Prospective Lymphedema Surveillance in a Clinic Setting
Abstract
:1. Introduction
1.1. Background and Significance
2. Review of Literature
2.1. Prospective Surveillance Model
2.1.1. Lymphedema Breast Cancer Questionnaire Tool
2.1.2. Limb Measurements
2.1.3. Cost
3. Results
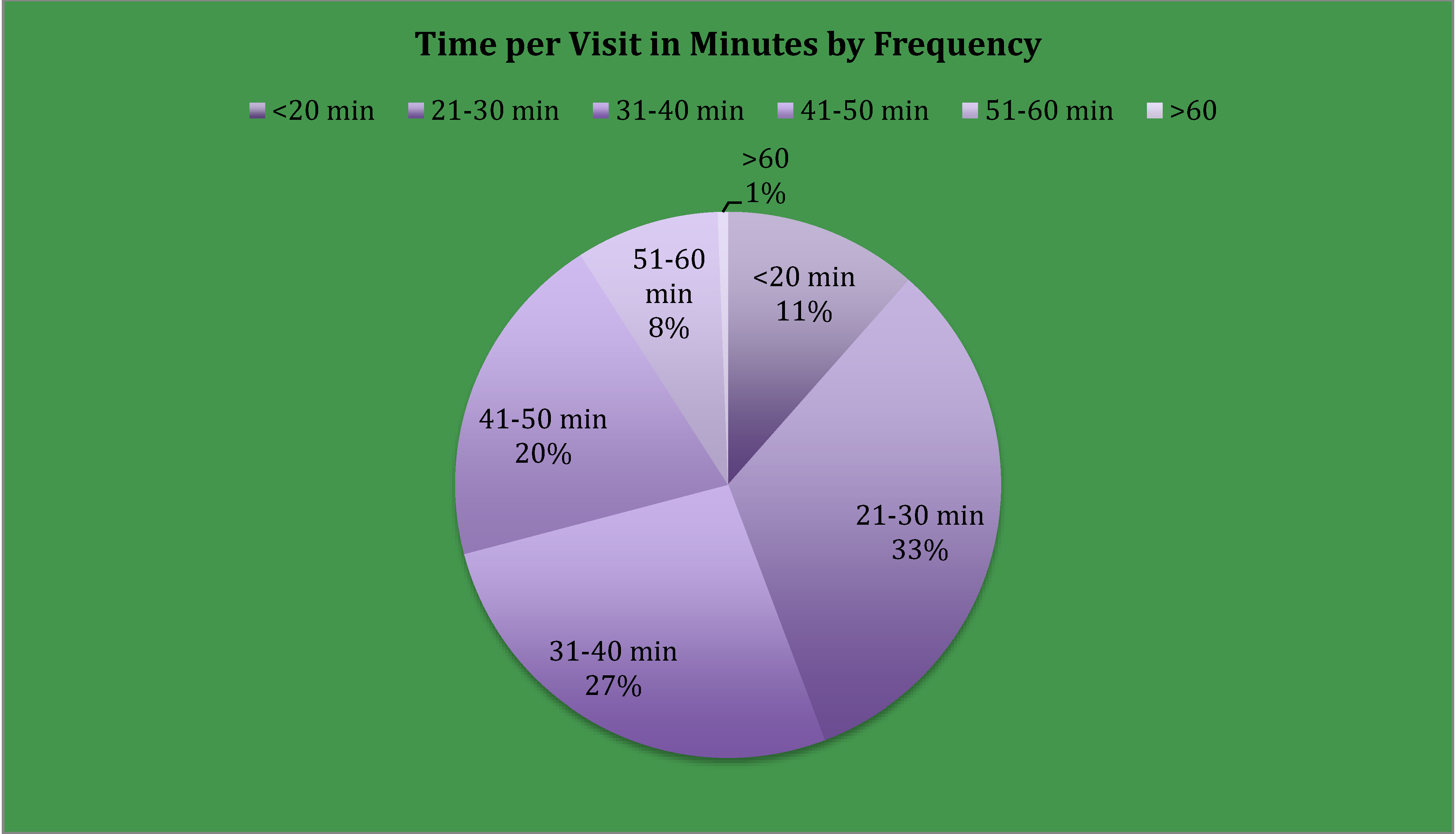
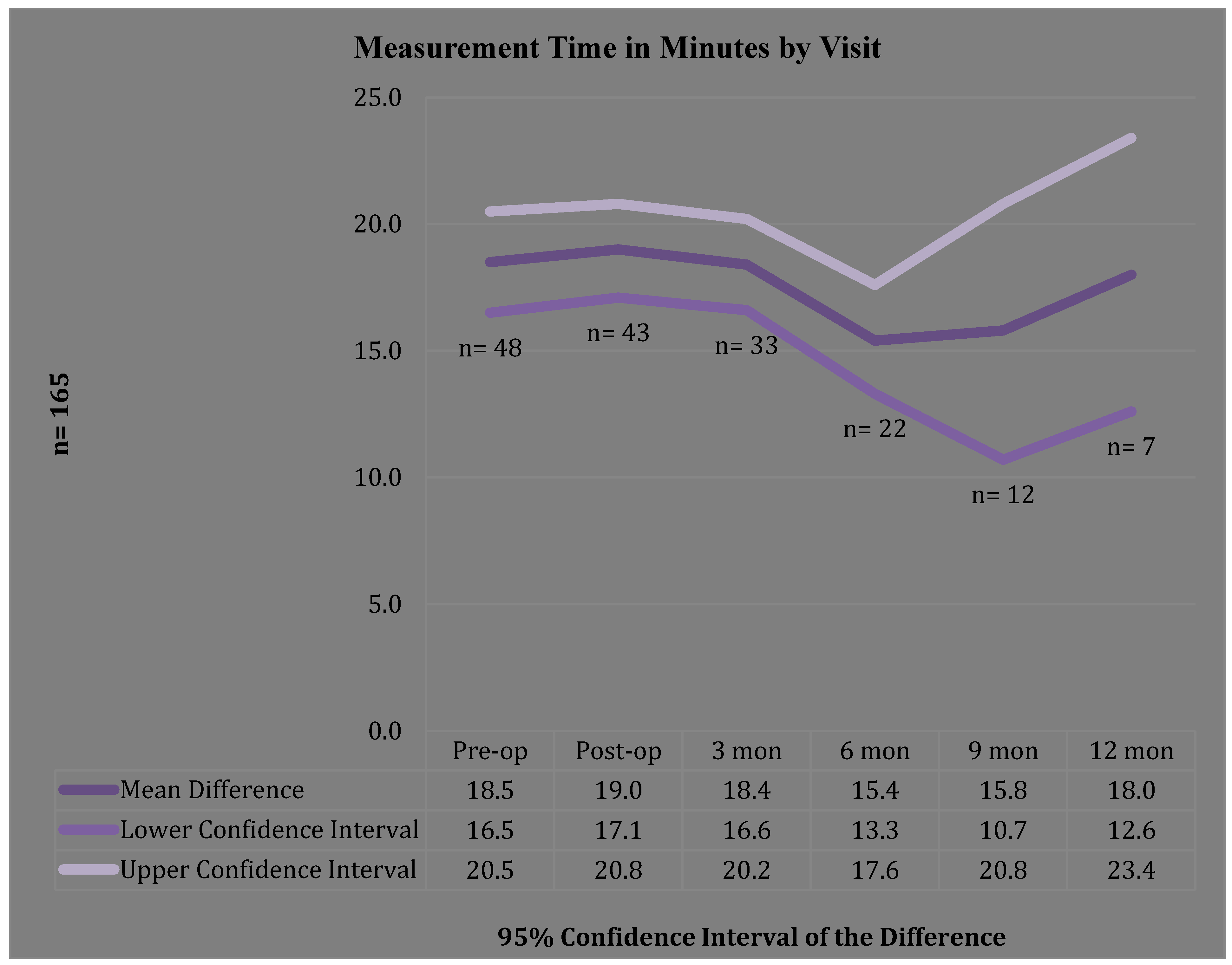
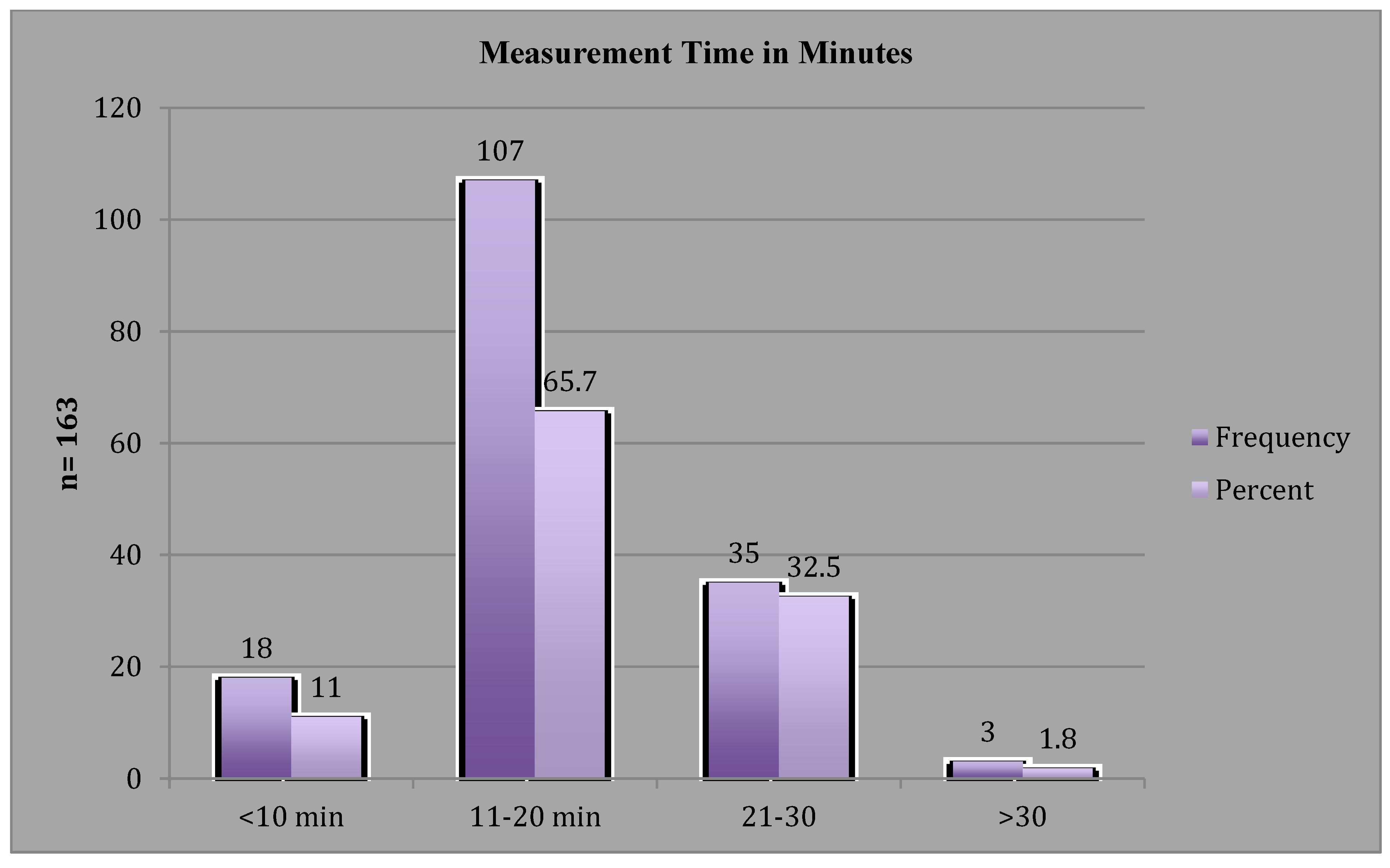
3.1. Clinic Time
3.2. Referral to LE Management
| Referral * Symptoms Crosstabulation | ||||
|---|---|---|---|---|
| Valid Number of responses = 115 | ||||
| No Symptoms | LBCQ Sym | LVI = 5% | Both LBCQ/LVI | |
| n | 85(73.9%) | 17(14.8%) | 13(11.3%) | 9(7.8%) |
| Referral No | 85 | 16 | 11 | 3 |
| Referral Yes | 0 | 1 | 2 | 6 |
| % not Referred | 100.0% | 94.1% | 84.6% | 33.3% |
| % Referred | 0% | 5.9% | 15.4% | 67.0% |
| Chi-Square Test | ||||
| Asymp. Sig | Exact Sig | |||
| Pearson Chi-Square | p = 0.000 | p = 0.000 | ||
3.3. Treatment Costs
4. Discussion
Limitations
5. Materials and Methods
- Sequential bilateral circumferential limb measurements, obtained during clinic visits preoperatively, and at 3-, 6-, 9-, 12-months postoperatively;
- Self-report symptoms assessments, obtained using the LBCQ tool by interview or patient entry into the web-based survey, obtained during clinic visits preoperatively, and at 3-, 6-, 9-, 12-months postoperatively, and FACT B+4 quality of life questionnaire, obtained preoperatively and 12-months postoperatively, and participant satisfaction with electronic capture of symptoms obtained at 12-months postoperatively;
- Referral point to LE specialist for assessment in patients presenting with a 5% LVI over baseline and/or reports of arm ‘feeling heavy’ in the past year, or ‘swelling now’ per the LBCQ tool;
- Nursing time required for the assessment (assessment start and stop times), inclusive of completion of LBCQ tool and circumferential measurements; and
- Institutional billed charges; comparisons were analyzed between a patient referred for treatment at the LE Surveillance parameter of ≥5% and <10% LVI versus a patient referred per the traditional parameter of ≥10% LVI.
Limb Measurements
6. Inclusion Criteria
7. Conclusions
8. Future Directions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- American Cancer Society. Breast Cancer Facts & Figures 2013–2014; America Cancer Society: Atlanta, GA, USA. Available online: http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-042725.pdf (accessed on 14 October 2014).
- Armer, J.M.; Stewart, B.R. A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat. Res. Biol. 2005, 3, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Armer, J.M.; Radina, M.E.; Porock, D.; Culbertson, S.D. Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs. Res. 2003, 52, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Poage, E.; Singer, M.; Armer, J.; Poundall, M.; Shellabarger, M.J. Demystifying lymphedema: Development of the lymphedema putting evidence into practice card. Clin. J. Oncol. Nurs. 2008, 12, 951–964. [Google Scholar] [CrossRef] [PubMed]
- Dell, D.D.; Doll, C. Caring for a patient with lymphedema. Nursing 2006, 6, 49–51. [Google Scholar] [CrossRef]
- Petrak, J.A.; Heelan, M.C. Incidence of breast carcinoma-related lymphedema. Cancer 1998, 83, 2776–2781. [Google Scholar] [CrossRef]
- Fu, M.R.; Ridner, S.H.; Armer, J.M. Post-breast cancer lymphedema: Part 2. Am. J. Nurs. 2009, 109, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Norman, S.A.; Localio, A.R.; Potashnik, S.L.; Torpey, H.A.S.; Kallan, M.J.; Weber, A.L.; Miller, L.T.; DeMichele, A.; Solin, L.J. Lymphedema in breast cancer survivors: Incidence, degree, time course, treatment, and symptoms. J. Clin. Oncol. 2009, 27. [Google Scholar] [CrossRef] [PubMed]
- Armer, J.M.; Heckathorn, P.W. Post-breast cancer lymphedema in aging women: Self-management and implicationsfornursing. J. Gerontol. Nurs. 2005, 31, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Boccardo, F.M.; Ansaldi, F.; Bellini, C.; Accogli, S.; Taddei, G.; Murdaca, G.; Campisi, C.C.; Villa, G.; Icardi, G.; Durando, P.; et al. Prospective evaluation of a prevention protocol for lymphedema following surgery for breast cancer. Lymphology 2009, 42, 1–9. [Google Scholar] [PubMed]
- Armer, J.M.; Shook, R.P.; Schneider, M.K.; Brooks, C.W.; Peterson, J.; Stewart, B.R. Enhancing supportive-educative nursing systems to reduce risk of post-breast cancer lymphedema. Self-Care Dependent Care Nurs. 2009, 17, 6–15. [Google Scholar]
- Lawenda, B.D.; Mondry, T.E.; Johnstone, P.A.S. Lymphedema: A primer on the identification and management of a chronic condition in oncologic treatment. CA Cancer J. Clin. 2009, 59, 2–24. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Johansson, K.; Stout, N.L.; Prosnitz, R.; Armer, J.M.; Gabram, S.; Schmitz, K.H. Upper-body morbidity after breast cancer: Incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer 2012, 118, S2237–S2249. [Google Scholar] [CrossRef] [PubMed]
- McWayne, J.; Heiney, S.P. Psychologic and social sequelae of secondary lymphedema: A review. Cancer 2005, 104, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Armer, J.M. The problem of post-breast cancer lymphedema: Impact and measurement. Cancer Investig. 2005, 23, 76–83. [Google Scholar] [CrossRef]
- Stout, N.L.; Pfalzer, L.A.; Springer, B.; Levy, E.; McGarvey, C.L.; Danoff, J.V.; Gerber, L.H.; Soballe, P.W. Breast cancer-related lymphedema: Comparing direct costs of a prospective surveillance model and a traditional model of care. Phys. Ther. 2012, 92, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Cormier, J.N.; Xing, Y.; Zaniletti, I.; Askew, R.L.; Stewart, B.R.; Armer, J.M. Minimal limb volume change has significant impact on breast cancer survivors. Lymphology 2009, 42, 161–175. [Google Scholar] [PubMed]
- Specht, M.C.; Miller, C.L.; Russel, T.A.; Horick, N.; Skolny, M.N.; O’Toole, J.A.; Jammallo, L.S.; Niemierko, A.; Sadek, B.T.; Shenouda, M.N.; et al. Defining a threshold for intervention in breast cancer-related lymphedema: What level of arm volume increase predicts progression? Breast Cancer Res. Treat 2013, 140, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Armer, J.M.; Stewart, B.R.; Smith, K.M.; Cormier, J.N. Lymphedema Following Cancer Treatment. In Cancer Rehabilitation and Survivorship: Transdisciplinary Approaches to Personalized Care; Lester, J.L., Schmitt, P., Eds.; Oncology Nursing Society: Pittsburgh, PA, USA, 2011. [Google Scholar]
- Czerniec, S.A.; Ward, L.C.; Refshauge, K.M.; Beith, J.; Lee, M.J.; York, S.; Kilbreath, S.L. Assessment of breast cancer-related arm lymphedema-comparison of physical measurement methods and self-report. Cancer Investig. 2010, 28, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Bulley, C.; Gaal, S.; Coutts, F.; Blyth, C.; Jack, W.; Chetty, U.; Barber, M.; Tan, C.-W. Comparison of breast cancer-related lymphedema (upper limb swelling) prevalence estimated using objective and subjective criteria and relationship with quality of life. BioMed. Res. Int. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Singh, C.; de Vera, M.; Campbell, K.L. The effect of prospective monitoring and early physiotherapy intervention on arm morbidity following surgery for breast cancer: A pilot study. Physiother. Can. 2013, 65, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Stout-Gergich, N.L.; Pfalzer, L.A.; McGarvery, C.; Springer, B.; Gerber, L.H.; Soballe, P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 2008, 112, 2809–2819. [Google Scholar] [CrossRef] [PubMed]
- Binkley, J.M.; Harris, S.R.; Levangie, P.K.; Pearl, M.; Guglielmino, J.; Kraus, V.; Rowden, D. Patient perspectives on breast cancer treatment side effects and prospective surveillance model for physical rehabilitation for women with breast cancer. Cancer 2012, 118, S2207–S2016. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Troxel, A.B.; Basford, J.R.; Kornblith, A.B. Prevalence and treatment patterns of physical impairments in patients with metastatic breast cancer. J. Clin. Oncol. 2008, 26, 2621–2629. [Google Scholar] [CrossRef] [PubMed]
- Armer, J.M.; Whitman, M. The problem of lymphedema following breast cancer treatment: Prevalence, symptoms, and self-management. Lymphology 2002, 35, S153–S159. [Google Scholar]
- Gartner, R.; Jensen, M.B.; Kronborg, I.; Ewertz, M.; Kehlet, H.; Kroman, N. Self-reported arm-lymphedema and functional impairment after breast cancer treatment—A nationwide study of prevalence and associated factors. Breast 2010, 19, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Keast, D.H.; Despatis, M.; Allen, J.O.; Brassard, A. Chronioedema/lymphedema: Under recognized and under-treated. Int. Wound J. 2014. [Google Scholar] [CrossRef]
- Shih, Y.C.; Xu, Y.; Cormier, J.N.; Giordano, S.; Ridner, S.H.; Buchholz, T.A.; Perkins, G.H.; Elting, L.S. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: A 2-year follow-up study. J. Clin. Oncol. 2009, 27, 2007–2014. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, C.J.; Franks, P.J.; Doherty, D.; Williams, A.F.; Badger, C.; Jeffs, E.; Bosanquet, N.; Mortimer, P.S. Lymphoedema: An underestimated health problem. Q. J. Med. 2003, 96, 731–738. [Google Scholar] [CrossRef]
- National Lymphedema Network Position Statement on Screening and Measurement for Early Detection of Breast Cancer-Related Lymphedema. Available online: http://www.lymphnet.org/pdfdocs/nlnbcle.pdf (accessed on 5 January 2015).
- IBM Corp. IBM SPSS Statistics for Windows; Version 21.0; IBM Corp: Armonk, NY, USA, 2012. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chance-Hetzler, J.; Armer, J.; Van Loo, M.; Anderson, B.; Harris, R.; Ewing, R.; Stewart, B. Prospective Lymphedema Surveillance in a Clinic Setting. J. Pers. Med. 2015, 5, 311-325. https://doi.org/10.3390/jpm5030311
Chance-Hetzler J, Armer J, Van Loo M, Anderson B, Harris R, Ewing R, Stewart B. Prospective Lymphedema Surveillance in a Clinic Setting. Journal of Personalized Medicine. 2015; 5(3):311-325. https://doi.org/10.3390/jpm5030311
Chicago/Turabian StyleChance-Hetzler, Janet, Jane Armer, Maggie Van Loo, Blake Anderson, Robin Harris, Rebecca Ewing, and Bob Stewart. 2015. "Prospective Lymphedema Surveillance in a Clinic Setting" Journal of Personalized Medicine 5, no. 3: 311-325. https://doi.org/10.3390/jpm5030311
APA StyleChance-Hetzler, J., Armer, J., Van Loo, M., Anderson, B., Harris, R., Ewing, R., & Stewart, B. (2015). Prospective Lymphedema Surveillance in a Clinic Setting. Journal of Personalized Medicine, 5(3), 311-325. https://doi.org/10.3390/jpm5030311





