2019, 29, 130–140. [Google Scholar] [CrossRef]
- Moran, S.T.; Dziedzic, C.E.; Cox, G.R. Feeding strategies of a female athlete during an ultraendurance running event. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 347–351. [Google Scholar] [CrossRef]
- Martinez, S.; Aguilo, A.; Rodas, L.; Lozano, L.; Moreno, C.; Tauler, P. Energy, macronutrient and water intake during a mountain ultramarathon event: The influence of distance. J. Sports Sci. 2018, 36, 333–339. [Google Scholar] [CrossRef]
- Kruseman, M.; Bucher, S.; Bovard, M.; Kayser, B.; Bovier, P.A. Nutrient intake and performance during a mountain marathon: An observational study. Eur. J. Appl. Physiol. 2005, 94, 151–157. [Google Scholar] [CrossRef]
- Burke, L.M.; Deakin, V. Clinical Sports Nutrition, 2nd ed.; McGraw-Hill Education: New York, NY, USA, 2010; p. 848. [Google Scholar]
- Burke, L.M.; Hawley, J.A.; Wong, S.H.S.; Jeukendrup, A.E. Carbohydrates for training and competition. J. Sports Sci. 2011. [Google Scholar] [CrossRef]
- Costa, R.J.S.; Crockford, M.J.; Moore, J.P.; Walsh, N.P. Heat acclimation responses of an ultra-endurance running group preparing for hot desert-based competition. Eur. J. Sport Sci. 2014, 14, 37–41. [Google Scholar] [CrossRef]
- Van Nieuwenhoven, M.A.; Brouns, F.; Kovacs, E.M.R. The effect of two sports drinks and water on GI complaints and performance during an 18-km run. Int. J. Sports Med. 2005, 26, 281–285. [Google Scholar] [CrossRef]
- Rijksinstituut voor Volksgezondheid en Milieu. Nederlands Voedingsstoffenbestand (NEVO). 2016. Available online: https://nevo-online.rivm.nl/ (accessed on 8 October 2018).
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 1998. [Google Scholar]
- Glace, B.; Murphy, C.; McHugh, M. Food and fluid intake and disturbances in gastrointestinal and mental function during an ultramarathon. Int. J. Sport Nutr. Exerc. Metab. 2002, 12, 414–427. [Google Scholar] [CrossRef]
- Moses, F.M. Exercise-associated intestinal ischemia. Curr. Sports Med. Rep. 2005, 4, 91–95. [Google Scholar] [CrossRef]
- van Wijck, K.; Verlinden, T.J.M.; van Eijk, H.M.H.; Dekker, J.; Buurman, W.A.; Dejong, C.H.C.; Lenaerts, K. Novel multi-sugar assay for site-specific gastrointestinal permeability analysis: A randomized controlled crossover trial. Clin. Nutr. 2013, 32, 245–251. [Google Scholar] [CrossRef]
- Jonvik, K.L.; Lenaerts, K.; Smeets, J.S.J.; Kolkman, J.J.; Van Loon, L.J.C.; Verdijk, L.B. Sucrose but Not Nitrate Ingestion Reduces Strenuous Cycling-induced Intestinal Injury. Med. Sci. Sports Exerc. 2019, 51, 436–444. [Google Scholar] [CrossRef]
- Snipe, R.M.J.; Khoo, A.; Kitic, C.M.; Gibson, P.R.; Costa, R.J.S. Carbohydrate and protein intake during exertional heat stress ameliorates intestinal epithelial injury and small intestine permeability. Appl. Physiol. Nutr. Metab. 2017, 42, 1283–1292. [Google Scholar] [CrossRef]
- Costa, R.J.S.; Miall, A.; Khoo, A.; Rauch, C.; Snipe, R.; Camões-Costa, V.; Gibson, P. Gut-training: The impact of two weeks repetitive gut-challenge during exercise on gastrointestinal status, glucose availability, fuel kinetics, and running performance. Appl. Physiol. Nutr. Metab. 2017, 42, 547–557. [Google Scholar] [CrossRef]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires—A review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef]
- Sunami, A.; Sasaki, K.; Suzuki, Y.; Oguma, N.; Ishihara, J.; Nakai, A.; Yasuda, J.; Yokoyama, Y.; Yoshizaki, T.; Tada, Y. Validity of a Semi-Quantitative Food Frequency Questionnaire for Collegiate Athletes. J. Epidemiol. 2016, 26, 284–291. [Google Scholar] [CrossRef]

| Characteristics | Combined Distances | Marathon | 60 km | 120 km | Significance |
|---|---|---|---|---|---|
| n = 149 | n = 98 | n = 43 | n = 8 | p-value | |
| Gender (M/F) | 119/30 | 75/23 | 36/7 | 8/0 | – |
| Age (years) | 43 (36;51) | 44 (35;51) | 43 (38;53) | 47 (41;51) | 0.50 |
| Weight (kg) | 73 (68;81) | 73 (68;81) | 74 (69;82) | 71 (64.5;73.75) | 0.27 |
| Height (cm) | 181 (175;185) | 180 (173;184) | 183 (178;187) | 183 (179;185) | 0.10 |
| Speed (km/h) | 9.9 (9.1;11.3) | 10.3 (9.0;11.6) | 9.5 (9.1;10.3) | 9.6 (9.0;10.3) | 0.13 |
| Finish time (hh:mm) | – | 4:16 (3:44;4;38) | 5:50 (5:10;6:40) | 12:30 (11:39;13:20) | – |
| Complaints During | Complaints After | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Type of Complaint | Category | Marathon n = 98 | 60 km n = 43 | 120 km n = 8 | p-Value | Marathon N = 75 | 60 km n = 43 | 120 km n = 8 | p-Value |
| Upper GI complaints | |||||||||
| Belching | Total | 41.7% | 44.2% | 62.5% | 0.53 | 9.3% | 14.0% | 25.0% | 0.30 |
| Severe | 6.1% | 2.3% | 25.0% | 0.048C | 1.3% | 0.0% | 25.0% | 0.000C | |
| Bloating | Total | 20.4% | 20.9% | 50.0% | 0.15 | 12.0% | 11.6% | 25.0% | 0.57 |
| Severe | 3.1% | 2.3% | 25.0% | 0.008C | 0.0% | 2.3% | 12.5% | 0.38 | |
| Reflux | Total | 17.3% | 23.3% | 37.5% | 0.33 | 2.7% | 11.6% | 12.5% | 0.12 |
| Severe | 5.1% | 0.0% | 25.0% | 0.009C | 0.0% | 0.0% | 12.5% | 0.001C | |
| Nausea | Total | 14.2% | 25.6% | 37.5% | 0.11 | 12.0% | 7.0% | 37.5% | 0.047C |
| Severe | 2.0% | 4.7% | 12.5% | 0.25 | 1.3% | 2.3% | 12.5% | 0.15 | |
| Stomach cramps | Total | 11.2% | 18.7% | 25.0% | 0.34 | 5.3% | 11.6% | 37.5% | 0.012C |
| Severe | 6.1% | 4.7% | 12.5% | 0.69 | 2.7% | 2.3% | 12.5% | 0.30 | |
| Heartburn | Total | 4.1% | 11.6% | 12.5% | 0.21 | 2.6% | 11.6% | 0.0% | 0.10 |
| Severe | 1.0% | 0.0% | 0.0% | 0.77 | 1.3% | 2.3% | 0.0% | 0.86 | |
| Vomiting | Total | 1.0% | 4.7% | 0.0% | 0.34 | 2.6% | 0.0% | 0.0% | 0.50 |
| Severe | 1.0% | 0.0% | 0.0% | 0.77 | 1.3% | 0.0% | 0.0% | 0.71 | |
| Lower GI complaints | |||||||||
| Flatulence | Total | 28.5% | 39.5% | 75.0% | 0.020C | 22.7% | 16.3% | 50.0% | 0.11 |
| Severe | 7.1% | 9.3% | 25.0% | 0.23 | 6.7% | 2.3% | 12.5% | 0.42 | |
| Side ache | Total | 15.3% | 34.9% | 12.5% | 0.027A | 2.7% | 0.0% | 12.5% | 0.10 |
| Severe | 4.1% | 11.6% | 12.5% | 0.21 | 2.7% | 0.0% | 12.5% | 0.10 | |
| Urge to defecate | Total | 13.3% | 18.6% | 37.5% | 0.18 | 6.7% | 16.3% | 12.5% | 0.27 |
| Severe | 5.1% | 9.3% | 25.0% | 0.10 | 2.7% | 2.3% | 0.0% | 0.90 | |
| Intestinal cramps | Total | 10.2% | 23.2% | 25.0% | 0.10 | 5.3% | 13.9% | 25.0% | 0.11 |
| Severe | 4.1% | 2.3% | 12.5% | 0.41 | 4.0% | 2.3% | 12.5% | 0.40 | |
| Abdominal pain | Total | 10.2% | 14.0% | 25.0% | 0.42 | 6.6% | 4.7% | 0.0% | 0.698 |
| Severe | 4.1% | 0.0% | 12.5% | 0.16 | 1.3% | 0.0% | 0.0% | 0.712 | |
| Diarrhea | Total | 1.0% | 0.0% | 12.5% | 0.017C | 6.6% | 7.0% | 12.5% | 0.80 |
| Severe | 0.0% | 0.0% | 12.5% | 0.000C | 1.3% | 2.3% | 0.0% | 0.15 | |
| Loose stool | Total | 1.0% | 2.3% | 0.0% | 0.78 | 1.3% | 0.0% | 0.0% | 0.71 |
| Severe | 1.0% | 2.3% | 0.0% | 0.78 | 0.0% | 0.0% | 0.0% | 1.00 | |
| Other exercise related complaints | |||||||||
| Muscle cramps | Total | 44.9% | 46.5% | 12.5% | 0.19 | 30.6% | 51.1% | 62.5% | 0.025AC |
| Severe | 21.4% | 20.9% | 12.5% | 0.84 | 13.3% | 20.9% | 50.0% | 0.034C | |
| Urge to urinate | Total | 43.8% | 53.5% | 62.5% | 0.40 | 10.7% | 13.9% | 12.5% | 0.89 |
| Severe | 18.4% | 7.0% | 12.5% | 0.21 | 4.0% | 2.3% | 0.0% | 0.77 | |
| Headache | Total | 11.2% | 7.0% | 12.5% | 0.72 | 16.3% | 7.0% | 12.5% | 0.13 |
| Severe | 2.0% | 0.0% | 0.0% | 0.59 | 2.0% | 2.3% | 0.0% | 0.90 | |
| Dizziness | Total | 9.2% | 2.3% | 37.5% | 0.005C | 5.3% | 7.0% | 25.0% | 0.11 |
| Severe | 4.1% | 0.0% | 25.0% | 0.004C | 1.3% | 0.0% | 12.5% | 0.034* | |
| Complaints During | Complaints After | ||||||
|---|---|---|---|---|---|---|---|
| Type of Complaint | Category | Marathon vs. 60 km (A) | 60 km vs. 120 km (B) | Marathon vs. 120 km (C) | Marathon vs. 60 km (A) | 60 km vs. 120 km (B) | Marathon vs. 120 km (C) |
| Upper GI complaints | |||||||
| Belching | Total | – | – | – | – | – | – |
| Severe | – | – | η² = −0.007, p = 0.001 | – | – | η² = −0.014, p = 0.001 | |
| Bloating | Total | – | – | – | – | – | – |
| Severe | – | – | η² = −0.010, p = 0.005 | – | – | – | |
| Reflux | Total | – | – | – | – | – | – |
| Severe | – | – | η² = −0.008, p = 0.030 | – | – | η² = −0.004, p = 0.002 | |
| Nausea | Total | – | – | – | – | – | η² = −0.018, p = 0.044 |
| Severe | – | – | – | – | – | – | |
| Stomach cramps | Total | – | – | – | – | – | η² = −0.026, p = 0.002 |
| Severe | – | – | – | – | – | – | |
| Lower GI complaints | |||||||
| Flatulence | Total | – | – | η² = −0.048, p = 0.006 | – | – | – |
| Severe | – | – | – | – | – | – | |
| Side ache | Total | η² = −0.025, p = 0.009 | – | – | – | – | – |
| Severe | – | – | – | – | – | – | |
| Diarrhea | Total | – | – | η² = −0.003, p = 0.021 | – | – | – |
| Severe | – | – | η² = −0.003, p < 0.001 | – | – | – | |
| Other exercise related complaints | |||||||
| Muscle cramps | Total | – | – | – | η² = −0.028, p = 0.036 | – | η² = −0.039, p = 0.032 |
| Severe | – | – | – | – | – | η² = −0.035, p = 0.009 | |
| Dizziness | Total | – | – | η² = −0.018, p = 0.013 | – | – | – |
| Severe | – | – | η² = −0.009, p = 0.014 | – | – | – | |
| Type of Complaint | All Distances (n = 149) | Marathon (n = 98) | 60 km (n = 43) | 120 km (n = 8) |
|---|---|---|---|---|
| Upper GI complaints | ||||
| Belching | – | 0.25 (p = 0.032) (0.05:0.43) | – | – |
| Reflux | 0.36 (p < 0.001) (0.21:0.49) | – | 0.49 (p = 0.001) (0.22:0.69) | – |
| Nausea | 0.36 (p < 0.001) (0.21:0.49) | 0.38 (p = 0.001) (0.60:0.80) | – | – |
| Stomach cramps | – | 0.32 (p = 0.005) (0.13:0.49) | 0.61 (p < 0.001) (0.38:0.77) | – |
| Vomiting | 0.42 (p < 0.001) (0.28:0.54) | 0.71 (p < 0.001) (0.60:0.80) | – | – |
| Lower GI complaints | ||||
| Flatulence | 0.43 (p < 0.001) (0.29:0.55) | 0.49 (p < 0.001) (0.32:0.63) | – | – |
| Side ache | – | – | – | 1.00 (p < 0.001) (1.00:1.00) |
| Urge to defecate | 0.35 (p < 0.001) (0.20:0.49) | – | 0.65 (p < 0.001) (0.43:0.79) | – |
| Intestinal cramps | 0.38 (p < 0.001) (0.23:0.51) | 0.33 (p = 0.004) (0.14:0.49) | 0.40 (p = 0.007) (0.12:0.63) | – |
| Abdominal pain | – | 0.25 (p = 0.031) (0.05:0.43) | – | – |
| Diarrhea | 0.46 (p < 0.001) (0.33:0.58) | 0.43 (p < 0.001) (0.25:0.58) | – | 1.00 (p < 0.001) (1.00:1.00) |
| Other exercise related complaints | ||||
| Muscle cramps | 0.44 (p < 0.001) (0.30:0.56) | 0.43 (p < 0.001) (0.25:0.58) | 0.54 (p < 0.001) (0.28:0.72) | – |
| Urge to urinate | 0.29 (p = 0.001) (0.13:0.43) | 0.36 (p = 0.002) (0.17:0.52) | – | – |
| Headache | – | – | – | 1.00 (p < 0.001) (1.00:1.00) |
| Dizziness | – | 0.33 (p = 0.004) (0.14:0.50) | – | – |
| Type of Complaint | All Distances (n = 149) | Marathon (n = 98) | 60 km (n = 43) | 120 km (n = 8) |
|---|---|---|---|---|
| Upper GI complaints | ||||
| Belching | −0.19 Fiber/h (p = 0.022) (0.03:0.34) | −0.23 Fat/h (p = 0.026) (−0.41:−0.03) −0.25 Fiber/h (p = 0.014) (−0.43:−0.05) | – | – |
| Reflux | – | – | 0.31 Fiber/h (p = 0.042) (0.01:0.56) | – |
| Vomiting | −0.17 Fat/h (p = 0.042) (0.01:0.32) | – | – | – |
| Lower GI complaints | ||||
| Urge to defecate | – | – | – | -0.78 CHO/h (p = 0.021) (−0.96:−0.18) |
| Intestinal cramps | – | – | – | 0.77 PRO/h (p = 0.026) (0.14:0.96) |
| Abdominal pain | −0.17 Fluid/h (p = 0.042) (−0.32:−0.01) | −0.23 Kcal/h (p = 0.039) (−0.41:−0.04) −0.20 PRO/h (p = 0.048) (−0.38:−0.01) 0.22 Fat/h (p = 0.033) (−0.40:−0.02) | – | – |
| Diarrhea | −0.17 CHO/h (p = 0.040) (−0.32:−0.01) | – | – | – |
| Other exercise related complaints | ||||
| Urge to urinate | – | – | 0.33 Kcal/h (p = 0.030) (0.04:0.58) 0.34 CHO/h (p = 0.028) (0.04:0.58) | – |
| Dizziness | – | −0.21 Kcal/h (p = 0.039) (−0.40:−0.02) −0.20 CHO/h (p = 0.049) (−0.39:−0.01) | – | – |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoogervorst, D.; van der Burg, N.; Versteegen, J.J.; Lambrechtse, K.J.; Redegeld, M.I.; Cornelissen, L.A.J.; Wardenaar, F.C. Gastrointestinal Complaints and Correlations with Self-Reported Macronutrient Intake in Independent Groups of (Ultra)Marathon Runners Competing at Different Distances. Sports 2019, 7, 140. https://doi.org/10.3390/sports7060140
Hoogervorst D, van der Burg N, Versteegen JJ, Lambrechtse KJ, Redegeld MI, Cornelissen LAJ, Wardenaar FC. Gastrointestinal Complaints and Correlations with Self-Reported Macronutrient Intake in Independent Groups of (Ultra)Marathon Runners Competing at Different Distances. Sports. 2019; 7(6):140. https://doi.org/10.3390/sports7060140
Chicago/Turabian StyleHoogervorst, Daan, Nancy van der Burg, Joline J. Versteegen, Karin J. Lambrechtse, Martijn I. Redegeld, Larissa A. J. Cornelissen, and Floris C. Wardenaar. 2019. "Gastrointestinal Complaints and Correlations with Self-Reported Macronutrient Intake in Independent Groups of (Ultra)Marathon Runners Competing at Different Distances" Sports 7, no. 6: 140. https://doi.org/10.3390/sports7060140
APA StyleHoogervorst, D., van der Burg, N., Versteegen, J. J., Lambrechtse, K. J., Redegeld, M. I., Cornelissen, L. A. J., & Wardenaar, F. C. (2019). Gastrointestinal Complaints and Correlations with Self-Reported Macronutrient Intake in Independent Groups of (Ultra)Marathon Runners Competing at Different Distances. Sports, 7(6), 140. https://doi.org/10.3390/sports7060140






