Effects of Leg-Length Discrepancy Compensation and Wedge Foot-Orthoses on Tensor Fasciae Latae EMG in Runners
Abstract
1. Introduction
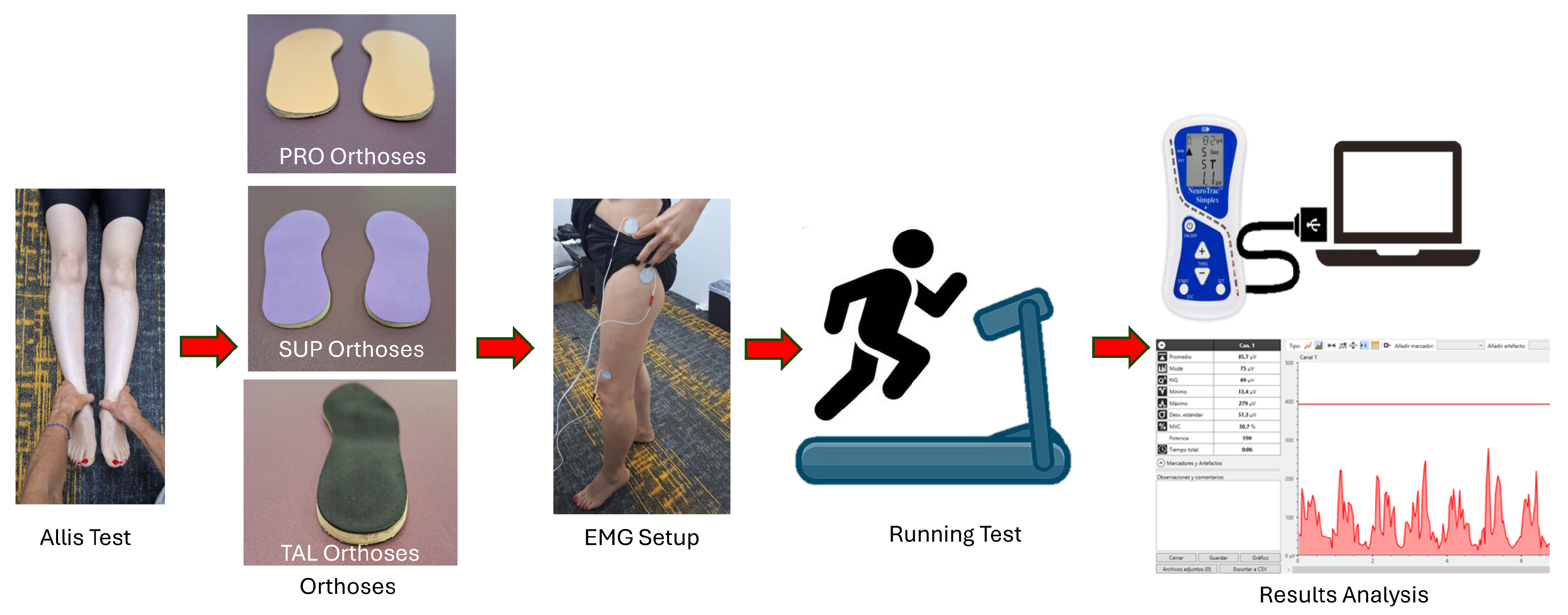
2. Material and Methods
2.1. Sample Size and Study Design
2.2. Participants
2.3. Instruments and Assessments
2.4. Materials
2.5. Procedure
2.5.1. Electrodes Placement
2.5.2. Runing Test
2.6. Statistical Analysis
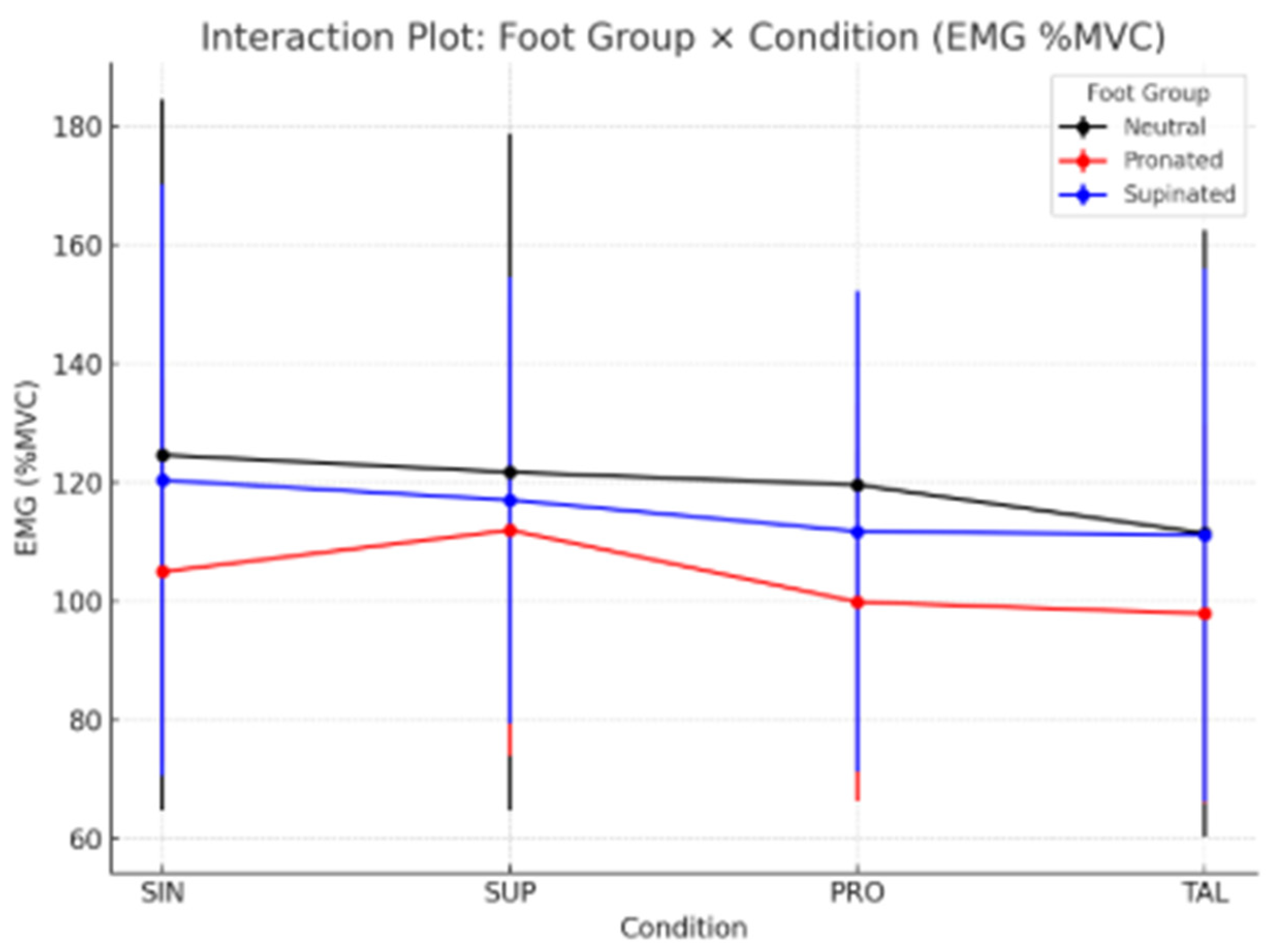
3. Results
4. Discussion
- The findings of this study advance current knowledge on the treatment of iliotibial band (ITB) syndrome in runners by moving beyond the traditional, knee-centered approach.
- Foot type, in combination with lower limb-length discrepancies, influenced pelvic alignment and, consequently, increased strain on the iliotibial band. By correcting these biomechanical imbalances through the use of foot orthoses, it would be possible to reduce mechanical stress on the ITB and promote faster recovery from the condition.
Limitations and Futures Lines of Investigation
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ellis, R.; Hing, W.; Reid, D. Iliotibial band friction syndrome—A systematic review. Man. Ther. 2007, 12, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Foch, E.; Brindle, R.A.; Pohl, M.B. Lower extremity kinematics during running and hip abductor strength in iliotibial band syndrome: A systematic review and meta-analysis. Gait Posture 2023, 101, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Noble, C.A. The treatment of iliotibial band friction syndrome. Br. J. Sports Med. 1979, 13, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Orava, S. Iliotibial tract friction syndrome in athletes—An uncommon exertion syndrome on the lateral side of the knee. J. Sports Med. 1978, 12, 69–73. [Google Scholar] [CrossRef]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. Is iliotibial band syndrome really a friction syndrome? J. Sci. Med. Sport. 2007, 10, 74–76; discussion 77–78. [Google Scholar] [CrossRef]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. The functional anatomy of the iliotibial band during flexion and extension of the knee: Implications for understanding iliotibial band syndrome. J. Anat. 2006, 208, 309–316. [Google Scholar] [CrossRef]
- Kaplan, E.B. The iliotibial tract; clinical and morphological significance. J. Bone Jt. Surg. Am. 1958, 40, 817–832. [Google Scholar] [CrossRef]
- Baker, R.L.; Fredericson, M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 53–77. [Google Scholar] [CrossRef]
- Novacheck, T.F. The biomechanics of running. Gait Posture 1998, 7, 77–95. [Google Scholar] [CrossRef]
- Baker, R.L.; Souza, R.B.; Rauh, M.J.; Fredericson, M.; Rosenthal, M.D. Differences in Knee and Hip Adduction and Hip Muscle Activation in Runners with and Without Iliotibial Band Syndrome. PM&R 2018, 10, 1032–1039. [Google Scholar] [CrossRef]
- Franco, V.; Cerullo, G.; Gianni, E.; Puddu, G. Iliotibial band friction syndrome. Oper. Tech. Sports Med. 1997, 5, 153–156. [Google Scholar] [CrossRef]
- Khamis, S.; Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.E.; Davis, L.E. Leg Length Discrepancy: The Natural History (And What Do We Really Know). J. Pediatr. Orthop. 2019, 39 (Suppl. 1), S10–S13. [Google Scholar] [CrossRef] [PubMed]
- Friede, M.C.; Innerhofer, G.; Fink, C.; Alegre, L.M.; Csapo, R. Conservative treatment of iliotibial band syndrome in runners: Are we targeting the right goals? Phys. Ther. Sport 2022, 54, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Geisler, P.R. Current Clinical Concepts: Synthesizing the Available Evidence for Improved Clinical Outcomes in Iliotibial Band Impingement Syndrome. J. Athl. Train. 2020, 56, 805–815. [Google Scholar] [CrossRef]
- Van der Worp, M.P.; van der Horst, N.; de Wijer, A.; Backx, F.J.G.; Nijhuis-van der Sanden, M.W. Iliotibial band syndrome in runners: A systematic review. Sports Med. 2012, 42, 969–992. [Google Scholar] [CrossRef]
- Aderem, J.; Louw, Q.A. Biomechanical risk factors associated with iliotibial band syndrome in runners: A systematic review. BMC Musculoskelet. Disord. 2015, 16, 356. [Google Scholar] [CrossRef]
- Geraci, M.C.; Brown, W. Evidence-based treatment of hip and pelvic injuries in runners. Phys. Med. Rehabil. Clin. N. Am. 2005, 16, 711–747. [Google Scholar] [CrossRef] [PubMed]
- Gross, M.T.; Foxworth, J.L. The role of foot orthoses as an intervention for patellofemoral pain. J. Orthop. Sports Phys. Ther. 2003, 33, 661–670. [Google Scholar] [CrossRef]
- Root, M.L.; Orien, W.P.; Weed, J.H. Normal and Abnormal Function of the Foot; Clinical Biomechanics Corp.: Los Angeles, CA, USA, 1977. [Google Scholar]
- Ferber, R.; Noehren, B.; Hamill, J.; Davis, I.S. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J. Orthop. Sports Phys. Ther. 2010, 40, 52–58. [Google Scholar] [CrossRef]
- Mousavi, S.H.; Hijmans, J.M.; Rajabi, R.; Diercks, R.; Zwerver, J.; van der Worp, H. Kinematic risk factors for lower limb tendinopathy in distance runners: A systematic review and meta-analysis. Gait Posture 2019, 69, 13–24. [Google Scholar] [CrossRef]
- Noehren, B.; Davis, I.; Hamill, J. ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin. Biomech. 2007, 22, 951–956. [Google Scholar] [CrossRef]
- Stickley, C.D.; Presuto, M.M.; Radzak, K.N.; Bourbeau, C.M.; Hetzler, R.K. Dynamic Varus and the Development of Iliotibial Band Syndrome. J. Athl. Train 2018, 53, 128–134. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, J.C.; Dinowitz, H.D.; Polchaninoff, M. Limb length discrepancy. An electrodynographic analysis. J. Am. Podiatr. Med. Assoc. 1985, 75, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Neumann, D.A. Kinesiology of the hip: A focus on muscular actions. J. Orthop. Sports Phys. Ther. 2010, 40, 82–94. [Google Scholar] [CrossRef]
- Selkowitz, D.M.; Beneck, G.J.; Powers, C.M. Comparison of Electromyographic Activity of the Superior and Inferior Portions of the Gluteus Maximus Muscle During Common Therapeutic Exercises. J. Orthop. Sports Phys. Ther. 2016, 46, 794–799. [Google Scholar] [CrossRef]
- Benito de Pedro, M.; Benito de Pedro, A.I.; Aguilera Rubio, Á.; Maté Muñoz, J.L.; Hernández Lougedo, J. Changes in the Activity of the Erector Spinae and Gluteus Medius Muscles with the Presence of Simulated Lower Limb Dysmetria. Sensors 2024, 24, 1223. [Google Scholar] [CrossRef]
- Bhatia, A.; Ajoy, S.M.; Galagali, D.A.; Debur, R. Electromyographic Analysis of Large Muscle Activity in Progressive Collapsing Foot Deformity. Foot Ankle Spec. 2024, 19386400241265547. [Google Scholar] [CrossRef]
- Cochrane, D.J.; Harnett, M.C.; Pinfold, S.C. Does short-term gluteal activation enhance muscle performance? Res. Sports Med. 2017, 25, 156–165. [Google Scholar] [CrossRef]
- Muyor, J.M.; Martín-Fuentes, I.; Rodríguez-Ridao, D.; Antequera-Vique, J.A. Electromyographic activity in the gluteus medius, gluteus maximus, biceps femoris, vastus lateralis, vastus medialis and rectus femoris during the Monopodal Squat, Forward Lunge and Lateral Step-Up exercises. PLoS ONE 2020, 15, e0230841. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Strobe Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Ricardo, G. Contributo alla diagnosi della dismetria. Acta Soc. Medicorum Nat. Mediolan. 1912. [Google Scholar]
- Beattie, P.; Isaacson, K.; Riddle, D.L.; Rothstein, J.M. Validity of derived measurements of leg-length differences obtained by use of a tape measure. Phys. Ther. 1990, 70, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Betsch, M.; Wild, M.; Große, B.; Rapp, W.; Horstmann, T. The effect of simulating leg length inequality on spinal posture and pelvic position: A dynamic rasterstereographic analysis. Eur. Spine J. 2012, 21, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Gómez, R.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Calvo-Lobo, C.; Navarro-Flores, E.; Palomo-López, P.; Romero-Morales, C.; López-López, D. Reliability Study of Diagnostic Tests for Functional Hallux Limitus. Foot Ankle Int. 2020, 41, 457–462. [Google Scholar] [CrossRef]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef]
- Sanchez-Gomez, R.; Gomez-Carrion, A.; Martinez-Sebastian, C.; Alou, L.; Sevillano, D.; Nuñez-Fernandez, A.; Sanz-Wozniak, P.; de la Cruz-Torres, B. Innovative Medial Cushioning Orthoses Affect Peroneus Longus Electromyographic Activity during Running. J. Clin. Med. 2022, 11, 1339. [Google Scholar] [CrossRef]
- Sanchez-Gomez, R.; Gomez-Carrion, A.; Martinez-Sebastian, C.; Alou, L.; Sevillano, D.; Nuñez-Fernandez, A.; Sanz-Wozniak, P.; de la Cruz-Torres, B. Assessment of a New Lateral Cushioned Casting Orthosis: Effects on Peroneus Longus Muscle Electromyographic Activity During Running. Orthop. J. Sports Med. 2021, 9, 23259671211059152. [Google Scholar] [CrossRef]
- Shih, Y.; Lin, K.L.; Shiang, T.Y. Is the foot striking pattern more important than barefoot or shod conditions in running? Gait Posture 2013, 38, 490–494. [Google Scholar] [CrossRef]
- Fleming, N.; Walters, J.; Grounds, J.; Fife, L.; Finch, A. Acute response to barefoot running in habitually shod males. Human. Mov. Sci. 2015, 42, 27–37. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting Intraclass Correlation Coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Saunders, P.U.; Pyne, D.B.; Telford, R.D.; Hawley, J.A. Reliability and variability of running economy in elite distance runners. Med. Sci. Sports Exerc. 2004, 36, 1972–1976. [Google Scholar] [CrossRef]
- Nguyen, A.P.; Detrembleur, C.; Van Cant, J. Conservative treatment for iliotibial band syndrome: Are we facing a research gap? A scoping review of 98 studies with clinical perspectives. Phys. Ther. Sport. 2023, 62, 25–31. [Google Scholar] [CrossRef]
- Clarke, G.R. Unequal leg length: An accurate method of detection and some clinical results. Rheumatol. Phys. Med. 1972, 11, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J. Bone Jt. Surg. Am. 2001, 83, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Chang, S.F.; Kao, C.Y.; Tsai, H.C. Muscle Strength, Physical Fitness, Balance, and Walking Ability at Risk of Fall for Prefrail Older People. BioMed Res. Int. 2022, 2022, 4581126. [Google Scholar] [CrossRef] [PubMed]
- Dewald, M.; Dalland, J.; Stockland, J. The Association of Joint Power Kinetic Variables with Running Injuries: A Case-Control Study. Int. J. Sports Phys. Ther. 2023, 18, 864–873. [Google Scholar] [CrossRef]
- Kim, H.K.; Mirjalili, S.A.; Fernandez, J. Gait kinetics, kinematics, spatiotemporal and foot plantar pressure alteration in response to long-distance running: Systematic review. Hum. Mov. Sci. 2018, 57, 342–356. [Google Scholar] [CrossRef]
- Trowell, D.; Kenneally-Dabrowski, C.; Bonacci, J. Effects of running-induced fatigue on joint kinematics and kinetics during overground running: A systematic review and meta-analysis. Sports Biomech. 2024, 1–27. [Google Scholar] [CrossRef]
- Colonna, S.; Casacci, F.; Borghi, C. Scoliosis and Lower Limb Inequality: To Lift or Not to Lift, That Is the Question. Cureus 2024, 16, e58443. [Google Scholar] [CrossRef]
- Busseuil, C.; Freychat, P.; Guedj, E.B.; Lacour, J.R. Rearfoot-forefoot orientation and traumatic risk for runners. Foot Ankle Int. 1998, 19, 32–37. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, D.C.; Clement, D.B.; Taunton, J.E. Running Shoes, Orthotics, and Injuries. Sports Med. 1985, 2, 334–347. [Google Scholar] [CrossRef] [PubMed]
- Messier, S.P.; Edwards, D.G.; Martin, D.F.; Lowery, R.B.; Cannon, D.W.; James, M.K.; Curl, W.W.; Read, H.M., Jr.; Hunter, D.M. Etiology of iliotibial band friction syndrome in distance runners. Med. Sci. Sports Exerc. 1995, 27, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical Risk Factors Associated with Running-Related Injuries: A Systematic Review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef]
| Total Population n = 41 | Neutral Group (Ng) n = 14 | Supinated Group (SPg) n = 11 | Pronated Group (PRg) n = 16 | |
|---|---|---|---|---|
| Variable | mean ± SD (95% CI) % | mean ± SD (95% CI) % | mean ± SD (95% CI) % | mean ± SD (95% CI) % |
| Age (years) | 32.27± 6.09 (30.40–34.14) | 32.71 ± 7.66 (28.68–36.74) | 36 ± 3.63 (33.56–38.44) | 28.12 ± 6.98 (24.40–31.84) |
| Height (cm) | 170.37 ± 8.15 (167.88–172.86) | 169.78 ± 9.32 (164.9–174.66) | 170.09 ± 8.33 (165.15–175.0.3) | 171.25 ± 6.8 (167.92–174.58) |
| Weight (kg) | 64.04 ± 9.71 (61.14–66.94) | 63.14 ± 7.87 (59–77.28) | 65 ± 10.58 (58.75–71.25) | 64 ± 10.7 (58.75–69.25) |
| Foot Size (Es) | 40.66 ± 1.9 (40.05–41.27) | 40.2 ± 2.1 (38.81–41.23) | 39.3 ± 2.4 (41.69–43.31) | 42.5 ± 1.2 (38.02–40.58) |
| BMI (kg/m2) | 21.81 ± 1.36 (21.39–22.23) | 21.9 ± 0.4 (21.69–22.11) | 21.08 ± 2.3 (19.72–22.14) | 22.46 ± 1.4 (21.77–23.15) |
| Neutral Group (Ng) n = 14 | Supinated Group (SPg) n = 11 | Pronated Group (PRg) n = 16 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | mean (%MVC) ± SD (95% CI) | ICC 95% IC (Li-Ls) | MDC | mean (%MVC) ± SD (95% CI) | ICC 95% IC (Li-Ls) | MDC | mean (%MVC) ± SD (95% CI) | ICC 95% IC (Li-Ls) | MDC |
| SIN | 105.64 ± 50.6 | 1 (0.999–1) | 2.318 | 140.02 ± 40.84 | 1 (0.999–1) | 2.25 | 91.82 ± 40.75 | 0.999 (0.997–0.999) | 4.36 |
| SUP | 111.99 ± 50.9 | 1 (1–1) | 1.8 | 139.52 ± 41.74 | 1 (1–1) | 1.35 | 92.95 ± 46.83 | 1 (1–1) | 1.84 |
| PRO | 100.16 ± 48.61 | 1 (0.999–1) | 2.85 | 119.51 ± 35.89 | 0.999 (0.998–1) | 2.42 | 86.73 ± 36.12 | 1 (0.999–1) | 2.12 |
| TAL | 93.49 ± 15.88 | 0.998 (0.995–0.99) | 5.79 | 105.81 ± 43.43 | 1 (0.999–1) | 1.81 | 80.08 ± 31.75 | 1 (0.999–1) | 1.72 |
| Foot Group (n) | Contrast | Mean ±SD (%MVC) (95% CI) | LMEM Estimate (Mean Difference %MVC) | Standard Error (SE) | p-Value |
|---|---|---|---|---|---|
| Neutral (Ng) (n = 14) | SIN | 105.64 ± 50.60 | Base | Base | Base |
| SIN vs. SUP | 111.99 ± 50.90 | −6.356 | 6.427 | 0.329 | |
| SIN vs. PRO | 100.16 ± 48.61 | 5.474 | 6.427 | 0.396 | |
| SIN vs. TAL | 93.49 ± 15.88 | 12.149 | 6.427 | 0.066 | |
| Pronated (PRg) (n = 16) | SIN | 91.82 ± 40.75 | Base | Base | Base |
| SIN vs. SUP | 92.95 ± 46.83 | −1.136 | 8.081 | 0.889 | |
| SIN vs. PRO | 86.73 ± 36.12 | 5.091 | 8.081 | 0.534 | |
| SIN vs. TAL | 80.08 ± 31.75 | 11.739 | 8.081 | 0.157 | |
| Supinated (SPg) (n = 11) | SIN | 140.02 ± 40.84 | Base | Base | Base |
| SIN vs. SUP | 139.52 ± 41.74 | 0.501 | 8.873 | 0.955 | |
| SIN vs. PRO | 119.51 ± 35.89 | 20.514 | 8.873 | 0.031 * | |
| SIN vs. TAL | 105.81 ± 43.43 | 34.217 | 8.873 | 0.001 ** |
| Foot Group | Contrast | Mean DIF ± SD EMG (%MVC) (SIN—Condition) | drm | Interpretation (Cohen’s drm) |
|---|---|---|---|---|
| Neutral (Ng) (n = 11) | SIN vs. SUP | 2.91 ± 5.99 | 0.49 | Medium |
| SIN vs. PRO | 5.04 ± 3.58 | 1.41 | Large | |
| SIN vs. TAL | 13.18 ± 6.97 | 1.89 | Very Large | |
| Pronated (PRg) (n = 9) | SIN vs. SUP | −6.99 ± 3.16 | −2.21 | Very Large (Detrimental Increase) |
| SIN vs. PRO | 5.12 ± 4.48 | 1.14 | Large | |
| SIN vs. TAL | 7.07 ± 3.29 | 2.15 | Very Large | |
| Supinated (SPg) (n = 11) | SIN vs. SUP | 13.34 ± 5.91 | 2.26 | Very Large |
| SIN vs. PRO | 8.62 ± 5.7 | 1.51 | Large | |
| SIN vs. TAL | 9.22 ± 6.96 | 1.32 | Large |
| Foot Group | Condition | mean ± SD (95% CI) EMG (%MVC) | Average % Change vs. SIN | Clinical Relevance (Summary) |
|---|---|---|---|---|
| Neutral (Ng) n = 11 | SIN | 124.63 ± 59.88 | Base 0% | Control without intervention. |
| SUP | 121.72 ± 57.06 | −2.33% | Slight reduction. | |
| PRO | 119.59 ± 5.73 | −4.05% | Significant decrease. | |
| TAL | 111.45 ± 51.04 | −10.58% | Largest reduction (LLLD compensation). | |
| Pronated (PRg) n = 9 | SIN | 104.97 ± 32.41 | Base 0% | Control without intervention. |
| SUP | 111.96 ± 37.95 | 6.66% | Increase (SUP would be contraindicated). | |
| PRO | 99.85 ± 33.47 | −4.88% | Decrease (supports pronation). | |
| TAL | 97.90 ± 31.95 | −6.73% | Best reduction effect. | |
| Supinated (SPg) n = 11 | SIN | 120.37 ± 49.82 | Base 0% | Control without intervention. |
| SUP | 117.03 ± 37.56 | −3.10% | Slight reduction. | |
| PRO | 111.75 ± 40.54 | −7.16% | Reduction. | |
| TAL | 111.15 ± 44.92 | −7.66% | Reduction. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanchez-Gomez, R.; Chang, B.P.; Lipik, V.; Sanz-Wozniak, P.; Alexe, D.I.; Garrido Cebrecos, J.; Vega, M.M.; Gomez Carrion, A. Effects of Leg-Length Discrepancy Compensation and Wedge Foot-Orthoses on Tensor Fasciae Latae EMG in Runners. Sports 2025, 13, 412. https://doi.org/10.3390/sports13110412
Sanchez-Gomez R, Chang BP, Lipik V, Sanz-Wozniak P, Alexe DI, Garrido Cebrecos J, Vega MM, Gomez Carrion A. Effects of Leg-Length Discrepancy Compensation and Wedge Foot-Orthoses on Tensor Fasciae Latae EMG in Runners. Sports. 2025; 13(11):412. https://doi.org/10.3390/sports13110412
Chicago/Turabian StyleSanchez-Gomez, Ruben, Boon Peng Chang, Vitali Lipik, Paola Sanz-Wozniak, Dan Iulian Alexe, Jimena Garrido Cebrecos, Marta Martín Vega, and Alvaro Gomez Carrion. 2025. "Effects of Leg-Length Discrepancy Compensation and Wedge Foot-Orthoses on Tensor Fasciae Latae EMG in Runners" Sports 13, no. 11: 412. https://doi.org/10.3390/sports13110412
APA StyleSanchez-Gomez, R., Chang, B. P., Lipik, V., Sanz-Wozniak, P., Alexe, D. I., Garrido Cebrecos, J., Vega, M. M., & Gomez Carrion, A. (2025). Effects of Leg-Length Discrepancy Compensation and Wedge Foot-Orthoses on Tensor Fasciae Latae EMG in Runners. Sports, 13(11), 412. https://doi.org/10.3390/sports13110412








