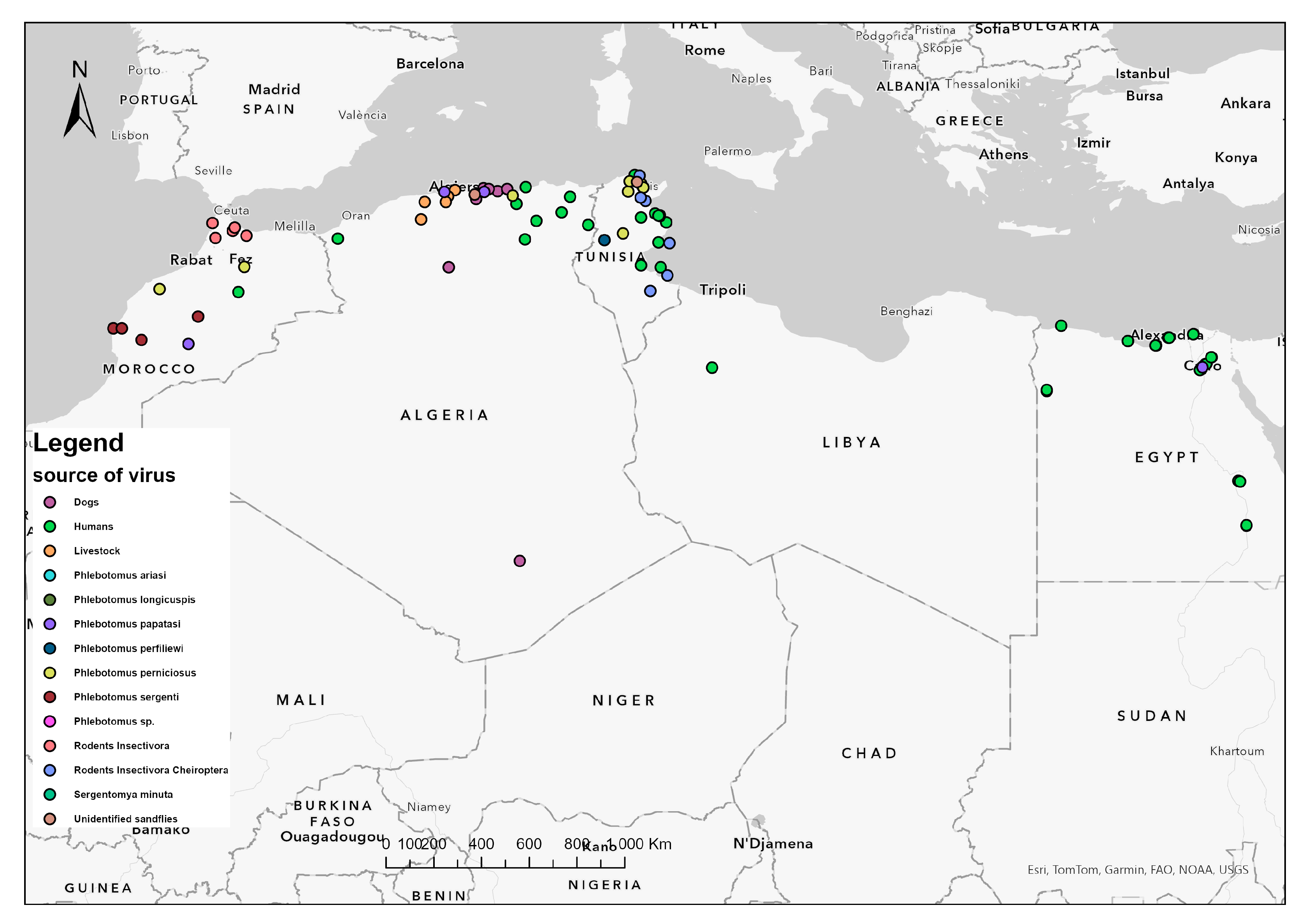
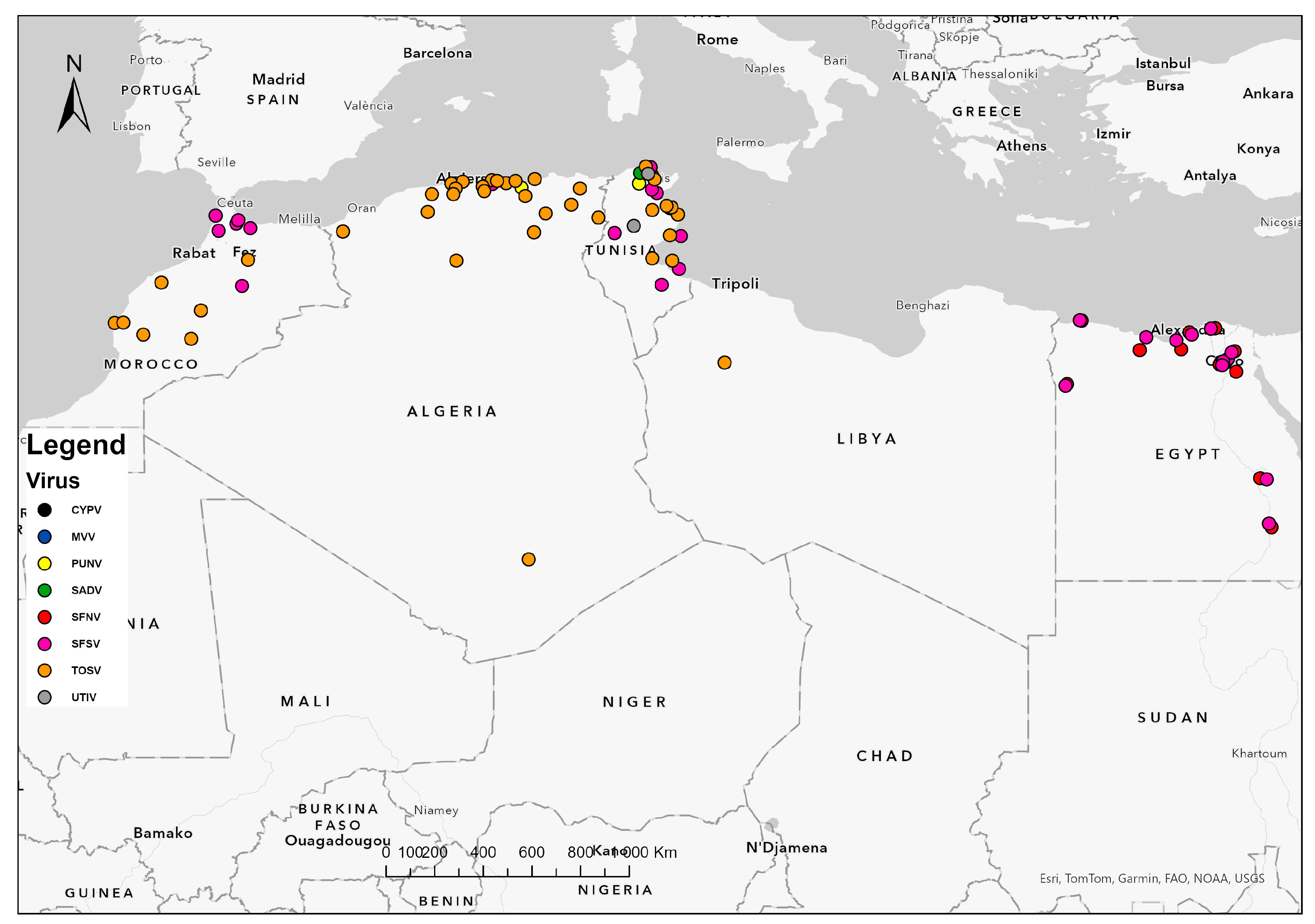
Epidemiology of Sandfly-Borne Phleboviruses in North Africa: An Overview
Simple Summary
Abstract
1. Introduction
2. Sandfly-Borne Phleboviruses in Algeria
2.1. Sicilian Virus
2.2. Cyprus Virus
2.3. Naples Virus
2.4. Toscana Virus
2.5. Punique Virus
3. In Morocco
3.1. Toscana Virus
3.2. Naples Virus
3.3. Sicilian Virus
4. In Tunisia
4.1. Sicilian and Sicilian-like Viruses
4.2. Cyprus Virus
4.3. Punique Virus
4.4. Naples Virus
4.5. Toscana Virus
4.6. Saddaguia Virus
4.7. Medjerda Valley Virus
5. In Libya
6. In Egypt
7. Discussion
| Country | Virus | Year | Area | Site Factors | Governorate | Region | Population | Prevalence | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| Algeria | SFSV | 2006 | Larbaa Nath Iraten | NA | Tizi Ouzou | North | Ph. ariasi | NA | [43] |
| Healthy humans | 5% (IgG) | ||||||||
| SFSV | 2007 | Bou Ismail | NA | Tipaza | North | Ph. longicuspis | NA | [44] | |
| Larbaa Nath Iraten | NA | Tizi Ouzou | North | ||||||
| SFSV | 2007 | Bou Ismail | NA | Tipaza | North | Outpatients | 10.6% (IgG) | [44] | |
| Larbaa Nath Iraten | NA | Tizi Ouzou | North | Healthy persons | 21.6% (IgG) | ||||
| CYPV | 2007 | Bou Ismail | NA | Tipaza | North | Ph. papatasi | NA | [44] | |
| Larbaa Nath Iraten | NA | Tizi Ouzou | North | ||||||
| TOSV | 2013 | Draa El Mizan | 36°32′146” N, 3°50′850” E 380 m altitude | Tizi Ouzou | North | Unidentified sandflies | NA | [31] | |
| Blood donors | 50% (Nt-Ab) | ||||||||
| TOSV | 2014 | Tifra | 36°39”59” N, 4°22”16” E | Bejaia | North | Watchdogs | 4.3% (Nt-Ab) | [46] | |
| Ouaguenoun | 36°46”12” N, 4°10”29” E | Tizi Ouzou | North | ||||||
| Azazga | 36°44”43” N, 4°22”16” E | Tizi Ouzou | North | ||||||
| TOSV * | 2017–2018 | NA | NA | Tlemcen | North | Owned dogs | 20% (IgG) | [45] | |
| NA | NA | Blida | North | ||||||
| NA | NA | Algiers | North | ||||||
| NA | NA | Medea | North | ||||||
| NA | NA | Bouira | North | ||||||
| NA | NA | Setif | North | ||||||
| NA | NA | Bejaia | North | ||||||
| NA | NA | Laghouat | Center | ||||||
| NA | NA | Tamanrasset | South | ||||||
| TOSV | 2017–2018 | NA | NA | Blida | North | Owned dogs | 4.56% (Nt-Ab) | [45] | |
| NA | NA | Algiers | North | ||||||
| NA | NA | Bejaia | North | ||||||
| NA | NA | Setif | North | ||||||
| NA | NA | Laghouat | Center | ||||||
| TOSV | 2016–2018 | NA | NA | Tlemcen | North | Hospitalized patients with neurological infection | 3.8% (RNA/Ig) | [34] | |
| NA | NA | Blida | North | ||||||
| NA | NA | Medea | North | ||||||
| NA | NA | Algiers | North | ||||||
| NA | NA | Jijel | North | ||||||
| NA | NA | Setif | North | ||||||
| NA | NA | Batna | North | ||||||
| NA | NA | Biskra | North | ||||||
| NA | NA | Guelma | North | ||||||
| NA | NA | Oum El Bouaghi | North | ||||||
| NA | NA | Tebessa | North | ||||||
| TOSV | 2017 | NA | NA | Tissemsilt | North | Livestock | 3.33–17.18% (Nt-Ab) | [35] | |
| NA | NA | Ain Defla | North | ||||||
| NA | NA | Tipaza | North | ||||||
| NA | NA | Blida | North | ||||||
| NA | NA | Medea | North | ||||||
| NA | NA | Algiers | North | ||||||
| PUNV | 2020 | Kherrata | 36°24′20′′ N, 5°16′37′′ E | Bejaia | North | Ph. perniciosus | 0.06% | [47] | |
| Morocco | SFNV | 1976 | Itzer | NA | Midelt | Center | Humans | 2.9% (Nt-Ab) | [38] |
| SFSV | 1976 | Itzer | NA | Midelt | Center | Humans | 5.7% (Nt-Ab) | [38] | |
| SFSV | 1979 | Bab Besen | 1600 m altitude, Humid | Chaouen | North | Rodents Insectivora | 9.4% (IgG) | [51] | |
| Chaouen | 600 m altitude, Sub-humid | Chaouen | North | ||||||
| Talembote | 400 m altitude, Semi-arid | Chaouen | North | ||||||
| Arbaoua | 130 m altitude, Sub-humid | Kenitra | North | ||||||
| Asilah | 200 m altitude, Sub-humid | Tanger | North | ||||||
| TOSV | 2008 | Louata | 338,319 latitude, 4828 longitude, 800 m altitude | Sefrou | North | Ph. perniciosus | 4/129 | [48] | |
| TOSV | 2011 | El Hanchane | 31°31′11′′ N, 9°26′02′′ W | Essaouira | Center | Ph. sergenti | NA | [49] | |
| TOSV | 2008–2011 | NA | NA | Azilal | Center | Ph. sergenti | NA | [30] | |
| NA | NA | Sefrou | North | Ph. longicuspis | NA | ||||
| TOSV | NA | NA | Bani Hassan: 31°59′50′′ N, 6°59′44′′ W 722 m altitude, Semi-arid | Azilal | Center | Ph. longicuspis | 0.18% | [50] | |
| Tabia: 32°01′49′′ N 6°47′48′′ W 563 m altitude Semi-arid | Ph. sergenti | ||||||||
| El Hanchane | 290–300 m altitude Semi-arid | Essaouira | Center | Ph. sergenti | 0.15% | ||||
| Ouarzazate | 1134 m altitude Arid | Ouarzazate | South | Ph. papatasi | 0.09% | ||||
| Louata | 674 m altitude | Sefrou | North | Ph. longicuspis | 0.33% | ||||
| Temperate | Ph. perniciosus | ||||||||
| TOSV | 2018 | Lalla Laaziza | 31°04′ N, 8°42′ W >912 m altitude | Chichaoua | Center | Ph. sergenti | NA | [11] | |
| Tunisia | SFSV | 1975 | NA | NA | Mixed | NA | Humans | 1.6% (Nt-Ab) | [38] |
| SFSV | 1980 | El Gharia | 750 m altitude | Bizerte | North | Rodents Insectivora Cheiroptera | 31% (IgG) | [52] | |
| Zarzis | 1 m altitude | Medenine | South | ||||||
| Kerkennah | 1–3 m altitude | Sfax | Center | ||||||
| Tataouine | 190 m altitude | Tataouine | South | ||||||
| Ezzriba | 70 m altitude | Zaghouan | North | ||||||
| Moghrane | 110 m altitude | Zaghouan | North | ||||||
| SFSV | 2011–2012 | Sousse | NA | Sousse | North | Patient with meningo- encephalitis | NA | [54] | |
| SFSV | 2013 | Haffouz | 34°51′ N, 9°29′ E Arid | Kairouan | Center | Dogs | 38.1% (Nt-Ab) | [32] | |
| Bouhajla | 35°24′ N, 9°56′ E Arid | ||||||||
| SFSV | 2014 | El Felta | 35°16′ N, 9°26′ E | Sidi Bouzid | Center | Ph. perfiliewi | NA | [25] | |
| SFSV | 2017 | NA | NA | Monastir | Center | Blood donors | 1.3% (IgG) | [55] | |
| NA | NA | Sousse | |||||||
| PUNV | 2008 | Utique | 37°2′ N, 10°2′ E Sub-humid | Bizerte | North | Ph. perniciosus | 0.13% | [53] | |
| Ph. longicuspis | |||||||||
| PUNV | 2009 | Utique | 37°08′ N, 7°74′ E | Bizerte | North | Ph. perniciosus | 0.11% | [33] | |
| PUNV | 2010 | Utique | 37°08′ N, 7°74′ E | Bizerte | North | Unidentified sandflies | 0.05% | [33] | |
| PUNV | 2011 | NA | NA | Bizerte | North | Humans | 8.72% (Nt-Ab) | [57] | |
| PUNV | 2011–2012 | Medjez El Bab | Semi-arid | Beja | North | Ph. perniciosus | NA | [54] | |
| PUNV | 2013 | Haffouz | 34°51′ N, 9°29′ E Arid | Kairouan | Center | Dogs | 43.5% (Nt-Ab) | [32] | |
| Bouhajla | 35°24′ N, 9°56′ E Arid | ||||||||
| UTIV | 2008 | Utique | 37°2′ N, 10°2′ E Sub-humid | Bizerte | North | Ph. perniciosus | 0.53% | [53] | |
| Ph. longicuspis | |||||||||
| Se. minuta | |||||||||
| UTIV | 2014 | Saddaguia | 35°05′ N, 9°25′ E | Sidi Bouzid | Center | Ph. perfiliewi | NA | [25] | |
| SFNV | 2017 | NA | NA | Monastir | Center | Blood donors | 1.1% (IgG) | [55] | |
| NA | NA | Sousse | |||||||
| TOSV | 2003–2009 | NA | NA | Mahdia | North | Neurological disease patients | 10% (IgM) 7% (IgG) | [58] | |
| NA | NA | Monastir | North | ||||||
| NA | NA | Sousse | North | ||||||
| NA | NA | Sfax | Center | ||||||
| NA | NA | Gabes | South | ||||||
| NA | NA | Djerba | South | ||||||
| TOSV | 2010 | Utique | 37°08′ N, 7°74′ E | Bizerte | North | Ph. perniciosus | 0.03% | [56] | |
| TOSV | 2011 | NA | NA | Bizerte | North | Outpatients | 41% (Nt-Ab) | [57] | |
| TOSV | 2011–2012 | NA | NA | Tunis | North | Patients with meningeal syndrome | 12.16% (IgM) 78% (IgG) 12.86% (RNA) | [54] | |
| Ph. perniciosus | NA | ||||||||
| Ph. perfiliewi | NA | ||||||||
| TOSV | 2013 | Haffouz | 34°51′ N, 9°29′ E Arid | Kairouan | Center | Dogs | 7.5% (Nt-Ab) | [32] | |
| Bouhajla | 35°24′ N, 9°56′ E Arid | ||||||||
| TOSV | 2014 | Saddaguia | 35°05′ N, 9°25′ E | Sidi Bouzid | Center | Ph. perfiliewi | 0.03% | [25] | |
| TOSV | 2014–2016 | Saddaguia | 35°05′ N, 9°25′ E | Sidi Bouzid | Center | Ph. perniciosus | 0.05–0.22% | [60] | |
| Ph. longicuspis | |||||||||
| Ph. perfiliewi | |||||||||
| TOSV | 2017 | NA | NA | Kairouan | Center | Blood donors | 13.3% (IgG) | [55] | |
| NA | NA | Monastir | |||||||
| NA | NA | Sousse | |||||||
| SADV | 2013 | Borj Youssef | Borj Youssef: 36°56′ N, 10°07′ E, Semi-arid | Ariana | North | Ph. perniciosus | 0.6% | [24] | |
| Utique: 37°08′ N, 7°74′ E, Semi-arid | Ph. longicuspis | ||||||||
| SADV | 2013 | Mateur | Mateur: 37°03′ N, 9°28′ E, Subhumid | Bizerte | North | Ph. perfiliewi | |||
| Sejnene: 36°56′ N, 9°21′ E, Humid | Ph. perniciosus | ||||||||
| SADV | 2013 | Saddaguia | Saddaguia: 35°05′ N, 9°25′ E, Arid | Sidi Bouzid | Center | Ph. perfiliewi | |||
| Bouhajla: 35°24′ N, 9°56′ E, Arid | Ph. perniciosus | ||||||||
| SADV | 2014 | El Felta | 35°16′ N, 9°26′ E | Sidi Bouzid | Center | Ph. perfiliewi | NA | [25] | |
| MVV | 2010 | Utique | 37°08′ N, 7°74′ E | Bizerte | North | Phlebotomus spp. | 0.02% | [61] | |
| Outpatients | 1.35% (Nt-Ab) | ||||||||
| CYPV | 2017 | NA | NA | Monastir | Center | Blood donors | 2.9% (IgG) | [55] | |
| NA | NA | Sousse | |||||||
| Libya | SFNV | 2008 | NA | NA | NA | NA | Febrile patients | 0.5% (IgG) | [62] |
| SFSV | 2008 | NA | NA | NA | NA | Febrile patients | 0.7% (IgG) | ||
| TOSV | 2014 | Yafran | 32°08′ N, 12°55′ E 691 m altitude Semi-arid | Jabal al Gharbi | North | Outpatients | 25% (IgG) | [63] | |
| Egypt | SFNV | 1950’s | NA | NA | NA | NA | Febrile patients | NA | [76] |
| 1952–1954 | Qalyub | NA | Qalyubia | North | Humans | 31% (Nt-Ab) | [38] | ||
| 1959–1961 | Metropolitan Cairo | NA | Cairo Giza Qalyubia | North | Ph. papatasi | NA | [64] | ||
| 1960–1963 | Giza | NA | Giza | North | Humans | 43.8% (Nt-Ab) | [38] | ||
| Alexandria | NA | Alexandria | North | Humans | 21.6% (Nt-Ab) | ||||
| Baltim-Borg Burulus | NA | Kafr El Sheikh | North | Humans | 6.7% (Nt-Ab) | ||||
| Luxor | NA | Luxor | South | Humans | 56.3% (Nt-Ab) | ||||
| Siwa | NA | Matruh | North | Humans | 3.9% (Nt-Ab) | ||||
| Sidi Barrani | NA | Matruh | North | Humans | 9.5% (Nt-Ab) | ||||
| Bahig | NA | Alexandria | North | Humans | 25% (Nt-Ab) | ||||
| El Daba | NA | Matruh | North | Humans | 13.9% (Nt-Ab) | ||||
| Aswan | NA | Aswan | South | Humans | 47.3% (Nt-Ab) | ||||
| 1975 | Cairo | NA | Cairo | North | Humans | 6.1% (Nt-Ab) | |||
| 1984 | Imbaba | NA | Giza | North | Hospitalized patients | 2/55 (IgG) | [77] | ||
| 1991 | Bilbeis | NA | Sharqiya | North | Humans | 2% (IgG) | [78] | ||
| SFSV | 1952–1954 | Qalyub | NA | Qalyubia | North | Humans | 22.6% (Nt-Ab) | [38] | |
| 1959–1961 | Metropolitan Cairo | NA | Cairo Giza Qalyubia | North | Ph. papatasi | NA | [64] | ||
| 1960–1963 | Giza | NA | Giza | North | Humans | 43.8% (Nt-Ab) | [38] | ||
| Alexandria | NA | Alexandria | North | Humans | 27% (Nt-Ab) | ||||
| Baltim-Borg Burulus | NA | Kafr El Sheikh | North | Humans | 8.9% (Nt-Ab) | ||||
| Luxor | NA | Luxor | South | Humans | 59.4% (Nt-Ab) | ||||
| Siwa | NA | Matruh | North | Humans | 2% (Nt-Ab) | ||||
| Sidi Barrani | NA | Matruh | North | Humans | 4.8%(Nt-Ab) | ||||
| Bahig | NA | Alexandria | North | Humans | 6.3% (Nt-Ab) | ||||
| El Daba | NA | Matruh | North | Humans | 8.3% (Nt-Ab) | ||||
| Aswan | NA | Aswan | South | Humans | 43.6% (Nt-Ab) | ||||
| 1969 | NA | NA | NA | NA | University students | 23% (IgG) | [79] | ||
| 1975 | Cairo | NA | Cairo | North | Humans | 5.0% (Nt-Ab) | [38] | ||
| 1984 | Imbaba | NA | Giza | North | Hospitalized patients | 1/55 (IgG) | [77] | ||
| 1989 | Bilbeis | NA | Sharqiya | North | Schoolchildren | 9% (IgG) | [80] | ||
| 1991 | Bilbeis | NA | Sharqiya | North | Humans | 4% (IgG) | [78] |
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Atkinson, B.; Hewson, R. Emerging arboviruses of clinical importance in Central Asia. J. Gen. Virol. 2018, 99, 1172–1184. [Google Scholar] [CrossRef] [PubMed]
- Krow-Lucal, E.; Lindsey, N.P.; Lehman, J.; Fischer, M.; Staples, J.E. West Nile Virus and Other Nationally Notifiable Arboviral Diseases—United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, V.; Shaw, J.; Volf, P. Parasite biology: The vectors. In The Leishmaniases: Old Neglected Tropical Diseases; Bruschi, F., Gradoni, L., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 31–77. [Google Scholar]
- Bichaud, L.; de Lamballerie, X.; Alkan, C.; Izri, A.; Gould, E.; Charrel, R. Arthropods as a source of new RNA viruses. Microb. Pathog. 2014, 77, 136–141. [Google Scholar] [CrossRef]
- Depaquit, J.; Grandadam, M.; Fouque, F.; Andry, P.E.; Peyrefitte, C. Arthropod-borne viruses transmitted by Phlebotomine sandflies in Europe: A review. Euro Surveill. 2010, 15, 19507. [Google Scholar] [CrossRef] [PubMed]
- Maroli, M.; Feliciangeli, M.D.; Bichaud, L.; Charrel, R.N.; Gradoni, L. Phlebotomine sandflies and the spreading of leishmaniases and other diseases of public health concern. Med. Vet. Entomol. 2013, 27, 123–147. [Google Scholar] [CrossRef] [PubMed]
- Ayhan, N.; Charrel, R.N. Of Phlebotomines (Sandflies) and Viruses: A Comprehensive Perspective on a Complex Situation. Curr. Opin. Insect Sci. 2017, 22, 117–124. [Google Scholar] [CrossRef]
- Chaves, L.F.; Calzada, J.E.; Valderrama, A.; Saldaña, A. Cutaneous Leishmaniasis and Sand Fly Fluctuations Are Associated with El Niño in Panamá. PLoS Negl. Trop. Dis. 2014, 8, e3210. [Google Scholar] [CrossRef]
- Jancarova, M.; Polanska, N.; Volf, P.; Dvorak, V. The role of sand flies as vectors of viruses other than phleboviruses. J. Gen. Virol. 2023, 104, 001837. [Google Scholar] [CrossRef]
- Killick-Kendrick, R. The biology and control of phlebotomine sand flies. Clin. Dermatol. 1999, 17, 279–289. [Google Scholar] [CrossRef]
- Daoudi, M.; Calzolari, M.; Boussaa, S.; Bonilauri, P.; Torri, D.; Romeo, G.; Lelli, D.; Lavazza, A.; Hafidi, M.; Dottori, M.; et al. Identification of Toscana virus in natural population of sand flies (Diptera: Psychodidae) from Moroccan leishmaniasis foci. J. Infect. Public Health 2022, 15, 406–411. [Google Scholar] [CrossRef]
- Ayhan, N.; Charrel, R.N. Sandfly-borne viruses of demonstrated/relevant medical importance. In Vectors and Vector-Borne Zoonotic Diseases; IntechOpen: London, UK, 2018; pp. 1–22. [Google Scholar]
- Kuhn, J.H.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Amarasinghe, G.K.; Anthony, S.J.; Avšic-Županc, T.; Ayllón, M.A.; Bahl, J.; Balkema-Buschmann, A.; et al. 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales. Arch. Virol. 2020, 165, 3023–3072. [Google Scholar] [CrossRef] [PubMed]
- Charrel, R.N.; Gallian, P.; Navarro-Mari, J.M.; Nicoletti, L.; Papa, A.; Sánchez-Seco, M.P.; Tenorio, A.; de Lamballerie, X. Emergence of Toscana virus in Europe. Emerg. Infect. Dis. 2005, 11, 1657–1663. [Google Scholar] [CrossRef] [PubMed]
- Moriconi, M.; Rugna, G.; Calzolari, M.; Bellini, R.; Albieri, A.; Angelini, P.; Cagarelli, R.; Landini, M.P.; Charrel, R.N.; Varani, S. Phlebotomine sand fly-borne pathogens in the Mediterranean Basin: Human leishmaniasis and phlebovirus infections. PLoS Negl. Trop. Dis. 2017, 11, e0005660. [Google Scholar] [CrossRef] [PubMed]
- Ergunay, K.; Ayhan, N.; Charrel, R.N. Novel and emergent sandfly-borne phleboviruses in Asia Minor: A systematic review. Rev. Med. Virol. 2017, 27, e1898. [Google Scholar] [CrossRef] [PubMed]
- Ayhan, N.; Charrel, R.N. An update on Toscana virus distribution, genetics, medical and diagnostic aspects. Clin. Microbiol. Infect. 2020, 26, 1017–1023. [Google Scholar] [CrossRef]
- Marklewitz, M.; Tchouassi, D.P.; Hieke, C.; Heyde, V.; Torto, B.; Sang, R.; Junglen, S. Insights into the evolutionary origin of Mediterranean sand fly fever viruses. MSphere 2020, 5, e00598-20. [Google Scholar] [CrossRef]
- Abudurexiti, A.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Avsic-Zupanc, T.; Ballinger, M.J.; Bente, D.A.; Beer, M.; Bergeron, E.; Blair, C.D.; et al. Taxonomy of the order Bunyavirales: Update 2019. Arch. Virol. 2019, 164, 1949–1965. [Google Scholar] [CrossRef]
- Maes, P.; Alkhovsky, S.V.; Bao, Y.; Beer, M.; Birkhead, M.; Briese, T.; Buchmeier, M.J.; Calisher, C.H.; Charrel, R.N.; Choi, I.R.; et al. Taxonomy of the family Arenaviridae and the order Bunyavirales: Update 2018. Arch. Virol. 2018, 163, 2295–2310. [Google Scholar] [CrossRef]
- Lambert, A.J.; Hughes, H.R. Clinically Important Phleboviruses and Their Detection in Human Samples. Viruses 2021, 13, 1500. [Google Scholar] [CrossRef]
- Polat, C.; Ayhan, N.; Saygan, M.B.; Karahan, S.; Charrel, R.; Ergünay, K. Comprehensive Cross-Sectional Evaluation of Human Sandfly-Borne Phlebovirus Exposure in an Endemic Region. Viruses 2023, 15, 1902. [Google Scholar] [CrossRef]
- Alkan, C.; Bichaud, L.; de Lamballerie, X.; Alten, B.; Gould, E.A.; Charrel, R.N. Sandfly-borne phleboviruses of Eurasia and Africa: Epidemiology, genetic diversity, geographic range, control measures. Antivir. Res. 2013, 100, 54–74. [Google Scholar] [CrossRef]
- Fares, W.; Charrel, R.N.; Dachraoui, K.; Bichaud, L.; Barhoumi, W.; Derbali, M.; Cherni, S.; Chelbi, I.; de Lamballerie, X.; Zhioua, E. Infection of sand flies collected from different bio-geographical areas of Tunisia with phleboviruses. Acta Trop. 2015, 141, 1–6. [Google Scholar] [CrossRef]
- Dachraoui, K.; Fares, W.; Bichaud, L.; Barhoumi, W.; Beier, J.C.; Derbali, M.; Cherni, S.; Lamballerie, X.; Chelbi, I.; Charrel, R.N.; et al. Phleboviruses associated with sand flies in arid bio-geographical areas of Central Tunisia. Acta Trop. 2016, 158, 13–19. [Google Scholar] [CrossRef]
- Tezcan, S.; Dincer, E.; Ulger, M.; Ozgur, D.; Erdogan, S.; Ozkul, A.; Emekdas, G.; Ergunay, K. Serological investigation of phlebovirus exposure in blood donors from the Mediterranean Province of Mersin, Turkey. Mikrobiyol. Bul. 2015, 49, 403–413. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ergunay, K.; Aydogan, S.; Ilhami Ozcebe, O.; Cilek, E.E.; Hacioglu, S.; Karakaya, J.; Ozkul, A.; Us, D. Toscana virus (TOSV) exposure is confirmed in blood donors from Central, North and South/Southeast Anatolia, Turkey. Zoonoses Public Health 2012, 59, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Elliott, R.M.; Brennan, B. Emerging phleboviruses. Curr. Opin. Virol. 2014, 5, 50–57. [Google Scholar] [CrossRef]
- Ergunay, K.; Saygan, M.B.; Aydogan, S.; Lo, M.M.; Weidmann, M.; Dilcher, M.; Sener, B.; Hascelik, G.; Pinar, A.; Us, D. Sandfly fever virus activity in central/northern Anatolia, Turkey: First report of Toscana virus infections. Clin. Microbiol. Infect. 2011, 17, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Es-sette, N.; Ajaoud, M.; Anga, L.; Mellouki, F.; Lemrani, M. Toscana virus isolated from sandflies, Morocco. Parasit. Vectors 2015, 8, 205. [Google Scholar] [CrossRef]
- Alkan, C.; Allal-Ikhlef, A.B.; Alwassouf, S.; Baklouti, A.; Piorkowski, G.; de Lamballerie, X.; Izri, A.; Charrel, R.N. Virus isolation, genetic characterization and seroprevalence of Toscana virus in Algeria. Clin. Microbiol. Infect. 2015, 21, 1040.e1–1040.e9. [Google Scholar] [CrossRef]
- Sakhria, S.; Alwassouf, S.; Fares, W.; Bichaud, L.; Dachraoui, K.; Alkan, C.; Zoghlami, Z.; de Lamballerie, X.; Zhioua, E.; Charrel, R.N. Presence of sandfly-borne phleboviruses of two antigenic complexes (Sandfly fever Naples virus and Sandfly fever Sicilian virus) in two different bio-geographical regions of Tunisia demonstrated by a microneutralisation-based seroprevalence study in dogs. Parasit. Vectors 2014, 7, 476. [Google Scholar]
- Dachraoui, K.; Chelbi, I.; Ben Said, M.; Ben Osman, R.; Cherni, S.; Charrel, R.; Zhioua, E. Transmission Dynamics of Punique Virus in Tunisia. Viruses 2022, 14, 904. [Google Scholar] [CrossRef] [PubMed]
- Benbetka, C.; Hachid, A.; Benallal, K.E.; Khardine, F.A.; Ayhan, N.; Bouredjoul, N.; Boulehbal, W.M.; Bellila, D.; Khaldi, A.; Charrel, R. Epidemiology, Isolation, and Genetic Characterization of Toscana Virus in Algerian Patients Displaying Neurological Infection, 2016–2018. IJID Reg. 2023, 7, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Sellali, S.; Lafri, I.; Ayhan, N.; Medrouh, B.; Messahel, N.E.; Lafri, M.; Charrel, R.; Bitam, I. Neutralizing based seroprevalence study of Toscana virus in livestock from Algeria. Comp. Immunol. Microbiol. Infect. Dis. 2023, 103, 102075. [Google Scholar] [CrossRef] [PubMed]
- Daoudi, M.; Romeo, G.; Marzani, K.; Petrella, A.; Bonilauri, P.; Lelli, D.; Boumezzough, A.; Boussaa, S.; Dottori, M.; Calzolari, M. New Isolation of Ponticelli III Virus (Bunyavirales: Phenuiviridae) in Emilia-Romagna Region, Italy. Viruses 2023, 15, 422. [Google Scholar] [CrossRef] [PubMed]
- Calzolari, M.; Russo, S.; Marzani, K.; Dalmonte, G.; Ricchi, M.; Bonilauri, P. Development of a real-time PCR assay for the detection of the phlebovirus fermo virus. Viruses 2023, 15, 2082. [Google Scholar] [CrossRef]
- Tesh, R.B.; Saidi, S.; Gajdamovic, S.J.; Rodhain, F.; Vesenjak-Hirjan, J. Serological studies on the epidemiology of sandfly fever in the Old World. Bull. World Health Organ. 1976, 54, 663–674. [Google Scholar]
- Ergünay, K.; Polat, C.; Özkul, A. Vector-Borne Viruses in Turkey: A Systematic Review and Bibliography. Antivir. Res. 2020, 183, 104934. [Google Scholar] [CrossRef]
- Calzolari, M.; Romeo, G.; Callegari, E.; Bonilauri, P.; Chiapponi, C.; Carra, E.; Rugna, G.; Taddei, R.; Lelli, D.; Dottori, M. Co-circulation of phleboviruses and Leishmania parasites in sand flies from a single site in Italy monitored between 2017 and 2020. Viruses 2021, 13, 1660. [Google Scholar] [CrossRef]
- Amaro, F.; Zé-Zé, L.; Alves, M.J. Sandfly-Borne Phleboviruses in Portugal: Four and Still Counting. Viruses 2022, 14, 1768. [Google Scholar] [CrossRef]
- Nasiri, Z.; Kalantari, M.; Amin, M.; Daliri, S.; Azizi, K. Phleboviruses (Family: Phenuiviridae) Worldwide, with Emphasis on the Middle East: A Systematic Review Study. J. Health Sci. Surveill. Syst. 2023, 11, 408–417. [Google Scholar]
- Izri, A.; Temmam, S.; Moureau, G.; Hamrioui, B.; De Lamballerie, X.; Charrel, R.N. Sandfly fever Sicilian virus, Algeria. Emerg. Infect. Dis. 2008, 14, 795. [Google Scholar] [CrossRef] [PubMed]
- Moureau, G.; Bichaud, L.; Salez, N.; Ninove, L.; Hamrioui, B.; Belazzoug, S.; De Lamballerie, X.; Izri, A.; Charrel, R.N. Molecular and serological evidence for the presence of novel phleboviruses in sandflies from northern Algeria. Open Virol. J. 2010, 4, 15. [Google Scholar] [CrossRef] [PubMed]
- Sellali, S.; Lafri, I.; Hachid, A.; Ayhan, N.; Benbetka, C.; Medrouh, B.; Messahel, N.E.; Bekara, M.A.; Lafri, M.; Charrel, R.N.; et al. Presence of the sandfly-borne phlebovirus (Toscana virus) in different bio-geographical regions of Algeria demonstrated by a microneutralisation-based seroprevalence study in owned dogs. Comp. Immunol. Microbiol. Infect. Dis. 2022, 88, 101861. [Google Scholar] [CrossRef] [PubMed]
- Tahir, D.; Alwassouf, S.; Loudahi, A.; Davoust, B.; Charrel, R.N. Seroprevalence of Toscana virus in dogs from Kabylia (Algeria). Clin. Microbiol. Infect. 2016, 22, e16–e17. [Google Scholar] [CrossRef] [PubMed]
- Manseur, H.; Hachid, A.; Khardine, A.F.; Benallal, K.E.; Bia, T.; Temani, M.; Hakem, A.; Sánchez-Seco, M.P.; Bitam, I.; Vázquez, A.; et al. First Isolation of Punique Virus from Sand Flies Collected in Northern Algeria. Viruses 2022, 14, 1796. [Google Scholar] [CrossRef]
- Es-Sette, N.; Nourlil, J.; Hamdi, S.; Mellouki, F.; Lemrani, M. First Detection of Toscana Virus RNA From Sand Flies in the Genus Phlebotomus (Diptera: Phlebotomidae) Naturally Infected in Morocco. J. Med. Entomol. 2012, 49, 1507–1509. [Google Scholar] [CrossRef]
- Es-Sette, N.; Ajaoud, M.; Bichaud, L.; Hamdi, S.; Mellouki, F.; Charrel, R.N.; Lemrani, M. Phlebotomus sergenti a common vector of Leishmania tropica and Toscana virus in Morocco. J. Vector Borne Dis. 2014, 51, 86–90. [Google Scholar]
- Es-Sette, N.; Ajaoud, M.; Charrel, R.N.; Lemrani, M. Epidemiologie moleculaire des phlebovirus dans quatre provinces du Maroc. Bull. Soci. Pathol. Exot. 2016, 109, 143–150. [Google Scholar] [CrossRef]
- Chastel, C.; Launay, H.; Bailly-Choumara, H.; Le Lay, G.; Beaucournu, J.C. Arbovirus infections in Morocco: Serosurvey in small wild mammals in the northern part of the country. Bull Soc. Pathol. Exot. Filiales. 1982, 75, 466–475. [Google Scholar]
- Chastel, C.; Bach-Hamba, D.; Launay, H.; Le Lay, G.; Hellal, H.; Beaucournu, J.C. Arbovirus infections in Tunisia: New serological survey of small wild mammals. Bull. Soc. Pathol. Exot. Filiales. 1983, 76, 21–33. [Google Scholar]
- Zhioua, E.; Moureau, G.; Chelbi, I.; Ninove, L.; Bichaud, L.; Derbali, M.; Champs, M.; Cherni, S.; Salez, N.; Cook, S.; et al. Punique virus, a novel phlebovirus, related to sandfly fever Naples virus, isolated from sand flies collected in Tunisia. J. Gen. Virol. 2010, 91, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Fezaa, O.; M’ghirbi, Y.; Savellini, G.G.; Ammari, L.; Hogga, N.; Triki, H.; Cusi, M.G.; Bouattour, A. Serological and molecular detection of Toscana and other Phleboviruses in patients and sandflies in Tunisia. BMC Infect. Dis. 2014, 14, 598. [Google Scholar] [CrossRef] [PubMed]
- Ayari, R.; Chaouch, H.; Findlay-Wilson, S.; Hachfi, W.; Ben Lasfar, N.; Bellazreg, F.; Dowall, S.; Hannachi, N.; Letaief, A. Seroprevalence and Risk Factors Associated with Phleboviruses and Crimean–Congo Hemorrhagic Fever Virus among Blood Donors in Central Tunisia. Pathogens 2024, 13, 348. [Google Scholar] [CrossRef] [PubMed]
- Bichaud, L.; Dachraoui, K.; Piorkowski, G.; Chelbi, I.; Moureau, G.; Cherni, S.; De Lamballerie, X.; Sakhria, S.; Charrel, R.N.; Zhioua, E. Toscana virus isolated from sandflies, Tunisia. Emerg. Infect. Dis. 2013, 19, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Sakhria, S.; Bichaud, L.; Mensi, M.; Salez, N.; Dachraoui, K.; Thirion, L.; Cherni, S.; Chelbi, I.; de Lamballerie, X.; Zhioua, E.; et al. Co-Circulation of Toscana virus and Punique virus in Northern Tunisia using a microneutralization-based serological study. PLoS Negl. Trop. Dis. 2013, 7, 2429. [Google Scholar] [CrossRef]
- Bahri, O.; Fazaa, O.; Ben Alaya-Bouafif, N.; Bouloy, M.; Triki, H.; Bouattour, A. Role of Toscana virus in meningo-encephalitis in Tunisia. Pathol. Biol. 2011, 59, e125–e127. [Google Scholar]
- Sghaier, W.; Bahri, O.; Kedous, E.; Fazaa, O.; Rezig, D.; Touzi, H.; Ben Yahia, A.; Meddeb, Z.; Triki, H. Retrospective study of viral causes of central nervous system infections in Tunisia (2003–2009). Med. Sante Trop. 2012, 22, 373–378. [Google Scholar] [CrossRef]
- Fares, W.; Dachraoui, K.; Barhoumi, W.; Cherni, S.; Chelbi, I.; Zhioua, E. Co-circulation of Toscana virus and Leishmania infantum in a focus of zoonotic visceral leishmaniasis from Central Tunisia. Acta Trop. 2020, 204, 105342. [Google Scholar] [CrossRef]
- Bichaud, L.; Dachraoui, K.; Alwassouf, S.; Alkan, C.; Mensi, M.; Piorkowski, G.; Sakhria, S.; Seston, M.; Fares, W.; De Lamballerie, X.; et al. Isolation, full genomic characterization and neutralization-based human seroprevalence of Medjerda Valley virus, a novel sandfly-borne phlebovirus belonging to the Salehabad virus complex in northern Tunisia. J. Gen. Virol. 2016, 97, 602–610. [Google Scholar] [CrossRef]
- Elahmer, O.R.; Abdelfadeel, M.; Safwat, S.; Smeo, M.N.; Abudher, A.; Sammoud, M.A. A retrospective study to define viral and bacterial etiologies causing acute febrile illness in Libya. In Proceedings of the Conference of Endemic and Emerging Infectious Diseases of Priority in the Middle East and North Africa—Research Opportunities and Biosafety in a Changing Environment, Istanbul, Turkey, 18–21 June 2012. [Google Scholar]
- Saadawi, W.K.; Abozaid, F.D.; Almukhtar, M.; Annajar, B.B.; Shaibi, T. Seroprevalence study of Toscana virus in Yafran area, Libya. J. Vector Borne Dis. 2022, 59, 186–189. [Google Scholar] [CrossRef]
- Schmidt, J.R.; Schmidt, M.L.; Said, M.I. Phlebotomus fever in Egypt. Isolation of phlebotomus fever viruses from Phlebotomus papatasi. Am. J. Trop. Med. Hyg. 1971, 20, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Pierro, A.; Ficarelli, S.; Ayhan, N.; Morini, S.; Raumer, L.; Bartoletti, M.; Mastroianni, A.; Prati, F.; Schivazappa, S.; Cenni, P.; et al. Characterization of antibody response in neuroinvasive infection caused by Toscana virus. Clin. Microbiol. Infect. 2017, 23, 868–873. [Google Scholar] [CrossRef] [PubMed]
- Ayhan, N.; Rodríguez-Teijeiro, J.D.; López-Roig, M.; Vinyoles, D.; Ferreres, J.A.; Monastiri, A.; Charrel, R.N.; Serra-Cobo, J. High rates of antibodies against Toscana and Sicilian phleboviruses in common quail Coturnix coturnix birds. Front. Microbiol. 2023, 13, 1091908. [Google Scholar] [CrossRef] [PubMed]
- Benallal, K.E.; Garni, R.; Harrat, Z.; Volf, P.; Dvorak, V. Phlebotomine sand flies (Diptera: Psychodidae) of the Maghreb region: A systematic review of distribution, morphology, and role in the transmission of the pathogens. PLoS Negl. Trop. Dis. 2022, 16, e0009952. [Google Scholar] [CrossRef] [PubMed]
- Munoz, C.; Ayhan, N.; Ortuno, M.; Ortiz, J.; Gould, E.A.; Maia, C.; Berriatua, E.; Charrel, R.N. Experimental Infection of Dogs with Toscana Virus and Sandfly Fever Sicilian Virus to Determine Their Potential as Possible Vertebrate Hosts. Microorganisms 2020, 8, 596. [Google Scholar] [CrossRef]
- Tchouassi, D.P.; Marklewitz, M.; Chepkorir, E.; Zirkel, F.; Agha, S.B.; Tigoi, C.C.; Koskei, E.; Drosten, C.; Borgemeister, C.; Torto, B.; et al. Sand fly–associated Phlebovirus with evidence of neutralizing antibodies in humans, Kenya. Emerg. Infect. Dis. 2019, 25, 681. [Google Scholar] [CrossRef]
- Calzolari, M.; Chiapponi, C.; Bellini, R.; Bonilauri, P.; Lelli, D.; Moreno, A.; Barbieri, I.; Pongolini, S.; Lavazza, A.; Dottori, M. Isolation of three novel reassortant phleboviruses, Ponticelli I, II, III, and of Toscana virus from field-collected sand flies in Italy. Parasites Vectors 2018, 11, 84. [Google Scholar] [CrossRef]
- Lelli, D.; Scanferla, V.; Moreno, A.; Sozzi, E.; Ravaioli, V.; Renzi, M.; Tosi, G.; Dottori, M.; Lavazza, A.; Calzolari, M. Serological evidence of phleboviruses in domestic animals on the pre-Apennine Hills (northern Italy). Viruses 2021, 13, 1577. [Google Scholar] [CrossRef]
- Dersch, R.; Sophocleous, A.; Cadar, D.; Emmerich, P.; Schmidt-Chanasit, J.; Rauer, S. Toscana virus encephalitis in Southwest Germany: A retrospective study. BMC Neurol. 2021, 21, 495. [Google Scholar] [CrossRef]
- Malik, M.; Mafi, A.; Mahjour, J.; Opoka, M.; Elhakim, M.; Muntasir, M.O. Novel coronavirus infection in the Eastern Mediterranean Region: Time to act. East Mediterr. Health J. 2013, 19, S31–S38. [Google Scholar] [CrossRef]
- Kniha, E.; Obwaller, A.G.; Dobler, G.; Poeppl, W.; Mooseder, G.; Walochnik, J. Phlebovirus seroprevalence in Austrian Army personnel returning from missions abroad. Parasites Vectors 2019, 12, 416. [Google Scholar] [CrossRef] [PubMed]
- Al-Numaani, S.A.; Al-Nemari, A.T.; El-Kafrawy, S.A.; Hassan, A.M.; Tolah, A.M.; Alghanmi, M.; Zawawi, A.; Masri, B.E.; Hindawi, S.I.; Alandijany, T.A.; et al. Seroprevalence of Toscana and sandfly fever Sicilian viruses in humans and livestock animals from western Saudi Arabia. One Health 2023, 17, 100601. [Google Scholar] [CrossRef] [PubMed]
- Feinsod, F.M.; Ksiazek, T.G.; Scott, R.M.; Soliman, A.K.; Farrag, I.H.; Ennis, W.H.; Peters, C.J.; El Said, S.; Darwish, M.A. Sand fly fever-Naples infection in Egypt. Am. J. Trop. Med. Hyg. 1987, 37, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Darwish, M.A.; Feinsod, F.M.; Scott, R.M.; Ksiazek, T.G.; Botros, B.A.; Farrag, I.H.; El Said, S. Arboviral causes of non-specific fever and myalgia in a fever hospital patient population in Cairo. Egypt. Trans. R. Soc. Trop. Med. Hyg. 1987, 81, 1001–1003. [Google Scholar] [CrossRef]
- Corwin, A.; Habib, M.; Watts, D.; Darwish, M.; Olson, J.; Botros, B.; Hibbs, R.; Kleinosky, M.; Lee, H.W.; Shope, R.; et al. Community-based prevalence profile of arboviral, rickettsial, and Hantaan-like viral antibody in the Nile River Delta of Egypt. Am. J. Trop. Med. Hyg. 1993, 48, 776–783. [Google Scholar] [CrossRef]
- Darwish, M.A.; Ibrahim, A.H. Prevalence of antibodies to arboviruses in Egypt. Results of a serological survey among 1,113 university students. Am. J. Trop. Med. Hyg. 1975, 24, 981–985. [Google Scholar] [CrossRef]
- Corwin, A.; Habib, M.; Olson, J.; Scott, D.; Ksiazek, T.; Watts, D.M. The prevalence of arboviral, rickettsial, and Hantaan-like viral antibody among schoolchildren in the Nile river delta of Egypt. Trans. R. Soc. Trop. Med. Hyg. 1992, 86, 677–679. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sellali, S.; Lafri, I.; Garni, R.; Manseur, H.; Besbaci, M.; Lafri, M.; Bitam, I. Epidemiology of Sandfly-Borne Phleboviruses in North Africa: An Overview. Insects 2024, 15, 846. https://doi.org/10.3390/insects15110846
Sellali S, Lafri I, Garni R, Manseur H, Besbaci M, Lafri M, Bitam I. Epidemiology of Sandfly-Borne Phleboviruses in North Africa: An Overview. Insects. 2024; 15(11):846. https://doi.org/10.3390/insects15110846
Chicago/Turabian StyleSellali, Sabrina, Ismail Lafri, Rafik Garni, Hemza Manseur, Mohamed Besbaci, Mohamed Lafri, and Idir Bitam. 2024. "Epidemiology of Sandfly-Borne Phleboviruses in North Africa: An Overview" Insects 15, no. 11: 846. https://doi.org/10.3390/insects15110846
APA StyleSellali, S., Lafri, I., Garni, R., Manseur, H., Besbaci, M., Lafri, M., & Bitam, I. (2024). Epidemiology of Sandfly-Borne Phleboviruses in North Africa: An Overview. Insects, 15(11), 846. https://doi.org/10.3390/insects15110846





