Investigating the Combined Effects of Fascial Distortion Model Manual Therapy and Balance–Strength Training in Individuals with Chronic Ankle Instability
Abstract
1. Introduction
2. Materials and Methods
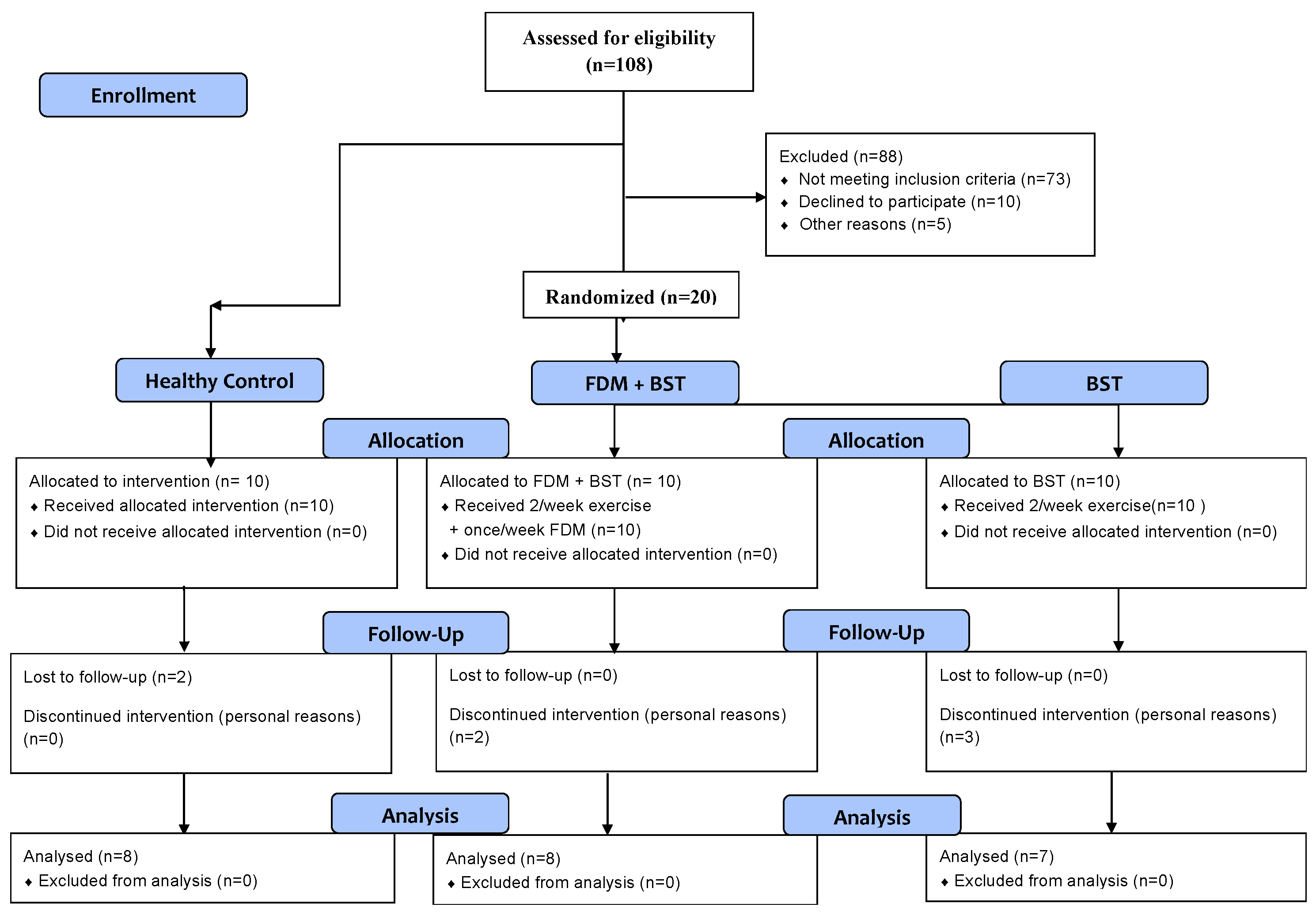
2.1. Participants
2.2. Outcome Measures
2.2.1. Y-Balance Test Lower Quarter (YBT-LQ)
2.2.2. Flamingo Balance Test (FBT)
2.2.3. Weight-Bearing Lunge Test (WBLT)
2.2.4. Cumberland Ankle Instability Tool (CAIT)
2.2.5. Ankle Joint Range of Motion
2.3. Interventions
2.3.1. Balance–Strength Training (BST)
2.3.2. FDM Manual Therapy
2.4. Statistical Analyses
3. Results
4. Discussion
4.1. Dynamic and Static Balance
4.2. Ankle Joint Mobility
4.3. Patients’ Reported Outcomes
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anandacoomarasamy, A.; Barnsley, L. Long term outcomes of inversion ankle injuries. Br. J. Sports Med. 2005, 39, e14, discussion e14. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Recovery From a First-Time Lateral Ankle Sprain and the Predictors of Chronic Ankle Instability: A Prospective Cohort Analysis. Am. J. Sports Med. 2016, 44, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- McKay, G. Ankle injuries in basketball injury rate and risk factors. Br. J. Sports Med. 2001, 35, 103–108. [Google Scholar] [CrossRef]
- Yeung, M.S.; Chan, K.M.; So, C.H.; Yuan, W.Y. An epidemiological survey on ankle sprain. Br. J. Sports Med. 1994, 28, 112–116. [Google Scholar] [CrossRef]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef]
- Lin, C.I.; Houtenbos, S.; Lu, Y.H.; Mayer, F.; Wippert, P.M. The epidemiology of chronic ankle instability with perceived ankle instability- a systematic review. J. Foot Ankle Res. 2021, 14, 41. [Google Scholar] [CrossRef]
- Thompson, C.; Schabrun, S.; Romero, R.; Bialocerkowski, A.; van Dieen, J.; Marshall, P. Factors Contributing to Chronic Ankle Instability: A Systematic Review and Meta-Analysis of Systematic Reviews. Sports Med. 2018, 48, 189–205. [Google Scholar] [CrossRef]
- Han, S.; Son, S.J.; Kim, H.; Lee, H.; Seeley, M.; Hopkins, T. Prelanding movement strategies among chronic ankle instability, coper, and control subjects. Sports Biomech. 2022, 21, 391–407. [Google Scholar] [CrossRef]
- Wang, H.; Yu, H.; Kim, Y.H.; Kan, W. Comparison of the Effect of Resistance and Balance Training on Isokinetic Eversion Strength, Dynamic Balance, Hop Test, and Ankle Score in Ankle Sprain. Life 2021, 11, 307. [Google Scholar] [CrossRef]
- Mollà-Casanova, S. Effects of balance training on functionality, ankle instability, and dynamic balance outcomes in people with chronic ankle instability: Systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 1694–1709. [Google Scholar] [CrossRef]
- Cain, M.S.; Ban, R.J.; Chen, Y.P.; Geil, M.D.; Goerger, B.M.; Linens, S.W. Four-Week Ankle-Rehabilitation Programs in Adolescent Athletes With Chronic Ankle Instability. J. Athl. Train. 2020, 55, 801–810. [Google Scholar] [CrossRef]
- Martin, R.L.; Davenport, T.E.; Fraser, J.J.; Sawdon-Bea, J.; Carcia, C.R.; Carroll, L.A.; Kivlan, B.R.; Carreira, D. Ankle Stability and Movement Coordination Impairments: Lateral Ankle Ligament Sprains Revision. J. Orthop. Sports Phys. Ther. 2021, 51, CPG1–CPG80. [Google Scholar] [CrossRef] [PubMed]
- Weerasekara, I.; Osmotherly, P.; Snodgrass, S.; Marquez, J.; de Zoete, R.; Rivett, D.A. Clinical Benefits of Joint Mobilization on Ankle Sprains: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1395–1412.e1395. [Google Scholar] [CrossRef]
- Shi, X.; Han, J.; Witchalls, J.; Waddington, G.; Adams, R. Does treatment duration of manual therapy influence functional outcomes for individuals with chronic ankle instability: A systematic review with meta-analysis? Musculoskelet. Sci. Pract. 2019, 40, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-J. Effect of Fascial Distortion Model on the Cobb’s Angle in Adolescents with Idiopathic Scoliosis. J. Korean Phys. Ther. 2019, 31, 31–34. [Google Scholar] [CrossRef]
- Lee, J.K.; Kim, C.M. Comparison of Maximum Isometric Strength, Proprioceptive, Dynamic Balance, and Maximum Angle by Applying the Fascial Distortion Model to Chronic Ankle Instability Subjects. J. Korean Phys. Ther. 2021, 33, 224–230. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.M.; Caulfield, B.; Docherty, C.L.; Fong, D.T.; Fourchet, F.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J. Athl. Train. 2014, 49, 121–127. [Google Scholar] [CrossRef]
- Jagger, K.; Frazier, A.; Aron, A.; Harper, B. Scoring Performance Variations between the Y-Balance Test, a Modified Y-Balance Test, and the Modified Star Excursion Balance Test. Int. J. Sports Phys. Ther. 2020, 15, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, S.W.; Teyhen, D.S.; Lorenson, C.L.; Warren, R.L.; Koreerat, C.M.; Straseske, C.A.; Childs, J.D. Y-balance test: A reliability study involving multiple raters. Mil. Med. 2013, 178, 1264–1270. [Google Scholar] [CrossRef]
- De Miguel-Etayo, P.; Gracia-Marco, L.; Ortega, F.B.; Intemann, T.; Foraita, R.; Lissner, L.; Oja, L.; Barba, G.; Michels, N.; Tornaritis, M.; et al. Physical fitness reference standards in European children: The IDEFICS study. Int. J. Obes. 2014, 38 (Suppl. 2), S57–S66. [Google Scholar] [CrossRef]
- Bennell, K.L.; Talbot, R.C.; Wajswelner, H.; Techovanich, W.; Kelly, D.H.; Hall, A.J. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust. J. Physiother. 1998, 44, 175–180. [Google Scholar] [CrossRef]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Reese, N. Joint Range of Motion and Muscle Length Testing; Elsevier Health Sciences: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Han, J.; Anson, J.; Waddington, G.; Adams, R.; Liu, Y. The Role of Ankle Proprioception for Balance Control in relation to Sports Performance and Injury. Biomed. Res. Int. 2015, 2015, 842804. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Son, S.J.; Seeley, M.K.; Hopkins, J.T. Altered movement strategies during jump landing/cutting in patients with chronic ankle instability. Scand. J. Med. Sci. Sports 2019, 29, 1130–1140. [Google Scholar] [CrossRef] [PubMed]
- Typaldos, S. FDM: Clinical and Theoretical Application of the Fascial Distortion Model Within the Practice of Medicine and Surgery; Orthopathic Global Health Publications: Brewer, ME, USA, 2002. [Google Scholar]
- Refshauge, K.M.; Kilbreath, S.L.; Raymond, J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med. Sci. Sports Exerc. 2000, 32, 10–15. [Google Scholar] [CrossRef]
- Brandolini, S.; Lugaresi, G.; Santagata, A.; Ermolao, A.; Zaccaria, M.; Marchand, A.M.; Stecco, A. Sport injury prevention in individuals with chronic ankle instability: Fascial Manipulation(®) versus control group: A randomized controlled trial. J. Bodyw. Mov. Ther. 2019, 23, 316–323. [Google Scholar] [CrossRef]
- Maetzler, M.; Ruescher, M.; Punzenberger, F.; Wang, W.; Abboud, R.J. Progressive rehabilitation of the sprained ankle: A novel treatment method. Foot 2020, 43, 101645. [Google Scholar] [CrossRef]
- Schleip, R.; Gabbiani, G.; Wilke, J.; Naylor, I.; Hinz, B.; Zorn, A.; Jäger, H.; Breul, R.; Schreiner, S.; Klingler, W. Fascia Is Able to Actively Contract and May Thereby Influence Musculoskeletal Dynamics: A Histochemical and Mechanographic Investigation. Front. Physiol. 2019, 10, 336. [Google Scholar] [CrossRef]
- Pirri, C.; Fede, C.; Stecco, A.; Guidolin, D.; Fan, C.; De Caro, R.; Stecco, C. Ultrasound Imaging of Crural Fascia and Epimysial Fascia Thicknesses in Basketball Players with Previous Ankle Sprains Versus Healthy Subjects. Diagnostics 2021, 11, 177. [Google Scholar]
- Hertel, J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin. Sports Med. 2008, 27, 353–370, vii. [Google Scholar] [CrossRef]
- Deodato, M.; Coan, L.; Buoite Stella, A.; Ajčević, M.; Martini, M.; Di Lenarda, L.; Ratti, C.; Accardo, A.; Murena, L. Inertial sensors-based assessment to detect hallmarks of chronic ankle instability during single-leg standing: Is the healthy limb “healthy”? Clin. Biomech. 2023, 107, 106036. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, V.; Hintermann, B.; Horisberger, M.; Fung, T.S. Ligamentous posttraumatic ankle osteoarthritis. Am. J. Sports Med. 2006, 34, 612–620. [Google Scholar] [CrossRef]
- Ziaei Ziabari, E.; Haghpanahi, M.; Razi, M.; Lubberts, B.; Ashkani-Esfahani, S.; DiGiovanni, C.W. The Effects of Chronic Ankle Instability on the Biomechanics of the Uninjured, Contralateral Ankle During Gait. Orthop. Surg. 2022, 14, 2238–2244. [Google Scholar] [CrossRef] [PubMed]
- Witchalls, J.; Pantanowitz, M.; Funk, S.; Waddington, G.; Band, S.S.; Adams, R.; Steinberg, N. Self-reported chronic ankle instability effects on the development of fitness during an Infantry Commanders Course. J. Sci. Med. Sport. 2021, 24, 1130–1135. [Google Scholar] [CrossRef]
- Ko, J.; Wikstrom, E.; Li, Y.; Weber, M.; Brown, C.N. Performance Differences Between the Modified Star Excursion Balance Test and the Y-Balance Test in Individuals With Chronic Ankle Instability. J. Sport. Rehabil. 2020, 29, 748–753. [Google Scholar] [CrossRef]
- Alawna, M.; Mohamed, A.A. Short-term and long-term effects of ankle joint taping and bandaging on balance, proprioception and vertical jump among volleyball players with chronic ankle instability. Phys. Ther. Sport. 2020, 46, 145–154. [Google Scholar] [CrossRef]
- Hall, E.A.; Docherty, C.L.; Simon, J.; Kingma, J.J.; Klossner, J.C. Strength-training protocols to improve deficits in participants with chronic ankle instability: A randomized controlled trial. J. Athl. Train. 2015, 50, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.A.; Docherty, C.L. Validity of clinical outcome measures to evaluate ankle range of motion during the weight-bearing lunge test. J. Sci. Med. Sport. 2017, 20, 618–621. [Google Scholar] [CrossRef]
- Vomacka, M.M.; Calhoun, M.R.; Lininger, M.R.; Ko, J. Dorsiflexion Range of Motion in Copers and Those with Chronic Ankle Instability. Int. J. Exerc. Sci. 2019, 12, 614–622. [Google Scholar]
- Mckeon, P.O.; Wikstrom, E.A. Sensory-Targeted Ankle Rehabilitation Strategies for Chronic Ankle Instability. Med. Sci. Sports Exerc. 2016, 48, 776–784. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Lomas Vega, R.; Osuna-Pérez, M.C.; Hita-Contreras, F.; Martínez-Amat, A. Effects of joint mobilization on chronic ankle instability: A randomized controlled trial. Disabil. Rehabil. 2015, 37, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Marrón-Gómez, D.; Rodríguez-Fernández, Á.L.; Martín-Urrialde, J.A. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys. Ther. Sport. 2015, 16, 10–15. [Google Scholar] [CrossRef]
- Allois, R.; Niglia, A.; Pernice, A.; Cuesta-Barriuso, R. Fascial therapy, strength exercises and taping in soccer players with recurrent ankle sprains: A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 27, 256–264. [Google Scholar] [CrossRef]
- Kamani, N.C.; Poojari, S.; Prabu, R.G. The influence of fascial manipulation on function, ankle dorsiflexion range of motion and postural sway in individuals with chronic ankle instability. J. Bodyw. Mov. Ther. 2021, 27, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Díaz, D.; Hita-Contreras, F.; Martínez-Amat, A.; Aibar-Almazán, A.; Kim, K.M. Ankle-Joint Self-Mobilization and CrossFit Training in Patients With Chronic Ankle Instability: A Randomized Controlled Trial. J. Athl. Train. 2020, 55, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of chronic ankle sprain on pain, range of motion, proprioception, and balance among athletes. Int. J. Environ. Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef] [PubMed]
- Donovan, L.; Hart, J.M.; Saliba, S.A.; Park, J.; Feger, M.A.; Herb, C.C.; Hertel, J. Rehabilitation for Chronic Ankle Instability With or Without Destabilization Devices: A Randomized Controlled Trial. J. Athl. Train. 2016, 51, 233–251. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J.; Kim, Y.E.; Jun, H.J.; Lee, J.S.; Ji, S.H.; Ji, S.G.; Seo, T.H.; Kim, Y.O. Which Treatment is More Effective for Functional Ankle Instability: Strengthening or Combined Muscle Strengthening and Proprioceptive Exercises? J. Phys. Ther. Sci. 2014, 26, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Zhang, X.; Zhu, F.; Zhu, W.; Wang, X.; Jia, F.; Chen, W.; Zhang, M. A randomized controlled trial comparing rehabilitation with isokinetic exercises and Thera-Band strength training in patients with functional ankle instability. PLoS ONE 2022, 17, e0278284. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Diaz, D.; Lomas-Vega, R.; Osuna-Perez, M.C.; Contreras, F.H.; Martinez-Amat, A. Effects of 6 Weeks of Balance Training on Chronic Ankle Instability in Athletes: A Randomized Controlled Trial. Int. J. Sports Med. 2015, 36, 754–760. [Google Scholar] [CrossRef]
| Mean ± SD | p (Effect Size) | |||
|---|---|---|---|---|
| Groups | FDM + BST | BST | Control | |
| Sample Size | 8 | 7 | 8 | |
| Age | 21.37 ± 3.24 | 20.43 ± 1.90 | 22.37 ± 2.66 | 0.394 (0.09) |
| Height (cm) | 173.5 ± 9.24 | 169.86 ± 9.61 | 174.87 ± 12.49 | 0.650 (0.04) |
| Weight (kg) | 68.5 ± 12.5 | 66.14 ± 11.24 | 71.25 ± 12.61 | 0.723 (0.03) |
| BMI (kg/m2) | 22.79 ± 3.93 | 22.31 ± 2.71 | 23.23 ± 2.90 | 0.862 (0.57) |
| Number of Sprains | 3.50 ± 1.69 | 4.29 ± 2.62 | 0.00 | <0.001 (0.01) |
| CAIT | 14.37 ± 14.38 | 19.71 ± 3.90 | 30.00 | <0.001 (0.76) |
| Participants | rmANOVA | ||||||
|---|---|---|---|---|---|---|---|
| FDM + BST | BST | Control | Group Effect p (ηp2) | Time Effect p (ηp2) | Time × Group p (ηp2) | ||
| Dorsiflexion (°) | pre-test | 12.13 ± 7.08 | 16.43 ± 9.14 | 21.13 ± 4.22 | <0.001 (0.539) | 0.088 (0.139) | 0.542 (0.059) |
| post-test | 10.63 ± 0.92 | 11.43 ± 1.40 | 19.75 ± 3.58 | ||||
| Plantarflexion (°) | pre-test | 48.13 ± 17.08 | 46.14 ± 10.29 | 58.13 ± 6.47 | 0.778 (0.025) | <0.001 (0.638) | 0.003 (0.449) |
| post-test | 66.63 ± 4.72 * | 65.00 ± 4.44 * | 58.75 ± 5.92 | ||||
| Pronation (°) | pre-test | 16.63 ± 8.21 | 15.57 ± 5.88 | 22.38 ± 4.90 | 0.682 (0.037) | 0.001 (0.461) | 0.029 (0.298) |
| post-test | 25.38 ± 8.50 * | 23.57 ± 8.73 * | 22.50 ± 5.24 | ||||
| Supination (°) | pre-test | 30.38 ± 9.53 | 31.57 ± 10.41 | 36.38 ± 6.68 | 0.828 (0.019) | <0.001 (0.615) | <0.001 (0.602) |
| post-test | 43.63 ± 9.86 * | 37.14 ± 6.91 | 35.63 ± 8.16 | ||||
| Participants | rmANOVA | ||||||
|---|---|---|---|---|---|---|---|
| FDM + BST | BST | Control | Group Effect p (ηp2) | Time Effect p (ηp2) | Time × Group p (ηp2) | ||
| WBLT (cm) | pre-test | 6.25 ± 2.25 | 8.93 ± 4.55 | 12.50 ± 2.83 | 0.010 (0.367) | 0.001 (0.460) | 0.009 (0.376) |
| post-test | 9.25 ± 2.72 * | 9.57 ± 2.76 * | 13.00 ± 3.25 | ||||
| FBT | pre-test | 6.00 ± 4.34 | 3.14 ± 2.12 | 1.63 ± 3.11 | 0.255 (0.127) | <0.001 (0.353) | 0.008 (0.379) |
| post-test | 1.63 ± 1.85 * | 2.29 ± 1.89 | 1.50 ± 3.21 | ||||
| YBT-LQ (%) | pre-test | 71.92 ± 7.96 | 80.02 ± 6.00 | 84.17 ± 5.99 | 0.030 (0.297) | <0.001 (0.531) | 0.026 (0.305) |
| post-test | 84.56 ± 4.10 * | 89.59 ± 7.85 | 85.49 ± 6.49 | ||||
| CAIT | pre-test | 14.38 ± 5.66 | 19.71 ± 3.90 | 30.00 ± 0.00 | <0.001 (0.734) | <0.001 (0.832) | <0.001 (0.763) |
| post-test | 22.50 ± 3.34 * | 24.29 ± 2.98 * | 30.00 ± 0.00 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammadi, A.; Sakhtemani, S.E.; Trimmel, L.; Petricsevics, K.; Makai, A.; Zsenak, I.; Melczer, C.; Tardi, P.S. Investigating the Combined Effects of Fascial Distortion Model Manual Therapy and Balance–Strength Training in Individuals with Chronic Ankle Instability. Sports 2024, 12, 33. https://doi.org/10.3390/sports12010033
Mohammadi A, Sakhtemani SE, Trimmel L, Petricsevics K, Makai A, Zsenak I, Melczer C, Tardi PS. Investigating the Combined Effects of Fascial Distortion Model Manual Therapy and Balance–Strength Training in Individuals with Chronic Ankle Instability. Sports. 2024; 12(1):33. https://doi.org/10.3390/sports12010033
Chicago/Turabian StyleMohammadi, Amin, Seyed Ehsan Sakhtemani, Lukas Trimmel, Krisztina Petricsevics, Alexandra Makai, Istvan Zsenak, Csaba Melczer, and Péter Sándor Tardi. 2024. "Investigating the Combined Effects of Fascial Distortion Model Manual Therapy and Balance–Strength Training in Individuals with Chronic Ankle Instability" Sports 12, no. 1: 33. https://doi.org/10.3390/sports12010033
APA StyleMohammadi, A., Sakhtemani, S. E., Trimmel, L., Petricsevics, K., Makai, A., Zsenak, I., Melczer, C., & Tardi, P. S. (2024). Investigating the Combined Effects of Fascial Distortion Model Manual Therapy and Balance–Strength Training in Individuals with Chronic Ankle Instability. Sports, 12(1), 33. https://doi.org/10.3390/sports12010033






